Health Disparities in Central Line-Associated Bloodstream Infections: Analysis of the U.S. National Inpatient Sample Database (2016–2022)
Abstract
1. Introduction
2. Methods
2.1. Ethics Statement
2.2. Data Source
2.3. Study Cohort
2.4. Outcomes
2.5. Health Disparities and Leading Health Indicators
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Baseline Demographic and Clinical Characteristics
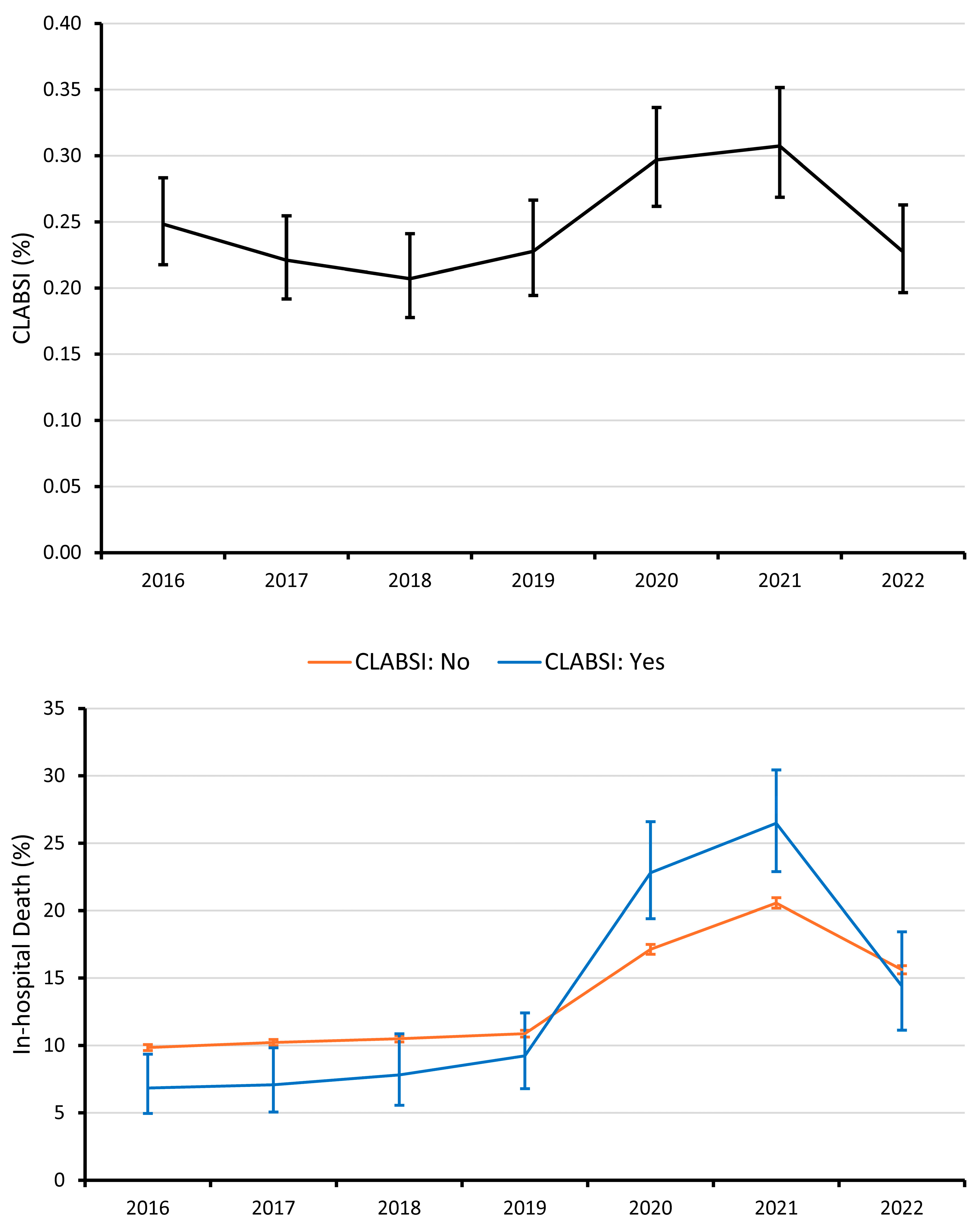
3.2. CLABSI Rate
3.3. In-Hospital Mortality Rate
3.4. Length of Stay
3.5. Inflation-Adjusted Hospital Cost
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Teja, B.; Bosch, N.A.; Diep, C.; Pereira, T.V.; Mauricio, P.; Sklar, M.C.; Sankar, A.; Wijeysundera, H.C.; Saskin, R.; Walkey, A. Complication Rates of Central Venous Catheters: A Systematic Review and Meta-Analysis. JAMA Intern. Med. 2024, 184, 474–482. [Google Scholar] [CrossRef]
- Kornbau, C.; Lee, K.C.; Hughes, G.D.; Firstenberg, M.S. Central line complications. Int. J. Crit. Illn. Inj. Sci. 2015, 5, 170–178. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC4613416/ (accessed on 14 May 2023). [CrossRef] [PubMed]
- National Healthcare Safety Network. Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-central Line Associated Bloodstream Infection). 2025. Available online: https://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf (accessed on 4 August 2025).
- Centers for Disease Control and Prevention. 2022 National and State Healthcare-Associated Infections Progress Report; CDC: Atlanta, GA, USA, 2014. [Google Scholar]
- Alwazzeh, M.J.; Alnimr, A.; Al Nassri, S.A.; Alwarthan, S.M.; Alhajri, M.; AlShehail, B.M.; Almubarak, M.; Alghamdi, N.S.; Wali, H.A. Microbiological trends and mortality risk factors of central line-associated bloodstream infections in an academic medical center 2015–2020. Antimicrob. Resist. Infect. Control 2023, 12, 128. [Google Scholar] [CrossRef]
- Buetti, N.; Marschall, J.; Drees, M.; Fakih, M.G.; Hadaway, L.; Maragakis, L.L.; Monsees, E.; Novosad, S.; O’Grady, N.P.; Rupp, M.E.; et al. Strategies to prevent central line-associated bloodstream infections in acute-care hospitals: 2022 Update. Infect. Control Hosp. Epidemiol. 2022, 43, 553–569. [Google Scholar] [CrossRef]
- Joint Commission International. Joint Commission Resources. 2021. International Patient Safety Goals. Available online: https://www.jointcommission.org/en/standards/international-patient-safety-goals (accessed on 4 August 2025).
- Quality and Disparities in Quality of Healthcare. In 2017 National Healthcare Quality and Disparities Report. Rockville: Agency for Healthcare Research and Quality (US); National Center for Biotechnology Information: Bethesda, MD, USA, 2018. Available online: https://www.ncbi.nlm.nih.gov/books/NBK579748/ (accessed on 4 August 2025).
- The Joint Commission. Preventing Central Line–Associated Bloodstream Infections: Useful Tools, an International Perspective; National Center for Biotechnology Information: Bethesda, MD, USA, 2013. [Google Scholar]
- Zingg, W.; Imhof, A.; Maggiorini, M.; Stocker, R.; Keller, E.; Ruef, C. Impact of a prevention strategy targeting hand hygiene and catheter care on the incidence of catheter-related bloodstream infections. Crit. Care Med. 2009, 37, 2167–2173. [Google Scholar] [CrossRef] [PubMed]
- Advani, S.; Reich, N.G.; Sengupta, A.; Gosey, L.; Milstone, A.M. Central line-associated bloodstream infection in hospitalized children with peripherally inserted central venous catheters: Extending risk analyses outside the intensive care unit. Clin. Infect. Dis. 2011, 52, 1108–1115. [Google Scholar] [CrossRef]
- Lafuente Cabrero, E.; Terradas Robledo, R.; Civit Cuñado, A.; García Sardelli, D.; Hidalgo López, C.; Giro Formatger, D.; Perez, L.L.; López, C.E.; Moreno, A.T.; Murt, A. Risk factors of catheter- associated bloodstream infection: Systematic review and meta-analysis. PLoS ONE 2023, 18, e0282290. [Google Scholar] [CrossRef]
- Moriyama, K.; Ando, T.; Kotani, M.; Tokumine, J.; Nakazawa, H.; Motoyasu, A.; Yorozu, T. Risk factors associated with increased incidences of catheter-related bloodstream infection. Medicine 2022, 101, e31160. [Google Scholar] [CrossRef]
- McGrath, C.L.; Bettinger, B.; Stimpson, M.; Bell, S.L.; Coker, T.R.; Kronman, M.P.; Zerr, D.M. Identifying and Mitigating Disparities in Central Line-Associated Bloodstream Infections in Minoritized Racial, Ethnic, and Language Groups. JAMA Pediatr. 2023, 177, 700–709. Available online: https://pubmed.ncbi.nlm.nih.gov/37252746/ (accessed on 4 August 2025). [CrossRef]
- Willer, B.L.; Tobias, J.D.; Suttle, M.L.; Nafiu, O.O.; Mpody, C. Trends of Racial/Ethnic Disparities in Pediatric Central Line-Associated Bloodstream Infections. Pediatrics 2022, 1, 150. Available online: https://pubmed.ncbi.nlm.nih.gov/35979730/ (accessed on 4 August 2025). [CrossRef]
- Lyren, A.; Haines, E.; Fanta, M.; Gutzeit, M.; Staubach, K.; Chundi, P.; Srinivasan, L.; Mackey, M.; Vonderhaar, M.; Sisson, P.; et al. Racial and ethnic disparities in common inpatient safety outcomes in a children’s hospital cohort. BMJ Qual. Saf. 2023, 33, 86–97. Available online: https://pubmed.ncbi.nlm.nih.gov/37460119/ (accessed on 4 August 2025). [CrossRef]
- Healthcare Cost and Utilization Project. Overview of the National (Nationwide) Inpatient Sample (NIS). Available online: https://hcup-us.ahrq.gov/nisoverview.jsp (accessed on 20 January 2025).
- Agency for Healthcare Research and Quality. Patient Safety Indicator 07 (PSI 07) Central Venous Catheter-Related Bloodstream Infection Rate; Healthcare Research and Quality: Rockville, MD, USA, 2024. [Google Scholar]
- Quan, H.; Eastwood, C.; Cunningham, C.T.; Liu, M.; Flemons, W.; De Coster, C.; A Ghali, W. Validity of AHRQ patient safety indicators derived online ICD-10 hospital discharge abstract data (chart review study). BMJ Open 2013, 3, e003716. Available online: https://pubmed.ncbi.nlm.nih.gov/24114372/ (accessed on 19 April 2025). [CrossRef]
- United States Bureau of Labor Statistics. CPI Inflation Calculator. Available online: https://www.bls.gov/data/inflation_calculator.htm (accessed on 20 January 2025).
- Alvidrez, J.; Castille, D.; Laude-Sharp, M.; Rosario, A.; Tabor, D. The National Institute on Minority Health and Health Disparities Research Framework. Am. J. Public Health 2019, 109, S16–S20. Available online: https://ajph.aphapublications.org/doi/10.2105/AJPH.2018.304883 (accessed on 2 July 2023). [CrossRef]
- Ochiai, E.; Kigenyi, T.; Sondik, E.; Pronk, N.; Kleinman, D.V.; Blakey, C.; Fromknecht, C.Q.B.; Heffernan, M.; Brewer, K.H. Healthy People 2030 Leading Health Indicators and Overall Health and Well-being Measures: Opportunities to Assess and Improve the Health and Well-being of the Nation. J. Public Health Manag. Pract. 2021, 27, S235–S241. Available online: https://pubmed.ncbi.nlm.nih.gov/34559740/ (accessed on 15 May 2024). [CrossRef]
- Glasheen, W.P.; Cordier, T.; Gumpina, R.; Haugh, G.; Davis, J.; Renda, A. Charlson Comorbidity Index: ICD-9 Update and ICD-10 Translation. Am. Health Drug Benefits 2019, 12, 188. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC6684052/ (accessed on 20 January 2025).
- Harrell, F. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis; Springer Nature: New York, NY, USA, 2015. [Google Scholar]
- Nationwide Data Use Agreement. Available online: https://hcup-us.ahrq.gov/team/NationwideDUA.jsp (accessed on 20 January 2025).
- Bakullari, A.; Metersky, M.L.; Wang, Y.; Eldridge, N.; Eckenrode, S.; Pandolfi, M.M.; Jaser, L.; Galusha, D.; Moy, E. Racial and ethnic disparities in healthcare-associated infections in the United States, 2009–2011. Infect Control Hosp. Epidemiol. 2014, 35 (Suppl. 3), S10–S16. Available online: https://pubmed.ncbi.nlm.nih.gov/25222888/ (accessed on 22 January 2025). [CrossRef]
- Gualandi, N.; Mu, Y.; Bamberg, W.M.; Dumyati, G.; Harrison, L.H.; Lesher, L.; Nadle, J.; Petit, S.; Ray, S.M.; Schaffner, W. Racial Disparities in Invasive Methicillin-resistant Staphylococcus aureus Infections, 2005–2014. Clin. Infect. Dis. 2018, 67, 1175–1181. Available online: https://pubmed.ncbi.nlm.nih.gov/29659728/ (accessed on 22 January 2025). [CrossRef]
- Argamany, J.R.; Delgado, A.; Reveles, K.R. Clostridium difficile infection health disparities by race among hospitalized adults in the United States, 2001 to 2010. BMC Infect. Dis. 2016, 16, 1175–1181. Available online: https://pubmed.ncbi.nlm.nih.gov/27568176/ (accessed on 22 January 2025). [CrossRef]
- Tripathi, S.; Walter, T.; McGarvey, J. Racial and ethnic disparities in central line-associated bloodstream infections (CLABSI) in hospitalized patients: A risk-adjusted analysis. Infect. Control Hosp. Epidemiol. 2025, 46, 356–362. Available online: https://pubmed.ncbi.nlm.nih.gov/39963838/ (accessed on 19 April 2025). [CrossRef]
- Purnell, T.S.; Calhoun, E.A.; Golden, S.H.; Halladay, J.R.; Krok-Schoen, J.L.; Appelhans, B.M.; Cooper, L.A. Achieving health equity: Closing the gaps in health care disparities, interventions, and research. Health Aff. 2016, 35, 1410–1415. [Google Scholar] [CrossRef]
- Arpey, N.C.; Gaglioti, A.H.; Rosenbaum, M.E. How Socioeconomic Status Affects Patient Perceptions of Health Care: A Qualitative Study. J. Prim. Care Community Health 2017, 8, 169–175. Available online: https://pubmed.ncbi.nlm.nih.gov/28606031/ (accessed on 22 January 2025). [CrossRef]
- Wong, S.W.; Gantner, D.; McGloughlin, S.; Leong, T.; Worth, L.J.; Klintworth, G.; Scheinkestel, C.; Pilcher, D.; Cheng, A.; Udy, A. The influence of intensive care unit-acquired central line-associated bloodstream infection on in-hospital mortality: A single-center risk-adjusted analysis. Am. J. Infect. Control 2016, 44, 587–592. Available online: https://pubmed.ncbi.nlm.nih.gov/26874406/ (accessed on 6 February 2025). [CrossRef]
- Alshahrani, K.M.; Alhuwaishel, A.Z.; Alangari, N.M.; Asiri, M.A.; Al-Shahrani, N.A.; Alasmari, A.A.; Alzahrani, O.J.; Ayedh, A.Y.; Qitmah, M.M. Clinical Impacts and Risk Factors for Central Line-Associated Bloodstream Infection: A Systematic Review. Cureus 2023, 15, e40954. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC10368959/ (accessed on 6 February 2025). [CrossRef]
- Weiner-Lastinger, L.M.; Pattabiraman, V.; Konnor, R.Y.; Patel, P.R.; Wong, E.; Xu, S.Y.; Smith, B.; Edwards, J.R.; Dudeck, M.A. The impact of coronavirus disease 2019 (COVID-19) on healthcare-Associated infections in 2020: A summary of data reported to the National Healthcare Safety Network. Infect. Control Hosp. Epidemiol. 2022, 43, 12–25. Available online: https://pubmed.ncbi.nlm.nih.gov/34473013/ (accessed on 21 January 2025). [CrossRef]
- Satta, G.; Rawson, T.M.; Moore, L.S.P. Coronavirus disease 2019 (COVID-19) impact on central-line-associated bloodstream infections (CLABSI): A systematic review. Infect. Prev. Pract. 2023, 5, 100313. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC10618700/ (accessed on 21 January 2025). [CrossRef]
- Alsaffar, M.J.; Alsheddi, F.M.; Humayun, T.; Aldalbehi, F.Z.; Alshammari, W.H.S.; Aldecoa, Y.S.; Burhan, N.M.; El-Saed, A.; Tawfeeq, S.; Alanazi, K.H. Impact of COVID-19 pandemic on the rates of central line–associated bloodstream infection and catheter-associated urinary tract infection in an intensive care setting: National experience. Am. J. Infect. Control 2023, 51, 1108–1113. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC10072974/ (accessed on 21 January 2025). [CrossRef]
- Milstone, A.M.; Sengupta, A. Do prolonged peripherally inserted central venous catheter dwell times increase the risk of bloodstream infection? Infect. Control Hosp. Epidemiol. 2010, 31, 1184–1187. Available online: https://pubmed.ncbi.nlm.nih.gov/20887217/ (accessed on 22 January 2025). [CrossRef]
- Stevens, M.P.; Doll, M.; Pryor, R.; Godbout, E.; Cooper, K.; Bearman, G. Impact of COVID-19 on traditional healthcare-associated infection prevention efforts. Infect. Control Hosp. Epidemiol. 2020, 41, 946–947. Available online: https://pubmed.ncbi.nlm.nih.gov/32297849/ (accessed on 22 January 2025). [CrossRef]
- Elangovan, S.; Lo, J.J.; Xie, Y.; Mitchell, B.; Graves, N.; Cai, Y. Impact of central-line-associated bloodstream infections and catheter-related bloodstream infections: A systematic review and meta-analysis. J. Hosp. Infect. 2024, 152, 126–137. Available online: https://pubmed.ncbi.nlm.nih.gov/39151801/ (accessed on 22 January 2025). [CrossRef]
- Hsu, H.E.; Wang, R.; Broadwell, C.; Horan, K.; Jin, R.; Rhee, C.; Lee, G.M. Association Between Federal Value-Based Incentive Programs and Health Care-Associated Infection Rates in Safety-Net and Non-Safety-Net Hospitals. JAMA Netw. Open 2020, 3, e209700. Available online: https://pubmed.ncbi.nlm.nih.gov/32639568/ (accessed on 22 January 2025). [CrossRef]
- Paredes, A.Z.; Hyer, J.M.; Diaz, A.; Tsilimigras, D.I.; Pawlik, T.M. Examining healthcare inequities relative to United States safety net hospitals. Am. J. Surg. 2020, 220, 525–531. Available online: https://pubmed.ncbi.nlm.nih.gov/32014296/ (accessed on 22 January 2025). [CrossRef] [PubMed]
- Cevasco, M.; Borzecki, A.M.; O’Brien, W.J.; Chen, Q.; Shin, M.H.; Itani, K.M.F.; Rosen, A.K. Validity of the AHRQ Patient Safety Indicator “central venous catheter-related bloodstream infections. J. Am. Coll. Surg. 2011, 212, 984–990. Available online: https://pubmed.ncbi.nlm.nih.gov/21489833/ (accessed on 19 April 2025). [CrossRef]
| Statistic | Range | |
|---|---|---|
| Hospitalizations Meeting Inclusion, count | ||
| Unweighted | 1,311,933 | |
| Weighted | 6,559,663 | |
| CVC Count, % | ||
| 1 | 90.9 | |
| 2 | 7.8 | |
| 3+ | 1.3 | |
| ICU (Intubation and/or Pressor), % | 31.2 | |
| Intubation | 29.9 | |
| Pressor | 3.6 | |
| CVC Placed in ICU, % | 24.4 | |
| Total Parenteral Nutrition, % | 2.3 | |
| Dialysis, % | 7.2 | |
| Age, median [IQR] | 63 [51–74] | 18–90 |
| Sex, % | ||
| Male | 52.0 | |
| Female | 48.0 | |
| Race, % | ||
| White | 69.3 | |
| Black | 15.5 | |
| Hispanic | 9.7 | |
| Other | 5.6 | |
| Primary Payer, % | ||
| Medicare | 54.5 | |
| Medicaid | 17.2 | |
| Private | 21.5 | |
| Other | 6.8 | |
| Income Quartile, % | ||
| 1 | 32.2 | |
| 2 | 26.4 | |
| 3 | 23.1 | |
| 4 | 18.2 | |
| Urban/Rural (patient), % | ||
| Urban | 83.3 | |
| Rural | 16.7 | |
| History of Alcohol Abuse, % | ||
| No | 92.6 | |
| Yes | 7.4 | |
| Health-related Social Needs, % | ||
| Employment Issue | 0.2 | |
| Family Issue | 0.2 | |
| Housing Issue | 1.1 | |
| Psycho-social Issue | 0.1 | |
| Socioeconomic Issue | 0.4 | |
| Charlson Comorbidity Index, median [IQR] | 2 [1–5] | 0–18 |
| Hospital Location-Teaching Status, % | ||
| Rural | 6.7 | |
| Urban Nonteaching | 20.9 | |
| Urban Teaching | 72.3 | |
| Year of Hospitalization, % | ||
| 2016 | 15.7 | |
| 2017 | 15.6 | |
| 2018 | 14.6 | |
| 2019 | 13.8 | |
| 2020 | 13.7 | |
| 2021 | 14.1 | |
| 2022 | 12.3 |
| Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|
| % | OR (95% CI) | p | OR (95% CI) | p | |
| Overall | 0.25 | - | - | - | - |
| CVC Count | |||||
| 3+ | 1.75 | 9.93 (8.73–11.03) | <0.001 | 8.29 (7.25–9.48) | <0.001 |
| 2 | 0.77 | 4.37 (4.01–4.76) | <0.001 | 4.01 (3.66–4.39) | <0.001 |
| 1 | 0.18 | Reference | Reference | ||
| CVC Placed in ICU | |||||
| Yes | 0.23 | 0.94 (0.87–1.03) | 0.176 | 0.68 (0.62–0.74) | <0.001 |
| No | 0.25 | Reference | Reference | ||
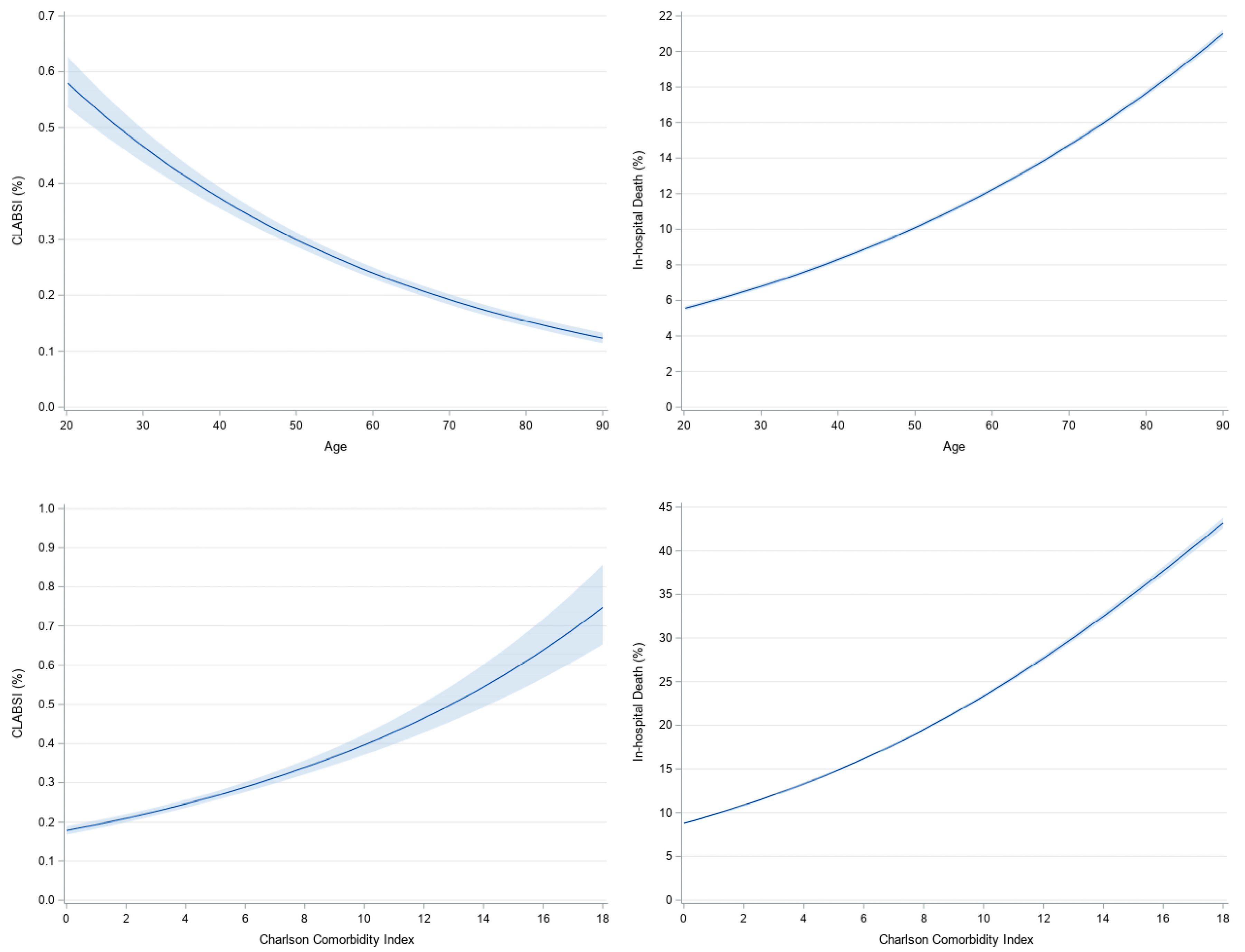
| Age (per 10 years) | Figure 2 | 0.80 (0.79–0.82) | <0.001 | 0.77 (0.75–0.79) | <0.001 |
| Sex | |||||
| Female | 0.24 | 0.92 (0.86–0.99) | 0.023 | 0.94 (0.88–1.02) | 0.123 |
| Male | 0.26 | Reference | Reference | ||
| Race | |||||
| Black | 0.36 | 1.71 (1.56–1.87) | <0.001 | 1.30 (1.18–1.43) | <0.001 |
| Hispanic | 0.29 | 1.38 (1.22–1.57) | <0.001 | 1.13 (0.99–1.28) | 0.062 |
| Other | 0.25 | 1.20 (1.03–1.40) | 0.022 | 1.06 (0.90–1.24) | 0.500 |
| White | 0.21 | Reference | Reference | ||
| Primary Payer | |||||
| Medicare | 0.20 | 0.80 (0.73–0.88) | <0.001 | 1.15 (1.03–1.28) | 0.012 |
| Medicaid | 0.38 | 1.51 (1.36–1.68) | <0.001 | 1.18 (1.06–1.32) | 0.002 |
| Other | 0.26 | 1.02 (0.88–1.19) | 0.786 | 0.96 (0.82–1.12) | 0.581 |
| Private | 0.25 | Reference | Reference | ||
| Income Quartile | |||||
| 1 | 0.28 | 1.28 (1.14–1.43) | <0.001 | 1.03 (0.92–1.16) | 0.577 |
| 2 | 0.23 | 1.07 (0.95–1.20) | 0.268 | 0.98 (0.87–1.10) | 0.716 |
| 3 | 0.23 | 1.06 (0.94–1.19) | 0.374 | 0.98 (0.87–1.11) | 0.759 |
| 4 | 0.22 | Reference | Reference | ||
| Urban/Rural (patient) | |||||
| Rural | 0.23 | 0.93 (0.84–1.03) | 0.187 | 1.06 (0.94–1.20) | 0.350 |
| Urban | 0.25 | Reference | Reference | ||
| History of Alcohol Abuse | |||||
| Yes | 0.22 | 0.90 (0.78–1.03) | 0.124 | 0.71 (0.62–0.82) | <0.001 |
| No | 0.25 | Reference | Reference | ||
| Health-related Social Needs | |||||
| Employment Issue | * | * | * | * | * |
| Family Issue | * | * | * | * | * |
| Housing Issue | |||||
| Yes | 0.28 | 1.13 (0.79–1.62) | 0.515 | 0.89 (0.62–1.29) | 0.543 |
| No | 0.25 | Reference | Reference | ||
| Psycho-social Issue | * | * | * | * | * |
| Socioeconomic Issue | |||||
| Yes | 0.27 | 1.11 (0.66–1.86) | 0.688 | 1.10 (0.66–1.81) | 0.717 |
| No | 0.25 | Reference | Reference | ||
| Charlson Comorbidity Index | Figure 2 | 1.08 (1.07–1.09) | <0.001 | 1.09 (1.08–1.11) | <0.001 |
| Hospital Location-Teaching Status | |||||
| Rural | 0.16 | 0.58 (0.48–0.69) | <0.001 | 0.65 (0.53–0.80) | <0.001 |
| Urban Nonteaching | 0.17 | 0.63 (0.57–0.70) | <0.001 | 0.73 (0.65–0.81) | <0.001 |
| Urban Teaching | 0.27 | Reference | Reference | ||
| Year of Hospitalization | |||||
| 2016 | 0.25 | 1.11 (0.95–1.29) | 0.191 | 1.22 (1.05–1.42) | 0.010 |
| 2017 | 0.22 | 0.98 (0.83–1.15) | 0.791 | 1.05 (0.89–1.23) | 0.574 |
| 2018 | 0.20 | 0.91 (0.77–1.07) | 0.250 | 0.96 (0.82–1.13) | 0.625 |
| 2019 | 0.23 | 1.02 (0.86–1.20) | 0.840 | 1.06 (0.90–1.25) | 0.495 |
| 2020 | 0.29 | 1.32 (1.13–1.53) | <0.001 | 1.30 (1.12–1.50) | 0.001 |
| 2021 | 0.31 | 1.38 (1.18–1.61) | <0.001 | 1.34 (1.15–1.56) | <0.001 |
| 2022 | 0.22 | Reference | Reference | ||
| Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|
| % | OR (95% CI) | p | aOR (95% CI) | p | |
| Overall | 13.3 | - | - | - | - |
| CLABSI | |||||
| Yes | 14.1 | 1.07 (0.96–1.19) | 0.218 | 0.91 (0.80–1.02) | 0.114 |
| No | 13.3 | Reference | Reference | ||
| CVC Count | |||||
| 3+ | 31.3 | 3.37 (3.25–3.49) | <0.001 | 2.34 (2.24–2.45) | <0.001 |
| 2 | 26.2 | 2.62 (2.57–2.68) | <0.001 | 2.02 (1.98–2.06) | <0.001 |
| 1 | 11.9 | Reference | Reference | ||
| CVC Placed in ICU | |||||
| Yes | 34.8 | 7.84 (7.73–7.94) | <0.001 | 7.20 (7.10–7.30) | <0.001 |
| No | 6.4 | Reference | Reference | ||
| Age (per 10 years) | Figure 2 | 1.24 (1.24–1.25) | <0.001 | 1.33 (1.32–1.33) | <0.001 |
| Sex | |||||
| Female | 12.2 | 0.84 (0.83–0.85) | <0.001 | 0.89 (0.88–0.90) | <0.001 |
| Male | 14.3 | Reference | Reference | ||
| Race | |||||
| Black | 12.9 | 1.01 (0.99–1.03) | 0.161 | 1.02 (1.00–1.04) | 0.022 |
| Hispanic | 15.7 | 1.27 (1.23–1.30) | <0.001 | 1.26 (1.23–1.29) | <0.001 |
| Other | 16.6 | 1.36 (1.32–1.39) | <0.001 | 1.20 (1.17–1.24) | <0.001 |
| White | 12.8 | Reference | Reference | ||
| Primary Payer | |||||
| Medicare | 14.9 | 1.48 (1.45–1.51) | <0.001 | 0.96 (0.94–0.98) | <0.001 |
| Medicaid | 11.0 | 1.04 (1.01–1.06) | 0.002 | 1.07 (1.04–1.09) | <0.001 |
| Other | 14.1 | 1.38 (1.34–1.42) | <0.001 | 1.28 (1.25–1.32) | <0.001 |
| Private | 10.6 | Reference | Reference | ||
| Income Quartile | |||||
| 1 | 13.9 | 1.10 (1.07–1.12) | <0.001 | 1.12 (1.10–1.15) | <0.001 |
| 2 | 13.1 | 1.03 (1.01–1.05) | 0.013 | 1.06 (1.04–1.08) | <0.001 |
| 3 | 13.0 | 1.02 (0.99–1.04) | 0.081 | 1.03 (1.01–1.05) | 0.005 |
| 4 | 12.8 | Reference | Reference | ||
| Urban/Rural (patient) | |||||
| Rural | 13.3 | 1.01 (0.99–1.03) | 0.534 | 1.07 (1.05–1.10) | <0.001 |
| Urban | 13.3 | Reference | Reference | ||
| History of Alcohol Abuse | |||||
| Yes | 15.9 | 1.26 (1.23–1.28) | <0.001 | 1.12 (1.10–1.15) | <0.001 |
| No | 13.1 | Reference | Reference | ||
| Health-related Social Needs | |||||
| Employment Issue | |||||
| Yes | 6.8 | 0.48 (0.39–0.57) | <0.001 | 0.65 (0.54–0.79) | <0.001 |
| No | 13.3 | Reference | Reference | ||
| Family Issue | |||||
| Yes | 10.9 | 0.79 (0.70–0.91) | <0.001 | 0.82 (0.71–0.94) | 0.006 |
| No | 13.3 | Reference | Reference | ||
| Housing Issue | |||||
| Yes | 6.8 | 0.48 (0.44–0.52) | <0.001 | 0.62 (0.57–0.68) | <0.001 |
| No | 13.3 | Reference | Reference | ||
| Psycho-social Issue | |||||
| Yes | 9.1 | 0.65 (0.51–0.84) | <0.001 | 0.74 (0.60–0.92) | 0.007 |
| No | 13.3 | Reference | Reference | ||
| Socioeconomic Issue | |||||
| Yes | 7.8 | 0.55 (0.50–0.62) | <0.001 | 0.55 (0.49–0.61) | <0.001 |
| No | 13.3 | Reference | Reference | ||
| Charlson Comorbidity Index | Figure 2 | 1.12 (1.12–1.12) | <0.001 | 1.05 (1.05–1.05) | <0.001 |
| Hospital Location-Teaching Status | |||||
| Rural | 11.5 | 0.81 (0.78–0.84) | <0.001 | 0.8 (0.77–0.83) | <0.001 |
| Urban Nonteaching | 11.9 | 0.84 (0.82–0.86) | <0.001 | 0.9 (0.88–0.92) | <0.001 |
| Urban Teaching | 13.8 | Reference | Reference | ||
| Year of Hospitalization | |||||
| 2016 | 9.8 | 0.59 (0.57–0.61) | <0.001 | 0.68 (0.66–0.71) | <0.001 |
| 2017 | 10.2 | 0.62 (0.60–0.64) | <0.001 | 0.68 (0.66–0.71) | <0.001 |
| 2018 | 10.4 | 0.63 (0.61–0.66) | <0.001 | 0.68 (0.65–0.70) | <0.001 |
| 2019 | 10.8 | 0.66 (0.64–0.69) | <0.001 | 0.68 (0.66–0.70) | <0.001 |
| 2020 | 17.0 | 1.12 (1.08–1.16) | <0.001 | 1.05 (1.01–1.09) | 0.009 |
| 2021 | 20.4 | 1.40 (1.36–1.45) | <0.001 | 1.39 (1.35–1.44) | <0.001 |
| 2022 | 15.5 | Reference | Reference | ||
| CLABSI vs. No CLABSI | |||
|---|---|---|---|
| aOR (95% CI) | p | Interaction p | |
| Sex | |||
| Female | 1.03 (0.85–1.24) | 0.777 | 0.097 |
| Male | 0.83 (0.81–0.98) | 0.025 | |
| Race | |||
| Black | 0.76 (0.57–1.01) | 0.062 | 0.085 |
| Hispanic | 1.22 (0.92–1.61) | 0.163 | |
| Other | 0.75 (0.46–1.22) | 0.243 | |
| White | 0.90 (0.77–1.06) | 0.215 | |
| Primary Payer | |||
| Medicare | 0.97 (0.82–1.16) | 0.764 | 0.025 |
| Medicaid | 0.67 (0.52–0.88) | 0.004 | |
| Other | 0.67 (0.40–1.11) | 0.121 | |
| Private | 1.12 (0.87–1.44) | 0.398 | |
| Income Quartile | |||
| 1 | 0.82 (0.66–1.01) | 0.062 | 0.492 |
| 2 | 0.99 (0.78–1.25) | 0.939 | |
| 3 | 1.01 (0.79–1.31) | 0.919 | |
| 4 | 0.85 (0.63–1.13) | 0.261 | |
| Urban/Rural (patient) | |||
| Rural | 1.12 (0.83–1.50) | 0.459 | 0.130 |
| Urban | 0.87 (0.76–0.99) | 0.041 | |
| History of Alcohol Abuse | |||
| Yes | 0.35 (0.20–0.61) | <0.001 | <0.001 |
| No | 0.97 (0.85–1.10) | 0.602 | |
| Health-related Social Needs | |||
| Employment Issue | |||
| Yes | * | * | * |
| No | * | * | |
| Family Issue | |||
| Yes | * | * | * |
| No | * | * | |
| Housing Issue | |||
| Yes | * | * | * |
| No | * | * | |
| Psycho-social Issue | |||
| Yes | * | * | * |
| No | * | * | |
| Socioeconomic Issue | |||
| Yes | * | * | * |
| No | * | * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mielke, N.; Walters, R.W.; Ahmad, F. Health Disparities in Central Line-Associated Bloodstream Infections: Analysis of the U.S. National Inpatient Sample Database (2016–2022). Infect. Dis. Rep. 2025, 17, 105. https://doi.org/10.3390/idr17050105
Mielke N, Walters RW, Ahmad F. Health Disparities in Central Line-Associated Bloodstream Infections: Analysis of the U.S. National Inpatient Sample Database (2016–2022). Infectious Disease Reports. 2025; 17(5):105. https://doi.org/10.3390/idr17050105
Chicago/Turabian StyleMielke, Nicholas, Ryan W. Walters, and Faran Ahmad. 2025. "Health Disparities in Central Line-Associated Bloodstream Infections: Analysis of the U.S. National Inpatient Sample Database (2016–2022)" Infectious Disease Reports 17, no. 5: 105. https://doi.org/10.3390/idr17050105
APA StyleMielke, N., Walters, R. W., & Ahmad, F. (2025). Health Disparities in Central Line-Associated Bloodstream Infections: Analysis of the U.S. National Inpatient Sample Database (2016–2022). Infectious Disease Reports, 17(5), 105. https://doi.org/10.3390/idr17050105







