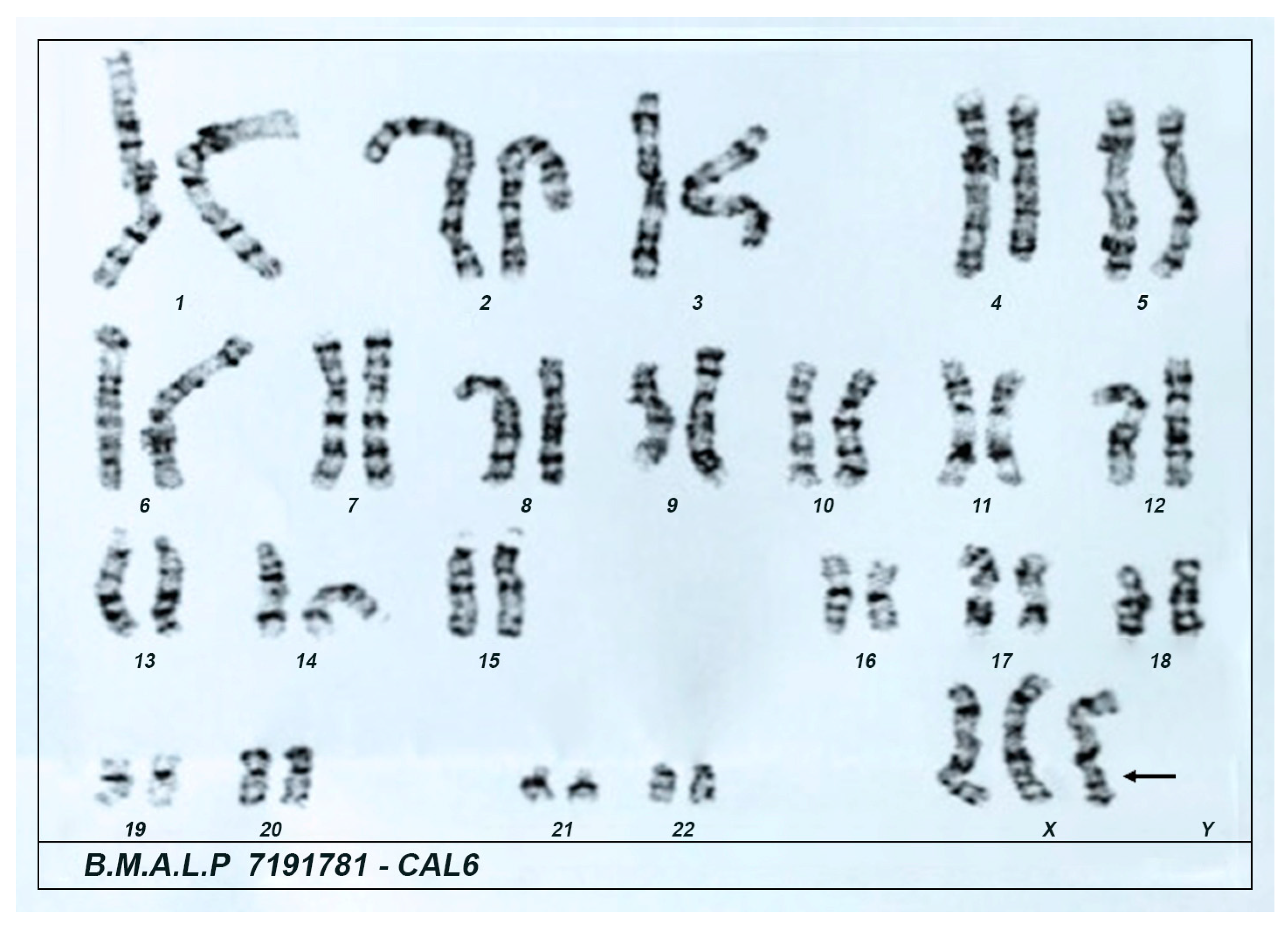
Unique Case Report: A Rare Association of 21-Hydroxylase Deficiency with Triple X Karyotype
Abstract
1. Introduction
2. Patient Information and Clinical Findings
3. Diagnostic Approach
3.1. Laboratory Assessment
3.2. Molecular Analysis of the CYP21A2 Gene
4. Follow-Up and Outcomes
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 17-OHP | 17-hydroxyprogesterone |
| 21OHD | 21-hydroxylase enzyme deficiency |
| ADHD | attention-deficit hyperactivity disorder |
| CAH | congenital adrenal hyperplasia |
| FSH | follicle stimulating hormone |
| FT4 | free thyroxine |
| IGF-1 | insulin-like growth factor 1 |
| LH | luteinizing hormone |
| NC-CAH | non-classical congenital adrenal hyperplasia |
| POF | primary ovarian failure |
| SDHEA | dehydroepiandrosterone sulfate |
| TSH | thyroid stimulating hormone |
References
- Carvalho, B.; Marques, C.J.; Santos-Silva, R.; Fontoura, M.; Carvalho, D.; Carvalho, F. Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency: An Update on Genetic Analysis of CYP21A2 Gene. Exp. Clin. Endocrinol. Diabetes 2021, 129, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Auer, M.K.; Nordenström, A.; Lajic, S.; Reisch, N. Congenital adrenal hyperplasia. Lancet 2023, 401, 227–244. [Google Scholar] [CrossRef] [PubMed]
- Kocova, M.; Concolino, P.; Falhammar, H. Characteristics of In2G Variant in Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency. Front. Endocrinol. 2022, 12, 788812. [Google Scholar] [CrossRef]
- El-Maouche, D.; Arlt, W.; Merke, D.P. Congenital adrenal hyperplasia. Lancet 2017, 390, 2194–2210. [Google Scholar] [CrossRef] [PubMed]
- Nordenström, A.; Falhammar, H. MANAGEMENT OF ENDOCRINE DISEASE: Diagnosis and management of the patient with non-classic CAH due to 21-hydroxylase deficiency. Eur. J. Endocrinol. 2019, 180, R127–R145. [Google Scholar] [CrossRef]
- Merke, D.P.; Auchus, R.J. Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency. N. Engl. J. Med. 2020, 383, 1248–1261. [Google Scholar] [CrossRef]
- Villanueva, A.L.; Rebar, R.W. Triple-X syndrome and premature ovarian failure. Obstet. Gynecol. 1983, 62 (Suppl. S3), 70s–73s. [Google Scholar]
- Otter, M.; Campforts, B.C.M.; Stumpel, C.T.R.M.; van Amelsvoort, T.A.M.J.; Drukker, M. Triple X syndrome: Psychiatric disorders and impaired social functioning as a risk factor. Eur. Psychiatry 2022, 66, e7. [Google Scholar] [CrossRef]
- Wigby, K.; D’Epagnier, C.; Howell, S.; Reicks, A.; Wilson, R.; Cordeiro, L.; Tartaglia, N. Expanding the phenotype of Triple X syndrome: A comparison of prenatal versus postnatal diagnosis. Am. J. Med. Genet. A 2016, 170, 2870–2881. [Google Scholar] [CrossRef]
- Moskwinska, K.; Sniadecki, M.; Wydra, D. Dysgerminoma of the ovary in a patient with triple-X syndrome (47,XXX) and Marfanoid habitus features. Ginekol. Pol. 2021, 92, 466–467. [Google Scholar] [CrossRef]
- Inácio, I.; Serra-Caetano, J.; Cardoso, R.; Dinis, I.; Mirante, A. Rare Coexistence of Congenital Adrenal Hyperplasia due to 21-Hydroxylase Deficiency and Turner Syndrome: A Case Report and Brief Literature Review. J. Clin. Res. Pediatr. Endocrinol. 2023, 15, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.F.; Chan, A.O.K.; Fok, J.M.C.; Mak, M.W.H.; Yu, K.C.; Lee, K.M.; Shek, C.C. Late presentation of simple virilising 21-hydroxylase deficiency in a Chinese woman with Turner’s syndrome. Hong Kong Med. J. = Xianggang Yi Xue Za Zhi 2013, 19, 268–271. [Google Scholar] [CrossRef] [PubMed]
- Kurtoğlu, S.; Atabek, M.E.; Akçakuş, M.; Ozkul, Y.; Saatçi, C. Triple-x syndrome accompanied by congenital adrenal hyperplasia: Case report. Turk. J. Pediatr. 2004, 46, 377–379. [Google Scholar] [PubMed]
- Speiser, P.W.; Arlt, W.; Auchus, R.J.; Baskin, L.S.; Conway, G.S.; Merke, D.P.; Meyer-Bahlburg, H.F.L.; Miller, W.L.; Murad, M.H.; Oberfield, S.E.; et al. Congenital Adrenal Hyperplasia Due to Steroid 21-Hydroxylase Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2018, 103, 4043–4088. [Google Scholar] [CrossRef]
- Coeli-Lacchini, F.B.; Turatti, W.; Elias, P.C.L.; Elias, L.L.K.; Martinelli, C.E.J.; Moreira, A.C.; Antonini, S.R.; de Castro, M. A rational, non-radioactive strategy for the molecular diagnosis of congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Gene 2013, 526, 239–245. [Google Scholar] [CrossRef]
- Yang, Z.; Mendoza, A.R.; Welch, T.R.; Zipf, W.B.; Yu, C.Y. Modular variations of the human major histocompatibility complex class III genes for serine/threonine kinase RP, complement component C4, steroid 21-hydroxylase CYP21, and tenascin TNX (the RCCX module). A mechanism for gene deletions and disease associations. J. Biol. Chem. 1999, 274, 12147–12156. [Google Scholar]
- Pignatelli, D.; Carvalho, B.L.; Palmeiro, A.; Barros, A.; Guerreiro, S.G.; Maçut, D. The complexities in genotyping of congenital adrenal hyperplasia: 21-hydroxylase deficiency. Front. Endocrinol. 2019, 10, 432. [Google Scholar] [CrossRef]
- Blanchong, C.A.; Zhou, B.; Rupert, K.L.; Chung, E.K.; Jones, K.N.; Sotos, J.F.; Zipf, W.B.; Rennebohm, R.M.; Yung Yu, C. Deficiencies of human complement component C4A and C4B and heterozygosity in length variants of RP-C4-CYP21-TNX (RCCX) modules in Caucasians: The load of RCCX genetic diversity on major histocompatibility complex-associated disease. J. Exp. Med. 2000, 191, 2183–2196. [Google Scholar] [CrossRef]
- Liang, D.; Han, M.; Xu, L.; Ren, Y.; Zhang, Y.; Yin, J.; Yang, J.; Liu, Y. Rare combination of simple virilizing form of 21-hydroxylase deficiency, Graves’ disease and 47,XXX in a woman: A case report. Medicine 2022, 101, e31443. [Google Scholar] [CrossRef]
- Kendirci, H.N.P.; Aycan, Z.; Çetinkaya, S.; Baş, V.N.; Ağladıoğlu, S.Y.; Önder, A. A rare combination: Congenital adrenal hyperplasia due to 21 hydroxylase deficiency and Turner syndrome. J. Clin. Res. Pediatr. Endocrinol. 2012, 4, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.T.; Xu, M.Z.; Zhang, Y.R.; Wang, B.R.; Li, M.R.; Gao, L. Refractory hypokalemia with sexual dysplasia and infertility caused by 17α-hydroxylase deficiency and triple X syndrome: A case report. Open Life Sci. 2023, 18, 20220548. [Google Scholar]
- Urakami, T. Tall stature in children and adolescents. Minerva Pediatr. 2020, 72, 472–483. [Google Scholar] [CrossRef] [PubMed]
- Otter, M.; Schrander-Stumpel, C.T.R.M.; Curfs, L.M.G. Triple X syndrome: A review of the literature. Eur. J. Hum. Genet. 2010, 18, 265–271. [Google Scholar]
- Goswami, R.; Goswami, D.; Kabra, M.; Gupta, N.; Dubey, S.; Dadhwal, V. Prevalence of the triple X syndrome in phenotypically normal women with premature ovarian failure and its association with autoimmune thyroid disorders. Fertil. Steril. 2003, 80, 1052–1054. [Google Scholar] [PubMed]
- Yang, Q.; Mumusoglu, S.; Qin, Y.; Sun, Y.; Hsueh, A.J. A kaleidoscopic view of ovarian genes associated with premature ovarian insufficiency and senescence. FASEB J. 2021, 35, e21753. [Google Scholar]
- Vujovic, S. Aetiology of premature ovarian failure. Menopause Int. 2009, 15, 72–75. [Google Scholar]
- Camats, N.; Pandey, A.V.; Fernández-Cancio, M.; Andaluz, P.; Janner, M.; Torán, N.; Moreno, F.; Bereket, A.; Akcay, T.; García-García, E.; et al. Ten novel mutations in the NR5A1 gene cause disordered sex development in 46,XY and ovarian insufficiency in 46,XX individuals. J. Clin. Endocrinol. Metab. 2012, 97, E1294–E1306. [Google Scholar] [CrossRef]
- Suntharalingham, J.P.; Buonocore, F. Europe PMC Funders Group human disease. Best Pract. Res. Clin. Endocrinol. Metab. 2016, 29, 607–619. [Google Scholar] [CrossRef]
- Collins, G.; Patel, B.; Thakore, S.; Liu, J. Primary Ovarian Insufficiency: Current Concepts. South. Med. J. 2017, 110, 147–153. [Google Scholar]

| Hormones | First Sample | Confirmatory Sample | Reference Values |
|---|---|---|---|
| TSH | 0.59 μIU/mL | 0.85 μIU/mL | 0.4–4.5 μIU/mL |
| FT4 | 1.2 μIU/mL | 1.4 μIU/mL | 0.7–1.8 μIU/mL |
| IGF-1 | NA | 214 ng⁄mL | 5–40 years 109.0–284.0 ng/mL |
| Prolactin | 11 ng/mL | 19 ng/mL | Non-pregnancy < 30 ng/mL |
| FSH | 90 IU/L | 105 IU/L | Post-menopause > 30 IU/L |
| LH | 50 IU/L | 69 IU/L | Post-menopause 5.2 to 62.9 IU/L |
| 17-OHP | 728 ng/dL | 1074 ng/dL | Follicular phase: up to 110 ng/dL Luteal phase: 86 to 400 ng/dL |
| Testosterone | 52 ng/dL | 84 ng/dL | Women > 21 years: 12.0–59.5 ng/dL |
| SDHEA | NE | 605 µg/dL | 35–44 years: 74.8–410 µg/dL |
| Time | Cortisol | 17-OH Progesterone |
|---|---|---|
| Basal 0′ | 10.3 NR: 5.0–25.0 µg/dL | 658 NR: FP 20–130 ng/dL NR: LP 100–450 ng/dL |
| After 30′ | 14.7 NR: >18 µg/dL | 1699 1500–6000 ng/dL confirm NC-CAH |
| After 60′ | 17.1 NR: >18 µg/dL | 5808 >1500–6000 ng/dL confirm NC-CAH |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Sousa Azulay, R.S.; Facundo, A.N.; Sousa, S.S.e.; Nascimento, G.C.; Magalhães, M.; de Oliveira Neto, C.P.; de Abreu, J.D.M.F.; Lago, D.C.F.; da Silva Pereira Damianse, S.; de Carvalho, V.C.; et al. Unique Case Report: A Rare Association of 21-Hydroxylase Deficiency with Triple X Karyotype. Genes 2025, 16, 354. https://doi.org/10.3390/genes16030354
de Sousa Azulay RS, Facundo AN, Sousa SSe, Nascimento GC, Magalhães M, de Oliveira Neto CP, de Abreu JDMF, Lago DCF, da Silva Pereira Damianse S, de Carvalho VC, et al. Unique Case Report: A Rare Association of 21-Hydroxylase Deficiency with Triple X Karyotype. Genes. 2025; 16(3):354. https://doi.org/10.3390/genes16030354
Chicago/Turabian Stylede Sousa Azulay, Rossana Santiago, Alexandre Nogueira Facundo, Sarah Sousa e Sousa, Gilvan Cortes Nascimento, Marcelo Magalhães, Clariano Pires de Oliveira Neto, Joana D’arc Matos França de Abreu, Débora Cristina Ferreira Lago, Sabrina da Silva Pereira Damianse, Viviane Chaves de Carvalho, and et al. 2025. "Unique Case Report: A Rare Association of 21-Hydroxylase Deficiency with Triple X Karyotype" Genes 16, no. 3: 354. https://doi.org/10.3390/genes16030354
APA Stylede Sousa Azulay, R. S., Facundo, A. N., Sousa, S. S. e., Nascimento, G. C., Magalhães, M., de Oliveira Neto, C. P., de Abreu, J. D. M. F., Lago, D. C. F., da Silva Pereira Damianse, S., de Carvalho, V. C., Nascimento, C. A., Rodrigues, V. P., Coeli-Lacchini, F. B., de Castro, M., & dos Santos Faria, M. (2025). Unique Case Report: A Rare Association of 21-Hydroxylase Deficiency with Triple X Karyotype. Genes, 16(3), 354. https://doi.org/10.3390/genes16030354






