Assessment of the Elastographic and Electromyographic of Pelvic Floor Muscles in Postmenopausal Women with Stress Urinary Incontinence Symptoms
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Acquisition
2.2. Outcomes
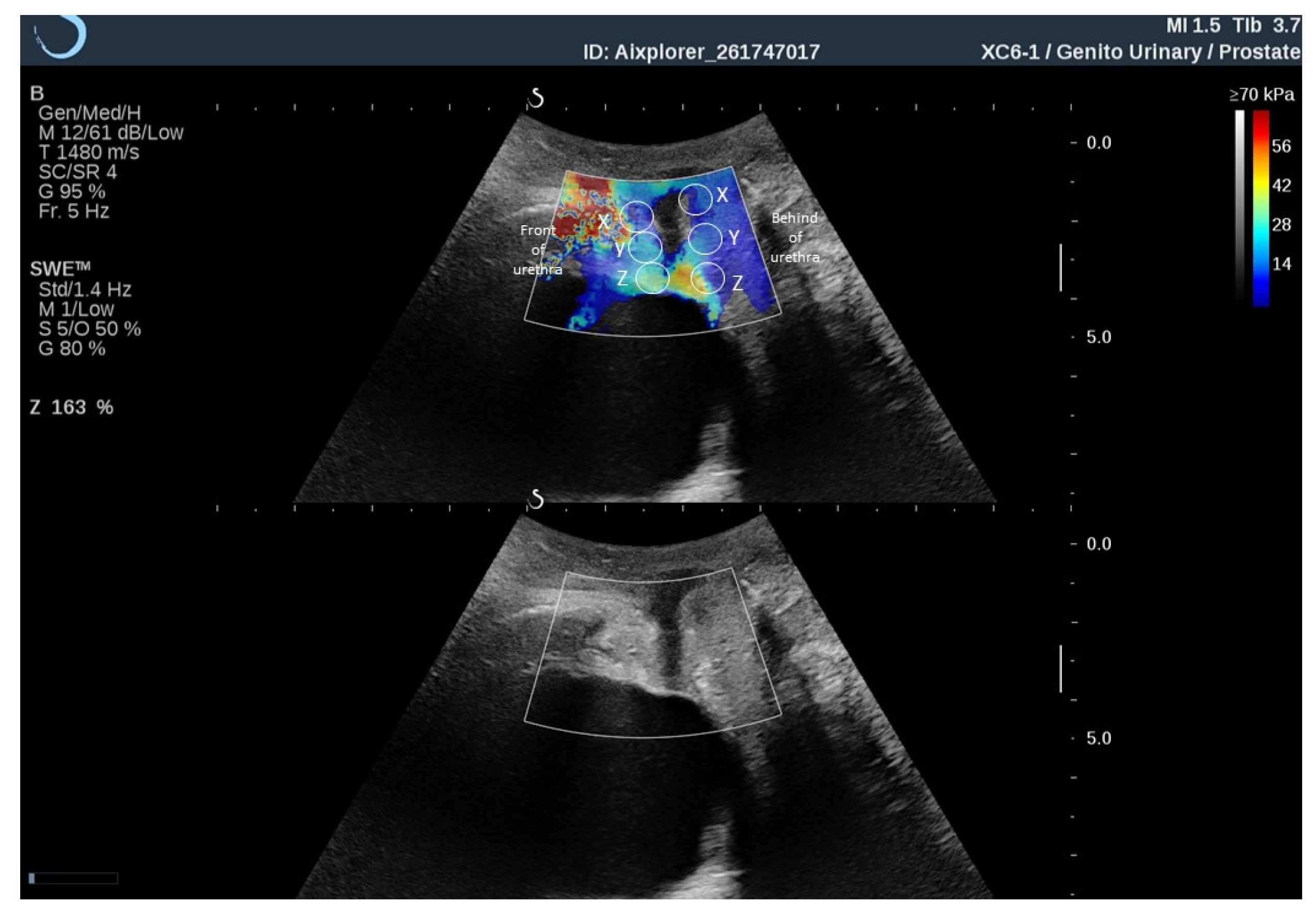
2.3. Ultrosound Elastography
2.4. Electromyography
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aguilar-Zavala, H.; Pérez-Luque, E.L.; Luna-Martínez, F.; Bassol-Mayagoitia, S.; Canto-de-Cetina, T.; López-Conesa, M.; Malacara, J.M. Symptoms at Postmenopause: Genetic and Psychosocial Factors. Menopause 2012, 19, 1140–1145. [Google Scholar] [CrossRef]
- Bauld, R.; Brown, R.F. Stress, Psychological Distress, Psychosocial Factors, Menopause Symptoms and Physical Health in Women. Maturitas 2009, 62, 160–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berg, J.A.; Larson, C.A.; Pasvogel, A.E. Menopausal Symptom Perception and Severity: Results from a Screening Questionnaire. J. Clin. Nurs. 2008, 17, 940–948. [Google Scholar] [CrossRef]
- Menezes, M.; Pereira, M.; Hextall, A. Predictors of Female Urinary Incontinence at Midlife and Beyond. Maturitas 2010, 65, 167–171. [Google Scholar] [CrossRef]
- Ptaszkowski, K.; Zdrojowy, R.; Ptaszkowska, L.; Bartnicki, J.; Taradaj, J.; Paprocka-Borowicz, M. Electromyographic Evaluation of Synergist Muscles of the Pelvic Floor Muscle Depending on the Pelvis Setting in Menopausal Women: A Prospective Observational Study. Gait Posture 2019, 71, 170–176. [Google Scholar] [CrossRef]
- Chiu, Y.-W.; Moore, R.W.; Hsu, C.E.; Huang, C.-T.; Liu, H.-W.; Chuang, H.-Y. Factors Influencing Women’s Quality of Life in the Later Half of Life. Climacteric J. Int. Menopause Soc. 2008, 11, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Cody, J.D.; Jacobs, M.L.; Richardson, K.; Moehrer, B.; Hextall, A. Oestrogen Therapy for Urinary Incontinence in Post-Menopausal Women. Cochrane Database Syst. Rev. 2012, 10, CD001405. [Google Scholar] [CrossRef] [PubMed]
- Ptaszkowski, K.; Zdrojowy, R.; Slupska, L.; Bartnicki, J.; Dembowski, J.; Halski, T.; Paprocka-Borowicz, M. Assessment of Bioelectrical Activity of Pelvic Floor Muscles Depending on the Orientation of the Pelvis in Menopausal Women with Symptoms of Stress Urinary Incontinence: Continued Observational Study. Eur. J. Phys. Rehabil. Med. 2017, 53, 564–574. [Google Scholar] [CrossRef]
- Bø, K.; Hilde, G.; Jensen, J.S.; Siafarikas, F.; Engh, M.E. Too Tight to Give Birth? Assessment of Pelvic Floor Muscle Function in 277 Nulliparous Pregnant Women. Int. Urogynecol. J. 2013, 24, 2065–2070. [Google Scholar] [CrossRef] [Green Version]
- Mørkved, S.; Salvesen, K.A.; Bø, K.; Eik-Nes, S. Pelvic Floor Muscle Strength and Thickness in Continent and Incontinent Nulliparous Pregnant Women. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2004, 15, 384–389. [Google Scholar] [CrossRef]
- Amaro, J.L.; Moreira, E.C.H.; De Oliveira Orsi Gameiro, M.; Padovani, C.R. Pelvic Floor Muscle Evaluation in Incontinent Patients. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2005, 16, 352–354. [Google Scholar] [CrossRef] [PubMed]
- Bø, K. Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice, 1st ed.; Churchill Livingstone: Edinburg, TX, USA, 2007; ISBN 978-0-443-10146-5. [Google Scholar]
- Alves, F.K.; Riccetto, C.; Adami, D.B.V.; Marques, J.; Pereira, L.C.; Palma, P.; Botelho, S. A Pelvic Floor Muscle Training Program in Postmenopausal Women: A Randomized Controlled Trial. Maturitas 2015, 81, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Betschart, C.; Mol, S.E.; Lütolf-Keller, B.; Fink, D.; Perucchini, D.; Scheiner, D. Pelvic Floor Muscle Training for Urinary Incontinence: A Comparison of Outcomes in Premenopausal versus Postmenopausal Women. Female Pelvic Med. Reconstr. Surg. 2013, 19, 219–224. [Google Scholar] [CrossRef]
- Balmforth, J.R.; Mantle, J.; Bidmead, J.; Cardozo, L. A Prospective Observational Trial of Pelvic Floor Muscle Training for Female Stress Urinary Incontinence. BJU Int. 2006, 98, 811–817. [Google Scholar] [CrossRef] [PubMed]
- McLean, L.; Varette, K.; Gentilcore-Saulnier, E.; Harvey, M.-A.; Baker, K.; Sauerbrei, E. Pelvic Floor Muscle Training in Women with Stress Urinary Incontinence Causes Hypertrophy of the Urethral Sphincters and Reduces Bladder Neck Mobility during Coughing. Neurourol. Urodyn. 2013, 32, 1096–1102. [Google Scholar] [CrossRef] [Green Version]
- Aukee, P.; Penttinen, J.; Airaksinen, O. The Effect of Aging on the Electromyographic Activity of Pelvic Floor Muscles. A Comparative Study among Stress Incontinent Patients and Asymptomatic Women. Maturitas 2003, 44, 253–257. [Google Scholar] [CrossRef]
- Ptaszkowski, K.; Paprocka-Borowicz, M.; Słupska, L.; Bartnicki, J.; Dymarek, R.; Rosińczuk, J.; Heimrath, J.; Dembowski, J.; Zdrojowy, R. Assessment of Bioelectrical Activity of Synergistic Muscles during Pelvic Floor Muscles Activation in Postmenopausal Women with and without Stress Urinary Incontinence: A Preliminary Observational Study. Clin. Interv. Aging 2015, 10, 1521–1528. [Google Scholar] [CrossRef] [Green Version]
- Ptaszkowski, K.; Malkiewicz, B.; Zdrojowy, R.; Paprocka-Borowicz, M.; Ptaszkowska, L. The Prognostic Value of the Surface Electromyographic Assessment of Pelvic Floor Muscles in Women with Stress Urinary Incontinence. J. Clin. Med. 2020, 9, 1967. [Google Scholar] [CrossRef]
- Aljuraifani, R.; Stafford, R.E.; Hug, F.; Hodges, P.W. Female Striated Urogenital Sphincter Contraction Measured by Shear Wave Elastography during Pelvic Floor Muscle Activation: Proof of Concept and Validation. Neurourol. Urodyn. 2018, 37, 206–212. [Google Scholar] [CrossRef]
- Kreutzkamp, J.M.; Schäfer, S.D.; Amler, S.; Strube, F.; Kiesel, L.; Schmitz, R. Strain Elastography as a New Method for Assessing Pelvic Floor Biomechanics. Ultrasound Med. Biol. 2017, 43, 868–872. [Google Scholar] [CrossRef]
- Xie, M.; Zhang, X.; Zhang, X.; Wang, W.; Hua, K. Can We Evaluate the Levator Ani after Kegel Exercise in Women with Pelvic Organ Prolapse by Transperineal Elastography? A Preliminary Study. J. Med. Ultrason. 2001 2018, 45, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Feng, Y.; Zhang, X.; Hua, K.; Ren, Y.; Wang, W. Evaluation of Pelvic Floor Muscle by Transperineal Elastography in Patients with Deep Infiltrating Endometriosis: Preliminary Observation. J. Med. Ultrason. 2001 2019, 46, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Stafford, R.E.; Aljuraifani, R.; Hug, F.; Hodges, P.W. Application of Shear-Wave Elastography to Estimate the Stiffness of the Male Striated Urethral Sphincter during Voluntary Contractions. BJU Int. 2017, 119, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Maßlo, K.; Möllers, M.; de Murcia, K.O.; Klockenbusch, W.; Schmitz, R. New Method for Assessment of Levator Avulsion Injury: A Comparative Elastography Study. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2019, 38, 1301–1307. [Google Scholar] [CrossRef]
- Jamard, E.; Blouet, M.; Thubert, T.; Rejano-Campo, M.; Fauvet, R.; Pizzoferrato, A.-C. Utility of 2D-Ultrasound in Pelvic Floor Muscle Contraction and Bladder Neck Mobility Assessment in Women with Urinary Incontinence. J. Gynecol. Obstet. Hum. Reprod. 2020, 49, 101629. [Google Scholar] [CrossRef]
- Ptaszkowski, K.; Malkiewicz, B.; Zdrojowy, R.; Ptaszkowska, L.; Paprocka-Borowicz, M. Assessment of the Short-Term Effects after High-Inductive Electromagnetic Stimulation of Pelvic Floor Muscles: A Randomized, Sham-Controlled Study. J. Clin. Med. 2020, 9, 874. [Google Scholar] [CrossRef] [Green Version]
- Mannella, P.; Palla, G.; Bellini, M.; Simoncini, T. The Female Pelvic Floor through Midlife and Aging. Maturitas 2013, 76, 230–234. [Google Scholar] [CrossRef]
- Basha, M.E.; Chang, S.; Burrows, L.J.; Lassmann, J.; Wein, A.J.; Moreland, R.S.; Chacko, S. Effect of Estrogen on Molecular and Functional Characteristics of the Rodent Vaginal Muscularis. J. Sex. Med. 2013, 10, 1219–1230. [Google Scholar] [CrossRef] [Green Version]
- Vitale, S.G.; La Rosa, V.L.; Rapisarda, A.M.C.; Laganà, A.S. Sexual Life in Women with Stress Urinary Incontinence. Oman Med. J. 2017, 32, 174–175. [Google Scholar] [CrossRef]
- Petros, P.E.; Ulmsten, U.I. An Integral Theory of Female Urinary Incontinence. Experimental and Clinical Considerations. Acta Obstet. Gynecol. Scand. Suppl. 1990, 153, 7–31. [Google Scholar] [CrossRef]
- Dimpfl, T.; Jaeger, C.; Mueller-Felber, W.; Anthuber, C.; Hirsch, A.; Brandmaier, R.; Schuessler, B. Myogenic Changes of the Levator Ani Muscle in Premenopausal Women: The Impact of Vaginal Delivery and Age. Neurourol. Urodyn. 1998, 17, 197–205. [Google Scholar] [CrossRef]
- Tang, J.-H.; Zhong, C.; Wen, W.; Wu, R.; Liu, Y.; Du, L.-F. Quantifying Levator Ani Muscle Elasticity Under Normal and Prolapse Conditions by Shear Wave Elastography: A Preliminary Study. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2020, 39, 1379–1388. [Google Scholar] [CrossRef] [PubMed]
- Gachon, B.; Nordez, A.; Pierre, F.; Fradet, L.; Fritel, X.; Desseauve, D. In Vivo Assessment of the Levator Ani Muscles Using Shear Wave Elastography: A Feasibility Study in Women. Int. Urogynecol. J. 2019, 30, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Machado L da, S.; Marques Cerentini, T.; Laganà, A.S.; Viana da Rosa, P.; Fichera, M.; Telles da Rosa, L.H. Pelvic floor evaluation in CrossFit® athletes and urinary incontinence: A cross-sectional observational study. Women Health 2021, 61, 490–499. [Google Scholar] [CrossRef] [PubMed]
| Variables | Postmenopausal Women (n = 14) | ||
|---|---|---|---|
| Me | Q1–Q3 | ||
| Age (years) | 53 | 46–56 | |
| Weight (kg) | 64 | 60–70 | |
| Height (m) | 1.65 | 1.64–1.66 | |
| BMI (kg/m2) | 24 | 22–24 | |
| Occurrence of urinary incontinence symptoms (years) | 4 | 2–10 | |
| ICIQ-UI SF score | 7 | 4–10 | |
| Qualitative variables | n | % | |
| Kind of work | Physical | 2 | 14 |
| Mental | 12 | 86 | |
| Number of deliveries | 0 | 1 | 8 |
| 1 | 3 | 21 | |
| 2 | 10 | 71 | |
| Q-Box | Rest Tone of PFM (kPa) | Contraction of PFM (kPa) | p-Value * | |||
|---|---|---|---|---|---|---|
| Me | Q1–Q3 | Me | Q1–Q3 | |||
| Front of urethra | X | 11.9 | 6.9–17.0 | 35.0 | 25.0–43.3 | 0.002 |
| Y | 15.1 | 9.9–20.0 | 35.9 | 28.0–51.0 | 0.001 | |
| Z | 15.0 | 10.3–17.0 | 18.5 | 15.0–28.0 | 0.024 | |
| Behind of urethra | X | 10.9 | 9.3–17.6 | 14.5 | 10.2–16.5 | 0.91 |
| Y | 11.2 | 8.7–14.0 | 10.8 | 9.4–15.5 | 0.89 | |
| Z | 12.0 | 8.8–15.0 | 12.6 | 9.0–14.0 | 0.63 | |
| Rest Tone of PFM (µV) | Contraction of PFM (µV) | p-Value * | |||
|---|---|---|---|---|---|
| Me | Q1–Q3 | Me | Q1–Q3 | ||
| Bioelectrical activity of PFM | 3.1 | 2.3–3.9 | 9.1 | 8.1–11.6 | <0.001 |
| Q-Box | Rest Tone of PFM (µV) | Contraction of PFM (µV) | |||
|---|---|---|---|---|---|
| rs | p | rs | p | ||
| Front of urethra (kPa) | X | 0.21 | 0.55 | 0.25 | 0.41 |
| Y | 0.11 | 0.73 | 0.18 | 0.55 | |
| Z | 0.21 | 0.54 | 0.15 | 0.64 | |
| Behind of urethra (kPa) | X | 0.19 | 0.55 | 0.44 | 0.15 |
| Y | 0.02 | 0.93 | 0.20 | 0.53 | |
| Z | 0.18 | 0.56 | 0.24 | 0.42 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ptaszkowski, K.; Małkiewicz, B.; Zdrojowy, R.; Paprocka-Borowicz, M.; Ptaszkowska, L. Assessment of the Elastographic and Electromyographic of Pelvic Floor Muscles in Postmenopausal Women with Stress Urinary Incontinence Symptoms. Diagnostics 2021, 11, 2051. https://doi.org/10.3390/diagnostics11112051
Ptaszkowski K, Małkiewicz B, Zdrojowy R, Paprocka-Borowicz M, Ptaszkowska L. Assessment of the Elastographic and Electromyographic of Pelvic Floor Muscles in Postmenopausal Women with Stress Urinary Incontinence Symptoms. Diagnostics. 2021; 11(11):2051. https://doi.org/10.3390/diagnostics11112051
Chicago/Turabian StylePtaszkowski, Kuba, Bartosz Małkiewicz, Romuald Zdrojowy, Malgorzata Paprocka-Borowicz, and Lucyna Ptaszkowska. 2021. "Assessment of the Elastographic and Electromyographic of Pelvic Floor Muscles in Postmenopausal Women with Stress Urinary Incontinence Symptoms" Diagnostics 11, no. 11: 2051. https://doi.org/10.3390/diagnostics11112051






