Crusted Scabies, a Neglected Tropical Disease: Case Series and Literature Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Case Reports
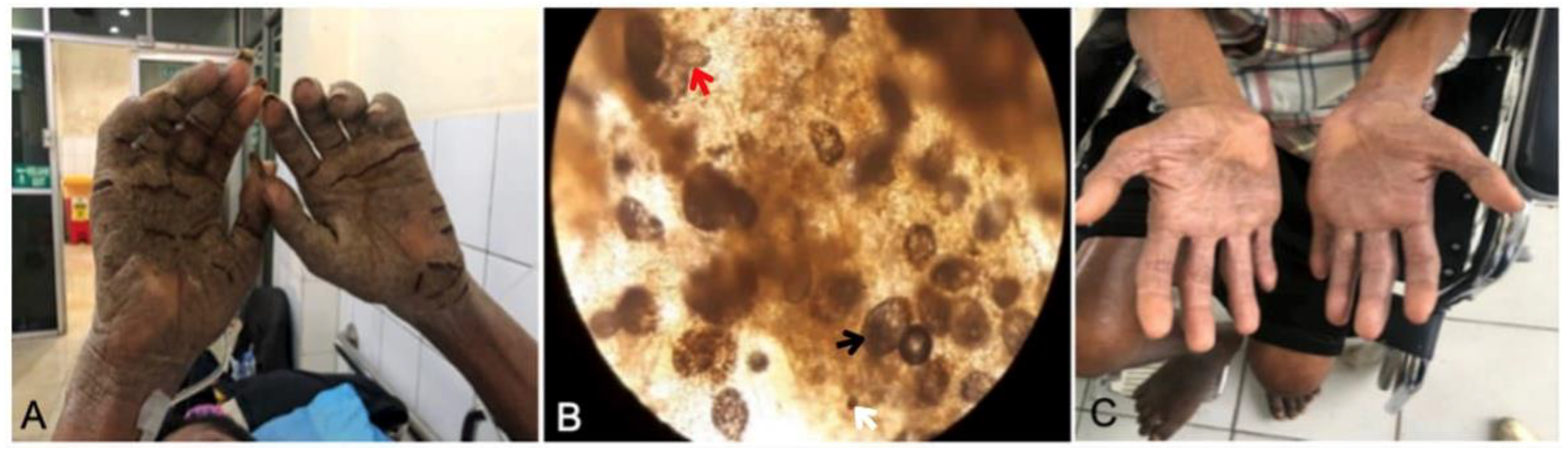
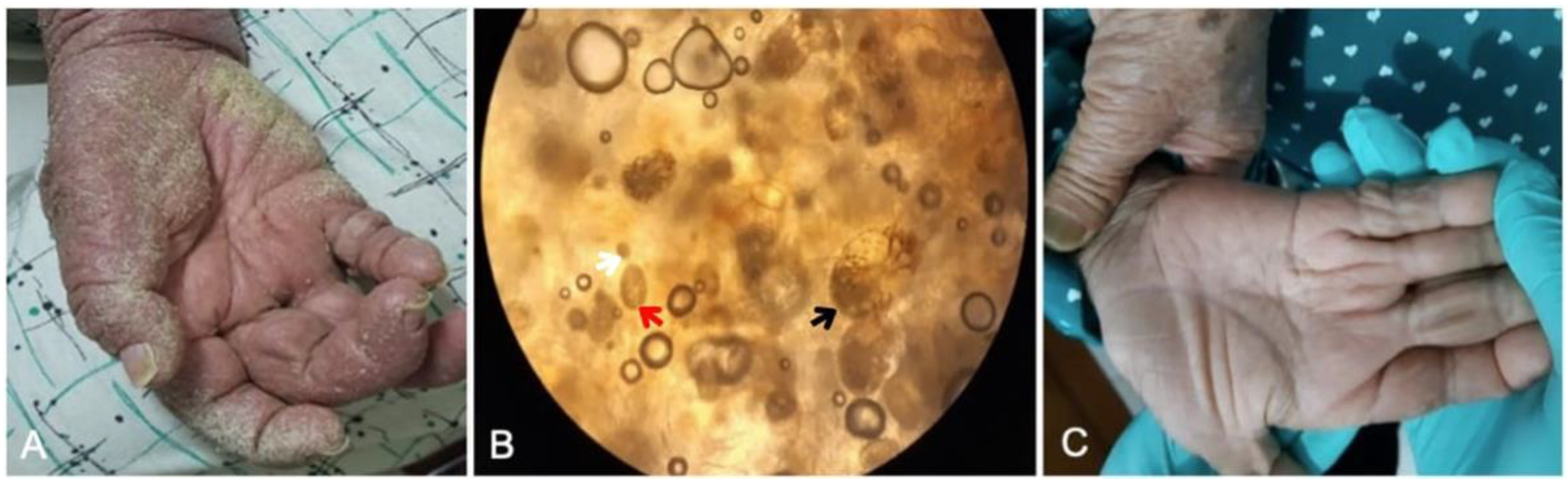
3.1.1. Case 1
3.1.2. Case 2
3.1.3. Case 3
3.2. Literature Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Engelman, D.; Marks, M.; Steer, A.C.; Beshah, A.; Biswas, G.; Chosidow, O.; Coffeng, L.E.; Lardizabal Dofitas, B.; Enbiale, W.; Fallah, M.; et al. A framework for scabies control. PLoS Negl. Trop. Dis. 2021, 15, e0009661. [Google Scholar] [CrossRef] [PubMed]
- Walton, S.F.; Currie, B.J. Problems in diagnosing scabies, a global disease in human and animal populations. Clin. Microbiol. Rev. 2007, 20, 268–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Moamly, A.A. Scabies as a part of the World Health Organization roadmap for neglected tropical diseases 2021–2030: What we know and what we need to do for global control. Trop. Med. Health 2021, 49, 64. [Google Scholar] [CrossRef] [PubMed]
- Chandler, D.J.; Fuller, L.C. A review of scabies: An infestation more than skin deep. Dermatology 2019, 235, 79–90. [Google Scholar] [CrossRef]
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef] [Green Version]
- Walton, S.F.; Pizzutto, S.; Slender, A.; Viberg, L.; Holt, D.; Hales, B.J.; Kemp, D.J.; Currie, B.J.; Rolland, J.M.; O’Hehir, R. Increased allergic immune response to Sarcoptes scabiei antigens in crusted versus ordinary scabies. Clin. Vaccine Immunol. 2010, 17, 1428–1438. [Google Scholar] [CrossRef] [Green Version]
- Bhat, S.A.; Mounsey, K.E.; Liu, X.; Walton, S.F. Host immune responses to the itch mite, Sarcoptes scabiei, in humans. Parasites Vectors 2017, 10, 385. [Google Scholar] [CrossRef] [Green Version]
- Walton, S.F.; Beroukas, D.; Roberts-Thomson, P.; Currie, B.J. New insights into disease pathogenesis in crusted (Norwegian) scabies: The skin immune response in crusted scabies. Br. J. Dermatol. 2008, 158, 1247–1255. [Google Scholar] [CrossRef]
- Fuller, L.C. Epidemiology of scabies. Curr. Opin. Infect. Dis. 2013, 26, 123–126. [Google Scholar] [CrossRef]
- Engelman, D.; Kiang, K.; Chosidow, O.; McCarthy, J.; Fuller, C.; Lammie, P.; Hay, R.; Steer, A. Toward the global control of human scabies: Introducing the International Alliance for the Control of Scabies. PLoS Negl. Trop. Dis. 2013, 7, e2167. [Google Scholar] [CrossRef] [Green Version]
- Banerji, A.; Canadian Paediatric Society Inuit and Métis Health Committee, F.N. Scabies. Paediatr. Child Health 2015, 20, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Hasan, T.; Krause, V.L.; James, C.; Currie, B.J. Crusted scabies; a 2-year prospective study from the Northern Territory of Australia. PLoS Negl. Trop. Dis. 2020, 14, e0008994. [Google Scholar] [CrossRef] [PubMed]
- Seidelman, J.; Garza, R.M.; Smith, C.M.; Fowler, V.G.J. More than a mite contagious: Crusted scabies. Am. J. Med. 2017, 130, 1042–1044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palaniappan, V.; Gopinath, H.; Kaliaperumal, K. Crusted scabies. Am. J. Trop. Med. Hyg. 2021, 104, 787–788. [Google Scholar] [CrossRef] [PubMed]
- Giannattasio, A.; Rosa, M.; Esposito, S.; Di Mita, O.; Angrisani, F.; Acierno, S.; D’Anna, C.; Barbato, F.; Tipo, V.; Ametrano, O. Concomitant SARS-CoV-2 infection and crusted scabies in a 4-month infant. J. Eur. Acad. Dermatol. Venereol. 2022, 36, e188–e190. [Google Scholar] [CrossRef]
- Sil, A.; Punithakumar, E.J.; Chakraborty, S.; Bhanja, D.B.; Panigrahi, A.; Das, A. Crusted scabies. Postgrad. Med. J. 2020, 96, 444. [Google Scholar] [CrossRef]
- Cuellar-Barboza, A.; Cardenas-de la Garza, J.A.; García-Lozano, J.A.; Martinez-Moreno, A.; Jaramillo-Moreno, G.; Ocampo-Candiani, J. A case of hyperkeratotic crusted scabies. PLoS Negl. Trop. Dis. 2020, 14, e0007918. [Google Scholar] [CrossRef]
- Cartron, A.M.; Boettler, M.; Chung, C.; Trinidad, J.C. Crusted scabies in an elderly woman. Dermatol. Online J. 2020, 26, 13. [Google Scholar] [CrossRef]
- Agyei, M.; Ofori, A.; Tannor, E.K.; Annan, J.J.; Norman, B.R. A forgotten parasitic infestation in an immunocompromised patient-a case report of crusted scabies. Pan Afr. Med. J. 2020, 36, 238. [Google Scholar] [CrossRef]
- Wang, M.K.; Chin-Yee, B.; Lo, C.K.-L.; Lee, S.; El-Helou, P.; Alowami, S.; Gangji, A.; Ribic, C. Crusted scabies in a renal transplant recipient treated with daily ivermectin: A case report and literature review. Transpl. Infect. Dis. 2019, 21, e13077. [Google Scholar] [CrossRef]
- Aukerman, W.; Curfman, K.; Urias, D.; Shayesteh, K. Norwegian Scabies management after prolonged disease course: A case report. Int. J. Surg. Case Rep. 2019, 61, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Heresi, G.; Al Hammoud, R. Norwegian scabies in a patient with down syndrome. J. Pediatr. 2019, 209, 253.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, A.K.C.; Leong, K.F.; Lam, J.M. Pruritic crusted scabies in an immunocompetent infant. Case Rep. Pediatr. 2019, 2019, 9542857. [Google Scholar] [CrossRef] [Green Version]
- Stingeni, L.; Tramontana, M.; Principato, M.; Moretta, I.; Principato, S.; Bianchi, L.; Hansel, K. Nosocomial outbreak of crusted scabies in immunosuppressed patients caused by Sarcoptes scabiei var. canis. Br. J. Dermatol. 2020, 182, 498–500. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.A.; Esteves, A.; Mahia, Y.; Rosmaninho, A.; Silva, A. An itchy problem: A clinical case of crusted scabies. Eur. J. Case Rep. Intern. Med. 2017, 4, 591. [Google Scholar] [CrossRef] [Green Version]
- Yari, N.; Malone, C.H.; Rivas, A. Misdiagnosed crusted scabies in an AIDS patient leads to hyperinfestation. Cutis 2017, 99, 202–204. [Google Scholar]
- Ebrahim, K.C.; Alves, J.B.; de Araújo Tomé, L.; de Moraes, C.F.; Gaspar, A.D.; Franck, K.F.; Hussein, M.A.; da Cruz, L.R.; Ebrahim, L.D.; de Oliveira Sidney, L.F. Norwegian scabies-rare case of atypical manifestation. An. Bras. Dermatol. 2016, 91, 826–828. [Google Scholar] [CrossRef] [Green Version]
- Nagsuk, P.; Moore, R.; Lopez, L. A case report of crusted scabies in an adult patient with Down syndrome. Dermatol. Online J. 2015, 21, 13. [Google Scholar] [CrossRef]
- Del Borgo, C.; Belvisi, V.; Tieghi, T.; Mastroianni, C.M. Atypical presentation of crusted (Norwegian) scabies. Infection 2015, 43, 623–624. [Google Scholar] [CrossRef] [Green Version]
- Da Rocha Lima, F.C.; Cerqueira, A.M.M.; Guimarães, M.B.S.; de Sousa Padilha, C.B.; Craide, F.H.; Bombardelli, M. Crusted scabies due to indiscriminate use of glucocorticoid therapy in infant. An. Bras. Dermatol. 2017, 92, 383–385. [Google Scholar] [CrossRef]
- Maghrabi, M.M.; Lum, S.; Joba, A.T.; Meier, M.J.; Holmbeck, R.J.; Kennedy, K. Norwegian crusted scabies: An unusual case presentation. J. Foot Ankle Surg. 2014, 53, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Vandergriff, T. Scabies of the nail unit. Dermatol. Online J. 2014, 20, 16. [Google Scholar] [CrossRef]
- Fujimoto, K.; Kawasaki, Y.; Morimoto, K.; Kikuchi, I.; Kawana, S. Treatment for crusted scabies: Limitations and side effects of treatment with ivermectin. J. Nippon Med. Sch. 2014, 81, 157–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Sánchez, M.; Saeb-Lima, M.; Alvarado-de la Barrera, C.; Reyes-Terán, G. Crusted scabies-associated immune reconstitution inflammatory syndrome. BMC Infect. Dis. 2012, 12, 323. [Google Scholar] [CrossRef] [Green Version]
- Karthikeyan, K. Crusted scabies. Indian J. Dermatol. Venereol. Leprol. 2009, 75, 340–347. [Google Scholar] [CrossRef]
- Kandi, V. Laboratory diagnosis of scabies using a simple saline mount: A clinical microbiologist’s report. Cureus 2017, 9, e1102. [Google Scholar] [CrossRef] [Green Version]
- Gualdi, G.; Bigi, L.; Galdo, G.; Pellacani, G. Neonatal Norwegian scabies: Three cooperating causes. J. Dermatol. Case Rep. 2009, 3, 34–37. [Google Scholar] [CrossRef]
- Arlian, L.G.; Vyszenski-Moher, D.L. Life cycle of Sarcoptes scabiei var. canis. J. Parasitol. 1988, 74, 427–430. [Google Scholar] [CrossRef]
- Arlian, L.G.; Morgan, M.S. A review of Sarcoptes scabiei: Past, present and future. Parasites Vectors 2017, 10, 297. [Google Scholar] [CrossRef]
- Siagian, F.E.; Ronny, R.; Susiantoro, U.; Widiyani, S.; Yulia, H.C.; Sisirawaty, S. Unusual microscopic appearance of Sarcoptes scabiei from skin scrapping sample and its epidemiology. Int. J. Res. Dermatol. 2020, 6, 688–692. [Google Scholar] [CrossRef]
- Gunning, K.; Kiraly, B.; Pippitt, K. Lice and scabies: Treatment update. Am. Fam. Physician 2019, 99, 635–642. [Google Scholar] [PubMed]
- Rahdar, M.; Maraghi, S. Norwegian scabies in two immune-compromised patients: A case report. Iran. J. Public Health. 2019, 48, 1169–1173. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Walton, S.F.; Murray, H.C.; King, M.; Kelly, A.; Holt, D.C.; Currie, B.J.; McCarthy, J.S.; Mounsey, K.E. Crusted scabies is associated with increased IL-17 secretion by skin T cells. Parasite Immunol. 2014, 36, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Talaga-Ćwiertnia, K. Sarcoptes infestation. What is already known, and what is new about Scabies at the beginning of the third decade of the 21st century? Pathogens 2021, 10, 868. [Google Scholar] [CrossRef]
- Sánchez-Borges, M.; González-Aveledo, L.; Capriles-Hulett, A.; Caballero-Fonseca, F. Scabies, crusted (Norwegian) scabies and the diagnosis of mite sensitisation. Allergol. Immunopathol. 2018, 46, 276–280. [Google Scholar] [CrossRef]
- Kulkarni, S.; Shah, H.; Patel, B.; Bhuptani, N. Crusted scabies: Presenting as erythroderma in a human immunodeficiency virus-seropositive patient. Indian J. Sex. Transm. Dis. AIDS 2016, 37, 72–74. [Google Scholar] [CrossRef] [Green Version]
- Baumrin, E.; Piette, E.; Micheletti, R. A crusted rash in a patient with AIDS. JAMA 2015, 313, 298–299. [Google Scholar] [CrossRef]
- Cohen, P.R. Classic and non-classic (surrepticius) scabies: Diagnostic and treatment considerations. Cureus 2020, 12, e7419. [Google Scholar] [CrossRef] [Green Version]
- Bollea Garlatti, L.A.; Torre, A.C.; Bollea Garlatti, M.L.; Galimberti, R.L.; Argenziano, G. Dermoscopy aids the diagnosis of crusted scabies in an erythrodermic patient. J. Am. Acad. Dermatol. 2015, 73, e93–e95. [Google Scholar] [CrossRef]
- Micali, G.; Lacarrubba, F.; Verzi, A.E.; Nasca, M.R. Low-cost equipment for diagnosis and management of endemic scabies outbreaks in underserved populations. Clin. Infect. Dis. 2015, 60, 327–329. [Google Scholar] [CrossRef] [Green Version]
- Mika, A.; Reynolds, S.L.; Pickering, D.; McMillan, D.; Sriprakash, K.S.; Kemp, D.J.; Fischer, K. Complement inhibitors from scabies mites promote streptococcal growth--a novel mechanism in infected epidermis? PLoS Negl. Trop. Dis. 2012, 6, e1563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fischer, K.; Holt, D.; Currie, B.; Kemp, D. Scabies: Important clinical consequences explained by new molecular studies. Adv. Parasitol. 2012, 79, 339–373. [Google Scholar] [CrossRef] [PubMed]
- Marks, M.I. Skin Infections BT-Pediatric Infectious Diseases for the Practitioner; Marks, M.I., Ed.; Springer: New York, NY, USA, 1985; pp. 476–568. [Google Scholar]
- Apap, C.; Piscopo, T.; Boffa, M.J. Crusted (Norwegian) scabies treated with oral ivermectin: A case report and overview. Malta Med. J. 2021, 25, 49–53. [Google Scholar]
- Gutte, R.M. Bullous scabies in an adult: A case report with review of literature. Indian Dermatol. Online J. 2013, 4, 311–313. [Google Scholar] [CrossRef]
- Thomas, J.; Peterson, G.M.; Walton, S.F.; Carson, C.F.; Naunton, M.; Baby, K.E. Scabies: An ancient global disease with a need for new therapies. BMC Infect. Dis. 2015, 15, 250. [Google Scholar] [CrossRef] [Green Version]
- Riebenbauer, K.; Weber, P.B.; Haitel, A.; Walochnik, J.; Valencak, J.; Meyersburg, D.; Kinaciyan, T.; Handisurya, A. Comparison of permethrin-based treatment strategies against scabies in infants and young children. J. Pediatr. 2022, in press. [Google Scholar] [CrossRef]
- Salavastru, C.M.; Chosidow, O.; Boffa, M.J.; Janier, M.; Tiplica, G.S. European guideline for the management of scabies. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1248–1253. [Google Scholar] [CrossRef] [Green Version]
- Karthikeyan, K. Treatment of scabies: Newer perspectives. Postgrad. Med. J. 2005, 81, 11–17. [Google Scholar] [CrossRef] [Green Version]
- van der Linden, N.; van Gool, K.; Gardner, K.; Dickinson, H.; Agostino, J.; Regan, D.G.; Dowden, M.; Viney, R. A systematic review of scabies transmission models and data to evaluate the cost-effectiveness of scabies interventions. PLoS Negl. Trop. Dis. 2019, 13, e0007182. [Google Scholar] [CrossRef] [Green Version]
- Chosidow, O. Scabies. N. Engl. J. Med. 2006, 354, 1718–1727. [Google Scholar] [CrossRef]
- Strong, M.; Johnstone, P. Interventions for treating scabies. Cochrane Database Syst. Rev. 2007, 2007, CD000320. [Google Scholar] [CrossRef] [PubMed]
- Ranjkesh, M.R.; Naghili, B.; Goldust, M.; Rezaee, E. The efficacy of permethrin 5% vs. oral ivermectin for the treatment of scabies. Ann. Parasitol. 2013, 59, 189–194. [Google Scholar] [PubMed]
- Khalil, S.; Abbas, O.; Kibbi, A.G.; Kurban, M. Scabies in the age of increasing drug resistance. PLoS Negl. Trop. Dis. 2017, 11, e0005920. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnstone, P.P.; Strong, M. Scabies. BMJ Clin. Evid. 2008, 2008, 1707. [Google Scholar] [PubMed]
- Davis, J.S.; McGloughlin, S.; Tong, S.Y.C.; Walton, S.F.; Currie, B.J. A novel clinical grading scale to guide the management of crusted scabies. PLoS Negl. Trop. Dis. 2013, 7, e2387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimose, L.; Munoz-Price, L.S. Diagnosis, prevention, and treatment of scabies. Curr. Infect. Dis. Rep. 2013, 15, 426–431. [Google Scholar] [CrossRef]
- Adji, A.; Rumokoy, L.J.M.; Salaki, C.L. Scabies vaccine as a new breakthrough for the challenge of Acaricides resistance BT. In Proceedings of the International Conference and the 10th Congress of the Entomological Society of Indonesia (ICCESI 2019), Bali, Indonesia, 6–9 October 2019; Atlantis Press: Amsterdam, The Netherlands, 2020; pp. 208–213. [Google Scholar]


| Location | Age (Year)/Sex | Comorbid | Treatment | Outcome |
|---|---|---|---|---|
| Beo, Talaud Island | 79, male | Neurological disorder (stroke) | Topical permethrin 5% cream every day for seven days, continued twice a week for three weeks and keratolytic agents | Complete regression |
| Tondano, Minahasa | 45, male | Metabolic disorder (diabetes mellitus) | Topical permethrin 5% cream every day for seven days, continued twice a week for three weeks and keratolytic agents | Complete regression |
| Modoinding, West Minahasa | 62, female | Neurological disorder (stroke) | Topical permethrin 5% cream every day for seven days, continued twice a week for one week | Complete regression |
| Country | Age (Year)/Sex | Associated Conditions | Treatment | Outcome | Reference |
|---|---|---|---|---|---|
| India | 54/male | Diabetes | Oral ivermectin, topical permethrin 5% cream | Complete regression | [15] |
| Italy | 0.3/male | SARS-CoV-2 infection | Oral ivermectin, topical permethrin 5% and urea 5% cream | Complete regression | [16] |
| India | 71/female | None | Oral ivermectin, permethrin cream | Complete regression | [17] |
| Mexico | 38/female | Down syndrome, dehydration | Intravenous fluids, oral ivermectin, topical permethrin 5% cream | Died | [18] |
| USA | Elderly/female | None | Oral ivermectin, topical permethrin 5% cream | Died (chronic aspiration) | [19] |
| Ghana | 44/female | HIV | Oral ivermectin, petroleum jelly, oral amoxycillin clavulanate (concomitant skin infection) | Complete regression | [20] |
| Canada | 65/male | Renal transplant recipient | Oral ivermectin | Complete regression | [21] |
| USA | 56/male | None | Oral ivermectin and topical permethrin, debridement | Complete regression | [22] |
| USA | 11/female | Down syndrome | Oral ivermectin, topical permethrin 5% cream, oral clindamycin (concomitant skin infection) | Improvement | [23] |
| Canada | 0.9/male | None | Topical permethrin 5% cream | Complete regression | [24] |
| Italy | 63/male | Bone marrow tranplantation | Oral ivermectin, benzyl benzoate ointment | Complete regression | [25] |
| USA | 53/female | None | Oral ivermectin, topical permethrin 5% cream | Complete regression | [13] |
| Portugal | 87/female | Mild vascular dementia | Oral ivermectin, topical sulfur 6% ointment, keratolytic creams | Complete regression | [26] |
| USA | 34/male | HIV | Oral ivermectin, topical permethrin 5% cream, oral trimethoprim-sulfamethoxazole, and oral combination elvitegravir-cobicistat-emtricitabine-tenofovir (for HIV) | Complete regression | [27] |
| Brazil | 19/male | None | Oral ivermectin, deltamethrin solution, oral amoxicillin clavulanate and clindamycin (concomitant skin infection) | Complete regression | [28] |
| USA | 46/female | Down syndrome | Oral ivermectin, topical permethrin 5% cream, oral doxycycline and sulfamethoxazole-trimethoprim (concomitant skin infection) | Complete regression | [29] |
| Italy | 67/male | HIV | Oral ivermectin, topical permethrin 5% cream, emollients, anti-keratolytic | Complete regression | [30] |
| Brazil | 0.3/male | None | Topical permethrin 1% lotion, intravenous antibiotic (concomitant skin infection) | Died | [31] |
| USA | 60/male | Bipolar disorder, schizoaffective disorder, hypertension, hepatitis C, and peripheral neuropathy secondary to alcoholism | Oral ivermectin and topical permethrin cream, oral Bactrim, in addition to the IV cefazolin (concomitant skin infection), debridement | Complete regression | [32] |
| USA | 66/male | Diabetes | Topical permethrin 5% cream | Complete regression | [33] |
| Japan | 90/male | Diabetes | Oral ivermectin, 1% gamma benzene hexachloride (γ-BHC) ointment, crotamiton ointment containing benzyl benzoate | Complete regression | [34] |
| Mexico | 28/female | HIV | Oral ivermectin, topical ointment containing balsam of Peru, precipitate sulfur and benzoate butter | Complete regression | [35] |
| Darwin, Northern Territory | 47 (median age)/female (59%) | Diabetic, kidney failure (dialysis), chronic lung disease, chronic liver disease, HTLV-1, other immunosuppression, no comorbidities | Oral ivermectin together with daily alternating topical scabicides and topical keratolytic cream. | Complete regression (84%), died (16%) | [12] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niode, N.J.; Adji, A.; Gazpers, S.; Kandou, R.T.; Pandaleke, H.; Trisnowati, D.M.; Tumbelaka, C.; Donata, E.; Djaafara, F.N.; Kusuma, H.I.; et al. Crusted Scabies, a Neglected Tropical Disease: Case Series and Literature Review. Infect. Dis. Rep. 2022, 14, 479-491. https://doi.org/10.3390/idr14030051
Niode NJ, Adji A, Gazpers S, Kandou RT, Pandaleke H, Trisnowati DM, Tumbelaka C, Donata E, Djaafara FN, Kusuma HI, et al. Crusted Scabies, a Neglected Tropical Disease: Case Series and Literature Review. Infectious Disease Reports. 2022; 14(3):479-491. https://doi.org/10.3390/idr14030051
Chicago/Turabian StyleNiode, Nurdjannah Jane, Aryani Adji, Shienty Gazpers, Renate Tamara Kandou, Herry Pandaleke, Dwi Martina Trisnowati, Christy Tumbelaka, Elrovita Donata, Fauziyyah Nurani Djaafara, Hendrix Indra Kusuma, and et al. 2022. "Crusted Scabies, a Neglected Tropical Disease: Case Series and Literature Review" Infectious Disease Reports 14, no. 3: 479-491. https://doi.org/10.3390/idr14030051
APA StyleNiode, N. J., Adji, A., Gazpers, S., Kandou, R. T., Pandaleke, H., Trisnowati, D. M., Tumbelaka, C., Donata, E., Djaafara, F. N., Kusuma, H. I., Rabaan, A. A., Garout, M., Almuthree, S. A., Alhani, H. M., Aljeldah, M., Albayat, H., Alsaeed, M., Alfouzan, W. A., Nainu, F., ... Tallei, T. E. (2022). Crusted Scabies, a Neglected Tropical Disease: Case Series and Literature Review. Infectious Disease Reports, 14(3), 479-491. https://doi.org/10.3390/idr14030051










