Mutations in GHR and IGF1R Genes as a Potential Reason for the Lack of Catch-Up Growth in SGA Children
Abstract
:1. Introduction
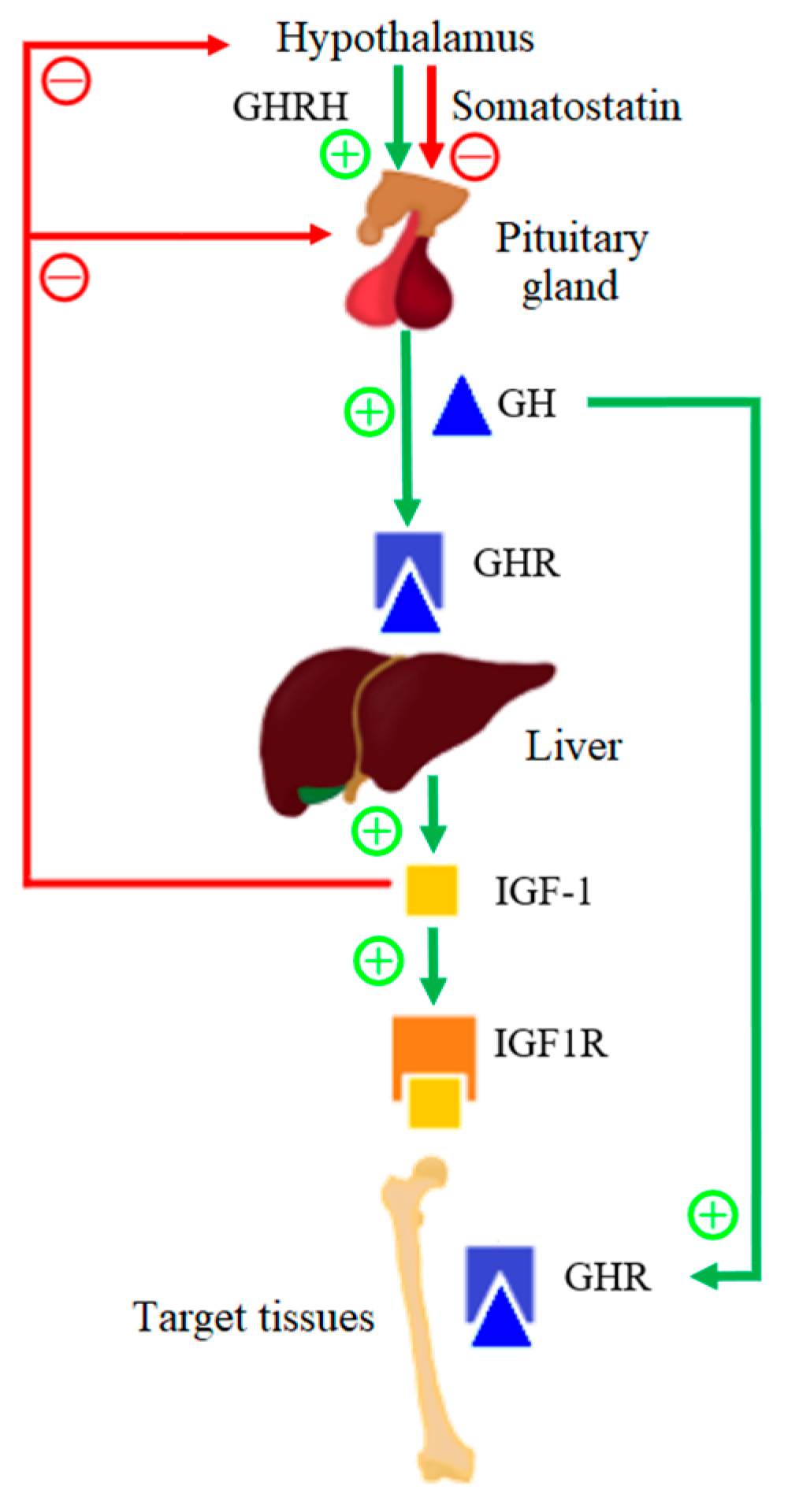
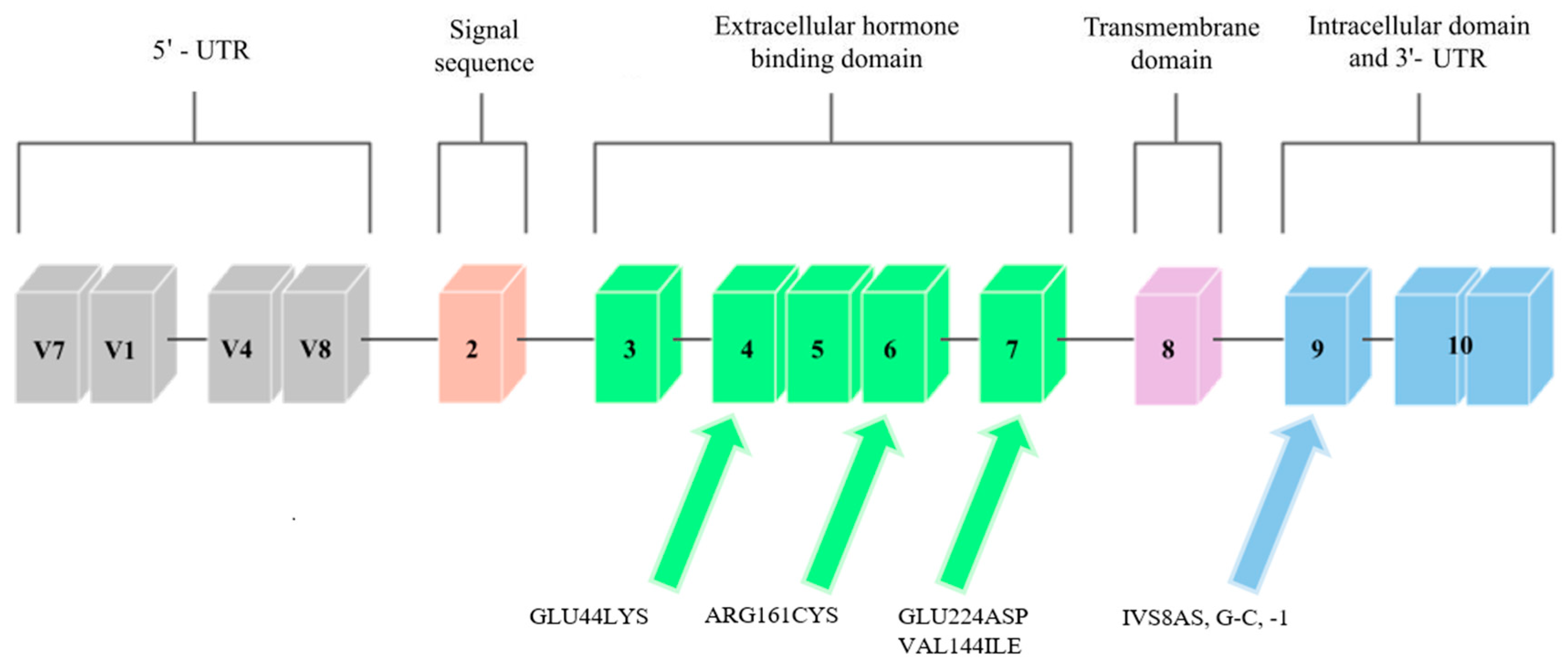
1.1. Growth Hormone Receptor
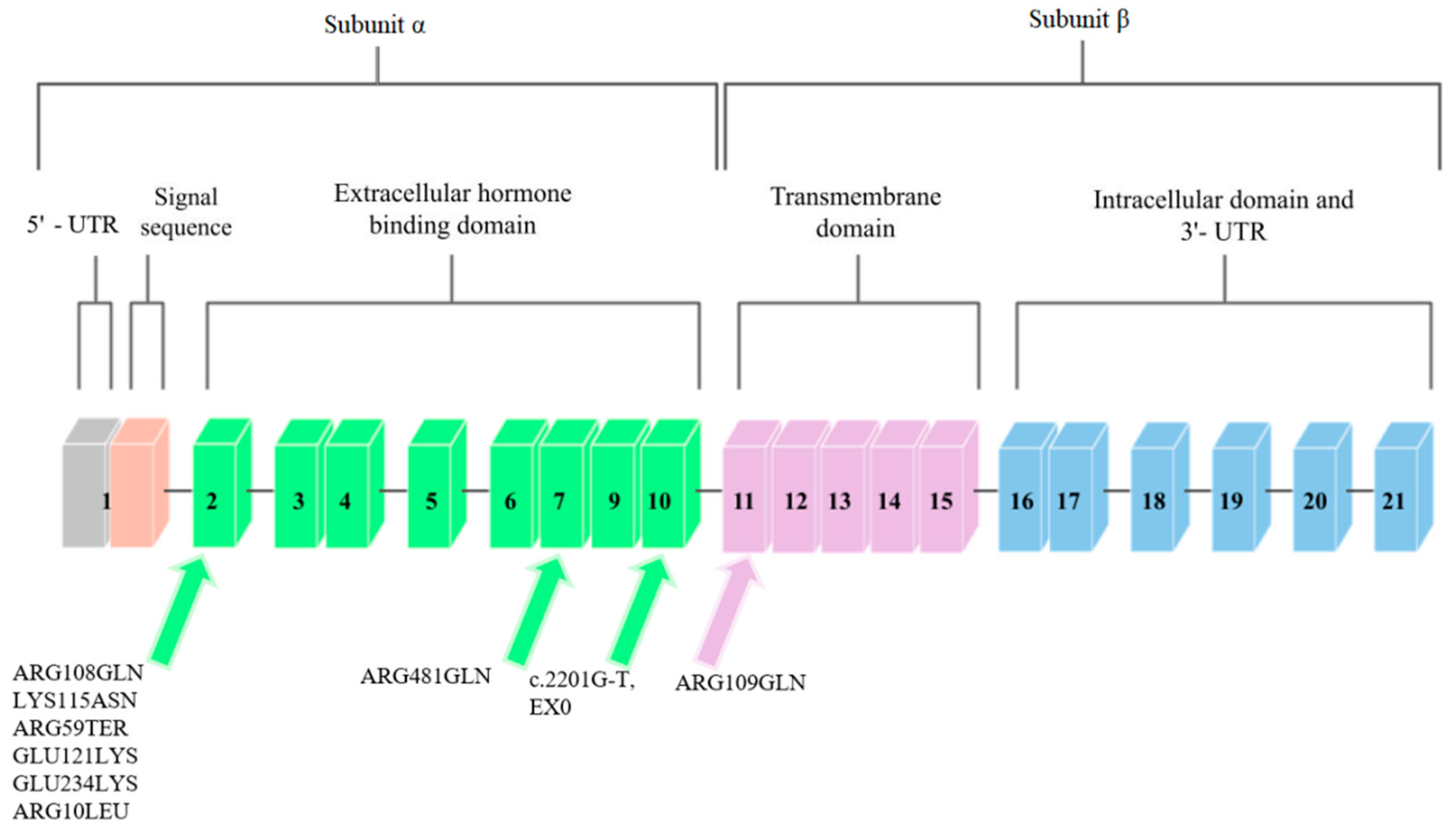
1.2. Insulin-like Growth Factor-1 Receptor
1.3. Methods
1.4. Mutations in the GHR Gene
1.4.1. GLU44LYS, rs121909361
1.4.2. ARG161CYS, rs121909362
1.4.3. GLU224ASP, rs45588036
1.4.4. IVS8AS, G-C, -1 rs730880308
1.4.5. VAL144ILE, rs6413484
1.5. Mutations in the IGF1R Gene
1.5.1. ARG108GLN, rs121912426
1.5.2. LYS115ASN, rs121912427
1.5.3. ARG59TER, rs121912428
1.5.4. ARG709GLN, rs121012429
1.5.5. ARG481GLN, rs33958176
1.5.6. GLU121LYS, rs1555434208
1.5.7. GLU234LYS, rs1253103806
1.5.8. ARG10LEU, rs1409058783
1.5.9. EX10, rs1555460945, c.2201G-T
2. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Anil, K.; Basel, P.; Singh, S. Low birth weight and its associated risk factors: Health facility-based case-control study. PLoS ONE 2020, 15, e0234907. [Google Scholar] [CrossRef]
- World Health Organization. Born Too Soon: The Global Action Report on Preterm Birth. 2012. Available online: http://apps.who.int/iris/bitstream/handle/10665/44864/9789241503433_eng.pdf;jsessionid=FDBEFAF6E212F2ED493326D19B7C7007?sequence=1 (accessed on 9 May 2022).
- Cho, W.K.; Suh, B.-K. Catch-up growth and catch-up fat in children born small for gestational age. Korean J. Pediatr. 2016, 59, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karlberg, J.; Albertsson-Wikland, K. Growth in Full- Term Small-for-Gestational-Age Infants: From Birth to Final Height. Pediatr. Res. 1995, 38, 733–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brooks, A.; Dai, W.; O’Mara, M.; Abankwa, D.; Chhabra, Y.; Pelekanos, R.; Gardon, O.; Tunny, K.; Blucher, K.; Morton, C.; et al. Mechanism of activation of protein kinase JAK2 by the growth hormone receptor. Science 2014, 344, 703–704. [Google Scholar] [CrossRef] [PubMed]
- Murray, P.G.; Clayton, P.E. Endocrine Control of Growth. Am. J. Med. Genet. Part C Semin. Med. Genet. 2013, 163, 76–85. [Google Scholar] [CrossRef]
- Amit, T.; Moussa, B.; Youdim, H.; Hochberg, Z. Does Serum Growth Hormone (GH) Binding Protein Reflect Human GH Receptor Function? J. Clin. Endocrinol. Metab. 2000, 85, 927–932. [Google Scholar] [CrossRef]
- Blum, W.F.; Alherbish, A.; AlSagheir, A.; El Awwa, A.; Kaplan, W.; Koledova, E.; Savage, M.O. The growth hormone–insulin-like growth factor-I axis in the diagnosis and treatment of growth disorders. Endocr. Connect. 2018, 7, 212–222. [Google Scholar] [CrossRef]
- Dehkhoda, F.; Lee, C.M.M.; Medina, J.; Brooks, A.J. The Growth Hormone Receptor: Mechanism of Receptor Activation, Cell Signaling, and Physiological Aspects. Front. Endocrinol. 2018, 9, 35. [Google Scholar] [CrossRef] [Green Version]
- Ding, H.; Wu, T. Insulin-Like Growth Factor Binding Proteins in Autoimmune Diseases. Front. Endocrinol. 2018, 9, 499. [Google Scholar] [CrossRef]
- Dias, C.; Giordano, M.; Frechette, R.; Bellone, S.; Polychronakos, C.; Legault, L.; Deal, C.L.; Goodyer, C.G. Genetic variations at the humangrowth hormone receptor (GHR)gene locus are associated with idiopathic short stature. J. Cell. Mol. Med. 2017, 21, 2985–2999. [Google Scholar] [CrossRef]
- Lin, S.; Li, C.; Li, C.; Zhang, X. Growth Hormone Receptor Mutations Related to Individual Dwarfism. Int. J. Mol. Sci. 2018, 19, 1433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez, J.; Perera, E.; Baumbach, L.; Cleveland, W. Growth Hormone Receptor Mutations in Children with Idiopathic Short Stature. J. Clin. Endocrinol. Metab. 1998, 83, 4079–4083. [Google Scholar] [CrossRef] [PubMed]
- Collett-Solberg, P.; Geoffrey, A.; Blackeljauw, P.; Bidlingmaier, M.; Biller, B.; Boguszewski, M.; Cheung, P.; Choong, C.; Cohen, L.; Cohen, P.; et al. Diagnosis, genetics, and therapy of short stature in children: A growth hormone research society international perspective. Horm. Res. Paediatr. 2020, 92, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Wit, J.; Van Duyvenvoorde, H.; Scheltinga, S.; De Bruin, S.; Hafkenscheid, L.; Kant, S.; Ruivenkamp, C.; Gijsbers, A.; Van Doorn, J.; Feigerlova, E.; et al. Genetic Analysis of Short Children with Apparent Growth Hormone Insensitivity. Horm. Res. Paediatr. 2012, 77, 320–333. [Google Scholar] [CrossRef]
- Godowski, P.; Leung, D.; Meacham, L.; Galgani, J.; Hellmiss, R.; Keret, R.; Rotwein, P.; Parks, J.; Laron, Z.; Wood, W. Characterization of the human growth hormone receptor gene and demonstration of a partial gene deletion in two patients with Laron-type dwarfism. Med. Sci. 1989, 86, 8083–8087. [Google Scholar] [CrossRef] [Green Version]
- Dos Santos, C.; Essioux, L.; Teinturier, C.; Tauber, M.; Goffin, V.; Bougnères, P. A common polymorphism of the growth hormone receptor is associated with increased responsiveness to growth hormone. Nat. Genet. 2004, 36, 720–724. [Google Scholar] [CrossRef]
- Wegmann, M.; Thankamony, A.; Roche, E.; Hoey, H.; Kirk, J.; Shaikh, G.; Ivarsson, S.; Söder, O.; Dunger, D.; Juul, A.; et al. The exon3-deleted growth hormone receptor gene polymorphism (d3-GHR) is associated with insulin and spontaneous growth in short SGA children (NESGAS). Growth Horm. IGF Res. 2017, 35, 45–51. [Google Scholar] [CrossRef]
- Gan, Y.; Buckels, A.; Liu, Y.; Zhang, Y.; Paterson, A.; Jiang, J.; Zinn, K.; Frank, S. Human GH receptor-IGF-1 receptor interaction: Implications for GH signaling. Mol. Endocrinol. 2014, 28, 1841–1854. [Google Scholar] [CrossRef] [Green Version]
- Amselem, S.; Sobrier, M.; Duquesnoy, P.; Rappaport, R.; Postel-Vinay, M.; Gourmelen, M.; Dallapiccola, B.; Goossens, M. Recurrent nonsense mutations in the growth hormone receptor from patients with Laron dwarfism. J. Clin. Investig. 1991, 87, 1098–1102. [Google Scholar] [CrossRef]
- Goddard, D.; Covello, R.; Luoh, S.; Clackson, T.; Attie, K.; Gesundheit, N.; Rundle, A.; Wells, J.; Carlsson, L. Mutations of the Growth Hormone Receptor in Children with Idiopathic Short Stature. The Growth Hormone Insensitivity Study Group. N. Engl. J. Med. 1995, 333, 1093–1098. [Google Scholar] [CrossRef]
- Francke, U.; Yang-Feng, T.; Brissenden, J.; Ullrich, A. Chromosomal mapping of genes involved in growth control. Cold Spring Harb. Symp. Quant. Biol. 1986, 51, 855–866. [Google Scholar] [CrossRef] [PubMed]
- Cooke, D.; Bankert, L.; Roberts, C., Jr.; LeRoith, D.; Casella, S. Analysis of the human type I insulin-like growth factor receptor promoter region. Biochem. Biophys. Res. Commun. 1991, 177, 1113–1120. [Google Scholar] [CrossRef]
- Abuzzahab, M.; Schneider, A.; Goddard, A.; Grigorescu, F.; Lautier, C.; Keller, E.; Kiess Wi Klammt, J.; Kratzsch, J.; Osgood, D.; Pfäffle, R.; et al. IGF-I Receptor Mutations Resulting in Intrauterine and Postnatal Growth Retardation. N. Engl. J. Med. 2003, 349, 2211–2222. [Google Scholar] [CrossRef] [PubMed]
- Gannagé-Yared, M.; Klammt, J.; Chouery, E.; Corbani, S.; Mégarbané, H.; Abou, G.; Choucair, N.; Pfäffle, R.; Mégarbané, A. Homozygous mutation of the IGF1 receptor gene in a patient with severe pre- and postnatal growth failure and congenital malformations. Eur. J. Endocrinol. 2013, 168, K1–K7. [Google Scholar] [CrossRef] [PubMed]
- Prontera, P.; Micale, L.; Verrotti, A.; Napolioni, V.; Stangoni, G.; Merla, G. A New Homozygous IGF1R Variant Defines a Clinically Recognizable Incomplete Dominant form of SHORT Syndrome. Hum. Mutat. 2015, 36, 1043–1047. [Google Scholar] [CrossRef]
- Roback, E.; Barakat, A.; Dev, V.; Mbikay, M.; Chretien, M.; Butler, M. An infant with deletion of the distal long arm of chromosome 15 (q26.1----qter) and loss of insulin-like growth factor 1 receptor gene. Am. J. Med. Genet. 1991, 38, 74–79. [Google Scholar] [CrossRef] [Green Version]
- Ayling, R.; Ross, R.; Towner, P.; Von Laue, S.; Finidori, J.; Moutoussamy, S.; Buchanan, C.; Clayton, P.; Norman, M. A dominant-negative mutation of the growth hormone receptor causes familial short stature. Nat. Genet. 1997, 16, 13–14. [Google Scholar] [CrossRef]
- Kawashima Yuki Kanzaki, S.; Yang, F.; Kinoshita, T.; Hanaki, K.; Nagaishi, J.; Ohtsuka, Y.; Hisatome, I.; Ninomoya, H.; Nanba, E.; Fukushima, T.; et al. Mutation at cleavage site of insulin-like growth factor receptor in a short-stature child born with intrauterine growth retardation. J. Clin. Endocrinol. Metab. 2005, 90, 4679–4687. [Google Scholar] [CrossRef]
- Inagaki, K.; Tiulpakov, A.; Rubtsov Petr Sverdlova, P.; Peterkova, V.; Yakar, S.; Terekhov, S.; LeRoith, D. A familial insulin-like growth factor-I receptor mutant leads to short stature: Clinical and biochemical characterization. J. Clin. Endocrinol. Metab. 2007, 92, 1542–1548. [Google Scholar] [CrossRef] [Green Version]
- Fang, P.; Cho, Y.; Derr, M.; Rosenfeld, R.; Hwa, V.; Cowell, C. Severe short stature caused by novel compound heterozygous mutations of the insulin-like growth factor 1 receptor (IGF1R). J. Clin. Endocrinol. Metab. 2012, 97, 224–243. [Google Scholar] [CrossRef] [Green Version]
- Raile, K.; Klammt, J.; Schneider, A.; Keller, A.; Laue, S.; Smith, R.; Pfäffle, R.; Kratzsch, J.; Keller, E.; Kiess, W. Clinical and functional characteristics of the human Arg59Ter insulin-like growth factor i receptor (IGF1R) mutation: Implications for a gene dosage effect of the human IGF1R. J. Clin. Endocrinol. Metab. 2006, 91, 2264–2271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Author, Year | Mutation | Number of Tested Persons | Qualifications for Research |
|---|---|---|---|
| Goddard et al., 1995 [21] | GLU44LYS, rs121909361; ARG161CYS, rs121909362; GLU224ASP, rs45588036 | 14 | Low body height; more than 2,5 SD below the mean; SD of the serum GHBP concentration less than −2 SD from the mean for age and sex; SD results for serum IGF-I concentration less than 0 for age and sex; maximum GH concentration in serum levels above 10 mg per liter; no systemic disease. |
| Ayling et al., 1997 [28] | IVS8AS, C-C, rs730880308 | 1 | Low body height |
| Sanchez et al., 1998 [13] | VAL144ILE, rs6413484 | 17 | Low body height; more than −2 SD below mean; normal serum GH level; normal IGF-1 level; children with known causes of low height were excluded. |
| Abuzzahab et al., 2003 [24] | ARG108GLN, rs121912426; LYS115ASN, rs121912427 | 42 | Children with IUGR; low body height (less than −2 SD after 18 months of age); children with serum IGF-1 and IGFBP-3 below the normal reference range for age were excluded; chronically ill children. |
| Abuzzahab et al., 2003 [24] | ARG59TER, rs121912428 | 50 | Children with potential IGF-1 resistance who had body heights more than −2,5 SD below the mean for a given age; a serum IGF-1 concentration more than 2 SD above the mean for age and sex. |
| Kawashima et al., 2005 [29] | ARG709GLN, rs121012429 | 24 | Low body height; more than −2 SD below the mean; IUGR defined at birth. |
| Inagaki et al., 2007 [30] | ARG481GLN, rs33958176 | 1 | Low body height; more than −5 SD below the mean SGA. |
| Fang et al., 2012 [31] | GLU121LYS, rs1555434208; GLU234LYS, rs1253103806 | 2 | Low body height; more than −3 SD below the mean; IUGR and SGA defined at birth. |
| Gannage-Yared et al., 2013 [31] | ARG10LEU, rs1409058783 | 1 | Low body height; more than −3 SD below the mean; IUGR defined at birth. |
| Prontera et al., 2015 [26] | EX10, rs1555460945, c.2201G-T | 1 | Low body height; more than −3 SD below the mean; IUGR defined at birth. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stróżewska, W.; Durda-Masny, M.; Szwed, A. Mutations in GHR and IGF1R Genes as a Potential Reason for the Lack of Catch-Up Growth in SGA Children. Genes 2022, 13, 856. https://doi.org/10.3390/genes13050856
Stróżewska W, Durda-Masny M, Szwed A. Mutations in GHR and IGF1R Genes as a Potential Reason for the Lack of Catch-Up Growth in SGA Children. Genes. 2022; 13(5):856. https://doi.org/10.3390/genes13050856
Chicago/Turabian StyleStróżewska, Weronika, Magdalena Durda-Masny, and Anita Szwed. 2022. "Mutations in GHR and IGF1R Genes as a Potential Reason for the Lack of Catch-Up Growth in SGA Children" Genes 13, no. 5: 856. https://doi.org/10.3390/genes13050856
APA StyleStróżewska, W., Durda-Masny, M., & Szwed, A. (2022). Mutations in GHR and IGF1R Genes as a Potential Reason for the Lack of Catch-Up Growth in SGA Children. Genes, 13(5), 856. https://doi.org/10.3390/genes13050856






