The Current State of Evidence Regarding Audiologist-Provided Cognitive Behavioural Therapy for the Management of Tinnitus: A Scoping Review
Abstract
1. Introduction
- To identify all sources of evidence relating to Audiologist-provided CBT, in order to determine the volume, range, and type of evidence available, identify any gaps in the current literature, and provide recommendations for future research;
- To map details relating to (a) the content and structure of Audiologist-provided CBT programs (procedural details), and (b) how research has been conducted on this topic (study details), in order to inform future research.
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.2.1. Population, Concept, and Context
2.2.2. Types of Sources
2.2.3. Other
2.3. Information Sources
2.4. Search
2.5. Selection of Sources of Evidence
2.6. Data Charting
2.7. Data Items
2.8. Synthesis of Results
3. Results
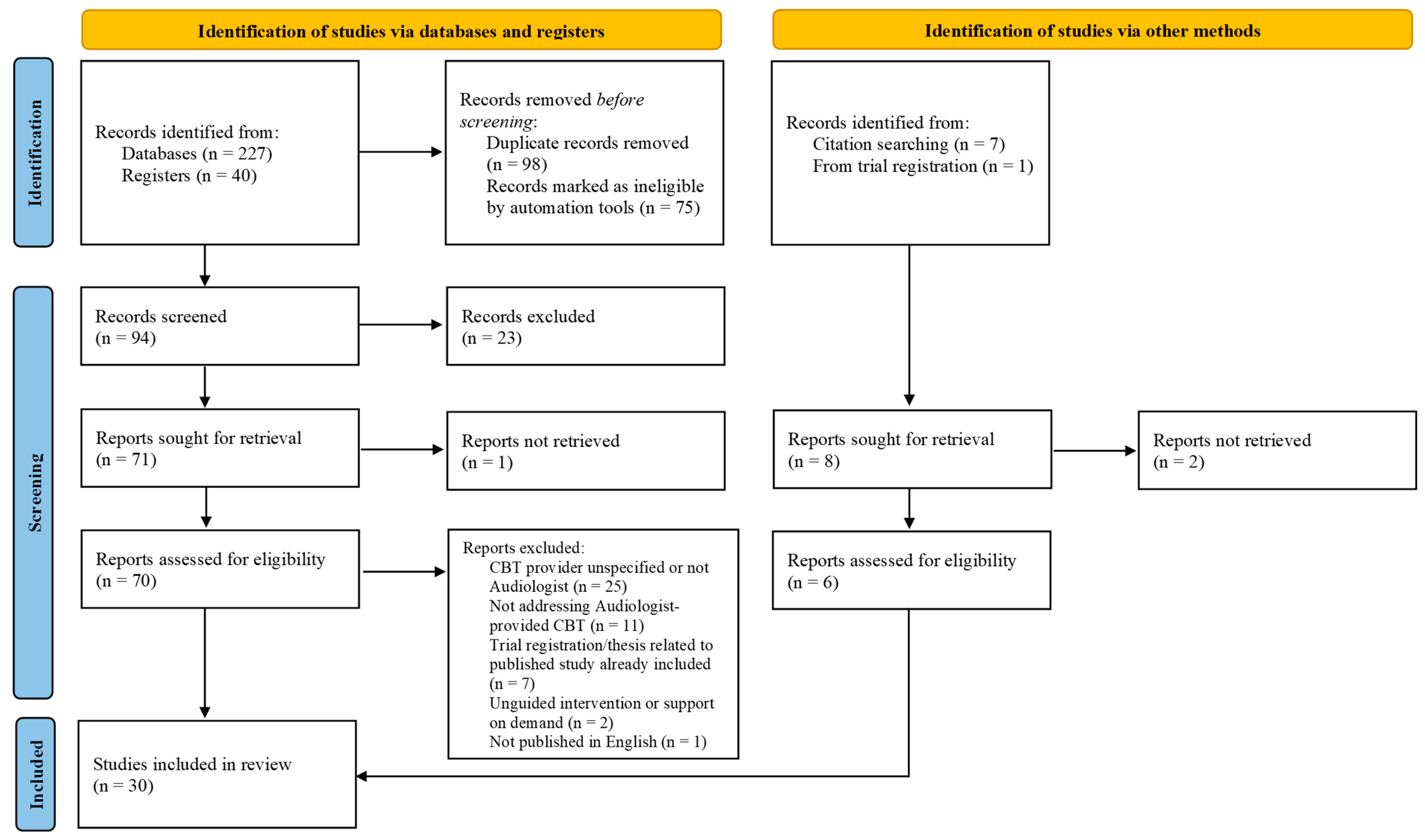
3.1. Selection of Sources of Evidence
3.2. Characteristics of Sources of Evidence
3.3. Results of Individual Sources of Evidence
3.4. Synthesis of Results
3.4.1. Key Characteristics
Setting, Unit, and Mode of Delivery
Dosage
Training and Role of Audiologists
Intervention Content
| Group of CBT studies led by Aazh: Aazh et al. [29]; Aazh and Moore [30]; Aazh, Bryant, and Moore [32] | ||||
| CBT Techniques Included | Training Received to Provide CBT | Details of Delivery | Dosage | Outcomes Assessed (Measure Used) |
| Socratic questioning, guided discovery, behavioural experiments, education, and filling in diaries of thoughts and feelings. | Attendance at a tinnitus master class which included elements of CBT, counselling, and motivational interviewing training. This involved 30 h of direct contract, 120 h of independent learning, 6 months of observation and supervised clinical practice, and ongoing coaching, support, clinical supervision, and informal training. | Setting: Audiology department of one NHS hospital Unit: Individual sessions Mode: Face-to-face Role of audiologists: To deliver all parts of the intervention | Six 1-h CBT sessions were provided across a 2–4-month time period, with typically one session per week. | Aazh et al. [28]; Aazh and Moore [29] Tinnitus severity (THI), hyperacusis severity (HQ), depression (HADS), tinnitus qualities (VAS loudness, annoyance, and effect on life), insomnia (ISI) |
| Aazh, Bryant, and Moore [31] Tinnitus severity (THI), hyperacusis severity (HQ), general anxiety (GAD-7), depression (PHQ-9), tinnitus qualities (VAS loudness, annoyance, and effect on life), insomnia (ISI) | ||||
| Group of CBT studies led by Beukes: UK-based studies: Beukes et al. [34]; Beukes, Baguley, et al. [35]; Beukes, Allen, et al. [36]; Beukes, Manchaiah, Baguley, et al. [37]; Beukes, Manchaiah, Davies, et al. [38]; Beukes, Andersson, et al. [39] USA-based studies: Beukes et al. [40]; Beukes et al. [41]; Beukes, Andersson, and Manchaiah [43]; Beukes, Andersson, Fagelson, and Manchaiah [44]; Beukes, Andersson, and Manchaiah [45] Related protocol: Beukes et al. [33] | ||||
| CBT Techniques Included | Training Received to Provide CBT | Details of Delivery | Dosage | Outcomes Assessed (Measure Used) |
| Recommended modules: Tinnitus overview, deep relaxation, positive imagery, diaphragmatic breathing, reinterpreting tinnitus, focusing techniques, rapid relaxation, thought analysis, relaxation in daily routines, relaxation in stressful situations, cognitive restructuring, exposure to tinnitus, reviewing helpful techniques, and maintenance and relapse preventio (additional mindfulness module in USA-based studies only). Optional modules: Sound enrichment, sleep guidelines, concentration tips, reducing sound sensitivity, and hearing tactics. | No formal CBT training. Supervision was provided by a clinical psychologist who was experienced in tinnitus management. | Setting: Online Unit: Individual Mode: Internet-based modules Role of audiologist: To guide participants to self-direct the intervention. Audiologists contacted participants, introduced module content, monitored progress, gave feedback and encouragement, and answered questions. | 2–3 modules were released weekly over an 8-week period. Each module involved 10–20 min of reading and additional daily practising. | UK-based studies Tinnitus severity (TFI), general anxiety (GAD-7), depression (PHQ-9), insomnia (ISI), hyperacusis severity (HQ), hearing handicap (HHIA-S), quality of life (SWLS), and cognitive function (CFQ) USA-based studies Tinnitus severity (TFI), general anxiety (GAD-7), depression (PHQ-9), insomnia (ISI), cognitions related to tinnitus (TCQ), HRQoL (EQ-5D-5L), and tinnitus, hearing, and hyperacusis-related problems (THS) |
| Individual study: Tay [52] | ||||
| CBT Techniques Included | Training Received to Provide CBT | Details of Delivery | Dosage | Outcomes Assessed (Measure Used) |
| Behavioural exposure techniques, mindfulness-based stress reduction, relaxation exercises, cognitive restructuring, sound enrichment, refocusing, concentration tips, and identifying negative thinking patterns. | No specific CBT training was reported. | Setting: Online Unit: Individual Mode: Internet or app-based modules Role of audiologist: To guide participants to self-direct the intervention and to assist in some CBT exercises e.g., facilitating the identification of negative thoughts | Not reported | Tinnitus severity (TFI, THI, and TRQ) |
| Individual study: Taylor et al. [54] Related protocol: Taylor et al. [53] | ||||
| CBT Techniques Included | Training Received to Provide CBT | Details of Delivery | Dosage | Outcomes Assessed (Measure Used) |
| Goal-setting, rapid relaxation, managing fear and avoidance behaviours, changing unhelpful negative thoughts and beliefs, promotion of physical exercise, promotion of good sleep habits, sound enrichment, and attention, monitoring, and acceptance. | Attendance at a 2-day workshop and use of a specially designed manual. | Setting: Audiology department of three NHS hospitals Unit: Individual Mode: Face-to-face Role of audiologist: To deliver all parts of the intervention | 1–3 CBT sessions (mean = 2.75) were provided. The frequency and length of the sessions were not reported. | Tinnitus severity (TFI), cognitions related to tinnitus (TCQ), and psychological well being and distress (CORE-OM). |
| Author (Year) | Eligibility Criteria | Participant Characteristics | |
|---|---|---|---|
| Sample size and demographic information | Tinnitus severity and duration at baseline | ||
| Aazh et al. (2016) [29] | Not applicable | Sample size: N = 92 Age: M = 62 years (SD = 15) Gender: 63%m, 37%f | THI: M = 47 (SD = 24) Duration: M = 10 years (SD = 10) |
| Aazh and Moore (2018) [30] | Not applicable | Sample size: N = 68 Age: M = 53 years (SD = 13) Gender: 57%f, 43%m | THI: M = 61 (SD = 18) Duration: Not reported |
| Aazh, Bryant, and Moore (2019) [32] | Not applicable | Sample size: N = 40 Age: M = 48 years (SD = 14) Gender: 55%f, 45%m | THI: M = 62 (SD = 16) Duration: Not reported |
| Beukes et al. (2017) [34] | Inclusion criteria: Aged ≥ 18 years; living in the UK; ability to read and type in English; tinnitus duration of ≥3 months. Exclusion criteria: Major self-reported medical or psychiatric disorder; uninvestigated tinnitus of a pulsatile, objective, or unilateral nature; tinnitus resulting from a medical disorder; undergoing any tinnitus therapy. | Sample size: N = 37 Age: M age range = 50-59 years (SD = 1) Gender: 51%f, 49%m | TFI: M = 56 (SD = 18) THI-S: M = 23 (SD = 8) Duration: Mo = 1-5 years |
| Beukes, Baguley, et al. (2018) [35]; Beukes, Manchaiah, Baguley, et al. (2018) [37] | Inclusion criteria: Aged ≥ 18 years; living in the UK; ability to read and type in English; tinnitus duration of at least 3 months; TFI score of ≥25. Exclusion criteria: Major self-reported medical, psychiatric, or mental disorder; uninvestigated tinnitus of a pulsatile, objective, or unilateral nature; tinnitus resulting from a medical disorder still under investigation; undergoing any tinnitus therapy. | Sample size: N = 146 Age: M = 56 years (SD = 13) Gender: 57%m, 43%f | TFI: M = 60 (SD = 18) Duration: M = 12 years (SD = 12) |
| Beukes, Allen, et al. (2018) [36] | Inclusion criterion: Completed iCBT intervention reported in Beukes, Baguley, et al. (2018). | Sample size: N = 139 Age: M = 58 years (SD = 13) Gender: 56%m, 44%f | TFI: M = 59 (SD = 17) Duration: M = 12 years (SD = 11) |
| Beukes, Manchaiah, Davies, et al. (2018) [38] | Inclusion criterion: Completed iCBT intervention reported in Beukes, Baguley, et al. (2018). | Sample size: N = 15 Age: M = 59 years (SD = 8) Gender: 53%f, 47%m | TFI: M = 58 (SD = 16) Duration: M = 9 years (SD = 9) |
| Beukes, Andersson, et al. (2018) [39] | Inclusion criteria: Aged ≥ 18 years; regular access to computer and internet. Exclusion criteria: Any major self-reported medical or psychiatric conditions; undergoing any tinnitus therapy. | iCBT group Sample size: n = 46 Age: M = 51 years (SD = 12) Gender: 63%m, 37%f Face-to-face group Sample size: n = 46 Age: M = 55 years (SD = 12) Gender: 57%m, 43%f | iCBT group TFI: M = 55 (SD = 22) THI: M = 45 (SD = 23) Duration: M = 5 years (SD = 9) Face-to-face group TFI: M = 57 (SD = 21) THI: M = 47 (SD = 20) Duration: M = 8 years (SD = 10) |
| Beukes et al. (2021a) [40] | Inclusion criteria: Aged ≥ 18 years; living in Texas, USA; ability to read and type in English or Spanish; tinnitus duration of at ≥3 months; TFI score of ≥25. Exclusion criteria: PHQ-9 scores of ≥15; major self-reported medical or psychiatric disorder; tinnitus of a pulsatile, objective, or unilateral nature which is uninvestigated or currently under investigation; undergoing any tinnitus therapy. | Sample size: N = 27 Age: M = 56 years (SD = 10) Gender: 67%f, 33%m | TFI: M = 58 years (SD = 15) Duration: M = 12 years (SD = 13) |
| Beukes et al. (2021b) [41] | Inclusion criteria: Aged ≥ 18 years; living in Texas, USA; ability to read and type in English; access to a computer, internet, and email; self-perceived need of tinnitus intervention. Exclusion criteria: Major self-reported medical condition or treatment; tinnitus of a pulsatile, objective, or unilateral nature which is uninvestigated or currently under investigation; undergoing tinnitus therapy. | iCBT group Sample size: n = 63 Age: M = 55 years (SD = 13) Gender: 59%f, 41%m Relaxation group Sample size: n = 63 Age: M = 57 years (SD = 13) Gender: 60%m, 40%f | iCBT group TFI: M = 50 (SD = 27) Duration: M = 10 years (SD = 11) Relaxation group TFI: M = 49 (SD = 26) Duration: M = 15 years (SD = 14) |
| Beukes, Andersson, Fagelson, and Manchaiah (2022) [44]; Beukes, Andersson, and Manchaiah (2021) [43] | As described in Beukes et al. (2021a). | Sample size: N = 158 Age: M = 57 years (SD = 12) Gender: 51%f, 49%m | TFI: Not reported Duration: M = 14 years (SD = 14) |
| Beukes, Andersson, and Manchaiah (2022) [45] | Inclusion criterion: Completed iCBT intervention reported in Beukes et al. (2021b) or Beukes, Andersson, Fagelson, & Manchaiah (2022). | Sample size: N = 132 Age: M = 56 years (SD = 13) Gender: 56%f, 44%m | TFI: M = 54 (SD = 21) Duration: M = 12 years (SD = 15) |
| Taylor et al. (2020) [53] | Inclusion criteria: Aged ≥ 18 years; capacity to consent; sufficient mobility to attend clinics; TFI score ≥ 25; willing to share experiences of participating. Exclusion criteria: Tinnitus with a medically treatable origin; unable to communicate in English; participated in other tinnitus management research after consenting to this study. | Manualized psychological care group Sample size: n = 11 Age: M = 59 years (SD = 11) Gender: 70%m, 30%f Treatment as usual group Sample size: n = 8 Age: M = 44 years (SD = 18) Gender: 63%m, 37%f | Manualized psychological care group TFI: M = 67 (SD = 24) Duration: Not reported Treatment as usual group TFI: M = 50 (SD = 24) Duration: Not reported |
| Tay (Unpublished work) [51] | Inclusion criteria: Aged ≥ 18 years; living in the Republic of Indonesia; ability to read and type in Bahasa Indonesia or English; referred by appropriately certified healthcare professional; TFI score of ≥50. Exclusion criteria: None reported. | Sample size: N = 40 Age: M = 47 years (SD = 16) Gender: 63%m, 38%f | TFI: M = 60 (SD = 5) Duration: M = 16 years (SD = 13) |
Outcome Assessment
3.4.2. Study Details
CBT Participants
Intervention Comparators
4. Discussion
4.1. Summary of Evidence
4.2. Directions for Future Research
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
- Tinnitus [MeSH term]
- Tinnit*
- 1 OR 2
- Audiologist-led
- Audiologist-supported
- Audiologist-delivered
- Audiologist-guided
- 4 OR 5 OR 6 OR 7
- Cognitive behavioral therapy [MeSH term]
- 1Cognit* AND behav*
- 9 OR 10
- 3 AND 8 AND 11
Appendix B
Appendix C
| Title of paper: | |
| Authors: | |
| Year of publication: | |
| Country of Origin: | |
| Type of source: | |
| Aims/purpose: | |
Population and sample size within the source of evidence (if applicable):
| |
| Methodology/methods: | |
Intervention type, comparator, and details of these:
| |
| Outcomes measured, when they were measured, and how they were measured (if applicable): |
References
- Cima, R.F.F.; Mazurek, B.; Haider, H.; Kikidis, D.; Lapira, A.; Noreña, A.; Hoare, D.J. A multidisciplinary European guideline for tinnitus: Diagnostics, assessment, and treatment. HNO 2019, 67 (Suppl. S1), 10–42. [Google Scholar] [CrossRef] [PubMed]
- McCormack, A.; Edmondson-Jones, M.; Somerset, S.; Hall, D. A systematic review of the reporting of tinnitus prevalence and severity. Hear. Res. 2016, 337, 70–79. [Google Scholar] [CrossRef]
- Biswas, R.; Lugo, A.; Akeroyd, M.A.; Schlee, W.; Gallus, S.; Hall, D.A. Tinnitus prevalence in Europe: A multi-country cross-sectional population study. Lancet 2021, 12, 100250. [Google Scholar] [CrossRef] [PubMed]
- Gu, H.; Kong, W.; Yin, H.; Zheng, Y. Prevalence of sleep impairment in patients with tinnitus: A systematic review and single-arm meta-analysis. Eur. Arch. Otorhinolaryngol. 2021, 279, 2211–2221. [Google Scholar] [CrossRef] [PubMed]
- Clarke, N.A.; Henshaw, H.; Akeroyd, M.A.; Adams, B.; Hoare, D.J. Associations between subjective tinnitus and cognitive performance: Systematic review and meta-analysis. Trends Hear. 2020, 24, 2331216520918416. [Google Scholar] [CrossRef] [PubMed]
- Pinto, P.C.L.; Marcelos, C.M.; Mezzasalma, M.A.; Osterne, F.J.V.; Melo Tavares de Lima, M.A.; Nardi, A.E. Tinnitus and its association with psychiatric disorders: Systematic review. J. Laryngol. Otol. 2014, 128, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Salazar, J.W.; Meisel, K.; Smith, E.R. Depression in patients with tinnitus: A systematic review. Otolaryngol. Head. Neck Surg. 2019, 161, 28–35. [Google Scholar] [CrossRef] [PubMed]
- McKenna, L.; Handscomb, L.; Hoare, D.J.; Hall, D.A. A scientific cognitive-behavioral model of tinnitus: Novel conceptualizations of tinnitus distress. Front. Neurol. 2014, 5, 196. [Google Scholar] [CrossRef] [PubMed]
- Fuller, T.; Cima, R.; Langguth, B.; Mazurek, B.; Vlaeyen, J.W.S.; Hoare, D.J. Cognitive behavioural therapy for tinnitus (review). Cochrane Database Sys Rev. 2020, 1, CD012614. [Google Scholar] [CrossRef]
- Martinez Devesa, P.; Waddell, A.; Perera, R.; Theodoulou, M. Cognitive behavioural therapy for tinnitus. Cochrane Database Sys Rev. 2007, 1, CD005233. [Google Scholar] [CrossRef]
- Hesser, H.; Weise, C.; Westin, V.Z.; Andersson, G. A systematic review and meta-analysis of randomized controlled trials of cognitive-behavioral therapy for tinnitus distress. Clin. Psychol. Rev. 2011, 31, 545–553. [Google Scholar] [CrossRef]
- British Society of Audiology. Practice Guidance: Tinnitus in Adults. 2021. Available online: https://www.thebsa.org.uk/wp-content/uploads/2023/10/OD104-95-BSA-practice-guidance-Tinnitus-in-adults-Publication-Nov-2021-1.pdf (accessed on 15 January 2024).
- National Institute for Health and Care Excellence. Tinnitus: Assessment and Management. 2020. Available online: https://www.nice.org.uk/guidance/ng155/chapter/Recommendations#management-of-tinnitus (accessed on 15 January 2024).
- McFerran, D.; Hoare, D.J.; Carr, S.; Ray, J.; Stockdale, D. Tinnitus services in the United Kingdom: A survey of patient experiences. BMC Health Serv. Res. 2018, 18, 110. [Google Scholar] [CrossRef]
- Hoare, D.J.; Broomhead, E.; Stockdale, D.; Kennedy, V. Equity and person-centeredness in provision of tinnitus services in UK National Health Service audiology departments. Eur. J. Pers. Cent. Healthc. 2015, 3, 318–326. [Google Scholar] [CrossRef]
- Gander, P.E.; Hoare, D.J.; Collins, L.; Smith, S.; Hall, D.A. Tinnitus referral pathways within the National Health Service in England: A survey of their perceived effectiveness among audiology staff. BMC Health Serv. Res. 2011, 11, 162. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Provision of services for adults with tinnitus. In A Good Practice Guide; Central Office of Information: London, UK, 2009. [Google Scholar]
- Kilroy, N.; El Refaie, A. Tinnitus management in Ireland: A pilot study of general practitioners. Ir. J. Med. Sci. 2020, 189, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.M.; Hall, D.A.; Walker, D.M.; Hoare, D.J. Psychological therapy for people with tinnitus: A scoping review of treatment components. Ear Hear. 2017, 38, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef] [PubMed]
- Hall, D.A.; Mohamad, N.; Firkins, L.; Fenton, M.; Stockdale, D. Identifying and prioritizing unmet research questions for people with tinnitus: The James Lind Alliance Tinnitus Priority Setting Partnership. Clin. Investig. 2013, 3, 21–28. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Khalil, H.; Peters, M.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Parker, D. An evidence-based approach to scoping reviews. Worldviews Evid. Based Nurs. 2016, 13, 118–123. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’ Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Pieper, D.; Puljak, L. Language restrictions in systematic reviews should not be imposed in the search strategy but in the eligibility criteria if necessary. J. Clin. Epidemiol. 2021, 132, 146–147. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Lockwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. JBI Manual for Evidence Synthesis. 2024. Available online: https://jbi-global-wiki.refined.site/space/MANUAL (accessed on 15 February 2024). [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Aazh, H.; Moore, B.C.; Lammaing, K.; Cropley, M. Tinnitus and hyperacusis therapy in a UK National Health Service audiology department: Patients’ evaluations of the effectiveness of treatments. Int. J. Audiol. 2016, 55, 514–522. [Google Scholar] [CrossRef]
- Aazh, H.; Moore, B.C.J. Effectiveness of audiologist-delivered cognitive behavioral therapy for tinnitus and hyperacusis rehabilitation: Outcomes for patients treated in routine practice. Am. J. Audiol. 2018, 27, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Aazh, H.; Landgrebe, M.; Danesh, A.A.; Moore, B.C. Cognitive behavioral therapy for alleviating the distress caused by tinnitus, hyperacusis and misophonia: Current perspectives. Psychol. Res. Behav. Manag. 2019, 12, 991–1002. [Google Scholar] [CrossRef] [PubMed]
- Aazh, H.; Bryant, C.; Moore, B.C.J. Patients’ perspectives about the acceptability and effectiveness of audiologist-delivered cognitive behavioral therapy for tinnitus and/or hyperacusis rehabilitation. Am. J. Audiol. 2019, 28, 973–985. [Google Scholar] [CrossRef]
- Beukes, E.W.; Manchaiah, V.; Allen, P.M.; Baguley, D.M.; Andersson, G. Internet-based cognitive behavioural therapy for adults with tinnitus in the UK: Study protocol for a randomised controlled trial. BMJ Open 2015, 5, e008241. [Google Scholar] [CrossRef]
- Beukes, E.W.; Allen, P.M.; Manchaiah, V.; Baguley, D.M.; Andersson, G. Internet-based intervention for tinnitus: Outcome of a single-group open trial. J. Am. Acad. Audiol. 2017, 28, 340–351. [Google Scholar] [CrossRef]
- Beukes, E.W.; Baguley, D.M.; Allen, P.M.; Manchaiah, V.; Andersson, G. Audiologist-guided internet-based cognitive behavior therapy for adults with tinnitus in the United Kingdom: A randomized controlled trial. Ear Hear. 2018, 39, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.W.; Allen, P.M.; Baguley, D.M.; Manchaiah, V.; Andersson, G. Long-term efficacy of audiologist-guided internet-based cognitive behavior therapy for tinnitus. Am. J. Audiol. 2018, 27, 431–447. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.W.; Manchaiah, V.; Baguley, D.M.; Allen, P.M.; Andersson, G. Process evaluation of internet-based cognitive behavioural therapy for adults with tinnitus in the context of a randomised control trial. Int. J. Audiol. 2018, 57, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.W.; Manchaiah, V.; Davies, A.S.A.; Allen, P.M.; Baguley, D.M.; Andersson, G. Participants’ experiences of an internet-based cognitive behavioural therapy intervention for tinnitus. Int. J. Audiol. 2018, 57, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.W.; Andersson, G.; Allen, P.M.; Manchaiah, V.; Baguley, D.M. Effectiveness of guided internet-based cognitive behavioral therapy vs face-to-face clinical care for treatment of tinnitus: A randomized clinical trial. JAMA Otolaryngol. Head. Neck Surg. 2018, 144, 1126–1133. [Google Scholar] [CrossRef]
- Beukes, E.W.; Andersson, G.; Fagelson, M.; Manchaiah, V. Audiologist-supported internet-based cognitive behavioral therapy for tinnitus in the United States: A pilot trial. Am. J. Audiol. 2021, 30, 717–729. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.W.; Andersson, G.; Fagelson, M.A.; Manchaiah, V. Dismantling internet-based cognitive behavioral therapy for tinnitus. The contribution of applied relaxation: A randomized controlled trial. Internet Interv. 2021, 25, 100402. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.; Andersson, G.; Manchaiah, V.; Kaldo, V. Cognitive Behavioural Therapy for Tinnitus; Plural Publishing: San Diego, CA, USA, 2021. [Google Scholar]
- Beukes, E.W.; Andersson, G.; Manchaiah, V. Patient uptake, experiences, and process evaluation of a randomized controlled trial of internet-based cognitive behavioral therapy for tinnitus in the United States. Front. Med. 2021, 8, 771646. [Google Scholar] [CrossRef]
- Beukes, E.W.; Andersson, G.; Fagelson, M.; Manchaiah, V. Internet-based audiologist-guided cognitive behavioral therapy for tinnitus: Randomized controlled trial. J. Med. Internet Res. 2022, 24, e27584. [Google Scholar] [CrossRef]
- Beukes, E.W.; Andersson, G.; Manchaiah, V. Long-term efficacy of audiologist-guided internet-based cognitive behaviour therapy for tinnitus in the United States: A repeated-measures design. Internet Interv. 2022, 30, 100583. [Google Scholar] [CrossRef]
- Beukes, E.W.; Manchaiah, V. Audiologist-delivered cognitive behavioral therapy for tinnitus. In Tinnitus: Advances in Prevention, Assessment, and Management; Plural Publishing: San Diego, CA, USA, 2022; pp. 193–208. [Google Scholar]
- Henry, J.A.; Zaugg, T.L.; Myers, P.J.; Kendall, C.J.; Turbin, M.B. Principles and application of educational counseling used in progressive audiologic tinnitus management. Noise Health 2009, 11, 33–48. [Google Scholar] [CrossRef]
- Henry, J.A.; Goodworth, M.C.; Lima, E.; Zaugg, T.; Thielman, E.J. Cognitive behavioral therapy for tinnitus: Addressing the controversy of its clinical delivery by audiologists. Ear Hear. 2022, 43, 283–289. [Google Scholar] [CrossRef] [PubMed]
- McFerran, D.J.; Baguley, D.M. Is psychology really the best treatment for tinnitus? Clin. Otolaryngol. 2009, 34, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Sweetow, R.W. Cognitive aspects of tinnitus patient management. Ear Hear. 1986, 7, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Sweetow, R.W. Cognitive-behavior modification. In Tinnitus Handbook; Tyler, R.S., Ed.; Singular Publishing Group: San Diego, CA, USA, 2000; pp. 297–311. [Google Scholar]
- Tay, K.W. Internet-based cognitive behavioural therapy (ICBT) as an effective treatment alternative to tinnitus management: An empirical research. Sci. Prepr. 2022; preprint. [Google Scholar] [CrossRef]
- Taylor, J.A.; Hall, D.A.; Walker, D.M.; McMurran, M.; Casey, A.; Stockdale, D.; Featherstone, D.; Thompson, D.M.; MacDonald, C.; Hoare, D.J. A psychologically informed, audiologist-delivered, manualised intervention for tinnitus: Protocol for a randomised controlled feasibility trial (TinMan study). Pilot. Feasibility Stud. 2017, 3, 24. [Google Scholar] [CrossRef]
- Taylor, J.A.; Thompson, D.M.; Hall, D.A.; Walker, D.M.; McMurran, M.; Casey, A.; Featherstone, D.; MacDonald, C.; Stockdale, D.; Hoare, D.J. The TinMan study: Feasibility trial of a psychologically informed, audiologist-delivered, manualised intervention for tinnitus. Int. J. Audiol. 2020, 59, 905–914. [Google Scholar] [CrossRef]
- Thompson, D.M. The sound—And the curing. ASHA Lead. 2017, 22, 16–18. [Google Scholar] [CrossRef]
- Thompson, D.M.; Taylor, J.; Hall, D.A.; Walker, D.M.; McMurran, M.; Casey, A.; Stockdale, D.; Featherstone, D.; Hoare, D.J. Patients’ and clinicians’ views of the psychological components of tinnitus treatment that could inform audiologists’ usual care: A delphi survey. Ear Hear. 2018, 39, 367–377. [Google Scholar] [CrossRef]
- Tyler, R.S.; Stouffer, J.L.; Schum, R. Audiological rehabilitation of the tinnitus client. J. Acad. Rehabil. Audiol. 1989, 22, 30–42. [Google Scholar]
- Translation and Validation of Internet Based Cognitive Behavioural Therapy (iCBT) for Tinnitus in Tamil, Kannada and Hindi—CBTIL [Clinical Trial Registration]. World Health Organization International Clinical Trials Registry Platform Identifier: CTRI/2020/10/028701. Posted October 28, 2020. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2020/10/028701 (accessed on 15 February 2024).
- Broadbent, D.E.; Cooper, P.F.; FitzGerald, P.; Parkes, K.R. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br. J. Clin. Psychol. 1982, 21, 1–16. [Google Scholar] [CrossRef]
- Barkham, M.; Mellor-Clark, J.; Connell, J.; Cahill, J. A core approach to practice-based evidence: A brief history of the origins and applications of the CORE-OM and CORE system. Couns. Psychother. Res. 2006, 6, 3–15. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.W.; Jacobson, G.P.; Hug, G.A.; Weinstein, B.E.; Malinoff, R.L. Practical method for quantifying hearing aid benefit in older adults. J. Am. Acad. Audiol. 1991, 2, 70–75. [Google Scholar]
- Khalfa, S.; Dubal, S.; Veuillet, E.; Perez-Diaz, F.; Jouvent, R.; Collet, L. Psychometric Normalization of a Hyperacusis Questionnaire. ORL J. Otorhinolaryngol. Relat. Spec. 2002, 64, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep. Med. 2001, 2, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Wilson, P.H.; Henry, J.L. Tinnitus Cognitions Questionnaire: Development and psychometric properties of a measure of dysfunctional cognitions associated with tinnitus. Int. Tinnitus J. 1989, 4, 23–30. [Google Scholar]
- Meikle, M.B.; Henry, J.A.; Griest, S.E.; Stewart, B.J.; Abrams, H.B.; McArdle, R.; Myers, P.J.; Newman, C.W.; Sandridge, S.; Turk, D.C.; et al. The Tinnitus Functional Index: Development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012, 33, 153–176. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.W.; Jacobson, G.P.; Spitzer, J.B. Development of the Tinnitus Handicap Inventory. Arch. Otolaryngol. Head. Neck Surg. 1996, 122, 143–148. [Google Scholar] [CrossRef]
- Henry, J.A.; Griest, S.; Zaugg, T.L.; Thielman, E.; Kaelin, C.; Galvez, G.; Carlson, K.F. Tinnitus and Hearing Survey: A screening tool to differentiate bothersome tinnitus from hearing difficulties. Am. J. Audiol. 2015, 24, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.H.; Henry, J.; Bowen, M.; Haralambous, G. Tinnitus Reaction Questionnaire: Psychometric properties of a measure of distress associated with tinnitus. J. Speech Lang. Hear. Res. 1991, 34, 197–201. [Google Scholar] [CrossRef]
- Maxwell, C. Sensitivity and accuracy of the Visual Analogue Scale: A psycho-physical classroom experiment. Br. J. Clin. Pharmacol. 1978, 6, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.W.; Sandridge, S.A.; Bolek, L. Development and psychometric adequacy of the screening version of the Tinnitus Handicap Inventory. Otol. Neurotol. 2008, 29, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Hall, D.A.; Smith, H.; Hibbert, A.; Colley, V.; Haider, H.F.; Horobin, A.; Londero, A.; Mazurek, B.; Thacker, B.; Fackrell, K.; et al. The COMiT’ID study: Developing core outcome domains sets for clinical trials of sound-, psychology-, and pharmacology-based interventions for chronic subjective tinnitus in adults. Trends Hear. 2018, 22, 2331216518814384. [Google Scholar] [CrossRef]
- Stewart, L.; Moher, D.; Shekelle, P. Why prospective registration of systematic reviews makes sense. Syst. Rev. 2012, 1, 7. [Google Scholar] [CrossRef]
| Authors (Year) | Source Type | Aims as They Related to This Review | Study Design | Country of Conduct |
|---|---|---|---|---|
| Aazh et al. (2016) [29] | Research article | To assess patients’ opinions on the effectiveness of an Audiologist-provided CBT program for tinnitus and hyperacusis. | Service evaluation using cross-sectional surveys. | UK |
| Aazh and Moore (2018) [30] | Research article | To evaluate the efficacy of an Audiologist-provided CBT program for tinnitus and hyperacusis. | Service evaluation using a single group pre-test/post-test design. | UK |
| Aazh, Landgrebe, et al. (2019) [31] | Literature review | To review the body of literature relating to the efficacy of CBT for managing tinnitus and hyperacusis. | --- | --- |
| Aazh, Bryant, and Moore (2019) [32] | Research article | To assess participants’ views on the effectiveness and acceptability of an Audiologist-provided CBT program for tinnitus and hyperacusis. | Service evaluation using cross-sectional surveys. | UK |
| Beukes et al. (2015) [33] | Clinical trial protocol | Protocol for an RCT to assess the efficacy of Audiologist-guided iCBT in improving tinnitus outcomes. | --- | --- |
| Beukes et al. (2017) [34] | Research article | To assess the feasibility of an Audiologist-guided iCBT intervention for tinnitus prior to undertaking an RCT. | Single group pre-test/post-test design. | UK |
| Beukes, Baguley, et al. (2018) [35] | Research article | To assess the efficacy of an Audiologist-guided iCBT intervention for tinnitus vs. weekly monitoring. | Two-arm delayed intervention RCT. | UK |
| Beukes, Allen, et al. (2018) [36] | Research article | To investigate the long-term effects of an Audiologist-guided iCBT intervention for tinnitus at 1-year post intervention. | Repeated measures design. | UK |
| Beukes, Manchaiah, Baguley, et al. (2018) [37] | Research article | To identify processes which facilitate or hinder implementation of Audiologist-guided iCBT intervention for tinnitus. | Process evaluation ran parallel to an RCT (Beukes, Baguley, et al., 2018). | UK |
| Beukes, Manchaiah, Davies, et al. (2018) [38] | Research article | To explore participants’ experiences of an Audiologist-guided iCBT intervention for tinnitus. | Qualitative study using semi-structured telephone interviews. | UK |
| Beukes, Andersson, et al. (2018) [39] | Research article | To assess the efficacy of an Audiologist-guided iCBT intervention vs. Audiologist-provided individualised face-to-face care for tinnitus. | Two-arm non-inferiority RCT. | UK |
| Beukes et al. (2021a) [40] | Research article | To assess the feasibility of an Audiologist-guided iCBT intervention for tinnitus prior to undertaking an RCT. | Single group pre-test/post-test design. | USA |
| Beukes et al. (2021b) [41] | Research article | To determine the individual contribution of applied relaxation within an Audiologist-provided iCBT program for tinnitus. | Two-arm parallel RCT. | USA |
| Beukes, Andersson, Manchaiah, and Kaldo (2021) [42] | Book | To describe the use of CBT in tinnitus management and its application by Audiologists, and to disseminate CBT materials which can be used by audiologists. | --- | --- |
| Beukes, Andersson, and Manchaiah (2021) [43] | Research article | To identify processes which facilitate or hinder implementation of Audiologist-guided iCBT. | Process evaluation ran parallel to an RCT (Beukes, Andersson, Fagelson, and Manchaiah, 2022). | USA |
| Beukes, Andersson, Fagelson, and Manchaiah (2022) [44] | Research article | To assess the efficacy of an Audiologist-guided iCBT intervention for tinnitus vs. weekly monitoring. | Two-arm delayed intervention RCT. | USA |
| Beukes, Andersson, and Manchaiah (2022) [45] | Research article | To investigate the long-term effects of an Audiologist-guided iCBT intervention for tinnitus at 1-year post intervention. | Repeated measures design. | USA |
| Beukes and Manchaiah (Unpublished work) [46] | Book chapter | To provide an overview of CBT management of tinnitus and the potential role for Audiologists in guiding iCBT interventions. | --- | --- |
| Henry et al. (2009) [47] | Descriptive article | To introduce and describe ‘progressive audiological tinnitus management’, a multilevel intervention which can include Audiologist-provided CBT. | --- | --- |
| Henry et al. (2022) [48] | Text/opinion piece | To present the evidence for and against Audiologist-provided CBT for tinnitus and to make recommendations for practice. | --- | --- |
| McFerran and Baguley (2009) [49] | Text/opinion piece | To highlight arguments against, and barriers to, Audiologist-provided CBT. | --- | --- |
| Sweetow (1986) [50] | Descriptive article | To introduce and describe ‘tinnitus patient management’, an intervention which can include Audiologist-provided CBT. | --- | USA |
| Sweetow (2000) [51] | Book chapter | To give an overview of CBT for tinnitus management, and to present arguments for Audiologist-provided CBT. | --- | --- |
| Tay (Unpublished work) [52] | Research article (under review) | To assess the efficacy of Audiologist-guided iCBT for tinnitus. | Non-inferiority single group pre-test/post-test design. | Indonesia |
| Taylor et al. (2017) [53] | Clinical trial protocol | Protocol for a psychologically informed, manualised, Audiologist-delivered intervention for tinnitus. | --- | --- |
| Taylor et al. (2020) [54] | Research article | To examine the acceptability and feasibility of an RCT of manualised Audiologist-provided psychological intervention (which includes CBT components). | RCT and post-test surveys and interviews to evaluate feasibility and acceptability. | UK |
| Thompson (2017) [55] | Text/opinion piece | To describe CBT as a management approach to tinnitus and to discuss the potential role of Audiologists in providing CBT. | --- | --- |
| Thompson et al. (2018) [56] | Research article | To determine which psychological components, including CBT techniques, Audiologists could and should provide. | A three-round Delphi survey. | UK |
| Tyler et al. (1989) [57] | Text/opinion piece | To advise on the assessment and management of tinnitus by Audiologists, including the potential role of Audiologists in providing CBT interventions. | --- | --- |
| Clinical trial registration ID CTRI/2020/10/028701 [58] | Clinical trial registration | To assess the acceptability and feasibility of an Audiologist-guided iCBT intervention for tinnitus after translation into three languages; Tamil, Kannada, and Hindi. | Proposed single group pre-test/post-test design. | India |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burke, L.A.; El Refaie, A. The Current State of Evidence Regarding Audiologist-Provided Cognitive Behavioural Therapy for the Management of Tinnitus: A Scoping Review. Audiol. Res. 2024, 14, 412-431. https://doi.org/10.3390/audiolres14030035
Burke LA, El Refaie A. The Current State of Evidence Regarding Audiologist-Provided Cognitive Behavioural Therapy for the Management of Tinnitus: A Scoping Review. Audiology Research. 2024; 14(3):412-431. https://doi.org/10.3390/audiolres14030035
Chicago/Turabian StyleBurke, Louise A., and Amr El Refaie. 2024. "The Current State of Evidence Regarding Audiologist-Provided Cognitive Behavioural Therapy for the Management of Tinnitus: A Scoping Review" Audiology Research 14, no. 3: 412-431. https://doi.org/10.3390/audiolres14030035
APA StyleBurke, L. A., & El Refaie, A. (2024). The Current State of Evidence Regarding Audiologist-Provided Cognitive Behavioural Therapy for the Management of Tinnitus: A Scoping Review. Audiology Research, 14(3), 412-431. https://doi.org/10.3390/audiolres14030035





