The Effect of Nanoparticle-Incorporated Natural-Based Biomaterials towards Cells on Activated Pathways: A Systematic Review
Abstract
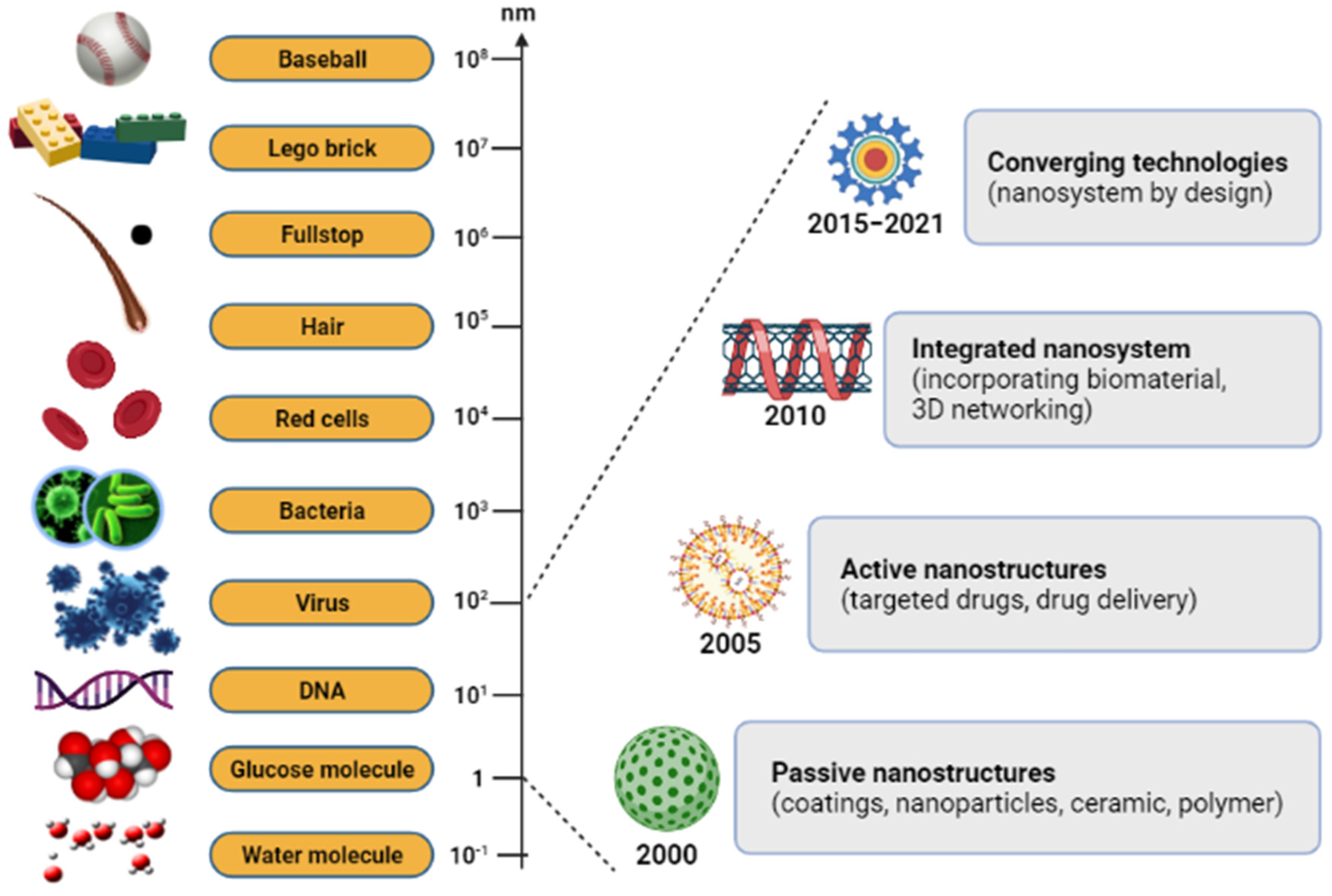
:1. Introduction
2. Methodology
2.1. Literature Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Data Extraction and Management
2.5. Quality Assessment
3. Results
3.1. Study Characteristics
3.2. Nanoparticles-Incorporated Biomaterial Platforms
3.2.1. Silver Nanoparticle-Embedded Electrospun Nanofibers
3.2.2. Chitosan-Based Nanocomposite Porous Bioscaffolds
3.2.3. Metallic Nanoparticle-Entrapped Hydrogel
3.2.4. Nanoparticle-Impregnated Polymeric Composite Films
4. Biological Cellular Effects and Signaling Pathways
5. Discussion
6. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bayda, S.; Adeel, M.; Tuccinardi, T.; Cordani, M.; Rizzolio, F. The history of nanoscience and nanotechnology: From chemical-physical applications to nanomedicine. Molecules 2020, 25, 112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, I.; Saeed, K.; Khan, I. Nanoparticles: Properties, applications and toxicities. Arab. J. Chem. 2019, 12, 908–931. [Google Scholar] [CrossRef]
- Kaur, P.; Luthra, R. Silver nanoparticles in dentistry: An emerging trend. SRM J. Res. Dent. Sci. 2016, 7, 162–165. [Google Scholar] [CrossRef]
- Mahor, A.; Prajapati, S.K.; Verma, A.; Gupta, R.; Singh, T.R.R.; Kesharwani, P. Development, in-vitro and in-vivo characterization of gelatin nanoparticles for delivery of an anti-inflammatory drug. J. Drug Deliv. Sci. Technol. 2016, 36, 55–61. [Google Scholar] [CrossRef]
- Gnach, A.; Lipinski, T.; Bednarkieicz, A.; Rybka, J.; Capobianco, J.A. Upconverting nanoparticles: Assessing the toxicity. Chem. Soc. Rev. 2015, 44, 1561–1584. [Google Scholar] [CrossRef]
- Fadilah, N.I.M.; Ahamd, H.; Rahman, M.F.A.; Rahman, N.A. Electrospun poly(vinyl alcohol) nanofibers doped with mesoporous silica nanoparticles for controlled release of hydrophilic model drug. Malays. J. Anal. Sci. 2019, 23, 212–218. [Google Scholar]
- Jeevanandam, J.; Barhoum, A.; Chan, Y.S.; Dufresne, A.; Danquah, M.K. Review on nanoparticles and nanostructured materials: Histroy, sources, toxicity and regulations. Beilstein J. Nanotechnol. 2018, 9, 1050–1074. [Google Scholar] [CrossRef] [Green Version]
- Fathi-Achachelouei, M.; Knopf-Margues, H.; Ribeiro da Silva, C.E.; Barthes, J.; Bat, E.; Tezcaner, A.; Vrana, N.E. Use of nanoparticles in tissue engineering and regenerative medicine. Front. Bioeng. Biotechnol. 2016, 7, 113–135. [Google Scholar] [CrossRef] [Green Version]
- Zheng, X.; Zhang, P.; Fu, Z.; Meng, S.; Dai, L.; Yang, H. Applications of nanomaterials in tissue engineering. RSC Adv. 2021, 11, 19041. [Google Scholar] [CrossRef]
- Kamoun, E.A.; Loutfy, S.A.; Hussein, Y.; Kenawy, E.S. Recent advances in PVA-polysaccharide based hydrogels and electrospun nanofibers in biomedical applications: A review. Int. J. Biol. Macromol. 2021, 187, 755–768. [Google Scholar] [CrossRef]
- Lickmichand, M.; Shaji, C.S.; Valarmathi, N.; Benjamin, A.S.; Kumar, R.K.; Nayak, S.; Saraswathy, R.; Sumathi, S.; Arunai, N.R.N. In Vitro biocompatibility and hyperthermia studies on synthesized cobalt ferrite nanoparticles encapsulated with polyethylene glycol for biomedical applications. Mater. Today Proc. 2019, 15, 252–261. [Google Scholar] [CrossRef]
- Islam, M.S.; Islam, M.M.; Islam, K.N. The effect of CaCO3 nanoparticles and chitosan on the properties of PLA based biomaterials for biomedical applications. Encycl. Renew. Sustain. Mater. 2020, 2, 736–745. [Google Scholar]
- Torgbo, S.; Sukyai, P. Biodegradation and thermal stability of bacterial cellulose as biomaterial: The relevance in biomedical applications. Polym. Degrad. Stab. 2020, 179, 109232. [Google Scholar] [CrossRef]
- Liu, X.; Zheng, C.; Luo, X.; Wang, X.; Jiang, H. Recent advances of collagen-based biomaterials: Multi-hierarchical structure, modification and biomedical applications. Mater. Sci. Eng. C 2019, 99, 1509–1522. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.; Fauzi, M.B. Current update of collagen nanomaterials-fabrication, characterization and its applications: A review. Pharmaceutics 2021, 13, 316. [Google Scholar] [CrossRef] [PubMed]
- El Fawal, G.; Hong, H.; Mo, X.; Wang, H. Fabrication of scaffold based on gelatin and polycaprolactone (PCL) for wound dressing application. J. Drug Deliv. Sci. Technol. 2021, 63, 102501. [Google Scholar] [CrossRef]
- Hu, B.; Guo, Y.; Li, H.; Liu, X.; Fu, Y.; Ding, F. Recent advances in chitosan-based layer-by-layer biomaterials and their biomedical applications. Carbohydr. Polym. 2021, 271, 118427. [Google Scholar] [CrossRef]
- Patil, P.P.; Reagen, M.R.; Bohara, R.A. Silk fibroin and silk-based biomaterial derivatives for ideal wound dressings. Int. J. Biol. Macromol. 2020, 164, 4613–4627. [Google Scholar] [CrossRef]
- Ucar, B. Natural biomaterials in brain repair: A focus on collagen. Neurochem. Int. 2021, 146, 105033. [Google Scholar] [CrossRef]
- Zulkiflee, I.; Fauzi, M.B. Gelatin-polyvinyl alcohol film for tissue engineering: A concise review. Biomedicines 2021, 9, 979. [Google Scholar] [CrossRef]
- Sun, J.; Tan, H. Alginate-based biomaterials for regenerative medicine applications. Materials 2013, 6, 1285–1309. [Google Scholar] [CrossRef]
- Lee, C.H.; Singla, A.; Lee, Y. Biomedical application of collagen. Int. J. Pharm. 2001, 221, 1–22. [Google Scholar] [CrossRef]
- Kalashnikova, I.; Das, S.; Seal, S. Nanomaterials for wound healing: Scope and advancement. Nanomedicine 2015, 10, 2593–2612. [Google Scholar] [CrossRef] [PubMed]
- Akrami-Hasan-Kohal, M.; Eskandari, M.; Solouk, A. Silk fibroin hydrogel/dexamethasone sodium phosphate loaded chitosan nanoparticles as a potential drug delivery system. Colloids Surf. B 2021, 205, 111892. [Google Scholar] [CrossRef]
- Huang, J.; Ren, J.; Chen, G.; Deng, Y.; Wang, G.; Wu, X. Evaluation of the xanthan-based film incorporated with silver nanoparticles for potential application in the non-healing infectious wound. J. Nanomater. 2017, 2017, 6802397. [Google Scholar] [CrossRef] [Green Version]
- Kumar, S.S.D.; Rajendran, N.K.; Houreld, N.N.; Abrahamse, H. Recent advances on silver nanoparticle and biopolymer-based biomaterials for wound healing applications. Int. J. Biol. Macromol. 2018, 115, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Nekounam, H.; Kandi, M.R.; Shaterabadi, D.; Samadian, H.; Mahmoodi, N.; Hasanzadeh, E.; Faridi-Majidi, R. Silica nanoparticles-incorporated carbon nanofibers as bioactive biomaterial for bone tissue engineering. Diam. Relat. Mater. 2021, 115, 108320. [Google Scholar] [CrossRef]
- Bapat, R.A.; Chaubal, T.V.; Joishi, C.P.; Bapat, P.R.; Choudhury, H.; Pandey, M.; Gorain, B.; Kesharwani, P. An overview of application of silver nanoparticles for biomaterials in dentistry. Mater. Sci. Eng. C 2018, 91, 881–898. [Google Scholar] [CrossRef]
- Bapat, R.A.; Chaubal, T.V.; Dharmadhikari, S.; Abdulla, A.M.; Bapat, P.; Alexander, A.; Dubey, S.K.; Kesharwani, P. Recent advances of gold nanoparticles as biomaterial in dentistry. Int. J. Pharm. 2020, 586, 119596. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, H.; Gao, F.; Xu, Z.; Dai, F.; Liu, W. An injectable supramolecular polymer nanocomposite hydrogel for prevention of breast cancer recurrence with theranostic and mammoplastic functions. Adv. Funct. Mater. 2018, 28, 1801000. [Google Scholar] [CrossRef]
- Mousa, M.; Evans, N.D.; Oreffo, R.O.C.; Dawson, J.I. Clay nanoparticles for regenerative medicine and biomaterial design: A review of clay bioactivity. Biomaterials 2018, 159, 204–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sebastiammal, S.; Fathima, A.S.L.; Devanesan, S.; AlSalhi, M.S.; Henry, J.; Govindarajan, M.; Vaseeharan, B. Curcumin-encased hydroxyapatite nanoparticles as novel biomaterials for antimicrobial, antioxidant and anticancer applications: A perspective of nano-based drug delivery. J. Drug Deliv. Sci. Technol. 2020, 57, 101752. [Google Scholar] [CrossRef]
- Zengin, A.; Sutthavas, P.; Rijt, S.V. Inorganic nanoparticle-based biomaterials for regenerative medicine. In Nanostructured Biomaterials for Regenerative Medicine; Woodhead Publishing: Cambridge, UK, 2020; Volume 1, pp. 293–312. [Google Scholar]
- Liu, Y.; Shi, J. Antioxidative nanomaterials and biomedical applications. Nano Today 2019, 27, 146–177. [Google Scholar] [CrossRef]
- Padmanabhan, J.; Kyriakides, T.R. Nanomaterials, inflammation and tissue engineering. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2015, 7, 355–370. [Google Scholar] [CrossRef] [Green Version]
- Hasan, A.; Morshed, M.; Memic, A.; Hassan, S.; Webster, T.J.; El-Sayed Marei, H. Nanoparticles in tissue engineering: Applications, challenges and prospects. Int. J. Nanomed. 2018, 13, 5637. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and metaanalyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Implement. 2015, 13, 132–140. [Google Scholar] [CrossRef] [Green Version]
- Sofi, H.S.; Akram, T.; Shabir, N.; Vasita, R.; Jadhav, A.H.; Sheikh, F.A. Regenerated cellulose nanofibers from cellulose acetate: Incorporating hydroxyapatite (HAp) and silver (Ag) nanoparticles (NPs), as a scaffold for tissue engineering applications. Mater. Sci. Eng. C 2021, 118, 111547. [Google Scholar] [CrossRef]
- Kaparekar, P.S.; Pathmanapan, S.; Anandasadagopan, S.K. Polymeric scaffold of Gallic acid loaded chitosan nanoparticles infused with collagen-fibrin for wound dressing application. Int. J. Biol. Macromol. 2020, 165, 930–947. [Google Scholar] [CrossRef]
- Ibrahim, H.M.; Reda, M.M.; Klingner, A. Preparation and characterization of green carboxymethylchitosan (CMCS)-polyvinyl alcohol (PVA) electrospun nanofibers containing gold nanoparticles (AuNPs) and its potential use as biomaterials. Int. J. Biol. Macromol. 2020, 151, 821–829. [Google Scholar] [CrossRef]
- Augustine, R.; Dalvi, Y.B.; Yadu, N.V.K.; Varghese, R.; Raghuveeran, V.; Hasan, A.; Thomas, S.; Sandhyarani, N. Yttrium oxide nanoparticle loaded scaffolds with enhanced cell adhesion and vascularization for tissue engineering applications. Mater. Sci. Eng. C 2019, 103, 109801. [Google Scholar] [CrossRef] [PubMed]
- Barros, J.; Ferraz, M.P.; Fernandes, M.H.; Gomes, P.S.; Monteiro, F.J. Alginate-nanohydroxyapatite hydrogel system: Optimizing the formulation for enhanced bone regeneration. Mater. Sci. Eng. C 2019, 105, 109985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shams, M.; Karimi, M.; Ghollasi, M.; Nezafati, N.; Salimi, A. Electrospun poly-L-lactic acid nanofibers decorated with melt-derived S53P4 bioactive glass nanoparticles: The effect of nanoparticles on proliferation and osteogenic differentiation of human bone marrow mesenchymal stem cells in vitro. Ceram. Int. 2018, 44, 20211–20219. [Google Scholar] [CrossRef]
- Liu, P.; Zhao, Y.; Yuan, Z.; Ding, H.; Hu, Y.; Yang, W.; Cai, K. Construction of Zn-incorporated multilayer films to promote osteoblasts growth and reduce bacterial adhesion. Mater. Sci. Eng. C 2017, 75, 998–1005. [Google Scholar] [CrossRef] [PubMed]
- Fahimirad, S.; Abtahi, H.; Satei, P.; Ghaznavi-Rad, E.; Moslehi, M.; Ganji, A. Wound healing performance of PCL/chitosan beased electrospun nanofiber electrosprayed with curcumin loaded chitosan nanoparticles. Carbohydr. Polym. 2021, 259, 117640. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhu, Z.; Pei, X.; Zhang, X.; Cheng, X.; Hu, S.; Gao, X.; Wang, G.J.; Chen, J.; Wan, Q. ZIF-8 modified multifunctional bone-adhesive hydrogels promoting angiogenesis and osteogenesis for bone regeneration. ACS Appl. Mater. Interfaces 2020, 12, 36978–36995. [Google Scholar] [CrossRef]
- Konop, M.; Czuwara, J.; Klodzinska, E.; Laskowska, A.K.; Sulejczak, D.; Damps, T.; Zielenkiewicz, U.; Brzozowska, I.; Sureda, A.; Kowalkowski, T.; et al. Evaluation of keratin biomaterial containing silver nanoparticles as a potential wound dressing in full-thickness skin wound model in diabetic mice. J. Tissue Eng. Regen. Med. 2020, 14, 334–346. [Google Scholar] [CrossRef]
- Zhang, S.; Ou, Q.; Xin, P.; Yuan, Q.; Wang, Y.; Wu, J. Polydopamine/puerin nanoparticles incorporated hybrid hydrogels for enhanced wound healing. Biomater. Sci. 2019, 10, 4230–4236. [Google Scholar] [CrossRef]
- Masood, N.; Ahmed, R.; Tariq, M.; Ahmed, Z.; Masoud, M.S.; Ali, I.; Asghar, R.; Andleeb, A.; Hasan, A. Silver nanoparticle impregnated chitosan-PEG hydrogel enhances wound healing in diabetes induced rabbits. Int. J. Pharm. 2019, 559, 23–36. [Google Scholar] [CrossRef]
- Kalantari, K.; Mostafavi, E.; Saleh, B.; Soltantabar, P.; Webster, T.J. Chitosa/PVA hydrogels incorporated with green synthesized cerium oxide nanoparticles for wound healing applications. Eur. Polym. J. 2020, 134, 109853. [Google Scholar] [CrossRef]
- Norouzi, M.A.; Montazer, M.; Harifi, T.; Karimi, P. Flower buds like PVA/ZnO composite nanofbers assembly: Antibacterial, in vivo wound healing, cytotoxicity and histological studies. Polym. Test. 2021, 93, 106914. [Google Scholar] [CrossRef]
- Fadilah, N.I.M.; Rahman, M.B.A.; Yusof, L.M.; Mustapha, N.M.; Ahmad, H. The therapeutic effect and in vivo assessment of Palmitoyl-GDPH on the wound healing process. Pharmaceutics 2021, 13, 193. [Google Scholar] [CrossRef]
- Chronopoulou, L.; Cacciotti, I.; Amalfitano, A.; Di Nitto, A.; D’Arienzo, V.; Nocca, G.; Palocci, C. Biosynthesis of innovative calcium phosphate/hydrogel composites: Physicochemical and biological characterization. Nanotechnology 2020, 32, 095102. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yan, L.; Yang, W.; Lan, Y.; Zhu, Q.; Xu, H.; Zheng, C.; Guo, R. Controlled-release neurotensin-loaded silk fibroin dressing improve wound healing in diabetic rat model. Bioact. Mater. 2019, 4, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Busra, F.M.; Chowdhury, S.R.; Saim, A.B.; Idrus, R.B. Genotoxicity and cytotoxicity of ovine collagen on human dermal fibroblast. Saudi Med. J. 2011, 32, 1311–1312. [Google Scholar] [PubMed]
- Kim, K.J.; Sung, W.S.; Suh, B.K.; Moon, S.K.; Choi, J.S.; Kim, J.G.; Lee, D.G. Antifungal activity and mode of action of silver nanoparticles on Candida albicans. Biometals 2009, 22, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.K.; Kim, B.H.; Jung, G. Antifungal activity of silver ions and nanoparticles on phytopathogenic fungi. Plant Dis. 2009, 93, 1037–1043. [Google Scholar] [CrossRef] [Green Version]
- Panacek, A.; Kolar, M.; Vecerova, R.; Prucek, R.; Soukupova, J.; Kryatof, V. Antifungal activity of silver nanoparticles against Candida spp. Biomaterials 2009, 31, 6333–6340. [Google Scholar] [CrossRef]
- Lara, H.H.; Garza-Trevino, E.N.; Ixtepan-Turrent, L. Silver nanoparticles are broad-spectrum bactericidal and virucidal compounds. J. Nanobiotechnol. 2011, 9, 30. [Google Scholar] [CrossRef] [Green Version]
- Lara, H.H.; Ayala-Nunez, N.V.; Ixtepan-Turrent, L.; Rodriguez-Padilla, C. Mode of antiviral action of silver nanoparticles against HIV-1. J. Nanobiotechnol. 2010, 8, 1. [Google Scholar] [CrossRef]
- Manea, F.; Motoc, S.; Pop, A.; Remes, A.; Schoonman, J. Silver-functionalized carbon nanofiber composite electrodes for ibuprofen detection. Nanoscale Res. 2012, 7, 331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez-Leon, E.; Iniguez-Palomares, R.; Navarro, R.E.; Herrera-Urbina, R.; Tanori, J.; Iniguez-Palomares, C.; Maldomado, A. Synthesis of silver nanoparticles using reducing agents obtained from natural sources (Rumex hymenosepalus extracts). Nanoscale Res. Lett. 2013, 8, 318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sondi, I.; Salopek-Sondi, B. Silver nanoparticles as antimicrobial agent: A case study on E. coli as a model for Gram-negative bacteria. J. Colloid Interface Sci. 2004, 275, 177–182. [Google Scholar] [CrossRef]
- Martinez-Castanon, G.A.; Nino-Martinez, N.; Martinez-Gutierrez, F.; Martinez-Mendoza, J.R.; Ruiz, F. Synthesis and antibacterial activity of silver nanoparticles with different sizes. J. Nanopart. Res. 2008, 10, 1343–1348. [Google Scholar] [CrossRef]
- Guzman, M.; Dille, J.; Godjet, S. Synthesis and antibacterial activity of silver nanoparticles against gram-positive and gram-negative bacteria. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Salleh, A.; Naomi, R.; Utami, N.D.; Mohammad, A.W.; Mahmoudi, E.; Mustafa, N.; Fauzi, M.B. The potential of silver nanoparticles for antiviral and antibacterial applications: A mechanism of action. Nanomaterials 2020, 10, 1566. [Google Scholar] [CrossRef] [PubMed]
- Szmyd, R.; Goralczyk, A.G.; Skalniak, L.; Cierniak, A.; Lipert, B.; Filon, F.L.; Crosera, M.; Borowczyk, J.; Laczna, E.; Drukala, J.; et al. Effect of silver nanoparticles on human primary keratinocytes. Biol. Chem. 2013, 394, 113–123. [Google Scholar] [CrossRef]
- Almetwally, A.A.; El-Sakhawy, M.; Elshakankery, M.H.; Kasem, M.H. Technology of nano-fibers: Production techniques and properties-Critical review. J. Text. Assoc. 2017, 78, 5–14. [Google Scholar]
- Bianco, A.; Cacciotti, I.; Fragala, M.E.; Lamastra, F.R.; Speghini, A.; Piccinelli, F.; Gusmano, G. Eu-doped titania nanofibers: Processing, thermal behavior and luminescent properties. J. Nanosci. Nanotechnol. 2010, 10, 5183–5190. [Google Scholar] [CrossRef]
- Zhang, S.; Tang, Y.; Vlahovic, B. A review on preparation and applications of silver-containing nanofibers. Nanoscale Res. Lett. 2016, 11, 80. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.F.; Zhang, J.; Liu, J.J.; Zhou, Q.H.; Liu, Z.; Hu, P.Y.; Yuan, Z.; Ramakrishna, S.; Yang, D.P.; Long, Y.Z. Bifunctional CuS composite nanofibers via in situ electrospinning for outdoor rapid hemostasis and simultaneous ablating superbug. Chem. Eng. J. 2020, 401, 126096. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, Y.T.; Hu, P.Y.; Liu, J.J.; Liu, X.F.; Hu, M.; Cui, Z.; Wang, N.; Niu, Z.; Xiang, H.F.; et al. Laparoscopic electrospinning for in situ hemostasis in minimally invasive operation. Chem. Eng. J. 2020, 395, 125089. [Google Scholar] [CrossRef]
- Xie, X.; Chen, Y.; Wang, X.; Xu, X.; Shen, Y.; Aldalbahi, A.; Fetz, A.E.; Bowlin, G.L.; El-Newehy, M.; Mo, X. Electrospinning nanofiber scaffolds for soft and hard tissue regeneration. J. Mater. Sci. Technol. 2020, 59, 243–261. [Google Scholar] [CrossRef]
- He, C.; Liu, X.; Zhou, Z.; Liu, N.; Ninga, X.; Miao, Y.; Long, Y.; Wu, T.; Leng, X. Harnessing biocompatible nanofibers and silver nanoparticles for wound healing: Sandwich wound dressing versus commercial silver sulfadiazine dressing. Mater. Sci. Eng. C 2021, 128, 112342. [Google Scholar] [CrossRef] [PubMed]
- Eghbalifam, N.; Shojaosadati, S.A.; Hashemi-Najafabadi, S.; Khorasani, A.C. Synthesis and characterization of antimicrobial wound dressing material based on silver nanoparticles loaded gum Arabic nanofibers. Int. J. Biol. Macromol. 2020, 155, 119–130. [Google Scholar] [CrossRef]
- El-Aassar, M.R.; Ibrahim, O.M.; Fouda, M.M.; El-Beheri, N.G.; Agwa, M.M. Wound healing of nanofiber comprising Polygalacturonic/Hyaluronic acid embedded silver nanoparticles: In-vitro and in-vivo studies. Carbohydr. Polym. 2020, 238, 116175. [Google Scholar] [CrossRef]
- Krishnan, P.D.; Banas, D.; Durai, R.D.; Kabanov, D.; Hosnedlova, B.; Kepinska, M.; Fernandez, C.; Ruttkay-Nedecky, B.; Nguyen, H.V.; Farid, A.; et al. Silver nanomaterials for wound dressing applications. Pharmaceutics 2020, 12, 821. [Google Scholar] [CrossRef]
- Nosrati, H.; Khouy, R.A.; Nosrati, A.; Khodaei, M.; Banitalebi-Dehkordi, M.; Ashrafi-Dehkordi, K.; Sanami, S.; Alizadeh, Z. Nanocomposite scaffolds for accelerating chronic wound healing by enhancing angiogenesis. J. Nanobiotechnol. 2021, 19, 1. [Google Scholar] [CrossRef]
- Ivashchenko, O.; Peplinska, B.; Przysiecka, Ł.; Coy, E.; Jarek, M.; Chybczynska, K.; Jurga, S. Nanocomposite Gel as Injectable Therapeutic Scaffold: Microstructural Aspects and Bioactive Properties. ACS Appl. Mater. Interfaces 2020, 12, 7840–7853. [Google Scholar] [CrossRef]
- Rezaei, V.; Mirzaei, E.; Taghizadeh, S.M.; Berenjian, A.; Ebrahiminezhad, A. Nano iron oxide-PCL composite as an improved soft tissue scaffold. Processes 2021, 9, 1559. [Google Scholar] [CrossRef]
- Kim, I.Y.; Seo, S.J.; Moon, H.S.; Yoo, M.K.; Park, I.Y.; Kim, B.C.; Cho, C.S. Chitosan and its derivatives for tissue engineering applications. Biotechnol. Adv. 2008, 26, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Mi, F.L.; Shyu, S.S.; Wu, Y.B.; Lee, S.T.; Shyong, J.Y.; Huang, R.N. Fabrication and characterization of a sponge-like asymmetric chitosan membrane as a wound dressing. Biomaterials 2001, 22, 165–173. [Google Scholar] [CrossRef]
- Li, J.; Zhuang, S. Antibacterial activity of chitosan and its derivatives and their interaction mechanism with bacteria: Current state and perspectives. Eur. Polym. J. 2020, 138, 109984. [Google Scholar] [CrossRef]
- Nowroozi, N.; Faraji, S.; Nouralishahi, A.; Shahrousvand, M. Biological and structural properties of graphene oxide/curcumin nanocomposite incorporated chitosan as a scaffold for wound healing application. Life Sci. 2021, 264, 118640. [Google Scholar] [CrossRef] [PubMed]
- Mariia, K.; Ariff, M.; Shi, J.; Song, F.; Chi, Z.; Liu, C. Novel chitosan-ulvan hydrogel reinforcement by cellulose nanocrystals with epidermal growth factor for enhanced wound healing: In vitro and in vivo analysis. Int. J. Biol. Macromol. 2021, 183, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Jayaramudu, T.; Ko, H.U.; Kim, H.C.; Kim, J.W.; Kim, J. Swelling behavior of polyacrylamide–cellulose nanocrystal hydrogels: Swelling kinetics, temperature, and pH effects. Materials 2019, 12, 2080. [Google Scholar] [CrossRef] [Green Version]
- Tan, H.L.; Teow, S.Y.; Pushpamalar, J. Application of metal nanoparticle-hydrogel composites in tissue regeneration. Bioengineering 2019, 6, 17. [Google Scholar] [CrossRef] [Green Version]
- Calo, E.; Khutoryanskiy, V.V. Biomedical applications of hydrogels: A review of patents and commercial products. Eur. Polym. J. 2015, 65, 252–267. [Google Scholar] [CrossRef] [Green Version]
- Mantha, S.; Pillai, S.; Khayambashi, P.; Upadhyay, A.; Zhang, Y.; Tao, O.; Pham, H.M.; Tran, S.D. Smart hydrogels in tissue engineering and regenerative medicine. Materials 2019, 12, 3323. [Google Scholar] [CrossRef] [Green Version]
- Ciocci, M.; Cacciotti, I.; Seliktar, D.; Melino, S. Injectable silk fibroin hydrogels functionalized with microspheres as adult stem cells-carrier system. Int. J. Biol. Macromol. 2018, 108, 960–971. [Google Scholar] [CrossRef]
- Do, A.V.; Khorsand, B.; Geary, S.M.; Salem, A.K. 3D printing of scaffolds for tissue regeneration applications. Adv. Healthc. Mater. 2015, 4, 1742–1762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaharwar, A.K.; Peppas, N.A.; Khademhosseini, A. Nanocomposite hydrogels for biomedical applications. Biotechnol. Bioeng. 2014, 111, 441–543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takeno, H.; Aoki, Y.; Kimura, K. Effects of silica and clay nanoparticles on the mechanical properties of poly (vinyl alcohol) nanocomposite hydrogels. Colloids Surf. A Physicochem. Eng. Asp. 2021, 630, 127592. [Google Scholar] [CrossRef]
- Cleetus, C.M.; Primo, F.A.; Fregoso, G.; Raveendran, N.L.; Noveron, J.C.; Spencer, C.T.; Ramana, C.V.; Joddar, B. Alginate hydrogels with embedded ZnO nanoparticles for wound healing therapy. Int. J. Nanomed. 2020, 15, 5097. [Google Scholar] [CrossRef]
- Zulkifli, F.H.; Hussain, F.S.J.; Zeyohannes, S.S.; Rasad, M.S.B.A.; Yusuff, M.M. A facile synthesis method of hydroxyethyl cellulose-silver nanoparticle scaffolds for skin tissue engineering applications. Mater. Sci. Eng. C 2017, 79, 151–160. [Google Scholar] [CrossRef] [Green Version]
- Mahmoud, N.N.; Hikmat, S.; Ghith, D.A.; Hajeer, M.; Hamadneh, L.; Qattan, D.; Khalil, E.A. Gold nanoparticles loaded into polymeric hydrogel for wound healing in rats: Effect of nanoparticles’ shape and surface modification. Int. J. Pharm. 2019, 565, 174–186. [Google Scholar] [CrossRef]
- Shanmugapriya, K.; Kim, H.; Saravana, P.S.; Chun, B.S.; Kang, H.W. Fabrication of multi-functional chitosan-based nanocomposite film with rapid healing and antibacterial effect for wound management. Int. J. Biol. Macromol. 2018, 118, 1713–1725. [Google Scholar] [CrossRef]
- Leng, Q.; Li, Y.; Pang, X.; Wang, B.; Wu, Z.; Lu, Y.; Xiong, K.; Zhao, L.; Zhou, P.; Fu, S. Curcumin nanoparticles incorporated in PVA/collagen composite films promote wound healing. Drug Deliv. 2020, 27, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wang, H.; Pan, S.; Fu, C.; Chang, Y.; Li, H.; Yang, X.; Qi, Z. Evaluation of new film based on chitosan/gold nanocomposites on antibacterial property and wound-healing efficacy. Adv. Mater. Sci. Eng. 2020, 2020, 6212540. [Google Scholar] [CrossRef]
- Mohandas, A.; Deepthi, S.; Biswas, R.; Jayakumar, R. Chitosan based metallic nanocomposite scaffolds as antimicrobial wound dressings. Bioact. Mater. 2018, 3, 267–277. [Google Scholar] [CrossRef]
- Vijayakumar, V.; Samal, S.K.; Mohanty, S.; Nayak, S.K. Recent advancements in biopolymer and metal nanoparticle-based materials in diabetic wound healing management. Int. J. Biol. Macromol. 2019, 122, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Verma, N.; Pramanik, K.; Singh, A.K.; Biswas, A. Design of magnesium oxide nanoparticle incorporated carboxy methyl cellulose/poly vinyl alcohol composite film with novel composition for skin tissue engineering. Mater. Technol. 2021. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, X.; Zhang, Y.; Liu, Y.; Wang, D.; Yu, X.; Wang, H.; Bai, Z.; Jiang, Y.C.; Li, X.; et al. Endothelial cell migration regulated by surface topography of poly (ε-caprolactone) nanofibers. ACS Biomater. Sci. Eng. 2021, 7, 4959–4970. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.S.D.; Abrahamse, H. Advancement of nanobiomaterials to deliver natural compounds for tissue engineering applications. Int. J. Mol. Sci. 2020, 21, 6752. [Google Scholar] [CrossRef]
- Ehterami, A.; Salehi, M.; Farzamfar, S.; Vaez, A.; Samadian, H.; Sahrapeyma, H.; Mirzaii, M.; Ghorbani, S.; Goodarzi, A. In vitro and in vivo study of PCL/COLL wound dressing loaded with insulin-chitosan nanoparticles on cutaneous wound healing in rats model. Int. J. Biol. Macromol. 2018, 117, 601–609. [Google Scholar] [CrossRef]
- Balakrishnan, S.B.; Kuppu, S.; Thambusamy, S. Biologically important alumina nanoparticles modified polyvinylpyrrolidone scaffolds in vitro characterizations and it is in vivo wound healing efficacy. J. Mol. Struct. 2021, 1246, 131195. [Google Scholar] [CrossRef]
- Zhang, M.; Wang, G.; Wang, D.; Zheng, Y.; Li, Y.; Meng, W.; Zhang, X.; Du, F.; Lee, S. Ag@MOF-loaded chitosan nanoparticle and polyvinyl alcohol/sodium alginate/chitosan bilayer dressing for wound healing applications. Int. J. Biol. Macromol. 2021, 175, 481–494. [Google Scholar] [CrossRef]
- Galandakova, A.; Frankova, J.; Ambrozova, N.; Habartova, K.; Pivodova, V.; Zalesak, B.; Safarova, K.; Smekalova, M.; Ulrichova, J. Effects of silver nanoparticles on human dermal fibroblasts and epidermal keratinocytes. Hum. Exp. Toxicol. 2016, 35, 946–957. [Google Scholar] [CrossRef]
- Azlan, A.Y.H.N.; Katas, H.; Busra, M.F.M.; Salleh, N.A.M.; Smandri, A. Metal nanoparticles and biomaterials: The multipronged approach for potential diabetic wound therapy. Nanotechnol. Rev. 2021, 10, 653–670. [Google Scholar] [CrossRef]
- Yang, H.S.; Tsai, Y.C.; Korivi, M.; Chang, C.T.; Hseu, Y.C. Lucidone promotes the cutaneous wound healing process via activation of the PI3K/AKT, Wnt/β-catenin and NF-κB signaling pathways. Biochim. Biophys. Acta 2017, 1864, 151–168. [Google Scholar] [CrossRef]
- Cheon, S.S.; Cheah, A.Y.; Turley, S.; Nadesan, P.; Poon, R.; Clevers, H.; Alman, B.A. β-catenin stabilization dysregulates mesenchymal cell proliferation, mortility, and invasiveness and causes aggressive fibromatosis and hyperplastic cutaneous wounds. Proc. Natl. Acad. Sci. USA 2002, 99, 6973–6978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clevers, H.; Nusse, R. Wnt/β-catenin signaling and disease. Cell 2012, 149, 1192–1205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Houschyar, K.S.; Momeni, A.; Pyles, M.N.; Maan, Z.N.; Whittam, A.J.; Siemers, F. Wnt signaling induces epithelial differentiation during cutaneous wound healing. Organogenesis 2015, 11, 95–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birdsey, G.M.; Shah, A.V.; Dufton, N. The endothelial transcription factor ERG promotes vascular stability and growth through Wnt/beta-catenin signaling. Dev. Cell 2015, 32, 82–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bielefeld, K.A.; Amini-Nik, S.; Alman, B.A. Cutaneous wound healing: Recruiting developmental pathways for regeneration. Cell. Mol. Life Sci. 2013, 70, 2059–2081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanpain, C.; Fuchs, E. Epidermal homeostasis: A balancing act of stem cells in the skin. Nat. Rev. Mol. Cell. Biol. 2009, 10, 207–217. [Google Scholar] [CrossRef] [Green Version]
- Okuyama, R.; Tagami, H.; Aiba, S. Notch signaling: Its role in epidermal homeostasis and in the pathogenesis of skin diseases. J. Dermatol. Sci. 2008, 49, 187–194. [Google Scholar] [CrossRef]
- Watt, F.M.; Estrach, S.; Ambler, C.A. Epidermal Notch signaling: Differentiation, cancer and adhesion. Curr. Opin. Cell. Biol. 2008, 20, 171–179. [Google Scholar] [CrossRef] [Green Version]
- Gridley, T. Notch signaling in the vasculature. Curr. Top. Dev. Biol. 2010, 92, 277–309. [Google Scholar]
- Lim, C.H.; Sun, Q.; Ratti, K.; Lee, S.H.; Zheng, Y.; Takeo, M.; Lee, W.; Rabbani, P.; Plikus, M.V.; Cain, J.E.; et al. Hedgehog stimulates hair follicle neogenesis by creating inductive dermis during murine skin wound healing. Nat. Commun. 2018, 9, 4903. [Google Scholar] [CrossRef]
- Chen, L.; Tredget, E.E.; Wu, P.Y. Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PLoS ONE 2008, 3, e1886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, Y.; Gang, X.; Sun, C.; Wang, G. Mesenchymal stem cells improve healing of diabetic foot ulcer. J. Diabetes Res. 2017, 2017, 9328347. [Google Scholar] [CrossRef] [PubMed]
- Reddy, M.; Ponnamma, D.; Choudhary, R.; Sadasivuni, K.K. A comparative review of natural and synthetic biopolymer composite scaffolds. Polymers 2021, 13, 1105. [Google Scholar] [CrossRef] [PubMed]
- Troy, E.; Tilbury, M.A.; Power, A.M.; Wall, J.G. Nature-based biomaterials and their application in biomedicine. Polymers 2021, 13, 3321. [Google Scholar] [CrossRef]
- Sattary, M.; Khorasani, M.T.; Rafienia, M.; Rozve, H.S. Incorporation of nanohydroxyapatite and vitamin D3 into electrospun PCL/gelatin scaffolds: The influence on the physical and chemical properties and cell behavior for bone tissue engineering. Polym. Adv. Technol. 2018, 29, 451–462. [Google Scholar] [CrossRef]
- Bozorgi, A.; Khazaei, M.; Soleimani, M.; Jamalpoor, Z. Application of nanoparticles in bone tissue engineering: A review on the molecular mechanism driving osteogenesis. Biomater. Sci. 2021, 9, 4541–4567. [Google Scholar] [CrossRef]
- Soderstjerna, E.; Bauer, P.; Cedervall, T.; Abdshill, H.; Johansson, F.; Johansson, U.E. Silver and gold nanoparticles exposure to in vitro cultured retina–studies on nanoparticle internalization, apoptosis, oxidative stress, glial-and microglial activity. PLoS ONE 2014, 9, e105359. [Google Scholar] [CrossRef]
- Boonkaew, B.; Kempf, M.; Kimble, R.; Cuttle, L. Cytotoxicity testing of silver-containing burn treatments using primary and immortal skin cells. Burns 2014, 40, 1562–1569. [Google Scholar] [CrossRef] [Green Version]
- Eming, S.A.; Martin, P.; Tomic-Canic, M. Wound repair and regeneration: Mechanisms, signaling, and translation. Sci. Transl. Med. 2014, 6, 265–301. [Google Scholar] [CrossRef] [Green Version]
- Hu, H.; Zhao, P.; Liu, J.; Ke, Q.; Zhang, C.; Guo, Y.; Ding, H.; Hu, H.; Zhao, P.; Liu, J.; et al. Lanthanum phosphate/chitosan scaffolds enhance cytocompatibility and osteogenic efficiency via the Wnt/β-catenin pathway. J. Nanobiotechnol. 2018, 16, 98. [Google Scholar] [CrossRef]
- Zhang, H.; Nie, X.; Shi, X.; Zhaou, J.; Chen, Y.; Yao, Q.; Sun, C.; Yang, J. Regulatory mechanisms of the Wnt/β-catenin pathway in diabetic cutaneous ulcers. Front. Pharmacol. 2018, 9, 1114–1124. [Google Scholar] [CrossRef] [PubMed]





| Advantages | Disadvantages |
|---|---|
| Biodegradability (natural degradation mostly can occur in the body) | Low mechanical strength |
| High biocompatibility | Possible immune reaction |
| Interaction with other cells/molecules | |
| Ability to support cell adhesion, migration, proliferation and differentiation | |
| Low toxicity | |
| Lower costs |
| No | Keywords |
|---|---|
| 1 | Nanoparticle * |
| 2 | Particle * |
| 3 | Biomaterial * |
| 4 | Material * |
| 5 | Natural material * |
| 6 | Cellular pathway * |
| 7 | Signaling pathway * |
| 8 | Biomedical application * |
| 9 | Regenerative medicine application * |
| 10 | Or/1–5 |
| 11 | Or/6–9 |
| 12 | And/10 & 11 |
| 13 | Limit 12 to period: 2014–2021 |
| Author/Year | Types of Biomaterials | Nanoparticle Used | Fabrication Format | Study Design | Application | Study Measure Outcome/Biological Effects | Conclusions |
|---|---|---|---|---|---|---|---|
| Sofi et al., 2021 [39] | Cellulose | Hydroxyapatite (HAp); 0.5–1.5 wt% Silver nanoparticles (Ag NPs); 3.0–7.0 wt% | Nanofibers | In vitro | Tissue engineering | Cell viability Antimicrobial activity | Nanofiber mat (1.5% HAp and 7% Ag NPs) was toxic to growth and proliferation of the fibroblast. |
| Kaparekar et al., 2020 [40] | Collagen-fibrin | Gallic acid (GA) Chitosan (CSNPs); 0.1–0.5 wt%) | Nanocomposite scaffolds | In vitro In vivo | Wound healing | Cell viability Cell toxicity Cell migration | There was increased collagen deposition, angiogenesis, epithelialization, and fibroblast migration in the GA–CSNPs scaffold treated group. |
| Ibrahim et al., 2020 [41] | Carboxymethyl chitosan (CMCS) Polyvinyl alcohol (PVA) | Gold nanoparticles (AuNPs); 0.35–1.09 wt% | Nanofibers | In vitro | Medical biomaterials | Antibacterial activity Cell viability | AuNPs capped by CMCS showed lower cytotoxicity, and its antibacterial activities were increased by increasing AuNPs wt% in the nanofibers. |
| Augustine et al., 2019 [42] | Polycaprolactone (PCL) | Yttrium oxide (Y2O3) | Fibers | In vitro In vivo | Tissue engineering | Behavior of cells Cell viability Cell proliferation and migration Angiogenesis Inflammatory response | Y2O3 nanoparticles can perform a vital role in tissue engineering scaffolds to promote cell proliferation and angiogenesis. |
| Barros et al., 2019 [43] | Alginate | Nano hydroxyapatite (nanoHA); 30–70 wt% | Hydrogel | In vitro Ex vivo | Bone regeneration | Metabolic activity Cell proliferation Cell morphology | The biological response of composites was influenced by nanoHA content:
|
| Shams et al., 2018 [44] | Poly-L-lactic acid (PLLA) | Bioactive glass nanoparticles (BGn) | Nanocomposites | In vitro | Medical biomaterials | Cell attachment Cell viability | PLLA nanofibers with BG nanoparticles caused improved cell behavior, including cell attachment, growth, and proliferation. |
| Liu et al., 2017 [45] | Chitosan/gelatin | Zinc ions (Zn); 5–40 wt% | Multilayer films (layer-by-layer; LBL) | In vitro | Medical biomaterials | Cell viability Cell morphology Bacterial growth | The optimal modified Ti substrate (Ti-LBL-Zn10) had the greatest potential for promoting osteoblast growth. |
| Nekounam et al., 2021 [27] | Polyacrylonitrile (PAN) | Silica nanoparticles (SNPs); 1–10 wt% | Nanofibers | In vitro | Tissue engineering | Cell cytotoxicity Cell proliferation | The cytotoxicity and proliferation assays showed a noticeable enhancement in the biological features of the NFs/SNPs composite. |
| Fahimirad et al., (2021) [46] | Polycaprolactone (PCL) | Curcumin (CUR) encapsulated Chitosan (CS) | Nanofibers | In vitro In vivo | Wound healing | Antibacterial activity Cell viability/proliferation Wound healing abilities | Potential application of PCL/CS/CUR with CURCSNPs as an effective novel wound dressing with significant antibacterial activity. |
| Liu et al., 2020 [47] | Catechol-chitosan (CA-CS) | Zeolitic imidazolate framework-8 nanoparticle (ZIF-8 NP); low (L), medium (M), high (H) | Hydrogel | In vitro In vivo | Bone regeneration | Cell proliferation Bacterial adhesion Osteogenic stability | Among the CA-CS/Z hydrogels, the CA-CS/ZM hydrogel showed acceptable adhesion properties and antibacterial properties, enhancing the stability of the implanting environment after bone transplantation and promoting the healing process of bone defects. |
| Konop et al., 2019 [48] | Keratin (fur keratin-derived powder; FKDP) | Silver nanoparticles (AgNPs) | Nanocomposite scaffolds | In vitro In vivo | Wound healing | Cell viability Cell migration | FKDP–AgNPs dressing consisting of an insoluble fraction of keratin, which is biocompatible, significantly accelerated wound healing in a diabetic mouse model. |
| Zhang et al., 2019 [49] | Polyethylene glycol diacrylate (PEG/DA) | Polydopamine/Puerarin nanoparticles (PDA/PUE) | Hydrogel | In vitro In vivo | Wound healing | Cell viability Intracellular antioxidation | PEG-DA/PDA/PUE hydrogels were conducive to cell growth and could accelerate wound healing. |
| Masood et al., 2019 [50] | Chitosan–Polyethylene glycol (CH-PEG) | Silver nanoparticles (AgNPs) | Hydrogel | In vitro In vivo | Wound healing | Antibacterial property Antioxidant property Re-epithelialization | Silver nanoparticle impregnated chitosan–PEG hydrogel can be a promising material for wound healing dressing for chronic diabetic wounds. |
| Kalantari et al., (2020) [51] | Polyvinyl alcohol—Chitosan (PVA/CH) | Cerium oxide nanoparticles (CeO2-NPs); 0–1 wt% | Hydrogel | In vitro | Wound healing | Cell viability Cell metabolic activity Antibacterial activity | The chitosan/PVA hydrogels incorporated with CeO2-NPs could be a potential candidate as a robust wound dressing agent that, impressively, may decrease wound infections without resorting to the use of antibiotics. |
| Norouzi et al., 2021 [52] | Polyvinyl alcohol (PVA) | Zinc oxide (ZnO) | Nanofiber | In vitro In vivo | Wound healing | Cell viability Antibacterial activity Keratinocyte migration | ZnO nanoparticles were responsible for accelerated epithelial regeneration and better cell attachment. Therefore, these composite fibers have potential in biomedical applications such as wound healing and tissue reconstruction. |
| Wnt Target Genes | Role in Wound Healing |
|---|---|
| Axin2 | Hair formation through activation of hair follicles |
| Collagen I | Key protein of ECM synthesized during the proliferative phase |
| Collagen III | Key protein of ECM synthesized during the early proliferative phase |
| EGFR | Regulation of keratinocyte migration to wound bed |
| Endothelin-1 | Regulation of fibrosis and calcification |
| Fibronectin | ECM formation and re-epithelialization |
| Keratin-14 | Re-epithelialization |
| VEGF | Stimulation of angiogenesis |
| WISP1 | Promotion of dermal fibroblast proliferation and migration |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fadilah, N.I.M.; Isa, I.L.M.; Zaman, W.S.W.K.; Tabata, Y.; Fauzi, M.B. The Effect of Nanoparticle-Incorporated Natural-Based Biomaterials towards Cells on Activated Pathways: A Systematic Review. Polymers 2022, 14, 476. https://doi.org/10.3390/polym14030476
Fadilah NIM, Isa ILM, Zaman WSWK, Tabata Y, Fauzi MB. The Effect of Nanoparticle-Incorporated Natural-Based Biomaterials towards Cells on Activated Pathways: A Systematic Review. Polymers. 2022; 14(3):476. https://doi.org/10.3390/polym14030476
Chicago/Turabian StyleFadilah, Nur Izzah Md, Isma Liza Mohd Isa, Wan Safwani Wan Kamarul Zaman, Yasuhiko Tabata, and Mh Busra Fauzi. 2022. "The Effect of Nanoparticle-Incorporated Natural-Based Biomaterials towards Cells on Activated Pathways: A Systematic Review" Polymers 14, no. 3: 476. https://doi.org/10.3390/polym14030476
APA StyleFadilah, N. I. M., Isa, I. L. M., Zaman, W. S. W. K., Tabata, Y., & Fauzi, M. B. (2022). The Effect of Nanoparticle-Incorporated Natural-Based Biomaterials towards Cells on Activated Pathways: A Systematic Review. Polymers, 14(3), 476. https://doi.org/10.3390/polym14030476










