Hypertrophic Cardiomyopathy: New Clinical and Therapeutic Perspectives of an “Old” Genetic Myocardial Disease
Abstract
1. Introduction
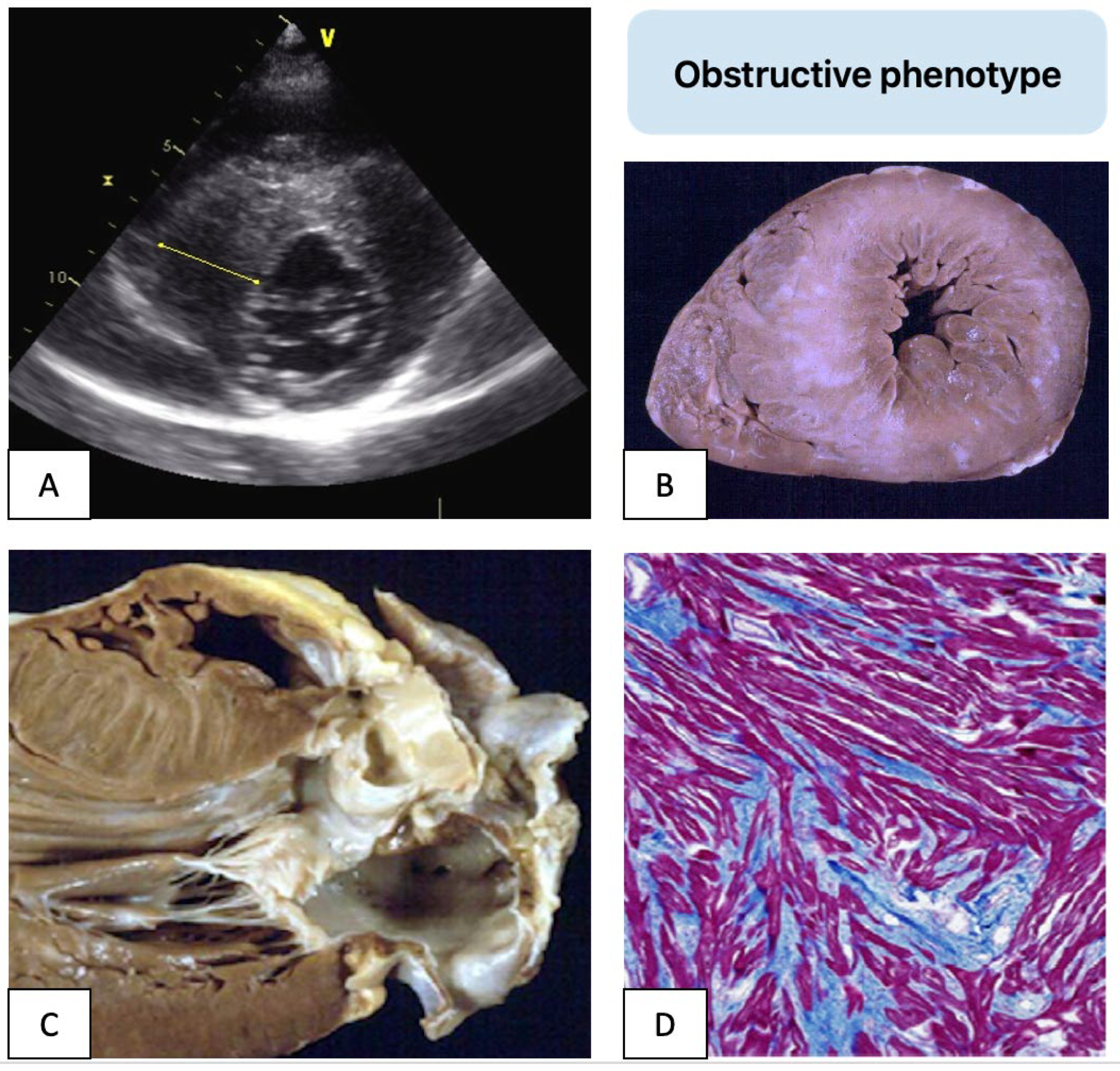
2. Sudden Death Prevention
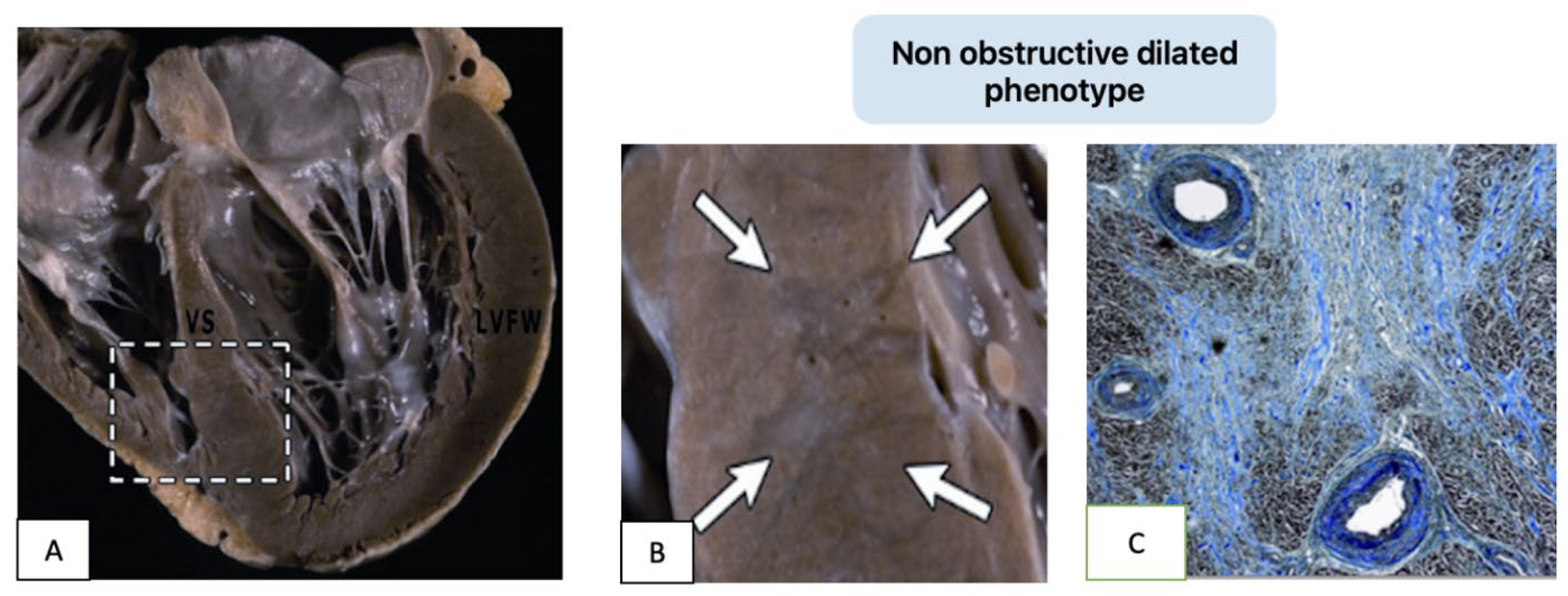
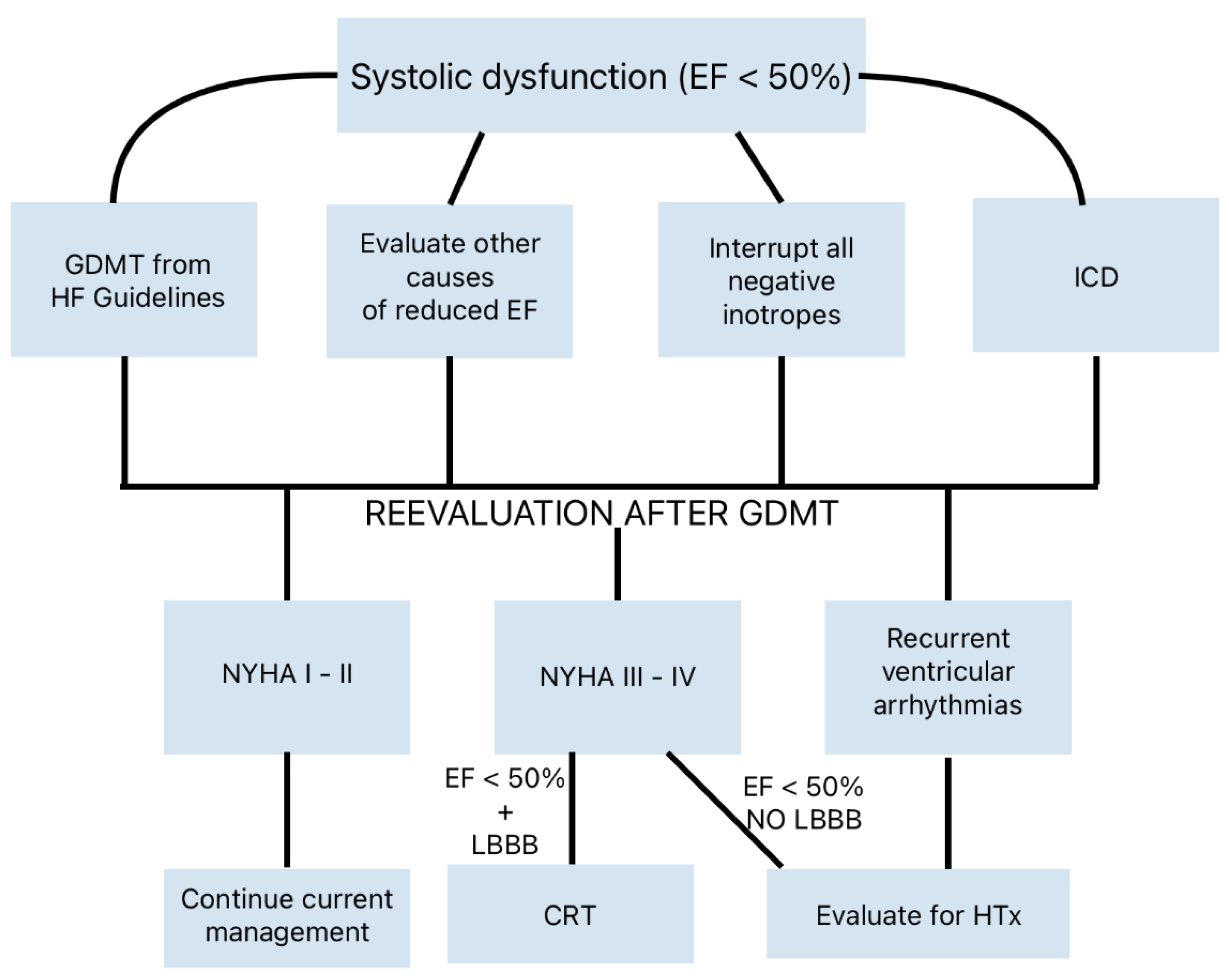
3. Heart Failure Pathways
4. Pharmacological Therapy
5. Interventional/Surgical Therapies
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thiene, G.; Calore, C.; De Gaspari, M.; Basso, C. Storytelling of Hypertrophic Cardiomyopathy Discovery. J. Cardiovasc. Dev. Dis. 2024, 11, 300. [Google Scholar] [CrossRef]
- Teare, D. Asymmetrical hypertrophy of the heart in young adults. Br. Heart J. 1958, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Morrow, A.G.; Braunwald, E. Functional aortic stenosis; a malformation characterized by resistance to left ventricular outflow without anatomic obstruction. Circulation 1959, 20, 181–189. [Google Scholar] [CrossRef]
- Aygen, M.M.; Hilbish, T.F.; Braunwald, E.; Morrow, A.G.; Cornell, W.P. Idiopathic hypertrophic subaortic stenosis: Clinical, hemodynamic and angiographic manifestations. Am. J. Med. 1960, 29, 924–945. [Google Scholar]
- Maron, B.J.; Bonow, R.O.; Salberg, L.; Roberts, W.C.; Braunwald, E. The first patient clinically diagnosed with hypertrophic cardiomyopathy. Am. J. Cardiol. 2008, 102, 1418–1420. [Google Scholar] [CrossRef] [PubMed]
- Jarcho, J.A.; McKenna, W.; Pare, J.A.; Solomon, S.D.; Holcombe, R.F.; Dickie, S.; Levi, T.; Donis-Keller, H.; Seidman, J.G.; Seidman, C.E. Mapping a gene for familial hypertrophic cardiomyopathy to chromosome 14q1. N. Engl. J. Med. 1989, 321, 1372–1378. [Google Scholar] [CrossRef] [PubMed]
- Geisterfer-Lowrance, A.A.; Kass, S.; Tanigawa, G.; Vosberg, H.P.; McKenna, W.; Seidman, C.E.; Seidman, J.G. A molecular basis for familial hypertrophic cardiomyopathy: A beta cardiac myosin heavy chain gene missense mutation. Cell 1990, 62, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Marian, A.J.; Braunwald, E. Hypertrophic Cardiomyopathy: Genetics, Pathogenesis, Clinical Manifestations, Diagnosis, and Therapy. Circ. Res. 2017, 121, 749–770. [Google Scholar] [CrossRef]
- Maron, B.J.; Maron, M.S. The Remarkable 50 Years of Imaging in HCM and How it Has Changed Diagnosis and Management: From M-Mode Echocardiography to CMR. JACC Cardiovasc. Imaging 2016, 9, 858–872. [Google Scholar] [CrossRef] [PubMed]
- Licordari, R.; Trimarchi, G.; Teresi, L.; Restelli, D.; Lofrumento, F.; Perna, A.; Campisi, M.; de Gregorio, C.; Grimaldi, P.; Calabrò, D.; et al. Cardiac Magnetic Resonance in HCM Phenocopies: From Diagnosis to Risk Stratification and Therapeutic Management. J. Clin. Med. 2023, 12, 3481. [Google Scholar] [CrossRef]
- Weng, Z.; Yao, J.; Chan, R.H.; He, J.; Yang, X.; Zhou, Y.; He, Y. Prognostic Value of LGE-CMR in HCM: A Meta-Analysis. JACC Cardiovasc. Imaging 2016, 12, 1392–1402. [Google Scholar] [CrossRef]
- Kim, R.J.; Judd, R.M. Gadolinium-enhanced magnetic resonance imaging in hypertrophic cardiomyopathy: In vivo imaging of the pathologic substrate for premature cardiac death? J. Am. Coll. Cardiol. 2003, 41, 1568–1572. [Google Scholar] [CrossRef]
- Corrado, D.; Basso, C.; Schiavon, M.; Thiene, G. Screening for hypertrophic cardiomyopathy in young athletes. N. Engl. J. Med. 1998, 339, 364–369. [Google Scholar] [CrossRef]
- Corrado, D.; Basso, C.; Thiene, G. Essay: Sudden death in young athletes. Lancet 2005, 366 (Suppl. 1), S47–S48. [Google Scholar] [CrossRef]
- Maron, B.J. Clinical Course and Management of Hypertrophic Cardiomyopathy. N. Engl. J. Med. 2018, 379, 655–668. [Google Scholar] [CrossRef]
- Ommen, S.R.; Ho, C.Y.; Asif, I.M.; Balaji, S.; Burke, M.A.; Day, S.M.; Dearani, J.A.; Epps, K.C.; Evanovich, L.; Ferrari, V.A.; et al. 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR Guideline for the Management of Hypertrophic Cardiomyopathy: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2024, 149, e1239–e1311. [Google Scholar] [CrossRef]
- Arbelo, E.; Protonotarios, A.; Gimeno, J.R.; Arbustini, E.; Barriales-Villa, R.; Basso, C.; Bezzina, C.R.; Biagini, E.; Blom, N.A.; de Boer, R.A.; et al. 2023 ESC Guidelines for the management of cardiomyopathies. Eur. Heart J. 2023, 44, 3503–3626. [Google Scholar]
- Basso, C.; Thiene, G.; Corrado, D.; Buja, G.; Melacini, P.; Nava, A. Hypertrophic cardiomyopathy and sudden death in the young: Pathologic evidence of myocardial ischemia. Hum. Pathol. 2000, 31, 988–998. [Google Scholar] [CrossRef]
- Maron, B.J.; Shen, W.K.; Link, M.S.; Epstein, A.E.; Almquist, A.K.; Daubert, J.P.; Bardy, G.H.; Favale, S.; Rea, R.F.; Boriani, G.; et al. Efficacy of implantable cardioverter-defibrillators for the prevention of sudden death in patients with hypertrophic cardiomyopathy. N. Engl. J. Med. 2000, 342, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Ommen, S.R.; Mital, S.; Burke, M.A.; Day, S.M.; Deswal, A.; Elliott, P.; Evanovich, L.L.; Hung, J.; Joglar, J.A.; Kantor, P.; et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2020, 142, e558–e631. [Google Scholar] [PubMed]
- Rowin, E.J.; Maron, B.J.; Haas, T.S.; Garberich, R.F.; Wang, W.; Link, M.S.; Maron, M.S. Hypertrophic Cardiomyopathy with Left Ventricular Apical Aneurysm: Implications for Risk Stratification and Management. J. Am. Coll. Cardiol. 2017, 69, 761–773. [Google Scholar] [CrossRef]
- Maron, B.J.; Desai, M.Y.; Nishimura, R.A.; Spirito, P.; Rakowski, H.; Towbin, J.A.; Rowin, E.J.; Maron, M.S.; Sherrid, M.V. Diagnosis and Evaluation of Hypertrophic Cardiomyopathy: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2022, 79, 372–389. [Google Scholar] [CrossRef]
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; Mahrholdt, H.; et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar] [PubMed]
- Maron, B.J.; Rowin, E.J.; Maron, M.S. Evolution of risk stratification and sudden death prevention in hypertrophic cardiomyopathy: Twenty years with the implantable cardioverter-defibrillator. Heart Rhythm. 2021, 18, 1012–1023. [Google Scholar] [CrossRef] [PubMed]
- Francia, P.; Ziacchi, M.; Adduci, C.; Ammendola, E.; Pieragnoli, P.; De Filippo, P.; Rapacciuolo, A.; Rella, V.; Migliore, F.; Viani, S.; et al. Clinical course of hypertrophic cardiomyopathy patients implanted with a transvenous or subcutaneous defibrillator. Europace 2023, 25, euad270. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.M.; Spirito, P.; Maron, M.S.; Zenovich, A.G.; Formisano, F.; Lesser, J.R.; Mackey-Bojack, S.; Manning, W.J.; Udelson, J.E.; Maron, B.J. Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation 2006, 114, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Rowin, E.J.; Maron, B.J.; Carrick, R.T.; Patel, P.P.; Koethe, B.; Wells, S.; Maron, M.S. Outcomes in Patients with Hypertrophic Cardiomyopathy and Left Ventricular Systolic Dysfunction. J. Am. Coll. Cardiol. 2020, 75, 3033–3043. [Google Scholar] [CrossRef] [PubMed]
- Melacini, P.; Basso, C.; Angelini, A.; Calore, C.; Bobbo, F.; Tokajuk, B.; Bellini, N.; Smaniotto, G.; Zucchetto, M.; Iliceto, S.; et al. Clinicopathological profiles of progressive heart failure in hypertrophic cardiomyopathy. Eur. Heart J. 2010, 31, 2111–2123. [Google Scholar] [CrossRef] [PubMed]
- Vio, R.; Angelini, A.; Basso, C.; Cipriani, A.; Zorzi, A.; Melacini, P.; Thiene, G.; Rampazzo, A.; Corrado, D.; Calore, C. Hypertrophic Cardiomyopathy and Primary Restrictive Cardiomyopathy: Similarities, Differences and Phenocopies. J. Clin. Med. 2021, 10, 1954. [Google Scholar] [CrossRef]
- Kubo, T.; Gimeno, J.R.; Bahl, A.; Steffensen, U.; Steffensen, M.; Osman, E.; Thaman, R.; Mogensen, J.; Elliott, P.M.; Doi, Y.; et al. Prevalence, Clinical Significance, and Genetic Basis of Hypertrophic Cardiomyopathy with Restrictive Phenotype. J. Am. Coll. Cardiol. 2007, 49, 2419–2426. [Google Scholar] [CrossRef]
- Mogensen, J.; Kubo, T.; Duque, M.; Uribe, W.; Shaw, A.; Murphy, R.; Gimeno, J.R.; Elliott, P.; McKenna, W.J. Idiopathic restrictive cardiomyopathy is part of the clinical expression of cardiac troponin I mutations. J. Clin. Investig. 2003, 111, 209–216. [Google Scholar] [CrossRef]
- Ader, F.; De Groote, P.; Réant, P.; Rooryck-Thambo, C.; Dupin-Deguine, D.; Rambaud, C.; Khraiche, D.; Perret, C.; Pruny, J.F.; Mathieu-Dramard, M.; et al. FLNC pathogenic variants in patients with cardiomyopathies: Prevalence and genotype-phenotype correlations. Clin. Genet. 2019, 96, 317–329. [Google Scholar] [CrossRef] [PubMed]
- Verdonschot, J.A.J.; Vanhoutte, E.K.; Claes, G.R.F.; Helderman-van den Enden, A.T.J.M.; Hoeijmakers, J.G.J.; Hellebrekers, D.M.E.I.; de Haan, A.; Christiaans, I.; Lekanne Deprez, R.H.; Boen, H.M.; et al. A mutation update for the FLNC gene in myopathies and cardiomyopathies. Hum. Mutat. 2020, 41, 1091–1111. [Google Scholar] [CrossRef] [PubMed]
- Celeghin, R.; Cipriani, A.; Bariani, R.; Bueno Marinas, M.; Cason, M.; Bevilacqua, M.; De Gaspari, M.; Rizzo, S.; Rigato, I.; Da Pozzo, S.; et al. Filamin-C variant-associated cardiomyopathy: A pooled analysis of individual patient data to evaluate the clinical profile and risk of sudden cardiac death. Heart Rhythm 2022, 19, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Gaudreault, N.; Ruel, L.J.; Henry, C.; Schleit, J.; Lagüe, P.; Champagne, J.; Sénéchal, M.; Sarrazin, J.F.; Philippon, F.; Bossé, Y.; et al. Novel filamin C (FLNC) variant causes a severe form of familial mixed hypertrophic-restrictive cardiomyopathy. Am. J. Med. Genet. A 2023, 191, 1508–1517. [Google Scholar] [CrossRef]
- Thiene, G.; Corrado, D.; Basso, C. Cardiomyopathies: Is it time for a molecular classification? Eur. Heart J. 2004, 25, 1772–1775. [Google Scholar] [CrossRef] [PubMed]
- Thiene, G.; Basso, C.; Calabrese, F.; Angelini, A.; Valente, M. Twenty years of progress and beckoning frontiers in cardiovascular pathology: Cardiomyopathies. Cardiovasc. Pathol. 2005, 14, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Thiene, G.; Corrado, D.; Basso, C. Revisiting definition and classification of cardiomyopathies in the era of molecular medicine. Eur. Heart J. 2008, 29, 144–146. [Google Scholar] [CrossRef]
- McKenna, W.J.; Maron, B.J.; Thiene, G. Classification, epidemiology, and global burden of cardiomyopathies. Circ. Res. 2017, 121, 722–730. [Google Scholar] [CrossRef] [PubMed]
- De Bortoli, M.; Vio, R.; Basso, C.; Calore, M.; Minervini, G.; Angelini, A.; Melacini, P.; Vitiello, L.; Vazza, G.; Thiene, G.; et al. Novel Missense Variant in MYL2 Gene Associated with Hypertrophic Cardiomyopathy Showing High Incidence of Restrictive Physiology. Circ. Genomic. Precis. Med. 2020, 13, e002824. [Google Scholar] [CrossRef]
- Burke, M.A.; Cook, S.A.; Seidman, J.G.; Seidman, C.E. Clinical and Mechanistic Insights into the Genetics of Cardiomyopathy. J. Am. Coll. Cardiol. 2016, 68, 2871–2886. [Google Scholar] [CrossRef]
- Goodwin, J.F.; Shah, S.P.; Oakley, C.M.; Cohen, J.; Yipintsoi, T.; Pocock, W. Clinical pharmacology of hypertrophic obstructive cardiomyopathy. In Ciba Foundation Symposium: Cardiomyopathies; Wolstenholme, G.E.W., O’Connor, M., Eds.; Little, Brown: Boston, MA, USA, 1964; pp. 189–213. [Google Scholar]
- Ommen, S.R. Sixty Years of Hemodynamic Pharmacology in Obstructive Hypertrophic Cardiomyopathy. N. Engl. J. Med. 2024, 390, 1914–1915. [Google Scholar] [CrossRef] [PubMed]
- Sherrid, M.V.; Shetty, A.; Winson, G.; Kim, B.; Musat, D.; Alviar, C.L.; Homel, P.; Balaram, S.K.; Swistel, D.G. Treatment of obstructive hypertrophic cardiomyopathy symptoms and gradient resistant to first-line therapy with b-blockade or verapamil. Circ. Heart Fail. 2013, 6, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Coppini, R.; Ferrantini, C.; Pioner, J.M.; Santini, L.; Wang, Z.J.; Palandri, C.; Scardigli, M.; Vitale, G.; Sacconi, L.; Stefàno, P.; et al. Electrophysiological and contractile effects of disopyra mide in patients with obstructive hypertrophic cardiomyopathy. JACC Basic Transl. Sci. 2019, 4, 795–813. [Google Scholar] [CrossRef]
- Adler, A.; Fourey, D.; Weissler-Snir, A.; Hindieh, W.; Chan, R.H.; Gollob, M.H.; Rakowski, H. Safety of Outpatient Initiation of Disopyramide for Obstructive Hypertrophic Cardiomyopathy Patients. J. Am. Heart Assoc. 2017, 6, e005152. [Google Scholar] [CrossRef] [PubMed]
- Coppini, R.; Ferrantini, C.; Yao, L.; Fan, P.; Del Lungo, M.; Stillitano, F.; Sartiani, L.; Tosi, B.; Suffredini, S.; Tesi, C.; et al. Late sodium current inhibition reverses electromechanical dysfunction human hypertrophic cardiomyopathy. Circulation 2013, 127, 575–584. [Google Scholar] [CrossRef]
- Olivotto, I.; Camici, P.G.; Merlini, P.A.; Rapezzi, C.; Patten, M.; Climent, V.; Sinagra, G.; Tomberli, B.; Marin, F.; Ehlermann, P. Efficacy of ranolazine in patients with symptomatic hypertrophic cardiomyopathy: The RESTYLE-HCM randomized, double-blind, placebocontrolled study. Circ. Heart Fail. 2018, 11, e004124. [Google Scholar] [CrossRef]
- Green, E.M.; Wakimoto, H.; Anderson, R.L.; Evanchik, M.J.; Gorham, J.M.; Harrison, B.C.; Henze, M.; Kawas, R.; Oslob, J.D.; Rodriguez, H.M.; et al. A small-molecule inhibitor of sarcomere contractility suppresses hypertrophic cardiomyopathy in mice. Science 2016, 351, 617–621. [Google Scholar] [CrossRef]
- Olivotto, I.; Oreziak, A.; Barriales-Villa, R.; Abraham, T.P.; Masri, A.; Garcia-Pavia, P.; Saberi, S.; Lakdawala, N.K.; Wheeler, M.T.; Owens, A.; et al. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2020, 396, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Pavia, P.; Oręziak, A.; Masri, A.; Barriales-Villa, R.; Abraham, T.P.; Owens, A.T.; Jensen, M.K.; Wojakowski, W.; Seidler, T.; Hagege, A.; et al. Long-term effect of mavacamten in obstructive hypertrophic cardiomyopathy. Eur. Heart J. 2024, 45, 5071–5083. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.Y.; Owens, A.; Geske, J.B.; Wolski, K.; Naidu, S.S.; Smedira, N.G.; Cremer, P.C.; Schaff, H.; McErlean, E.; Sewell, C.; et al. Myosin inhibition in patients with obstructive hypertrophic cardiomyopathy referred for septal reduction therapy. J. Am. Coll. Cardiol. 2022, 80, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Maron, M.S.; Masri, A.; Nassif, M.E.; Barriales-Villa, R.; Arad, M.; Cardim, N.; Choudhury, L.; Claggett, B.; Coats, C.J.; Düngen, H.-D.; et al. Aficamten for symptomatic obstructive hypertrophic cardiomyopathy. N. Engl. J. Med. 2024, 390, 1849–1861. [Google Scholar] [CrossRef] [PubMed]
- Marstrand, P.; Han, L.; Day, S.M.; Olivotto, I.; Ashley, E.A.; Michels, M.; Pereira, A.C.; Wittekind, S.G.; Helms, A.; Saberi, S.; et al. Hypertrophic cardiomyopathy with left ventricular systolic dysfunction: Insights from the SHaRe registry. Circulation 2020, 141, 1371–1383. [Google Scholar] [CrossRef] [PubMed]
- Argirò, A.; Zampieri, M.; Marchi, A.; Cappelli, F.; Del Franco, A.; Mazzoni, C.; Cecchi, F.; Olivotto, I. Stage-specific therapy for hypertrophic cardiomyopathy. Eur. Heart J. Suppl. 2023, 25 (Suppl. C), C155–C161. [Google Scholar] [CrossRef]
- MacIntyre, C.; Lakdawala, N.K. Management of atrial fibrillation in hypertrophic cardiomyopathy. Circulation 2016, 133, 1901–1905. [Google Scholar] [CrossRef]
- Boll, G.; Rowin, E.J.; Maron, B.J.; Wang, W.; Rastegar, H.; Maron, M.S. Efficacy of combined Cox-Maze IV and ventricular septal myectomy for treatment of atrial fibrillation in patients with obstructive hypertrophic cardiomyopathy. Am. J. Cardiol. 2020, 125, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Rowin, E.J.; Link, M.S.; Maron, M.S.; Maron, B.J. Evolving Contemporary Management of Atrial Fibrillation in Hypertrophic Cardiomyopathy. Circulation 2023, 148, 1797–1811. [Google Scholar] [CrossRef]
- Ferrazzi, P.; Spirito, P.; Iacovoni, A.; Calabrese, A.; Migliorati, K.; Simon, C.; Pentiricci, S.; Poggio, D.; Grillo, M.; Amigoni, P.; et al. Transaortic chordal cutting: Mitral valve repair for obstructive hypertrophic cardiomyopathy with mild septal hypertrophy. J. Am. Coll. Cardiol. 2015, 66, 1687–1696. [Google Scholar] [CrossRef]
- Laredo, M.; Khraiche, D.; Raisky, O.; Gaudin, R.; Bajolle, F.; Maltret, A.; Chevret, S.; Bonnet, D.; Vouhé, P.R. Long-term results of the modified Konno procedure in high-risk children with obstructive hypertrophic cardiomyopathy. J. Thorac. Cardiovasc. Surg. 2018, 156, 2285–2294. [Google Scholar] [CrossRef]
- Maron, B.J.; A Dearani, J.; Ommen, S.R.; Maron, M.S.; Schaff, H.V.; A Nishimura, R.; Ralph-Edwards, A.; Sherrid, M.V.; Swistel, D.G.; Balaram, S.; et al. Low operative mortality achieved with surgical septal myectomy: Role of dedicated hypertrophic cardiomyopathy centers in the management of dynamic subaortic obstruction. J. Am. Coll. Cardiol. 2015, 66, 1307–1308. [Google Scholar] [CrossRef] [PubMed]
- Rastegar, H.; Boll, G.; Rowin, E.J.; Dolan, N.; Carroll, C.; Udelson, J.E.; Wang, W.; Carpino, P.; Maron, B.J.; Maron, M.S.; et al. Results of surgical septal myectomy for obstructive hypertrophic cardiomyopathy: The Tufts experience. Ann. Cardiothorac. Surg. 2017, 6, 353–363. [Google Scholar] [CrossRef] [PubMed]
- McLeod, C.J.; Ommen, S.R.; Ackerman, M.J.; Weivoda, P.L.; Shen, W.K.; Dearani, J.A.; Schaff, H.V.; Tajik, A.J.; Gersh, B.J. Surgical septal myectomy decreases the risk of appropriate implantable cardioverter-defibrillator discharges in obstructive hypertrophic cardiomyopathy. Eur. Heart J. 2007, 28, 2583–2588. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.Y.; Bhonsale, A.; Smedira, N.G.; Naji, P.; Thamilarasan, M.; Lytle, B.W.; Lever, H.M. Predictors of long-term outcomes in symptomatic hypertrophic obstructive cardiomyopathy patients undergoing surgical relief of left ventricular outflow tract obstruction. Circulation 2013, 128, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Vriesendorp, P.A.; Liebregts, M.; Steggerda, R.C.; Schinkel, A.F.; Willems, R.; Cate, F.J.T.; van Cleemput, J.; Berg, J.M.T.; Michels, M. Long-term outcomes after medical and invasive treatment in patients with hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. Heart Fail. 2014, 2, 630–636. [Google Scholar]
- Bytyci, I.; Nistri, S.; Morner, S.; Henein, M.Y. Alcohol septal ablation versus septal myectomy treatment of obstructive hypertrophic cardiomyopathy: A systematic review and meta-analysis. J. Clin. Med. 2020, 9, 3062. [Google Scholar] [CrossRef] [PubMed]
- Maurizi, N.; Antiochos, P.; Owens, A.; Lakdwala, N.; Saberi, S.; Russell, M.W.; Fumagalli, C.; Skalidis, I.; Lin, K.Y.; Nathan, A.S.; et al. Long-Term Outcomes After Septal Reduction Therapies in Obstructive Hypertrophic Cardiomyopathy: Insights from the SHARE Registry. Circulation 2024, 150, 1377–1390. [Google Scholar] [CrossRef]
- Greenbaum, A.B.; Ueyama, H.A.; Gleason, P.T.; Khan, J.M.; Bruce, C.G.; Halaby, R.N.; Rogers, T.; Hanzel, G.S.; Xie, J.X.; Byku, I.; et al. Transcatheter Myotomy to Reduce Left Ventricular Outflow Obstruction. J. Am. Coll. Cardiol. 2024, 83, 1257–1272. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J.; Rowin, E.J.; Casey, S.A.; Maron, M.S. How Hypertrophic Cardiomyopathy Became a Contemporary Treatable Genetic Disease with Low Mortality: Shaped by 50 Years of Clinical Research and Practice. JAMA Cardiol. 2016, 1, 98–105. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calore, C.; Mangia, M.; Basso, C.; Corrado, D.; Thiene, G. Hypertrophic Cardiomyopathy: New Clinical and Therapeutic Perspectives of an “Old” Genetic Myocardial Disease. Genes 2025, 16, 74. https://doi.org/10.3390/genes16010074
Calore C, Mangia M, Basso C, Corrado D, Thiene G. Hypertrophic Cardiomyopathy: New Clinical and Therapeutic Perspectives of an “Old” Genetic Myocardial Disease. Genes. 2025; 16(1):74. https://doi.org/10.3390/genes16010074
Chicago/Turabian StyleCalore, Chiara, Mario Mangia, Cristina Basso, Domenico Corrado, and Gaetano Thiene. 2025. "Hypertrophic Cardiomyopathy: New Clinical and Therapeutic Perspectives of an “Old” Genetic Myocardial Disease" Genes 16, no. 1: 74. https://doi.org/10.3390/genes16010074
APA StyleCalore, C., Mangia, M., Basso, C., Corrado, D., & Thiene, G. (2025). Hypertrophic Cardiomyopathy: New Clinical and Therapeutic Perspectives of an “Old” Genetic Myocardial Disease. Genes, 16(1), 74. https://doi.org/10.3390/genes16010074





