Abstract
Vaccination against the coronavirus disease 2019 (COVID-19) started in early December of 2020 in the USA. The efficacy of the vaccines vary depending on the SARS-CoV-2 variant. Some countries have been able to deploy strong vaccination programs, and large proportions of their populations have been fully vaccinated. In other countries, low proportions of their populations have been vaccinated, due to different factors. For instance, countries such as Afghanistan, Cameroon, Ghana, Haiti and Syria have less than of their populations fully vaccinated at this time. Implementing an optimal vaccination program is a very complex process due to a variety of variables that affect the programs. Besides, science, policy and ethics are all involved in the determination of the main objectives of the vaccination program. We present two nonlinear mathematical models that allow us to gain insight into the optimal vaccination strategy under different situations, taking into account the case fatality rate and age-structure of the population. We study scenarios with different availabilities and efficacies of the vaccines. The results of this study show that for most scenarios, the optimal allocation of vaccines is to first give the doses to people in the 55+ age group. However, in some situations the optimal strategy is to first allocate vaccines to the 15–54 age group. This situation occurs whenever the SARS-CoV-2 transmission rate is relatively high and the people in the 55+ age group have a transmission rate 50% or less that of those in the 15–54 age group. This study and similar ones can provide scientific recommendations for countries where the proportion of vaccinated individuals is relatively small or for future pandemics.
1. Introduction
The COVID-19 pandemic has generated more than 437 million confirmed cases and currently about 5.96 million deaths [1,2]. Various non-pharmaceutical intervention strategies have been designed in order to try to slow down the COVID-19 pandemic [3,4,5,6]. The factors that affect SARS-CoV-2’s spread around the world are many, and some of their effects are currently uncertain [7,8,9,10,11]. These factors include social behavior, non-pharmaceutical interventions and vaccines. Other important factors include SARS-CoV-2 variants and immunocompetence [12,13,14]. The study of the dynamics of the spread of SARS-CoV-2 is of paramount importance for public health. Obviously the most important aims are to save lives, and avoid hospitalizations and long term health consequences. Besides these main aspects, the COVID-19 pandemic has had profound economical and psychological impacts on people’s lives worldwide.
Forecasting the consequences of the COVID-19 pandemic has been extremely difficult due to the great number of factors that affect its dynamics [15,16,17,18]. Moreover, with the appearance of vaccines against SARS-CoV-2, the forecasting has been even more difficult [19,20,21,22,23,24,25,26]. Forecasting of epidemics related to influenza and other viruses is less difficult, since social behavior has not been changed much due to them, since those viruses are less lethal and/or have been around for a longer time [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41].
During 2020 and 2021, several countries, including the USA, the UK and European nations, have deployed different vaccination campaigns, and their populations have high percentages of vaccinated people [42]. The vaccine campaigns have been different in different countries due to several factors, such as vaccine availability, prioritization and willingness of people to be vaccinated. The design of a vaccination program needs to take into account different aspects, such as vaccine availability, human resources, vaccination rate, age, geographical factors, immune system, health status and even type of vaccine [6,43,44,45,46]. Thus, an optimal vaccination campaign needs to consider the aforementioned factors. The governments of the USA and the UK have implemented different vaccination strategies, and some researchers have been investigating the optimal vaccination programs [47,48,49,50,51]. It has been found that the vaccination rate and the efficacy of the vaccine are the main factors in reducing some health outcomes, such as number of deaths, number of infected and hospitalizations [25,44,45,52,53,54]. For instance, in [53] the author found that an incidence-minimizing vaccination strategy is highly sensitive to vaccine efficacy, and vaccines with lower efficacy should be administered to teenagers and adults aged 50–59 years. Some researchers have studied the effects of delayed second doses on important health outcomes, such as death [6,48,50,51,55].
National regulatory authorities have granted emergency use authorizations for twenty-two vaccines. Six of those have been approved for emergency or full use by at least one WHO-recognized, stringent regulatory authority [56]. The first vaccine used against SARS-CoV-2 was developed by the the Gamaleya Research Institute of Epidemiology and Microbiology in Moscow (widespread use on August 2020); and on December 2020, the United Kingdom granted emergency use authorization for BNT162 developed by Pfizer and BioNTech [57]. The efficacy of the different vaccines against the SARS-CoV-2 vary and also depend on the SARS-CoV-2 variant.
Mathematical models have been used to study many epidemics (including the COVID-19 pandemic) and predict different health outcomes [58,59,60,61,62,63]. The models can be used to investigate the effects of non-pharmaceutical interventions on important aspects without the need for making forecasts, which is a more complex issue. In this work, we were interested in studying different vaccination strategies in regard to which groups to vaccinate first. Different mathematical models that include vaccinated people and take into account the efficacy of the vaccine have been developed [64,65,66,67]. For instance, in [65] the authors proposed a stochastic epidemic model, and they found that white noise can result in the extinction of the disease even with a smaller reproduction number. In all these works it has been shown that vaccination can reduce the burden of the disease. Previous studies have proposed mathematical models to investigate vaccination strategies specifically [6,48,51,55,68]. Some studies found that a delayed second dose strategy might be the optimal strategy under some circumstances and always under the assumption that there is a limit to vaccine availability [6,48,51,53,55]. Countries such as Afghanistan, Haiti and Syria have low percentages of their populations fully vaccinated.
In this article, we develop two nonlinear mathematical models of COVID-19 transmission that take into account the age structure of the population in order to study the optimal vaccination strategy under different situations. We study many scenarios with different vaccine availability levels and levels of vaccine efficacy. The aim of this study is to provide scientific guidelines for countries where the proportions of vaccinated individuals are relatively small, or for future pandemics. Our aim here is not to precisely forecast the COVID-19 pandemic, but rather to understand the effects of using different vaccination strategies on paramount health outcomes, such as number of deaths. That is, we do not present an accurate forecast of the number of deaths at some particular future time. Besides the priority target age group, to design the optimal vaccination strategy there are other factors to consider. Including all of them in one study is complex and might not provide a clear picture of the effects of all those factors. Choosing a priority target subpopulation is something that governments can relatively easily manage or design. Here we also consider scenarios where the vaccination pace is different; and this is related to vaccine availability, human resources attached to the inoculation process and the willingness of people to be vaccinated [25,69,70,71]. It is important to mention that many countries currently have low percentages of their populations vaccinated, and obtaining scientific support for designing the optimal vaccination program is of paramount importance under the limitations of vaccine availability. An interesting previous work proposed a continuous age-structured model to study the COVID-19 pandemic [72]. The authors used the age-structured model, since data show that the fatality of the disease is high in elderly people. The authors also studied the impact of a shortage of proper personal protective equipment on the spread of the disease [72]. In [73], the authors developed an interesting agent-based model for COVID-19 disease dynamics where the population has a social structure. These factors, such as age and social, are important for studying the COVID-19 pandemic.
One main advantage of mathematical models is that many different simulations can be done, allowing the investigation of various factors under a variety of scenarios. In this article, we construct two mathematical models based on nonlinear ordinary differential equations, where each variable represents different subpopulations with regard to COVID disease progression, vaccination status and age group. We numerically solve the differential equations with different parameter values in order to provide insight into the optimal vaccination strategy with regard to priority target age group. The models include symptomatic and asymptomatic individuals. The inclusion of asymptomatic people is important, since they are crucial contributors to the dynamics of the COVID-19 pandemic [11,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88]. Thus, overall, we propose a mathematical approach to investigate a variety of vaccination strategies under different scenarios to consider the variability of situations in different countries where the transmission rates vary due to social behavior, the prevalences of different SARS-CoV-2 variants, and vaccine availability. Health authorities can benefit from the results presented in this study. Thus, this type of study can provide further insights about vaccination strategies against SARS-CoV-2.
2. Materials and Methods
The mathematical models presented here are based on a nonlinear system of ordinary differential equations. The models divide the total population into different subpopulations or compartments based on age group, the COVID-19 progression and vaccination status. The compartments or subpopulations considered are: susceptible, infected (able to infect others), asymptomatic (able to infect others), recovered (not infectious) and vaccinated. The mathematical models consider transitions or flow of individuals through the aforementioned compartments. The models assume that recovered individuals have permanent immunity against reinfection during a period of study that is shorter than one year. In reality this is not totally true, but the percentage of breakthrough cases before one year is very low. We also assume that only susceptible individuals can be vaccinated.
The individuals transit from the susceptible subpopulation to vaccinated if they receive the vaccine. Both models assume a simplification of reality where there are vaccines that are one or two doses. The models consider the possibility of infection for individuals who are vaccinated regardless of whether they are symptomatic or asymptomatic, even though these cases are very low with comparison to infections of unvaccinated people. The mathematical models implicitly assume that transitions follow an exponential distribution. Although this is standard in this type of model, other models consider different distributions, such the Erlang distribution, which makes the models more complex and increases the number of parameters [89,90,91,92,93]. Both mathematical models consider that only symptomatic individuals (vaccinated or not) can die due to COVID-19 [4,94,95,96]. This last health outcome is of paramount importance for the comparison of different vaccination strategies, and is used in this study and others extensively [4,47,48,49,51,53,97,98,99,100].
The first mathematical model developed is based on a -type epidemiological model. The model includes parameters related to the vaccine efficacy, vaccination pace and vaccine availability. The values of these parameters can be used to generate and investigate infinitely many different scenarios. Thus, we are able to approximate the situations of different places [63,69,70,101,102,103,104,105,106]. Figure 1 depicts the transits between the different subpopulations based on the disease and the vaccination status of the individuals.
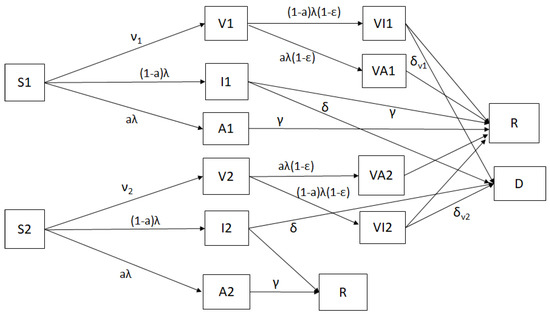
Figure 1.
Diagram for the COVID-19 mathematical model including a vaccination program (1). The boxes represent the different classes and the arrows the transitions between these classes.
Next, the first mathematical model is given by the following differential equation with
where is the vector of the different states of the subpopulations that compose the total population. Thus, the dynamics of COVID-19 disease in the human population is governed by the following ODE system
and the initial conditions in written as
and represents the number of deaths caused by the disease. The expression is the force of infection, which is given by
and describes the rate at which a susceptible person becomes infected through interaction with another person who can spread the disease. In this case, it is a linear combination of the classes that can transmit the virus and is measured by the transmission rates.
The state variables, and , represent the susceptible subpopulations from the 15–54 and age groups. When a susceptible and an infectious individual come into infectious contact, the susceptible individual contracts the disease and transitions to the asymptomatic or infected subpopulation. The subpopulations and include individuals that are able to infect others, but the subpopulations and include individuals that are asymptomatic. The model disregards natural births and deaths, since it focuses on a short period for the deployment of the vaccination program.
Both models consider two subpopulations of vaccinated people: The first, , includes the individuals that have been vaccinated from the 15–54 age group, and includes those vaccinated from the age group. Based on the efficacies of the vaccines, those vaccinated can become infected with various probabilities. The first model that we consider assumes a constant proportion vaccination rate, i.e., a proportion of the subpopulations and is vaccinated per day or per unit time. Delivering a specific number of inoculations per day is difficult, since it depends on many factors, such as willingness to be vaccinated, human resources and vaccine availability. Those vaccinated individuals from the 15–54 age group can still get infected and become part of subpopulations and (asymptomatic). Similarly, those vaccinated individuals from the age group can still get infected and become part of subpopulations and (asymptomatic). The model assumes that people in states , , and are not able transmit SARS-CoV-2. The compartment represents the number of deaths due to the SARS-CoV-2 virus.
The mathematical model (1) has an advantage from an analysis point of view, since the positivity of the subpopulations is guaranteed for any time, as we will see in the next section. However, it has the disadvantage that the number of vaccinated people per unit time decreases, since the susceptible population decreases. This does not always occur in reality, since at the beginning of the vaccination programs, it is common to have limited availability of vaccines. Therefore, we propose a second mathematical model where the number of vaccines available per day is fixed. This alternative model has the same subpopulations, but the terms and are replaced by and . Thus, we achieve a constant fixed number of vaccinations per day or per unit time. From a mathematical point of view, negative values for the susceptible subpopulations and can be obtained. However, to avoid a long simulation time or period of study, negative subpopulations do not arise. In reality what happens is that some part of the population will not be vaccinated due to various reasons. For a long term simulation a more complex model that includes people that are not willing to get vaccinated and demographics is necessary. Figure 2 shows the cumulative number of vaccine doses administered in different countries. If we assume the second mathematical model, the graph should look similar to a line due to the fixed amount of vaccinations per unit time. On the other hand, if the first mathematical model is used, the graph should be similar to an exponential curve due to the fact that the number of inoculations per unit time is proportional to the number of susceptible individuals. Notice that in the case of USA, the graph can be approximated by a line or even by a quadratic, concave, downward trend, which is the opposite of what happens when the vaccination is proportional to the susceptible subpopulations. Thus, for the USA the second model might be more realistic in order to consider the vaccination program implemented.
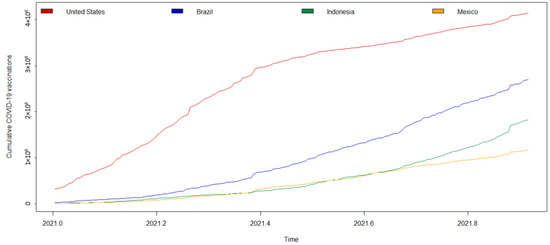
Figure 2.
Cumulative numbers of vaccine doses administered in different countries.
In this study, we used parameter values that can be found in the scientific articles and on the CDC’s website, even though there are some uncertain values, such as the proportion of asymptomatic infections. In this work, we were interested in finding the impact of allocating vaccines to two different age groups. In addition, we considered other factors, such as the vaccination pace, virus transmissibility and vaccine efficacy. All these factors play important roles in the outcomes regarding infections and deaths. In the in silico simulations we assumed that the transmission rates of SARS-CoV-2 were constant from the beginning of the period of study. Implicitly, this assumed that social behavior was in a steady state before implementing the vaccination campaign. In reality, it has been mentioned that people might change behavior (on average) when a vaccination program is well advanced due to a perception of less risk [6]. We assumed that social contacts would not change because many health policies would have been already long implemented before the vaccination campaign had begun. We also considered that for a short time horizon of study (less than year), the immunity provided by the vaccines does not diminish.
For the scenarios studied here, we tried to replicate the conditions in the USA just before the vaccination campaign started. However, since the general results are qualitative, the conclusions presented here can be applied to other countries. For the proportion of asymptomatic cases, we chose a conservative approach in which the percentage of asymptomatic infections was [2]. For the parameters related to transmissibility of the different subpopulations, we assumed a variety of values that have been used in some studies [4,81,107,108,109,110]. In particular, we assumed that the transmissibility of the age group is half that of the 15–54 age group. This can be justified by the fact that younger people are less reluctant to stay at home or take preventive measurements. For instance, in South Korea, the 20–29 age group had the highest transmission incidence per capita [53]. On the other hand, the case–fatality rate is highest among the elderly [53]. Thus, based on data related to the USA we assumed a case-fatality rate ten times higher for the age group compared to the 15–54 age group.
Finally, for the initial conditions we tried to replicate the conditions of the USA, but initial conditions can be changed easily [1]. Moreover, for any country for which the percentages of vaccinated and of recovered people are low, the qualitative results would be similar due to the structure of the population. In Table 1 we present the initial conditions. The initial vaccinated people was taken as zero. Thus, the initial susceptible subpopulation was given by . This can be modified to consider, for instance, that initially some part of the population is vaccinated.

Table 1.
Initial conditions for the subpopulations.
Positive Solutions
The mathematical model (1) has been designed for a relative short period, since the behavior of people reluctant to be vaccinated has not been taken into account and this affects the long term dynamics in a crucial way. Despite the mathematical analysis presented in this subsection being more devoted to long term dynamics, it still helps to provide insights into the dynamics of the COVID-19 pandemic, especially the initial part. Thus, we decided to include a brief mathematical analysis of the first proposed model (1). From a fundamental theory of differential equations (see [111,112]), the solution of system (1) exists and it is unique for the initial conditions given by (2). Indeed, the system (1) can be written as and it is represented by vector notation as
and the initial conditions showed in (2). We use the following theorem:
Theorem 1.
Suppose Ω is an open set in and is continuous, and is locally Lipschitz in in each open set in Then for each there exists a unique solution of the initial value problem (1) in some open interval containing
Proof.
See [112] (p. 10). □
Let be the Banach space of continuous functions mapping the interval into with the sup-norm. The function F given by (5) is defined in and is continuous satisfying a local Lipschitz condition. Indeed, if being a compact set,
and such that , we obtain that
where Then, by Theorem 1 for any there exists a unique solution of the system (1) such that Since the system of equations given by (1) represents a model of populations from the biological point of view, its solutions must be positive for all positive initial conditions according to (2). Therefore, positivity and boundedness of the solution of the system (1) in must be guaranteed. Now, we will show these properties in the following statements.
Theorem 2.
Proof.
From the first equation of system (1), one gets that
Therefore, if Thus, from the second equation of system (1), it follows that
Applying the Gronwall inequalities, we obtain that
Accordingly, for In the same way, we can prove that if and for On the other hand, from the equations (third-sixth) and (ninth-twelfth) of model (1) we have
where
Therefore,
Since
is positive, for Next, taking the third equation of system (1) and if we suppose that exists a such that and one gets
which is a contradiction. Hence, for all With this methodology we can prove that for all Furthermore, for □
Note: The second mathematical model considers that the amount of vaccine available per day is fixed and the terms and are replaced by and . Therefore, positivity and boundedness cannot be guaranteed for the second model. However, in practice some part of the population will not be vaccinated and using a relative initial short period of study avoids negative subpopulations.
3. Results
We performed in silico simulations with various scenarios in order to provide a great spectrum of health outcomes under different circumstances. We varied the vaccination pace, transmissibility (to consider different SARS-CoV-2 variants and different social behaviors) and vaccine efficacy (to consider different brands and variants). The transmission rate of SARS-CoV-2 varies depending on non-pharmaceutical interventions and social behavior. We considered two main cases regarding the transmission rate, one with high transmission and another with low transmission. Both cases had constant transmissibility. The numerical simulations were based on the mathematical model (1), and we computed the number of deaths under different scenarios. Table 1 shows the initial conditions and Table 2 the numerical values of the parameters.

Table 2.
Parameters’ values used in the simulations.
We performed a variety of numerical simulations with different efficacies for the vaccines in order to consider the different types of vaccines and the fact that SARS-CoV-2 variants affect the efficacy of the vaccines. In addition, we considered a variety of inoculation rates, but assumed that these rates were constant over the period of study.
3.1. Scenarios with Proportional Vaccination Rates
The first scenario that we considered is when the vaccination program features a proportional vaccination rate. In this type of program there are more vaccinations of susceptible individuals at the beginning of the period of study. Thus, the maximum number of doses are required when the vaccination program starts. Figure 3 shows the dynamics of several subpopulations without a vaccination program. The susceptible subpopulations and decrease due to the fact that susceptible people get infected and transit to the infected subpopulations (either symptomatic or asymptomatic). The infected subpopulations decrease, since the transmission rate in this scenario is low and the situation is under epidemic control. Figure 4 shows the dynamics of several subpopulations with a proportional vaccination rate program. It can be observed that the susceptible subpopulations and decrease faster than the previously considered case since now susceptible individuals transit to the vaccinated subpopulations ( or ) and people are still getting infected (but less since there are less susceptible individuals).
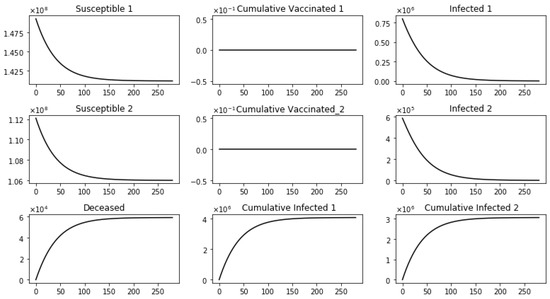
Figure 3.
Dynamics of several subpopulations without a vaccination program.
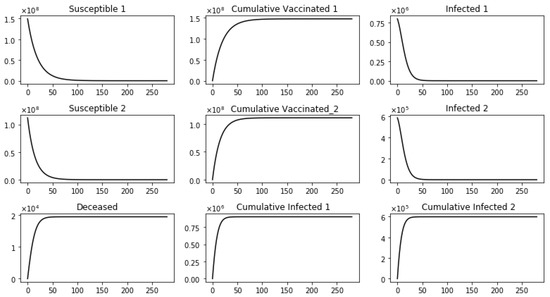
Figure 4.
Dynamics of several subpopulations with a proportional vaccination rate program. This scenario considers a transmission rate such that the basic reproduction number is greater than one. We consider a vaccine efficacy of 90%, vaccination rate for age group one () of and vaccination rate for age group two () of .
Figure 5 shows the number of deaths and infected individuals from the two different age groups. This scenario considers that the transmission rate of people in the 55+ age group is half of the transmission rate of 15–54 years-old due to the fact that older people in general take more protective measures against getting the virus. In addition, the values of the transmission rate and the proportion of vaccine devoted to each age group were varied. We considered a vaccine efficacy of 90%, a maximum constant proportional vaccination rate for age group one of and for age group two . The rate is higher for 55+ age group in order to take into consideration that there are fewer people in that age group, and therefore, a greater proportion of this subpopulation can be vaccinated under the assumption of limited vaccines. It can be seen, as expected, that increasing the proportion of vaccinated people for either age group reduces the number of deaths. Moreover, it reduces the number of infected people for each age group. If the proportion is increased, the number of infected people from age group 1 is reduced more than the number of infected people of the 55+ age group. Conversely, if the proportion is increased, the number of infected people from the 55+ age group is reduced more than the number of infected people of the 15–54 age group. These results are intuitively correct, but our aim was to find the optimal allocation of vaccines for each age group. Using a constant proportion vaccination rate does not allow one to consider a fixed amount of vaccines per unit time due to the changes in the sizes of the susceptible populations and . Despite this, Figure 5 shows that more deaths are averted when the constant proportion vaccination rate is increased. Thus, the results suggest that first allocating more vaccines to the 55+ age group is better in order to avert more deaths.
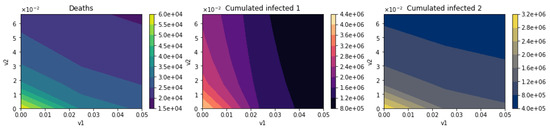
Figure 5.
Number of deaths and infected individuals from the two different age groups. This scenario considers that the transmission rate of people in the 55+ age group is half of the transmission rate of 15–54 years-old. Vaccine efficacy is assumed 90%, and .
Figure 6 shows the number of vaccinated individuals from the 55+ age group at the end of simulation and the total number of vaccinated for each age group. As expected, the vaccinated people for each age group increases uniformly as the constant vaccination rate increases for each age group, respectively. This uniformity does not occur for the infected people in each age group, as can be observed in Figure 5. This is due to the fact that even if the vaccination program does not allocate vaccines for one of the age groups, the number of deaths for that particular age group is reduced, since fewer people from the other group are going to be able to spread the virus. This is what can be called collective societal benefits of vaccinations, and it is related to herd-immunity.
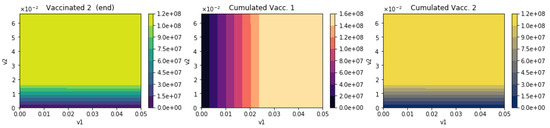
Figure 6.
Number of vaccinated individuals from the 55+ age group at the end of simulation and the total number of vaccinated for each age group. The transmission rate of people in the 55+ age group is half of the transmission rate of 15–54 years-old. Vaccine efficacy is assumed 90%, and .
3.2. Scenarios with Fixed Numbers of Vaccines
Now, we consider a more realistically accurate vaccination program where the number of vaccines available per unit time is limited or fixed. Thus, the aim is to find the optimal allocation per unit time for this fixed amount of vaccine for each age group. In this case the mathematical model (1) just needs a small change. This alternative model has the same subpopulations, but the terms and are replaced by and . Thus, we achieve a constant fixed number of vaccines per day. We study here more scenarios than in the previous section since this situation is closer to reality with regard to number of inoculations per day. We consider different scenarios varying the allocation of vaccines for each age group, the transmission rate with low and high transmission, vaccination pace, the probability of infection for 55+ age group with respect to the 15–54 age group and finally the efficacy of the SARS-CoV-2 vaccine. All these factors vary for each region or country, and thus the qualitative analysis presented here allows the consideration of different situations related to different countries. As has been mentioned, the main metric used here to measure the optimality of the vaccine program is the number of deaths under each vaccination strategy. Next we will evaluate different scenarios considering always a parameter p that denotes the proportion of vaccines allocated to 55+ age group. Conversely, the proportion of vaccines allocated for 15–54 age group is given by ; thus a value of means that all the available vaccines are allocated to 55+ age group.
3.2.1. Scenarios Varying Vaccination Pace
The first scenario that we consider is varying the vaccination pace which translates on varying the amount of vaccines inoculated per unit time (per day) and as well the allocation of vaccines to each age group. Figure 7 shows the number of deaths and the cumulative number of infected people for each age group. We can see that if the proportion of vaccines allocated for one age group is increased then the number of infected people for that specific age group increases. However, the main finding is that increasing the proportion of inoculations in the 55+ age group decreases the total amount of deaths due to SARS-CoV-2. This result suggest that the optimal vaccination program should vaccinate first the people from 55+ age group. The explanation for this is that these people have a higher case fatality rate (CFR). We need to keep in perspective that in this scenario the mathematical model assumes that the probability to get infected for people from 55+ age group is half of that of 15–54 age group. We will vary this probability in other scenarios in order to provide more insightful analysis. Figure 8 shows the number of deaths and the cumulative number of infected people for each age group, but now with a higher SARS-CoV-2 transmission. In this case for low vaccination paces (≈200,000–400,000 doses per day) the optimal allocation of vaccines is not to first inoculate individuals from the 55+ age group. However, the total number of deaths does not vary significantly when the vaccines are allocated in different proportions among the the age groups. On the other hand, for high vaccination paces (>800,000 doses per day) the optimal strategy to avert more deaths is to allocate the vaccines to people in the 55+ age group. Thus, these scenarios show that the optimal vaccine strategy varies depending on the vaccination pace and the SARS-CoV-2 transmission.
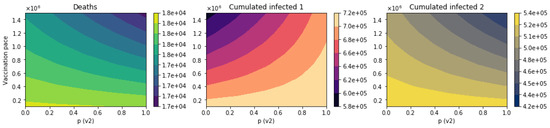
Figure 7.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a relatively low SARS-CoV-2 transmission rate and vaccine efficacy of 90%. The factors that are varied are the vaccination pace and the proportion of vaccines allocated to each age group.
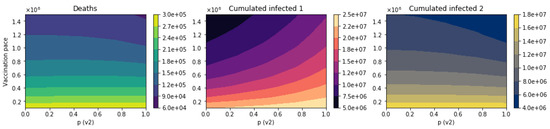
Figure 8.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a relatively high SARS-CoV-2 transmission rate and vaccine efficacy of 90%. The factors that are varied are the vaccination pace and the proportion of vaccines allocated to each age group.
3.2.2. Scenarios Varying the Transmission Rate of the Age Group
The second scenario that we consider is varying the transmission rate of age group under a low SARS-CoV-2 transmission rate. Figure 9 shows the total number of deaths and the cumulative number of infected people for each age group. We can see on the y-axis the ratio of transmission rate of 15–54 age group and . Thus, the ratio means that the SARS-CoV-2 transmission rate of 55+ age group is 25% of the one of 15–54 age group. In this case the optimal strategy is to first allocate the vaccines to people in the 55+ age group. Figure 10 shows the case when the SARS-CoV-2 transmission is relatively high. In this case for a large ratio r the optimal strategy is to first vaccinate the people in 15–54 age group. This strategy is the opposite to what some countries have done. On the hand, for low ratio r the optimal strategy to avert more deaths is to allocate the vaccines to people in the 55+ age group. This is explained by the fact that under a high contagiously SARS-CoV-2 and individuals in the 55+ age group highly protected it is better to avoid infections of individuals in 15–54 age group since they are able to spread SARS-CoV-2 faster and then cause more deaths. Thus, having a highly contagious SARS-CoV-2 variant can affect which is the optimal strategy. With regard to total infected cases, the results are similar to those for total deaths.
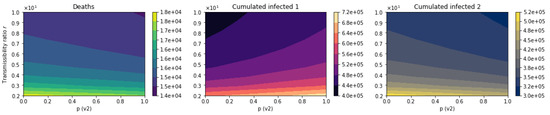
Figure 9.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a relatively low SARS-CoV-2 transmission rate. The factors that is varied is the transmission rate of 55+ age group.
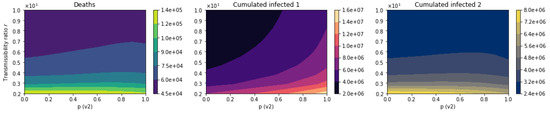
Figure 10.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a relatively high SARS-CoV-2 transmission rate. The factor that is varied is the transmission rate of 55+ age group.
We included one more scenario with higher SARS-CoV-2 transmission to see more clearly how the optimal vaccine strategy varies. Figure 11 shows that the larger the ratio r, the more clear it becomes that the optimal strategy is to first vaccinate the people in the 15–54 age group.
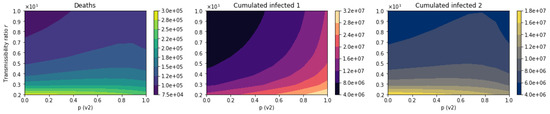
Figure 11.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a high SARS-CoV-2 transmission rate. The factor that is varied is the transmission rate of 55+ age group.
3.2.3. Scenarios Varying SARS-CoV-2 Transmission Rate
The third scenario that we consider is varying the SARS-CoV-2 transmission rate for all age groups. Figure 12 shows the total number of deaths and the cumulative number of infected people for each age group when the transmission ratio is (transmission rate of 55+ age group is 50%). In this case it is clear that when SARS-CoV-2 transmission rate is not high the the optimal strategy is to first allocate the vaccines to people in the 55+ age group. Figure 13 shows the case when the ratio is . The optimal strategy is still to first vaccinate the people in the 55+ age group. However, the worst outcome is when the allocation of the first vaccines is approximately even (50–90% for the 55+ age group) for both age groups. This result is important for designing the most suitable vaccination strategy.
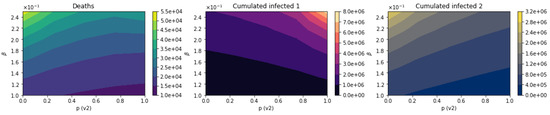
Figure 12.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a ratio . The factor that is varied is the SARS-CoV-2 transmission rate.
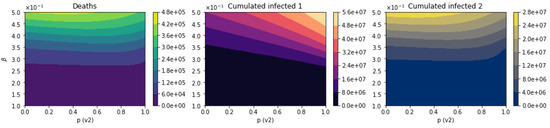
Figure 13.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a ratio . The factor that is varied is the SARS-CoV-2 transmission rate.
3.2.4. Scenarios Varying the Efficacy of the Vaccine
The last scenario that we consider is varying the efficacy of the vaccine against SARS-CoV-2 under a relatively high SARS-CoV-2 transmission rate. Figure 14 shows clearly that the optimal strategy is to first allocate the vaccines to people in the 55+ age group. Figure 15 shows the case when the ratio (transmission rate of 55+ age group is 25%), and the optimal strategy is still to first vaccinate the people in the 55+ age group. However, it can be seen that the worst strategy is to allocate approximately evenly the vaccines between the people of both age groups. This result is important from a public health point of view, since some countries have implemented similar strategies to allocate the vaccines. Thus, some countries might be causing the worst scenario for averting deaths.
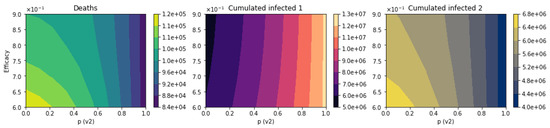
Figure 14.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a ratio . The factor that is varied is the efficacy of the vaccine.
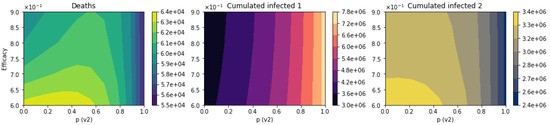
Figure 15.
Total number of deaths and the cumulative number of infected people for each age group. This scenario considers a ratio . The factor that is varied is the efficacy of the vaccine.
4. Discussion and Conclusions
Many countries have strong vaccination campaigns, and large proportions of their populations are fully vaccinated. However, not all countries have well advanced vaccination programs [2,42,101,116,117,118,119]. For instance, at this time countries such as Afghanistan, Algeria, Haiti and Turkmenistan have less than of their populations fully vaccinated. Different vaccination campaigns produce different public health outcomes [25,45,51,54,55,69]. The design of an optimal vaccination strategy is a complex problem, since there are many factors that affect the spread of SARS-CoV-2. There are vaccination campaigns that first allocate vaccines to health care workers or elderly people [97]. Thus, governments have implemented a variety of vaccination campaigns.
In this study, we constructed two mathematical models to study the optimal allocation of vaccines between the 15–54 and 55+ age groups. We varied several factors that affect public health outcomes of the vaccination programs. The factors that considered in this study were vaccine availability, vaccine efficacy, SARS-CoV-2 transmission rate, SARS-CoV-2 transmission rate of the 55+ age group and vaccination pace. We assessed the vaccination strategies using cumulative mortality and cumulative infective for each age group. The study of COVID-19 vaccination strategies is crucial to diminish the hospitalizations and deaths related to the COVID-19 pandemic [25,50,51,55,105,120,121].
For most of the scenarios we fixed the efficacy of the vaccine as 90%, even though it has been estimated that two of the most popular vaccines such as Pfizer-BioNTech and Moderna have an efficacy of approximately 95% [50]. It is important to mention that in reality the transmission rate under the current COVID-19 pandemic varies over time. Making a study with a time dependent SARS-CoV-2 transmission rate is extremely complex due to the high variability of social behavior of people. However, this behavior is more stable after more than year into the pandemic. Mathematical models in conjunction with in silico simulations give useful insights regarding the optimal vaccination strategy. In general in this study we considered two SARS-CoV-2 transmission rate scenarios: one with a relatively low one and another one with high. This, helps to apply the results of this study to a variety of countries.
Using two mathematical epidemiological models based on differential equations, we found that for most scenarios the optimal allocation of vaccines is to give the first doses to people in the 55+ age group. This result agrees with previous studies that used a different mathematical approach [49,122]. However, in particular situations the optimal strategy is to allocate vaccines to the 15–54 age group. This situation occurs whenever the SARS-CoV-2 transmission rate is relatively high and the people in the 55+ age group have a transmission rate 50% or less than that of the 15–54 age group. Another important situation that we found is that when the allocation of vaccines is approximately even between the two age groups, the worst results arise regarding the number of deaths. It is important to remark that despite this result, some countries have implemented this strategy.
The variations in the optimal strategy under different scenarios are partially due to the nonlinearity of the spread of the SARS-CoV-2 and the mathematical model. These nonlinearities have been correctly taken into account in previous studies [51,54,55].
The results presented here are qualitative and are not forecasts about the number of deaths for particular countries. Previous results have proven that accomplishing an accurate forecast regarding the outcomes of the COVID-19 pandemic is a very challenging problem due to the high variability of the social behavior of people [4,20,22,23,24,123,124]. Besides, including in the numerical simulations accurate vaccination rates is an extremely difficult task due to changes in government policies, the approval of new vaccines and accounting for the resources available for vaccine distribution. Nevertheless, we varied the vaccination rate in order to provide useful information towards improving and designing better vaccination campaigns.
The numerical simulations presented in this study considered a short time period. Thus, these did not deal with the complication of the resistance of a certain sector of the population to getting vaccinated [18,70,125,126].
As in any study involving mathematical models, there were natural limitations due to various ,reasons including the complexity of the real world. The results of using mathematical models are dependent on the assumptions and the underlying data. Thus, it is important to mention the limitations and hypotheses to avoid reaching wrong conclusions. Nonetheless, the findings are useful to scientifically support health policies [53,127,128,129,130,131,132,133,134]. The models presented here have some assumptions. One important one is that inoculation rates and SARS-CoV-2 transmission rates are time-invariant. We assumed that a steady state of social behavior had been reached before the start of the vaccination campaign, and was maintained during the simulation. The mathematical models presented here do not include demographic factors due to the short time period of study [135,136]. The period of study was assumed to be shorter than one year due to several factors—for instance, the waning of vaccine efficacy and natural immunity. In addition, we did not take into account the resistance of some people to getting vaccinated. If the waning of natural immunity against the SARS-CoV-2 is taken into account, then the developed mathematical models need to be changed. Similarly, if the protection of the vaccine is shorter than 8 months, the model presented here needs to be modified. In summary, more complex mathematical models are necessary to consider the appearance of new SARS-CoV-2 variants and waning immunity [21,54].
The results of this study provide scientific guidelines for countries where vaccination programs are starting or the percentage of vaccinated people is small. The results presented here are based on measuring certain public health outcomes, such as cumulative mortality and cumulative infected. The results presented here help to design optimal vaccination programs under constraints in the vaccine availability.
Finally, the results obtained in this work encourage health authorities to identify which scenario they have before designing the vaccination program. It has been suggested that age groups at higher risk also should be prioritized [55]. However, that vaccination program does not always produce optimal results. Future work should include further analysis of different vaccination programs and other mathematical models to consider other heterogeneities, such as comorbidities. Moreover, depending on ongoing research about the efficacy of the SARS-CoV-2 vaccine, future studies might require considering the waning of the immunity.
Author Contributions
Conceptualization, G.G.-P. and A.J.A.; Formal analysis, G.G.-P., M.R.C. and A.J.A.; Investigation, G.G.-P., M.R.C. and A.J.A.; Methodology, G.G.-P., M.R.C. and A.J.A.; Software, G.G.-P. and M.R.C.; Supervision, G.G.-P. and A.J.A.; Validation, G.G.-P., M.R.C. and A.J.A.; Visualization, G.G.-P. and M.R.C.; Writing—original draft, G.G.-P., M.R.C. and A.J.A.; Writing—review and editing, G.G.-P. and A.J.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors are grateful to the reviewers for their careful reading of this manuscript and their useful comments to improve the content of this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Johns Hopkins University and Medicine. 2022. Available online: https://coronavirus.jhu.edu (accessed on 1 March 2022).
- Centers for Disease Control and Prevention. 2020. Available online: https://www.cdc.gov/coronavirus/2019-nCoV/index.html (accessed on 1 March 2022).
- Asamoah, J.K.K.; Owusu, M.A.; Jin, Z.; Oduro, F.; Abidemi, A.; Gyasi, E.O. Global stability and cost-effectiveness analysis of COVID-19 considering the impact of the environment: Using data from Ghana. Chaos Solitons Fractals 2020, 140, 110103. [Google Scholar] [CrossRef]
- Ferguson, N.M.; Laydon, D.; Nedjati-Gilani, G.; Imai, N.; Ainslie, K.; Baguelin, M.; Bhatia, S.; Boonyasiri, A.; Cucunubá, Z.; Cuomo-Dannenburg, G.; et al. Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand; Imperial College: London, UK, 2020. [Google Scholar]
- Haushofer, J.; Metcalf, C.J.E. Which interventions work best in a pandemic? Science 2020, 368, 1063–1065. [Google Scholar] [CrossRef]
- Moore, S.; Hill, E.M.; Tildesley, M.J.; Dyson, L.; Keeling, M.J. Vaccination and non-pharmaceutical interventions for COVID-19: A mathematical modelling study. Lancet Infect. Dis. 2021, 21, 793–802. [Google Scholar] [CrossRef]
- Mandal, S.; Bhatnagar, T.; Arinaminpathy, N.; Agarwal, A.; Chowdhury, A.; Murhekar, M.; Gangakhedkar, R.R.; Sarkar, S. Prudent public health intervention strategies to control the coronavirus disease 2019 transmission in India: A mathematical model-based approach. Indian J. Med Res. 2020, 151, 190. [Google Scholar]
- Reis, R.F.; de Melo Quintela, B.; de Oliveira Campos, J.; Gomes, J.M.; Rocha, B.M.; Lobosco, M.; dos Santos, R.W. Characterization of the COVID-19 pandemic and the impact of uncertainties, mitigation strategies, and underreporting of cases in South Korea, Italy, and Brazil. Chaos Solitons Fractals 2020, 136, 109888. [Google Scholar] [CrossRef]
- Wang, X.; Pasco, R.F.; Du, Z.; Petty, M.; Fox, S.J.; Galvani, A.P.; Pignone, M.; Johnston, S.C.; Meyers, L.A. Impact of social distancing measures on coronavirus disease healthcare demand, central Texas, USA. Emerg. Infect. Dis. 2020, 26, 2361. [Google Scholar] [CrossRef]
- Pinky, L.; Dobrovolny, H.M. SARS-CoV-2 coinfections: Could influenza and the common cold be beneficial? J. Med. Virol. 2020, 92, 2623–2630. [Google Scholar] [CrossRef]
- Dobrovolny, H.M. Modeling the role of asymptomatics in infection spread with application to SARS-CoV-2. PLoS ONE 2020, 15, e0236976. [Google Scholar] [CrossRef]
- Zhang, X.; Tan, Y.; Ling, Y.; Lu, G.; Liu, F.; Yi, Z.; Jia, X.; Wu, M.; Shi, B.; Xu, S.; et al. Viral and host factors related to the clinical outcome of COVID-19. Nature 2020, 583, 437–440. [Google Scholar] [CrossRef]
- Ran, L.; Chen, X.; Wang, Y.; Wu, W.; Zhang, L.; Tan, X. Risk factors of healthcare workers with corona virus disease 2019: A retrospective cohort study in a designated hospital of Wuhan in China. Clin. Infect. Dis. 2020, 71, 2218–2222. [Google Scholar] [CrossRef]
- Yang, H.; Duan, G. Analysis on the epidemic factors for the corona virus disease. Zhonghua Yu Fang Yi Xue Za Zhi [Chinese J. Prev. Med. 2020, 54, E021. [Google Scholar]
- Block, P.; Hoffman, M.; Raabe, I.J.; Dowd, J.B.; Rahal, C.; Kashyap, R.; Mills, M.C. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nat. Hum. Behav. 2020, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Eker, S. Validity and usefulness of COVID-19 models. Humanit. Soc. Sci. Commun. 2020, 7, 1–5. [Google Scholar] [CrossRef]
- Jentsch, P.C.; Anand, M.; Bauch, C.T. Prioritising COVID-19 vaccination in changing social and epidemiological landscapes: A mathematical modelling study. Lancet Infect. Dis. 2021, 21, 1097–1106. [Google Scholar] [CrossRef]
- Qazi, A.; Qazi, J.; Naseer, K.; Zeeshan, M.; Hardaker, G.; Maitama, J.Z.; Haruna, K. Analyzing situational awareness through public opinion to predict adoption of social distancing amid pandemic COVID-19. J. Med. Virol. 2020, 92, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Altmann, D.M.; Boyton, R.J.; Beale, R. Immunity to SARS-CoV-2 variants of concern. Science 2021, 371, 1103–1104. [Google Scholar] [CrossRef]
- Roda, W.C.; Varughese, M.B.; Han, D.; Li, M.Y. Why is it difficult to accurately predict the COVID-19 epidemic? Infect. Dis. Model. 2020, 5, 271–281. [Google Scholar] [CrossRef]
- Gonzalez-Parra, G.; Martínez-Rodríguez, D.; Villanueva-Micó, R.J. Impact of a new SARS-CoV-2 variant on the population: A mathematical modeling approach. Math. Comput. Appl. 2021, 26, 25. [Google Scholar] [CrossRef]
- Holmdahl, I.; Buckee, C. Wrong but useful- what COVID-19 epidemiologic models can and cannot tell us. N. Engl. J. Med. 2020, 383, 303–305. [Google Scholar] [CrossRef]
- Jewell, N.P.; Lewnard, J.A.; Jewell, B.L. Caution warranted: Using the Institute for Health Metrics and Evaluation model for predicting the course of the COVID-19 pandemic. Ann. Intern. Med. 2020, 173, 226–227. [Google Scholar] [CrossRef]
- Kuniya, T. Prediction of the Epidemic Peak of Coronavirus Disease in Japan, 2020. J. Clin. Med. 2020, 9, 789. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Rodríguez, D.; Gonzalez-Parra, G.; Villanueva, R.J. Analysis of key factors of a SARS-CoV-2 vaccination program: A mathematical modeling approach. Epidemiologia 2021, 2, 140–161. [Google Scholar] [CrossRef]
- Walensky, R.P.; Walke, H.T.; Fauci, A.S. SARS-CoV-2 variants of concern in the United States—Challenges and opportunities. JAMA 2021, 325, 1037–1038. [Google Scholar] [CrossRef] [PubMed]
- Al-Qaness, M.A.; Ewees, A.A.; Fan, H.; Abd Elaziz, M. Optimized forecasting method for weekly influenza confirmed cases. Int. J. Environ. Res. Public Health 2020, 17, 3510. [Google Scholar] [CrossRef] [PubMed]
- Araz, O.M.; Bentley, D.; Muelleman, R.L. Using Google Flu Trends data in forecasting influenza-like–illness related ED visits in Omaha, Nebraska. Am. J. Emerg. Med. 2014, 32, 1016–1023. [Google Scholar] [CrossRef] [PubMed]
- Chretien, J.P.; George, D.; Shaman, J.; Chitale, R.A.; McKenzie, F.E. Influenza forecasting in human populations: A scoping review. PLoS ONE 2014, 9, e94130. [Google Scholar] [CrossRef]
- Hogan, A.B.; Anderssen, R.S.; Davis, S.; Moore, H.C.; Lim, F.J.; Fathima, P.; Glass, K. Time series analysis of RSV and bronchiolitis seasonality in temperate and tropical Western Australia. Epidemics 2016, 16, 49–55. [Google Scholar] [CrossRef]
- González-Parra, G.; Arenas, A.; Diego, F.; Aranda, L.S. Modeling the epidemic waves of AH1N1/09 influenza around the world. Spat. Spatio-Temporal Epidemiol. 2011, 2, 219–226. [Google Scholar] [CrossRef]
- González-Parra, G.; Villanueva, R.J.; Ruiz-Baragaño, J.; Moraño, J.A. Modelling influenza A (H1N1) 2009 epidemics using a random network in a distributed computing environment. Acta Trop. 2015, 143, 29–35. [Google Scholar] [CrossRef]
- Moore, H.C.; Jacoby, P.; Hogan, A.B.; Blyth, C.C.; Mercer, G.N. Modelling the seasonal epidemics of respiratory syncytial virus in young children. PLoS ONE 2014, 9, e100422. [Google Scholar] [CrossRef]
- Osthus, D.; Hickmann, K.S.; Caragea, P.C.; Higdon, D.; Del Valle, S.Y. Forecasting seasonal influenza with a state-space SIR model. Ann. Appl. Stat. 2017, 11, 202. [Google Scholar] [CrossRef] [PubMed]
- Reich, N.G.; Brooks, L.C.; Fox, S.J.; Kandula, S.; McGowan, C.J.; Moore, E.; Osthus, D.; Ray, E.L.; Tushar, A.; Yamana, T.K.; et al. A collaborative multiyear, multimodel assessment of seasonal influenza forecasting in the United States. Proc. Natl. Acad. Sci. USA 2019, 116, 3146–3154. [Google Scholar] [CrossRef] [PubMed]
- Shaman, J.; Karspeck, A. Forecasting seasonal outbreaks of influenza. Proc. Natl. Acad. Sci. USA 2012, 109, 20425–20430. [Google Scholar] [CrossRef] [PubMed]
- Shaman, J.; Karspeck, A.; Yang, W.; Tamerius, J.; Lipsitch, M. Real-time influenza forecasts during the 2012–2013 season. Nat. Commun. 2013, 4, 2837. [Google Scholar] [CrossRef] [PubMed]
- Sloan, C.; Heaton, M.; Kang, S.; Berrett, C.; Wu, P.; Gebretsadik, T.; Sicignano, N.; Evans, A.; Lee, R.; Hartert, T. The impact of temperature and relative humidity on spatiotemporal patterns of infant bronchiolitis epidemics in the contiguous United States. Health Place 2017, 45, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Soliman, M.; Lyubchich, V.; Gel, Y.R. Complementing the power of deep learning with statistical model fusion: Probabilistic forecasting of influenza in Dallas County, Texas, USA. Epidemics 2019, 28, 100345. [Google Scholar] [CrossRef]
- Yang, W.; Cowling, B.J.; Lau, E.H.; Shaman, J. Forecasting influenza epidemics in Hong Kong. PLoS Comput. Biol. 2015, 11, e1004383. [Google Scholar] [CrossRef]
- Walton, N.A.; Poynton, M.R.; Gesteland, P.H.; Maloney, C.; Staes, C.; Facelli, J.C. Predicting the start week of respiratory syncytial virus outbreaks using real time weather variables. BMC Med. Inform. Decis. Mak. 2010, 10, 68. [Google Scholar] [CrossRef]
- Robertson, J.F.; Sewell, H.F.; Stewart, M. Delayed second dose of the BNT162b2 vaccine: Innovation or misguided conjecture? Lancet 2021, 397, 879–880. [Google Scholar] [CrossRef]
- Acedo, L.; Cortés, J.C.; Díez-Domingo, J.; Sánchez-Alonso, V.; Tuells, J.; Villanueva, R.J. Uncertainty and sensitivity of the sexual behavior changes to the current human papillomavirus vaccination campaign in Spain. Math. Methods Appl. Sci. 2021, 44, 7845–7857. [Google Scholar] [CrossRef]
- Acuña-Zegarra, M.A.; Díaz-Infante, S.; Baca-Carrasco, D.; Olmos-Liceaga, D. COVID-19 optimal vaccination policies: A modeling study on efficacy, natural and vaccine-induced immunity responses. Math. Biosci. 2021, 337, 108614. [Google Scholar] [CrossRef] [PubMed]
- Paltiel, A.D.; Schwartz, J.L.; Zheng, A.; Walensky, R.P. Clinical Outcomes Of A COVID-19 Vaccine: Implementation Over Efficacy: Study examines how definitions and thresholds of vaccine efficacy, coupled with different levels of implementation effectiveness and background epidemic severity, translate into outcomes. Health Aff. 2021, 40, 42–52. [Google Scholar]
- Rodrigues, H.S.; Monteiro, M.T.T.; Torres, D.F. Vaccination models and optimal control strategies to dengue. Math. Biosci. 2014, 247, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ferranna, M.; Cadarette, D.; Bloom, D.E. COVID-19 Vaccine Allocation: Modeling Health Outcomes and Equity Implications of Alternative Strategies. Engineering 2021, 7, 924–935. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Parra, G. Analysis of Delayed Vaccination Regimens: A Mathematical Modeling Approach. Epidemiologia 2021, 2, 271–293. [Google Scholar] [CrossRef]
- I Arolas, H.P.; Acosta, E.; Myrskylä, M. Optimal vaccination age varies across countries. Proc. Natl. Acad. Sci. USA 2021, 118, e2105987118. [Google Scholar] [CrossRef]
- Kadire, S.R.; Wachter, R.M.; Lurie, N. Delayed second dose versus standard regimen for COVID-19 vaccination. N. Engl. J. Med. 2021, 384, e28. [Google Scholar] [CrossRef]
- Moghadas, S.M.; Vilches, T.N.; Zhang, K.; Nourbakhsh, S.; Sah, P.; Fitzpatrick, M.C.; Galvani, A.P. Evaluation of COVID-19 vaccination strategies with a delayed second dose. PLoS Biol. 2021, 19, e3001211. [Google Scholar] [CrossRef]
- Alvarez, M.M.; Bravo-González, S.; Trujillo-de Santiago, G. Modeling vaccination strategies in an Excel spreadsheet: Increasing the rate of vaccination is more effective than increasing the vaccination coverage for containing COVID-19. PLoS ONE 2021, 16, e0254430. [Google Scholar] [CrossRef]
- Shim, E. Optimal Allocation of the Limited COVID-19 Vaccine Supply in South Korea. J. Clin. Med. 2021, 10, 591. [Google Scholar] [CrossRef]
- Tuite, A.R.; Zhu, L.; Fisman, D.N.; Salomon, J.A. Alternative dose allocation strategies to increase benefits from constrained COVID-19 vaccine supply. Ann. Intern. Med. 2021, 174, 570–572. [Google Scholar] [CrossRef] [PubMed]
- Romero-Brufau, Santiago, e.a. Public health impact of delaying second dose of BNT162b2 or mRNA-1273 COVID-19 vaccine: Simulation agent based modeling study. BMJ 2021, 373, n1334. [Google Scholar] [CrossRef]
- Wikipedia. 2021. Available online: https://en.wikipedia.org/wiki/COVID-19vaccineclinicalresearch (accessed on 1 July 2021).
- Mohamadi, M.; Lin, Y.; Vulliet, M.V.S.; Flahault, A.; Rozanova, L.; Fabre, G. COVID-19 Vaccination Strategy in China: A Case Study. Epidemiologia 2021, 2, 402–425. [Google Scholar] [CrossRef]
- Afzal, A.; Saleel, C.A.; Bhattacharyya, S.; Satish, N.; Samuel, O.D.; Badruddin, I.A. Merits and Limitations of Mathematical Modeling and Computational Simulations in Mitigation of COVID-19 Pandemic: A Comprehensive Review. Arch. Comput. Methods Eng. 2021, 29, 1–27. [Google Scholar] [CrossRef]
- Din, A.; Khan, A.; Zeb, A.; Sidi Ammi, M.R.; Tilioua, M.; Torres, D.F. Hybrid Method for Simulation of a Fractional COVID-19 Model with Real Case Application. Axioms 2021, 10, 290. [Google Scholar] [CrossRef]
- Padmanabhan, R.; Abed, H.S.; Meskin, N.; Khattab, T.; Shraim, M.; Al-Hitmi, M.A. A review of mathematical model-based scenario analysis and interventions for COVID-19. Comput. Methods Programs Biomed. 2021, 206, 106301. [Google Scholar] [CrossRef]
- Mahrouf, M.; Boukhouima, A.; Zine, H.; Lotfi, E.M.; Torres, D.F.; Yousfi, N. Modeling and forecasting of COVID-19 spreading by delayed stochastic differential equations. Axioms 2021, 10, 18. [Google Scholar] [CrossRef]
- Rowan, N.J.; Moral, R.A. Disposable face masks and reusable face coverings as non-pharmaceutical interventions (NPIs) to prevent transmission of SARS-CoV-2 variants that cause Coronavirus disease (COVID-19): Role of new sustainable NPI design innovations and predictive mathematical modelling. Sci. Total Environ. 2021, 772, 145530. [Google Scholar]
- Wintachai, P.; Prathom, K. Stability analysis of SEIR model related to efficiency of vaccines for COVID-19 situation. Heliyon 2021, 7, e06812. [Google Scholar] [CrossRef]
- Allegretti, S.; Bulai, I.M.; Marino, R.; Menandro, M.A.; Parisi, K. Vaccination effect conjoint to fraction of avoided contacts for a Sars-Cov-2 mathematical model. Math. Model. Numer. Simul. Appl. 2021, 1, 56–66. [Google Scholar] [CrossRef]
- Ikram, R.; Khan, A.; Zahri, M.; Saeed, A.; Yavuz, M.; Kumam, P. Extinction and stationary distribution of a stochastic COVID-19 epidemic model with time-delay. Comput. Biol. Med. 2022, 141, 105115. [Google Scholar] [CrossRef] [PubMed]
- Tchoumi, S.Y.; Rwezaura, H.; Diagne, M.L.; González-Parra, G.; Tchuenche, J. Impact of Infective Immigrants on COVID-19 Dynamics. Math. Comput. Appl. 2022, 27, 11. [Google Scholar] [CrossRef]
- Yavuz, M.; Coşar, F.Ö.; Günay, F.; Özdemir, F.N. A new mathematical modeling of the COVID-19 pandemic including the vaccination campaign. Open J. Model. Simul. 2021, 9, 299–321. [Google Scholar] [CrossRef]
- Albani, V.V.; Loria, J.; Massad, E.; Zubelli, J.P. The impact of COVID-19 vaccination delay: A data-driven modeling analysis for Chicago and New York City. Vaccine 2021, 39, 6088–6094. [Google Scholar] [CrossRef]
- Abila, D.B.; Dei-Tumi, S.D.; Humura, F.; Aja, G.N. We need to start thinking about promoting the demand, uptake, and equitable distribution of COVID-19 vaccines NOW! Public Health Pract. 2020, 1, 100063. [Google Scholar] [CrossRef] [PubMed]
- Dermody, T.S.; DiMaio, D.; Enquist, L.W. Vaccine Safety, Efficacy, and Trust Take Time. Annu. Rev. Virol. 2020, 8, iii–iv. [Google Scholar] [CrossRef]
- Buonomo, B.; Della Marca, R.; d’Onofrio, A.; Groppi, M. A behavioural modelling approach to assess the impact of COVID-19 vaccine hesitancy. J. Theor. Biol. 2022, 534, 110973. [Google Scholar] [CrossRef]
- Bentout, S.; Tridane, A.; Djilali, S.; Touaoula, T.M. Age-structured modeling of COVID-19 epidemic in the USA, UAE and Algeria. Alex. Eng. J. 2021, 60, 401–411. [Google Scholar] [CrossRef]
- Simoy, M.; Aparicio, J. Socially structured model for COVID-19 pandemic: Design and evaluation of control measures. Comput. Appl. Math. 2021, 41. [Google Scholar] [CrossRef]
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.Y.; Chen, L.; Wang, M. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020, 323, 1406–1407. [Google Scholar] [CrossRef]
- Buitrago-Garcia, D.; Egli-Gany, D.; Counotte, M.J.; Hossmann, S.; Imeri, H.; Ipekci, A.M.; Salanti, G.; Low, N. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Med. 2020, 17, e1003346. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Zhang, X.; Zhang, X.; Wei, Z.; Zhang, L.; Xu, J.; Liang, P.; Xu, Y.; Zhang, C.; Xu, A. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16–23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J. Infect. 2020, 80, e1–e13. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, K.; Kagaya, K.; Zarebski, A.; Chowell, G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance 2020, 25, 2000180. [Google Scholar] [CrossRef] [PubMed]
- Park, S.W.; Cornforth, D.M.; Dushoff, J.; Weitz, J.S. The time scale of asymptomatic transmission affects estimates of epidemic potential in the COVID-19 outbreak. Epidemics 2020, 31, 100392. [Google Scholar] [CrossRef]
- Shao, S.; Zhou, D.; He, R.; Li, J.; Zou, S.; Mallery, K.; Kumar, S.; Yang, S.; Hong, J. Risk assessment of airborne transmission of COVID-19 by asymptomatic individuals under different practical settings. J. Aerosol Sci. 2020, 151, 105661. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, M.; Yokoe, D.S.; Havlir, D.V. Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control COVID-19. N. Engl. J. Med. 2020, 382, 2158–2160. [Google Scholar] [CrossRef]
- Kinoshita, R.; Anzai, A.; Jung, S.m.; Linton, N.M.; Miyama, T.; Kobayashi, T.; Hayashi, K.; Suzuki, A.; Yang, Y.; Akhmetzhanov, A.R.; et al. Containment, Contact Tracing and Asymptomatic Transmission of Novel Coronavirus Disease (COVID-19): A Modelling Study. J. Clin. Med. 2020, 9, 3125. [Google Scholar] [CrossRef]
- Han, D.; Li, R.; Han, Y.; Zhang, R.; Li, J. COVID-19: Insight into the asymptomatic SARS-CoV-2 infection and transmission. Int. J. Biol. Sci. 2020, 16, 2803. [Google Scholar] [CrossRef]
- Teixeira, S.C. Mild and asymptomatic cases of COVID-19 are potential threat for faecal–oral transmission. Braz. J. Infect. Dis. 2020, 24, 368. [Google Scholar] [CrossRef]
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; Hernán, M.A.; Pérez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; de Larrea, N.F.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): A nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Nikolai, L.A.; Meyer, C.G.; Kremsner, P.G.; Velavan, T.P. Asymptomatic SARS Coronavirus 2 infection: Invisible yet invincible. Int. J. Infect. Dis. 2020, 100, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Kronbichler, A.; Kresse, D.; Yoon, S.; Lee, K.H.; Effenberger, M.; Shin, J.I. Asymptomatic patients as a source of COVID-19 infections: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 98, 180–186. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Guo, Y.; Mao, R.; Zhang, J. Proportion of asymptomatic coronavirus disease 2019: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 820–830. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.A.; Quandelacy, T.M.; Kada, S.; Prasad, P.V.; Steele, M.; Brooks, J.T.; Slayton, R.B.; Biggerstaff, M.; Butler, J.C. SARS-CoV-2 Transmission From People Without COVID-19 Symptoms. JAMA Netw. Open 2021, 4, e2035057. [Google Scholar] [CrossRef]
- İşlier, Z.G.; Güllü, R.; Hörmann, W. An exact and implementable computation of the final outbreak size distribution under Erlang distributed infectious period. Math. Biosci. 2020, 325, 108363. [Google Scholar] [CrossRef] [PubMed]
- González-Parra, G.; Acedo, L.; Villanueva-Micó, R.J.; Arenas, A.J. Modeling the social obesity epidemic with stochastic networks. Phys. A Stat. Mech. Its Appl. 2010, 389, 3692–3701. [Google Scholar] [CrossRef]
- Roberts, M.; Andreasen, V.; Lloyd, A.; Pellis, L. Nine challenges for deterministic epidemic models. Epidemics 2015, 10, 49–53. [Google Scholar] [CrossRef] [PubMed]
- González-Parra, G.; Dobrovolny, H.M. Assessing uncertainty in A2 respiratory syncytial virus viral dynamics. Comput. Math. Methods Med. 2015, 2015, 567589. [Google Scholar] [CrossRef][Green Version]
- Wearing, H.J.; Rohani, P.; Keeling, M.J. Appropriate models for the management of infectious diseases. PLoS Med 2005, 2, e174. [Google Scholar] [CrossRef]
- Faes, C.; Abrams, S.; Van Beckhoven, D.; Meyfroidt, G.; Vlieghe, E.; Hens, N.; Belgian Collaborative Group on COVID-19 Hospital Surveillance. Time between symptom onset, hospitalisation and recovery or death: Statistical analysis of belgian COVID-19 patients. Int. J. Environ. Res. Public Health 2020, 17, 7560. [Google Scholar] [CrossRef]
- Faust, J.S.; del Rio, C. Assessment of Deaths From COVID-19 and From Seasonal Influenza. JAMA Intern. Med. 2020, 180, 1045–1046. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Matrajt, L.; Eaton, J.; Leung, T.; Brown, E.R. Vaccine optimization for COVID-19, who to vaccinate first? Science Advances 2021, 7, eabf1374. [Google Scholar] [CrossRef]
- Walsh, F. Loss and resilience in the time of COVID-19: Meaning making, hope, and transcendence. Fam. Process 2020, 59, 898–911. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, B.B.; Wiegand, S.d.C.B. Losses in times of a pandemic: Bioethical perceptions about mourning caused by COVID-19 in Brazil. Voices Bioeth. 2020, 6. [Google Scholar] [CrossRef]
- Zhai, Y.; Du, X. Loss and grief amidst COVID-19: A path to adaptation and resilience. Brain, Behav. Immun. 2020, 87, 80–81. [Google Scholar] [CrossRef]
- Knoll, M.D.; Wonodi, C. Oxford–AstraZeneca COVID-19 vaccine efficacy. Lancet 2020, 397, 72–74. [Google Scholar] [CrossRef]
- Krause, P.; Fleming, T.R.; Longini, I.; Henao-Restrepo, A.M.; Peto, R.; Dean, N.; Halloran, M.; Huang, Y.; Fleming, T.; Gilbert, P.; et al. COVID-19 vaccine trials should seek worthwhile efficacy. Lancet 2020, 396, 741–743. [Google Scholar] [CrossRef]
- Hodgson, S.H.; Mansatta, K.; Mallett, G.; Harris, V.; Emary, K.R.; Pollard, A.J. What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical efficacy of vaccines against SARS-CoV-2. Lancet Infect. Dis. 2020, 21, e26–e35. [Google Scholar] [CrossRef]
- Lipsitch, M.; Dean, N.E. Understanding COVID-19 vaccine efficacy. Science 2020, 370, 763–765. [Google Scholar] [CrossRef]
- Bartsch, S.M.; O’Shea, K.J.; Ferguson, M.C.; Bottazzi, M.E.; Wedlock, P.T.; Strych, U.; McKinnell, J.A.; Siegmund, S.S.; Cox, S.N.; Hotez, P.J.; et al. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am. J. Prev. Med. 2020, 59, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; MacDonald, N.E. How can a global pandemic affect vaccine hesitancy? Expert Rev. Vaccines 2020, 19, 899–901. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wang, A.; Yi, B.; Ding, K.; Wang, H.; Wang, J.; Xu, G. The epidemiological characteristics of infection in close contacts of COVID-19 in Ningbo city. Chin. J. Epidemiol. 2020, 41, 668–672. [Google Scholar]
- Mc Evoy, D.; McAloon, C.G.; Collins, A.B.; Hunt, K.; Butler, F.; Byrne, A.W.; Casey, M.; Barber, A.; Griffin, J.M.; Lane, E.A.; et al. Relative infectiousness of asymptomatic SARS-CoV-2 infected persons compared with symptomatic individuals: A rapid scoping review. BMJ Open 2021, 11, e042354. [Google Scholar] [CrossRef]
- Santarpia, J.L.; Rivera, D.N.; Herrera, V.; Morwitzer, M.J.; Creager, H.; Santarpia, G.W.; Crown, K.K.; Brett-Major, D.; Schnaubelt, E.; Broadhurst, M.J.; et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci. Rep. 2020, 110, 12732. [Google Scholar] [CrossRef]
- Zhao, H.j.; Lu, X.x.; Deng, Y.b.; Tang, Y.j.; Lu, J.c. COVID-19: Asymptomatic carrier transmission is an underestimated problem. Epidemiol. Infect. 2020, 148, 1–7. [Google Scholar] [CrossRef]
- Driver, R.D. Ordinary and Delay Differential Equations, 1st ed.; Applied Mathematical Sciences 20; Springer: New York, NY, USA, 1977. [Google Scholar]
- Luis Barreira, C.V. Ordinary Differential Equations: Qualitative Theory, 1st ed.; Graduate Studies in Mathematics, American Mathematical Society: Providence, RI, USA, 2012. [Google Scholar]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.; Lau, E.H.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus—Infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Statista. 2021. Available online: https://www.statista.com/statistics/1105431/covidcasefatalityratesUSbyagegroup/ (accessed on 1 August 2021).
- Oran, D.P.; Topol, E.J. Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review. Ann. Intern. Med. 2020, 173, 362–367. [Google Scholar] [CrossRef]
- Ahn, D.G.; Shin, H.J.; Kim, M.H.; Lee, S.; Kim, H.S.; Myoung, J.; Kim, B.T.; Kim, S.J. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19). J. Microbiol. Biotechnol. 2020, 30, 313–324. [Google Scholar] [CrossRef]
- Burki, T.K. The Russian vaccine for COVID-19. Lancet Respir. Med. 2020, 8, e85–e86. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Tregoning, J.S.; Brown, E.S.; Cheeseman, H.M.; Flight, K.E.; Higham, S.L.; Lemm, N.M.; Pierce, B.F.; Stirling, D.C.; Wang, Z.; Pollock, K.M. Vaccines for COVID-19. Clin. Exp. Immunol. 2020, 202, 162–192. [Google Scholar] [CrossRef] [PubMed]
- Dinleyici, E.C.; Borrow, R.; Safadi, M.A.P.; van Damme, P.; Munoz, F.M. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum. Vaccines Immunother. 2020, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Yamey, G.; Schaferhoff, M.; Hatchett, R.; Pate, M.; Zhao, F.; McDade, K.K. Ensuring global access to COVID-19 vaccines. Lancet 2020, 395, 1405–1406. [Google Scholar] [CrossRef]
- Goldstein, J.R.; Cassidy, T.; Wachter, K.W. Vaccinating the oldest against COVID-19 saves both the most lives and most years of life. Proc. Natl. Acad. Sci. USA 2021, 118, e2026322118. [Google Scholar] [CrossRef]
- Sperrin, M.; Grant, S.W.; Peek, N. Prediction models for diagnosis and prognosis in COVID-19. BMJ 2020, 369, m1464. [Google Scholar] [CrossRef]
- Stutt, R.O.; Retkute, R.; Bradley, M.; Gilligan, C.A.; Colvin, J. A modelling framework to assess the likely effectiveness of facemasks in combination with lock-down in managing the COVID-19 pandemic. Proc. R. Soc. A 2020, 476, 20200376. [Google Scholar] [CrossRef]
- Haque, A.; Pant, A.B. Efforts at COVID-19 Vaccine Development: Challenges and Successes. Vaccines 2020, 8, 739. [Google Scholar] [CrossRef]
- Verger, P.; Dubé, E. Restoring confidence in vaccines in the COVID-19 era. Expert Rev. Vaccines 2020, 19, 991–993. [Google Scholar] [CrossRef]
- Ayoub, H.H.; Chemaitelly, H.; Abu-Raddad, L.J. Epidemiological Impact of Novel Preventive and Therapeutic HSV-2 Vaccination in the United States: Mathematical Modeling Analyses. Vaccines 2020, 8, 366. [Google Scholar] [CrossRef]
- Benest, J.; Rhodes, S.; Quaife, M.; Evans, T.G.; White, R.G. Optimising Vaccine Dose in Inoculation against SARS-CoV-2, a Multi-Factor Optimisation Modelling Study to Maximise Vaccine Safety and Efficacy. Vaccines 2021, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Chaves, L.F.; Hurtado, L.A.; Rojas, M.R.; Friberg, M.D.; Rodríguez, R.M.; Avila-Aguero, M.L. COVID-19 basic reproduction number and assessment of initial suppression policies in Costa Rica. Math. Model. Nat. Phenom. 2020, 15, 32. [Google Scholar] [CrossRef]
- Contreras, S.; Villavicencio, H.A.; Medina-Ortiz, D.; Saavedra, C.P.; Olivera-Nappa, Á. Real-time estimation of Rt for supporting public-health policies against COVID-19. Front. Public Health 2020, 8, 556689. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Parra, G.; Díaz-Rodríguez, M.; Arenas, A.J. Mathematical modeling to design public health policies for Chikungunya epidemic using optimal control. Optim. Control Appl. Methods 2020, 41, 1584–1603. [Google Scholar] [CrossRef]
- Nistal, R.; de la Sen, M.; Gabirondo, J.; Alonso-Quesada, S.; Garrido, A.J.; Garrido, I. A Modelization of the Propagation of COVID-19 in Regions of Spain and Italy with Evaluation of the Transmission Rates Related to the Intervention Measures. Biology 2021, 10, 121. [Google Scholar] [CrossRef]
- van Oosterhout, C.; Hall, N.; Ly, H.; Tyler, K.M. COVID-19 evolution during the pandemic–Implications of new SARS-CoV-2 variants on disease control and public health policies. Virulence 2021, 12, 507. [Google Scholar] [CrossRef]
- Zenk, L.; Steiner, G.; Pina e Cunha, M.; Laubichler, M.D.; Bertau, M.; Kainz, M.J.; Jäger, C.; Schernhammer, E.S. Fast Response to Superspreading: Uncertainty and Complexity in the Context of COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 7884. [Google Scholar] [CrossRef]
- Hethcote, H.W. Mathematics of infectious diseases. SIAM Rev. 2005, 42, 599–653. [Google Scholar] [CrossRef]
- Gumel, A.B.; Iboi, E.A.; Ngonghala, C.N.; Elbasha, E.H. A primer on using mathematics to understand COVID-19 dynamics: Modeling, analysis and simulations. Infect. Dis. Model. 2021, 6, 148–168. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).