Brachial Plexus Injury Associated with Median Sternotomy during Cardiac Surgery: Three Cases of C8 Radiculopathy Due to the Fracture of the First Rib
Abstract
1. Introduction
2. Case Report
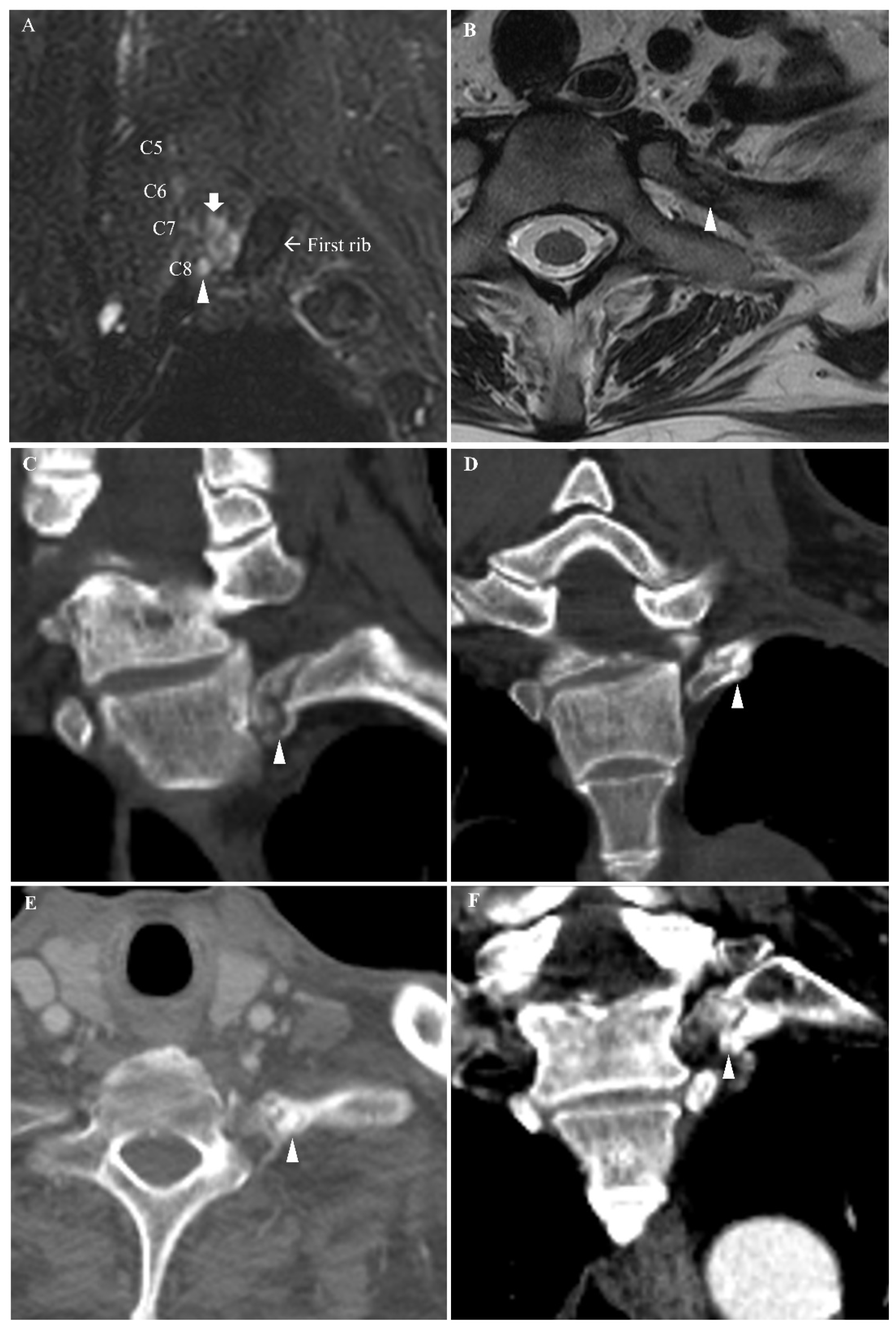
2.1. Case 1
2.2. Case 2
2.3. Case 3
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Unlü, Y.; Velioğlu, Y.; Koçak, H.; Becit, N.; Ceviz, M. Brachial plexus injury following median sternotomy. Interact. Cardiovasc. Thorac. Surg. 2007, 6, 235–237. [Google Scholar] [CrossRef] [PubMed]
- Healey, S.; O’Neill, B.; Bilal, H.; Waterworth, P. Does retraction of the sternum during median sternotomy result in brachial plexus injuries? Interact. Cardiovasc. Thorac. Surg. 2013, 17, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Chong, A.Y.; Clarke, C.E.; Dimitri, W.R.; Lip, G.Y. Brachial plexus injury as an unusual complication of coronary artery bypass graft surgery. Postgrad. Med. J. 2003, 79, 84–86. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sharma, A.D.; Parmley, C.L.; Sreeram, G.; Grocott, H.P. Peripheral nerve injuries during cardiac surgery: Risk factors, diagnosis, prognosis, and prevention. Anesth. Analg. 2000, 91, 1358–1369. [Google Scholar] [CrossRef] [PubMed]
- Levin, K.H.; Wilbourn, A.J.; Maggiano, H.J. Cervical rib and median sternotomy-related brachial plexopathies: A reassessment. Neurology 1998, 50, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Vahl, C.F.; Carl, I.; Müller-Vahl, H.; Struck, E. Brachial plexus injury after cardiac surgery. The role of internal mammary artery preparation: A prospective study on 1000 consecutive patients. J. Thorac. Cardiovasc. Surg. 1991, 102, 724–729. [Google Scholar] [CrossRef]
- Canbaz, S.; Turgut, N.; Halici, U.; Sunar, H.; Balci, K.; Duran, E. Brachial plexus injury during open heart surgery—Controlled prospective study. Thorac. Cardiovasc. Surg. 2005, 53, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Grocott, H.P.; Clark, J.A.; Homi, H.M.; Sharma, A. “Other” neurologic complications after cardiac surgery. Semin. Cardiothorac. Vasc. Anesth. 2004, 8, 213–226. [Google Scholar] [CrossRef] [PubMed]
- Vander Salm, T.J.; Cereda, J.M.; Cutler, B.S. Brachial plexus injury following median sternotomy. J. Thorac. Cardiovasc. Surg. 1980, 80, 447–452. [Google Scholar] [CrossRef]
- Greenwald, L.V.; Baisden, C.E.; Symbas, P.N. Rib fractures in coronary bypass patients: Radionuclide detection. Radiology 1983, 148, 553–554. [Google Scholar] [CrossRef] [PubMed]
| Nerve | SNAP Amplitude (µV) (Baseline to Peak) | CMAP Amplitude (mV) (Baseline to Peak) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Record | Right | Left * | NLL | Record | Right | Left * | NLL | ||
| Case 1 | Median | Digit II | 37.6 | 39.4 | >28.0 | APB | 6.7 | 2.5 | >8.3 |
| Ulnar | Digit V | 28.6 | 24.2 | >23.8 | ADM | 7.6 | 2.7 | >8.0 | |
| Radial | 1st DWS | 29.6 | 14.3 | >15.0 | EIP | 3.7 | 1.3 | >2.0 | |
| MABC | Forearm | 14.8 | 13.1 | >5.5 | |||||
| Case 2 | Median | Digit II | 38.5 | 35.0 | >16.3 | APB | 9.6 | 8.8 | >7.5 |
| Ulnar | Digit V | 28.1 | 21.6 | >15.0 | ADM | 11.2 | 10.2 | >7.5 | |
| MABC | Forearm | 13.0 | 14.0 | >8.5 | |||||
| Case 3 | Median | Digit II | 29.5 | 31.4 | >14.9 | APB | 6.7 | 7.5 | >5.7 |
| Ulnar | Digit V | 15.4 | NR | >14.9 | ADM | 7.8 | 1.7 | >7.3 | |
| DUCN | 4th DWS | 12.4 | 4.4 | >8.0 | |||||
| MABC | Forearm | 12.0 | 6.7 | >5.8 | |||||
| Muscle (Left) | ASA | MUAP | R | ||||
|---|---|---|---|---|---|---|---|
| PSWs | Fibs | Amp | Dur | Phases | IP | ||
| Case 1 | APB | None | None | ↑ | ↑ | Normal | Reduced |
| ADM | 1+ | 1+ | Normal | ↑ | Poly | Reduced | |
| FDI | 1+ | 1+ | Normal | Normal | Poly | Reduced | |
| EDC | None | 1+ | Normal | ↑ | Poly | Reduced | |
| EPL | 1+ | None | Normal | Normal | Poly | Reduced | |
| EIP | None | 1+ | Normal | ↑ | Normal | Reduced | |
| Lower cervical PSP | None | None | |||||
| Case 2 | APB | None | None | Normal | Normal | Normal | Complete |
| ADM | 1+ | None | Normal | Normal | Normal | Reduced | |
| FDI | None | 1+ | Normal | Normal | Normal | Reduced | |
| EDC, EIP | None | None | Normal | Normal | Normal | Reduced | |
| Lower cervical PSP | None | None | |||||
| Case 3 | APB | None | None | Normal | Normal | Normal | Complete |
| FCU | 2+ | None | Normal | ↑ | Normal | Complete | |
| ADM | 1+ | None | Normal | ↑ | Normal | Reduced | |
| FDI | 3+ | None | Normal | ↑ | Normal | Reduced | |
| Lower cervical PSP | None | None | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Im, Y.J.; Kang, M.S.; Kim, S.W.; Sung, D.H. Brachial Plexus Injury Associated with Median Sternotomy during Cardiac Surgery: Three Cases of C8 Radiculopathy Due to the Fracture of the First Rib. Diagnostics 2021, 11, 1896. https://doi.org/10.3390/diagnostics11101896
Im YJ, Kang MS, Kim SW, Sung DH. Brachial Plexus Injury Associated with Median Sternotomy during Cardiac Surgery: Three Cases of C8 Radiculopathy Due to the Fracture of the First Rib. Diagnostics. 2021; 11(10):1896. https://doi.org/10.3390/diagnostics11101896
Chicago/Turabian StyleIm, Yu Jin, Min Soo Kang, Sun Woong Kim, and Duk Hyun Sung. 2021. "Brachial Plexus Injury Associated with Median Sternotomy during Cardiac Surgery: Three Cases of C8 Radiculopathy Due to the Fracture of the First Rib" Diagnostics 11, no. 10: 1896. https://doi.org/10.3390/diagnostics11101896
APA StyleIm, Y. J., Kang, M. S., Kim, S. W., & Sung, D. H. (2021). Brachial Plexus Injury Associated with Median Sternotomy during Cardiac Surgery: Three Cases of C8 Radiculopathy Due to the Fracture of the First Rib. Diagnostics, 11(10), 1896. https://doi.org/10.3390/diagnostics11101896






