Neck Disability Index Is Better in Classification of Recovery after Whiplash Injury in Comparison with Ultrasound Shear Wave Elastography of Trapezius Muscle
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Variables
2.4. Outcomes
2.5. Data Measurement
2.6. Study Size
2.7. Statistical Methods
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spitzer, W.O.; Skovron, M.L.; Salmi, L.R.; Cassidy, J.D.; Duranceau, J.; Suissa, S.; Zeiss, E. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: Redefining “whiplash” and its management. Spine 1995, 20, 1S–73S. [Google Scholar]
- Carroll, L.J.; Holm, L.W.; Hogg-Johnson, S.; Cote, P.; Cassidy, J.D.; Haldeman, S.; Nordin, M.; Hurwitz, E.L.; Carragee, E.J.; van der Velde, G.; et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, S83–S92. [Google Scholar] [CrossRef] [PubMed]
- Holm, L.W.; Carroll, L.J.; Cassidy, J.D.; Hogg-Johnson, S.; Cote, P.; Guzman, J.; Peloso, P.; Nordin, M.; Hurwitz, E.; van der Velde, G.; et al. The burden and determinants of neck pain in whiplash-associated disorders after traffic collisions: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, S52–S59. [Google Scholar] [CrossRef] [PubMed]
- Scholten-Peeters, G.G.; Verhagen, A.P.; Bekkering, G.E.; van der Windt, D.A.; Barnsley, L.; Oostendorp, R.A.; Hendriks, E.J. Prognostic factors of whiplash-associated disorders: A systematic review of prospective cohort studies. Pain 2003, 104, 303–322. [Google Scholar] [CrossRef]
- Sarrami, P.; Armstrong, E.; Naylor, J.M.; Harris, I.A. Factors predicting outcome in whiplash injury: A systematic meta-review of prognostic factors. J. Orthop. Traumatol. 2017, 18, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M. Clinical Guidelines for Best Practice Management of Acute and Chronic Whiplash-Associated Disorders; South Australian Centre for Trauma and Injury Recovery (TRACsa): Adelaide, Australia, 2008. [Google Scholar]
- Ritchie, C.; Hendrikz, J.; Jull, G.; Elliott, J.; Sterling, M. External validation of a clinical prediction rule to predict full recovery and ongoing moderate/severe disability following acute whiplash injury. J. Orthop. Sports Phys. Ther. 2015, 45, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Griffin, A.; Jagnoor, J.; Arora, M.; Cameron, I.D.; Kifley, A.; Sterling, M.; Kenardy, J.; Rebbeck, T. Evidence-based care in high- and low-risk groups following whiplash injury: A multi-centre inception cohort study. BMC Health Serv. Res. 2019, 19, 806. [Google Scholar] [CrossRef]
- Hoving, J.L.; O’Leary, E.F.; Niere, K.R.; Green, S.; Buchbinder, R. Validity of the neck disability index, Northwick Park neck pain questionnaire, and problem elicitation technique for measuring disability associated with whiplash-associated disorders. Pain 2003, 102, 273–281. [Google Scholar] [CrossRef]
- Walton, D.M.; Macdermid, J.C.; Giorgianni, A.A.; Mascarenhas, J.C.; West, S.C.; Zammit, C.A. Risk factors for persistent problems following acute whiplash injury: Update of a systematic review and meta-analysis. J. Orthop. Sports Phys. Ther. 2013, 43, 31–43. [Google Scholar] [CrossRef]
- Bobos, P.; MacDermid, J.C.; Walton, D.M.; Gross, A.; Santaguida, P.L. Patient-Reported Outcome Measures Used for Neck Disorders: An Overview of Systematic Reviews. J. Orthop. Sports Phys. Ther. 2018, 48, 775–788. [Google Scholar] [CrossRef]
- Beltsios, M.; Savvidou, O.; Mitsiokapa, E.A.; Mavrogenis, A.F.; Kaspiris, A.; Efstathopoulos, N.; Papagelopoulos, P.J. Sagittal alignment of the cervical spine after neck injury. Eur. J. Orthop. Surg. Traumatol. 2013, 23 (Suppl. 1), S47–S51. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, P.S.; Evans, P.F.; Wright, V. The straight cervical spine: Does it indicate muscle spasm? J. Bone Jt. Surg. Br. 1994, 76, 103–106. [Google Scholar] [CrossRef]
- Malik, A.A.; Robinson, S.; Khan, W.S.; Dillon, B.; Lovell, M.E. Assessment of Range of Movement, Pain and Disability Following a Whiplash Injury. Open Orthop. J. 2017, 11, 541–545. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Taljanovic, M.S.; Gimber, L.H.; Becker, G.W.; Latt, L.D.; Klauser, A.S.; Melville, D.M.; Gao, L.; Witte, R.S. Shear-Wave Elastography: Basic Physics and Musculoskeletal Applications. Radiographics 2017, 37, 855–870. [Google Scholar] [CrossRef]
- Aljinovic, J.; Barisic, I.; Poljicanin, A.; Kuzmicic, S.; Vukojevic, K.; Gugic Bokun, D.; Vlak, T. Can measuring passive neck muscle stiffness in whiplash injury patients help detect false whiplash claims? Wien Klin. Wochenschr. 2020, 132, 506–514. [Google Scholar] [CrossRef]
- Aljinović, J.; Barun, B.; Poljičanin, A.; Marinović, I.; Vlak, T.; Pivalica, D.; Benzon, B. Croatian version of the neck disability index can distinguish between acute, chronic and no neck pain: Results of a validation study. Wien Klin. Wochenschr. 2021, 9. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284–290. [Google Scholar] [CrossRef]
- Baiocchi, G.; Distaso, W. GRETL: Econometric software for the GNU generation. J. Appl. Econom. 2003, 18, 105–110. [Google Scholar] [CrossRef]
- Blain, M.; Bedretdinova, D.; Bellin, M.F.; Rocher, L.; Gagey, O.; Soubeyrand, M.; Creze, M. Influence of thoracolumbar fascia stretching on lumbar back muscle stiffness: A supersonic shear wave elastography approach. Clin. Anat. 2019, 32, 73–80. [Google Scholar] [CrossRef]
- Chen, B.; Zhao, H.; Liao, L.; Zhang, Z.; Liu, C. Reliability of shear-wave elastography in assessing thoracolumbar fascia elasticity in healthy male. Sci. Rep. 2020, 10, 19952. [Google Scholar] [CrossRef] [PubMed]
- Leong, H.T.; Ng, G.Y.; Leung, V.Y.; Fu, S.N. Quantitative estimation of muscle shear elastic modulus of the upper trapezius with supersonic shear imaging during arm positioning. PLoS ONE 2013, 8, e67199. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, C.L.; Feng, Y.N.; Zhang, H.Q.; Li, Y.P.; Zhu, Y.; Zhang, Z.J. Assessing the viscoelastic properties of upper trapezius muscle: Intra- and inter-tester reliability and the effect of shoulder elevation. J. Electromyogr. Kinesiol. 2018, 43, 226–229. [Google Scholar] [CrossRef] [PubMed]
- Moreau, B.; Vergari, C.; Gad, H.; Sandoz, B.; Skalli, W.; Laporte, S. Non-invasive assessment of human multifidus muscle stiffness using ultrasound shear wave elastography: A feasibility study. Proc. Inst. Mech. Eng. H 2016, 230, 809–814. [Google Scholar] [CrossRef] [PubMed]
- Lallemant-Dudek, P.; Vergari, C.; Dubois, G.; Forin, V.; Vialle, R.; Skalli, W. Ultrasound shearwave elastography to characterize muscles of healthy and cerebral palsy children. Sci. Rep. 2021, 11, 3577. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Yu, J.; Liu, C.; Tang, C.; Zhang, Z. Modulation in Elastic Properties of Upper Trapezius with Varying Neck Angle. Appl. Bionics Biomech. 2019, 2019, 6048562. [Google Scholar] [CrossRef]
- Goldsmith, R.; Wright, C.; Bell, S.F.; Rushton, A. Cold hyperalgesia as a prognostic factor in whiplash associated disorders: A systematic review. Man. Ther. 2012, 17, 402–410. [Google Scholar] [CrossRef]
- Kamper, S.J.; Rebbeck, T.J.; Maher, C.G.; McAuley, J.H.; Sterling, M. Course and prognostic factors of whiplash: A systematic review and meta-analysis. Pain 2008, 138, 617–629. [Google Scholar] [CrossRef]
- Kelly, J.; Ritchie, C.; Sterling, M. Clinical prediction rules for prognosis and treatment prescription in neck pain: A systematic review. Musculoskelet. Sci. Pract. 2017, 27, 155–164. [Google Scholar] [CrossRef]
- Williams, M.; Williamson, E.; Gates, S.; Lamb, S.; Cooke, M. A systematic literature review of physical prognostic factors for the development of Late Whiplash Syndrome. Spine 2007, 32, E764–E780. [Google Scholar] [CrossRef]
- Ohrndorf, S.; Naumann, L.; Grundey, J.; Scheel, T.; Scheel, A.K.; Werner, C.; Backhaus, M. Is musculoskeletal ultrasonography an operator-dependent method or a fast and reliably teachable diagnostic tool? Interreader agreements of three ultrasonographers with different training levels. Int. J. Rheumatol. 2010, 2010, 164518. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Muraki, T.; Morise, S.; Sekiguchi, Y.; Yamamoto, N.; Itoi, E.; Izumi, S.I. Changes in stiffness of the dorsal scapular muscles before and after computer work: A comparison between individuals with and without neck and shoulder complaints. Eur. J. Appl. Physiol. 2017, 117, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Leong, H.T.; Hug, F.; Fu, S.N. Increased Upper Trapezius Muscle Stiffness in Overhead Athletes with Rotator Cuff Tendinopathy. PLoS ONE 2016, 11, e0155187. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.Y.; Choi, J.H. The effects of cervical traction, cranial rhythmic impulse, and Mckenzie exercise on headache and cervical muscle stiffness in episodic tension-type headache patients. J. Phys. Ther. Sci. 2016, 28, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Maher, R.M.; Hayes, D.M.; Shinohara, M. Quantification of dry needling and posture effects on myofascial trigger points using ultrasound shear-wave elastography. Arch. Phys. Med. Rehabil. 2013, 94, 2146–2150. [Google Scholar] [CrossRef] [PubMed]
- Akagi, R.; Shikiba, T.; Tanaka, J.; Takahashi, H. A Six-Week Resistance Training Program Does Not Change Shear Modulus of the Triceps Brachii. J. Appl. Biomech. 2016, 32, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Dankel, S.J.; Razzano, B.M. The impact of acute and chronic resistance exercise on muscle stiffness: A systematic review and meta-analysis. J. Ultrasound 2020, 23, 473–480. [Google Scholar] [CrossRef]
- Ochi, E.; Maruo, M.; Tsuchiya, Y.; Ishii, N.; Miura, K.; Sasaki, K. Higher Training Frequency Is Important for Gaining Muscular Strength Under Volume-Matched Training. Front. Physiol. 2018, 9, 744. [Google Scholar] [CrossRef]
- Thompson, D.P.; Oldham, J.A.; Urmston, M.; Woby, S.R. Cognitive determinants of pain and disability in patients with chronic whiplash-associated disorder: A cross-sectional observational study. Physiotherapy 2010, 96, 151–159. [Google Scholar] [CrossRef]
- Vernon, H.; Guerriero, R.; Kavanaugh, S.; Soave, D.; Moreton, J. Psychological factors in the use of the neck disability index in chronic whiplash patients. Spine 2010, 35, E16–E21. [Google Scholar] [CrossRef]



| Patients (n = 30) | |
|---|---|
| Age, Median (IQR) | 37.5 (31–52) |
| Female, n (%) | 17 (57) |
| Time from accident, Mean ± SD | 30.3 ± 12.8 |
| Drivers, n (%) | 26 (87) |
| Doctor’s office visits, Mean ± SD | 3.9 ± 1.2 |
| Absence from work, n (%) | 20 (67) |
| VAS of pain, Mean ± SD | 5.1 ± 2.7 |
| Analgesic drugs use, n (%) | |
| Occasionally | 5 (17) |
| 1 time/day | 24 (80) |
| 2 or more times/day | 1 (3) |
| Myorelaxant drugs use, n (%) | 18 (60) |
| Elastography of Muscle | Radiologist No1 | Radiologist No2 | ||
|---|---|---|---|---|
| ICC Coefficient | 95% CI | ICC Coefficient | 95% CI | |
| Before PT | ||||
| Trapezius R | 0.79 | (0.636, 0.8946) | 0.75 | (0.6779, 0.9091) |
| Trapezius L | 0.75 | (0.5839, 0.8755) | 0.85 | (0.7388, 0.9289) |
| After PT | ||||
| Trapezius R | 0.94 | (0.9001, 0.9768) | 0.93 | [0.8716, 0.9698) |
| Trapezius L | 0.88 | (0.782, 0.9459) | 0.88 | [0.7888, 0.9478) |
| Elastography of Muscle | ICC Coefficient | 95% CI |
|---|---|---|
| Before PT | ||
| Trapezius R | 0.8787 | (0.7211, 0.9474) |
| Trapezius L | 0.7828 | (0.4955, 0.9062) |
| After PT | ||
| Trapezius R | 0.795 | (0.5131, 0.9144) |
| Trapezius L | 0.7839 | (0.4857, 0.9099) |
| Variables in Model | AIC | Accuracy |
|---|---|---|
| SWE before PT | 46.6 | 63.6% |
| SWE after PT | 46.6 | 40.9% |
| ΔSWE | 46.47 | 50% |
| Relative ΔSWE | 46.62 | 50% |
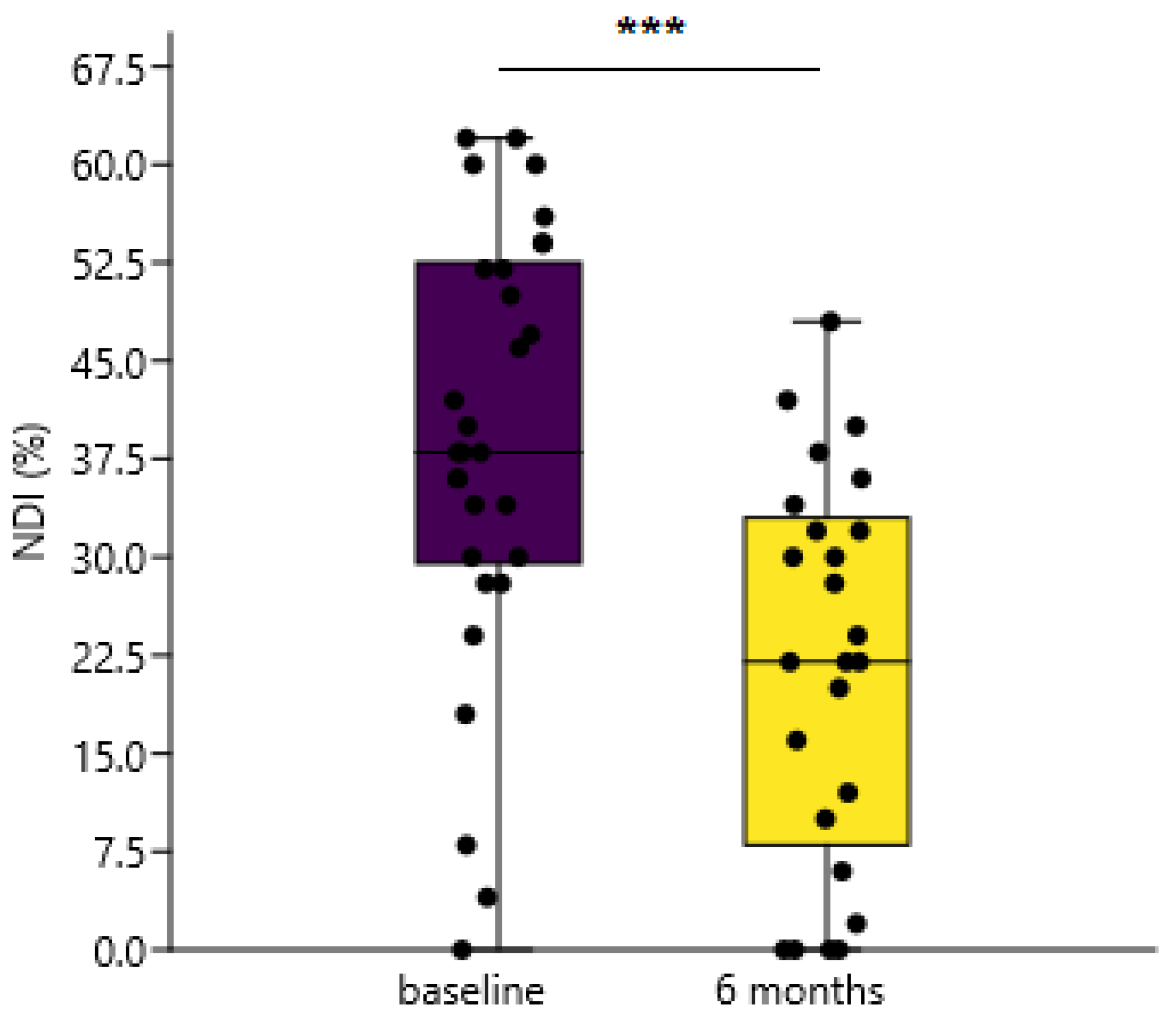
| NDI (%) before PT | 49.66 | 56.5% |
| NDI (%) after PT | 33.74 | 69.6% |
| ΔNDI | 47.37 | 60.9% |
| Relative ΔNDI | 39.21 | 73.9% |
| PHQ9 | 44.54 | 47.8% |
| PHQ9 and SWE after PT | 44.29 | 54.5% |
| NDI (%) after PT and PHQ9 | 34.02 | 69.6% |
| NDI (%) after PT and SWE after PT | 32.85 | 77.3% |
| SWE after PT, NDI (%) after PT and PHQ9 | 34.2 | 72.7% |
| Model with Single Variable | ||
|---|---|---|
| Variable (x) | Coefficient (β) | Std. Error |
| Relative ΔNDI | 0.048 | 0.017 |
| cut1 | −2.72 | 1.08 |
| cut2 | 1.59 | 0.83 |
| Model with Combined Variables | ||
| Variable (x) | Coefficient (β) | Std. Error |
| SWE after PT | −0.025 | 0.031 |
| NDI (%) after PT | 0.13 | 0.07 |
| cut1 | 0.15 | 2.64 |
| cut2 | 4.8 | 2.79 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barun, B.; Barišić, I.; Krnić, A.; Benzon, B.; Vlak, T.; Aljinović, J. Neck Disability Index Is Better in Classification of Recovery after Whiplash Injury in Comparison with Ultrasound Shear Wave Elastography of Trapezius Muscle. Diagnostics 2021, 11, 2077. https://doi.org/10.3390/diagnostics11112077
Barun B, Barišić I, Krnić A, Benzon B, Vlak T, Aljinović J. Neck Disability Index Is Better in Classification of Recovery after Whiplash Injury in Comparison with Ultrasound Shear Wave Elastography of Trapezius Muscle. Diagnostics. 2021; 11(11):2077. https://doi.org/10.3390/diagnostics11112077
Chicago/Turabian StyleBarun, Blaž, Igor Barišić, Ana Krnić, Benjamin Benzon, Tonko Vlak, and Jure Aljinović. 2021. "Neck Disability Index Is Better in Classification of Recovery after Whiplash Injury in Comparison with Ultrasound Shear Wave Elastography of Trapezius Muscle" Diagnostics 11, no. 11: 2077. https://doi.org/10.3390/diagnostics11112077
APA StyleBarun, B., Barišić, I., Krnić, A., Benzon, B., Vlak, T., & Aljinović, J. (2021). Neck Disability Index Is Better in Classification of Recovery after Whiplash Injury in Comparison with Ultrasound Shear Wave Elastography of Trapezius Muscle. Diagnostics, 11(11), 2077. https://doi.org/10.3390/diagnostics11112077






