The Value of Posterior Cervical Angle as a Predictor of Vaginal Delivery: A Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Characteristics
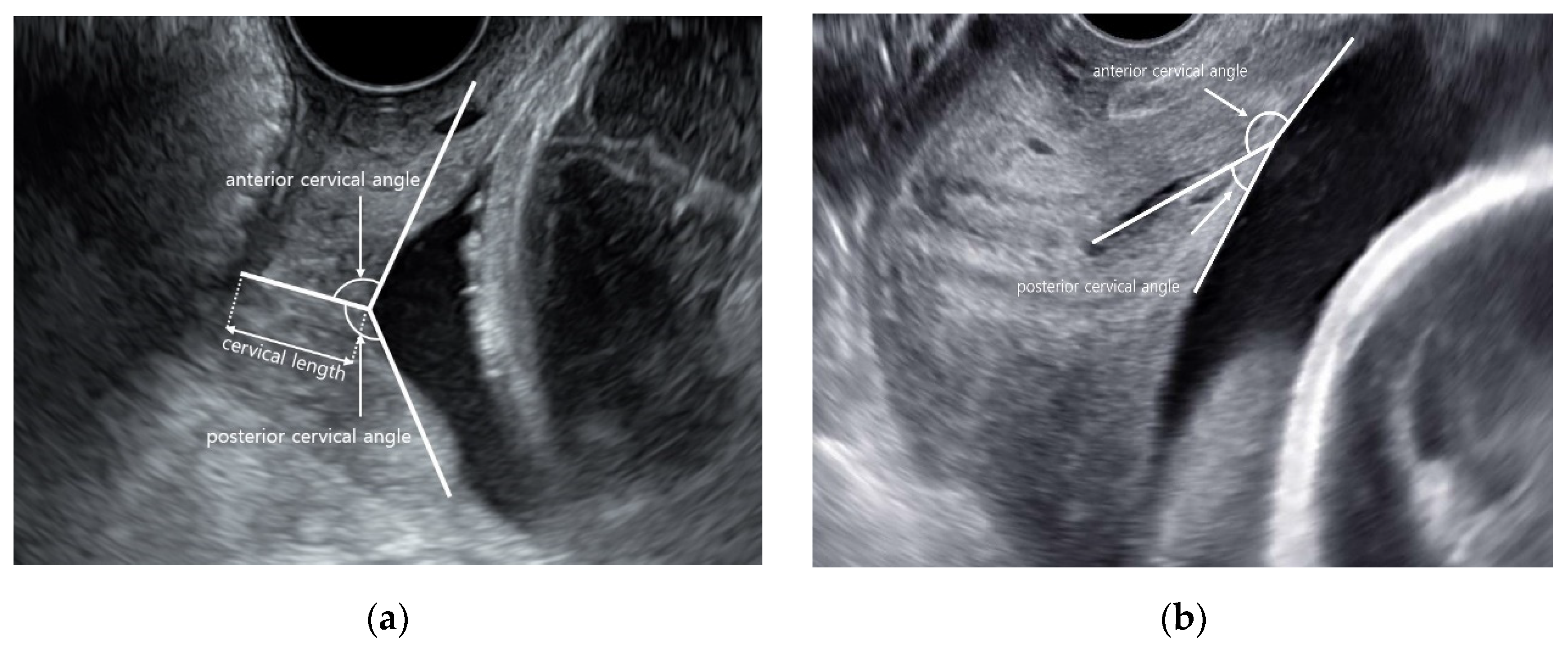
2.2. Ultrasound Examinations
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Neuhoff, D.; Burke, S.M.; Porreco, R.P. Cesarean Birth for Failed Progress in Labor. Am. J. Obstet. Gynecol. 1989, 73, 915–920. [Google Scholar] [CrossRef]
- Gifford, D.S.; Morton, S.C.; Fiske, M.; Keesey, J.; Keeler, E.; Kahn, K.L. Lack of Progress in Labor as a Reason for Cesarean. Obstet. Gynecol. 2000, 95, 589–595. [Google Scholar] [CrossRef]
- Yeo, L.; Romero, R. Sonographic evaluation in the second stage of labor to improve the assessment of labor progress and its outcome. Ultrasound Obstet. Gynecol. 2009, 33, 253–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bishop, E.H. PELVIC SCORING FOR ELECTIVE INDUCTION. Obstet. Gynecol. 1964, 24, 266–268. [Google Scholar]
- Dhall, K.; Mittal, S.C.; Kumar, A. Evaluation of Preinduction Scoring Systems. Aust. N. Z. J. Obstet. Gynaecol. 1987, 27, 309–311. [Google Scholar] [CrossRef] [PubMed]
- Rane, S.M.; Guirgis, R.R.; Higgins, B.; Nicolaides, K.H. The value of ultrasound in the prediction of successful induction of labor. Ultrasound Obstet. Gynecol. 2004, 24, 538–549. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.; Shi, G.; Qi, Z.; Zheng, J.; Chen, S. Advancements in the Application of Ultrasound Elastography in the Cervix. Ultrasound Med. Biol. 2021, 47, 2048–2063. [Google Scholar] [CrossRef]
- Taha, O.T.; Elprince, M.; Atwa, K.A.; Elgedawy, A.M.; Ahmed, A.A.; Khamees, R.E. Antenatal cervical length measurement as a predictor of successful vaginal birth. BMC Pregnancy Childbirth 2020, 20, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Dziadosz, M.; Bennett, T.-A.; Dolin, C.; Honart, A.W.; Pham, A.; Lee, S.S.; Pivo, S.; Roman, A.S. Uterocervical angle: A novel ultrasound screening tool to predict spontaneous preterm birth. Am. J. Obstet. Gynecol. 2016, 215, 376.e1–376.e7. [Google Scholar] [CrossRef]
- Sepúlveda-Martínez, A.; Díaz, F.; Muñoz, H.; Valdés, E.; Parra-Cordero, M. Second-Trimester Anterior Cervical Angle in a Low-Risk Population as a Marker for Spontaneous Preterm Delivery. Fetal Diagn. Ther. 2017, 41, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Llobet, A.F.; Martí, L.R.; Higueras, T.; Fernández, I.Z.C.; Portalés, A.G.; Canino, M.M.G.; Moratonas, E.C. The uterocervical angle and its relationship with preterm birth. J. Matern. Neonatal Med. 2017, 31, 1881–1884. [Google Scholar] [CrossRef] [PubMed]
- Szlachetka, K.; Seligman, N.S.; Lynch, T.A. Ultrasonographic Change in Uterocervical Angle is not a Risk Factor for Preterm Birth in Women with a Short Cervix. Am. J. Perinatol. 2017, 34, 1058–1064. [Google Scholar] [CrossRef]
- Cannie, M.M.; Dobrescu, O.G.; Gucciardo, L.; Strizek, B.B.; Ziane, S.S.; Sakkas, E.G.E.; Schoonjans, F.; Divano, L.; Jani, J.C. Arabin cervical pessary in pregnant women at high-risk of premature birth: An MR imaging observational follow-up study. Ultrasound Obstet. Gynecol. 2013, 42, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Tenbrink, E.; Onslow, M.; Patil, A.S.; Knight, J.C. Uterocervical Angle Measurement Improves Prediction of Preterm Birth in Twin Gestation. Am. J. Perinatol. 2017, 35, 648–654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NICE. Intrapartum Care for Healthy Women and Babies; National Institute for Health and Care Excellence: London, UK, 2014; Available online: https://www.nice.org.uk/guidance/cg190 (accessed on 19 October 2021).
- Sundtoft, I.; Langhoff-Roos, J.; Sandager, P.; Sommer, S.; Uldbjerg, N. Cervical collagen is reduced in non-pregnant women with a history of cervical insufficiency and a short cervix. Acta Obstet. et Gynecol. Scand. 2017, 96, 984–990. [Google Scholar] [CrossRef] [Green Version]
- Yao, W.; Gan, Y.; Myers, K.; Vink, J.Y.; Wapner, R.; Hendon, C.P. Collagen Fiber Orientation and Dispersion in the Upper Cervix of Non-Pregnant and Pregnant Women. PLoS ONE 2016, 11, e0166709. [Google Scholar] [CrossRef]
- Keepanasseril, A.; Suri, V.; Bagga, R.; Aggarwal, N. Pre-induction sonographic assessment of the cervix in the prediction of successful induction of labour in nulliparous women. Aust. N. Z. J. Obstet. Gynaecol. 2007, 47, 389–393. [Google Scholar] [CrossRef]
- Al-Adwy, A.M.; Sobh, S.M.; Belal, D.S.; Omran, E.F.; Hassan, A.; Saad, A.H.; Afifi, M.M.; Nada, A.M. Diagnostic accuracy of posterior cervical angle and cervical length in the prediction of successful induction of labor. Int. J. Gynecol. Obstet. 2018, 141, 102–107. [Google Scholar] [CrossRef]
- Eggebø, T.M.; Økland, I.; Heien, C.; Gjessing, L.K.; Romundstad, P.; Salvesen, K.Å. Can ultrasound measurements replace digitally assessed elements of the Bishop score? Acta Obstet. et Gynecol. Scand. 2009, 88, 325–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sebire, N.; Jolly, M.; Harris, J.; Wadsworth, J.; Joffe, M.; Beard, R.; Regan, L.; Robinson, S. Maternal obesity and pregnancy outcome: A study of 287 213 pregnancies in London. Int. J. Obes. 2001, 25, 1175–1182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheiner, E.; Levy, A.; Feinstein, U.; Hershkovitz, R.; Hallak, M.; Mazor, M. Obstetric risk factors for failure to progress in the first versus the second stage of labor. J. Matern. Neonatal Med. 2002, 11, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Daskalakis, G.; Theodora, M.; Antsaklis, P.; Sindos, M.; Grigoriadis, T.; Antsaklis, A.; Papantoniou, N.; Loutradis, D.; Pergialiotis, V. Assessment of Uterocervical Angle Width as a Predictive Factor of Preterm Birth: A Systematic Review of the Literature. BioMed Res. Int. 2018, 2018, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozenberg, P.; Chevret, S.; Chastang, C.; Ville, Y. Comparison of digital and ultrasonographic examination of the cervix in predicting time interval from induction to delivery in women with a low Bishop score. BJOG Int. J. Obstet. Gynaecol. 2005, 112, 192–196. [Google Scholar] [CrossRef] [PubMed]


| Vaginal Delivery (n = 68) | Cesarean Section (n = 22) | p-Value | |
|---|---|---|---|
| Age (years) | 32.6 ± 4.5 | 33.1 ± 5.8 | 0.703 |
| Gestational age (days) | 264.9 ± 14.5 | 270.6 ± 11.8 | 0.101 |
| Multiparity (%) | 36.8 | 4.5 | 0.004 |
| Abortion (%) | 30.8 | 50 | 0.127 |
| BMI (kg/ht2) | 26.3(19.5–43.3) | 29.2(20.6–41.8) | 0.033 |
| Epidural anesthesia (%) | 58.8 | 40.9 | 0.218 |
| Induction of labor (%) | 27.9 | 50 | 0.062 |
| PROM or PPROM (%) | 25 | 22.7 | 0.829 |
| Preterm labor (%) | 13.2 | 4.5 | 0.440 |
| ART (%) | 0 | 18.2 | 0.003 |
| Hypertension (%) | 5.9 | 9.1 | 0.632 |
| Diabetes (%) | 11.8 | 18.2 | 0.478 |
| Neonatal male gender (%) | 52.9 | 40.9 | 0.328 |
| Birth weight (kg) | 3.31 ± 0.40 | 3.46 ± 0.41 | 0.07 |
| Vaginal Delivery (n = 68) | Cesarean Section (n = 22) | p-Value | |
|---|---|---|---|
| AFI (cm) | 11.7 (9–14.7) | 12.6 (10.3–15) | 0.33 |
| Cervical length (mm) | 25.5 ± 1.26 | 32.4 ± 1.37 | 0.034 |
| Anterior cervical angle (°) | 115.2 ± 21.4 | 117.4 ± 33.2 | 0.619 |
| Posterior cervical angle (°) | 106.8 ± 26.9 | 88.7 ± 30.4 | 0.0096 |
| OR | p = Value | aORs (95% CI) * | p = Value | |
|---|---|---|---|---|
| Maternal BMI | 0.883 (0.800, 0.976) | 0.015 | 0.861 (0.764, 0.971) | 0.013 |
| Multiparity | 12.209 (1.547, 96.348) | 0.018 | 20.393 (1.818, 228.8) | 0.015 |
| Cervical length | 0.652 (0.434, 0.978) | 0.039 | 0.669 (0.411–1.09) | 0.107 |
| Posterior cervical angle ≥ 96.5° | 4.012 (1.467, 10.975) | 0.007 | 5.342 (1.553, 18.369) | 0.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, E.-J.; Heo, J.-M.; Kim, H.-Y.; Ahn, K.-H.; Cho, G.-J.; Hong, S.-C.; Oh, M.-J.; Lee, N.-W.; Kim, H.-J. The Value of Posterior Cervical Angle as a Predictor of Vaginal Delivery: A Preliminary Study. Diagnostics 2021, 11, 1977. https://doi.org/10.3390/diagnostics11111977
Kim E-J, Heo J-M, Kim H-Y, Ahn K-H, Cho G-J, Hong S-C, Oh M-J, Lee N-W, Kim H-J. The Value of Posterior Cervical Angle as a Predictor of Vaginal Delivery: A Preliminary Study. Diagnostics. 2021; 11(11):1977. https://doi.org/10.3390/diagnostics11111977
Chicago/Turabian StyleKim, Eun-Ju, Ji-Man Heo, Ho-Yeon Kim, Ki-Hoon Ahn, Geum-Joon Cho, Soon-Cheol Hong, Min-Jeong Oh, Nak-Woo Lee, and Hai-Joong Kim. 2021. "The Value of Posterior Cervical Angle as a Predictor of Vaginal Delivery: A Preliminary Study" Diagnostics 11, no. 11: 1977. https://doi.org/10.3390/diagnostics11111977
APA StyleKim, E.-J., Heo, J.-M., Kim, H.-Y., Ahn, K.-H., Cho, G.-J., Hong, S.-C., Oh, M.-J., Lee, N.-W., & Kim, H.-J. (2021). The Value of Posterior Cervical Angle as a Predictor of Vaginal Delivery: A Preliminary Study. Diagnostics, 11(11), 1977. https://doi.org/10.3390/diagnostics11111977








