Probiotics as Therapeutic Tools against Pathogenic Biofilms: Have We Found the Perfect Weapon?
Abstract
1. Introduction
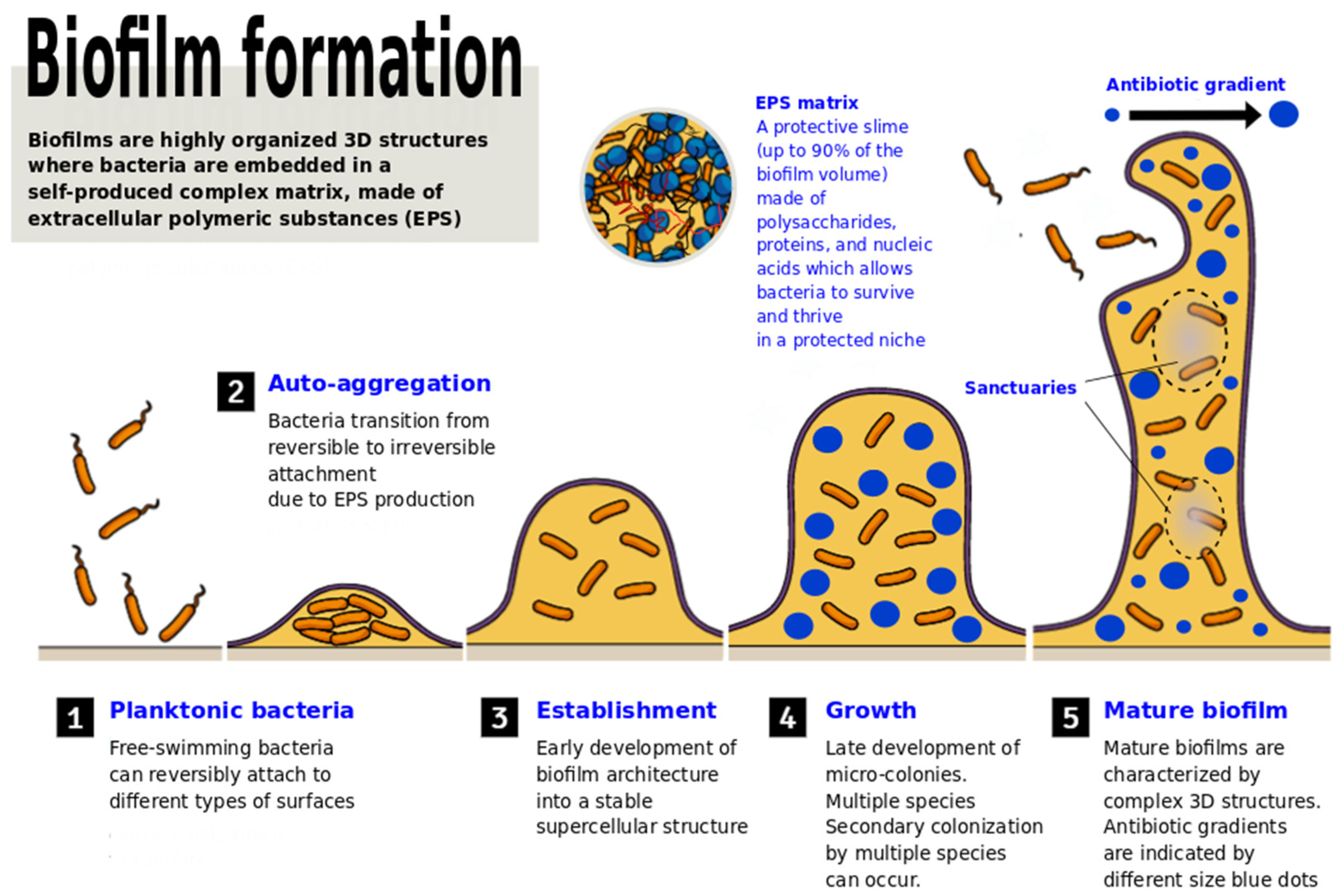
2. Biofilms: The Good, the Bad, and the Ugly
3. Methods: Dataset and Databases Used for Literature Searching
4. Methods for the Detection and Evaluation of Antibiofilm Activity
5. The Battle of LAB against Pathogenic Biofilms
5.1. How Lactobacillus May Contrast Biofilm Formation and Stability
5.2. How Bifodobacteria May Contrast Pathogenic Biofilms
6. Lactobacilli and Bifidobacteria as Interfering Agents against Quorum-Sensing
7. Strategies and Mechanisms Used by LAB to Fight Biofilms
8. Discussion
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Khan, F.; Pham, D.T.N.; Oloketuyi, S.F.; Kim, Y.-M. Antibiotics Application Strategies to Control Biofilm Formation in Pathogenic Bacteria. Curr. Pharm. Biotechnol. 2020, 21, 270–286. [Google Scholar] [CrossRef]
- Mann, R.; Holmes, A.; McNeilly, O.; Cavaliere, R.; Sotiriou, G.A.; Rice, S.A.; Gunawan, C. Evolution of biofilm-forming pathogenic bacteria in the presence of nanoparticles and antibiotic: Adaptation phenomena and cross-resistance. J. Nanobiotechnol. 2021, 19, 1–17. [Google Scholar] [CrossRef]
- Moons, P.; Michiels, C.; Aertsen, A. Bacterial interactions in biofilms. Crit. Rev. Microbiol. 2009, 35, 157–168. [Google Scholar] [CrossRef] [PubMed]
- Karygianni, L.; Ren, Z.; Koo, H.; Thurnheer, T. Biofilm Matrixome: Extracellular Components in Structured Microbial Communities. Trends Microbiol. 2020, 28, 668–681. [Google Scholar] [CrossRef]
- Bakhtiari, N.M.; Gooraninezhad, S.; Karami, M. Biofilm-Producing Ability of Bovine Extraintestinal Pathogenic Escherichia coli and Its Correlation with Attachment Factors. Jundishapur J. Heal. Sci. 2018, 10. [Google Scholar] [CrossRef]
- Cergole-Novella, M.C.; Pignatari, A.C.; Guth, B.E. Adhesion, biofilm and genotypic characteristics of antimicrobial resistant Escherichia coli isolates. Braz. J. Microbiol. 2015, 46, 167–171. [Google Scholar] [CrossRef][Green Version]
- Olsen, I. Biofilm-specific antibiotic tolerance and resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 877–886. [Google Scholar] [CrossRef]
- Fakruddin, M.D.; Bin Mannan, K.S.; Mazumdar, R.M. Correlation Between in vitro Biofilm Formation and Virulence Properties of Extra-Intestinal Pathogenic Escherichia Coli (Expec). Online J. Biol. Sci. 2014, 14, 261–270. [Google Scholar] [CrossRef][Green Version]
- Wood, T.K.; Barrios, A.F.G.; Herzberg, M.; Lee, J. Motility influences biofilm architecture in Escherichia coli. Appl. Microbiol. Biotechnol. 2006, 72, 361–367. [Google Scholar] [CrossRef]
- Prüß, B.M.; Besemann, C.; Denton, A.; Wolfe, A.J. A Complex Transcription Network Controls the Early Stages of Biofilm Development by Escherichia coli. J. Bacteriol. 2006, 188, 3731–3739. [Google Scholar] [CrossRef]
- Cai, P.; Sun, X.; Wu, Y.; Gao, C.; Mortimer, M.; Holden, P.A.; Redmile-Gordon, M.; Huang, Q. Soil biofilms: Microbial interactions, challenges, and advanced techniques for ex-situ characterization. Soil Ecol. Lett. 2019, 1, 85–93. [Google Scholar] [CrossRef]
- Yi, L.; Li, J.; Liu, B.; Wang, Y. Advances in research on signal molecules regulating biofilms. World J. Microbiol. Biotechnol. 2019, 35, 130. [Google Scholar] [CrossRef]
- Campoccia, D.; Mirzaei, R.; Montanaro, L.; Arciola, C.R. Hijacking of immune defences by biofilms: A multifront strategy. Biofouling 2019, 35, 1055–1074. [Google Scholar] [CrossRef] [PubMed]
- Esanchez-Vizuete, P.; Eorgaz, B.; Eaymerich, S.; Le Coq, D.; Ebriandet, R. Pathogens protection against the action of disinfectants in multispecies biofilms. Front. Microbiol. 2015, 6, 705. [Google Scholar] [CrossRef]
- González, J.F.; Hahn, M.; Gunn, J.S. Chronic biofilm-based infections: Skewing of the immune response. Pathog. Dis. 2018, 76. [Google Scholar] [CrossRef]
- Sharma, D.; Misba, L.; Khan, A.U. Antibiotics versus biofilm: An emerging battleground in microbial communities. Antimicrob. Resist. Infect. Control 2019, 8, 76. [Google Scholar] [CrossRef]
- CDC Antibiotic Resistance Threats in the United State; Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019; pp. 1–113. [CrossRef]
- Manyi-Loh, C.; Mamphweli, S.; Meyer, E.; Okoh, A. Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Molecules 2018, 23, 795. [Google Scholar] [CrossRef] [PubMed]
- Marquardt, R.R.; Li, S. Antimicrobial resistance in livestock: Advances and alternatives to antibiotics. Anim. Front. 2018, 8, 30–37. [Google Scholar] [CrossRef]
- Bjorkman, I.; Berg, J.; Roing, M.; Erntell, M.; Lundborg, C.S. Perceptions among Swedish hospital physicians on prescribing of antibiotics and antibiotic resistance. BMJ Qual. Saf. 2010, 19, e8. [Google Scholar] [CrossRef]
- Kumar, S.; Little, P.; Britten, N. Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study. BMJ 2003, 326, 138. [Google Scholar] [CrossRef] [PubMed]
- Machowska, A.; Lundborg, C.S. Drivers of Irrational Use of Antibiotics in Europe. Int. J. Environ. Res. Public Health 2018, 16, 27. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, L.; McKee, M. Factors influencing antibiotic prescribing in China: An exploratory analysis. Health Policy 2009, 90, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Sirota, M.; Round, T.; Samaranayaka, S.; Kostopoulou, O. Expectations for antibiotics increase their prescribing: Causal evidence about localized impact. Health Psychol. 2017, 36, 402–409. [Google Scholar] [CrossRef]
- Ouwehand, A.C.; Tiihonen, K.; Saarinen, M.; Putaala, H.; Rautonen, N. Influence of a combination ofLactobacillus acidophilusNCFM and lactitol on healthy elderly: Intestinal and immune parameters. Br. J. Nutr. 2008, 101, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Binda, S.; Hill, C.; Johansen, E.; Obis, D.; Pot, B.; Sanders, M.E.; Tremblay, A.; Ouwehand, A.C. Criteria to Qualify Microorganisms as “Probiotic” in Foods and Dietary Supplements. Front. Microbiol. 2020, 11, 1662. [Google Scholar] [CrossRef]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. Expert Consensus Document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef]
- Collins, S.; Reid, G. Distant Site Effects of Ingested Prebiotics. Nutrients 2016, 8, 523. [Google Scholar] [CrossRef] [PubMed]
- Fijan, S.; Frauwallner, A.; Langerholc, T.; Krebs, B.; Younes, J.A.T.H.; Heschl, A.; Turk, D.M.; Rogelj, I. Efficacy of Using Probiotics with Antagonistic Activity against Pathogens of Wound Infections: An Integrative Review of Literature. BioMed Res. Int. 2019, 2019, 7585486. [Google Scholar] [CrossRef] [PubMed]
- Szántó, M.; Dózsa, A.; Antal, D.; Szabó, K.; Kemény, L.; Bai, P. Targeting the gut-skin axis—Probiotics as new tools for skin disorder management? Exp. Dermatol. 2019, 28, 1210–1218. [Google Scholar] [CrossRef] [PubMed]
- Kothari, D.; Patel, S.; Kim, S.-K. Probiotic supplements might not be universally-effective and safe: A review. Biomed. Pharmacother. 2018, 111, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Lerner, A.; Shoenfeld, Y.; Matthias, T. Probiotics: If It Does Not Help It Does Not Do Any Harm. Really? Microorganisms 2019, 7, 104. [Google Scholar] [CrossRef] [PubMed]
- Barzegari, A.; Kheyrolahzadeh, K.; Khatibi, S.M.H.; Sharifi, S.; Memar, M.Y.; Vahed, S.Z. The Battle of Probiotics and Their Derivatives against Biofilms. Infect. Drug Resist. 2020, 13, 659–672. [Google Scholar] [CrossRef]
- Bustamante, M.; Oomah, B.D.; Oliveira, W.P.; Burgos-Díaz, C.; Rubilar, M.; Shene, C. Probiotics and prebiotics potential for the care of skin, female urogenital tract, and respiratory tract. Folia Microbiol. 2019, 65, 245–264. [Google Scholar] [CrossRef] [PubMed]
- Sib, E.; Voigt, A.M.; Wilbring, G.; Schreiber, C.; Faerber, H.; Skutlarek, D.; Parcina, M.; Mahn, R.; Wolf, D.; Brossart, P.; et al. Antibiotic resistant bacteria and resistance genes in biofilms in clinical wastewater networks. Int. J. Hyg. Environ. Health 2019, 222, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Wickremasinghe, H.; Yu, H.; Azad, M.; Zhao, J.; Bergen, P.; Velkov, T.; Zhou, Q.; Zhu, Y.; Li, J. Clinically Relevant Concentrations of Polymyxin B and Meropenem Synergistically Kill Multidrug-Resistant Pseudomonas aeruginosa and Minimize Biofilm Formation. Antibiotics 2021, 10, 405. [Google Scholar] [CrossRef]
- Rao, Y.; Shang, W.; Yang, Y.; Zhou, R.; Rao, X. Fighting Mixed-Species Microbial Biofilms With Cold Atmospheric Plasma. Front. Microbiol. 2020, 11, 1000. [Google Scholar] [CrossRef]
- Orazi, G.; O’Toole, G.A. “It Takes a Village”: Mechanisms Underlying Antimicrobial Recalcitrance of Polymicrobial Biofilms. J. Bacteriol. 2019, 202, e00530-19. [Google Scholar] [CrossRef] [PubMed]
- Trifilio, S.; Zhou, Z.; Fong, J.; Zomas, A.; Liu, D.; Zhao, C.; Zhang, J.; Mehta, J. Polymicrobial bacterial or fungal infections: Incidence, spectrum of infection, risk factors, and clinical outcomes from a large hematopoietic stem cell transplant center. Transpl. Infect. Dis. 2015, 17, 267–274. [Google Scholar] [CrossRef]
- Liu, Z.; Li, L.; Fang, Z.; Lee, Y.; Zhao, J.; Zhang, H.; Chen, W.; Li, H.; Lu, W. Integration of Transcriptome and Metabolome Reveals the Genes and Metabolites Involved in Bifidobacterium bifidum Biofilm Formation. Int. J. Mol. Sci. 2021, 22, 7596. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, B.R.; Malof, M.E.; Shaw, L.N. A global transcriptomic analysis of Staphylococcus aureus biofilm formation across diverse clonal lineages. Microb. Genom. 2021, 7, 000598. [Google Scholar] [CrossRef] [PubMed]
- Hermsen, R.; Deris, J.B.; Hwa, T. On the rapidity of antibiotic resistance evolution facilitated by a concentration gradient. Proc. Natl. Acad. Sci. USA 2012, 109, 10775–10780. [Google Scholar] [CrossRef]
- Sandoval-Motta, S.; Aldana, M. Adaptive resistance to antibiotics in bacteria: A systems biology perspective. Wiley Interdiscip. Rev. Syst. Biol. Med. 2016, 8, 253–267. [Google Scholar] [CrossRef] [PubMed]
- Ren, D.; Li, C.; Qin, Y.; Yin, R.; Du, S.; Ye, F.; Liu, C.; Liu, H.; Wang, M.; Li, Y.; et al. In vitro evaluation of the probiotic and functional potential of Lactobacillus strains isolated from fermented food and human intestine. Anaerobe 2014, 30, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Favaro, L.; Basaglia, M.; Casella, S.; Hue, I.; Dousset, X.; de Melo Franco, D.G.; Todorov, S. Bacteriocinogenic potential and safety evaluation of non-starter Enterococcus faecium strains isolated from home made white brine cheese. Food Microbiol. 2014, 38, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-N.; Han, Y.; Zhou, Z.-J. Lactic acid bacteria in traditional fermented Chinese foods. Food Res. Int. 2011, 44, 643–651. [Google Scholar] [CrossRef]
- Palomino, J.M.; del Árbol, J.T.; Benomar, N.; Abriouel, H.; Cañamero, M.M.; Gálvez, A.; Pulido, R.P. Application of Lactobacillus plantarum Lb9 as starter culture in caper berry fermentation. LWT 2015, 60, 788–794. [Google Scholar] [CrossRef]
- Han, S.; Lu, Y.; Xie, J.; Fei, Y.; Zheng, G.; Wang, Z.; Liu, J.; Lv, L.; Ling, Z.; Berglund, B.; et al. Probiotic Gastrointestinal Transit and Colonization After Oral Administration: A Long Journey. Front. Cell. Infect. Microbiol. 2021, 11, 102. [Google Scholar] [CrossRef] [PubMed]
- Salas-Jara, M.J.; Ilabaca, A.; Vega, M.; García, A. Biofilm Forming Lactobacillus: New Challenges for the Development of Probiotics. Microorganisms 2016, 4, 35. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zijlstra, R.T.; Gänzle, M.G. Feeding Limosilactobacillus fermentum K9-2 and Lacticaseibacillus casei K9-1, or Limosilactobacillus reuteri TMW1.656 Reduces Pathogen Load in Weanling Pigs. Front. Microbiol. 2020, 11, 3187. [Google Scholar] [CrossRef]
- Aoudia, N.; Rieu, A.; Briandet, R.; Deschamps, J.; Chluba, J.; Jego, G.; Garrido, C.; Guzzo, J. Biofilms of Lactobacillus plantarum and Lactobacillus fermentum: Effect on stress responses, antagonistic effects on pathogen growth and immunomodulatory properties. Food Microbiol. 2016, 53, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.; Usman, J.; Kaleem, F.; Omair, M.; Khalid, A.; Iqbal, M. Evaluation of different detection methods of biofilm formation in the clinical isolates. Braz. J. Infect. Dis. 2011, 15, 305–311. [Google Scholar] [CrossRef]
- Xu, Z.; Liang, Y.; Lin, S.; Chen, D.; Li, B.; Li, L.; Deng, Y. Crystal Violet and XTT Assays on Staphylococcus aureus Biofilm Quantification. Curr. Microbiol. 2016, 73, 474–482. [Google Scholar] [CrossRef]
- Roberts, A.E.; Kragh, K.N.; Bjarnsholt, T.; Diggle, S.P. The Limitations of In Vitro Experimentation in Understanding Biofilms and Chronic Infection. J. Mol. Biol. 2015, 427, 3646–3661. [Google Scholar] [CrossRef]
- Stepanović, S.; Vuković, D.; Hola, V.; DI Bonaventura, G.; Djukić, S.; Ćirković, I.; Ruzicka, F. Quantification of biofilm in microtiter plates: Overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS 2007, 115, 891–899. [Google Scholar] [CrossRef]
- Coenye, T.; Nelis, H.J. In vitro and in vivo model systems to study microbial biofilm formation. J. Microbiol. Methods 2010, 83, 89–105. [Google Scholar] [CrossRef]
- Berry, R.E.; Klumpp, D.J.; Schaeffer, A.J. Urothelial Cultures Support Intracellular Bacterial Community Formation by Uropathogenic Escherichia coli. Infect. Immun. 2009, 77, 2762–2772. [Google Scholar] [CrossRef]
- Rudney, J.; Chen, R.; Lenton, P.; Li, J.; Li, Y.; Jones, R.; Reilly, C.; Fok, A.; Aparicio, C. A reproducible oral microcosm biofilm model for testing dental materials. J. Appl. Microbiol. 2012, 113, 1540–1553. [Google Scholar] [CrossRef]
- Anderl, J.N.; Franklin, M.J.; Stewart, P. Role of Antibiotic Penetration Limitation in Klebsiella pneumoniae Biofilm Resistance to Ampicillin and Ciprofloxacin. Antimicrob. Agents Chemother. 2000, 44, 1818–1824. [Google Scholar] [CrossRef] [PubMed]
- Zuroff, T.R.; Bernstein, H.; Lloyd-Randolfi, J.; Jimenez-Taracido, L.; Stewart, P.S.; Carlson, R.P. Robustness analysis of culturing perturbations on Escherichia coli colony biofilm beta-lactam and aminoglycoside antibiotic tolerance. BMC Microbiol. 2010, 10, 185. [Google Scholar] [CrossRef]
- Christensen, G.D.; Simpson, W.A.; Younger, J.J.; Baddour, L.M.; Barrett, F.F.; Melton, D.M.; Beachey, E.H. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: A quantitative model for the adherence of staphylococci to medical devices. J. Clin. Microbiol. 1985, 22, 996–1006. [Google Scholar] [CrossRef] [PubMed]
- Genevaux, P.; Muller, S.; Bauda, P. A rapid screening procedure to identify mini-Tn10 insertion mutants of Escherichia coli K-12 with altered adhesion properties. FEMS Microbiol. Lett. 1996, 142, 27–30. [Google Scholar] [CrossRef]
- Chavant, P.; Gaillard-Martinie, B.; Talon, R.; Hébraud, M.; Bernardi, T. A new device for rapid evaluation of biofilm formation potential by bacteria. J. Microbiol. Methods 2007, 68, 605–612. [Google Scholar] [CrossRef]
- Ceri, H.; Olson, M.; Stremick, C.; Read, R.R.; Morck, D.; Buret, A. The Calgary Biofilm Device: New Technology for Rapid Determination of Antibiotic Susceptibilities of Bacterial Biofilms. J. Clin. Microbiol. 1999, 37, 1771–1776. [Google Scholar] [CrossRef]
- Heydorn, A.; Nielsen, A.T.; Hentzer, M.; Sternberg, C.; Givskov, M.; Ersbøll, B.K.; Molin, S. Quantification of biofilm structures by the novel computer program comstat. Microbiology 2000, 146, 2395–2407. [Google Scholar] [CrossRef]
- Ghigo, J.-M. Natural conjugative plasmids induce bacterial biofilm development. Nature 2001, 412, 442–445. [Google Scholar] [CrossRef]
- Van Der Mei, H.; Free, R.; Van Weissenbruch, R.; Busscher, H.; Elving, G.; Albers, F.J. Effect of probiotic bacteria on prevalence of yeasts in oropharyngeal biofilms on silicone rubber voice prostheses in vitro. J. Med Microbiol. 2000, 49, 713–718. [Google Scholar] [CrossRef]
- Donlan, R.M.; Piede, J.A.; Heyes, C.D.; Sanii, L.; Murga, R.; Edmonds, P.; El-Sayed, I.; El-Sayed, M.A. Model System for Growing and Quantifying Streptococcus pneumoniae Biofilms In Situ and in Real Time. Appl. Environ. Microbiol. 2004, 70, 4980–4988. [Google Scholar] [CrossRef] [PubMed]
- Bueno, J. Anti-Biofilm Drug Susceptibility Testing Methods: Looking for New Strategies against Resistance Mechanism. J. Microb. Biochem. Technol. 2011, s3. [Google Scholar] [CrossRef]
- Perrin, A.; Herbelin, P.; Jorand, F.P.A.; Skali-Lami, S.; Mathieu, L. Design of a rotating disk reactor to assess the colonization of biofilms by free-living amoebae under high shear rates. Biofouling 2018, 34, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-Y.; Sun, K.; Abulimiti, A.; Xu, P.-P.; Li, Z.-Y. Microfluidic System for Observation of Bacterial Culture and Effects on Biofilm Formation at Microscale. Micromachines 2019, 10, 606. [Google Scholar] [CrossRef]
- Schwartz, K.; Stephenson, R.; Hernandez, M.; Jambang, N.; Boles, B.R. The Use of Drip Flow and Rotating Disk Reactors for Staphylococcus aureus Biofilm Analysis. J. Vis. Exp. 2010, e2470. [Google Scholar] [CrossRef]
- Shang, L.; Deng, D.; Buskermolen, J.K.; Roffel, S.; Janus, M.M.; Krom, B.P.; Crielaard, W.; Gibbs, S. Commensal and Pathogenic Biofilms Alter Toll-Like Receptor Signaling in Reconstructed Human Gingiva. Front. Cell. Infect. Microbiol. 2019, 9, 282. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Park, H.-D.; Chung, S. Microfluidic Approaches to Bacterial Biofilm Formation. Molecules 2012, 17, 9818–9834. [Google Scholar] [CrossRef] [PubMed]
- Grønnemose, R.B.; Saederup, K.L.; Kolmos, H.J.; Hansen, S.; Asferg, C.A.; Rasmussen, K.J.; Palarasah, Y.; Andersen, T.E. A novel in vitro model for haematogenous spreading ofS. aureusdevice biofilms demonstrating clumping dispersal as an advantageous dissemination mechanism. Cell. Microbiol. 2017, 19, e12785. [Google Scholar] [CrossRef] [PubMed]
- Moreau-Marquis, S.; Redelman, C.V.; Stanton, B.A.; Anderson, G.G. Co-culture Models of Pseudomonas aeruginosa Biofilms Grown on Live Human Airway Cells. J. Vis. Exp. 2010, e2186. [Google Scholar] [CrossRef]
- Sternberg, C.; Bjarnsholt, T.; Shirtliff, M. Methods for Dynamic Investigations of Surface-Attached In Vitro Bacterial and Fungal Biofilms. Microb. Biofilms 2014, 1147, 3–22. [Google Scholar] [CrossRef]
- Wong, E.H.J.; Ng, C.G.; Goh, K.L.; Vadivelu, J.; Ho, B.; Loke, M.F. Metabolomic analysis of low and high biofilm-forming Helicobacter pylori strains. Sci. Rep. 2018, 8, 1409. [Google Scholar] [CrossRef]
- Munusamy, K.; Loke, M.F.; Vadivelu, J.; Tay, S.T. LC-MS analysis reveals biological and metabolic processes essential for Candida albicans biofilm growth. Microb. Pathog. 2020, 152, 104614. [Google Scholar] [CrossRef] [PubMed]
- An, A.Y.; Choi, K.-Y.G.; Baghela, A.S.; Hancock, R.E.W. An Overview of Biological and Computational Methods for Designing Mechanism-Informed Anti-biofilm Agents. Front. Microbiol. 2021, 12, 845. [Google Scholar] [CrossRef] [PubMed]
- Turner, N.A.; Sharma-Kuinkel, B.K.; Maskarinec, S.; Eichenberger, E.; Shah, P.P.; Carugati, M.; Holland, T.L.; Fowler, V.G. Methicillin-resistant Staphylococcus aureus: An overview of basic and clinical research. Nat. Rev. Genet. 2019, 17, 203–218. [Google Scholar] [CrossRef]
- Sikorska, H.; Smoragiewicz, W. Role of probiotics in the prevention and treatment of meticillin-resistant Staphylococcus aureus infections. Int. J. Antimicrob. Agents 2013, 42, 475–481. [Google Scholar] [CrossRef]
- Melo, T.A.; Dos Santos, T.F.; De Almeida, M.E.; Junior, L.A.G.F.; Andrade, E.F.; Rezende, R.P.; Marques, L.M.; Romano, C.C. Inhibition of Staphylococcus aureus biofilm by Lactobacillus isolated from fine cocoa. BMC Microbiol. 2016, 16, 250. [Google Scholar] [CrossRef] [PubMed]
- Gomaa, S.; Serry, F.; Abdellatif, H.; Abbas, H. Elimination of multidrug-resistant Proteus mirabilis biofilms using bacteriophages. Arch. Virol. 2019, 164, 2265–2275. [Google Scholar] [CrossRef] [PubMed]
- Shaaban, M.; Abd El-Rahman, O.A.; Al-Qaidi, B.; Ashour, H.M. Antimicrobial and Antibiofilm Activities of Probiotic Lactobacilli on Antibiotic-Resistant Proteus Mirabilis. Microorganisms 2020, 8, 960. [Google Scholar] [CrossRef]
- Campbell, K. Oral microbiome findings challenge dentistry dogma. Nature 2021. [Google Scholar] [CrossRef] [PubMed]
- Wasfi, R.; El-Rahman, O.A.A.; Zafer, M.M.; Ashour, H.M. Probiotic Lactobacillu ssp. inhibit growth, biofilm formation and gene expression of caries-inducingStreptococcus mutans. J. Cell. Mol. Med. 2018, 22, 1972–1983. [Google Scholar] [CrossRef]
- Tan, Y.; Leonhard, M.; Moser, D.; Schneider-Stickler, B. Inhibition activity of Lactobacilli supernatant against fungal-bacterial multispecies biofilms on silicone. Microb. Pathog. 2017, 113, 197–201. [Google Scholar] [CrossRef]
- Vuotto, C.; Barbanti, F.; Mastrantonio, P.; Donelli, G. Lactobacillus brevisCD2 inhibitsPrevotella melaninogenicabiofilm. Oral Dis. 2013, 20, 668–674. [Google Scholar] [CrossRef]
- Kaur, S.; Sharma, P.; Kalia, N.; Singh, J.; Kaur, S. Anti-biofilm Properties of the Fecal Probiotic Lactobacilli Against Vibrio spp. Front. Cell. Infect. Microbiol. 2018, 8, 120. [Google Scholar] [CrossRef]
- Phukan, N.; Brooks, A.; Simoes-Barbosa, A. A Cell Surface Aggregation-Promoting Factor from Lactobacillus gasseri Contributes to Inhibition of Trichomonas vaginalis Adhesion to Human Vaginal Ectocervical Cells. Infect. Immun. 2018, 86. [Google Scholar] [CrossRef]
- Song, Y.-G.; Lee, S.-H. Inhibitory effects of Lactobacillus rhamnosus and Lactobacillus casei on Candida biofilm of denture surface. Arch. Oral Biol. 2017, 76, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, P. Use of Lactobacillus casei Subspecies Rhamnosus GG and Gastrointestinal Colonization by Candida Species in Preterm Neonates. J. Pediatr. Gastroenterol. Nutr. 2007, 45, S190–S194. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, V.H.; Wang, Y.; Bandara, H.M.H.N.; Mayer, M.P.A.; Samaranayake, L.P. Probiotic lactobacilli inhibit early stages of Candida albicans biofilm development by reducing their growth, cell adhesion, and filamentation. Appl. Microbiol. Biotechnol. 2016, 100, 6415–6426. [Google Scholar] [CrossRef] [PubMed]
- Bambirra, F.; Lima, K.; Franco, B.; Cara, D.; Nardi, R.; Barbosa, F.; Nicoli, J. Protective effect of Lactobacillus sakei 2a against experimental challenge with Listeria monocytogenes in gnotobiotic mice. Lett. Appl. Microbiol. 2007, 45, 663–667. [Google Scholar] [CrossRef]
- Fangous, M.-S.; Gosset, P.; Galakhoff, N.; Gouriou, S.; Guilloux, C.-A.; Payan, C.; Vallet, S.; Héry-Arnaud, G.; Le Berre, R. Priming with intranasal lactobacilli prevents Pseudomonas aeruginosa acute pneumonia in mice. BMC Microbiol. 2021, 21, 195. [Google Scholar] [CrossRef]
- Ku, S.; Park, M.S.; Ji, G.E.; You, H.J. Review on Bifidobacterium bifidum BGN4: Functionality and Nutraceutical Applications as a Probiotic Microorganism. Int. J. Mol. Sci. 2016, 17, 1544. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, J.W.; Kang, S.-G.; Oh, S.; Griffiths, M.W. Bifidobacterium spp. influences the production of autoinducer-2 and biofilm formation by Escherichia coli O157:H7. Anaerobe 2012, 18, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Valdez, R.M.A.; Ximenez-Fyvie, L.A.; Caiaffa, K.S.; dos Santos, V.R.; Cervantes, R.M.G.; Almaguer-Flores, A.; Duque, C. Antagonist effect of probiotic bifidobacteria on biofilms of pathogens associated with periodontal disease. Microb. Pathog. 2020, 150, 104657. [Google Scholar] [CrossRef]
- Collado, M.C.; Jalonen, L.; Meriluoto, J.; Salminen, S. Protection mechanism of probiotic combination against human pathogens: In vitro adhesion to human intestinal mucus. Asia Pac. J. Clin. Nutr. 2006, 15, 570–575. [Google Scholar]
- Miyazaki, Y.; Yokota, H.; Takahashi, H.; Fukuda, M.; Kawakami, H.; Kamiya, S.; Hanawa, T. Effect of probiotic bacterial strains of Lactobacillus, Bifidobacterium, and Enterococcus on enteroaggregative Escherichia coli. J. Infect. Chemother. 2010, 16, 10–18. [Google Scholar] [CrossRef]
- Whiteley, M.; Diggle, S.P.; Greenberg, E.P. Progress in and promise of bacterial quorum sensing research. Nature 2017, 551, 313–320. [Google Scholar] [CrossRef]
- Nealson, K.H.; Platt, T.; Hastings, J.W. Cellular Control of the Synthesis and Activity of the Bacterial Luminescent System. J. Bacteriol. 1970, 104, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Fuqua, W.C.; Winans, S.C.; Greenberg, E.P. Quorum sensing in bacteria: The LuxR-LuxI family of cell density-responsive transcriptional regulators. J Bacteriol 1994, 176, 269–275. [Google Scholar] [CrossRef]
- Waters, C.M.; Bassler, B.L. QUORUM SENSING: Cell-to-Cell Communication in Bacteria. Annu. Rev. Cell Dev. Biol. 2005, 21, 319–346. [Google Scholar] [CrossRef]
- Slater, H.; Crow, M.; Everson, L.; Salmond, G.P.C. Phosphate availability regulates biosynthesis of two antibiotics, prodigiosin and carbapenem, in Serratia via both quorum-sensing-dependent and -independent pathways. Mol. Microbiol. 2008, 47, 303–320. [Google Scholar] [CrossRef]
- Vadakkan, K.; Alam Choudhury, A.; Gunasekaran, R.; Hemapriya, J.; Vijayanand, S. Quorum sensing intervened bacterial signaling: Pursuit of its cognizance and repression. J. Genet. Eng. Biotechnol. 2018, 16, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Rieu, A.; Weidmann, S.; Garmyn, D.; Piveteau, P.; Guzzo, J. agr System of Listeria monocytogenes EGD-e: Role in Adherence and Differential Expression Pattern. Appl. Environ. Microbiol. 2007, 73, 6125–6133. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, S.T.; Bassler, B.L. Bacterial Quorum Sensing: Its Role in Virulence and Possibilities for Its Control. Cold Spring Harb. Perspect. Med. 2012, 2, a012427. [Google Scholar] [CrossRef] [PubMed]
- Ali, L.; Goraya, M.U.; Arafat, Y.; Ajmal, M.; Chen, J.-L.; Yu, D. Molecular Mechanism of Quorum-Sensing in Enterococcus faecalis: Its Role in Virulence and Therapeutic Approaches. Int. J. Mol. Sci. 2017, 18, 960. [Google Scholar] [CrossRef]
- Sturme, M.H.; Kleerebezem, M.; Nakayama, J.; Akkermans, A.D.; Vaughan, E.E.; Vos, W.M. Cell to cell communication by autoinducing peptides in gram-positive bacteria. Antonie Van Leeuwenhoek 2002, 81, 233–243. [Google Scholar] [CrossRef]
- Zhang, B.; Ku, X.; Zhang, X.; Zhang, Y.; Chen, G.; Chen, F.; Zeng, W.; Li, J.; Zhu, L.; He, Q. The AI-2/luxS Quorum Sensing System Affects the Growth Characteristics, Biofilm Formation, and Virulence of Haemophilus parasuis. Front. Cell. Infect. Microbiol. 2019, 9, 62. [Google Scholar] [CrossRef]
- Ma, Y.; Hao, L.; Ke, H.; Liang, Z.; Ma, J.; Liu, Z.; Li, Y. LuxS /AI-2 in Streptococcus agalactiae reveals a key role in acid tolerance and virulence. Res. Vet. Sci. 2017, 115, 501–507. [Google Scholar] [CrossRef]
- Guo, M.; Gamby, S.; Zheng, Y.; Sintim, H.O. Small Molecule Inhibitors of AI-2 Signaling in Bacteria: State-of-the-Art and Future Perspectives for Anti-Quorum Sensing Agents. Int. J. Mol. Sci. 2013, 14, 17694–17728. [Google Scholar] [CrossRef]
- Torres-Cerna, C.E.; Morales, J.A.; Hernandez-Vargas, E.A. Modeling Quorum Sensing Dynamics and Interference on Escherichia coli. Front. Microbiol. 2019, 10, 1835. [Google Scholar] [CrossRef] [PubMed]
- Van Houdt, R.; Michiels, C. Role of bacterial cell surface structures in Escherichia coli biofilm formation. Res. Microbiol. 2005, 156, 626–633. [Google Scholar] [CrossRef]
- Martínez, O.F.; Rigueiras, P.O.; Pires, D.S.; Porto, W.F.; Silva, O.N.; De La Fuente-Nunez, C.; Franco, O.L. Interference With Quorum-Sensing Signal Biosynthesis as a Promising Therapeutic Strategy Against Multidrug-Resistant Pathogens. Front. Cell. Infect. Microbiol. 2019, 8, 444. [Google Scholar] [CrossRef] [PubMed]
- Munir, S.; Shah, A.A.; Shahid, M.; Manzoor, I.; Aslam, B.; Rasool, M.H.; Saeed, M.; Ayaz, S.; Khurshid, M. Quorum Sensing Interfering Strategies and Their Implications in the Management of Biofilm-Associated Bacterial Infections. Braz. Arch. Biol. Technol. 2020, 63. [Google Scholar] [CrossRef]
- Fischer, T.L.; White, R.J.; Mares, K.F.; Molnau, D.E.; Donato, J.J. ucFabV Requires Functional Reductase Activity to Confer Reduced Triclosan Susceptibility in Escherichia coli. J. Mol. Microbiol. Biotechnol. 2015, 25, 394–402. [Google Scholar] [CrossRef]
- Chang, Y.; Wang, P.-C.; Ma, H.-M.; Chen, S.-Y.; Fu, Y.-H.; Liu, Y.-Y.; Wang, X.; Yu, G.-C.; Huang, T.; Hibbs, D.E.; et al. Design, synthesis and evaluation of halogenated furanone derivatives as quorum sensing inhibitors in Pseudomonas aeruginosa. Eur. J. Pharm. Sci. 2019, 140, 105058. [Google Scholar] [CrossRef] [PubMed]
- Kusada, H.; Tamaki, H.; Kamagata, Y.; Hanada, S.; Kimura, N. A Novel Quorum-Quenching N -Acylhomoserine Lactone Acylase from Acidovorax sp. Strain MR-S7 Mediates Antibiotic Resistance. Appl. Environ. Microbiol. 2017, 83. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; He, X.; Brancaccio, V.F.; Yuan, J.; Riedel, C.U. Bifidobacteria Exhibit LuxS-Dependent Autoinducer 2 Activity and Biofilm Formation. PLoS ONE 2014, 9, e88260. [Google Scholar] [CrossRef]
- Song, J.; Qin, Q.; Li, T.; Ren, F.; Zhang, H.; Xie, Y.; Jin, J. Impact of carbohydrates on autoinducer-2 secretion of Bifidobacterium longum subsp. longum BBMN68. Lett. Appl. Microbiol. 2018, 66, 340–346. [Google Scholar] [CrossRef]
- Asahara, T.; Shimizu, K.; Nomoto, K.; Hamabata, T.; Ozawa, A.; Takeda, Y. Probiotic Bifidobacteria Protect Mice from Lethal Infection with Shiga Toxin-Producing Escherichia coli O157:H7. Infect. Immun. 2004, 72, 2240–2247. [Google Scholar] [CrossRef]
- Li, J.; Yang, X.; Shi, G.; Chang, J.; Liu, Z.; Zeng, M. Cooperation of lactic acid bacteria regulated by the AI-2/LuxS system involve in the biopreservation of refrigerated shrimp. Food Res. Int. 2018, 120, 679–687. [Google Scholar] [CrossRef]
- Onbas, T.; Osmanagaoglu, O.; Kiran, F. Potential Properties of Lactobacillus plantarum F-10 as a Bio-control Strategy for Wound Infections. Probiotics Antimicrob. Proteins 2018, 11, 1110–1123. [Google Scholar] [CrossRef]
- Valdéz, J.C.; Peral, M.C.; Rachid, M.; Santana, M.; Perdigón, G. Interference of Lactobacillus plantarum with Pseudomonas aeruginosa in vitro and in infected burns: The potential use of probiotics in wound treatment. Clin. Microbiol. Infect. 2005, 11, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Hossain, I.; Kim, K.; Mizan, F.R.; Toushik, S.H.; Ashrafudoulla, M.; Roy, P.K.; Nahar, S.; Jahid, I.K.; Choi, C.; Park, S.H.; et al. Comprehensive molecular, probiotic, and quorum-sensing characterization of anti-listerial lactic acid bacteria, and application as bioprotective in a food (milk) model. J. Dairy Sci. 2021, 104, 6516–6534. [Google Scholar] [CrossRef] [PubMed]
- Invernici, M.M.; Salvador, S.L.; Silva, P.H.F.; Soares, M.S.M.; Casarin, R.; Palioto, D.B.; Souza, S.L.S.; Taba, M.; Novas, A.B., Jr.; Furlaneto, F.A.C.; et al. Effects of Bifidobacterium probiotic on the treatment of chronic periodontitis: A randomized clinical trial. J. Clin. Periodontol. 2018, 45, 1198–1210. [Google Scholar] [CrossRef]
- Isolation and Characterisation of Probiotics for Antagonising the Cariogenic Bacterium Streptococcus mutans and Preventing Biofilm Formation. Preprints 2016, 16, 445–455. [CrossRef]
- Rossoni, R.D.; Velloso, M.D.S.; de Barros, P.P.; de Alvarenga, J.A.; dos Santos, J.D.; Prado, A.C.C.D.S.; Ribeiro, F.D.C.; Anbinder, A.L.; Junqueira, J.C. Inhibitory effect of probiotic Lactobacillus supernatants from the oral cavity on Streptococcus mutans biofilms. Microb. Pathog. 2018, 123, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-C.; Lin, C.-T.; Wu, C.-Y.; Peng, W.-S.; Lee, M.-J.; Tsai, Y.-C. Inhibitory effect ofLactobacillus salivariusonStreptococcus mutansbiofilm formation. Mol. Oral Microbiol. 2014, 30, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Krzyściak, W.; Kościelniak, D.; Papież, M.; Vyhouskaya, P.; Zagórska-Świeży, K.; Kołodziej, I.; Bystrowska, B.; Jurczak, A. Effect of a Lactobacillus Salivarius Probiotic on a Double-Species Streptococcus Mutans and Candida Albicans Caries Biofilm. Nutrients 2017, 9, 1242. [Google Scholar] [CrossRef] [PubMed]
- Rossoni, R.D.; de Barros, P.P.; De Alvarenga, J.A.; Ribeiro, F.; Velloso, M.D.S.; Fuchs, B.B.; Mylonakis, E.; Jorge, A.O.C.; Junqueira, J. Antifungal activity of clinical Lactobacillus strains against Candida albicans biofilms: Identification of potential probiotic candidates to prevent oral candidiasis. Biofouling 2018, 34, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Chew, S.Y.; Cheah, Y.K.; Seow, H.F.; Sandai, D.; Than, L.T.L. In vitro modulation of probiotic bacteria on the biofilm of Candida glabrata. Anaerobe 2015, 34, 132–138. [Google Scholar] [CrossRef]
- Lee, S.-H.; Kim, Y.-J. A comparative study of the effect of probiotics on cariogenic biofilm model for preventing dental caries. Arch. Microbiol. 2014, 196, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Chen, X.; Tu, Y.; Wang, S.; Chen, H. Effect of Probiotic Lactobacilli on the Growth of Streptococcus Mutans and Multispecies Biofilms Isolated from Children with Active Caries. Med. Sci. Monit. 2017, 23, 4175–4181. [Google Scholar] [CrossRef]
- Jeong, D.; Kim, D.-H.; Song, K.-Y.; Seo, K.-H. Antimicrobial and anti-biofilm activities of Lactobacillus kefiranofaciens DD2 against oral pathogens. J. Oral Microbiol. 2018, 10, 1472985. [Google Scholar] [CrossRef]
- James, K.M.; Macdonald, K.W.; Chanyi, R.M.; Cadieux, P.A.; Burton, J. Inhibition of Candida albicans biofilm formation and modulation of gene expression by probiotic cells and supernatant. J. Med. Microbiol. 2016, 65, 328–336. [Google Scholar] [CrossRef]
- Tan, Y.; Leonhard, M.; Moser, D.; Ma, S.; Schneider-Stickler, B. Inhibitory effect of probiotic lactobacilli supernatants on single and mixed non- albicans Candida species biofilm. Arch. Oral Biol. 2018, 85, 40–45. [Google Scholar] [CrossRef]
- Merghni, A.; Dallel, I.; Noumi, E.; Kadmi, Y.; Hentati, H.; Tobji, S.; Ben Amor, A.; Mastouri, M. Antioxidant and antiproliferative potential of biosurfactants isolated from Lactobacillus casei and their anti-biofilm effect in oral Staphylococcus aureus strains. Microb. Pathog. 2017, 104, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Sarikhani, M.; Kermanshahi, R.K.; Ghadam, P.; Gharavi, S. The role of probiotic Lactobacillus acidophilus ATCC 4356 bacteriocin on effect of HBsu on planktonic cells and biofilm formation of Bacillus subtilis. Int. J. Biol. Macromol. 2018, 115, 762–766. [Google Scholar] [CrossRef] [PubMed]
- Mahdhi, A.; Leban, N.; Chakroun, I.; Bayar, S.; Mahdouani, K.; Majdoub, H.; Kouidhi, B. Use of extracellular polysaccharides, secreted by Lactobacillus plantarum and Bacillus spp., as reducing indole production agents to control biofilm formation and efflux pumps inhibitor in Escherichia coli. Microb. Pathog. 2018, 125, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Harjai, K.; Shukla, G. Effect of bacteriocin and exopolysaccharides isolated from probiotic on P. aeruginosa PAO1 biofilm. Folia Microbiol. 2017, 63, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Soltani, S.; Hammami, R.; Cotter, P.D.; Rebuffat, S.; Ben Said, L.; Gaudreau, H.; Bédard, F.; Biron, E.; Drider, D.; Fliss, I. Bacteriocins as a new generation of antimicrobials: Toxicity aspects and regulations. FEMS Microbiol. Rev. 2021, 45, fuaa039. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS); Younes, M.; Aggett, P.; Aguilar, F.; Crebelli, R.; Dusemund, B.; Filipič, M.; Frutos, M.J.; Galtier, P.; Gundert-Remy, U.; et al. Safety of nisin (E 234) as a food additive in the light of new toxicological data and the proposed extension of use. EFSA J. 2017, 15, e05063. [Google Scholar] [CrossRef] [PubMed]
- Hagiwara, A.; Imai, N.; Nakashima, H.; Toda, Y.; Kawabe, M.; Furukawa, F.; Delves-Broughton, J.; Yasuhara, K.; Hayashi, S.-M. A 90-day oral toxicity study of nisin A, an anti-microbial peptide derived from Lactococcus lactis subsp. lactis, in F344 rats. Food Chem. Toxicol. 2010, 48, 2421–2428. [Google Scholar] [CrossRef] [PubMed]
- Zupančič, J.; Raghupathi, P.K.; Houf, K.; Burmølle, M.; Sørensen, S.; Gunde-Cimerman, N. Synergistic Interactions in Microbial Biofilms Facilitate the Establishment of Opportunistic Pathogenic Fungi in Household Dishwashers. Front. Microbiol. 2018, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Skariyachan, S.; Sridhar, V.S.; Packirisamy, S.; Kumargowda, S.T.; Challapilli, S.B. Recent perspectives on the molecular basis of biofilm formation by Pseudomonas aeruginosa and approaches for treatment and biofilm dispersal. Folia Microbiol. 2018, 63, 413–432. [Google Scholar] [CrossRef]
- Yadav, P.; Verma, S.; Bauer, R.; Kumari, M.; Dua, M.; Johri, A.K.; Yadav, V.; Spellerberg, B. Deciphering Streptococcal Biofilms. Microorganisms 2020, 8, 1835. [Google Scholar] [CrossRef]
- Sadykov, M.R.; Hartmann, T.; Mattes, T.; Hiatt, M.; Jann, N.J.; Zhu, Y.; Ledala, N.; Landmann, R.; Herrmann, M.; Rohde, H.; et al. CcpA coordinates central metabolism and biofilm formation in Staphylococcus epidermidis. Microbiology 2011, 157, 3458–3468. [Google Scholar] [CrossRef]
- Seidl, K.; Goerke, C.; Wolz, C.; Mack, D.; Berger-Bächi, B.; Bischoff, M. Staphylococcus aureus CcpA Affects Biofilm Formation. Infect. Immun. 2008, 76, 2044–2050. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Kim, H.; Desai, S.; Deep, K.; Rice, K.C. Regulation ofcidandlrgexpression by CodY inStreptococcus mutans. MicrobiologyOpen 2020, 9, e1040. [Google Scholar] [CrossRef] [PubMed]
- Muscariello, L.; Marino, C.; Capri, U.; Vastano, V.; Marasco, R.; Sacco, M. CcpA and three newly identified proteins are involved in biofilm development inLactobacillus plantarum. J. Basic Microbiol. 2012, 53, 62–71. [Google Scholar] [CrossRef]
- Goswami, M.; Espinasse, A.; Carlson, E.E. Disarming the virulence arsenal of Pseudomonas aeruginosa by blocking two-component system signaling. Chem. Sci. 2018, 9, 7332–7337. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Sun, D.; Zhu, J.; Liu, J.; Liu, W. The Regulation of Bacterial Biofilm Formation by cAMP-CRP: A Mini-Review. Front. Microbiol. 2020, 11, 802. [Google Scholar] [CrossRef] [PubMed]
- Valentini, M.; Filloux, A. Biofilms and Cyclic di-GMP (c-di-GMP) Signaling: Lessons from Pseudomonas aeruginosa and Other Bacteria. J. Biol. Chem. 2016, 291, 12547–12555. [Google Scholar] [CrossRef]
- Hall-Stoodley, L.; Costerton, J.W.; Stoodley, P. Bacterial biofilms: From the Natural environment to infectious diseases. Nat. Rev. Genet. 2004, 2, 95–108. [Google Scholar] [CrossRef]
- Verderosa, A.D.; Totsika, M.; Fairfull-Smith, K.E. Bacterial Biofilm Eradication Agents: A Current Review. Front. Chem. 2019, 7, 824. [Google Scholar] [CrossRef]
- Redman, W.K.; Welch, G.S.; Rumbaugh, K.P. Differential Efficacy of Glycoside Hydrolases to Disperse Biofilms. Front. Cell. Infect. Microbiol. 2020, 10, 379. [Google Scholar] [CrossRef] [PubMed]
- Nijland, R.; Hall, M.; Burgess, J.G. Dispersal of Biofilms by Secreted, Matrix Degrading, Bacterial DNase. PLoS ONE 2010, 5, e15668. [Google Scholar] [CrossRef]
- Sugimoto, S.; Sato, F.; Miyakawa, R.; Chiba, A.; Onodera, S.; Hori, S.; Mizunoe, Y. Broad impact of extracellular DNA on biofilm formation by clinically isolated Methicillin-resistant and -sensitive strains of Staphylococcus aureus. Sci. Rep. 2018, 8, 2254. [Google Scholar] [CrossRef]
- Kaplan, J.B.; Mlynek, K.D.; Hettiarachchi, H.; Alamneh, Y.A.; Biggemann, L.; Zurawski, D.V.; Black, C.C.; Bane, C.E.; Kim, R.K.; Granick, M.S. Extracellular polymeric substance (EPS)-degrading enzymes reduce staphylococcal surface attachment and biocide resistance on pig skin in vivo. PLoS ONE 2018, 13, e0205526. [Google Scholar] [CrossRef]
- Pinto, R.M.; Soares, F.A.; Reis, S.; Nunes, C.; Van Dijck, P. Innovative Strategies Toward the Disassembly of the EPS Matrix in Bacterial Biofilms. Front. Microbiol. 2020, 11, 952. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.M.; Koskella, B.; Lin, H.C. Phage therapy: An alternative to antibiotics in the age of multi-drug resistance. World J. Gastrointest. Pharmacol. Ther. 2017, 8, 162–173. [Google Scholar] [CrossRef]
- Tian, F.; Li, J.; Nazir, A.; Tong, Y. Bacteriophage—A Promising Alternative Measure for Bacterial Biofilm Control. Infect. Drug Resist. 2021, 14, 205–217. [Google Scholar] [CrossRef]
- Han, C.; Song, J.; Hu, J.; Fu, H.; Feng, Y.; Mu, R.; Xing, Z.; Wang, Z.; Wang, L.; Zhang, J.; et al. Smectite promotes probiotic biofilm formation in the gut for cancer immunotherapy. Cell Rep. 2021, 34, 108706. [Google Scholar] [CrossRef] [PubMed]
- Mitra, A.; Mukhopadhyay, S. Biofilm mediated decontamination of pollutants from the environment. AIMS Environ. Sci. 2016, 3, 44–59. [Google Scholar] [CrossRef]
- Singh, R.; Paul, D.; Jain, R.K. Biofilms: Implications in bioremediation. Trends Microbiol. 2006, 14, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Canon, F.; Nidelet, T.; Guédon, E.; Thierry, A.; Gagnaire, V. Understanding the Mechanisms of Positive Microbial Interactions That Benefit Lactic Acid Bacteria Co-cultures. Front. Microbiol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Canon, F.; Maillard, M.-B.; Henry, G.; Thierry, A.; Gagnaire, V. Positive Interactions between Lactic Acid Bacteria Promoted by Nitrogen-Based Nutritional Dependencies. Appl. Environ. Microbiol. 2021, 87. [Google Scholar] [CrossRef]
| Models | Properties | Uses | Advantages | References |
|---|---|---|---|---|
| Static systems | ||||
| Colony biofilm | Colonies grow over agar, maintenance of basic biofilm characteristics (e.g., chemical gradient) | Antibiotic susceptibility assay | Simple and reproducible, high throughput | [59,60] |
| Microtiter plate | Most widely used, bacterial adhere to well surfaces | Semiquantitative evaluation of biofilm formation of strains, biofilm antibiotic tolerance test, study of antibiofilm efficiency | Simple to perform, molecular genetic tests are allowed, high throughput | [61,62] |
| Biofilm ring test | Use of magnetic beads to immobilize bacteria | Quantitative evaluation of biofilm formation of strains | Rapid monitoring of biofilm formation, investigation of early adhesion | [63] |
| Calgary biofilm device | Use of a lid with 96 pegs on which biofilms develop | Biofilm antibacterial tolerance and resistance, efficiency of antibiofilm/antibiotic products | Pegs are individually removable, avoiding cross contamination | [64] |
| Open systems | ||||
| Flow cell | Flat walled transparent chambers continuously sprinkled with medium, automatic system | Evaluation of biofilm formation in real-time (chamber is under microscope), efficiency of antibiofilm/antibiotic products | Continuous image record, single cell observation | [65] |
| Microfermentors | Chemostat-based, biofilms are formed over a removable spatula (mode of different materials) | Evaluation of biofilm formation of strains, efficiency of antibiotic products | Lare scale biofilm biomass production; genetic, biochemical, and microscopic analyses are allowed; easy conversion into microcosms | [66] |
| Modified Robbins device | Linear rectangular array of ports in which plugs are inserted | Artificial throat used to evaluate the efficiency of product in rubber trachea-oesophageal prostheses | Each plug can be removed individually and aseptically | [67] |
| CDC biofilm reactors | Consists of eight polypropylene coupon holder rods suspended from a polyethylene ported lid | Evaluation of biofilm formation, antibiotic resistance and tolerance; study of biofilm over time | Easy sampling event at different time | [68] |
| Kadouri system | Based on microtiter plate assay with continuous medium replacement | Testing multiple nutritional condition and treatments | Formation of high amount of mature biofilm in wells | [69] |
| Rotating disc reactor | Rotor embedded with a magnetic stir holding 6 to 24 coupons over which biofilms will form | Used to study multispecies biofilm; evaluation of antibacterial molecules | Modification of liquid shear forces over the coupons | [70] |
| Microfluidic biochips | Chip located in aluminium support in which dielectric sensors control temperature | Quantitative cell and population analyses | Measurement of biofilm growth and maturation with high sensitivity | [71] |
| Drip flow reactors | Consists of four test channels, each holding one standard glass microscope slide sized coupon | Evaluation of antimicrobial and antibiofilm substances; study biofilm heterogeneity | Establishment of both solid-air and solid-liquid interfaces | [72] |
| Microcosms | ||||
| Reconstituted human epithelia (RHE) | Human keratinocytes (from buccal mucosa) serve as surface to growth biofilm | Oral biofilm formation | Possibility to study oral receptor specificity | [73] |
| Microfluidic co-culture model | HeLa cells covered with microfluidic channels over which biofilm forms | Mimic gastrointestinal environment | Real-time visualization of biofilm growth | [74] |
| Endothelial cells under flow model | Microvascular endothelial cells are attached on microscope slide allowing biofilm development | Monitoring of blood vessel microenvironment and biofilm formation dynamics | Biofilm formation stages and cell can be stained with fluorescent dyes and monitored | [75] |
| Airway epithelial cell model | Collagen coated membranes allow growth of airway epithelial cells for biofilm development | Oral biofilm formation (cystic fibrosis, chronic rhinosinusitis) | Investigation of air-liquid biofilm model | [76] |
| Pathway | QS Signal Molecules | Core Proteins | Main Bacterial Species | References |
|---|---|---|---|---|
| luxslR | N-acyl-homoserine lactones (AHL) | LuxI, LuxR | V. fischeri | [105] |
| SmaI/SmaR | PhoR, PhoB | Serratia sp. | [106] | |
| LasIR-RhlIR | Lasl, LasR, RhlI, RhlR | P. aeruginosa | [107] | |
| Agr | Autoinducing peptides (AIP) | AgrA, AgrB, AgrC | S. aureus, L. monocytogenes | [108,109] |
| Extracellular protease processed AIP | plcR, OPP | B. cereus | [109] | |
| Competitive quorum-sensing system | RapB,RapC, ComP, ComQ | B. subtilis | [107] | |
| Cytolysin quorum-sensing system | CylA, CylB, CylM | E. faecalis | [110] | |
| Fsr | FsrA,FsrB, FsrC | S. aureus, E. faecalis | [110,111] | |
| LuxS/AI-2 | autoinducer 2 (AI-2) | Pfs, LuxS | V. harveyi, Haemophilus parasuis, Streptococcus agalactiae | [112,113,114] |
| Lsr | LsrK, LsrR | E. coli | [115] |
| Probiotics | Pathogens | Mechanism of Action | Study | References |
|---|---|---|---|---|
| Bifidobacterium animalis subsp. lactis | Periodontitis | Decrease of pro-inflammatory cytokine levels, blocked the recolonization of periodontal pockets. | CT | [129] |
| L. crispatus BCRC 14618, L. pentosus | S. mutans, cariogenic bacteria | Biofilm formation associated with sucrose-dependent cell-cell adhesion and the gtfC level of enzyme in the biofilm were decreased. | In vitro | [130] |
| L. fermentum, L. paracasei, L. paracasei, and L. paracasei | S. mutans | Decreased S. mutans biofilms. | In vitro | [131] |
| L. salivarius strains | S. mutans | Reduced bacterial growth and expression levels of gtfB, gtfC, and gtfD gtfs as well as EPS production. | In vitro | [132] |
| L. salivarius | S. mutans with C. albicans | Secretory factors inhibited the formation of biofilm and fungal morphological transformation, with reduction of C. albicans pathogenicity. | In vitro | [133] |
| L. fermentum 20.4, L. paracasei 28.4, and L. rhamnosus 5.2 | C. albicans | Reduced expression levels of ALS3, HWP1, CPH1, and EFG1. | In vitro | [134] |
| L. rhamnosus GR-1 and L. reuteri RC-14 | C. glabrata | Reduced expression of biofilm-related genes (EPA6 and YAK1). | In vitro | [135] |
| B.bifidum, L. acidophilus, L. brevis, L. casei, and L. rhamnosus GG | S. mutans | Reduced expression of gtfs and glucan. | In vitro | [136] |
| L. casei Shirota, L. casei LC01, L. plantarum ST-III, and L. paracasei LPC37 | S. mutans strains, multispecies biofilms | Prevention of S. mutans and multispecies biofilms growth. | In vitro | [137] |
| L. kefiranofaciens, L. plantarum, L. rhamnosus, L. johnsonii | S. mutans, S. sobrinus | Shutdown of all biofilm-associated genes encoding carbohydrate metabolism, regulatory biofilm, and adhesion proteins. | Na | [138] |
| L. casei, L.reuteri, L. plantarum, L. salivarius | S. mutans | Decrease in expression of genes involved in acid tolerance, QS and EPS production. L. salivarius had peroxide-dependent antimicrobial and antibiofilm activities. | Na | [87] |
| Combinations of L. plantarum, L. helveticus, and S. salivarius | C. albicans | Reduced expression of EFG1, HWP1, ALS3, and SAP5. | Na | [139] |
| L. gasseri and L. rhamnosus supernatant | C. tropicalis, C. krusei and C. parapsilosis | Disruption of mature biofilm, inhibition of mixed biofilms, and cell damages on silicone surface. | In vitro | [140] |
| L. pentosus strain LAP1 | C. albicans, C. tropicalis, and C. krusei. | Antibiofilm property. | In vitro | [139] |
| L. casei LBl | S. aureus strains 9P and 29P | Biosurfactants dispersed the preformed biofilms. | In vitro | [141] |
| L. acidophilus ATCC 4356 | B. subtilis BM19 | Growth and biofilm formation inhibition. | Na | [142] |
| L. plantarum F-10 supernatant | P. aeruginosa PAO1, MRSA and hospital-derived strains | Downregulation of QS signals, oxidative stress in wound healing stages, inhibition of the virulence factors (motility, activity of protease and elastase, production of pyocyanin and rhamnolipid). | Na | [126] |
| EPS-Lp from L. plantarum and EPS-B from Bacillus spp. | E. coli ATCC 35218 | EPSs reduced cell surface hydrophobicity level, indole production, prevented biofilm formation, reduced efflux pumps devoted to bacterial adhesion and antimicrobial resistance. | Na | [143] |
| L. fermentum TCUESC01 and L. plantarum TCUESC02 | S. aureus | Biofilm formation inhibition by alteration of the ica operon (icaA and icaR). | Na | [83] |
| L. fermentum (KT998657) isolated from neonatal fecal samples | P. aeruginosa PAO1 | Reduced biofilm forming due to postbiotics (bacteriocin and EPS), bacteriocins creates pores in the cell membrane resulting in cell death. Alteration of matrix and cell assembly, cell-cell interaction and attachment to form biofilms. | Na | [144] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meroni, G.; Panelli, S.; Zuccotti, G.; Bandi, C.; Drago, L.; Pistone, D. Probiotics as Therapeutic Tools against Pathogenic Biofilms: Have We Found the Perfect Weapon? Microbiol. Res. 2021, 12, 916-937. https://doi.org/10.3390/microbiolres12040068
Meroni G, Panelli S, Zuccotti G, Bandi C, Drago L, Pistone D. Probiotics as Therapeutic Tools against Pathogenic Biofilms: Have We Found the Perfect Weapon? Microbiology Research. 2021; 12(4):916-937. https://doi.org/10.3390/microbiolres12040068
Chicago/Turabian StyleMeroni, Gabriele, Simona Panelli, Gianvincenzo Zuccotti, Claudio Bandi, Lorenzo Drago, and Dario Pistone. 2021. "Probiotics as Therapeutic Tools against Pathogenic Biofilms: Have We Found the Perfect Weapon?" Microbiology Research 12, no. 4: 916-937. https://doi.org/10.3390/microbiolres12040068
APA StyleMeroni, G., Panelli, S., Zuccotti, G., Bandi, C., Drago, L., & Pistone, D. (2021). Probiotics as Therapeutic Tools against Pathogenic Biofilms: Have We Found the Perfect Weapon? Microbiology Research, 12(4), 916-937. https://doi.org/10.3390/microbiolres12040068








