Prospective Study of the Phenotypic and Mutational Spectrum of Ocular Albinism and Oculocutaneous Albinism
Abstract
:1. Introduction
2. Materials and Methods
3. Results
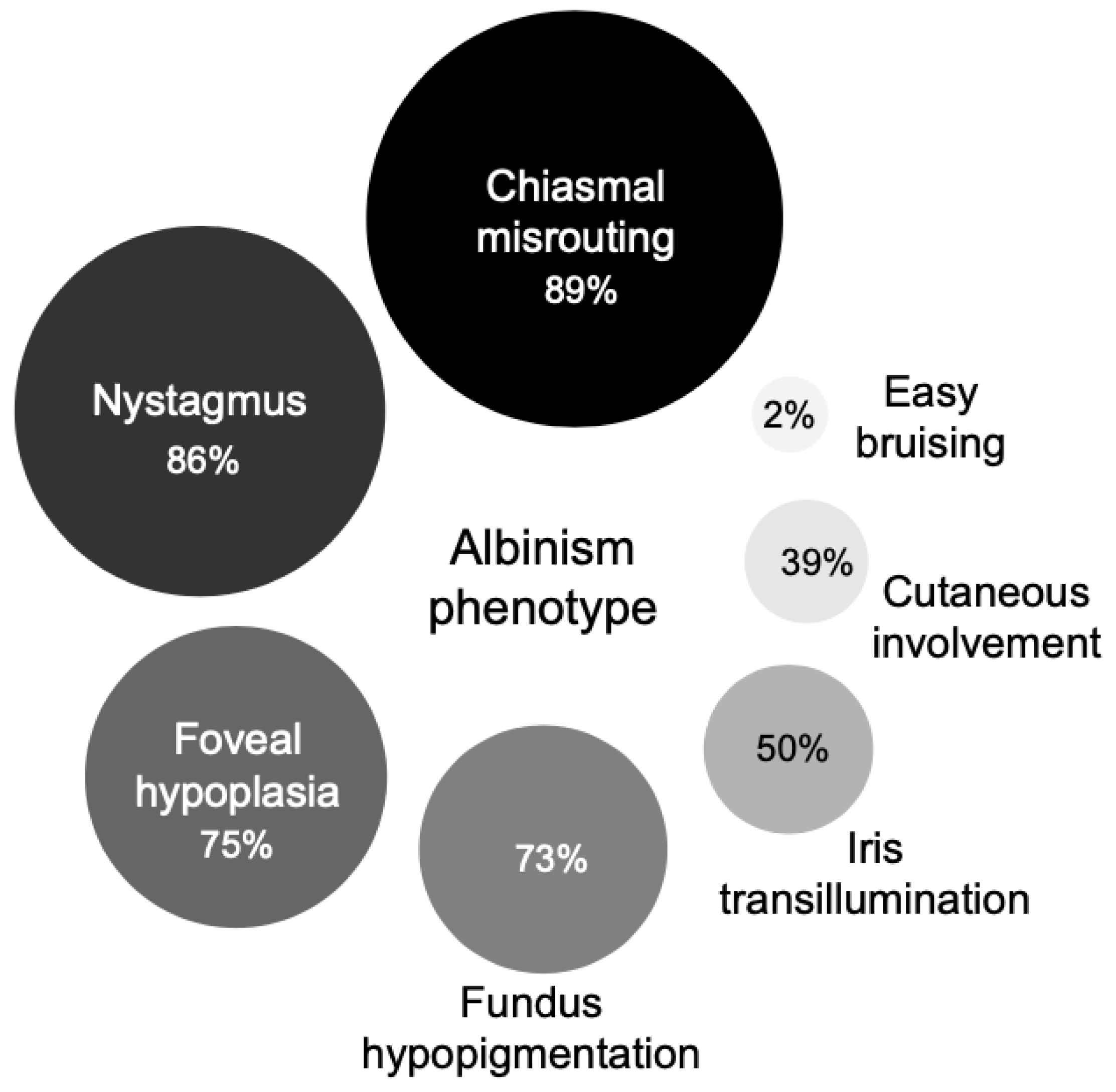
3.1. Clinical Findings
3.2. Genetic Sequencing Outcomes
3.3. Genotype-Phenotype Correlation
3.3.1. Oculocutaneous Albinism Type I (TYR)
3.3.2. Oculocutaneous Albinism Type II (OCA2)
3.3.3. Hermansky–Pudlak Syndrome (HPS)
3.3.4. Ocular Albinism (GPR143)
3.3.5. Non-Albinism Cases
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bharti, K.; Nguyen, M.-T.T.; Skuntz, S.; Bertuzzi, S.; Arnheiter, H. The other pigment cell: Specification and development of the pigmented epithelium of the vertebrate eye. Pigment. Cell Res. 2006, 19, 380–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Surace, E.M.; Angeletti, B.; Ballabio, A.; Marigo, V. Expression pattern of the ocular albinism type 1 (Oa1) gene in the murine retinal pigment epithelium. Investig. Ophthalmol. Vis. Sci. 2000, 41, 4333–4337. [Google Scholar]
- Sturm, R.A.; Duffy, D.L. Human pigmentation genes under environmental selection. Genome Biol. 2012, 13, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strongin, A.C.; Guillery, R.W. The distribution of melanin in the developing optic cup and stalk and its relation to cellular degeneration. J. Neurosci. 1981, 1, 1193–1204. [Google Scholar] [CrossRef]
- Silver, J.; Sapiro, J. Axonal guidance during development of the optic nerve: The role of pigmented epithelia and other extrinsic factors. J. Comp. Neurol. 1981, 202, 521–538. [Google Scholar] [CrossRef] [PubMed]
- Silver, J. Studies on the factors that govern directionality of axonal growth in the embryonic optic nerve and at the chiasm of mice. J. Comp. Neurol. 1984, 223, 238–251. [Google Scholar] [CrossRef]
- Tsang, S.H.; Sharma, T. X-linked Ocular Albinism. Tissue Eng. 2018, 1085, 49–52. [Google Scholar] [CrossRef]
- Hutton, S.M.; Spritz, R.A. Comprehensive Analysis of Oculocutaneous Albinism among Non-Hispanic Caucasians Shows that OCA1 Is the Most Prevalent OCA Type. J. Investig. Dermatol. 2008, 128, 2442–2450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grønskov, K.; Ek, J.; Brondum-Nielsen, K. Oculocutaneous albinism. Orphanet J. Rare Dis. 2007, 2, 43. [Google Scholar] [CrossRef] [Green Version]
- Simeonov, D.R.; Wang, X.; Wang, C.; Sergeev, Y.; Dolinska, M.; Bower, M.; Fischer, R.; Winer, D.; Dubrovsky, G.; Balog, J.Z.; et al. DNA Variations in Oculocutaneous Albinism: An Updated Mutation List and Current Outstanding Issues in Molecular Diagnostics. Hum. Mutat. 2013, 34, 827–835. [Google Scholar] [CrossRef] [Green Version]
- Rooryck, C.; Morice-Picard, F.; Elçioglu, N.H.; Lacombe, D.; Taieb, A.; Arveiler, B. Molecular diagnosis of oculocutaneous albinism: New mutations in the OCA1-4 genes and practical aspects. Pigment. Cell Melanoma Res. 2008, 21, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Kromberg, J.G.; Jenkins, T. Prevalence of albinism in the South African negro. S. Afr. Med. J. 1982, 61, 383–386. [Google Scholar]
- Kromberg, J.G.R.; Bothwell, J.; Kidson, S.H.; Manga, P.; Kerr, R.; Jenkins, T. Types of Albinism in the Black Southern Africa Population. East Afr. Med. J. 2012, 89, 20–27. [Google Scholar] [PubMed]
- Manga, P.; Kerr, R.; Ramsay, M.; Kromberg, J.G.R. Biology and genetics of oculocutaneous albinism and vitiligo—Common pigmentation disorders in southern Africa. S. Afr. Med. J. 2013, 103, 984–988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schiaffino, M.V. Signaling pathways in melanosome biogenesis and pathology. Int. J. Biochem. Cell Biol. 2010, 42, 1094–1104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- David, C.V. Oculocutaneous albinism. Cutis 2013, 91, E1–E4. [Google Scholar] [PubMed]
- Kobayashi, T.; Imokawa, G.; Bennett, D.C.; Hearing, V.J. Tyrosinase Stabilization by Tyrp1 (the brown Locus Protein). J. Biol. Chem. 1998, 273, 31801–31805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki, T.; Tomita, Y. Recent advances in genetic analyses of oculocutaneous albinism types 2 and 4. J. Dermatol. Sci. 2008, 51, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kausar, T.; Bhatti, M.A.; Ali, M.; Shaikh, R.S.; Ahmed, Z.M. OCA5, a novel locus for non-syndromic oculocutaneous albinism, maps to chromosome 4q24. Clin. Genet. 2013, 84, 91–93. [Google Scholar] [CrossRef]
- Montoliu, L.; Grønskov, K.; Wei, A.-H.; Martínez-García, M.; Fernández, A.; Arveiler, B.; Morice-Picard, F.; Riazuddin, S.; Suzuki, T.; Ahmed, Z.M.; et al. Increasing the complexity: New genes and new types of albinism. Pigment. Cell Melanoma Res. 2013, 27, 11–18. [Google Scholar] [CrossRef]
- Pennamen, P.; Tingaud-Sequeira, A.; Gazova, I.; Keighren, M.; McKie, L.; Marlin, S.; Msc, S.G.H.; Kaplan, J.; Delevoye, C.; Lacombe, D.; et al. Dopachrome tautomerase variants in patients with oculocutaneous albinism. Genet. Med. 2021, 23, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Schiaffino, M.V.; D’Addio, M.; Alloni, A.; Baschirotto, C.; Valetti, C.; Cortese, K.; Puri, C.; Bassi, M.T.; Colla, C.; de Luca, M.; et al. Ocular albinism: Evidence for a defect in an intracellular signal transduction system. Nat. Genet. 1999, 23, 108–112. [Google Scholar] [CrossRef]
- Shen, B.; Rosenberg, B.; Orlow, S.J. Intracellular Distribution and Late Endosomal Effects of the Ocular Albinism Type 1 Gene Product: Consequences of Disease-Causing Mutations and Implications for Melanosome Biogenesis. Traffic 2001, 2, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Garner, A.; Jay, B.S. Macromelanosomes in X-linked ocular albinism. Histopathology 1980, 4, 243–254. [Google Scholar] [CrossRef]
- Palmisano, I.; Bagnato, P.; Palmigiano, A.; Innamorati, G.; Rotondo, G.; Altimare, D.; Venturi, C.; Sviderskaya, E.V.; Piccirillo, R.; Coppola, M.; et al. The ocular albinism type 1 protein, an intracellular G protein-coupled receptor, regulates melanosome transport in pigment cells. Hum. Mol. Genet. 2008, 17, 3487–3501. [Google Scholar] [CrossRef]
- Lam, B.L.; Fingert, J.H.; Shutt, B.C.; Singleton, E.M.; Merin, L.M.; Brown, H.H.; Sheffield, V.C.; Stone, E.M. Clinical and molecular characterization of a family affected with X-linked ocular albinism (OA1). Ophthalmic Genet. 1997, 18, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.-L.; Wang, J.-P.; Tseng, Y.-J.; Liu, L.; Kang, Y.-C.; Chen, K.-J.; Chao, A.-N.; Yeh, L.-K.; Chen, T.-L.; Hwang, Y.-S.; et al. Multimodal Imaging of Mosaic Retinopathy in Carriers of Hereditary X-Linked Recessive Diseases. Retina 2018, 38, 1047–1057. [Google Scholar] [CrossRef] [PubMed]
- Huizing, M.; Malicdan, M.C.V.; Wang, J.A.; Pri-Chen, H.; Hess, R.A.; Fischer, R.; O’Brien, K.J.; Merideth, M.A.; Gahl, W.A.; Gochuico, B.R. Hermansky–Pudlak syndrome: Mutation update. Hum. Mutat. 2019, 41, 543–580. [Google Scholar] [CrossRef] [PubMed]
- Pennamen, P.; Le, L.; Tingaud-Sequeira, A.; Fiore, M.; Bauters, A.; Béatrice, N.V.D.; Coste, V.; Bordet, J.-C.; Plaisant, C.; Diallo, M.; et al. BLOC1S5 pathogenic variants cause a new type of Hermansky–Pudlak syndrome. Genet. Med. 2020, 22, 1–10. [Google Scholar] [CrossRef] [PubMed]
- The National Genomics Research and Healthcare Knowledgebase v5; Genomics England: London, UK, 2019.
- Patel, A.; Hayward, J.D.; Tailor, V.; Nyanhete, R.; Ahlfors, H.; Gabriel, C. The Oculome Panel Test: Next-Generation Sequencing to Diagnose a Diverse Range of Genetic Developmental Eye Disorders. Ophthalmology 2019, 126, 888–907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, D.; Malka, S.; Harding, P.; Palma, J.; Dunbar, H.; Moosajee, M. Molecular diagnostic challenges for non-retinal developmental eye disorders in the United Kingdom. Am. J. Med. Genet. Part C Semin. Med. Genet. 2020, 184, 578–589. [Google Scholar] [CrossRef]
- Taylor, R.L.; Arno, G.; Poulter, J.A.; Khan, K.N.; Morarji, J.; Hull, S.; Pontikos, N.; Martin, A.R.; Smith, K.R.; Ali, M.; et al. Association of Steroid 5α-Reductase Type 3 Congenital Disorder of Glycosylation with Early-Onset Retinal Dystrophy. JAMA Ophthalmol. 2017, 135, 339–347. [Google Scholar] [CrossRef] [Green Version]
- Adzhubei, I.A.; Schmidt, S.; Peshkin, L.; Ramensky, V.E.; Gerasimova, A.; Bork, P. A method and server for predicting damaging missense mutations. Nat. Methods 2010, 7, 248–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, P.C.; Henikoff, S. Predicting Deleterious Amino Acid Substitutions. Genome Res. 2001, 11, 863–874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spritz, R.A.; Ho, L.; Furumura, M.; Hearing, V.J. Mutational Analysis of Copper Binding by Human Tyrosinase. J. Investig. Dermatol. 1997, 109, 207–212. [Google Scholar] [CrossRef] [Green Version]
- Halaban, R.; Svedine, S.; Cheng, E.; Smicun, Y.; Aron, R.; Hebert, D.N. Endoplasmic reticulum retention is a common defect associated with tyrosinase-negative albinism. Proc. Natl. Acad. Sci. USA 2000, 97, 5889–5894. [Google Scholar] [CrossRef] [Green Version]
- Chaki, M.; Mukhopadhyay, A.; Chatterjee, S.; Das, M.; Samanta, S.; Ray, K. Higher prevalence of OCA1 in an ethnic group of eastern India is due to a founder mutation in the tyrosinase gene. Mol. Vis. 2005, 11, 531–534. [Google Scholar] [PubMed]
- Ganguly, K.; Dutta, T.; Saha, A.; Sarkar, D.; Sil, A.; Ray, K.; Sengupta, M. Mapping the TYR gene reveals novel and previously reported variants in Eastern Indian patients highlighting preponderance of the same changes in multiple unrelated ethnicities. Ann. Hum. Genet. 2020, 84, 303–312. [Google Scholar] [CrossRef]
- Monfermé, S.; Lasseaux, E.; Duncombe-Poulet, C.; Hamel, C.; Defoort-Dhellemmes, S.; Drumare, I.; Zanlonghi, X.; Dollfus, H.; Perdomo, Y.; Bonneau, D.; et al. Mild form of oculocutaneous albinism type 1: Phenotypic analysis of compound heterozygous patients with the R402Q variant of the TYR gene. Br. J. Ophthalmol. 2019, 103, 1239–1247. [Google Scholar] [CrossRef] [Green Version]
- Lewis, R.A. Oculocutaneous Albinism Type 2—Retired Chapter, for Historical Reference Only; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Eds.; GeneReviews: Seatle, WA, USA, 1993. [Google Scholar]
- Oetting, W.S.; Garrett, S.S.; Brott, M.; King, R.A. P gene mutations associated with oculocutaneous albinism type II (OCA2). Hum. Mutat. 2005, 25, 323. [Google Scholar] [CrossRef]
- Andersen, J.D.; Pietroni, C.; Johansen, P.; Andersen, M.M.; Pereira, V.A.E.S.; Børsting, C.; Morling, N. Importance of nonsynonymous OCA 2 variants in human eye color prediction. Mol. Genet. Genom. Med. 2016, 4, 420–430. [Google Scholar] [CrossRef] [Green Version]
- Saitoh, S.; Oiso, N.; Wada, T.; Narazaki, O.; Fukai, K. Oculocutaneous albinism type 2 with a P gene missense mutation in a patient with Angelman syndrome. J. Med. Genet. 2000, 37, 392–394. [Google Scholar] [CrossRef] [Green Version]
- Hawkes, J.E.; Cassidy, P.B.; Manga, P.; Boissy, R.E.; Goldgar, D.; Cannon-Albright, L.; Florell, S.R.; Leachman, S.A. Report of a novel OCA2 gene mutation and an investigation of OCA2 variants on melanoma risk in a familial melanoma pedigree. J. Dermatol. Sci. 2013, 69, 30–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Vijlder, H.C.; de Vijlder, J.J.; Neumann, H.A. Oculocutaneous albinism and skin cancer risk. J. Eur. Acad. Dermatol. Venereol. 2013, 27, e433–e434. [Google Scholar] [CrossRef]
- Gradstein, L.; Fitz-Gibbon, E.J.; Tsilou, E.T.; Rubin, B.I.; Huizing, M.; Gahl, W.A. Eye Movement Abnormalities in Hermansky-Pudlak Syndrome. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2005, 9, 369–378. [Google Scholar] [CrossRef]
- Schiff, E.; Tailor, V.; Chan, H.; Theodorou, M.; Webster, A.; Moosajee, M. Novel Biallelic Variants and Phenotypic Features in Patients with SLC38A8-Related Foveal Hypoplasia. Int. J. Mol. Sci. 2021, 22, 1130. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.G.; Kumar, A.; Mohammad, S.; Proudlock, F.A.; Engle, E.C.; Andrews, C. Structural grading of foveal hypoplasia using spectral-domain optical coherence tomography a predictor of visual acuity? Ophthalmology 2011, 118, 1653–1660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, S.; Proudlock, F.A.; Sarvananthan, N.; Roberts, E.O.; Awan, M.; McLean, R.; Surendran, M.; Kumar, A.S.A.; Farooq, S.J.; Degg, C.; et al. Phenotypical characteristics of idiopathic infantile nystagmus with and without mutations in FRMD7. Brain 2008, 131, 1259–1267. [Google Scholar] [CrossRef] [Green Version]
- Betts-Henderson, J.; Bartesaghi, S.; Crosier, M.; Lindsay, S.; Chen, H.-L.; Salomoni, P.; Gottlob, I.; Nicotera, P. The nystagmus-associated FRMD7 gene regulates neuronal outgrowth and development. Hum. Mol. Genet. 2009, 19, 342–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, M.G.; Crosier, M.; Lindsay, S.; Kumar, A.; Araki, M.; Leroy, B.P.; McLean, R.J.; Sheth, V.; Maconachie, G.; Thomas, S.; et al. Abnormal retinal development associated with FRMD7 mutations. Hum. Mol. Genet. 2014, 23, 4086–4093. [Google Scholar] [CrossRef] [Green Version]
- Lasseaux, E.; Plaisant, C.; Michaud, V.; Pennamen, P.; Trimouille, A.; Gaston, L.; Monfermé, S.; Lacombe, D.; Rooryck, C.; Morice-Picard, F.; et al. Molecular characterization of a series of 990 index patients with albinism. Pigment. Cell Melanoma Res. 2018, 31, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Lenassi, E.; Clayton-Smith, J.; Douzgou, S.; Ramsden, S.C.; Ingram, S.; Hall, G. Clinical utility of genetic testing in 201 preschool children with inherited eye disorders. Genet. Med. 2020, 22, 745–751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craig, J.E.; Neighboarhood Consortium; Han, X.; Qassim, A.; Hassall, M.; Bailey, J.N.C.; Kinzy, T.G.; Khawaja, A.P.; An, J.; Marshall, H.; et al. Multitrait analysis of glaucoma identifies new risk loci and enables polygenic prediction of disease susceptibility and progression. Nat. Genet. 2020, 52, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Lima-Cunha, D.; Arno, G.; Corton, M.; Moosajee, M. The Spectrum of PAX6 Mutations and Genotype-Phenotype Correlations in the Eye. Genes 2019, 10, 1050. [Google Scholar] [CrossRef] [Green Version]
- Lima-Cunha, D.; Owen, N.; Tailor, V.; Corton, M.; Theodorou, M.; Moosajee, M. PAX6 missense variants in two families with isolated foveal hypoplasia and nystagmus: Evidence of paternal postzygotic mosaicism. Eur. J. Hum. Genet. 2020, 29, 349–355. [Google Scholar] [CrossRef]
- Stenson, P.D.; Mort, M.; Ball, E.V.; Chapman, M.; Evans, K.; Azevedo, L. The Human Gene Mutation Database (HGMD((R))): Optimizing its use in a clinical diagnostic or research setting. Hum. Genet. 2020, 139, 1197–1207. [Google Scholar] [CrossRef]
- Dolinska, M.B.; Kus, N.J.; Farney, S.K.; Wingfield, P.T.; Brooks, B.P.; Sergeev, Y.V. Oculocutaneous albinism type 1: Link between mutations, tyrosinase conformational stability, and enzymatic activity. Pigment. Cell Melanoma Res. 2017, 30, 41–52. [Google Scholar] [CrossRef] [Green Version]
- Chiang, P.-W.; Spector, E.; Tsai, A.C.-H. Oculocutaneous albinism spectrum. Am. J. Med. Genet. Part A 2009, 149A, 1590–1591. [Google Scholar] [CrossRef]
- Norman, C.S.; O’Gorman, L.; Gibson, J.; Pengelly, R.J.; Baralle, D.; Ratnayaka, J.A.; Griffiths, H.; Rose-Zerilli, M.; Ranger, M.; Bunyan, D.; et al. Identification of a functionally significant tri-allelic genotype in the Tyrosinase gene (TYR) causing hypomorphic oculocutaneous albinism (OCA1B). Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef]
- Grønskov, K.; Jespersgaard, C.; Bruun, G.H.; Harris, P.; Brøndum-Nielsen, K.; Andresen, B.S.; Rosenberg, T. A pathogenic haplotype, common in Europeans, causes autosomal recessive albinism and uncovers missing heritability in OCA1. Sci. Rep. 2019, 9, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Jagirdar, K.; Smit, D.J.; Ainger, S.A.; Lee, K.J.; Brown, D.L.; Chapman, B. Molecular analysis of common polymorphisms within the human Tyrosinase locus and genetic association with pigmentation traits. Pigment. Cell Melanoma Res. 2014, 27, 552–564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tripathi, R.K.; Giebel, L.B.; Strunk, K.M.; Spritz, R.A. A polymorphism of the human tyrosinase gene is associated with temperature-sensitive enzymatic activity. Gene Expr. 2018, 1, 103–110. [Google Scholar]
- Chaki, M.; Sengupta, M.; Mondal, M.; Bhattacharya, A.; Mallick, S.; Bhadra, R.; Indian Genome Variation Consortium; Ray, K. Molecular and Functional Studies of Tyrosinase Variants Among Indian Oculocutaneous Albinism Type 1 Patients. J. Investig. Dermatol. 2011, 131, 260–262. [Google Scholar] [CrossRef]
- Kessel, L.; Kjer, B.; Lei, U.; Duno, M.; Grønskov, K. Genotype-phenotype associations in Danish patients with ocular and oculocutaneous albinism. Ophthalmic Genet. 2021, 2021, 1–9. [Google Scholar] [CrossRef]
- Karczewski, K.J.; Francioli, L.C.; Tiao, G.; Cummings, B.B.; Alföldi, J.; Wang, Q. Variation across 141,456 human exomes and genomes reveals the spectrum of loss-of-function intolerance across human protein-coding genes. bioRxiv 2019. bioRxiv:531210. [Google Scholar]
- Oetting, W.S.; Fryer, J.P.; Shriram, S.; King, R.A. Oculocutaneous Albinism Type 1: The Last 100 Years. Pigment. Cell Res. 2003, 16, 307–311. [Google Scholar] [CrossRef]
- Lamason, R.L.; Mohideen, M.A.; Mest, J.R.; Wong, A.C.; Norton, H.L.; Aros, M.C. SLC24A5, a putative cation exchanger, affects pigmentation in zebrafish and humans. Science 2005, 310, 1782–1786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wasmeier, C.; Romao, M.; Plowright, L.; Bennett, D.C.; Raposo, G.; Seabra, M.C. Rab38 and Rab32 control post-Golgi trafficking of melanogenic enzymes. J. Cell Biol. 2006, 175, 271–281. [Google Scholar] [CrossRef] [Green Version]
- Chiang, P.-W.; Fulton, A.B.; Spector, E.; Hisama, F.M. Synergistic interaction of theOCA2andOCA3genes in a family. Am. J. Med. Genet. Part A 2008, 146A, 2427–2430. [Google Scholar] [CrossRef]
- Zuk, O.; Hechter, E.; Sunyaev, S.R.; Lander, E.S. The mystery of missing heritability: Genetic interactions create phantom heritability. Proc. Natl. Acad. Sci. USA 2012, 109, 1193–1198. [Google Scholar] [CrossRef] [Green Version]
- Chiang, P.-W.; Drautz, J.M.; Tsai, A.C.-H.; Spector, E.; Clericuzio, C.L. A new hypothesis of OCA1B. Am. J. Med. Genet. Part A 2008, 146A, 2968–2970. [Google Scholar] [CrossRef] [PubMed]
- Huizing, M.; Helip-Wooley, A.; Westbroek, W.; Gunay-Aygun, M.; Gahl, W.A. Disorders of Lysosome-Related Organelle Biogenesis: Clinical and Molecular Genetics. Annu. Rev. Genom. Hum. Genet. 2008, 9, 359–386. [Google Scholar] [CrossRef] [Green Version]
- Vicary, G.W.; Vergne, Y.; Santiago-Cornier, A.; Young, L.R.; Roman, J. Pulmonary Fibrosis in Hermansky-Pudlak Syndrome. Ann. Am. Thorac. Soc. 2016, 13, 1839–1846. [Google Scholar] [CrossRef] [Green Version]
- De Jesus-Rojas, W.; Young, L.R. Hermansky-Pudlak Syndrome. Semin. Respir Crit Care Med. 2020, 41, 238–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seward, S.L.; Gahl, W.A. Hermansky-Pudlak Syndrome: Health Care Throughout Life. Pediatrics 2013, 132, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wildsoet, C.F.; Oswald, P.J.; Clark, S. Albinism: Its implications for refractive development. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1–7. [Google Scholar]
- Yahalom, C.; Tzur, V.; Blumenfeld, A.; Greifner, G.; Eli, D.; Rosenmann, A.; Glanzer, S.; Anteby, I. Refractive profile in oculocutaneous albinism and its correlation with final visual outcome. Br. J. Ophthalmol. 2011, 96, 537–539. [Google Scholar] [CrossRef]




| Gene (OMIM) | Phenotype (OMIM) | Inheritance | Family ID (Ethnicity) [Consanguinity] | Allele 1 Allele2 | Variant type | Zygosity | ClinVar ID | gnomAD | Polyphen-2 | SIFT | Pathogenicity ACMG Classification | ACMG Arguments |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TYR(606933) | Albinism, oculocutaneous, type 1A; OCA1A (203100) | AR | 26352 (Middle Eastern) [No] | c.996G>A, p.(Met332Ile) | Missense | Het | Absent | Absent | Probably damaging | Deleterious | 4 | PM1; PM2; PM5; PP3; PP5; BP1 |
| c.1037-7T>A | Splice | Het | 99527 | 0.000861, 0.015 in AJs | NA | NA | 4 | PP5; PM2; BP4 | ||||
| 22151 (White British) [No] | c.1336G>A, p.(Gly446Ser) | Missense | Het | 3801 | 0.00005327 | Possibly damaging | Deleterious | 5 | PP5; PM2; PP3; BP1 | |||
| c.242C>T, p.(Pro81Leu) | Missense | Het | 3772 | 0.00009205 | Probably damaging | Deleterious | 5 | PP5; PM1; PM2; PP3; BP1 | ||||
| 23192-1; 23192-2; 23192-3 (South Asian) [No] | c.1037-7T>A | Splice | Hom | Absent | Absent | NA | NA | 4 | PP5; PM2; BP4 | |||
| 13332 (White British) [No] | c.1118C>A p.(Thr373Lys) | Missense | Het | 3774 | 0.0003541 | Probably damaging | Deleterious | 5 | PP5; PM1; PM2; PP3; BP1 | |||
| c.1A>G p.(Met1Val) | Missense | Het | 3807 | Absent | Possibly damaging | Deleterious | 5 | PVS1; PM2; PP3; PP5 | ||||
| Albinism, oculocutaneous, type IB; OCA1B (606952) | AR | 26680 (White British) [No] | c.575C>A, p.(Ser192Tyr) 1 | Missense | Het | 3778 | 0.2502 | Probably damaging (both variants) | Deleterious (both variants) | Hypomorphic alleles 1 | See text | |
| c.1205G>A, p.(Arg402Gln) 1 | Missense | 3779 | 0.1765 | |||||||||
| c.242C>T, p.(Pro81Leu) | Missense | Het | 3772 | 0.00009205 | Probably damaging | Deleterious | 5 | PP5; PM1; PM2; PP3; BP1 | ||||
| 27560 (White British) [No] | c.1217C>T, p.(Pro406Leu) | Missense | Het | 3777 | 0.003918 | Probably damaging | Deleterious | 5 | PP5; PM1; PM2; PP3; BP1 | |||
| c.1291C>A, p.(Pro431Thr) | Missense | Het | Absent | 0.000007986 | Probably damaging | Deleterious | 4 | PM1; PM2; PP3; PP5; BP1 | ||||
| 26903 (South Asian) [Yes] | c.832C>T, p.(Arg278*) | Nonsense | Hom | 99583 | 0.0001699, 0.001274 in S Asians | NA | NA | 5 | PP5; PVS1; PM2; PP3 | |||
| 27079 (White British) [No] | c.661G>A, p.(Glu221Lys) | Missense | Het | 212524 | 0.00000399 | Possibly damaging | Deleterious | 4 | PM1; PM2; PP3; PP5; BP1 | |||
| c.575C>A, p.(Ser192Tyr) 1 | Missense | Het | 3778 | 0.2502 | Probably damaging (both variants) | Deleterious (both variants) | Hypomorphic alleles 1 | See text | ||||
| c.1205G>A, p.(Arg402Gln) 1 | Missense | 3779 | 0.1765 | |||||||||
| 27430 (White British) [No] | c.823G>T, p.(Val275Phe) | Missense | Het | 3773 | 0.00009916 | Possibly damaging | Deleterious | 5 | PP5; PM2; PP3; BP1 | |||
| c.575C>A, p.(Ser192Tyr) 1 | Missense | Het | 3778 | 0.2502 | Probably damaging (both variants) | Deleterious (both variants) | Hypomorphic alleles 1 | See text | ||||
| c.1205G>A, p.(Arg402Gln) 1 | Missense | 3779 | 0.1765 | |||||||||
| OCA2(611409) | Albinism, oculocutaneous, type II (203200) | AR | 25578 (Mixed: White / African) [No] | c.619_636del, p.(Leu207_Leu212del) | Deletion | Het | 372713 | 0.0008030 in African / African Americans | NA | NA | 4 | PP5; PM2; PM4; PP3 |
| c.1327G>A, p.(Val443Ile) | Missense | Het | 955 | 0.003056 | Probably damaging | Deleterious | 4 | PS3; PM3; PP3; PP4; PP5; BS2 | ||||
| 25246 (Middle Eastern) [No] | c.1286T>C, p.(Leu429Pro) | Missense | Het | 627601 | Absent | Probably damaging | Deleterious | 4 | PM1; PM2; PP3; PP5; BP1 | |||
| c.1327G>A, p.(Val443Ile) | Missense | Het | 955 | 0.003056 | Probably damaging | Deleterious | 4 | PS3; PM3; PP3; PP4; PP5; BS2 | ||||
| 26947 (Mixed: White / African) [No] | c.2177_2181del, p.(Val726Glyfs*13) | Deletion | Het | 498226 | Absent | NA | NA | 5 | PVS1; PM2; PP3; PP5 | |||
| c.1255C>T, p.(Arg419Trp) | Missense | Het | 194160 | 0.0002659 | Probably damaging | Deleterious | 4 | PM2; PP3; PP5; PM3 | ||||
| 27321 (Black African) [No] | c.2228C>T, p.(Pro743Leu) | Missense | Het | 956 | 0.0001344 | Probably damaging | Deleterious | 5 | PP5; PM2; PP3; BP1 | |||
| c.1182+1G>A | Splice | Het | 436099 | 0.0000566 | Probably damaging | Deleterious | 5 | PVS1; PM2; PP3; PP5 | ||||
| HPS1(604982) | Hermansky- Pudlak syndrome 1 (203300) | AR | 26677 (South Asian) [No] | c.972dup, p.(Met325Hisfs*128) | Duplication | Hom | Absent | 0.000262 | NA | NA | 5 | PVS1; PM2; PP3; PP5 |
| HPS3(606118) | Hermansky- Pudlak syndrome 3 (614072) | AR | 26847 (South Asian) [Yes] | c.850del, p.(Arg284Glufs*57) | Deletion | Hom | 664198 | Absent | NA | NA | 5 | PVS1; PM2; PP3 |
| HPS6(607522) | Hermansky- Pudlak syndrome 6 (614075) | AR | 25888-1; 25888-2 (Mixed: White / African) [No] | c.1228_1252del, p.(Tyr410Valfs*9) | Deletion | Hom | Absent | Absent | NA | NA | 5 | PVS1; PM2; PP3 |
| GPR143(300808) | Ocular albinism, type I, Nettleship-Falls type (300500) | XL | 25806 (African) [No] | c.11C>G, p.(Pro4Arg) | Missense | Hemi | Absent | Absent | Probably damaging | Deleterious | 4 | PM2; PP2; PP3; PP4; PP5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, H.W.; Schiff, E.R.; Tailor, V.K.; Malka, S.; Neveu, M.M.; Theodorou, M.; Moosajee, M. Prospective Study of the Phenotypic and Mutational Spectrum of Ocular Albinism and Oculocutaneous Albinism. Genes 2021, 12, 508. https://doi.org/10.3390/genes12040508
Chan HW, Schiff ER, Tailor VK, Malka S, Neveu MM, Theodorou M, Moosajee M. Prospective Study of the Phenotypic and Mutational Spectrum of Ocular Albinism and Oculocutaneous Albinism. Genes. 2021; 12(4):508. https://doi.org/10.3390/genes12040508
Chicago/Turabian StyleChan, Hwei Wuen, Elena R. Schiff, Vijay K. Tailor, Samantha Malka, Magella M. Neveu, Maria Theodorou, and Mariya Moosajee. 2021. "Prospective Study of the Phenotypic and Mutational Spectrum of Ocular Albinism and Oculocutaneous Albinism" Genes 12, no. 4: 508. https://doi.org/10.3390/genes12040508







