Mechanical Behavior of Alkasite Posterior Restorations in Comparison to Polymeric Materials: A 3D-FEA Study
Abstract
1. Introduction
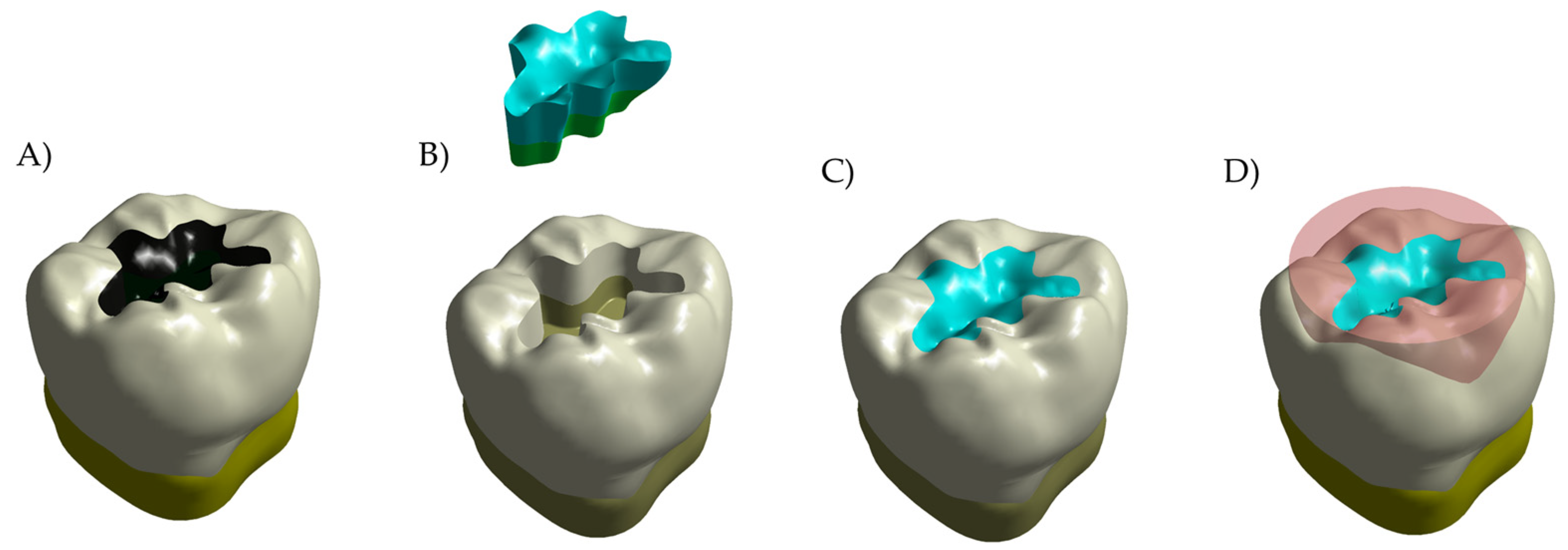
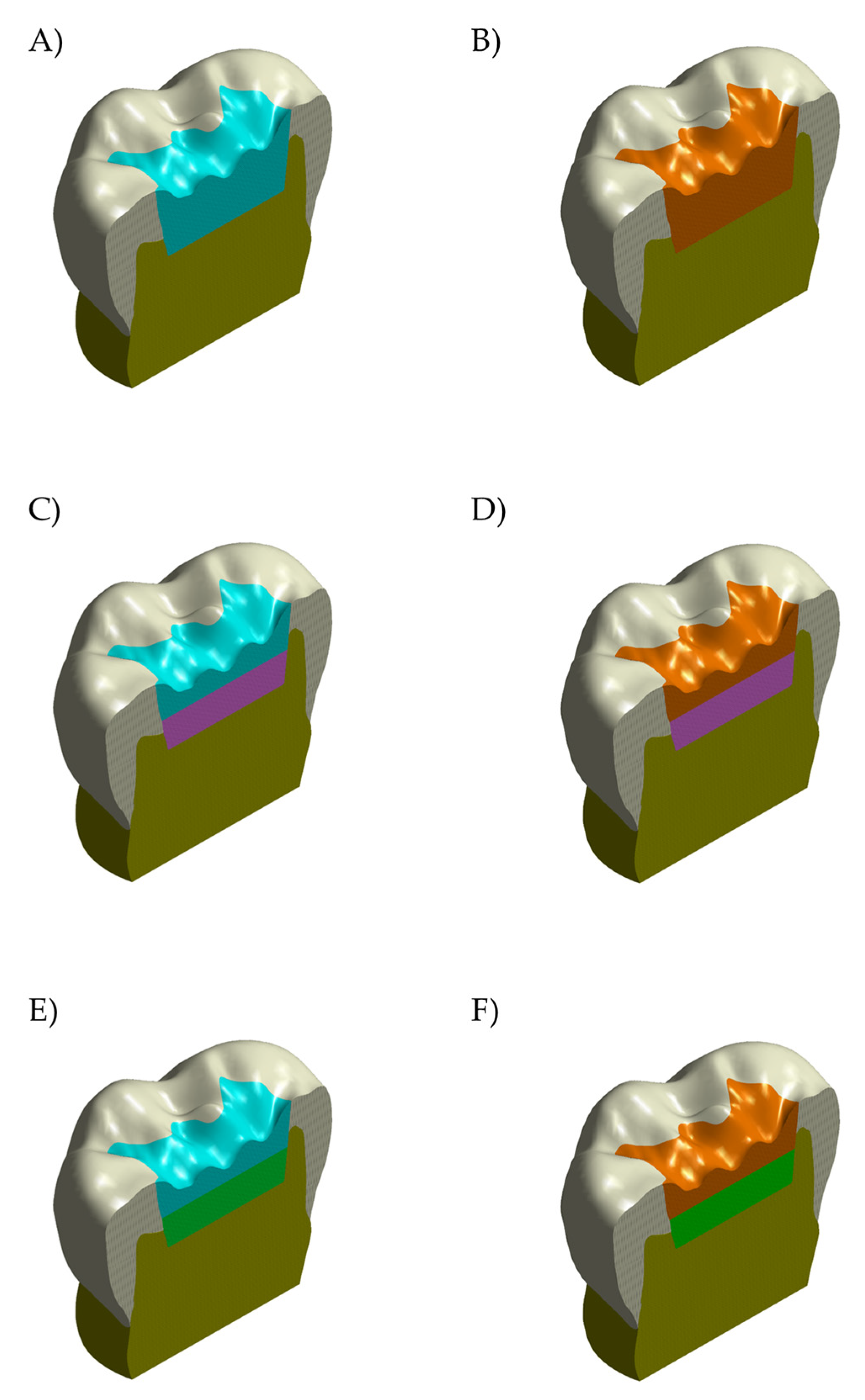
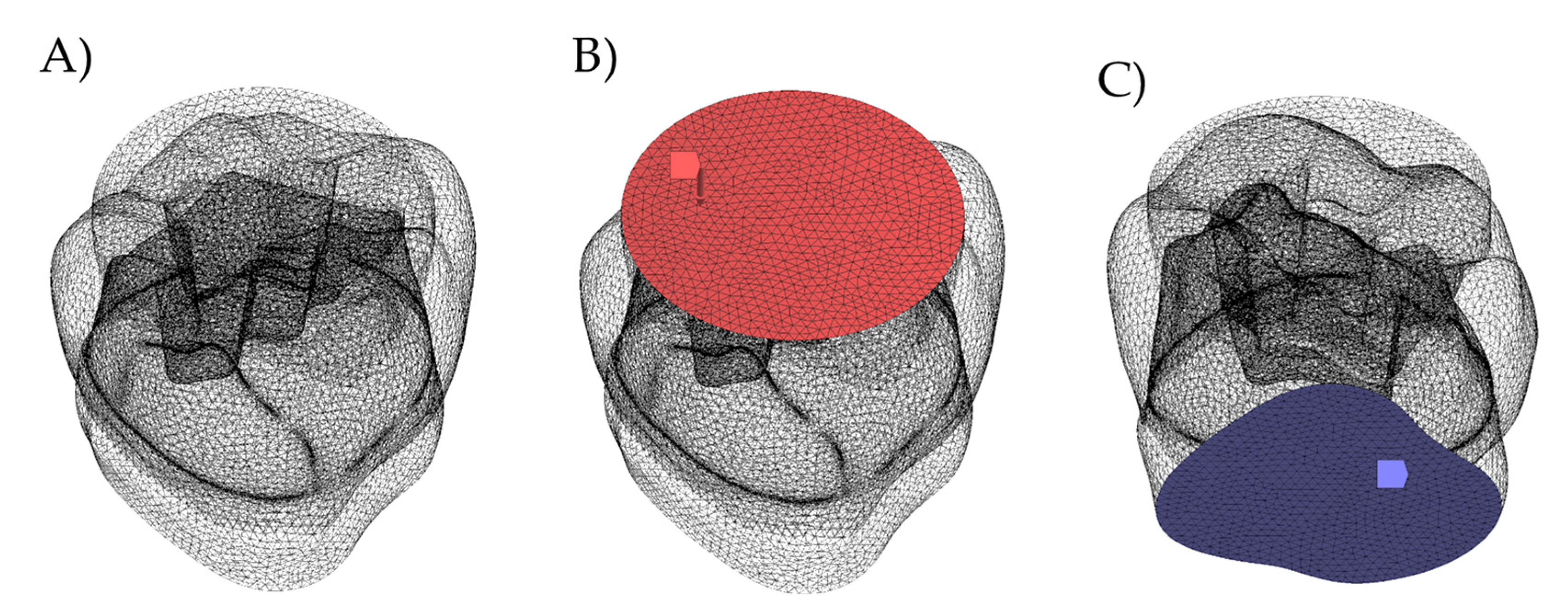
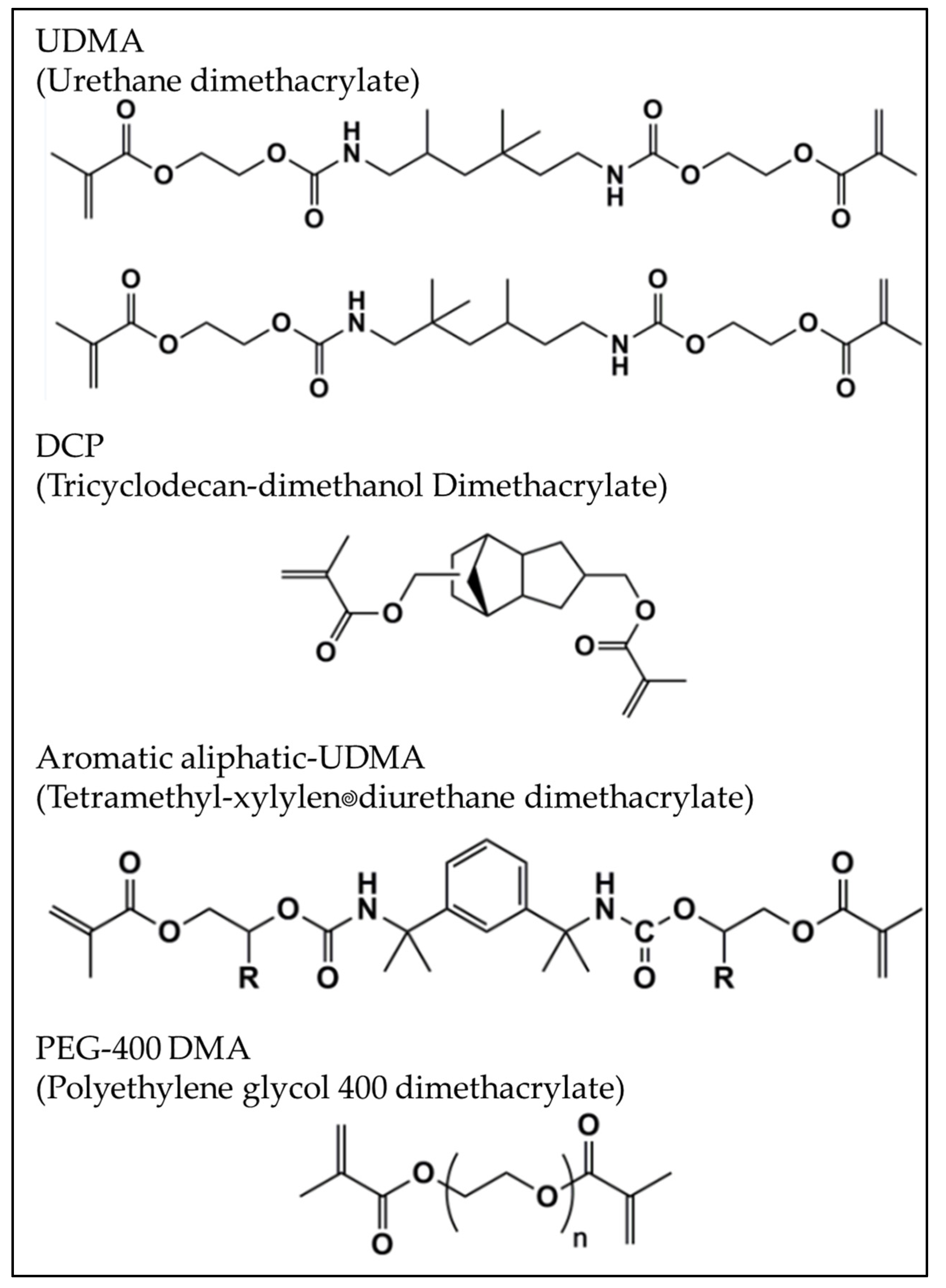
2. Materials and Methods
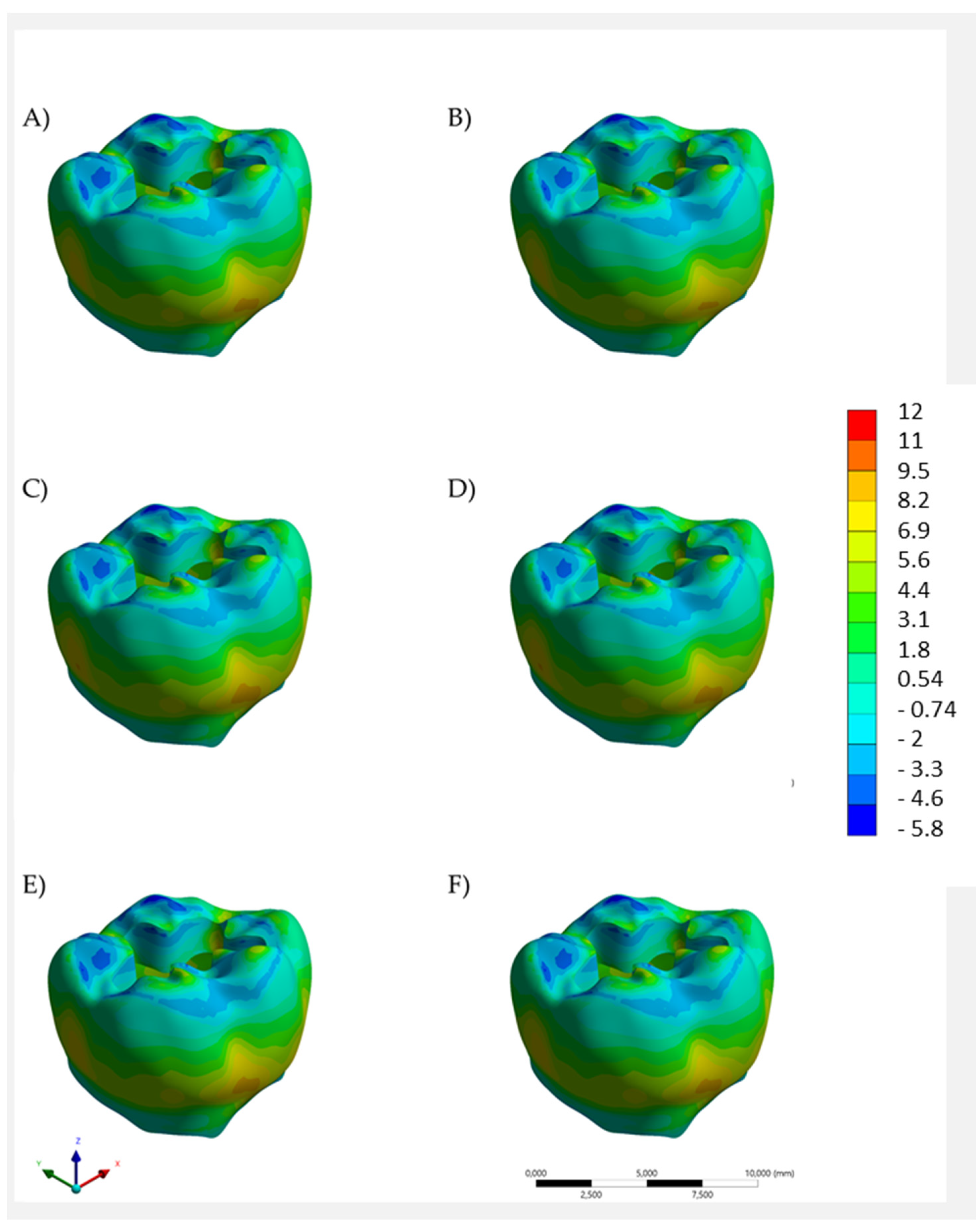
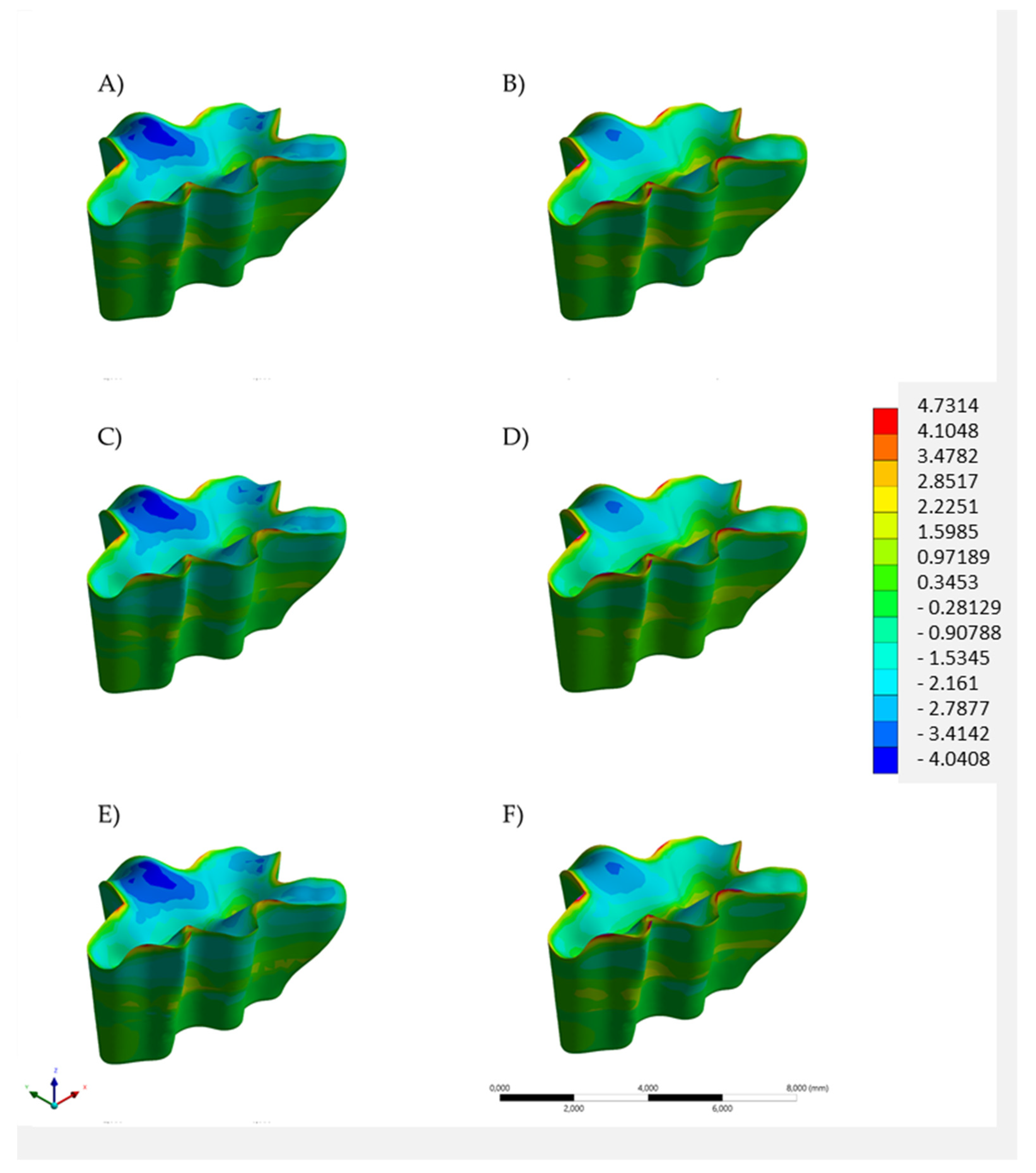
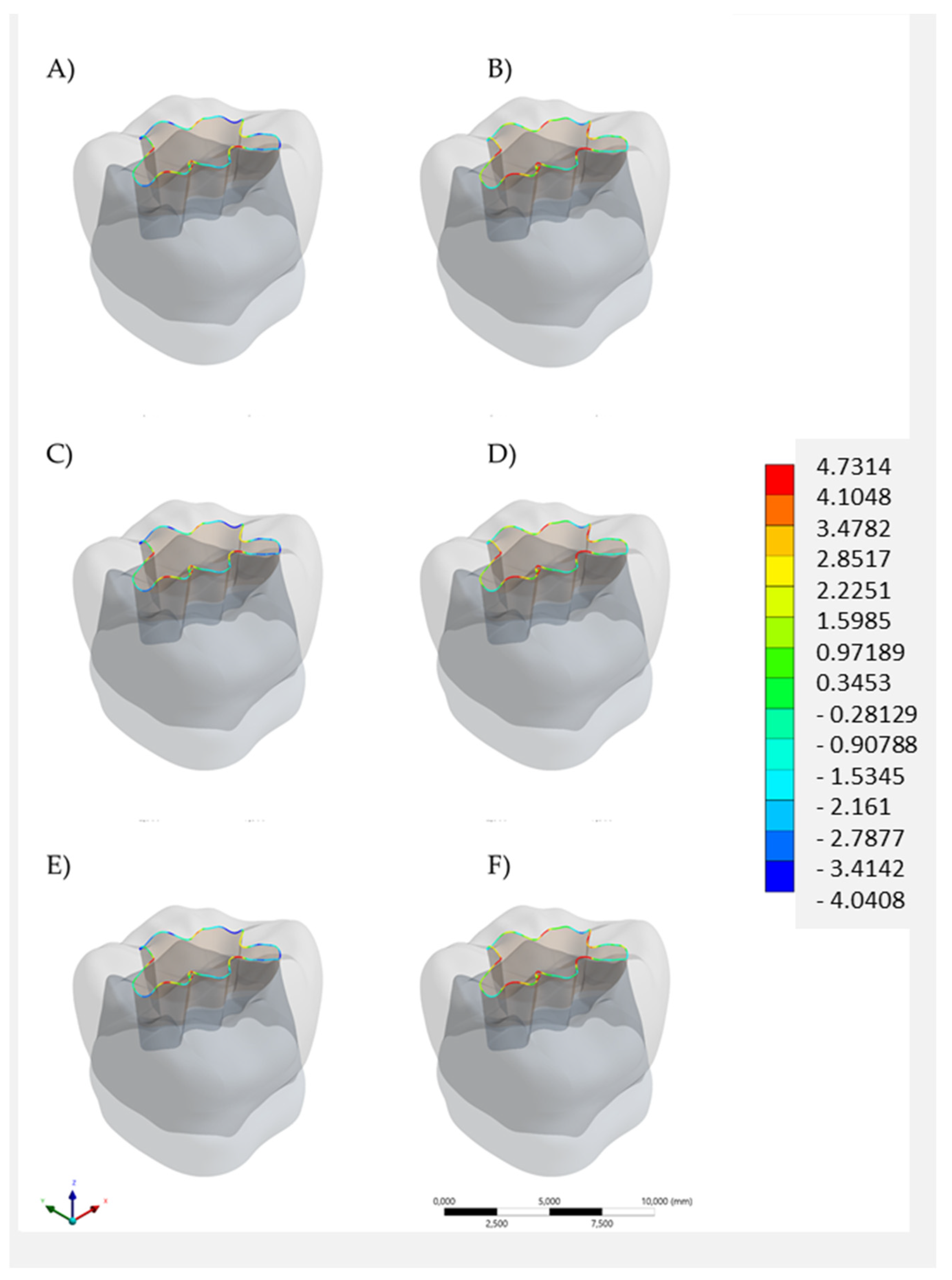
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yadav, R.; Kumar, M. Dental restorative composite materials: A review. J. Oral Biosci. 2019, 61, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Piva, A.D.; Borges, A.; Lanzotti, A.; Zamparini, F.; Epifania, E.; Tribst, J.M. Effect of Shrinking and No Shrinking Dentine and Enamel Replacing Materials in Posterior Restoration: A 3D-FEA Study. Appl. Sci. 2021, 11, 2215. [Google Scholar] [CrossRef]
- Borgia, E.; Baron, R.; Borgia, J.L. Quality and Survival of Direct Light-Activated Composite Resin Restorations in Poste-Rior Teeth: A 5- to 20-Year Retrospective Longitudinal Study. J. Prosthodont. 2019, 28, e195–e203. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Cassese, A.; Miele, C.; Beguinot, F.; Garcia-Godoy, F.; Di Jeso, B.; Ulianich, L. Cytotoxicity of Dental Resin Composites: An in Vitro Evaluation. J. Appl. Toxicol. 2013, 33, 451–457. [Google Scholar] [CrossRef]
- Treglia, A.S.; Turco, S.; Ulianich, L.; Ausiello, P.; Lofrumento, D.D.; Nicolardi, G.; Miele, C.; Garbi, C.; Beguinot, F.; Di Jeso, B. Cell Fate Following ER Stress: Just a Matter of Quo Ante Recovery or Death? Histol. Histol. Histopathol. 2012, 27, 1–12. [Google Scholar] [PubMed]
- Rosatto, C.M.; Bicalho, A.A.; Veríssimo, C.; Bragança, G.F.; Rodrigues, M.P.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Mechanical Properties, Shrinkage Stress, Cuspal Strain and Fracture Resistance of Molars Restored with Bulk-Fill Compo-Sites and Incremental Filling Technique. J. Dent. 2015, 43, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Van Ende, A.; De Munck, J.; Van Landuyt, K.; Van Meerbeek, B. Effect of Bulk-filling on the Bonding Efficacy in Occlusal Class I Cavities. J. Adhes. Dent. 2016, 18, 119–124. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Apicella, A.; Di Palma, L.; Aversa, R.; Ausiello, P. DSC Kinetic Characterization of Dental Composites Using Different Light Sources. J. Adv. Mater. 2002, 34, 22–25. [Google Scholar]
- Ausiello, P.; Ciaramella, S.; Di Rienzo, A.; Lanzotti, A.; Ventre, M.; Watts, D.C. Adhesive class I restorations in sound molar teeth incorporating combined resin-composite and glass ionomer materials: CAD-FE modeling and analysis. Dent. Mater. 2019, 35, 1514–1522. [Google Scholar] [CrossRef]
- Das, A.; Mazumdar, P.; Das, U.K. Comparative evaluation of microleakage of three different direct restorative materials (Silver Amalgam, Glass Ionomer Cement, Cention N), in Class II restorations using stereomicroscope: An In vitro Study. Indian J. Dent. Res. 2019, 30, 277–281. [Google Scholar] [CrossRef]
- Samanta, S.; Das, U.K.; Mitra, A. Comparison of Microleakage in Class V Cavity Restored with Flowable Composite Resin, Glass Ionomer Cement and Centionn. Imp. J. Interdiscip. Res. 2017, 3, 180–183. [Google Scholar]
- Sharma, A.; Babaji, P.; Sujith, R.; Yadav, T.G.; Pitalia, D.; Apoorva, K. Comparative Evaluation of Mechanical and Microleakage Properties of Cention-N, Composite, and Glass Ionomer Cement Restorative Materials. J. Contemp. Dent. Pract. 2020, 21, 691–695. [Google Scholar] [CrossRef]
- Sridhar, N.; Balagopal, S.; Kaur, K. An In Vitro Evaluation of the Mechanical Properties and Fluoride-releasing Ability of a New Self-cure Filling Material. J. Contemp. Dent. Pract. 2021, 22, 134–139. [Google Scholar] [CrossRef]
- Naz, F.; Khan, A.S.; Kader, M.A.; Al Gelban, L.O.S.; Mousa, N.M.A.; Asiri, R.S.H.; Hakeem, A.S. Comparative evaluation of mechanical and physical properties of a new bulk-fill Alkasite with conventional restorative materials. Saudi Dent. J. 2021, 33, 666–673. [Google Scholar] [CrossRef] [PubMed]
- François, P.; Remadi, A.; Le Goff, S.; Abdel-Gawad, S.; Attal, J.-P.; Dursun, E. Flexural properties and dentin adhesion in recently developed self-adhesive bulk-fill materials. J. Oral Sci. 2021, 63, 139–144. [Google Scholar] [CrossRef]
- Tiskaya, M.; Al-Eesa, N.; Wong, F.; Hill, R. Characterization of the bioactivity of two commercial composites. Dent. Mater. 2019, 35, 1757–1768. [Google Scholar] [CrossRef]
- Naik, N.; Pai, S.; Bhat, V.; Patil, V.; Awasthi, S.; Nayak, N. Numerical three-dimensional finite element modeling of cavity shape and optimal material selection by analysis of stress distribution on class V cavities of mandibular premolars. J. Int. Soc. Prev. Community Dent. 2020, 10, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Pai, S.; Naik, N.; Patil, V.; Kaur, J.; Awasti, S.; Nayak, N. Evaluation and Comparison of Stress Distribution in Restored Cervical Lesions of Mandibular Premolars: Three-dimensional Finite Element Analysis. J. Int. Soc. Prev. Community Dent. 2019, 9, 605–611. [Google Scholar] [CrossRef]
- Penteado, M.M.; Tribst, J.P.M.; Dal Piva, A.M.; Ausiello, P.; Zarone, F.; Garcia-Godoy, F.; Borges, A.L. Mechanical behavior of conceptual posterior dental crowns with functional elasticity gradient. Am. J. Dent. 2019, 32, 165–168. [Google Scholar]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; Lo Giudice, R.; Borges, A.L.S.; Bottino, M.A.; Epifania, E.; Ausiello, P. The Influence of Custom-Milled Framework Design for an Implant-Supported Full-Arch Fixed Dental Prosthesis: 3D-FEA Study. Int. J. Environ. Res. Public Health 2020, 17, 4040. [Google Scholar] [CrossRef]
- Ausiello, P.P.; Ciaramella, S.; Lanzotti, A.; Ventre, M.; Borges, A.L.; Tribst, J.P.; Piva, A.D.; Garcia-Godoy, F. Mechanical behavior of Class I cavities restored by different material combinations under loading and polymerization shrinkage stress. A 3D-FEA study. Am. J. Dent. 2019, 32, 55–60. [Google Scholar] [PubMed]
- Ausiello, P.; Ciaramella, S.; De Benedictis, A.; Lanzotti, A.; Tribst, J.P.M.; Watts, D.C. The use of different adhesive filling material and mass combinations to restore class II cavities under loading and shrinkage effects: A 3D-FEA. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Cention N_Scientific Documentation_English_V01_23015.pdf. Download Center Ivoclar Vivadent. Available online: https://downloadcenter.ivoclar.com/ (accessed on 28 March 2022).
- Yao, C.; Ahmed, M.H.; Zhang, F.; Mercelis, B.; Van Landuyt, K.L.; Huang, C.; Van Meerbeek, B. Structural/Chemical Characterization and Bond Strength of a New Self-Adhesive Bulk-fill Restorative. J. Adhes. Dent. 2020, 22, 85–97. [Google Scholar] [CrossRef]
- de Araújo-Neto, V.G.; Sebold, M.; de Castro, E.F.; Feitosa, V.P.; Giannini, M. Evaluation of physico-mechanical properties and filler particles characterization of conventional, bulk-fill, and bioactive resin-based composites. J. Mech. Behav. Biomed. Mater. 2021, 115, 104288. [Google Scholar] [CrossRef] [PubMed]
- Chaharom, M.E.E.; Bahari, M.; Kahnamoui, M.A.; Kimyai, S.; Sattari, Z. Effect of curing method and thermocycling on flexural strength and microhardness of a new composite resin with alkaline filler. Dent. Res. J. 2021, 18, 96. [Google Scholar] [CrossRef]
- Mohammadi, N.; Kimyai, S.; Lahij, Y.G.; Bahari, M.; Ajami, A.A.; Kahnamouei, M.A.; Daneshpooy, M. Correction to: Comparison of the effect of bleaching with 15% carbamide peroxide and 35% hydrogen peroxide on flexural strength of Cention N in self-cured and dual-cured polymerization modes. J. Dent. Res. Dent. Clin. Dent. Prospect. 2020, 14, 262. [Google Scholar] [CrossRef] [PubMed]
- Dal Piva, A.M.d.O.; Tribst, J.P.M.; Borges, A.L.S.; de Assunção E Souza, R.O.; Bottino, M.A. CAD-FEA modeling and analysis of different full crown monolithic restorations. Dent. Mater. 2018, 34, 1342–1350. [Google Scholar] [CrossRef] [PubMed]
- Campaner, L.M.; Silveira, M.P.M.; de Andrade, G.S.; Borges, A.L.S.; Bottino, M.A.; de OliveiraDal Piva, A.M.; Lo Giudice, R.; Ausiello, P.; Tribst, J.P.M. Influence of polymeric restorative materials on the stress distribution in posterior fixed partial dentures: 3D finite element analysis. Polymers 2021, 13, 758. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, I.V.; Tribst, J.P.M.; Silva-Concilio, L.R.; Bottino, M.A. Effect of Different Ceramic Materials on Fatigue Resistance and Stress Distribution in Upper Canines with Palatal Veneers. Eur. J. Dent. 2022, 16, 225. [Google Scholar] [CrossRef] [PubMed]
- Donly, K.J.; Liu, J.A. Dentin and enamel demineralization inhibition at restoration margins of Vitremer, Z 100 and Cention N. Am. J. Dent. 2018, 31, 166–168. [Google Scholar] [PubMed]
- Dennis, D.; Pintauli, S.; Debora, S. Microleakage Comparative Evaluation of RMGIC and Alkasite with and without Adhesive System in Class V Cavity: An In Vitro Study. J. Contemp. Dent. Pract. 2021, 22, 735–738. [Google Scholar] [CrossRef] [PubMed]
- Correia, A.; Andrade, M.R.; Tribst, J.; Borges, A.; Caneppele, T. Influence of Bulk-fill Restoration on Polymerization Shrinkage Stress and Marginal Gap Formation in Class V Restorations. Oper. Dent. 2020, 45, E207–E216. [Google Scholar] [CrossRef] [PubMed]
- Kowalska, A.; Sokolowski, J.; Gozdek, T.; Krasowski, M.; Kopacz, K.; Bociong, K. The Influence of Various Photoinitiators on the Properties of Commercial Dental Composites. Polymers 2021, 13, 3972. [Google Scholar] [CrossRef] [PubMed]
- Theerarath, T.; Sriarj, W. An Alkasite restorative material effectively remineralized artificial interproximal enamel caries in vitro. Clin. Oral Investig. 2022, 26, 4407. [Google Scholar] [CrossRef]
- Verma, V.; Mathur, S.; Sachdev, V.; Singh, D. Evaluation of compressive strength, shear bond strength, and microhardness values of glass-ionomer cement Type IX and Cention N. J. Conserv. Dent. 2020, 23, 550–553. [Google Scholar] [CrossRef]
- Abdallah, A. Elemental and Micromorphological Analysis of New Alkasite Based Restorative Material/Tooth Interface. Egypt. Dent. J. 2022, 68, 1065–1072. [Google Scholar] [CrossRef]
- Giordano, M.; Ausiello, P.; Martorelli, M. Accuracy evaluation of surgical guides in implant dentistry by non-contact reverse engineering techniques. Dent. Mater. 2012, 28, e178–e185. [Google Scholar] [CrossRef]

| Material/Structure | Elastic Modulus (GPa) | Poisson Ratio |
|---|---|---|
| Enamel [18] | 84.1 | 0.33 |
| Dentin [18] | 18 | 0.30 |
| Bulk-fill resin composite [22] | 12.0 | 0.25 |
| Flowable resin composite [22] | 8.0 | 0.25 |
| Glass ionomer cement [17] | 10.8 | 0.30 |
| Alkasite [19] | 13.0 | 0.3 |
| Model | Region | Stress (MPa) |
|---|---|---|
| Bulk restoration in bulk-fill resin composite | Enamel | 11.12 |
| Dentin | 4.15 | |
| Restoration | 5.93 | |
| Flowable resin composite below the bulk-fill resin composite restoration | Enamel | 11.27 |
| Dentin | 4.26 | |
| Restoration | 5.98 | |
| Glass ionomer cement below the bulk-fill resin composite restoration | Enamel | 11.25 |
| Dentin | 4.26 | |
| Restoration | 5.99 | |
| Bulk restoration in Alkasite | Enamel | 12.04 |
| Dentin | 4.49 | |
| Restoration | 4.73 | |
| Flowable resin composite below the Alkasite restoration | Enamel | 12.41 |
| Dentin | 4.50 | |
| Restoration | 4.76 | |
| Glass ionomer cement below the Alkasite restoration | Enamel | 12.23 |
| Dentin | 4.51 | |
| Restoration | 4.74 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ausiello, P.; Dal Piva, A.M.d.O.; di Lauro, A.E.; Garcia-Godoy, F.; Testarelli, L.; Tribst, J.P.M. Mechanical Behavior of Alkasite Posterior Restorations in Comparison to Polymeric Materials: A 3D-FEA Study. Polymers 2022, 14, 1502. https://doi.org/10.3390/polym14081502
Ausiello P, Dal Piva AMdO, di Lauro AE, Garcia-Godoy F, Testarelli L, Tribst JPM. Mechanical Behavior of Alkasite Posterior Restorations in Comparison to Polymeric Materials: A 3D-FEA Study. Polymers. 2022; 14(8):1502. https://doi.org/10.3390/polym14081502
Chicago/Turabian StyleAusiello, Pietro, Amanda Maria de Oliveira Dal Piva, Alessandro Espedito di Lauro, Franklin Garcia-Godoy, Luca Testarelli, and João Paulo Mendes Tribst. 2022. "Mechanical Behavior of Alkasite Posterior Restorations in Comparison to Polymeric Materials: A 3D-FEA Study" Polymers 14, no. 8: 1502. https://doi.org/10.3390/polym14081502
APA StyleAusiello, P., Dal Piva, A. M. d. O., di Lauro, A. E., Garcia-Godoy, F., Testarelli, L., & Tribst, J. P. M. (2022). Mechanical Behavior of Alkasite Posterior Restorations in Comparison to Polymeric Materials: A 3D-FEA Study. Polymers, 14(8), 1502. https://doi.org/10.3390/polym14081502










