Digits-in-Noise Test as an Assessment Tool for Hearing Loss and Hearing Aids
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
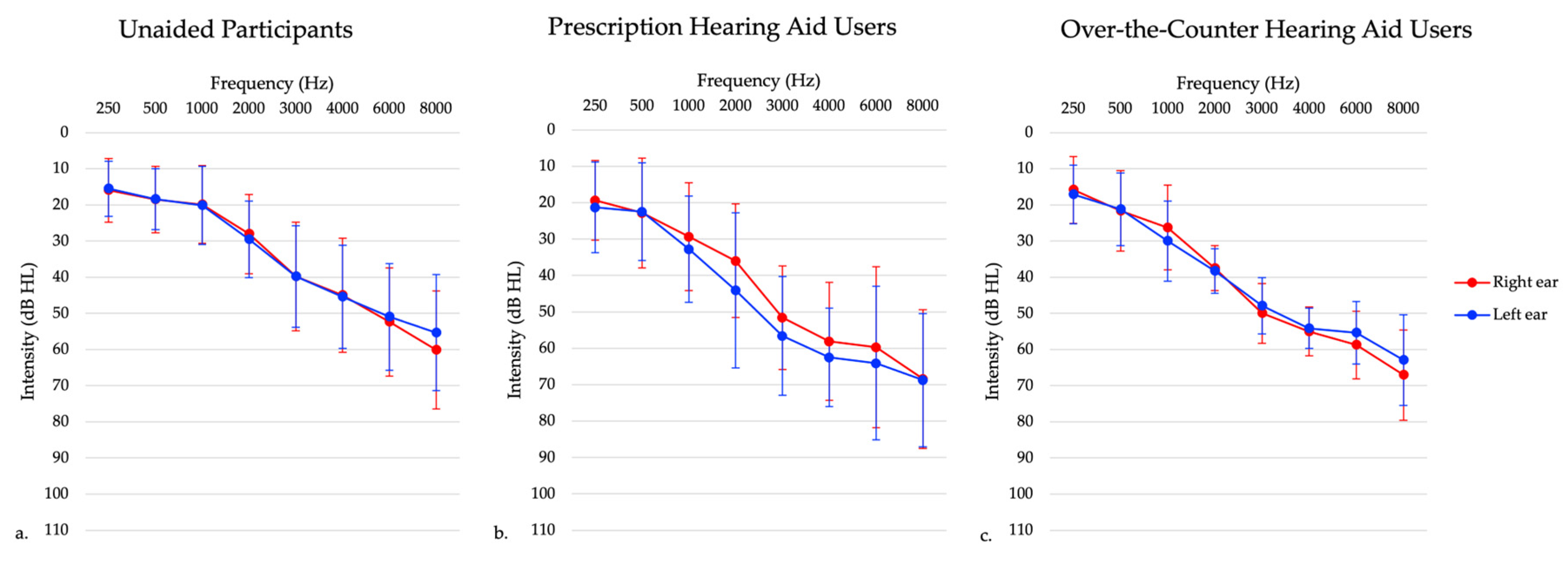
2.1.1. Experiment 1: Individuals with Untreated Hearing Loss
2.1.2. Experiment 2: Prescriptions Hearing Aid Users
2.1.3. Experiment 3: Over-the-Counter (OTC) Hearing Aid Users
2.2. Speech Intelligibility Testing
2.3. Statistical Analysis
3. Results
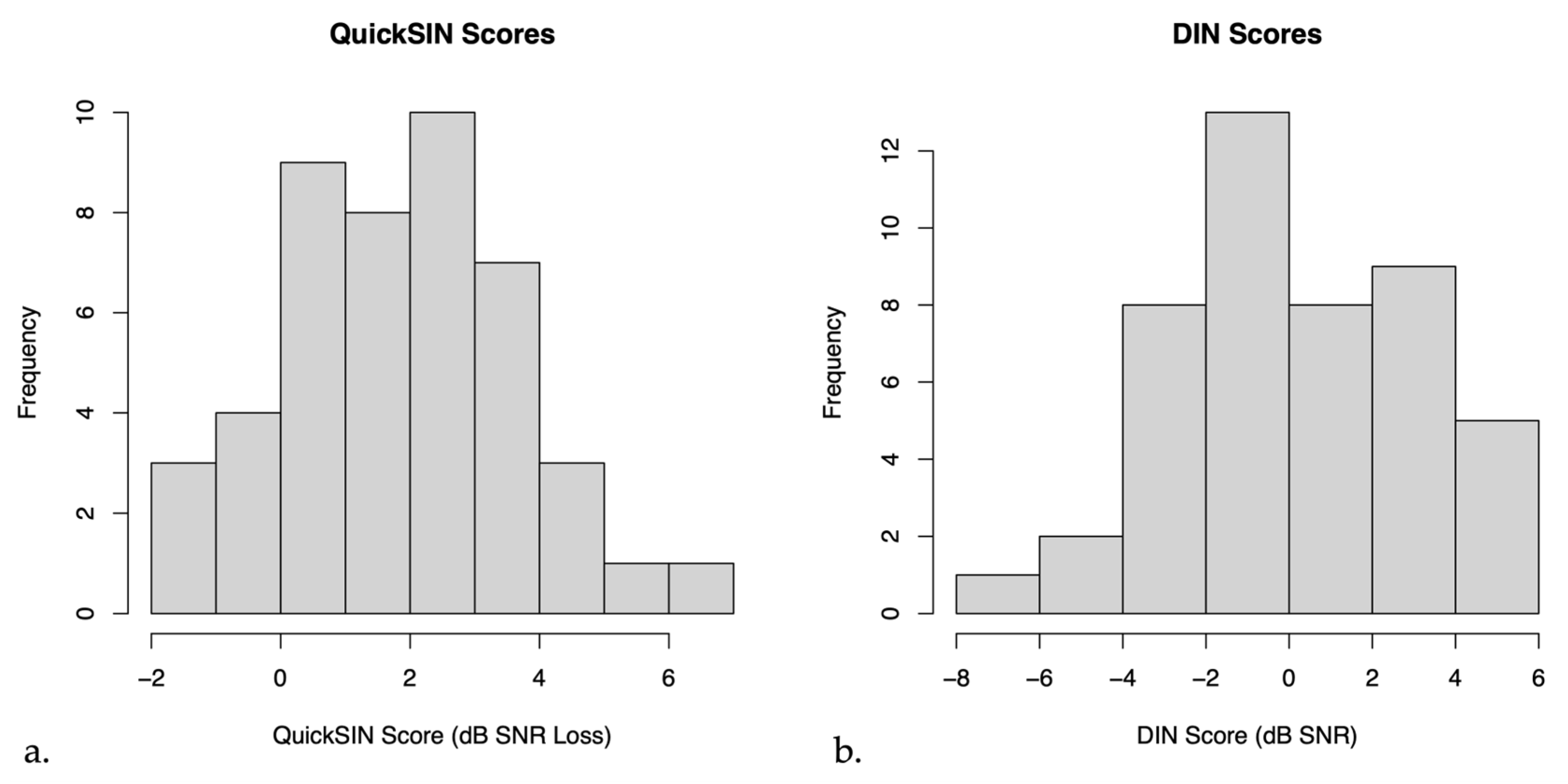
3.1. Experiment 1: Individuals with Untreated Hearing Loss
3.2. Experiment 2: Prescription Hearing Aid Users
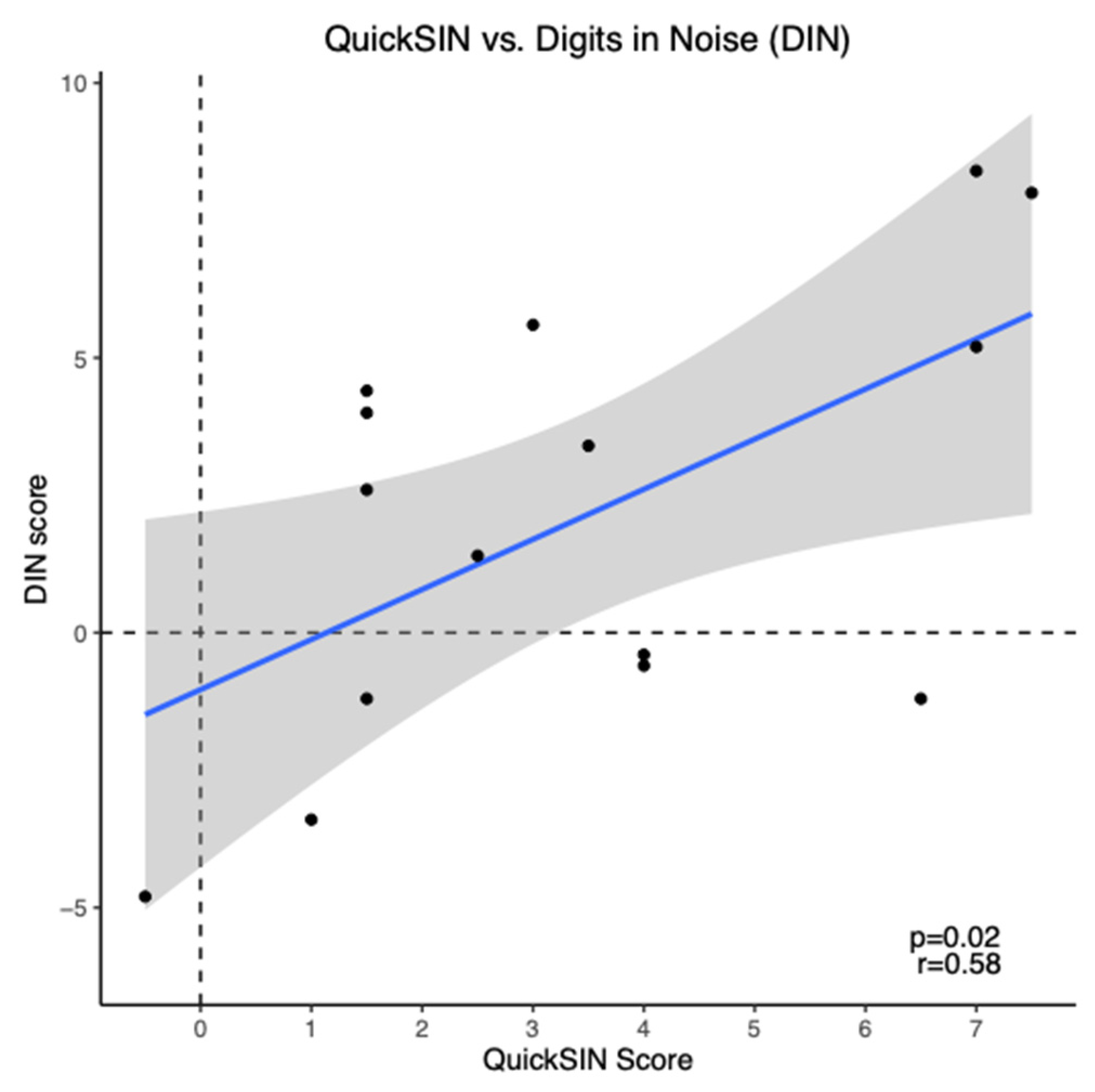
3.3. Experiment 3: Over-the-Counter Hearing Aid Users
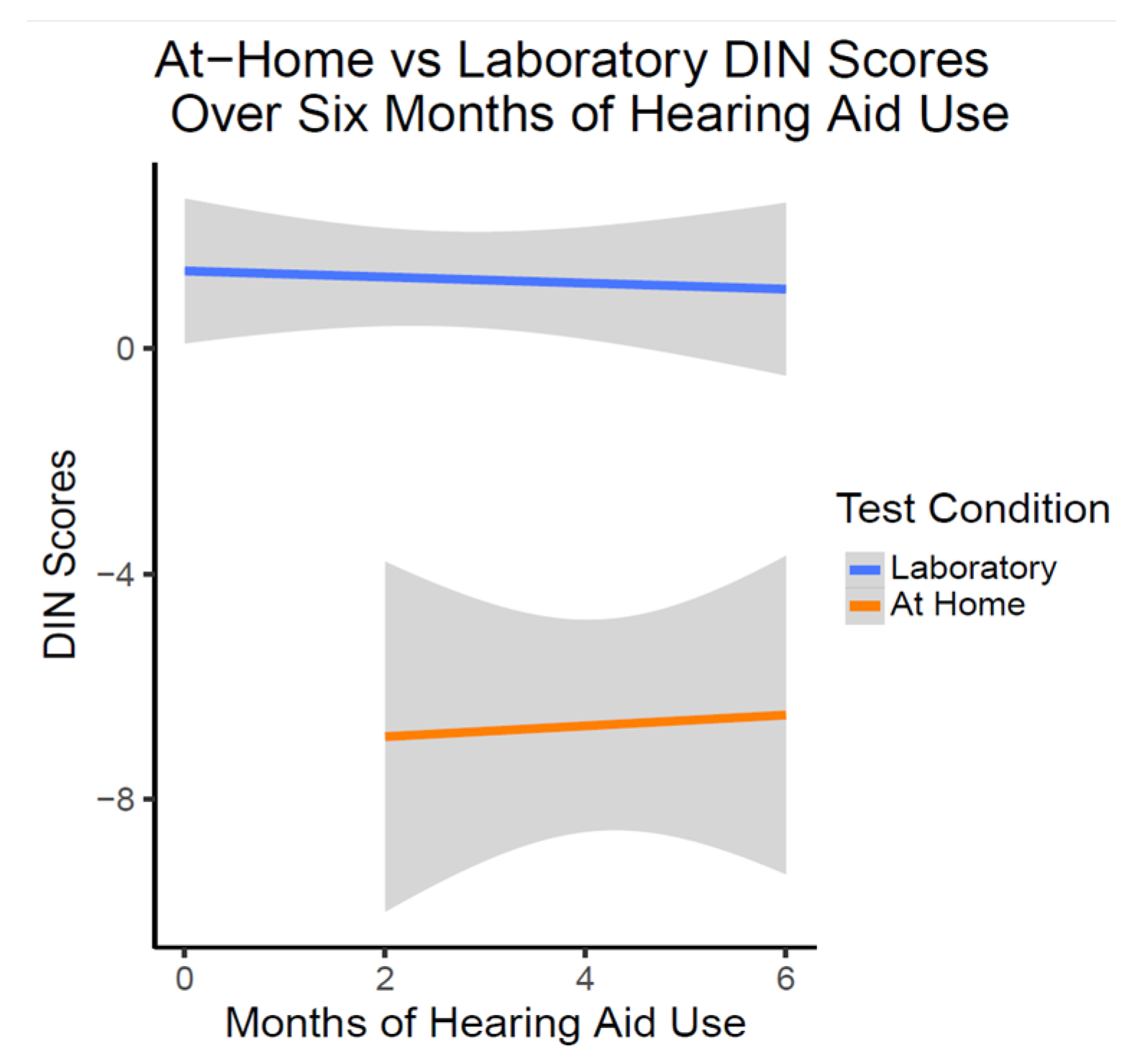
DIN Testing Remotely Versus In-Person
4. Discussion
4.1. Experiment 1: Individuals with Untreated Hearing Loss
4.2. Experiment 2: Prescription Hearing Aid Users
4.3. Experiment 3: Over-the-Counter (OTC) Hearing Aid Users
4.3.1. Relationship of DIN and QuickSIN
4.3.2. Remote versus In-Person Testing for OTC Hearing Aids
4.3.3. Speech Perception in Noise Testing Longitudinally in OTC HA Users
4.4. Considerations for the Digits in Noise Test
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Glick, H.; Sharma, A. Cortical Neuroplasticity and Cognitive Function in Early-Stage, Mild-Moderate Hearing Loss: Evidence of Neurocognitive Benefit from Hearing Aid Use. Front. Neurosci. 2020, 14, 93. [Google Scholar] [CrossRef] [PubMed]
- Castiglione, A.; Benatti, A.; Velardita, C.; Favaro, D.; Padoan, E.; Severi, D.; Pagliaro, M.; Bovo, R.; Vallesi, A.; Gabelli, C.; et al. Aging, cognitive decline and hearing loss: Effects of auditory rehabilitation and training with hearing aids and cochlear implants on cognitive function and depression among older adults. Audiol. Neurootol. 2016, 21 (Suppl. S1), 21–28. [Google Scholar] [CrossRef] [PubMed]
- Sarant, J.; Harris, D.; Busby, P.; Maruff, P.; Schembri, A.; Lemke, U.; Launer, S. The effect of hearing aid use on cognition in older adults: Can we delay decline or even improve cognitive function? J. Clin. Med. 2020, 9, 254. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.R.; Ferrucci, L.; An, Y.; Goh, J.O.; Doshi, J.; Metter, E.J.; Davatzikos, C.; Kraut, M.A.; Resnick, S.M. Association of hearing impairment with brain volume changes in older adults. NeuroImage 2014, 90, 84–92. [Google Scholar] [CrossRef]
- Peelle, J.E.; Troiani, V.; Grossman, M.; Wingfield, A. Hearing loss in older adults affects neural systems supporting speech comprehension. J. Neurosci. 2011, 31, 12638–12643. [Google Scholar] [CrossRef] [PubMed]
- Eckert, M.A.; Vaden, K.I.; Dubno, J.R. Age-related hearing loss associations with changes in brain morphology. Trends Hear. 2019, 23, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Orji, A.; Kamenov, K.; Dirac, M.; Davis, A.; Chadha, S.; Vos, T. Global and regional needs, unmet needs and access to hearing aids. Int. J. Audiol. 2020, 59, 166–172. [Google Scholar] [CrossRef]
- Mahboubi, H.; Lin, H.W.; Bhattacharyya, N. Prevalence, characteristics, and treatment patterns of hearing difficulty in the United States. JAMA Otolaryngol. Head Neck 2018, 144, 65–70. [Google Scholar] [CrossRef]
- Franks, I.; Timmer, B.H.B. Reasons for the non-use of hearing aids: Perspectives of non-users, past users, and family members. Int. J. Audiol. 2023, 1–8. [Google Scholar] [CrossRef]
- Meyer, C.; Hickson, L.; Lovelock, K.; Lampert, M.; Khan, A. An investigation of factors that influence help-seeking for hearing impairment in older adults. Int. J. Audiol. 2014, 53 (Suppl. S1), S3–S17. [Google Scholar] [CrossRef]
- D’Onofrio, K.L.; Zeng, F.-G. Tele-audiology: Current state and future directions. Front. Digit. Health 2022, 3, 788103. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, D.W. eHealth technologies enable more accessible hearing care. Semin. Hear. 2020, 41, 133–140. [Google Scholar] [CrossRef] [PubMed]
- U.S. Senate, 115th Congress. (18 August 2017). S.670, Over-the-Counter Hearing Aid Act of 2017. Available online: https://www.congress.gov/bill/115th-congress/senate-bill/670/all-actions?r=18 (accessed on 9 December 2023).
- Levesque, J.-F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef] [PubMed]
- Lazar, M.; Davenport, L. Barriers to health care access for low income families: A review of literature. J. Community Health Nurs. 2018, 35, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Houtgast, T.; Festen, J.M. On the auditory and cognitive functions that may explain an individual’s elevation of the speech reception threshold in noise. Int. J. Audiol. 2008, 47, 287–295. [Google Scholar] [CrossRef]
- Phatak, S.A.; Brungart, D.S.; Zion, D.J.; Grant, K.W. Clinical assessment of functional hearing deficits: Speech-in-noise performance. Ear Hear. 2019, 40, 426. [Google Scholar] [CrossRef]
- Pang, J.; Beach, E.F.; Gilliver, M.; Yeend, I. Adults who report difficulty hearing speech in noise: An exploration of experiences, impacts and coping strategies. Int. J. Audiol. 2019, 58, 851–860. [Google Scholar] [CrossRef]
- Killion, M.C.; Niquette, P.A.; Gudmundsen, G.I.; Revit, L.J.; Banerjee, S. Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. J. Acoust. Soc. Am. 2004, 116, 2395–2405. [Google Scholar] [CrossRef]
- Smits, S.C.; Goverts, T.; Festen, J.M. The digits-in-noise test: Assessing auditory speech recognition abilities in noise. J. Acoust. Soc. Am. 2013, 133, 1693–1706. [Google Scholar] [CrossRef]
- Smits, C. Development and validation of an automatic speech-in-noise screening test by telephone. Int. J. Audiol. 2004, 43, 15–28. [Google Scholar] [CrossRef]
- Smits, C.; Houtgast, T. Results from the Dutch speech-in-noise screening test by telephone. Ear Hear. 2005, 26, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Smits, C.; Kramer, S.E.; Houtgast, T. Speech reception thresholds in noise and self-reported hearing disability in a general adult population. Ear Hear. 2006, 27, 538–549. [Google Scholar] [CrossRef] [PubMed]
- Watson, C.S.; Kidd, G.R.; Miller, J.D.; Smits, C.; Humes, L.E. Telephone screening tests for functionally impaired hearing: Current use in seven countries and development of a US version. J. Am. Acad. Audiol. 2012, 23, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.; Mahomed-Asmail, F.; De Sousa, K.C.; Swanepoel, D.W. Performance and reliability of a smartphone digits-in-noise test in the sound field. Am. J. Audiol. 2019, 28 (Suppl. S3), 736–741. [Google Scholar] [CrossRef] [PubMed]
- Potgieter, J.-M.; Swanepoel, D.W.; Smits, C. Evaluating a smartphone digits-in-noise test as part of the audiometric test battery. S. Afr. J. Commun. Disord. 2018, 65, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Jansen, S.; Luts, H.; Wagener, K.C.; Kollmeier, B.; Del Rio, M.; Dauman, R.; James, C.; Fraysse, B.; Vormès, E.; Frachet, B.; et al. Comparison of three types of French speech-in-noise tests: A multi-center study. Int. J. Audiol. 2012, 51, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Vlaming, M.S.M.G.; MacKinnon, R.C.; Jansen, M.; Moore, D.R. Automated screening for high-frequency hearing loss. Ear Hear. 2014, 35, 667–679. [Google Scholar] [CrossRef] [PubMed]
- Jansen, S.; Luts, H.; Wagener, K.C.; Frachet, B.; Wouters, J. The French digit triplet test: A hearing screening tool for speech intelligibility in noise. Int. J. Audiol. 2010, 49, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Koole, A.; Nagtegaal, A.P.; Homans, N.C.; Hofman, A.; Baatenburg de Jong, R.J.; Goedegebure, A. Using the digits-in-noise test to estimate age-related hearing loss. Ear Hear. 2016, 37, 508–513. [Google Scholar] [CrossRef]
- McArdle, R.A.; Wilson, R.H.; Burks, C.A. Speech recognition in multitalker babble using digits, words, and sentences. J. Am. Acad. Audiol. 2005, 16, 726–739. [Google Scholar] [CrossRef]
- Kaandorp, M.W.; Smits, C.; Merkus, P.; Goverts, S.T.; Festen, J.M. Assessing speech recognition abilities with digits in noise in cochlear implant and hearing aid users. Int. J. Audiol. 2015, 54, 48–57. [Google Scholar] [CrossRef]
- Kim, S.; You, S.; Sohn, M.E.; Han, W.; Seo, J.-H.; Oh, Y. A comparison between the Korean digits-in-noise test and the korean speech perception-in-noise test in normal-hearing and hearing-impaired listeners. J. Audiol. Otol. 2021, 25, 171–177. [Google Scholar] [CrossRef]
- Vermiglio, A.J.; Soli, S.D.; Freed, D.J.; Fang, X. The effect of stimulus audibility on the relationship between pure-tone average and speech recognition in noise ability. J. Am. Acad. Audiol. 2020, 31, 224–232. [Google Scholar] [CrossRef]
- Keidser, G.; Dillon, H.; Flax, M.; Ching, T.; Brewer, S. The NAL-NL2 prescription procedure. Audiol. Res. 2011, 1, e24. [Google Scholar] [CrossRef]
- McCreery, R.W.; Bentler, R.A.; Roush, P.A. Characteristics of hearing aid fittings in infants and young children. Ear. Hear. 2013, 34, 701–710. [Google Scholar] [CrossRef]
- Position Statement: Red Flags-Warning of Ear Disease. American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS). Available online: https://www.entnet.org/resource/position-statement-red-flags-warning-of-ear-disease/ (accessed on 14 March 2024).
- Motlagh Zadeh, L.; Silbert, N.H.; Swanepoel, D.W.; Moore, D.R. Improved sensitivity of digits-in-noise test to high-frequency hearing loss. Ear. Hear. 2021, 42, 565. [Google Scholar] [CrossRef]
- Overholser, B.R.; Sowinski, K.M. Biostatistics primer: Part 2. Nutr. Clin. Pract. 2008, 23, 76–84. [Google Scholar] [CrossRef]
- Frosolini, A.; Cinquemani, P.; de Filippis, C.; Lovato, A. Age at fitting affected unilateral versus bilateral hearing aids choice in asymmetric hearing loss. J. Int. Adv. Otol. 2023, 19, 116–120. [Google Scholar] [CrossRef]
- Zobay, O.; Naylor, G.; Saunders, G.H.; Dillard, L.K. Fitting a hearing aid on the better ear, worse ear, or both: Associations of hearing-aid fitting laterality with outcomes in a large sample of us veterans. Trends Hear. 2023, 27. [Google Scholar] [CrossRef]
- Monson, B.B.; Buss, E. Spectral degradations in the TIMIT, QuickSIN, NU-6, and other popular bandlimited speech materials. J. Acoust. Soc. Am. 2023, 152, 1639. [Google Scholar] [CrossRef]
- Motlagh Zadeh, L.; Silbert, N.H.; Sternasty, K.; Swanepoel, D.W.; Hunter, L.L.; Moore, D.R. Extended high-frequency hearing enhances speech perception in noise. Proc. Natl. Acad. Sci. USA 2019, 116, 23753–23759. [Google Scholar] [CrossRef]
- De Sousa, K.C.; Manchaiah, V.; Moore, D.R.; Graham, M.A.; Swanepoel, D.W. Effectiveness of an Over-the-Counter Self-fitting Hearing Aid Compared with an Audiologist-Fitted Hearing Aid. JAMA Otolaryngol. Head Neck Surg. 2023, 149, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Hoge, C.; Bowling, C.B.; Dunlop-Thomas, C.; Pearce, B.D.; Drenkard, C.; Lim, S.S.; Plantinga, L.C. Remote administration of physical and cognitive performance assessments in a predominantly black cohort of persons with systemic lupus erythematosus. ACR Open Rheumatol. 2023, 5, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Karawani, H.; Jenkins, K.A.; Anderson, S. Neural and behavioral changes after the use of hearing aids. Clin. Neurophysiol. 2018, 129, 1254–1267. [Google Scholar] [CrossRef] [PubMed]
- Dawes, P.; Munro, K.J. Auditory distraction and acclimatization to hearing aids. Ear Hear. 2017, 38, 174. [Google Scholar] [CrossRef] [PubMed]
- Humes, L.E.; Wilson, D.L.; Barlow, N.N.; Garner, C. Changes in hearing-aid benefit following 1 or 2 years of hearing-aid use by older adults. J. Speech Lang. Hear. Res. 2002, 45, 772–782. [Google Scholar] [CrossRef] [PubMed]
- Dawes, P.; Munro, K.J.; Kalluri, S.; Edwards, B. Auditory acclimatization and hearing aids: Late auditory evoked potentials and speech recognition following unilateral and bilateral amplification. J. Acoust. Soc. Am. 2014, 135, 3560–3569. [Google Scholar] [CrossRef] [PubMed]
- Laplante-Lévesque, A.; Nielsen, C.; Jensen, L.D.; Naylor, G. Patterns of hearing aid usage predict hearing aid use amount (Data logged and self-reported) and overreport. J. Am. Acad. Audiol. 2014, 25, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Solheim, J.; Hickson, L. Hearing aid use in the elderly as measured by datalogging and self-report. Int. J. Audiol. 2017, 56, 472–479. [Google Scholar] [CrossRef]
- Swanepoel, D.W.; Oosthuizen, I.; Graham, M.A.; Manchaiah, V. Comparing hearing aid outcomes in adults using over-the-counter and hearing care professional service delivery models. Am. J. Audiol. 2023, 32, 314–322. [Google Scholar] [CrossRef]
- Wilson, R.H.; Carnell, C.S.; Cleghorn, A.L. The Words-in-Noise (WIN) Test with Multitalker Babble and Speech-Spectrum Noise Maskers. J. Am. Acad. Audiol. 2007, 18, 522–529. [Google Scholar] [CrossRef]
- Wilson, R.H.; McArdle, R.A.; Smith, S.L. An evaluation of the BKB-SIN, HINT, QuickSIN and WIN materials on listeners with normal hearing and listeners with hearing loss. J. Speech Lang. Hear. Res. 2007, 50, 844–856. [Google Scholar] [CrossRef]
- Theunissen, M.; Swanepoel, D.W.; Hanekom, J. Sentence recognition in noise: Variables in compilation and interpretation of tests. Int. J. Audiol. 2009, 48, 743–757. [Google Scholar] [CrossRef]
- De Sousa, K.C.; Smits, C.; Moore, D.R.; Chada, S.; Myburgh, H.; Swanepoel, D.W. Global use and outcomes of the hearWHO mHealth hearing test. Digit. Health 2022, 8. [Google Scholar] [CrossRef]
- Swanepoel, D.W.; De Sousa, K.C.; Smits, C.; Moore, D.R. Mobile applications to detect hearing impairment: Opportunities and challenges. Bull. World Health Organ. 2019, 97, 717–718. [Google Scholar] [CrossRef]

| Characteristic | Untreated Hearing Loss (n = 46) | Prescription HA (n = 15) | OTC HA (n = 12) |
|---|---|---|---|
| Age, years, mean ± SD (range) | 68 ± 8.4 (46–84) | 71 ± 6 (61–79) | 70 ± 7.8 (56–81) |
| Gender, n (%) | |||
| Male | 19 (41%) | 9 (60%) | 4 (33%) |
| Female | 27 (59%) | 6 (40%) | 8 (67%) |
| Three frequency puretone average (0.5, 1, 2 kHz; PTA-3), dB HL | 22.5 ± 8.3 (8.3–44.2) | 31.5 ± 12.6 (8.3–52.5) | 29.17 ± 7.89 (18.3–44.2) |
| Four frequency puretone Average (0.5, 1, 2, 4 kHz; PTA-4), dB HL, mean ± SD (range) | 28.5 ± 8.4 (11.3–48.8) | 38.6 ± 11.4 (16.3–52.5) | 35.5 ± 6.3 (26.9–48.8) |
| High frequency puretone average (3, 4, 6 kHz; PTA-HF), mean ± SD (range) | 45.7 ± 13 (20–70) | 58.6 ± 12.9 (37.5–87.9) | 53.5 ± 6.4 (45.8–61.7) |
| Duration of hearing aid use in years (prescription HA) or months (OTC HA), mean ± SD (range) | - | 7 ± 5.68 (2–23) | 5.73 ± 0.47 |
| Daily hearing aid use, hours/day, mean ± SD (range) | - | 8.65 ± 5.12 (0.5–16) | 6.75 ± 2.71 (0.71–13.55) |
| Root mean square error (RMSE) in real ear probe measures, mean ± SD (range) | - | 5.5 ± 2.5 (2.3–11) | 7.5 ± 2.8 (3.9–11.9) |
| Correlations between Puretone Average and Speech in Noise Testing | ||
|---|---|---|
| DIN | QuickSIN | |
| PTA-3 | 0.33 * | 0.35 * |
| PTA-4 | 0.49 *** | 0.54 *** |
| PTA-HF | 0.65 *** | 0.57 *** |
| WRS | −0.51 *** | −0.47 ** |
| Measurements in Aided Conditions | QuickSIN Score (dB SNR Loss) (Mean ± SEM) | DIN Score (dB SNR) (Mean ± SEM) |
|---|---|---|
| Baseline (i.e., 0 months) | 2.54 ± 0.41 | 1.28 ± 0.41 |
| First follow up (i.e., 1 month) | 2.75 ± 0.37 | 0.93 ± 0.44 |
| Second follow up (i.e., 4 months) | 1.86 ± 0.21 | 1.94 ± 0.47 |
| Third follow up (i.e., 6 months) | 2.05 ± 0.31 | 0.93 ± 0.38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schimmel, C.; Cormier, K.; Manchaiah, V.; Swanepoel, D.W.; Sharma, A. Digits-in-Noise Test as an Assessment Tool for Hearing Loss and Hearing Aids. Audiol. Res. 2024, 14, 342-358. https://doi.org/10.3390/audiolres14020030
Schimmel C, Cormier K, Manchaiah V, Swanepoel DW, Sharma A. Digits-in-Noise Test as an Assessment Tool for Hearing Loss and Hearing Aids. Audiology Research. 2024; 14(2):342-358. https://doi.org/10.3390/audiolres14020030
Chicago/Turabian StyleSchimmel, Carly, Kayla Cormier, Vinaya Manchaiah, De Wet Swanepoel, and Anu Sharma. 2024. "Digits-in-Noise Test as an Assessment Tool for Hearing Loss and Hearing Aids" Audiology Research 14, no. 2: 342-358. https://doi.org/10.3390/audiolres14020030
APA StyleSchimmel, C., Cormier, K., Manchaiah, V., Swanepoel, D. W., & Sharma, A. (2024). Digits-in-Noise Test as an Assessment Tool for Hearing Loss and Hearing Aids. Audiology Research, 14(2), 342-358. https://doi.org/10.3390/audiolres14020030







