1. Introduction
The first to report a clinical case of elongated styloid process was Weinlecher in 1872, but it was Watt W. Eagle in 1947 who described a set of symptoms resulting from the lengthening and excessive calcification of the styloid process of the temporal bone and calcification of the ligaments attaching to this process, i.e., the styloid and stylomandibular ligaments [
1,
2,
3]. This abnormality is found in around 4% of the population, but for most cases, it is asymptomatic. The main symptom is the pain located in the temporomandibular area, neck, and ear. Various head movements might trigger it [
4,
5]. Patients may also feel a foreign body sensation in their throat, dysphagia, tinnitus, and balance disorders. The most dangerous symptoms are direct trauma of the elongated styloid process to the internal carotid artery, including epileptic attacks and stroke [
5,
6]. There is a possibility to treat patients with both non-invasive and invasive treatment, but surgery is the treatment of choice with the highest success rate [
5,
7].
We describe the case of a 39-year-old man who presented with discomfort and foreign body sensation in his throat.
2. Case Description
The patient was a Caucasian male aged 39, who reported to a neurologist because of his throat’s discomfort and foreign body sensation. The throat discomfort had been occurring periodically for many years. The throat discomfort and the foreign body sensation intensified following an episode of vomiting several weeks prior to the visit. The vomiting episode was related to a dietary error. He denied odynophagia, dysphagia, tinnitus, vision disturbances, headaches, and relevant risk factors or medication. He had an otherwise healthy life before the event, reporting no invasive procedures at the area of the throat and larynx, cervical part of spine as well as cranial area. In his childhood, he was only diagnosed with thyroid nontoxic goiter.
On physical examination, head movements or opening the mouth do not cause pain, but currently, there is pressure soreness in the submandibular area on the left side. There were no neurological deficits.
The neck ultrasound did not show any enlarged lymph nodes or nodal packages.
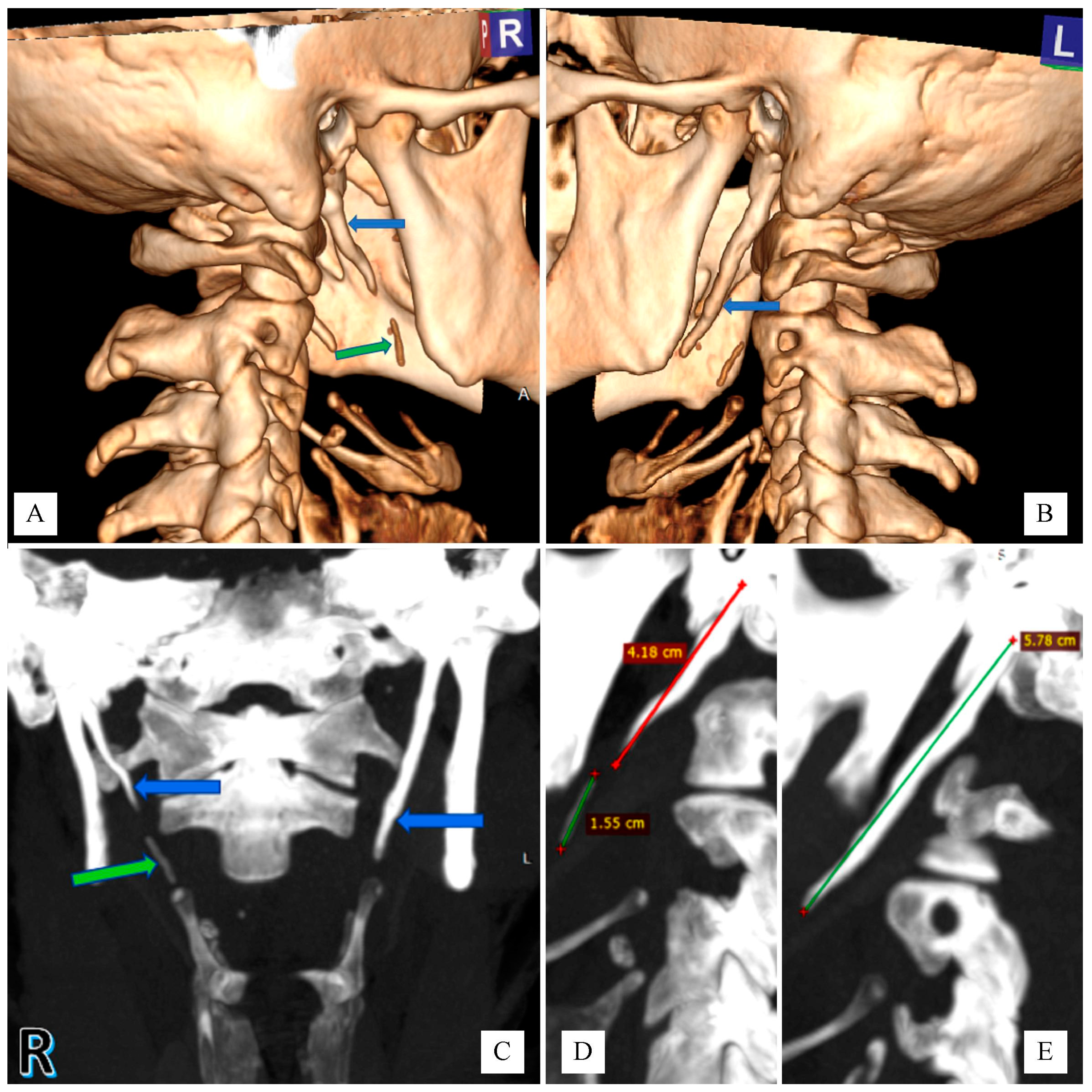
The computed tomography (CT) scan showed a bilaterally elongated styloid process: 57–58 mm on the left side, and the right side was 41–42 mm (
Figure 1). Below the top of the right styloid process, there was placed a well-calcified shadow about 15–16 mm long, which could correspond to its continuation, without a clear connection with the top of the process (
Figure 1). In addition, the study showed adenoid tissue overgrowth of Waldeyer’s lymph ring with the presence of minor polycyclic calcifications, abolition of physiological cervical lordosis and degenerative changes in the cervical spine.
Eventually, the diagnosis of the classic type of Eagle’s syndrome (ES) was made; on the left side, so called elongated type, and on the right-side the segmented type (consisting of an uninterrupted segments of mineralized ligament). The patient underwent laryngological and surgical consultation. Due to the lack of symptoms related to the compression of the carotid arteries, no surgery was recommended. Pharmacological treatment was prescribed—first of all, painkillers. In the event of persistent symptoms, it was recommended to consider the inclusion of steroid and antiepileptic drugs in the treatment. The patient is under follow-up. An evaluation of the effectiveness of treatment with painkillers has been planned.
3. Discussion
The styloid process is a bony structure coming out from the temporal bone anteriorly from the stylomastoid foramen. It is clinically significant because of the structures surrounding it, and especially because the tip of the styloid process is located close to the external carotid artery laterally and also it has proximity to the internal carotid artery, the internal jugular vein, the jugular part of the sympathetic trunk and the V, VII and IX-XII cranial nerves [
8,
9].
The etiopathogenesis of Eagle’s syndrome has not been fully elucidated, but it is associated with the compression of the elongated styloid process on the above-mentioned cranial nerves. In some cases, it was diagnosed after tonsillectomy or after direct trauma [
5,
10]. Dental procedures are also suspected to be the cause of iatrogenic ES [
11].
It is assumed that the styloid process measures 2.5–3 cm in length; when it surpasses 3 cm, it is elongated. Nevertheless, some analysis shows that in around 15% of cases shorter styloid process might also cause ES symports [
2,
5].
There are two main types of Eagle’s syndrome—the “classic type” and the “stylo-carotid artery type” [
8,
12]. The first one presents typical symptoms such as a persistent sore throat with a foreign body sensation, dysphagia, taste disturbances, change in tone of voice or trismus.
The stylo-carotid artery type symptoms are caused by the pressure of the styloid process on the jugular vessels. Pressure on the internal carotid artery can lead to pain radiating along the artery’s course, while pressure on the external carotid artery causes facial pain.
Compression-induced blood flow restriction in the internal carotid artery can cause neurological disorders, ranging from nausea and fainting to aphasia and visual disturbances. There are several cases of bilateral carotid dissection, ischemic strokes secondary to Eagle’s syndrome [
3,
5,
13].
An elongated styloid process might cause venous reflux obstruction and, in effect, internal jugular stenosis [
14,
15].
The diagnosis of Eagle’s syndrome is usually based on a physical examination by palpation of the elongated styloid process and radiographs. The X-ray testing of the styloid process is enough to determine the length of the process; however, CT enables the precise evaluating of the anatomical relationship between the process and surrounding structures, such as nerves and blood vessels and now is treated as a “gold standard” [
16,
17]. It is accepted that multiple row CT and 3D reconstruction is the best method of diagnosing Eagle syndrome [
5,
18,
19].
Treatment for Eagle syndrome includes non-invasive treatment and surgery, and it depends on the patient’s symptoms. Non-invasive treatment includes painkillers, injecting steroids and/or antiepileptic drugs. Surgical treatment can shorten the elongated styloid process by oral or external access [
5,
15,
16,
19,
20]. In this case, the patient is treated with painkillers. The evaluation of the effectiveness of the treatment is planned.
4. Conclusions
Eagle syndrome is a rare clinical condition that is associated with styloid process elongation. Imaging diagnostics like computed tomography is a valuable tool for diagnosis and implementation of appropriate treatment.
Author Contributions
Investigation, P.J. and M.P. (Maria Pawłowska); resources, I.W.; writing—original draft preparation, I.W.; writing—review and editing, M.P. (Małgorzata Poręba) and P.G.; visualization, P.J. and P.G.; supervision, R.P. and M.P. (Małgorzata Poręba). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The manuscript contains a presentation of the description of diagnostic tests of a selected patient; the work does not describe a medical experiment—the opinion of the bioethics committee was not required.
Informed Consent Statement
The authors certify that they have obtained all appropriate patient consent.
Data Availability Statement
The study did not provide any data that could be used as a database.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Eagle, W.W. Elongated styloid processes: Report of Two Cases. Arch. Otolaryngol. 1937, 25, 584–587. [Google Scholar] [CrossRef]
- Bahgat, M.; Bahgat, Y.; Bahgat, A. Eagle’s syndrome, a rare cause of neck pain. BJM Case Rep. 2012, 2012, bcr2012006278. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, S.; Farooq, M.U.; Gorelick, P.B. Ischemic Stroke Secondary to Stylocarotid Variant of Eagle Syndrome. Neurohospitalist 2019, 9, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Costantinides, F.; Vidoni, G.; Bodin, C.; Di Lenarda, R. Eagle’s Syndrome: Signs and Symptoms. CRANIO® 2013, 31, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Lisan, Q.; Rubin, F.; Werner, A.; Guiquerro, S.; Bonfils, P.; Laccourreye, O. Management of stylohyoid syndrome: A systematic review following PRISMA guidelines. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2019, 136, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Ogura, T.; Mineharu, Y.; Todo, K.; Kohara, N.; Sakai, N. Carotid artery dissection caused by an elongated styloid process: Three case reports and review of the literature. NMC Case Rep. J. 2014, 2, 21–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, M.K.; Kim, D.W.; Yang, J.Y. Non Surgical Treatment of Eagle’s Syndrome—A Case Report. Korean J. Pain 2013, 26, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Terayama, H.; Miyaki, Y.; Kiyoshima, D.; Qu, N.; Kanae, U.; Tanaka, O.; Naito, M.; Sakabe, K. A gross anatomical study of the styloid process of the temporal bone in Japanese cadavers. Folia Morphologica 2021. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Greco, F.; De Corso, E.; Lucidi, D.; Deli, R.; D’addona, A.; Paludetti, G. Eagle’s Syndrome, from clinical presentation to diagnosis and surgical treatment: A case report. Acta Otorhinolaryngol. Ital. 2018, 38, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Blatt, N.; Jacob, J.; Gupta, N.; Kumar, Y.; Smith, S. Provoked Eagle syndrome after dental procedure: A review of the literature. Neuroradiol. J. 2018, 31, 426–429. [Google Scholar] [CrossRef] [PubMed]
- Piagkou, M.; Anagnostopoulou, S.; Kouladouros, K.; Piagkos, G. Eagle’s syndrome: A review of the literature. Clin. Anat. 2009, 22, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Ikenouchi, H.; Takagi, M.; Nishimura, A.; Yamaguchi, E.; Koge, J.; Saito, K.; Toyoda, K.; Koga, M. Bilateral carotid artery dissection due to Eagle syndrome in a patient with vascular Ehlers-Danlos syndrome: A case report. BMC Neurol. 2020, 20, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Aldakkan, A.; Dunn, M.; Warsi, N.M.; Mansouri, A.; Marotta, T.R. Vascular Eagle’s Syndrome: Two Cases Illustrating Distinct Mechanisms of Cerebral Ischemia. J. Radiol. Case Rep. 2017, 11, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Sun, Y.; Chan, C.C.; Fan, C.; Ji, X.; Meng, R. Internal jugular vein stenosis associated with elongated styloid process: Five case reports and literature review. BMC Neurol. 2019, 19, 112. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.H.; Yoon, T.M.; Lee, J.K.; Lim, S.C. The role of 3D-printing technology in the diagnosis of Eagle syndrome: A case report. Medicine 2018, 97, e9989. [Google Scholar] [CrossRef] [PubMed]
- Badhey, A.; Jategaonkar, A.; Kovacs, A.J.A.; Kadakia, S.; De Deyn, P.P.; Ducic, Y.; Schantz, S.; Shin, E. Eagle syndrome: A comprehensive review. Clin. Neurol. Neurosurg. 2017, 159, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Farina, R.; Foti, P.V.; Pennisi, I.; Conti, A.; Meli, G.A.; Vasile, T.; Gozzo, C.; Tallamona, E.; Inì, C.; Palmucci, S.; et al. Stylo-Jugular Venous Compression Syndrome: Lessons Based on a Case Report. Am. J. Case Rep. 2021, 22, e932035. [Google Scholar] [CrossRef] [PubMed]
- Raina, D.; Gothi, R.; Rajan, S. Eagle syndrome. Indian J. Radiol. Imaging 2009, 19, 107–108. [Google Scholar] [CrossRef] [PubMed]
- Cohn, J.E.; Scharf, J. Eagle Syndrome. J. Osteopath. Med. 2018, 118, 629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeckler, S.R.; Betancur, A.G.; Yaniv, G. The eagle is landing: Eagle syndrome—An important differential diagnosis. Br. J. Gen. Pract. 2012, 62, 501–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).