Impact of Climate Change on Waterborne Diseases: Directions towards Sustainability
Abstract
1. Introduction
2. Materials and Methods
3. Results and Discussion
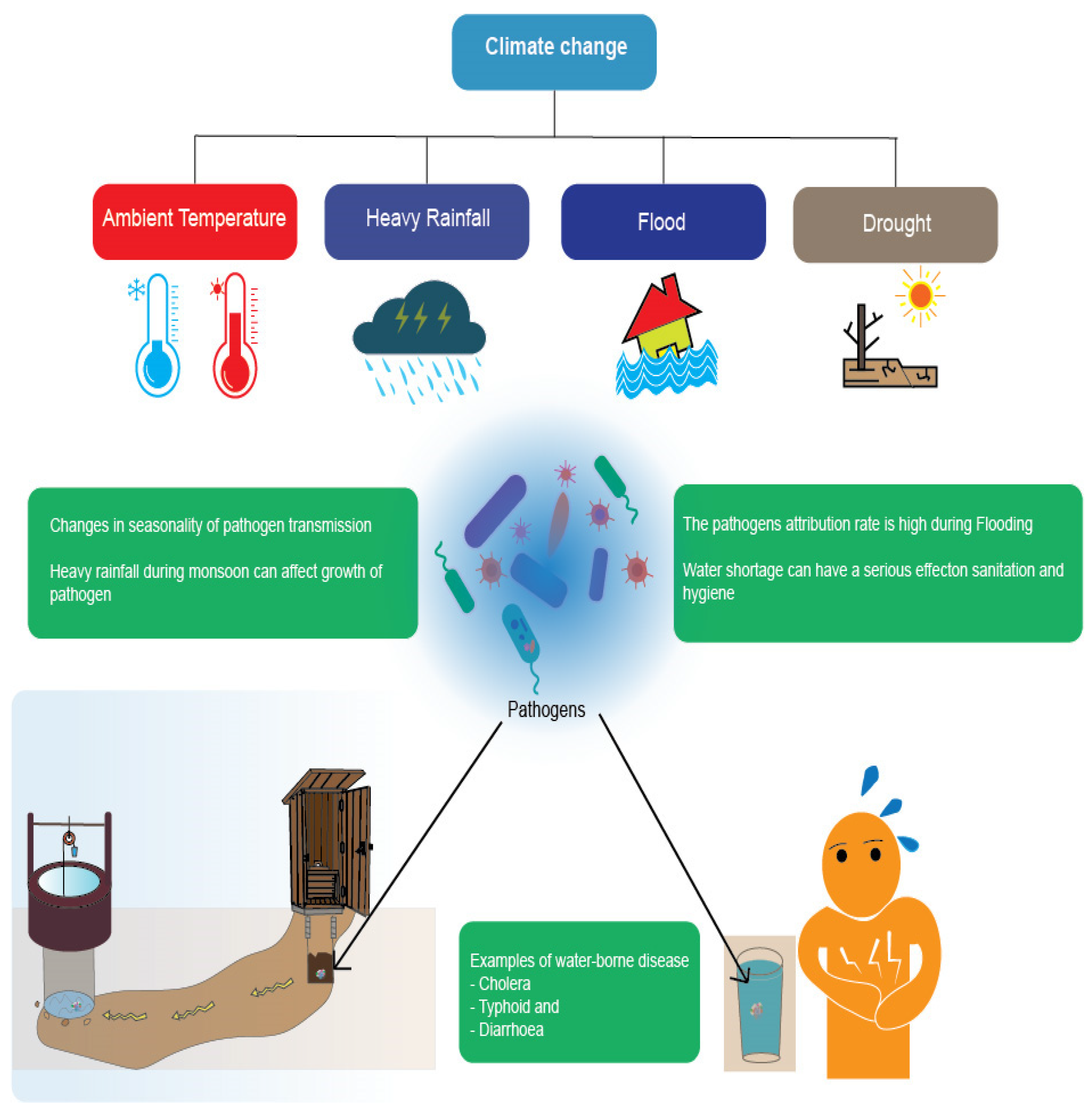
3.1. Perspectives on the Impact of Climate Change on WBDs
3.2. Directions towards Sustainability: SDGs and Climate Change-Related WBDs
3.3. Challenges and Blueprint
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Goggins, W.B.; Chan, E.Y.; Yang, C.; Chong, M. Associations between mortality and meteorological and pollutant variables during the cool season in two Asian cities with sub-tropical climates: Hong Kong and Taipei. Environ. Health 2013, 12, 59. [Google Scholar] [CrossRef] [PubMed]
- Mishra, V.; Ganguly, A.R.; Nijssen, B.; Lettenmaier, D.P. Changes in observed climate extremes in global urban areas. Environ. Res. Lett. 2015, 10, 024005. [Google Scholar] [CrossRef]
- Parliari, D.; Giannaros, C.; Keppas, S. Assessment of heat and cold waves phenomena and impacts on environment. In Extremes in Atmospheric Processes and Phenomenon: Assessment, Impacts and Mitigation; Springer Nature: Singapore, 2022; pp. 141–167. [Google Scholar]
- Revich, B.; Shaposhnikov, D. The influence of heat and cold waves on mortality in Russian subarctic cities with varying climates. Int. J. Biometeorol. 2022, 66, 2501–2515. [Google Scholar] [CrossRef]
- International Strategy for Disaster Reduction (ISDR). Economic Losses, Poverty, and Disasters 1998–2017; ISDR: Geneva, Switzerland, 2018; pp. 1–33. [Google Scholar]
- Braks, M.; Giglio, G.; Tomassone, L.; Sprong, H.; Leslie, T. Making vector-borne disease surveillance work: New opportunities from the SDG perspectives. Front. Vet. Sci. 2019, 6, 232. [Google Scholar] [CrossRef]
- Lee, J.; Perera, D.; Glickman, T.; Taing, L. Water-related disasters and their health impacts: A global review. Prog. Disaster Sci. 2020, 8, 100–123. [Google Scholar] [CrossRef]
- Berry, H.L.; Waite, T.D.; Dear, K.B.G.; Capon, A.G.; Murray, V. The case for systems thinking about climate change and mental health. Nat. Clim. Change 2018, 8, 282–290. [Google Scholar] [CrossRef]
- Kendrovski, V.; Gjorgjev, D. Climate change: Implication for foodborne diseases (Salmonella and food poisoning among humans in R. Macedonia). In Structure and Function of Food Engineering; IntechOpen: Rijeka, Croatia, 2012; pp. 151–170. [Google Scholar]
- Guzman Herrador, B.R.G.; de Blasio, B.F.; MacDonald, E.; Nichols, G.; Sudre, B.; Vold, L.; Semenza, J.C.; Nygård, K. Analytical studies assessing the association between extreme precipitation or temperature and drinking water-related waterborne infections: A review. Environ. Health 2015, 14, 29. [Google Scholar] [CrossRef]
- Levy, K.; Woster, A.P.; Goldstein, R.S.; Carlton, E.J. Untangling the impacts of climate change on waterborne diseases: A systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ. Sci. Technol. 2016, 50, 4905–4922. [Google Scholar] [CrossRef]
- Lo Iacono, G.; Armstrong, B.; Fleming, L.E.; Elson, R.; Kovats, S.; Vardoulakis, S.; Nichols, G.L. Challenges in developing methods for quantifying the effects of weather and climate on water-associated diseases: A systematic review. PLoS Negl. Trop. Dis. 2017, 11, e0005659. [Google Scholar] [CrossRef] [PubMed]
- Semenza, J.C.; Herbst, S.; Rechenburg, A.; Suk, J.E.; Höser, C.; Schreiber, C.; Kistemann, T. Climate change impact assessment of food- and waterborne diseases. Crit. Rev. Environ. Sci. Technol. 2012, 42, 857–890. [Google Scholar] [CrossRef]
- Funari, E.; Manganelli, M.; Sinisi, L. Impact of climate change on waterborne diseases. Ann. Ist. Super. Sanità 2012, 48, 473–487. [Google Scholar] [CrossRef] [PubMed]
- Cissé, G.; Menezes, J.A.; Confalonieri, U. Climate-sensitive infectious diseases. In The Adaptation Gap Report; United Nations Environment Programme (UN Environmental Program): Nairobi, Kenya, 2018; pp. 49–59. [Google Scholar]
- Khan, M.D.; Thi Vu, H.H.; Lai, Q.T.; Ahn, J.W. Aggravation of human diseases and climate change nexus. Int. J. Environ. Res. Public Health. 2019, 16, 2799. [Google Scholar] [CrossRef]
- Wu, X.; Lu, Y.; Zhou, S.; Chen, L.; Xu, B. Impact of climate change on human infectious diseases: Empirical evidence and human adaptation. Environ. Int. 2016, 86, 14–23. [Google Scholar] [CrossRef]
- Murphy, H.M.; Pintar, K.D.M.; McBean, E.A.; Thomas, M.K. A systematic review of waterborne disease burden methodologies from developed countries. J. Water Health 2014, 12, 634–655. [Google Scholar] [CrossRef]
- UNFCC. Climate Change: Impacts, Vulnerabilities and Adaptation in Developing Countries Framework for Climate Convention; United Nations: Bonn, Germany, 2007; Volume 1, Available online: https://unfccc.int/resource/docs/publications/impacts.pdf (accessed on 1 February 2023).
- Cheesbrough, M. District Laboratory Practice in Tropical Countries, Part 2; Cambridge University Press: Cambridge, UK, 2005. [Google Scholar]
- Bidhuri, S.; Taqi, M.; Khan, M.M.A. Water-borne disease: Link between human health and water use in the Mithepur and Jaitpur area of the NCT of Delhi. J. Public Health 2018, 26, 119–126. [Google Scholar] [CrossRef]
- Sinclair, R.G.; Jones, E.L.; Gerba, C.P. Viruses in recreational water-borne disease outbreaks: A review. J. Appl. Microbiol. 2009, 107, 1769–1780. [Google Scholar] [CrossRef]
- Bekturganov, Z.; Tussupova, K.; Berndtsson, R.; Sharapatova, N.; Aryngazin, K.; Zhanasova, M. Water related health problems in Central Asia—A review. Water 2016, 8, 219. [Google Scholar] [CrossRef]
- DeJarnett, N.; Robb, K.; Castellanos, I.; Dettman, L.; Patel, S.S. The American Public Health Association’s 2017 year of climate change and health: Time for action. Am. J. Public Health 2018, 108 (Suppl. 2), S76–S77. [Google Scholar] [CrossRef] [PubMed]
- Lake, I.R.; Barker, G.C. Climate change, foodborne pathogens, and illness in higher-income countries. Curr. Environ. Health Rep. 2018, 5, 187–196. [Google Scholar] [CrossRef]
- Levy, K.; Smith, S.M.; Carlton, E.J. Climate change impacts on waterborne diseases: Moving toward designing interventions. Curr. Environ. Health Rep. 2018, 5, 272–282. [Google Scholar] [CrossRef]
- Schijven, J.; Bouwknegt, M.; de Roda Husman, A.M.; Rutjes, S.; Sudre, B.; Suk, J.E.; Semenza, J.C. A decision support tool to compare waterborne and foodborne infection and/or illness risks associated with climate change. Risk Anal. 2013, 33, 2154–2167. [Google Scholar] [CrossRef] [PubMed]
- Cann, K.F.; Thomas, D.R.; Salmon, R.L.; Wyn-Jones, A.P.; Kay, D. Extreme water-related weather events and waterborne disease. Epidemiol. Infect. 2013, 141, 671–686. [Google Scholar] [CrossRef]
- Bain, R.; Cronk, R.; Hossain, R.; Bonjour, S.; Onda, K.; Wright, J.; Yang, H.; Slaymaker, T.; Hunter, P.; Prüss-Ustün, A.; et al. Global assessment of exposure to faecal contamination through drinking water based on a systematic review. Trop. Med. Int. Health 2014, 19, 917–927. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for Laboratory and Field Testing of Mosquito Larvicides; (No. WHO/CDS/WHOPES/GCDPP/2005.13); World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- McMichael, A.J.; Campbell-Lendrum, D.H.; Corvalán, C.F.; Ebi, K.L.; Githeko, A.; Scheraga, J.D.; Woodward, A. Climate Change and Human Health: Risks and Responses; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Parker, D.J. Floods in cities: Increasing exposure and rising impact potential. Built Environ. 1995, 21, 114–125. [Google Scholar]
- Rashid, S.F. The urban poor in Dhaka City: Their struggles and coping strategies during the floods of 1998. Disasters 2000, 24, 240–253. [Google Scholar] [CrossRef]
- Hernández-Delgado, E.A. The emerging threats of climate change on tropical coastal ecosystem services, public health, local economies and livelihood sustainability of small islands: Cumulative impacts and synergies. Mar. Pollut. Bull. 2015, 101, 5–28. [Google Scholar] [CrossRef] [PubMed]
- Keim, M.E. Building human resilience: The role of public health preparedness and response as an adaptation to climate change. Am. J. Prev. Med. 2008, 35, 508–516. [Google Scholar] [CrossRef]
- Harris, A.M.; Chowdhury, F.; Begum, Y.A.; Khan, A.I.; Faruque, A.S.; Svennerholm, A.M.; Harris, J.B.; Ryan, E.T.; Cravioto, A.; Calderwood, S.B.; et al. Shifting prevalence of major diarrheal pathogens in patients seeking hospital care during floods in 1998, 2004, and 2007 in Dhaka, Bangladesh. Am. J. Trop. Med. Hyg. 2008, 79, 708–714. [Google Scholar] [CrossRef]
- Schwartz, B.S.; Harris, J.B.; Khan, A.I.; Larocque, R.C.; Sack, D.A.; Malek, M.A.; Faruque, A.S.; Qadri, F.; Calderwood, S.B.; Luby, S.P.; et al. Diarrheal epidemics in Dhaka, Bangladesh, during three consecutive floods: 1988, 1998, and 2004. Am. J. Trop. Med. Hyg. 2006, 74, 1067–1073. [Google Scholar] [CrossRef]
- World Health Organization. Drinking Water Quality in the South-East Asia Region (No. SEA-EH-567); WHO Regional Office for South-East Asia: New Delhi, India, 2010; Available online: https://apps.who.int/iris/rest/bitstreams/910446/retrieve (accessed on 2 February 2023).
- Halvorson, S.J.; Williams, A.L.; Ba, S.; Dunkel, F.V. Water quality and waterborne disease in the Niger River Inland Delta, Mali: A study of local knowledge and response. Health Place 2011, 17, 449–457. [Google Scholar] [CrossRef]
- Beirne, J.; Renzhi, N.; Volz, U. Bracing for the typhoon: Climate change and sovereign risk in Southeast Asia. Sustain. Dev. 2021, 29, 537–551. [Google Scholar] [CrossRef]
- Gödeke, S.H.; Malik, O.A.; Lai, D.T.C.; Bretzler, A.; Schirmer, M.; Mansor, N.H. Water quality investigation in Brunei Darussalam: Investigation of the influence of climate change. Environ. Earth Sci. 2020, 79, 419. [Google Scholar] [CrossRef]
- Seah, S.; Martinus, M.; Jiahui, Q. The Southeast Asia Climate Outlook: 2021 Survey Report. Available online: https://www.think-asia.org/handle/11540/14136 (accessed on 5 February 2023).
- World Health Organization. Joint External Evaluation of IHR Core Capacities of Brunei Darussalam: Mission Report, 28 October–1 November 2019. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/332937/9789240006973-eng.pdf (accessed on 5 February 2023).
- Eckstein, D.; Künzel, V.; Schäfer, L.; Winges, M. Global Climate Risk Index 2020; Germanwatch: Bonn, Germany, 2019; Available online: https://germanwatch.org/sites/default/files/20-2-01e%20Global%20Climate%20Risk%20Index%202020_15.pdf (accessed on 5 February 2023).
- Tofiloski, S. Geospatial Analysis of Water-Associated Infectious Diseases: Case of Myanmar. 2018. Available online: https://www.etd.ceu.edu/2018/tofiloski_slobodan.pdf (accessed on 5 February 2023).
- Davies, G.I.; McIver, L.; Kim, Y.; Hashizume, M.; Iddings, S.; Chan, V. Water-borne diseases and extreme weather events in Cambodia: Review of impacts and implications of climate change. Int. J. Environ. Res. Public Health 2014, 12, 191–213. [Google Scholar] [CrossRef] [PubMed]
- Irvine, K.; Murphy, T.P.; Sampson, M.; Dany, V.; Vermette, S.; Tang, T. An overview of water quality issues in Cambodia. J. Water Manag. Model 2020, 6, 14, 17–52. [Google Scholar] [CrossRef]
- Molyneux, N.; Da Cruz, G.R.; Williams, R.L.; Andersen, R.; Turner, N.C. Climate change and population growth in Timor Leste: Implications for food security. Ambio 2012, 41, 823–840. [Google Scholar] [CrossRef]
- Pinto, A.M. Traditional Knowledge and Water Quality in Timor-Leste: Climate Change Adaptation Strategies Used by Local Communities in Laco-Mesac and Ulmera Villages. Doctoral Dissertation, Ohio University, Ironton, OH, USA, 2014. [Google Scholar]
- Wirawan, I.M. Public health responses to climate change health impacts in Indonesia. Asia Pac. J. Public Health 2010, 22, 25–31. [Google Scholar] [CrossRef]
- Willetts, J.; Priadi, C.; Ombasta, O.; Wulandari, D.; Imtiyaz, I.; Sudhiastiningsih, N.N.S.N.; Kohlitz, J.; Mills, F.; Listyasari, M. Co-developing evidence-informed adaptation actions for resilient citywide sanitation: Local government response to climate change in Indonesia. Environ. Plan. B Urban Anal. City Sci. 2022, 49, 2129–2150. [Google Scholar] [CrossRef]
- Pink, R.M. Laos: The poorest country in Asia. In Water Rights in Southeast Asia and India; Palgrave MacMillan: New York, NY, USA, 2016; pp. 119–138. [Google Scholar]
- Alhoot, M.A.; Tong, W.T.; Low, W.Y.; Sekaran, S.D. Climate change and health: The Malaysia scenario. In Climate Change and Human Health Scenario in South and Southeast Asia; Akhtar, R., Ed.; Springer: Cham, Switzerland, 2016; pp. 243–268. [Google Scholar]
- Annua, Z.F.; Azmi, W.N.F.W.; Ahmad, N.I.; Sham, N.M.; Mahiyuddin, W.R.W.; Veloo, Y.; Abdullah, N.A. Drinking water quality in Malaysia: A review on its current status. Int. J. Environ. Nat. Res. 2020, 24, 556132. [Google Scholar] [CrossRef]
- Asia, G.S. The state of water resources in the Philippines. Clean Water Proj. East Kamias. 2007, pp. 82–91. Available online: https://koreascience.kr/article/CFKO200810335355190.pdf (accessed on 10 March 2023).
- Chua, P.L.; Dorotan, M.M.; Sigua, J.A.; Estanislao, R.D.; Hashizume, M.; Salazar, M.A. Scoping review of climate change and health research in the Philippines: A complementary tool in research Agenda-Setting. Int. J. Environ. Res. Public Health 2019, 16, 2624. [Google Scholar] [CrossRef]
- Dennis, S.; Fisher, D. Climate change and infectious diseases: The next 50 years. Ann. Acad. Med. Singap. 2018, 47, 401–404. [Google Scholar] [CrossRef]
- Ivanov, V. Bacteriological monitoring of ships ballast water in Singapore and its potential importance for the management of coastal ecosystems. Environ. Toxicol. 2006, 1, 59–63. [Google Scholar] [CrossRef]
- Kruawal, K.; Sacher, F.; Werner, A.; Müller, J.; Knepper, T.P. Chemical water quality in Thailand and its impacts on the drinking water production in Thailand. Sci. Total Environ. 2005, 340, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Marks, D. Climate change and Thailand: Impact and response. Contemp. Southeast Asia 2011, 33, 229–258. [Google Scholar] [CrossRef]
- Mai Kien, T.; Thi Tuyet Hanh, T.; Duc Cuong, H.; Shaw, R. Identifying linkages between rates and distributions of malaria, water-borne diseases and influenza with climate variability and climate change in Vietnam. In Climate Change Adaptation and Disaster Risk Reduction: An Asian Perspective; Shaw, R., Pulhin, J.M., Pereira, J.J., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2010; Volume 5. [Google Scholar]
- Phung, D.; Huang, C.; Rutherford, S.; Chu, C.; Wang, X.; Nguyen, M. Climate change, water quality, and water-related diseases in the Mekong Delta Basin: A systematic review. Asia Pac. J. Public Health 2015, 27, 265–276. [Google Scholar] [CrossRef]
- Nichols, G.; Lake, I.; Heaviside, C. Climate change and water-related infectious diseases. Atmosphere 2018, 9, 385. [Google Scholar] [CrossRef]
- Simane, B.; Beyene, H.; Deressa, W.; Kumie, A.; Berhane, K.; Samet, J. Review of climate change and health in Ethiopia: Status and gap analysis. Ethiop. J. Health Dev. 2016, 30, 28–41. [Google Scholar] [PubMed]
- Griggs, D.J.; Nilsson, M.; Stevance, A.; McCollum, D. A Guide to SDG Interactions: From Science to Implementation; International Council for Science: Paris, France, 2017; Available online: http://pure.iiasa.ac.at/id/eprint/14591/ (accessed on 7 February 2023).
| Country | Extreme Climate Events | Common WBDs | GCRI | Source of Drinking Water | References |
|---|---|---|---|---|---|
| Brunei Darussalam | Floods, sea-level rise, and heat waves | Diarrhea | 175 | Surface water (rivers) and tap water | [40,41,42,43] |
| Burma (Myanmar) | Floods, cyclones, and droughts | Acute diarrhea, cholera, dysentery, and typhoid | 2 | Surface water (rivers and lakes), and groundwater (tube and dug wells) | [40,44,45] |
| Cambodia | Floods, droughts, and typhoons | Diarrhea and typhoid | 12 | Surface water (rivers), and groundwater (hand-dug wells) | [40,46,47] |
| Timor-Leste | Floods and droughts | Diarrhea, cholera, and typhoid | nd | Surface water, spring water, and groundwater | [48,49] |
| Indonesia | Tropical cyclones, floods, droughts, and tsunamis | Diarrhea, cholera, typhoid, and leptospirosis | 77 | Surface water (rivers) and groundwater | [40,50,51] |
| Laos | Floods and droughts | Diarrhea and cholera | 76 | Surface water (rivers; the Mekong) and groundwater | [40,52] |
| Malaysia | Floods, rainfall-induced landslides, and droughts | Cholera and typhoid | 114 | Surface water (rivers), tap water, spring water, and groundwater | [40,53,54] |
| The Philippines | Typhoons, ambient temperatures, heat waves, and floods | Cholera, acute bloody diarrhea, and typhoid | 4 | Surface water (rivers, lakes, and river basins) and groundwater reservoir | [40,44,55,56] |
| Singapore | Sea-level rise, heat waves, and floods | Cholera and typhoid (only in rare cases) | 180 | Imported water, local catchment area, reclaimed water, and desalinated (purified) water | [40,57,58] |
| Thailand | Sea-level rise, floods, and droughts | Cholera, typhoid, and paratyphoid | 8 | Groundwater and surface water (river basins) | [40,44,59,60] |
| Vietnam | Sea-level rise, floods, and droughts | Cholera, dysentery, typhoid, and diarrhea | 6 | Surface water (rivers; the Red and Mekong rivers) and groundwater | [40,44,61,62] |
| SDGs | The Interrelationship between the Impacts of Climate Change on WBDs and SDGs | Specific Targets of the SDGs |
|---|---|---|
 | Attempt to eradicate WBDs by the end of 2030 and enhance global cooperation to recognize, control, and mitigate local and foreign health risks | 3.3 and 3.d |
 | Aim to ensure widespread access to affordable and sanitary drinking water, increase funding for water- and sanitation-related initiatives, such as desalination technology and wastewater treatment methods, and boost engagement of local people by the end of 2030 | 6.1, 6.a, and 6.b |
 | Try to reduce the proportion of fatalities and financial losses caused by water-related diseases, with an emphasis on developing countries, and promote financial and technical help to construct sustainable and sound structures using local materials by the end of 2030 | 11.5 and 11.c |
 | Aim to increase global preparedness for climate-related risks and natural catastrophes and the effectiveness of climate change strategy planning, mitigation, and adaptation (including early warning signs) | 13.1, 13.2, and 13.3 |
 | Aim to strengthen the global partnership for the SDGs and share information, technology, and financial resources with developing countries and respect each country’s policies and strategies for implementing efforts to eradicate poverty and achieve the SDGs | 17.15 and 17.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, Y.-J.; Khant, N.A.; Kim, H.; Namkoong, S. Impact of Climate Change on Waterborne Diseases: Directions towards Sustainability. Water 2023, 15, 1298. https://doi.org/10.3390/w15071298
Jung Y-J, Khant NA, Kim H, Namkoong S. Impact of Climate Change on Waterborne Diseases: Directions towards Sustainability. Water. 2023; 15(7):1298. https://doi.org/10.3390/w15071298
Chicago/Turabian StyleJung, Yong-Ju, Naing Aung Khant, Heejung Kim, and Sim Namkoong. 2023. "Impact of Climate Change on Waterborne Diseases: Directions towards Sustainability" Water 15, no. 7: 1298. https://doi.org/10.3390/w15071298
APA StyleJung, Y.-J., Khant, N. A., Kim, H., & Namkoong, S. (2023). Impact of Climate Change on Waterborne Diseases: Directions towards Sustainability. Water, 15(7), 1298. https://doi.org/10.3390/w15071298











