Cultivatable Bacteriota of Chronic Wound of Patients with Diabetic Foot Syndrome with Critical Limb Ischemia Based on Wound Biopsy in Peri-Revascularization Period
Abstract
1. Introduction
2. Materials and Methods
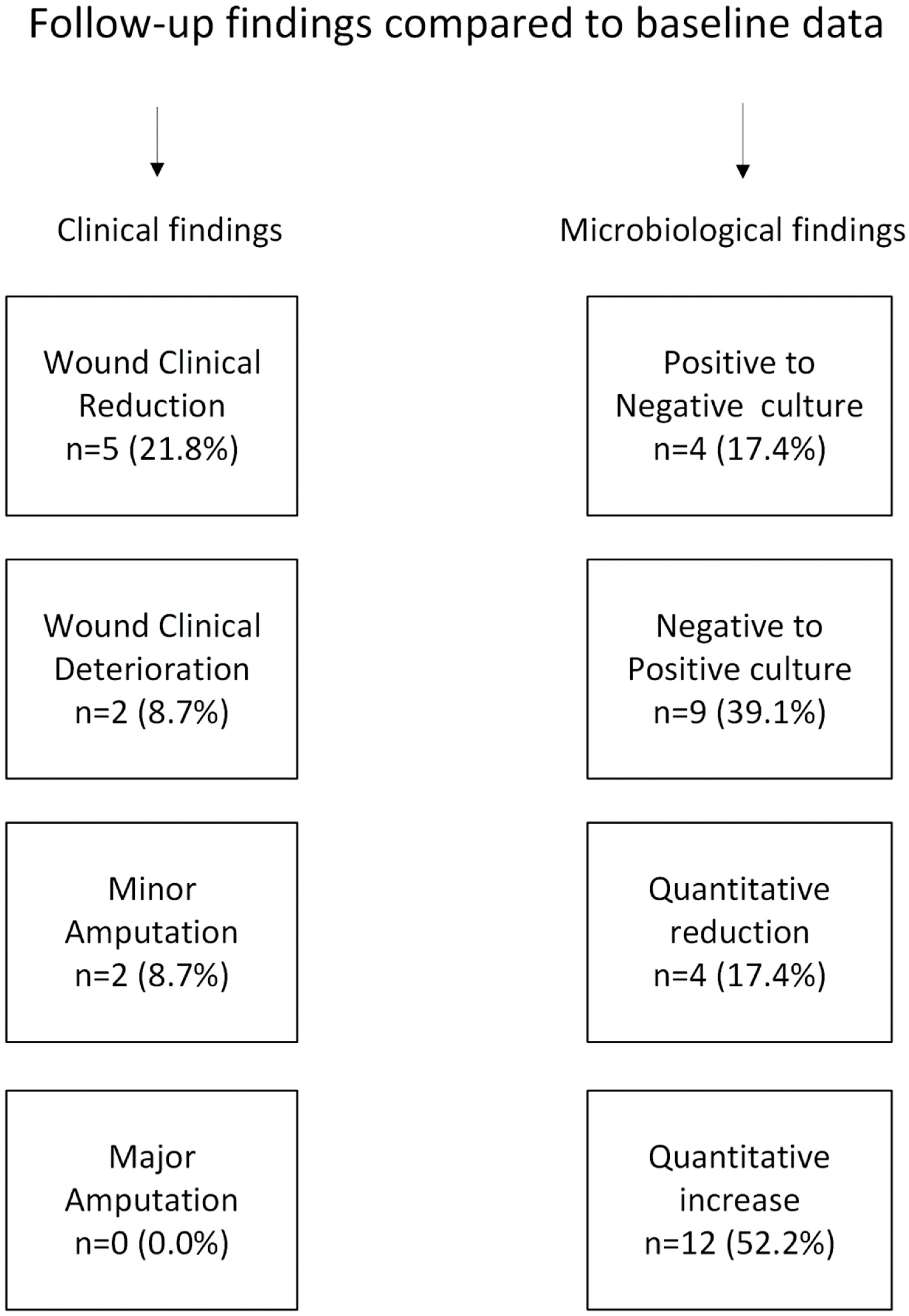
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oliver, T.I.; Mutluoglu, M. Diabetic Foot Ulcer. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://pubmed.ncbi.nlm.nih.gov/30726013/ (accessed on 26 October 2024).
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation (IDF): Belgium, Brussels, 2021; Available online: https://www.diabetesatlas.org (accessed on 26 October 2024).
- Lin, C.; Liu, J.; Sun, H. Risk factors for lower extremity amputation in patients with diabetic foot ulcers: A meta-analysis. PLoS ONE 2020, 15, e0239236. [Google Scholar] [CrossRef] [PubMed]
- Hingorani, A.; LaMuraglia, G.M.; Henke, P.; Meissner, M.H.; Loretz, L.; Zinszer, K.M.; Driver, V.R.; Frykberg, R.; Carman, T.L.; Marston, W.; et al. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J. Vasc. Surg. 2016, 63 (Suppl. 2), 3S–21S. [Google Scholar] [CrossRef] [PubMed]
- Tuttolomondo, A.; Maida, C.; Pinto, A. Diabetic foot syndrome: Immune-inflammatory features as possible cardiovascular markers in diabetes. World J. Orthop. 2015, 6, 62–76. [Google Scholar] [CrossRef]
- Ma, J.; Fang, Y.; Yu, H.; Yi, J.; Ma, Y.; Lei, P.; Yang, Q.; Jin, L.; Wu, W.; Li, H.; et al. Recent Advances in Living Algae Seeding Wound Dressing: Focusing on Diabetic Chronic Wound Healing. Adv. Funct. Mater. 2024, 34, 2308387. [Google Scholar] [CrossRef]
- Meloni, M.; Morosetti, D.; Giurato, L.; Stefanini, M.; Loreni, G.; Doddi, M.; Panunzi, A.; Bellia, A.; Gandini, R.; Brocco, E.; et al. Foot Revascularization Avoids Major Amputation in Persons with Diabetes and Ischaemic Foot Ulcers. J. Clin. Med. 2021, 10, 3977. [Google Scholar] [CrossRef] [PubMed]
- Jörneskog, G. Why critical limb ischemia criteria are not applicable to diabetic foot and what the consequences are. Scand. J. Surg. SJS 2012, 101, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Baltzis, D.; Eleftheriadou, I.; Veves, A. Pathogenesis and treatment of impaired wound healing in diabetes mellitus: New insights. Adv. Ther. 2014, 31, 817–836. [Google Scholar] [CrossRef] [PubMed]
- Račytė, A.; Pikturnaitė, G.; Baltrūnas, T.; Kalvaitis, E.; Vaitėnas, G.; Skrebūnas, A.; Baltrūnienė, V.; Ručinskas, K. Oxygen Saturation Increase in Ischemic Wound Tissues after Direct and Indirect Revascularization. Biomedicines 2024, 12, 367. [Google Scholar] [CrossRef] [PubMed]
- Kalan, L.R.; Meisel, J.S.; Loesche, M.A.; Horwinski, J.; Soaita, I.; Chen, X.; Uberoi, A.; Gardner, S.E.; Grice, E.A. Strain- and Species-Level Variation in the Microbiome of Diabetic Wounds Is Associated with Clinical Outcomes and Therapeutic Efficacy. Cell Host Microbe 2019, 25, 641–655.e5. [Google Scholar] [CrossRef]
- Jones, D.P.; Aw, T.Y.; Shan, X.Q. Drug metabolism and toxicity during hypoxia. Drug Metab. Rev. 1989, 20, 247–260. [Google Scholar] [CrossRef]
- Vieceli Dalla Sega, F.; Cimaglia, P.; Manfrini, M.; Fortini, F.; Marracino, L.; Bernucci, D.; Pompei, G.; Scala, A.; Trichilo, M.; De Carolis, B.; et al. Circulating Biomarkers of Endothelial Dysfunction and Inflammation in Predicting Clinical Outcomes in Diabetic Patients with Critical Limb Ischemia. Int. J. Mol. Sci. 2022, 23, 10641. [Google Scholar] [CrossRef] [PubMed]
- Alex Cheong, J.Z.; Irvine, J.M.; Roesemann, S.; Nora, A.; Morgan, C.E.; Daniele, C.; Kalan, L.R.; Brennan, M.B. Ankle brachial indices and anaerobes: Is peripheral arterial disease associated with anaerobic bacteria in diabetic foot ulcers? Ther. Adv. Endocrinol. Metab. 2022, 13, 20420188221118747. [Google Scholar] [CrossRef] [PubMed]
- Murphy-Lavoie, H.M.; Ramsey, A.; Nguyen, M.; Singh, S. Diabetic Foot Infections. [Updated 2023 July 4]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK441914/ (accessed on 26 October 2024).
- van Baal, J.G.; Harding, K.G.; Lipsky, B.A. Foot Infections in Diabetic Patients: An Overview of the Problem. Clin. Infect. Dis. 2004, 39, S71–S72. [Google Scholar] [CrossRef]
- Stevens, D.L.; Bisno, A.L.; Chambers, H.F.; Dellinger, E.P.; Goldstein, E.J.; Gorbach, S.L.; Hirschmann, J.V.; Kaplan, S.L.; Montoya, J.G.; Wade, J.C.; et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin. Infect. Dis. 2014, 59, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Kalan, L.R.; Brennan, M.B. The role of the microbiome in nonhealing diabetic wounds. Ann. N. Y. Acad. Sci. 2019, 1435, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Lavery, L.A.; Armstrong, D.G.; Murdoch, D.P.; Peters, E.J.; Lipsky, B.A. Validation of the Infectious Diseases Society of America’s Diabetic Foot Infection Classification System. Clin. Infect. Dis. 2007, 44, 562–565. [Google Scholar] [CrossRef] [PubMed]
- DiPietro, L.A. Angiogenesis and wound repair: When enough is enough. J. Leukoc. Biol. 2016, 100, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Hsia, H.C. The Impact of Microbial Communities on Wound Healing: A Review. Ann. Plast. Surg. 2018, 81, 113–123. [Google Scholar] [CrossRef] [PubMed]
- McBride, M.J.; Brown, J.M.; Chiu, E.S. Lower extremity revascularization in peripheral artery disease. Surgery 2018, 163, 519–525. [Google Scholar]
- Mustoe, T. Understanding chronic wounds: A unifying hypothesis on their pathogenesis and implications for therapy. Am. J. Surg. 2004, 187, 65S–70S. [Google Scholar] [CrossRef] [PubMed]
- Gregory, S.; Bruce, M. Molecular Analysis of the Environments of Healing and Chronic Wounds: Cytokines, Proteases and Growth Factors. Prim. Intent. 1999, 7, 7–15. [Google Scholar]
- Clark, S.T.; Forbes, J.D.; Matukas, L.M. Wound swab quality grading is dependent on Gram smear screening approach. Sci. Rep. 2023, 13, 3160. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Cao, Y.; Zou, M.; Luo, X.; Jiang, Y.; Xue, Y.; Gao, F. A Comparison of Tissue versus Swab Culturing of Infected Diabetic Foot Wounds. Int. J. Endocrinol. 2016, 2016, 8198714. [Google Scholar] [CrossRef] [PubMed]
- Bakker, K.; Apelqvist, J.; Schaper, N.C.; International Working Group on Diabetic Foot Editorial Board. Practical guidelines on the management and prevention of the diabetic foot 2011. Diabetes/Metab. Res. Rev. 2012, 28 (Suppl. 1), 225–231. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, K.E.; Boeckh, S.; Stacey, H.J.; Jones, J.D. The microbiology of diabetic foot infections: A meta-analysis. BMC Infect. Dis. 2021, 21, 770. [Google Scholar] [CrossRef] [PubMed]
- Brocklehurst, J.D. The Validity and Reliability of the SINBAD Classification System for Diabetic Foot Ulcers. Adv. Ski. Wound Care 2023, 36, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Bruyndonckx, R.; Adriaenssens, N.; Versporten, A.; Hens, N.; Monnet, D.L.; Molenberghs, G.; Goossens, H.; Weist, K.; Coenen, S.; ESAC-Net Study Group. Consumption of antibiotics in the community, European Union/European Economic Area, 1997-2017. J. Antimicrob. Chemother. 2021, 76 (Suppl. 2), ii7–ii13. [Google Scholar] [CrossRef]
- Wojkowska-Mach, J.; Godman, B.; Glassman, A.; Kurdi, A.; Pilc, A.; Rozanska, A.; Skoczyński, S.; Wałaszek, M.; Bochenek, T. Antibiotic consumption and antimicrobial resistance in Poland; findings and implications. Antimicrob. Resist. Infect. Control 2018, 7, 136. [Google Scholar] [CrossRef] [PubMed]
- Gajda, M.; Załugowicz, E.; Pomorska-Wesołowska, M.; Bochenek, T.; Gryglewska, B.; Romaniszyn, D.; Chmielarczyk, A.; Wójkowska-Mach, J. Virulence and Drug-Resistance of Staphylococcus aureus Strains Isolated from Venous Ulcers in Polish Patients. Int. J. Environ. Res. Public Health 2021, 18, 4662. [Google Scholar] [CrossRef] [PubMed]
- Asma, S.T.; Imre, K.; Morar, A.; Herman, V.; Acaroz, U.; Mukhtar, H.; Arslan-Acaroz, D.; Shah SR, A.; Gerlach, R. An Overview of Biofilm Formation-Combating Strategies and Mechanisms of Action of Antibiofilm Agents. Life 2022, 12, 1110. [Google Scholar] [CrossRef] [PubMed]
- Disabling and Potentially Permanent Side Effects Lead to Suspension or Restrictions of Quinolone and Fluoroquinolone Antibiotics EMA/175398/2019. Available online: https://www.ema.europa.eu/en/medicines/human/referrals/quinolone-fluoroquinolone-containing-medicinal-products (accessed on 13 October 2024).
- Altmann, D.; Waibel, F.W.A.; Forgo, G.; Grigorean, A.; Lipsky, B.A.; Uçkay, I.; Schöni, M. Timing of Revascularization and Parenteral Antibiotic Treatment Associated with Therapeutic Failures in Ischemic Diabetic Foot Infections. Antibiotics 2023, 12, 685. [Google Scholar] [CrossRef] [PubMed]
- Jodheea-Jutton, A.; Hindocha, S.; Bhaw-Luximon, A. Health economics of diabetic foot ulcer and recent trends to accelerate treatment. Foot 2022, 52, 101909. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, J.C.; Browning, K.K. Smoking, chronic wound healing, and implications for evidence-based practice. J. Wound Ostomy Cont. Nurs. 2014, 41, 415–423; quiz E1–E2. [Google Scholar] [CrossRef] [PubMed]
- Hahad, O.; Kuntic, M.; Kuntic, I.; Daiber, A.; Münzel, T. Tobacco smoking and vascular biology and function: Evidence from human studies. Pflug. Arch. Eur. J. Physiol. 2023, 475, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, L. Nicotine, CO and HCN: The detrimental effects of smoking on wound healing. Br. J. Community Nurs. 2003, 8, S22–S26. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, L.T.; Jørgensen, S.; Petersen, L.J.; Hemmingsen, U.; Bülow, J.; Loft, S.; Gottrup, F. Acute effects of nicotine and smoking on blood flow, tissue oxygen, and aerobe metabolism of the skin and subcutis. J. Surg. Res. 2009, 152, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Saint-André, V.; Charbit, B.; Biton, A.; Rouilly, V.; Possémé, C.; Bertrand, A.; Rotival, M.; Bergstedt, J.; Patin, E.; Albert, M.L.; et al. Smoking changes adaptive immunity with persistent effects. Nature 2024, 626, 827–835. [Google Scholar] [CrossRef]
- Mazzolai, L.; Teixido-Tura, G.; Lanzi, S.; Boc, V.; Bossone, E.; Brodmann, M.; Bura-Rivière, A.; De Backer, J.; Deglise, S.; Della Corte, A.; et al. 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases: Developed by the task force on the management of peripheral arterial and aortic diseases of the European Society of Cardiology (ESC) Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS), the European Reference Network on Rare Multisystemic Vascular Diseases (VASCERN), and the European Society of Vascular Medicine (ESVM). Eur. Heart J. 2024, 45, 3538–3700. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Weng, H.; Chen, L.; Yang, H.; Luo, G.; Mai, L.; Jin, G.; Yan, L. Transcutaneous oxygen pressure measurement in diabetic foot ulcers: Mean values and cut-point for wound healing. J. Wound Ostomy Cont. Nurs. 2013, 40, 585–589. [Google Scholar] [CrossRef] [PubMed]
| Studied Factor | N = 23 |
|---|---|
| Gender, male n (%) | 19 (82.6%) |
| Age, median (IQR) | |
| Males | 70.0 (63.0; 75.0) |
| Females | 61.5 (54.5; 68.5) |
| Smoker n (%) | |
| Current | 2 (8.7%) |
| Former (non-smoker at day of admission) | 14 (60.9%) |
| Non-smoker | 7 (30.4%) |
| Rutherford ischemia classification n (%) | |
| 5 | 15 (65.2%) |
| 6 | 8 (34.8%) |
| Hypertension n (%) | 21 (91.3%) |
| Coronary Artery Disease n (%) | 5 (21.7%) |
| Heart Failure n (%) | 10 (43.5%) |
| Atrial Fibrillation n (%) | 5 (21.7%) |
| Stroke n (%) | 2 (8.7%) |
| Chronic Kidney Disease n (%) | 3 (13.0%) |
| Chronic Venous Insufficiency n (%) | 3 (13.0%) |
| Factor | Pre-Intervention | Post-Intervention |
|---|---|---|
| Median (IQR) | ||
| Toe-Brachial Index | 0.1 (0.06; 0.20) | 0.3 (0.18; 0.42) |
| Ankle-Brachial Index | 0.7 (0.36; 0.78) | 0.9 (0.78; 1.04) |
| TCPO2 [mmHg] | 15.0 (10.00; 25.00) | 38.5 (26.00; 43.00) |
| SINBAD score | 4.0 (3.00; 5.00) | 3.00 (2.00; 4.00) |
| Age | Sex | Rutherford | Infection (Based on WIfI) | Quantitative Culture [CFU/g] | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | ||
| 54 | F | 5 | 5 | mild | no | 7 × 107 (*) | 5 × 107 (*) |
| 66 | M | 6 | 6 | mild | mild | 0 | 4 × 104 |
| 74 | M | 5 | 5 | moderate | mild | 2 × 107 (*) | 1 × 108 (*) |
| 63 | M | 5 | 5 | moderate | moderate | 1 × 107 | 4 × 104 |
| 68 | F | 6 | 5 | mild | moderate | 1 × 105 | 7 × 104 |
| 66 | M | 5 | 5 | moderate | moderate | 0 | 2 × 105 |
| 55 | F | 6 | 6 | moderate | moderate | 6 × 105 | 8 × 107 (*) |
| 62 | M | 6 | 6 | moderate | mild | 0 | 4 × 105 |
| 70 | M | 5 | 5 | moderate | moderate | 3 × 107 (*) | 4 × 106 |
| 79 | M | 5 | 5 | mild | no | 2 × 107 (*) | 0 |
| 81 | M | 5 | 5 | no | no | 0 | 2 × 108 (*) |
| 73 | M | 5 | 5 | moderate | no | 3 × 105 | 0 |
| 75 | M | 5 | 5 | no | mild | 0 | 5 × 106 (*) |
| 55 | M | 5 | 5 | no | no | 4 × 107 (*) | 3 × 107 (*) |
| 74 | M | 5 | 5 | mild | no | 2 × 108 | 0 |
| 57 | M | 6 | 6 | moderate | moderate | 0 | 1 × 106 |
| 69 | F | 5 | 5 | no | no | 0 | 0 |
| 83 | M | 5 | 5 | no | mild | 2 × 106 | 0 |
| 68 | M | 6 | 6 | mild | no | 0 | 1 × 105 |
| 74 | M | 5 | - | moderate | no data | 0 | 4 × 105 |
| 63 | M | 6 | 6 | moderate | moderate | 2 × 107 | 2 × 105 |
| 57 | M | 5 | 5 | moderate | mild | 0 | 0 |
| 84 | M | 6 | 6 | mild | no | 0 | 6 × 106 |
| WIfI Classification Parameter | Pre-Intervention | Post-Intervention |
|---|---|---|
| Wound | ||
| No ulcer, no gangrene | 0 (0.0%) | 1 (4.3%) |
| Small ulcer, no gangrene | 8 (34.8%) | 10 (43.5%) |
| Deep ulcer and gangrene limited to toes | 13 (56.5%) | 9 (39.1%) |
| Extensive ulcer or gangrene | 2 (8.7%) | 2 (8.7%) |
| Ischemia | ||
| Toe pressure\tcpO2 > 60 mmHg | 0 (0.0%) | 5 (21.7%) |
| 40–59 mmHg | 1 (4.3%) | 8 (34.8%) |
| 30–39 mmHg | 2 (8.7%) | 3 (13.0%) |
| <30 mmHg | 20 (87.0%) | 6 (26.1%) |
| Infection | ||
| Lack of infection | 5 (21.7%) | 9 (39.1%) |
| Mild < 2 cm cellulitis | 7 (30.4%) | 6 (26.1%) |
| Moderate > 2 cm cellulitis/purulence | 11 (47.8%) | 7 (30.4%) |
| Severe systemic response | 0 (0.0%) | 0 (0.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hussaini, S.S.; Grubesa, F.D.; Gajda, M.; Schönborn, M.; Bogucka, K.; Maga, M.; Maga, P.; Wójkowska-Mach, J. Cultivatable Bacteriota of Chronic Wound of Patients with Diabetic Foot Syndrome with Critical Limb Ischemia Based on Wound Biopsy in Peri-Revascularization Period. Microbiol. Res. 2025, 16, 25. https://doi.org/10.3390/microbiolres16010025
Hussaini SS, Grubesa FD, Gajda M, Schönborn M, Bogucka K, Maga M, Maga P, Wójkowska-Mach J. Cultivatable Bacteriota of Chronic Wound of Patients with Diabetic Foot Syndrome with Critical Limb Ischemia Based on Wound Biopsy in Peri-Revascularization Period. Microbiology Research. 2025; 16(1):25. https://doi.org/10.3390/microbiolres16010025
Chicago/Turabian StyleHussaini, Syedah Sarah, Fran Dominic Grubesa, Mateusz Gajda, Martyna Schönborn, Katarzyna Bogucka, Mikołaj Maga, Paweł Maga, and Jadwiga Wójkowska-Mach. 2025. "Cultivatable Bacteriota of Chronic Wound of Patients with Diabetic Foot Syndrome with Critical Limb Ischemia Based on Wound Biopsy in Peri-Revascularization Period" Microbiology Research 16, no. 1: 25. https://doi.org/10.3390/microbiolres16010025
APA StyleHussaini, S. S., Grubesa, F. D., Gajda, M., Schönborn, M., Bogucka, K., Maga, M., Maga, P., & Wójkowska-Mach, J. (2025). Cultivatable Bacteriota of Chronic Wound of Patients with Diabetic Foot Syndrome with Critical Limb Ischemia Based on Wound Biopsy in Peri-Revascularization Period. Microbiology Research, 16(1), 25. https://doi.org/10.3390/microbiolres16010025








