Anti-Methicillin-Resistant Staphylococcus aureus Efficacy of Layer-by-Layer Silver Nanoparticle/Polyacrylic Acid-Coated Titanium Using an In-House Dip Coater
Abstract
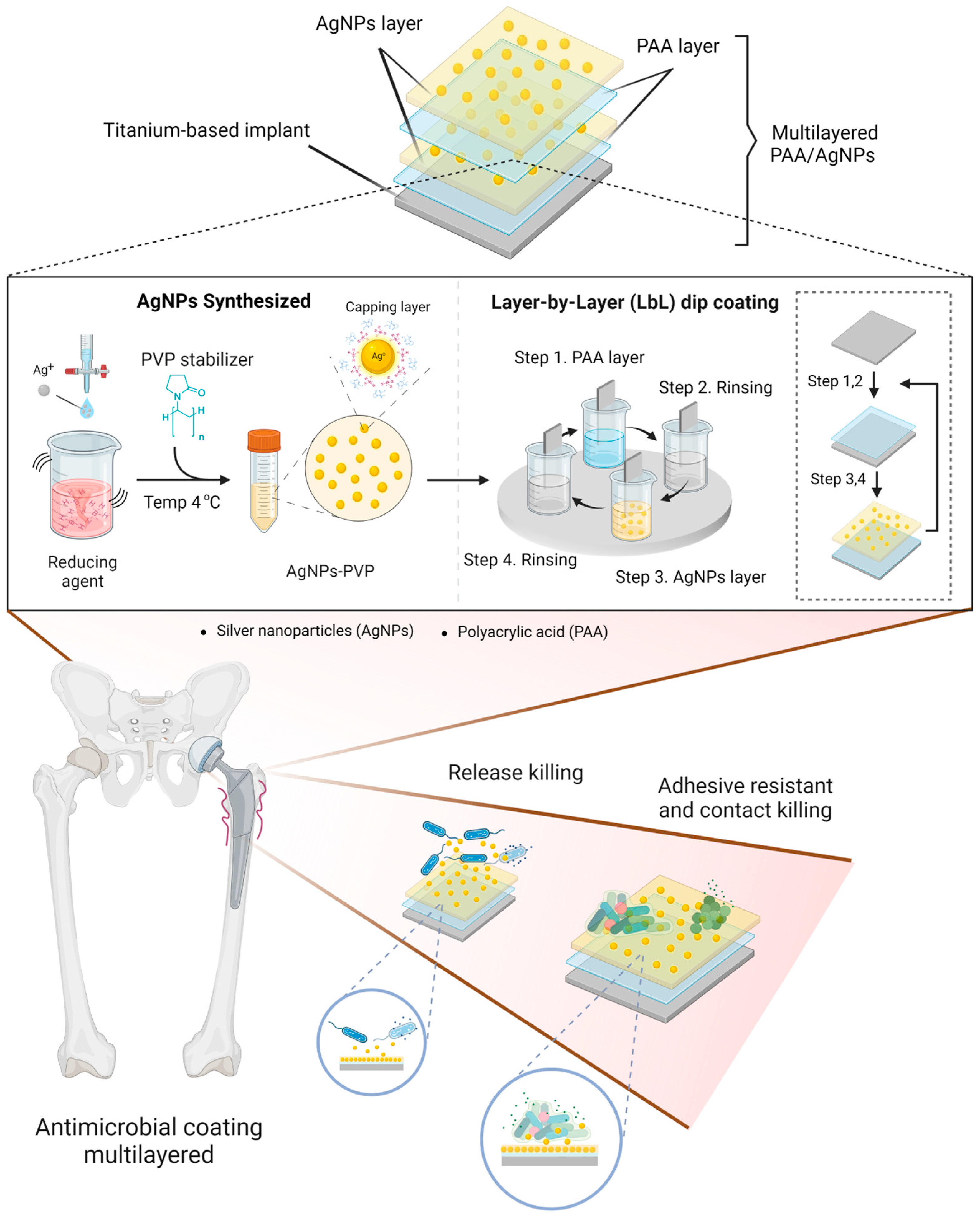
1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Synthesis of Silver Nanoparticles
2.3. Layer-by-Layer Dip Coating
2.4. Characterization of AgNP/PAA/Ti Plate Coating
2.5. Bacterial Culture
2.6. In Vitro Antimicrobial Assay
2.7. Antibiofilm Investigation
2.8. Cytotoxicity Testing
2.9. Statistical Analysis
3. Results and Discussion
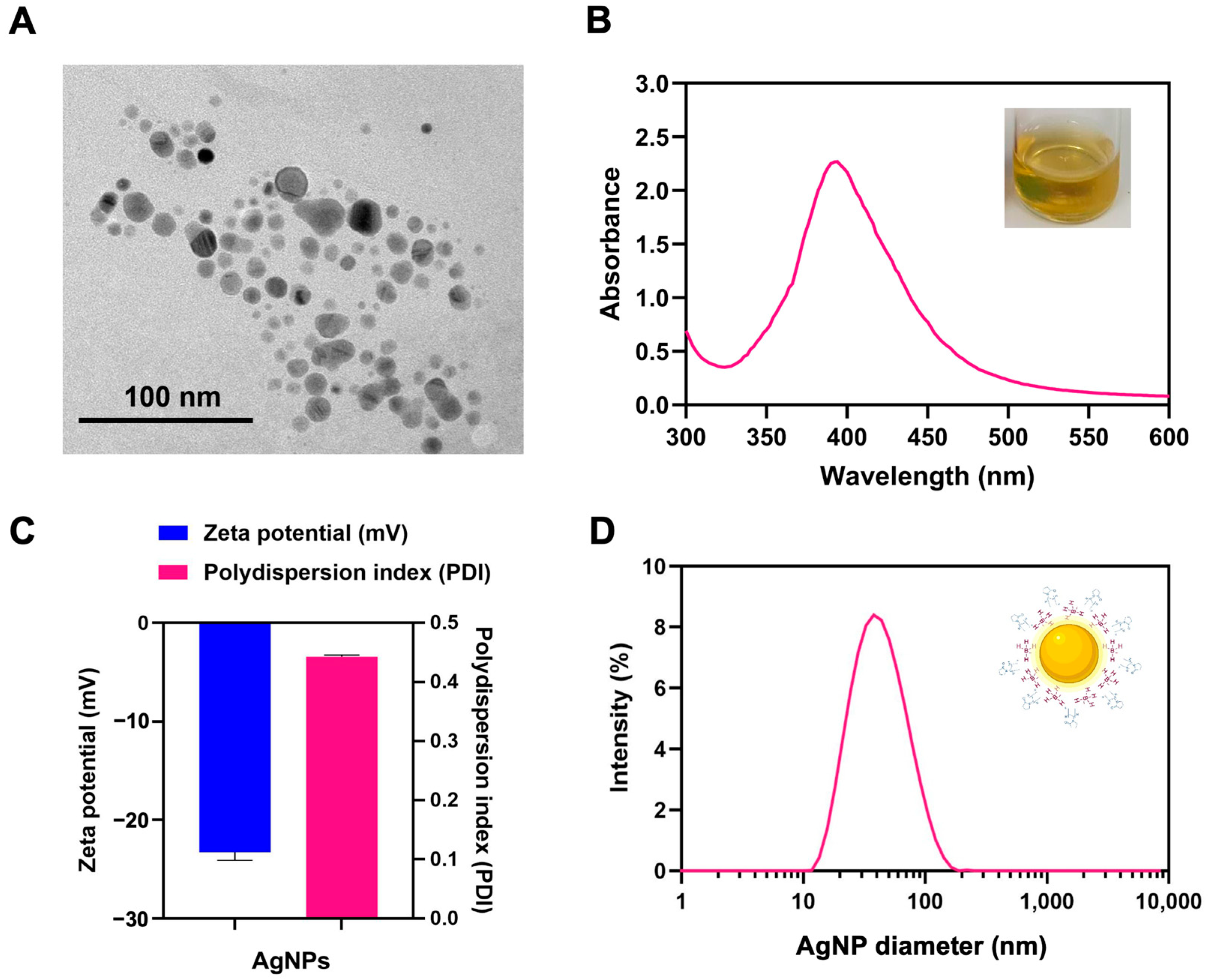
3.1. Characterization of Silver Nanoparticles
3.2. Coating Characterization
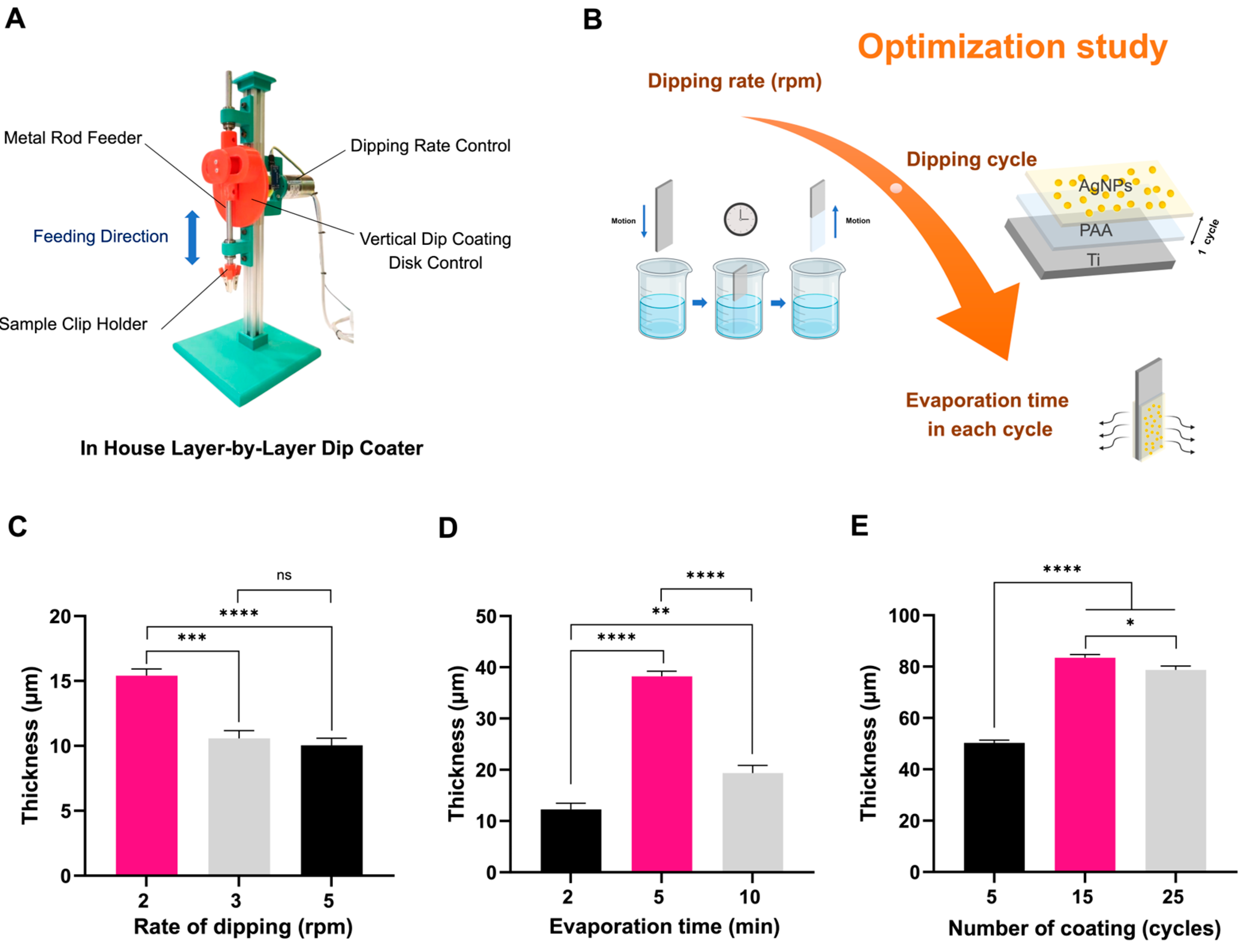
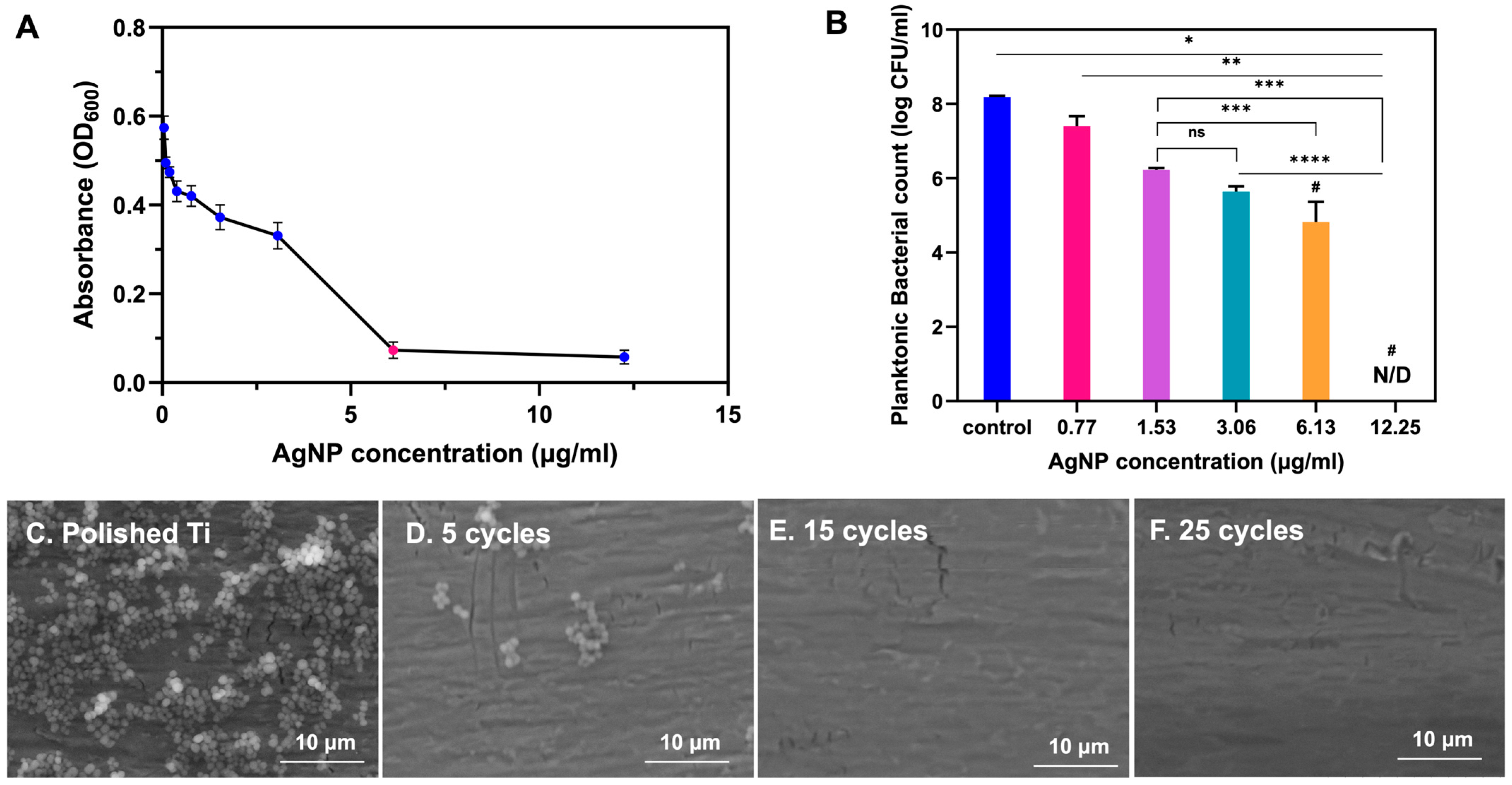
3.2.1. LBL-Based Coating Optimization
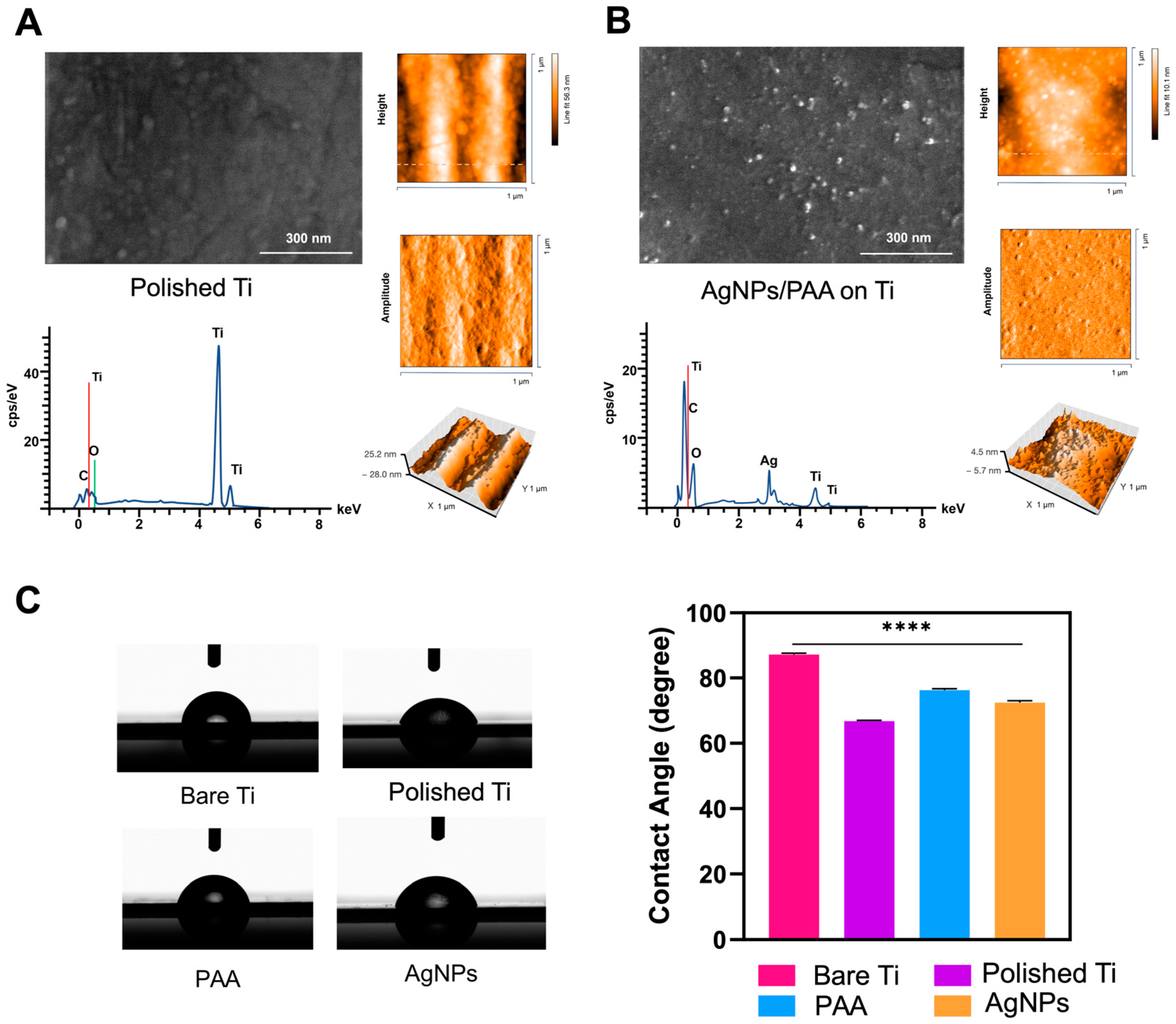
3.2.2. Surface Characterization
3.3. Antibacterial Performances
3.3.1. MIC and MBC Determination
3.3.2. Antibiofilm Performance
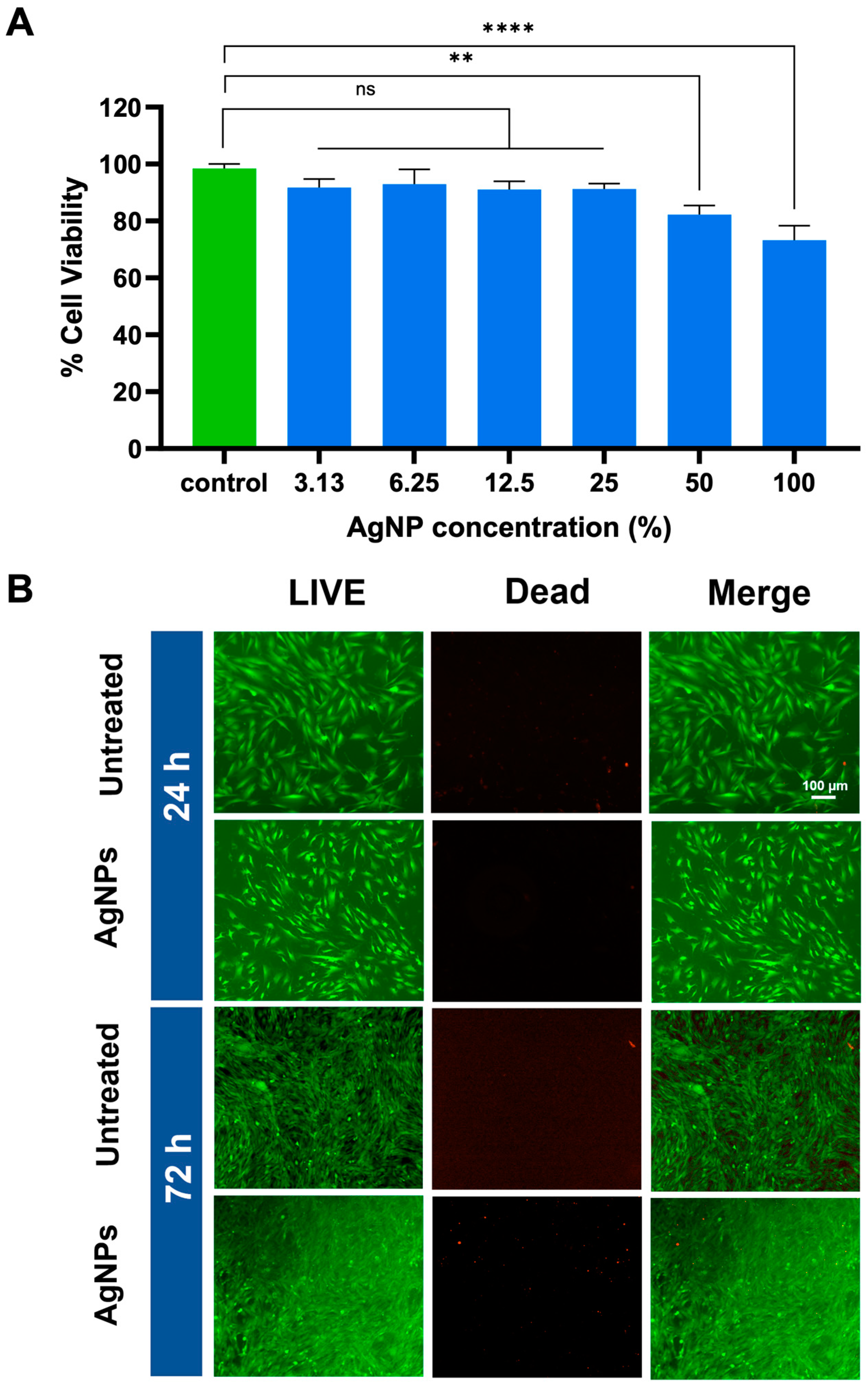
3.4. Biocompatibility Performance
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ciandrini, E.; Morroni, G.; Cirioni, O.; Kamysz, W.; Kamysz, E.; Brescini, L.; Baffone, W.; Campana, R. Synergistic Combinations of Antimicrobial Peptides Against Biofilms of Methicillin-Resistant Staphylococcus aureus (MRSA) on Polystyrene and Medical Devices. J. Glob. Antimicrob. Resist. 2020, 21, 203–210. [Google Scholar] [CrossRef]
- Xiang, Y.; Xuan, Y.-Y.; Li, G. Successful Treatment for Acute Prosthetic Joint Infection Due to MRSA and Candida albicans: A Case Report and Literature Review. Ther. Clin. Risk Manag. 2018, 14, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Agochukwu, N.; Boustany, A.; Rinker, B. Late Breast Implant Infections: A Delayed MRSA Infection from Hematogenous Spread in an Intravenous Drug User. Eur. J. Plast. Surg. 2018, 41, 351–354. [Google Scholar] [CrossRef]
- Schvartz, N.; Haidary, A.; Wakili, R.; Hecker, F.; Kupusovic, J.; Zsigmond, E.-J.; Miklos, M.; Saghy, L.; Szili-Torok, T.; Erath, J.W.; et al. Risk of Cardiac Implantable Electronic Device Infection after Early Versus Delayed Lead Repositioning. J. Cardiovasc. Dev. Dis. 2024, 11, 117. [Google Scholar] [CrossRef]
- Weinstein, R.A.; Darouiche, R.O. Device-Associated Infections: A Macroproblem That Starts with Microadherence. Clin. Infect. Dis. 2001, 33, 1567–1572. [Google Scholar] [CrossRef]
- Parvizi, J.; Azzam, K.; Ghanem, E.; Austin, M.S.; Rothman, R.H. Periprosthetic Infection Due to Resistant Staphylococci: Serious Problems on the Horizon. Clin. Orthop. Relat. Res. 2009, 467, 1732–1739. [Google Scholar] [CrossRef]
- Reina, N.; Delaunay, C.; Chiron, P.; Ramdane, N.; Hamadouche, M. Infection as a Cause of Primary Total Hip Arthroplasty Revision and Its Predictive Factors. Orthop. Traumatol. Surg. Res. 2013, 99, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Webster, T.J. Bacteria Antibiotic Resistance: New Challenges and Opportunities for Implant-Associated Orthopedic Infections. J. Orthop. Res. 2018, 36, 22–32. [Google Scholar] [CrossRef]
- Sahoo, J.; Sarkhel, S.; Mukherjee, N.; Jaiswal, A. Nanomaterial-Based Antimicrobial Coating for Biomedical Implants: New Age Solution for Biofilm-Associated Infections. ACS Omega 2022, 7, 45962–45980. [Google Scholar] [CrossRef]
- Knetsch, M.L.W.; Koole, L.H. New Strategies in the Development of Antimicrobial Coatings: The Example of Increasing Usage of Silver and Silver Nanoparticles. Polymers 2011, 3, 340–366. [Google Scholar] [CrossRef]
- Vijayakumar, S.; Vinoj, G.; Malaikozhundan, B.; Shanthi, S.; Vaseeharan, B. Plectranthus Amboinicus Leaf Extract Mediated Synthesis of Zinc Oxide Nanoparticles and Its Control of Methicillin Resistant Staphylococcus aureus Biofilm and Blood Sucking Mosquito Larvae. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2015, 137, 886–891. [Google Scholar] [CrossRef] [PubMed]
- Ayala-Núñez, N.V.; Lara Villegas, H.H.; Del Carmen Ixtepan Turrent, L.; Rodríguez Padilla, C. Silver Nanoparticles Toxicity and Bactericidal Effect Against Methicillin-Resistant Staphylococcus aureus: Nanoscale Does Matter. Nanobiotechnol 2009, 5, 2–9. [Google Scholar] [CrossRef]
- Chang, T.Y.; Chen, C.C.; Cheng, K.M.; Chin, C.Y.; Chen, Y.H.; Chen, X.A.; Sun, J.R.; Young, J.J.; Chiueh, T.S. Trimethyl Chitosan-Capped Silver Nanoparticles with Positive Surface Charge: Their Catalytic Activity and Antibacterial Spectrum Including Multidrug-Resistant Strains of Acinetobacter baumannii. Colloids Surf. B Biointerfaces 2017, 155, 61–70. [Google Scholar] [CrossRef]
- Yin, I.X.; Zhang, J.; Zhao, I.S.; Mei, M.L.; Li, Q.; Chu, C.H. The Antibacterial Mechanism of Silver Nanoparticles and Its Application in Dentistry. Int. J. Nanomed. 2020, 15, 2555–2562. [Google Scholar] [CrossRef]
- Lok, C.-N.; Ho, C.-M.; Chen, R.; He, Q.-Y.; Yu, W.-Y.; Sun, H.; Tam, P.K.-H.; Chiu, J.-F.; Che, C.-M. Proteomic Analysis of the Mode of Antibacterial Action of Silver Nanoparticles. J. Proteome Res. 2006, 5, 916–924. [Google Scholar] [CrossRef] [PubMed]
- Milić, M.; Leitinger, G.; Pavičić, I.; Zebić Avdičević, M.; Dobrović, S.; Goessler, W.; Vinković Vrček, I. Cellular Uptake and Toxicity Effects of Silver Nanoparticles in Mammalian Kidney Cells. J. Appl. Toxicol. 2015, 35, 581–592. [Google Scholar] [CrossRef]
- Hussain, S.M.; Hess, K.L.; Gearhart, J.M.; Geiss, K.T.; Schlager, J.J. In Vitro Toxicity of Nanoparticles in BRL 3A Rat Liver Cells. Toxicol. In Vitro 2005, 19, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Somogyi Škoc, M.; Meštrović, E.; Mouthuy, P.-A.; Rezić, I. Synthesis, Characterization and Application of Advanced Antimicrobial Electrospun Polymers. Polymers 2024, 16, 2443. [Google Scholar] [CrossRef]
- Lee, W.-F.; Wang, L.-Y.; Renn, T.-Y.; Yang, J.-C.; Fang, L.-S.; Lee, Y.-H.; Peng, P.-W. Characterization and Antibacterial Properties of Polyetherketoneketone Coated with a Silver Nanoparticle-in-Epoxy Lining. Polymers 2022, 14, 2906. [Google Scholar] [CrossRef] [PubMed]
- Illanes Tormena, R.P.; Medeiros Salviano Santos, M.-K.; Oliveira Da Silva, A.; Félix, F.M.; Chaker, J.A.; Freire, D.O.; Rodrigues Da Silva, I.C.; Moya, S.E.; Sousa, M.H. Enhancing the Antimicrobial Activity of Silver Nanoparticles Against Pathogenic Bacteria by Using Pelargonium sidoides DC Extract in Microwave Assisted Green Synthesis. RSC Adv. 2024, 14, 22035–22043. [Google Scholar] [CrossRef]
- Dai, Z.; Li, Y.; Yan, Y.; Wan, R.; Ran, Q.; Lu, W.; Qiao, B.; Li, H. Evaluation of the Internal Fixation Effect of Nano-Calcium-Deficient Hydroxyapatite/Poly-Amino Acid Composite Screws for Intraarticular Fractures in Rabbits. Int. J. Nanomed. 2018, 13, 6625–6636. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, C.M.; Niederauer, G.G.; Athanasiou, K.A. Fabrication and Characterization of PLA-PGA Orthopedic Implants. Tissue Eng. 1995, 1, 241–252. [Google Scholar] [CrossRef]
- Wozniak, A.; Humblot, V.; Vayron, R.; Delille, R.; Falentin-Daudré, C. Simple UV-Grafting of PolyAcrylic and PolyMethacrylic Acid on Silicone Breast Implant Surfaces: Chemical and Mechanical Characterizations. Coatings 2023, 13, 1888. [Google Scholar] [CrossRef]
- Athanasiou, K. Sterilization, Toxicity, Biocompatibility and Clinical Applications of Polylactic Acid/Polyglycolic Acid Copolymers. Biomaterials 1996, 17, 93–102. [Google Scholar] [CrossRef]
- Xi, W.; Hegde, V.; Zoller, S.D.; Park, H.Y.; Hart, C.M.; Kondo, T.; Hamad, C.D.; Hu, Y.; Loftin, A.H.; Johansen, D.O.; et al. Point-of-Care Antimicrobial Coating Protects Orthopaedic Implants from Bacterial Challenge. Nat. Commun. 2021, 12, 5473. [Google Scholar] [CrossRef] [PubMed]
- Meti, R.S.; Neelagund, S.E.; Urs, D.; Dharmappa, K.K.; Kotresh, K.R. Green Synthesis of Silver Nanoparticles from Acacia sinuata Seed Extract and Evaluation of Their Mosquitocidal and Anticancer (Caco-2 and MG-63 Cell) Activity. Biomass Convers. Biorefin. 2025, 15, 175–184. [Google Scholar] [CrossRef]
- Salwiczek, M.; Qu, Y.; Gardiner, J.; Strugnell, R.A.; Lithgow, T.; McLean, K.M.; Thissen, H. Emerging Rules for Effective Antimicrobial Coatings. Trends Biotechnol. 2014, 32, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Kargupta, R.; Bok, S.; Darr, C.M.; Crist, B.D.; Gangopadhyay, K.; Gangopadhyay, S.; Sengupta, S. Coatings and Surface Modifications Imparting Antimicrobial Activity to Orthopedic Implants. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2014, 6, 475–495. [Google Scholar] [CrossRef]
- Iarikov, D.D.; Kargar, M.; Sahari, A.; Russel, L.; Gause, K.T.; Behkam, B.; Ducker, W.A. Antimicrobial Surfaces Using Covalently Bound Polyallylamine. Biomacromolecules 2014, 15, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Hiflan, F.S.; Abeygoonawardena, H.; Karawgoda, R.A.; Chandrasiri, N.S.; Balasuriya, A.; Senanayake, N.P. Comparison of Broth Microdilution and E-Test for Susceptibility of MRSA to Vancomycin. Sri Lankan J. Infect. Dis. 2024, 14, 1–6. [Google Scholar] [CrossRef]
- Moise, P.A.; Sakoulas, G.; Forrest, A.; Schentag, J.J. Vancomycin In Vitro Bactericidal Activity and Its Relationship to Efficacy in Clearance of Methicillin-Resistant Staphylococcus aureus Bacteremia. Antimicrob. Agents Chemother. 2007, 51, 2582–2586. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zain Alaabedin, A.A.; Abdul Majeed, A.M.; Hamza, B.H. Green Synthesis of Silver Nanoparticles and Their Effect on the Skin Determined Using IR Thermography. Kuwait J. Sci. 2024, 51, 100076. [Google Scholar] [CrossRef]
- Wulandari, P.; Nagahiro, T.; Fukada, N.; Kimura, Y.; Niwano, M.; Tamada, K. Characterization of Citrates on Gold and Silver Nanoparticles. J. Colloid Interface Sci. 2015, 438, 244–248. [Google Scholar] [CrossRef]
- Gindri, I.M.; Siddiqui, D.A.; Frizzo, C.P.; Martins, M.A.P.; Rodrigues, D.C. Ionic Liquid Coatings for Titanium Surfaces: Effect of IL Structure on Coating Profile. ACS Appl. Mater. Interfaces 2015, 7, 27421–27431. [Google Scholar] [CrossRef]
- Qi, S.; Kiratzis, I.; Adoni, P.; Tuekprakhon, A.; Hill, H.J.; Stamataki, Z.; Nabi, A.; Waugh, D.; Rodriguez, J.R.; Clarke, S.M.; et al. Porous Cellulose Thin Films as Sustainable and Effective Antimicrobial Surface Coatings. ACS Appl. Mater. Interfaces 2023, 15, 20638–20648. [Google Scholar] [CrossRef] [PubMed]
- Grosso, D. How to Exploit the Full Potential of the Dip-Coating Process to Better Control Film Formation. J. Mater. Chem. 2011, 21, 17033. [Google Scholar] [CrossRef]
- Alissawi, N.; Peter, T.; Strunskus, T.; Ebbert, C.; Grundmeier, G.; Faupel, F. Plasma-Polymerized HMDSO Coatings to Adjust the Silver Ion Release Properties of Ag/Polymer Nanocomposites. J. Nanopart. Res. 2013, 15, 2080. [Google Scholar] [CrossRef]
- Iqbal, T.; Ejaz, A.; Abrar, M.; Afsheen, S.; Batool, S.S.; Fahad, M.; Tahir, M.B. Qualitative and Quantitative Analysis of Nanoparticles Using Laser-Induced Breakdown Spectroscopy (LIBS) and Energy Dispersive X-Ray Spectroscopy (EDS). Laser Phys. 2019, 29, 116001. [Google Scholar] [CrossRef]
- Zulfiqar; Afzal, S.; Khan, R.; Zeb, T.; ur Rahman, M.; Burhanullah; Ali, S.; Khan, G.; ur Rahman, Z.; Hussain, A. Structural, Optical, Dielectric and Magnetic Properties of PVP Coated Magnetite (Fe3O4) Nanoparticles. J. Mater. Sci. Mater. Electron. 2018, 29, 20040–20050. [Google Scholar] [CrossRef]
- El Hadad, A.A.; Barranco, V.; Jiménez-Morales, A.; Peón, E.; Hickman, G.J.; Perry, C.C.; Galván, J.C. Enhancing In Vitro Biocompatibility and Corrosion Protection of Organic–Inorganic Hybrid Sol–Gel Films with Nanocrystalline Hydroxyapatite. J. Mater. Chem. B 2014, 2, 3886–3896. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.I.; Kwak, H.J.; Park, C.; Choi, C.; Sapkal, N.P.; Hong, J.; Kim, M.H. Wetting Criteria of Intrinsic Contact Angle To Distinguish Between Hydrophilic and Hydrophobic Micro-/Nanotextured Surfaces: Experimental and Theoretical Analysis with Synchrotron X-Ray Imaging. Langmuir 2019, 35, 3607–3614. [Google Scholar] [CrossRef] [PubMed]
- Lorenzetti, M.; Dogša, I.; Stošicki, T.; Stopar, D.; Kalin, M.; Kobe, S.; Novak, S. The Influence of Surface Modification on Bacterial Adhesion to Titanium-Based Substrates. ACS Appl. Mater. Interfaces 2015, 7, 1644–1651. [Google Scholar] [CrossRef]
- Chan, Y.W.; Siow, K.S.; Ng, P.Y.; Gires, U.; Yeop Majlis, B. Plasma Polymerized Carvone as an Antibacterial and Biocompatible Coating. Mater. Sci. Eng. C 2016, 68, 861–871. [Google Scholar] [CrossRef]
- Siritongsuk, P.; Hongsing, N.; Thammawithan, S.; Daduang, S.; Klaynongsruang, S.; Tuanyok, A.; Patramanon, R. Two-Phase Bactericidal Mechanism of Silver Nanoparticles Against Burkholderia pseudomallei. PLoS ONE 2016, 11, e0168098. [Google Scholar] [CrossRef] [PubMed]
- Ishihama, H.; Ishii, K.; Nagai, S.; Kakinuma, H.; Sasaki, A.; Yoshioka, K.; Kuramoto, T.; Shiono, Y.; Funao, H.; Isogai, N.; et al. An Antibacterial Coated Polymer Prevents Biofilm Formation and Implant-Associated Infection. Sci. Rep. 2021, 11, 3602. [Google Scholar] [CrossRef]
- Li, P.; Yin, R.; Cheng, J.; Lin, J. Bacterial Biofilm Formation on Biomaterials and Approaches to Its Treatment and Prevention. Int. J. Mol. Sci. 2023, 24, 11680. [Google Scholar] [CrossRef] [PubMed]
- Roh, J.; Umh, H.N.; Sim, J.; Park, S.; Yi, J.; Kim, Y. Dispersion Stability of Citrate- and PVP-AgNPs in Biological Media for Cytotoxicity Test. Korean J. Chem. Eng. 2013, 30, 671–674. [Google Scholar] [CrossRef]
- Neto, F.N.S.; Morais, L.A.; Gorup, L.F.; Ribeiro, L.S.; Martins, T.J.; Hosida, T.Y.; Francatto, P.; Barbosa, D.B.; Camargo, E.R.; Delbem, A.C.B. Facile Synthesis of PVP-Coated Silver Nanoparticles and Evaluation of Their Physicochemical, Antimicrobial and Toxic Activity. Colloids Interfaces 2023, 7, 66. [Google Scholar] [CrossRef]
- Bondarenko, O.; Ivask, A.; Käkinen, A.; Kurvet, I.; Kahru, A. Particle-Cell Contact Enhances Antibacterial Activity of Silver Nanoparticles. PLoS ONE 2013, 8, e64060. [Google Scholar] [CrossRef] [PubMed]
- Käosaar, S.; Kahru, A.; Mantecca, P.; Kasemets, K. Profiling of the Toxicity Mechanisms of Coated and Uncoated Silver Nanoparticles to Yeast Saccharomyces cerevisiae BY4741 Using a Set of Its 9 Single-Gene Deletion Mutants Defective in Oxidative Stress Response, Cell Wall or Membrane Integrity and Endocytosis. Toxicol. In Vitro 2016, 35, 149–162. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puttawong, J.; Yingkajorn, M.; Khongkow, P.; Thamphiwatana, S.D.; Phairatana, T. Anti-Methicillin-Resistant Staphylococcus aureus Efficacy of Layer-by-Layer Silver Nanoparticle/Polyacrylic Acid-Coated Titanium Using an In-House Dip Coater. Polymers 2025, 17, 333. https://doi.org/10.3390/polym17030333
Puttawong J, Yingkajorn M, Khongkow P, Thamphiwatana SD, Phairatana T. Anti-Methicillin-Resistant Staphylococcus aureus Efficacy of Layer-by-Layer Silver Nanoparticle/Polyacrylic Acid-Coated Titanium Using an In-House Dip Coater. Polymers. 2025; 17(3):333. https://doi.org/10.3390/polym17030333
Chicago/Turabian StylePuttawong, Julinthip, Mingkwan Yingkajorn, Pasarat Khongkow, Soracha D. Thamphiwatana, and Tonghathai Phairatana. 2025. "Anti-Methicillin-Resistant Staphylococcus aureus Efficacy of Layer-by-Layer Silver Nanoparticle/Polyacrylic Acid-Coated Titanium Using an In-House Dip Coater" Polymers 17, no. 3: 333. https://doi.org/10.3390/polym17030333
APA StylePuttawong, J., Yingkajorn, M., Khongkow, P., Thamphiwatana, S. D., & Phairatana, T. (2025). Anti-Methicillin-Resistant Staphylococcus aureus Efficacy of Layer-by-Layer Silver Nanoparticle/Polyacrylic Acid-Coated Titanium Using an In-House Dip Coater. Polymers, 17(3), 333. https://doi.org/10.3390/polym17030333





