Weissella koreensis KJ, Which Increases Gut Tight Junction Protein Expression, Alleviates TNBS-Induced Colitis by Suppressing Inflammatory Cytokines
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Isolation and Preparation of LABs from Kimchi
2.3. Viability in Gastric and Intestinal Juice
2.4. Ability to Attach to Intestinal Epithelial Cells
2.5. Preparation of Macrophages
2.6. Animals
2.7. Induction and Evaluation of Colitis in Mice
2.8. MPO Activity Assay
2.9. Immunoblot Analysis and ELISA
2.10. H&E Staining of Colon Tissue
2.11. Immunohistochemistry (IHC) Staining
2.12. Statistical Analysis
3. Results
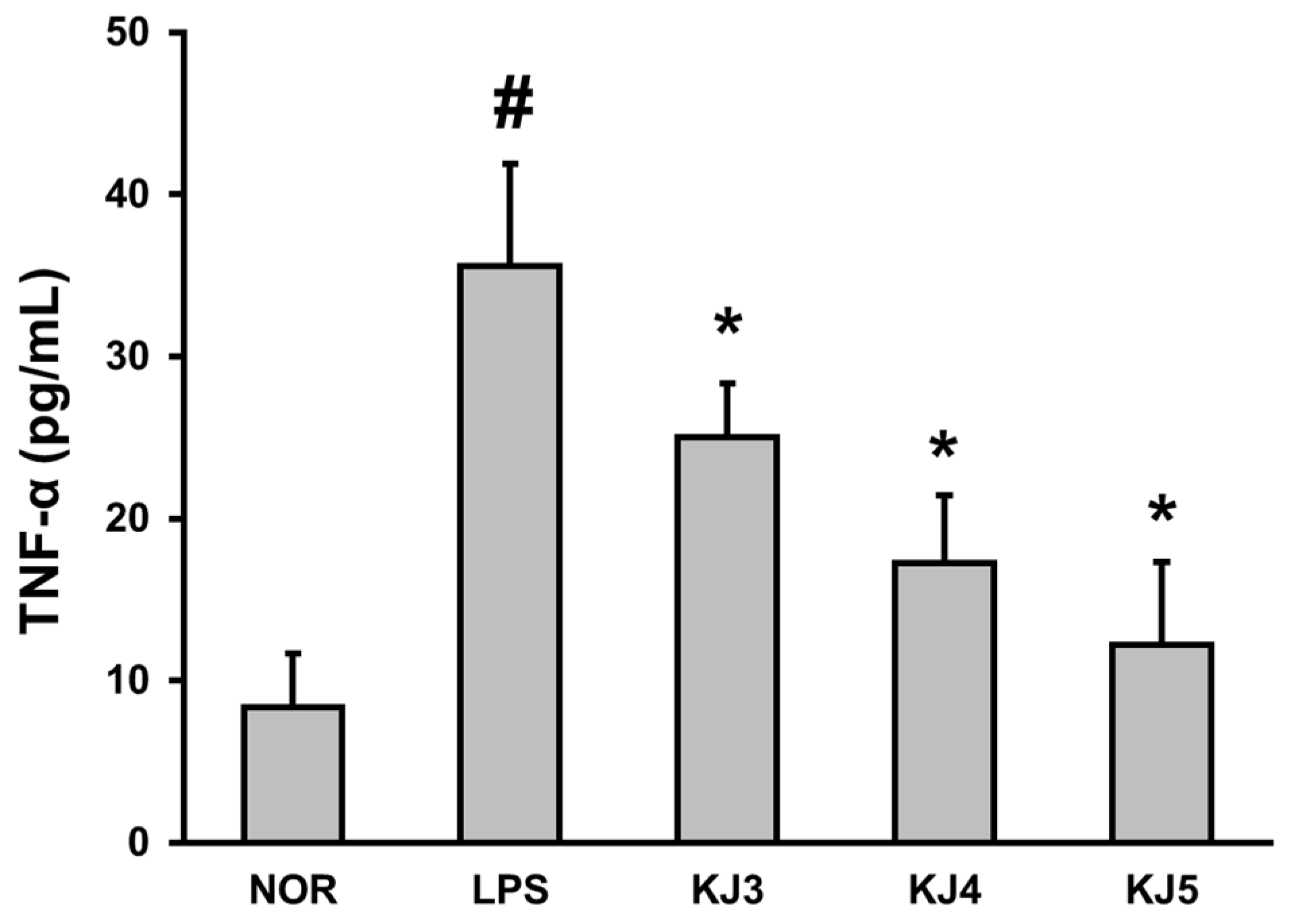
3.1. W. koreensis KJ Suppresses the Expression of Pro-Inflammatory Cytokines in LPS-Stimulated Peritoneal Macrophages
3.2. Characterization of W. koreensis KJ for Application in Humans
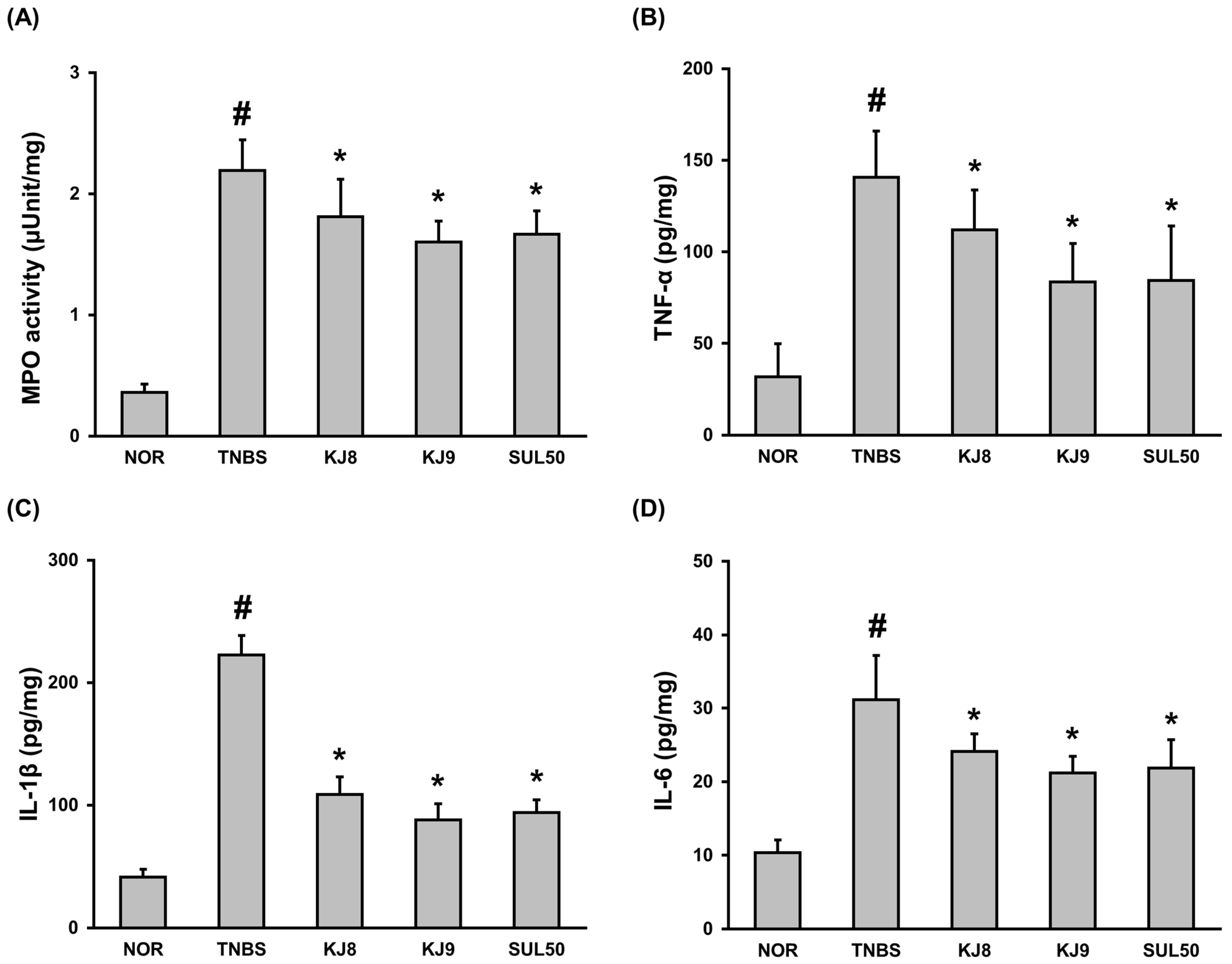
3.3. W. koreensis KJ Ameliorates TNBS-Induced Colitis in Mice
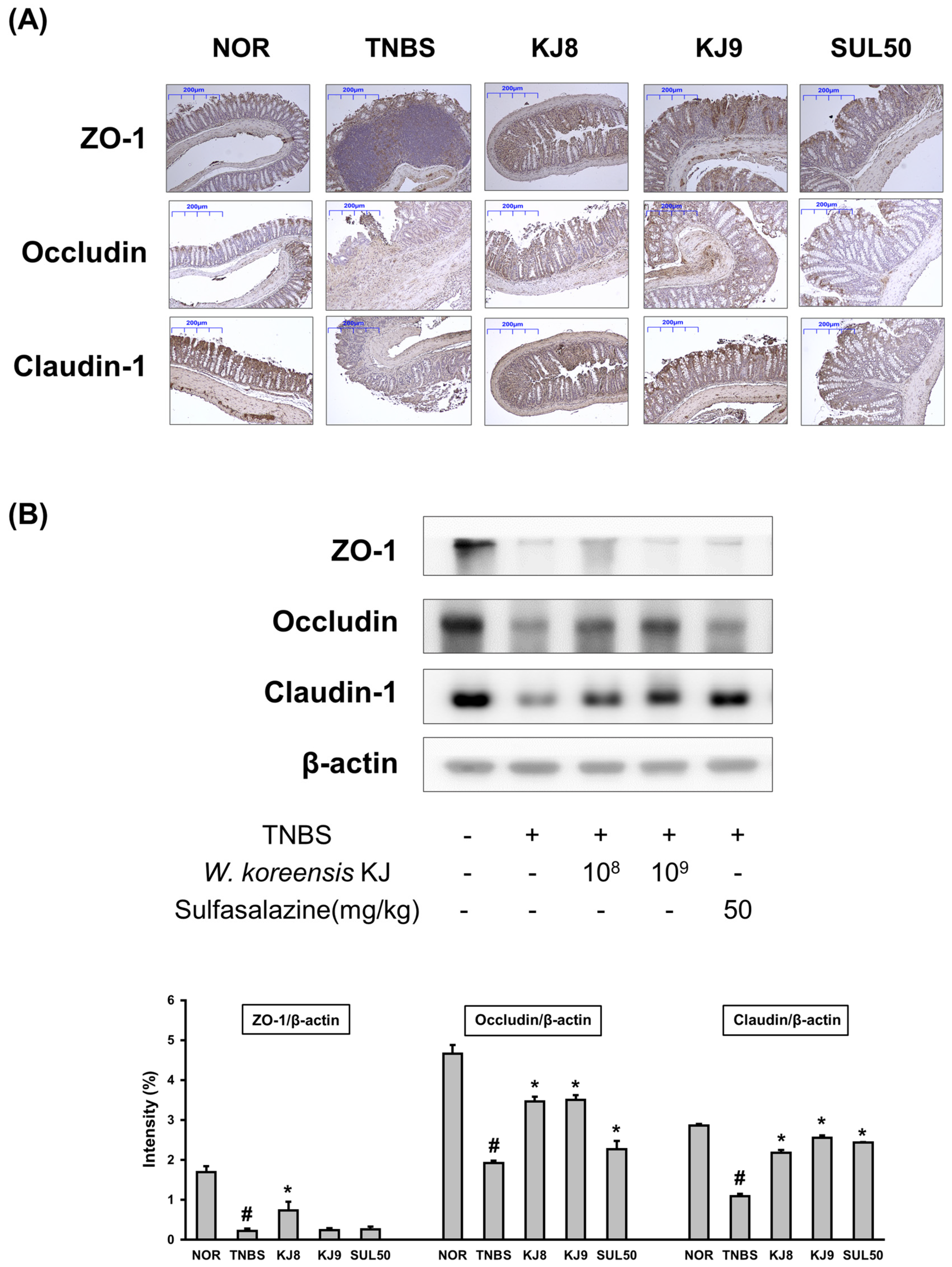
3.4. W. koreensis KJ Increases the Expression of Intestinal Tight Junction Proteins
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, K.J.; Kyung, S.; Jin, H.; Im, M.; Kim, J.W.; Kim, H.S.; Jang, S.E. Lactic acid bacteria isolated from human breast milk improve colitis induced by 2,4,6-trinitrobenzene sulfonic acid by inhibiting NF-κB signaling in mice. J. Microbiol. Biotechnol. 2023, 33, 1057–1065. [Google Scholar] [CrossRef] [PubMed]
- Caviglia, G.P.; Garrone, A.; Bertolino, C.; Vanni, R.; Bretto, E.; Poshnjari, A.; Tribocco, E.; Frara, S.; Armandi, A.; Astegiano, M.; et al. Epidemiology of Inflammatory Bowel Diseases: A Population Study in a Healthcare District of North-West Italy. J. Clin. Med. 2023, 12, 641. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.R. Intestinal musosal barrier function in health and disease. Nat. Rev. Immunol. 2009, 9, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C.; Barbara, G.; Buurman, W.; Ockhuizen, T.; Schulzke, J.D.; Serino, M.; Tilg, H.; Watson, A.; Wells, J.M. Intestinal permeability—A new target for disease prevention and therapy. BMC Gastroenterol. 2014, 14, 189. [Google Scholar] [CrossRef] [PubMed]
- Aleman, R.S.; Moncada, M.; Aryana, K.J. Leaky Gut and the Ingredients That Help Treat It: A Review. Molecules 2023, 28, 619. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, S.; Wang, S.; Nagpal, R.; Wang, B.; Jain, S.; Razazan, A.; Mishra, S.P.; Zhu, X.; Wang, Z.; Kavanagh, K.; et al. A human-origin probiotic cocktail ameliorates aging-related leaky gut and inflammation via modulating the microbiota/taurine/tight junction axis. JCI Insight 2020, 5, e132055. [Google Scholar] [CrossRef] [PubMed]
- Jeon, W.K. Leaky Gut Syndrome. Korean J. Fam. Pract. 2020, 10, 316–323. [Google Scholar]
- Yan, M.; Man, S.; Sun, B.; Guo, L.; Huang, L.; Gao, W. Gut liver brain axis in disease: The implications for therapeutic interventions. Signal Transduct. Target. Ther. 2023, 8, 443. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.Y.; Son, Y.H.; Yoo, J.W.; Joo, M.K.; Kim, D.H. Tight Junction Protein Expression-Inducing Probiotics Alleviate TNBS-Induced Cognitive Impairment with Colitis in Mice. Nutrients 2022, 14, 2975. [Google Scholar] [CrossRef]
- Aderem, A.; Ulevitch, R.J. Toll-like receptors in the induction of the innate immune response. Nature 2000, 406, 782–787. [Google Scholar] [CrossRef]
- Min, S.W.; Ryu, S.N.; Kim, D.H. Anti-inflammatory effects of black rice, cyanidin-3-O-β-D-glycoside, and its metabolites, cyanidin and protocatechuic acid. Int. Immunopharmacol. 2010, 10, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, S.; Choo-Kang, B.S.; Bundick, R.V.; Leishman, A.J.; Brewer, J.M.; McInnes, I.B.; Garside, P. Tumour necrosis factor-alpha blockade suppresses murine allergic airways inflammation. Clin. Exp. Immunol. 2008, 151, 114–122. [Google Scholar] [CrossRef]
- Morgan, M.M.; Clayton, C.C.; Heinricher, M.M. Dissociation of hyperalgesia from fever following intracerebroventricular administration of interleukin-1beta in the rat. Brain Res. 2004, 1022, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.E.; Min, S.W. Lactobacillus sakei S1 Improves Colitis Induced by 2,4,6-Trinitrobenzene Sulfonic Acid by the Inhibition of NF-κB Signaling in Mice. J. Microbiol. Biotechnol. 2020, 30, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Fiorucci, S.; Mencrelli, A.; Palazzetti, B.; Sprague, A.G.; Distrutti, E.; Morelli, A.; Novobrantseva, T.I.; Cirino, G.; Koteliansky, V.E.; de Fougerolles, A.R. Importance of innate immunity and collagen binding integrin alpha1beta1 in TNBS-induced colitis. Immunity 2002, 17, 769–780. [Google Scholar] [CrossRef] [PubMed]
- Neurath, M.F.; Fuss, I.; Pasparakis, M.; Alexopoulou, L.; Haralambous, S.; Meyer zum Büschenfelde, K.H.; Strober, W.; Kollias, G. Predominant pathogenic role of tumor necrosis factor in experimental colitis in mice. Eur. J. Immunol. 1997, 27, 1743–1750. [Google Scholar] [CrossRef]
- Fiorucci, S.; Mencarelli, A.; Palazzetti, B.; Distrutti, E.; Vergnolle, N.; Hollenberg, M.D.; Wallace, J.L.; Morelli, A.; Cirino, G. Proteinase-activated receptor (PAR)-2 is an anti-inflammatory signal for colonic lamina propria lymphocytes in a mouse model of colitis. Proc. Natl. Acad. Sci. USA 2001, 98, 13936–13941. [Google Scholar] [CrossRef]
- Rao, K.; Qin, S.; Yang, Y.; Zhan, K.; Wu, H.; Zheng, H.; Huang, S. Shenling Baizhu Powder Alleviates TNBS-Induced Colitis in Rats by Improving Intestinal Epithelial Permeability and Inhibiting Inflammation Through the TLR5/MyD88/NF-κB Pathway. Front. Pharmacol. 2022, 13, 883918. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.E.; Han, M.J.; Kim, S.Y.; Kim, D.H. Lactobacillus plantarum CLP-0611 ameliorates colitis in mice by polarizing M1 to M2-like macrophages. Int. Immunopharmacol. 2014, 21, 186–192. [Google Scholar] [CrossRef]
- Jang, S.E.; Joh, E.H.; Lee, H.Y.; Ahn, Y.T.; Lee, J.H.; Huh, C.S.; Han, M.J.; Kim, D.H. Lactobacillus plantarum HY7712 ameliorates cyclophosphamide-induced immunosuppression in mice. J. Microbiol. Biotechnol. 2013, 23, 414–421. [Google Scholar] [CrossRef]
- Jang, S.E.; Trinh, H.T.; Chung, Y.H.; Han, M.J.; Kim, D.H. Anti-scratching behavioral effect of Lactobacillus plantarum PM008 isolated from kimchi in mice. Immunopharmacol. Immunotoxicol. 2011, 33, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Gomaa, E.Z. Human gut microbiota/microbiome in health and diseases: A review. Antonie Van Leeuwenhoek 2020, 113, 2019–2040. [Google Scholar] [CrossRef] [PubMed]
- Borchers, A.T.; Selmi, C.; Meyers, F.J.; Keen, C.L.; Gershwin, M.E. Probiotics and immunity. J. Gastroenterol. 2009, 44, 26–46. [Google Scholar] [CrossRef] [PubMed]
- Park, K.Y.; Jeong, J.K.; Lee, Y.E. Health benefits of kimchi (Korean fermented vegetables) as a probiotic food. J. Med. Food 2014, 17, 6–20. [Google Scholar] [CrossRef] [PubMed]
- d’Angelo, M.; Brandolini, L.; Catanesi, M.; Castelli, V.; Giorgio, C.; Alfonsetti, M.; Tomassetti, M.; Zippoli, M.; Benedetti, E.; Cesta, M.C.; et al. Differential Effects of Nonsteroidal Anti-Inflammatory Drugs in an In Vitro Model of Human Leaky Gut. Cells 2023, 12, 728. [Google Scholar] [CrossRef] [PubMed]
- Kos, B.; Suskovic, J.; Vukovic, S.; Simpraga, M.; Frece, J.; Matosic, S. Adhesion and aggregation ability of probiotic strain Lactobacillus acidophilus M92. J. Appl. Microbiol. 2003, 94, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Joh, E.H.; Lee, I.A.; Jung, I.H.; Kim, D.H. Ginsenoside Rb1 and its metabolite compound K inhibit IRAK-1 activation—The key step of inflammation. Biochem. Pharmacol. 2011, 82, 278–289. [Google Scholar] [CrossRef] [PubMed]
- Joh, E.H.; Kim, D.H. Kalopanaxsaponin A ameliorates experimental colitis in mice by inhibiting IRAK-1 activation in the NF-κB and MAPK pathways. Br. J. Pharmacol. 2011, 162, 1731–1742. [Google Scholar] [CrossRef]
- Lee, K.W.; Park, J.Y.; Sa, H.D.; Jeong, J.H.; Jin, D.E.; Heo, H.J.; Kim, J.H. Probiotic properties of Pediococcus strains isolated from Jeotgals, salted and fermented Korean sea-food. Ananerobe 2014, 28, 199–206. [Google Scholar] [CrossRef]
- Lim, S.M.; Kim, D.H. Bifidobacterium adolescentis IM38 ameliorates high-fat diet-induced colitis in mice by inhibiting NF-κB activation and lipopolysaccharide production by gut microbiota. Nutr. Res. 2017, 41, 86–96. [Google Scholar] [CrossRef]
- Kim, D.H.; Cheon, J.H. Pathogenesis of Inflammatory Bowel Disease and Recent Advances in Biologic Therapies. Immune Netw. 2017, 17, 25–40. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.A.; Rodrigues, B.L.; Ayrizono, M.L.; Leal, R.F. The Immunological Basis of Inflammatory Bowel Disease. Gastroenterol. Res. Pract. 2016, 2016, 2097274. [Google Scholar] [CrossRef] [PubMed]
- Yeshi, K.; Ruscher, R.; Hunter, L.; Daly, N.L.; Loukas, A.; Wangchuk, P. Revisiting Inflammatory Bowel Disease: Pathology, Treatments, Challenges and Emerging Therapeutics Including Drug Leads from Natural Products. J. Clin. Med. 2020, 9, 1273. [Google Scholar] [CrossRef] [PubMed]
- Perrotta, C.; Pellegrino, P.; Moroni, E.; De Palma, C.; Cervia, D.; Danelli, P.; Clementi, E. Five-aminosalicylic Acid: An update for the reappraisal of an old drug. Gastroenterol. Res. Pract. 2015, 2015, 45689. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.S.; Mayers, J.R.; Zhang, Y.; Bhosle, A.; Glasser, N.R.; Nguyen, L.H.; Ma, W.; Bae, S.; Branck, T.; Song, K.; et al. Gut microbial metabolism of 5-ASA diminishes its clinical efficacy in inflammatory bowel disease. Nat. Med. 2023, 29, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Noth, R.; Lange-Grumfeld, J.; Stüber, E.; Kruse, M.L.; Ellrichmann, M.; Häsler, R.; Hampe, J.; Bewig, B.; Rosenstiel, P.; Schreiber, S.; et al. Increased intestinal permeability and tight junction disruption by altered expression and localization of occludin in a murine graft versus host disease model. BMC Gastroenterol. 2011, 11, 109. [Google Scholar] [CrossRef]
- Lee, B.; Moon, K.M.; Kim, C.Y. Tight Junction in the Intestinal Epithelium: Its Association with Diseases and Regulation by Phytochemicals. J. Immunol. Res. 2018, 2018, 2645465. [Google Scholar] [CrossRef]
- Michielan, A.; D’Incà, R. Intestinal Permeability in Inflammatory Bowel Disease: Pathogenesis, Clinical Evaluation, and Therapy of Leaky Gut. Mediat. Inflamm. 2015, 2015, 628157. [Google Scholar] [CrossRef]
- Luo, M.; Xin, R.J.; Hu, F.R.; Yao, L.; Hu, S.J.; Bai, F.H. Role of gut microbiota in the pathogenesis and therapeutics of minimal hepatic encephalopathy via the gut-liver-brain axis. World J. Gastroenterol. 2023, 29, 144–156. [Google Scholar] [CrossRef]
- Yoo, J.W.; Shin, Y.J.; Ma, X.; Son, Y.H.; Jang, H.M.; Lee, C.K.; Kim, D.H. The Alleviation of Gut Microbiota-Induced Depression and Colitis in Mice by Anti-Inflammatory Probiotics NK151, NK173, and NK175. Nutrients 2022, 14, 2080. [Google Scholar] [CrossRef]
- Jang, S.E.; Jeong, J.J.; Kim, J.K.; Han, M.J.; Kim, D.H. Simultaneous Amelioration of Colitis and Liver Injury in Mice by Bifidobacterium longum LC67 and Lactobacillus plantarum LC27. Sci. Rep. 2018, 8, 7500. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Kim, S.W.; Verma, R.; Noh, J.; Park, J.C.; Park, S.; Lee, H.; Park, H.E.; Kim, C.J.; Byun, S.; et al. Probiotic Consortium Confers Synergistic Anti-Inflammatory Effects in Inflammatory Disorders. Nutrients 2024, 16, 790. [Google Scholar] [CrossRef] [PubMed]
- Kimura, A.; Kishimoto, T. IL-6: Regulator of Treg/Th17 balance. Eur. J. Immunol. 2010, 40, 1830–1835. [Google Scholar] [CrossRef]

| Viable Cell Counts (CFU/mL) | Auto-Aggregation (%) | |||
|---|---|---|---|---|
| Gastric Juice | Intestinal Juice | Adhesion | ||
| Weissella koreensis KJ | 2.5 ± 1.3 × 107 | 1.5 ± 0.4 × 108 | 3.2 ± 0.9 × 105 | 40.3 ± 4.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.-J.; Lee, H.; Oh, Y.S.; Jang, S.-E. Weissella koreensis KJ, Which Increases Gut Tight Junction Protein Expression, Alleviates TNBS-Induced Colitis by Suppressing Inflammatory Cytokines. Microbiol. Res. 2024, 15, 721-733. https://doi.org/10.3390/microbiolres15020047
Kim K-J, Lee H, Oh YS, Jang S-E. Weissella koreensis KJ, Which Increases Gut Tight Junction Protein Expression, Alleviates TNBS-Induced Colitis by Suppressing Inflammatory Cytokines. Microbiology Research. 2024; 15(2):721-733. https://doi.org/10.3390/microbiolres15020047
Chicago/Turabian StyleKim, Kyung-Joo, Hyoleem Lee, Yoon Sin Oh, and Se-Eun Jang. 2024. "Weissella koreensis KJ, Which Increases Gut Tight Junction Protein Expression, Alleviates TNBS-Induced Colitis by Suppressing Inflammatory Cytokines" Microbiology Research 15, no. 2: 721-733. https://doi.org/10.3390/microbiolres15020047
APA StyleKim, K.-J., Lee, H., Oh, Y. S., & Jang, S.-E. (2024). Weissella koreensis KJ, Which Increases Gut Tight Junction Protein Expression, Alleviates TNBS-Induced Colitis by Suppressing Inflammatory Cytokines. Microbiology Research, 15(2), 721-733. https://doi.org/10.3390/microbiolres15020047






