Cardiac Involvement in COVID-19 Patients: A Contemporary Review
Abstract
1. Introduction
2. Methods
3. Results and Critical Findings
3.1. ECG Results
3.2. Results of Cardiac Ultrasound and Advanced Imaging
3.3. Histopathological Tests Results
3.4. Therapies and Advanced Treatment
4. Discussion
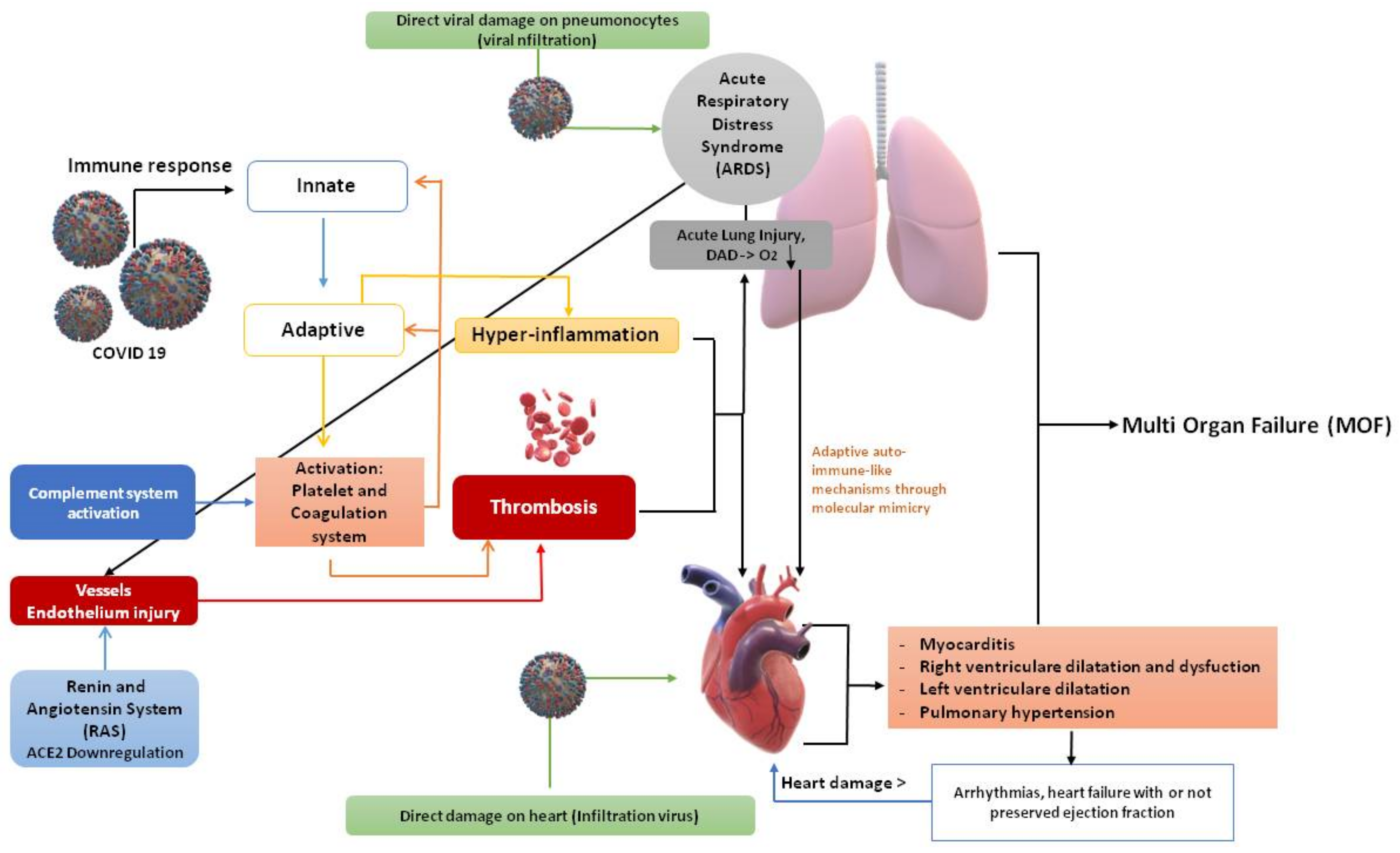
4.1. Biomolecular Hypotheses about COVID-19-Induced Myocardial Injury
- (a)
- Myocardial damage due to the direct viral action on the tissue, or to extrapulmonary migration of infected alveolar macrophages. Thus, a direct myocardial damage through binding to ACE2 receptors because of viral action on the tissue or due to extra pulmonary migration of infected alveolar macrophages. SARS-CoV-2 uses spike protein to bind to ACE2 receptors on the myocardial cell membrane. In theory, following SARS-CoV-2’s engagement to the ACE2 receptors on the myocardium and the subsequent down-regulation of the receptors themselves, the accumulation of angiotensin II may enhance myocardial remodeling by diverting all its activity to type 1 angiotensin II receptors (AT1R) of the heart [1,70,71]. Interestingly, a polybasic furin site that structurally differentiates SARS-CoV-2 from SARS, when cleaved, expands the types of cells the virus can infect. The virus, by binding to ACE2 receptors throughout the body, facilitates cell entry through its spike protein, together with the cooperation of the serine protease transmembrane protease serine 2, heparan sulfate, and other proteases. The heart is one of the many organs with high ACE2 expression [72,73,74,75]. Tropism to other organs besides the lungs was studied from autopsy samples: SARS-CoV-2 genomic RNA was highest in the lungs, but the heart, kidneys, and liver also showed substantial amounts, and copies of the virus were detected in the heart of 16 of the 22 patients who died. In an autopsy series of 39 patients who died from COVID-19, the virus was undetectable in the myocardium in 38% of patients, while 31% had a high viral load greater than 1000 copies in the heart [76,77].
- (b)
- Via cell-mediated cytotoxicity in which CD8 T lymphocytes migrate to cardiomyocytes and cause inflammation of the myocardium. Cytokine release syndrome, proposed as the main mechanism underlying COVID-19-induced acute fulminant myocarditis, is thus unleashed [1,9,10,11]. This triggers the pro-inflammatory cytokine release syndrome, a severe systemic inflammatory response resulting in hypoxia and apoptosis of the cardiomyocytes. In fact, the released cytokines increase the activation of T lymphocytes, which release further cytokines with consequent positive feedback of immune activation and myocardial damage [9].
- (c)
- The mechanism of hyperactivation of the autoimmune system with possible interferon-mediated hyperactivation of the innate and adaptive immune system has also been proposed [78]. Myocarditis can cause the onset of arrhythmias, during the acute phase, due to a direct cytopathic effect, which causes electrical imbalance and ischemia due to microvascular and gap-junctions dysfunction due to reduced myocardial expression of connexins [79]. Thus, the main biomolecular mechanism responsible for heart damage, and in turn heart failure, is an abnormal state of systemic inflammation with low oxygen levels and thrombosis. In addition, the presence of the SARS-CoV-2 genome was detected in the myocardium [54].
4.2. Cardiovascular Signs and Symptoms during the Infection
4.3. Main Laboratory Markers of Cardiovascular Severe Prognosis
4.4. Instrumental Diagnostics
4.5. Histological Findings of Myocarditis
4.6. Management and Treatment Strategies
4.7. Knowledge Gaps and Future Directions
4.8. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Santacroce, L.; Charitos, I.A.; Carretta, D.M.; De Nitto, E.; Lovero, R. The human coronaviruses (HCoVs) and the molecular mechanisms of SARS-CoV-2 infection. J. Mol. Med. 2021, 93–106. [Google Scholar] [CrossRef]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Santacroce, L.; Charitos, I.A.; Del Prete, R. COVID-19 in Italy: An Overview from the First Case to Date. Electron. J. Gen. Med. 2020, 17, em235. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus. Available online: https://www.who.int/health-topics/coronavirus (accessed on 1 December 2020).
- Li, S.; Li, S.; Disoma, C.; Zheng, R.; Zhou, M.; Razzaq, A.; Liu, P.; Zhou, Y.; Dong, Z.; Du, A.; et al. SARS-CoV-2: Mechanism of infection and emerging technologies for future prospects. Rev. Med. Virol. 2021, 31, e2168. [Google Scholar] [CrossRef]
- Charitos, I.A.; Ballini, A.; Bottalico, L.; Cantore, S.; Passarelli, P.C.; Inchingolo, F.; D’Addona, A.; Santacroce, L. Special features of SARS-CoV-2 in daily practice. World J. Clin. Cases 2020, 8, 3920–3933. [Google Scholar] [CrossRef] [PubMed]
- Wujtewicz, M.; Dylczyk-Sommer, A.; Aszkiełowicz, A.; Zdanowski, S.; Piwowarczyk, S.; Owczuk, R. COVID-19—What should anaethesiologists and intensivists know about it? Anaesthesiol. Intensive Ter. 2020, 52, 34–41. [Google Scholar] [CrossRef]
- Santacroce, L.; Bottalico, L.; Charitos, I.A. The Impact of COVID-19 on Italy: A Lesson for the Future. Int. J. Occup. Environ. Med. 2020, 11, 151–152. [Google Scholar] [CrossRef]
- Gralinski, L.E.; Baric, R.S. Molecular pathology of emerging coronavirus infections. J. Pathol. 2015, 235, 185–195. [Google Scholar] [CrossRef]
- Cazzolla, A.P.; Lovero, R.; Muzio, L.L.; Testa, N.F.; Schirinzi, A.; Palmieri, G.; Pozzessere, P.; Procacci, V.; Di Comite, M.; Ciavarella, D.; et al. Taste and Smell Disorders in COVID-19 Patients: Role of Interleukin-6. Acs Chem. Neurosci. 2020, 11, 2774–2781. [Google Scholar] [CrossRef]
- Fox, S.E.; Akmatbekov, A.; Harbert, J.L.; Li, G.; Brown, J.Q.; Heide, R.S.V. Pulmonary and Cardiac Pathology in Covid-19: The First Autopsy Series from New Orleans. medRxiv 2020. [Google Scholar] [CrossRef]
- Mohanty, S.K.; Satapathy, A.; Naidu, M.M.; Mukhopadhyay, S.; Sharma, S.; Barton, L.M.; Stroberg, E.; Duval, E.J.; Pradhan, D.; Tzankov, A.; et al. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19)—Anatomic pathology perspective on current knowledge. Diagn. Pathol. 2020, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- Atri, D.; Siddiqi, H.K.; Lang, J.; Nauffal, V.; Morrow, D.A.; Bohula, E.A. COVID-19 for the cardiologist: A current review of the virology, clinical epidemiology, cardiac and other clinical manifestations and potential therapeutic strategies. J. Am. Coll. Cardiol. Basic Transl. Sci. 2020, 5, 518–536. [Google Scholar] [CrossRef]
- Schirinzi, A.; Cazzolla, A.P.; Lovero, R.; Muzio, L.L.; Testa, N.F.; Ciavarella, D.; Palmieri, G.; Pozzessere, P.; Procacci, V.; Di Serio, F.; et al. New Insights in Laboratory Testing for COVID-19 Patients: Looking for the Role and Predictive Value of Human epididymis secretory protein 4 (HE4) and the Innate Immunity of the Oral Cavity and Respiratory Tract. Microorganisms 2020, 8, 1718. [Google Scholar] [CrossRef]
- Alhogbani, T. Acute myocarditis associated with novel Middle East respiratory syndrome coronavirus. Ann. Saudi Med. 2016, 36, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Babapoor-Farrokhran, S.; Gill, D.; Walker, J.; Rasekhi, R.T.; Bozorgnia, B.; Amanullah, A. Myocardial injury and COVID-19: Possible mechanisms. Life Sci. 2020, 253, 117723. [Google Scholar] [CrossRef]
- Asif, T.; Ali, Z. Transient ST Segment Elevation in Two Patients with COVID-19 and a Normal Transthoracic Echocardio-gram. Eur. J. Case Rep. Intern. Med. 2020, 7. [Google Scholar] [CrossRef]
- Beri, A.; Kotak, K. Cardiac injury, arrhythmia, and sudden death in a COVID-19 patient. HeartRhythm Case Rep. 2020, 6, 367–369. [Google Scholar] [CrossRef] [PubMed]
- Bernal-Torres, W.; Herrera-Escandón, Á.; Hurtado-Rivera, M.; Plata-Mosquera, C.A. COVID-19 fulminant myocarditis: A case report. Eur. Heart J. Case Rep. 2020, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Beşler, M.S.; Arslan, H. Acute myocarditis associated with COVID-19 infection. Am. J. Emerg. Med. 2020, 38, 2489.e1–2489.e2. [Google Scholar] [CrossRef]
- Cizgici, A.Y.; Agus, H.Z.; Yildiz, M. COVID-19 myopericarditis: It should be kept in mind in today’s conditions. Am. J. Emerg. Med. 2020, 38, 1547.e5–1547.e6. [Google Scholar] [CrossRef]
- Coyle, J.; Igbinomwanhia, E.; Sanchez-Nadales, A.; Danciu, S.; Chu, C.; Shah, N. A Recovered Case of COVID-19 Myocarditis and ARDS Treated With Corticosteroids, Tocilizumab, and Experimental AT-001. JACC Case Rep. 2020, 2, 1331–1336. [Google Scholar] [CrossRef]
- Craver, R.; Huber, S.; Sandomirsky, M.; McKenna, D.; Schieffelin, J.; Finger, L. Fatal Eosinophilic Myocarditis in a Healthy 17-Year-Old Male with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2c). Fetal Pediatr. Pathol. 2020, 39, 263–268. [Google Scholar] [CrossRef]
- Dolhnikoff, M.; Ferranti, J.F.; Monteiro, R.A.D.A.; Duarte-Neto, A.N.; Gomes-Gouvêa, M.S.; Degaspare, N.V.; Delgado, A.F.; Fiorita, C.M.; Leal, G.N.; Rodrigues, R.M.; et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet Child Adolesc. Health 2020, 4, 790–794, Erratum in 2020, 4, e39, doi:10.1016/s2352-4642(20)30257-1. [Google Scholar] [CrossRef]
- Doyen, D.; Moceri, P.; Ducreux, D.; Dellamonica, J. Myocarditis in a patient with COVID-19: A cause of raised troponin and ECG changes. Lancet 2020, 395, 1516. [Google Scholar] [CrossRef]
- Fried, J.A.; Ramasubbu, K.; Bhatt, R.; Topkara, V.K.; Clerkin, K.J.; Horn, E.; Rabbani, L.; Brodie, D.; Jain, S.S.; Kirtane, A.J.; et al. The Variety of Cardiovascular Presentations of COVID-19. Circulation 2020, 141, 1930–1936. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Ma, F.; Wei, X.; Fang, Y. Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin. Eur. Heart J. 2021, 42, 206. [Google Scholar] [CrossRef] [PubMed]
- Inciardi, R.M.; Lupi, L.; Zaccone, G.; Italia, L.; Raffo, M.; Tomasoni, D.; Cani, D.S.; Cerini, M.; Farina, D.; Gavazzi, E.; et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 819–824. [Google Scholar] [CrossRef]
- Irabien-Ortiz, Á.; Carreras-Mora, J.; Sionis, A.; Pàmies, J.; Montiel, J.; Tauron, M. Fulminant myocarditis due to COVID-19. Rev. Española Cardiol. (Engl. Ed.) 2020, 73, 503–504. [Google Scholar] [CrossRef]
- Jacobs, J.P.; Stammers, A.H.; Louis, J.S.; Hayanga, J.W.A.; Firstenberg, M.S.; Mongero, L.B.; Tesdahl, E.A.; Rajagopal, K.; Cheema, F.H.; Coley, T.; et al. Extracorporeal Membrane Oxygenation in the Treatment of Severe Pulmonary and Cardiac Compromise in Coronavirus Disease 2019: Experience with 32 Patients. ASAIO J. 2020, 66, 722–730. [Google Scholar] [CrossRef] [PubMed]
- Juusela, A.; Nazir, M.; Gimovsky, M. Two cases of coronavirus 2019—Related cardiomyopathy in pregnancy. Am. J. Obstet. Gynecol. MFM 2020, 2, 100113. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.-C.; Kim, J.Y.; Kim, H.A.; Han, S. COVID-19-related myocarditis in a 21-year-old female patient. Eur. Heart J. 2020, 41, 1859. [Google Scholar] [CrossRef]
- Luetkens, J.A.; Isaak, A.; Zimmer, S.; Nattermann, J.; Sprinkart, A.M.; Boesecke, C.; Rieke, G.J.; Zachoval, C.; Heine, A.; Velten, M.; et al. Diffuse Myocardial Inflammation in COVID-19 Associated Myocarditis Detected by Multiparametric Cardiac Magnetic Resonance Imaging. Circ. Cardiovasc. Imaging 2020, 13, e010897. [Google Scholar] [CrossRef]
- Naneishvili, T.; Khalil, A.; O’Leary, R.; Prasad, N. Fulminant myocarditis as an early presentation of SARS-CoV-2. BMJ Case Rep. 2020, 13, e237553. [Google Scholar] [CrossRef]
- Oberweis, M.-L.; Codreanu, A.; Boehm, W.; Olivier, D.; Pierron, C.; Tsobo, C.; Kohnen, M.; Abdelrahman, T.T.; Nguyen, N.T.; Wagner, K.; et al. Pediatric Life-Threatening Coronavirus Disease 2019 With Myocarditis. Pediatr. Infect. Dis. J. 2020, 39, e147–e149. [Google Scholar] [CrossRef] [PubMed]
- Oleszak, F.; Maryniak, A.; Botti, E.; Abrahim, C.; Salifu, M.O.; Youssef, M.; Henglein, V.L.; McFarlane, S.I. Myocarditis Associated With COVID-19. Am. J. Med. Case Rep. 2020, 8, 498–502. [Google Scholar] [CrossRef]
- Paul, J.-F.; Charles, P.; Richaud, C.; Caussin, C.; Diakov, C. Myocarditis revealing COVID-19 infection in a young patient. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 776. [Google Scholar] [CrossRef]
- Pavon, A.G.; Meier, D.; Samim, D.; Rotzinger, D.C.; Fournier, S.; Marquis, P.; Monney, P.; Muller, O.; Schwitter, J. First Documentation of Persistent SARS-Cov-2 Infection Presenting With Late Acute Severe Myocarditis. Can. J. Cardiol. 2020, 36, 1326.e5–1326.e7. [Google Scholar] [CrossRef] [PubMed]
- Radbel, J.; Narayanan, N.; Bhatt, P.J. Use of Tocilizumab for COVID-19-Induced Cytokine Release Syndrome. Chest 2020, 158, e15–e19. [Google Scholar] [CrossRef] [PubMed]
- Rauf, A.; Vijayan, A.; John, S.T.; Krishnan, R.; Latheef, A. Multisystem Inflammatory Syndrome with Features of Atypical Kawasaki Disease during COVID-19 Pandemic. Indian J. Pediatr. 2020, 87, 745–747. [Google Scholar] [CrossRef]
- Sala, S.; Peretto, G.; Gramegna, M.; Palmisano, A.; Villatore, A.; Vignale, D. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur. Heart J. 2020, 41, 1861–1862. [Google Scholar] [CrossRef]
- Sardari, A.; Tabarsi, P.; Borhany, H.; Mohiaddin, R.; Houshmand, G. Myocarditis detected after COVID-19 recovery. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 131–132. [Google Scholar] [CrossRef]
- Tavazzi, G.; Pellegrini, C.; Maurelli, M.; Belliato, M.; Sciutti, F.; Bottazzi, A.; Sepe, P.A.; Resasco, T.; Camporotondo, R.; Bruno, R.; et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur. J. Heart Fail. 2020, 22, 911–915. [Google Scholar] [CrossRef]
- Trogen, B.; Gonzalez, F.J.; Shust, G.F. COVID-19-Associated Myocarditis in an Adolescent. Pediatr. Infect. Dis. J. 2020, 39, e204–e205. [Google Scholar] [CrossRef] [PubMed]
- Warchoł, I.; Dębska-Kozłowska, A.; Karcz-Socha, I.; Książczyk, M.; Szymańska, K.; Lubiński, A. Terra incognita: Clinically suspected myocarditis in a patient with severe acute respiratory syndrome coronavirus 2 infection. Pol. Arch. Intern. Med. 2020. [Google Scholar] [CrossRef]
- Yuan, W.; Tang, X.; Zhao, X. An ‘asymptomatic’ driver with COVID-19: Atypical suspected myocarditis by SARS-CoV-2. Cardiovasc. Diagn. Ther. 2020, 10, 242–243. [Google Scholar] [CrossRef]
- Zeng, J.-H.; Liu, Y.-X.; Yuan, J.; Wang, F.-X.; Wu, W.-B.; Li, J.-X.; Wang, L.-F.; Gao, H.; Wang, Y.; Dong, C.-F.; et al. First case of COVID-19 complicated with fulminant myocarditis: A case report and insights. Infection 2020, 48, 773–777. [Google Scholar] [CrossRef]
- Beaudry, J.T.; Dietrick, B.; Lammert, D.B.; Constas, A.; McCaw, J.; Hammond, J.; Buendia, M.; Stein, J.E.; Pekosz, A.; Schuette, J.; et al. Fatal SARS-CoV-2 Inflammatory Syndrome and Myocarditis in an Adolescent: A Case Report. Pediatr. Infect. Dis. J. 2021, 40, e72–e76. [Google Scholar] [CrossRef]
- Cairns, L.; El Khaleq, Y.A.; Storrar, W.; Scheuermann-Freestone, M. COVID-19 myopericarditis with cardiac tamponade in the absence of respiratory symptoms: A case report. J. Med. Case Rep. 2021, 15, 31. [Google Scholar] [CrossRef] [PubMed]
- Garot, J.; Amour, J.; Pezel, T.; Dermoch, F.; Messadaa, K.; Felten, M.-L.; Raymond, V.; Baubillier, E.; Sanguineti, F.; Garot, P. SARS-CoV-2 Fulminant Myocarditis. JACC Case Rep. 2020, 2, 1342–1346. [Google Scholar] [CrossRef] [PubMed]
- Buja, L.M.; Wolf, D.A.; Zhao, B.; Akkanti, B.; McDonald, M.; Lelenwa, L.; Reilly, N.; Ottaviani, G.; Elghetany, M.T.; Trujillo, D.O.; et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): Report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc. Pathol. 2020, 48, 107233. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhou, Y.; Wang, D.W. SARS-CoV-2: A potential novel etiology of fulminant myocarditis. Herz 2020, 45, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Liu, W.; Liu, K.; Fang, Y.-Y.; Shang, J.; Zhou, L.; Wang, K.; Leng, F.; Wei, P.-F.; Chen, L.; et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: A retrospective study. Chin. Med. J. 2020, 133, 1261–1267. [Google Scholar] [CrossRef] [PubMed]
- Escher, F.; Pietsch, H.; Aleshcheva, G.; Bock, T.; Baumeier, C.; Elsaesser, A.; Wenzel, P.; Hamm, C.; Westenfeld, R.; Schultheiss, M.; et al. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Heart Fail. 2020, 7, 2440–2447. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Halushka, M.K.; Heide, R.S.V. Myocarditis is rare in COVID-19 autopsies: Cardiovascular findings across 277 postmortem examinations. Cardiovasc. Pathol. 2021, 50, 107300. [Google Scholar] [CrossRef]
- Han, H.; Xie, L.; Liu, R.; Yang, J.; Liu, F.; Wu, K.; Chen, L.; Hou, W.; Feng, Y.; Zhu, C. Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China. J. Med. Virol. 2020, 92, 819–823. [Google Scholar] [CrossRef]
- Sawalha, K.; Abozenah, M.; Kadado, A.J.; Battisha, A.; Al-Akchar, M.; Salerno, C.; Hernandez-Montfort, J.; Islam, A.M. Systematic Review of COVID-19 Related Myocarditis: Insights on Management and Outcome. Cardiovasc. Revasc. Med. 2021, 23, 107–113. [Google Scholar] [CrossRef]
- Duarte-Neto, A.N.; Monteiro, R.A.D.A.; Da Silva, L.F.F.; Malheiros, D.M.A.C.; De Oliveira, E.P.; Theodoro-Filho, J.; Pinho, J.R.R.; Gomes-Gouvêa, M.S.; Salles, A.P.M.; De Oliveira, I.R.S.; et al. Pulmonary and systemic involvement in COVID-19 patients assessed with ultrasound-guided minimally invasive autopsy. Histopathology 2020, 77, 186–197. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265. [Google Scholar] [CrossRef]
- Rajpal, S.; Tong, M.S.; Borchers, J.; Zareba, K.M.; Obarski, T.P.; Simonetti, O.P.; Daniels, C.J. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol. 2021, 116–118. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Hu, J.; Zhu, C. Obesity aggravates COVID-19: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 257–261. [Google Scholar] [CrossRef]
- Azarkish, M.; Laleh Far, V.; Eslami, M.; Mollazadeh, R. Transient complete heart block in a patient with critical COVID-19. Eur. Heart J. 2020, 41, 2131. [Google Scholar] [CrossRef] [PubMed]
- Baldi, E.; Sechi, G.M.; Mare, C.; Canevari, F.; Brancaglione, A.; Primi, R.; Klersy, C.; Palo, A.; Contri, E.; Ronchi, V.; et al. Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy. N. Engl. J. Med. 2020, 383, 496–498. [Google Scholar] [CrossRef]
- Santacroce, L.; D’agostino, D.; Charitos, I.A.; Bottalico, L.; Ballini, A. A short review about electrophysiology and bi-oimpedance: History and perspectives. Indian J. Public Health Res. Dev. 2018, 9, 577–591. [Google Scholar] [CrossRef]
- Bhatla, A.; Mayer, M.M.; Adusumalli, S.; Hyman, M.C.; Oh, E.; Tierney, A.; Moss, J.; Chahal, A.A.; Anesi, G.; Denduluri, S.; et al. COVID-19 and cardiac arrhythmias. Hear. Rhythm. 2020, 17, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, A.S.; Cleland, J.G.F.; Katus, H.A. Myocardial injury in severe COVID-19 infection. Eur. Heart J. 2020, 41, 2080–2082. [Google Scholar] [CrossRef]
- Albert, C.L.; Carmona-Rubio, A.E.; Weiss, A.J.; Procop, G.G.; Starling, R.C.; Rodriguez, E.R. The Enemy Within: Sudden-Onset Reversible Cardiogenic Shock With Biopsy-Proven Cardiac Myocyte Infection by Severe Acute Respiratory Syndrome Coronavirus 2. Circulation 2020, 142, 1865–1870. [Google Scholar] [CrossRef]
- Ranard, L.S.; Fried, J.A.; Abdalla, M.; Anstey, D.E.; Givens, R.C.; Kumaraiah, D.; Kodali, S.K.; Takeda, K.; Karmpaliotis, D.; Rabbani, L.E.; et al. Approach to Acute Cardiovascular Complications in COVID-19 Infection. Circ Heart Fail. 2020, 13, e007220. [Google Scholar] [CrossRef]
- Nicin, L.; Abplanalp, W.T.; Mellentin, H.; Kattih, B.; Tombor, L.; John, D.; Schmitto, J.D.; Heineke, J.; Emrich, F.; Arsalan, M.; et al. Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts. Eur. Heart J. 2020, 41, 1804–1806. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Clerkin, K.J.; Fried, J.A.; Raikhelkar, J.; Sayer, G.; Griffin, J.M.; Masoumi, A. COVID-19 and cardiovascular disease. Circulation 2020, 141, 1648–1655. [Google Scholar] [CrossRef] [PubMed]
- Colon, C.M.; Barrios, J.G.; Chiles, J.W.; McElwee, S.K.; Russell, D.W.; Maddox, W.R.; Kay, G.N. Atrial Arrhythmias in COVID-19 Patients. JACC Clin. Electrophysiol. 2020, 6, 1189–1190. [Google Scholar] [CrossRef] [PubMed]
- Fox, S.E.; Akmatbekov, A.; Harbert, J.L.; Li, G.; Brown, J.Q.; Heide, R.S.V. Pulmonary and cardiac pathology in African American patients with COVID-19: An autopsy series from New Orleans. Lancet Respir. Med. 2020, 8, 681–686. [Google Scholar] [CrossRef]
- Lindner, D.; Fitzek, A.; Bräuninger, H.; Aleshcheva, G.; Edler, C.; Meissner, K.; Scherschel, K.; Kirchhof, P.; Escher, F.; Schultheiss, H.-P.; et al. Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. JAMA Cardiol. 2020, 5, 1281. [Google Scholar] [CrossRef] [PubMed]
- McMurray, J.C.; May, J.W.; Cunningham, M.W.; Jones, O.Y. Multisystem Inflammatory Syndrome in Children (MIS-C), a Post-viral Myocarditis and Systemic Vasculitis-A Critical Review of Its Pathogenesis and Treatment. Front. Pediatr. 2020, 8, 626182. [Google Scholar] [CrossRef]
- Babapoor-Farrokhran, S.; Rasekhi, R.T.; Gill, D.; Babapoor, S.; Amanullah, A. Arrhythmia in COVID-19. SN Compr. Clin. Med. 2020, 2, 1430–1435. [Google Scholar] [CrossRef]
- Lazzerini, P.E.; Boutjdir, M.; Capecchi, P.L. COVID-19, Arrhythmic Risk, and Inflammation: Mind the Gap! Circulation 2020, 142, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Buja, L.M.; Stone, J.R. A novel coronavirus meets the cardiovascular system: Society for Cardiovascular Pathology Symposium 2021. Cardiovasc. Pathol. 2021, 53, 107336. [Google Scholar] [CrossRef] [PubMed]
- Barber, C. COVID-19 Can Wreck Your Heart, Even if You Haven’t Had Any Symptoms. Sci. Am. 2020. Available online: https://www.scientificamerican.com/article/covid-19-can-wreck-your-heart-even-if-you-havent-had-any-symptoms/ (accessed on 15 May 2021).
- Santacroce, L.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Luperto, P.; De Nitto, E.; Topi, S. The Human Respiratory System and its Microbiome at a Glimpse. Biology 2020, 9, 318. [Google Scholar] [CrossRef] [PubMed]
- Djomkam, A.L.Z.; Olwal, C.O.; Sala, T.B.; Paemka, L. Commentary: SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Front. Oncol. 2020, 10, 1448. [Google Scholar] [CrossRef] [PubMed]
- Blauwet, L.A.; Cooper, L.T. Myocarditis. Prog. Cardiovasc. Dis. 2010, 52, 274–288. [Google Scholar] [CrossRef]
- Rubini, G.; Ferrari, C.; Carretta, D.; Santacroce, L.; Ruta, R.; Iuele, F.; Lavelli, V.; Merenda, N.; D’Agostino, C.; Sardaro, A.; et al. Usefulness of 18F-FDG PET/CT in Patients with Cardiac Implantable Electronic Device Suspected of Late Infection. J. Clin. Med. 2020, 9, 2246. [Google Scholar] [CrossRef] [PubMed]
- Birchak, J.; Khan, A.; Singh, G.; Schuger, C.; Maskoun, W. An unusual case of sustained ventricular tachycardia from acute pulmonary embolism. J. Am. Coll. Cardiol. 2020, 75, 2820. [Google Scholar] [CrossRef]
- Biesbroek, P.S.; Beek, A.M.; Germans, T.; Niessen, H.W.; van Rossum, A.C. Diagnosis of myocarditis: Current state and future perspectives. Int. J. Cardiol. 2015, 191, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Channappanavar, R.; Zhao, J.; Perlman, S. T cell-mediated immune response to respiratory coronaviruses. Immunol. Res. 2014, 59, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Gnoni, A.; Ballini, A.; Trentadue, R.; Taurino, F.; Santacroce, L.; Ferrara, P.; Massaro, F.; Brienza, N.; Massari, A.M.; Sardaro, N.; et al. Induction of mitochondrial dysfunction in patients under cardiopulmonary by-pass: Preliminary results. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 8115–8123. [Google Scholar]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef]
- Yang, C.; Jin, Z. An Acute Respiratory Infection Runs Into the Most Common Noncommunicable Epidemic-COVID-19 and Cardiovascular Diseases. JAMA Cardiol. 2020, 5, 743–744. [Google Scholar] [CrossRef]
- Roshdy, A.; Zaher, S.; Fayed, H.; Coghlan, J.G. COVID-19 and the Heart: A Systematic Review of Cardiac Autopsies. Front Cardiovasc. Med. 2021, 7, 626975. [Google Scholar] [CrossRef]
- Goyal, P.; Choi, J.J.; Pinheiro, L.C.; Schenck, E.J.; Chen, R.; Jabri, A.; Satlin, M.J.; Campion, T.R.; Nahid, M.; Ringel, J.B.; et al. Clinical Characteristics of Covid-19 in New York City. N. Engl. J. Med. 2020, 382, 2372–2374. [Google Scholar] [CrossRef]
- Dabbagh, M.F.; Aurora, L.; D’Souza, P.; Weinmann, A.J.; Bhargava, P.; Basir, M.B. Cardiac Tamponade Secondary to COVID-JACC. Case Rep. 2020, 2, 1326–1330. [Google Scholar] [CrossRef]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef]
- Thakkar, S.; Arora, S.; Kumar, A.; Jaswaney, R.; Faisaluddin, M.; Ammad Ud Din, M.; Shariff, M.; Barssoum, K.; Patel, H.P.; Nirav, A.; et al. A Systematic Review of the Cardiovascular Manifestations and Outcomes in the Setting of Coronavirus-19 Disease. Clin. Med. Insights Cardiol. 2020, 14, 1179546820977196. [Google Scholar] [CrossRef] [PubMed]
- Lakkireddy, D.R.; Chung, M.K.; Gopinathannair, R.; Patton, K.K.; Gluckman, T.J.; Turagam, M.; Cheung, J.W.; Patel, P.; Sotomonte, J.; Lampert, R.; et al. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Heart Rhythm. 2020, 17, e233–e241. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, M.S.; Heikkilä, J.; Karjalainen, J. Echocardiography in acute infectious myocarditis: Relation to clinical and electrocardiographic findings. Am. J. Cardiol. 1984, 53, 1331–1337. [Google Scholar] [CrossRef]
- Felker, G.M.; Boehmer, J.P.; Hruban, R.H.; Hutchins, G.M.; Kasper, E.K.; Baughman, K.L. Echocardiographic findings in fulminant and acute myocarditis. J. Am. Coll. Cardiol. 2000, 36, 227–232. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef] [PubMed]
- Fung, G.; Luo, H.; Qiu, Y.; Yang, D.; McManus, B. Myocarditis. Circ. Res. 2016, 118, 496–514. [Google Scholar] [CrossRef]
- Chen, H.S.; Wang, W.; Wu, S.N.; Liu, J.P. Corticosteroids for viral myocarditis. Cochrane Database Syst. Rev. 2013, 2013, CD004471. [Google Scholar] [CrossRef] [PubMed]
- Verhoef, P.A.; Kannan, S.; Sturgill, J.L.; Tucker, E.W.; Morris, P.E.; Miller, A.C.; Sexton, T.R.; Koyner, J.L.; Hejal, R.; Brakenridge, S.C.; et al. Severe Acute Respiratory Syndrome-Associated Coronavirus 2 Infection and Organ Dysfunction in the ICU: Opportunities for Translational Research. Crit. Care Explor. 2021, 3, e0374. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef]
- Hasan, S.S.; Capstick, T.; Ahmed, R.; Kow, C.S.; Mazhar, F.; Merchant, H.A.; Zaidi, S.T.R. Mortality in COVID-19 patients with acute respiratory distress syndrome and corticosteroids use: A systematic review and meta-analysis. Expert Rev. Respir. Med. 2020, 14, 1149–1163. [Google Scholar] [CrossRef]
- Lythgoe, M.P.; Middleton, P. Ongoing Clinical Trials for the Management of the COVID-19 Pandemic. Trends Pharmacol. Sci. 2020, 41, 363–382. [Google Scholar] [CrossRef]
- Kow, C.S.; Hasan, S.S. Glucocorticoid versus immunoglobulin in the treatment of COVID-19-associated fulminant myocarditis. Infection 2020, 48, 805–806. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yu, Y.; Chen, S.; Liao, Y.; Du, J. Corticosteroids and Intravenous Immunoglobulin in Pediatric Myocarditis: A Meta-Analysis. Front. Pediatr. 2019, 7, 342. [Google Scholar] [CrossRef]
- Jin, Y.-H.; Cai, L.; Cheng, Z.-S.; Cheng, H.; Deng, T.; Fan, Y.-P.; Fang, C.; Huang, D.; Huang, L.-Q.; Huang, Q.; et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil. Med. Res. 2020, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Farooqi, F.; Dhawan, N.; Morgan, R.; Dinh, J.; Nedd, K.; Yatzkan, G. Treatment of Severe COVID-19 with Tocilizumab Mitigates Cytokine Storm and Averts Mechanical Ventilation During Acute Respiratory Distress: A Case Report and Literature Review. Trop. Med. Infect. Dis. 2020, 5, 112. [Google Scholar] [CrossRef] [PubMed]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; Mehta, A.K.; Zingman, B.S.; Kalil, A.C.; Hohmann, E.; Chu, H.Y.; Luetkemeyer, A.; Kline, S.; et al. Remdesivir for the Treatment of Covid-19—Final Report. N. Engl. J. Med. 2020, 383, 1813–1826. [Google Scholar] [CrossRef]
- Castiglione, V.; Chiriacò, M.; Emdin, M.; Taddei, S.; Vergaro, G. Statin therapy in COVID-19 infection. Eur. Heart J. Cardiovasc. Pharmacol. 2020, 6, 258–259. [Google Scholar] [CrossRef]
- European Society of Cardiology Working Group on Myocardial and Pericardial Diseases guidelines. Available online: https://www.escardio.org/Guidelines (accessed on 1 December 2020).
- Fiore, A.; Piscitelli, M.; Adodo, D.K.; Thomas, C.; Dessap, A.M.; Bagate, F.; Folliguet, T. Successful Use of Extracorporeal Membrane Oxygenation Postpartum as Rescue Therapy in a Woman With COVID-19. J. Cardiothorac. Vasc. Anesth. 2020, 35, 2140–2143. [Google Scholar] [CrossRef] [PubMed]
- Alom, S.; Haiduc, A.A.; Melamed, N.; Axiaq, A.; Harky, A. Use of ECMO in Patients With Coronavirus Disease 2019: Does the Evidence Suffice? J. Cardiothorac. Vasc. Anesth. 2021, 35, 1256–1262. [Google Scholar] [CrossRef]
- Charitos, I.A.; Topi, S.; Castellaneta, F.; D’Agostino, D. Current Issues and Perspectives in Patients with Possible Sepsis at Emergency Departments. Antibiotics 2019, 8, 56. [Google Scholar] [CrossRef]
- Siripanthong, B.; Nazarian, S.; Muser, D.; Deo, R.; Santangeli, P.; Khanji, M.Y.; Cooper, L.T.; Chahal, C.A.A. Recognizing COVID-19–related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020, 17, 1463–1471. [Google Scholar] [CrossRef]
- Topol, E.J. COVID-19 can affect the heart. Science 2020, 370, 408–409. [Google Scholar] [CrossRef]
- Bonow, R.O.; Yancy, C.W. Explanation for the Corrections for the Study of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019. JAMA Cardiol. 2020, 5, 1308. [Google Scholar] [CrossRef]
- Ho, J.S.; Sia, C.H.; Chan, M.Y.; Lin, W.; Wong, R.C. Coronavirus-induced myocarditis: A meta-summary of cases. Heart Lung 2020, 49, 681–685. [Google Scholar] [CrossRef]
- Salman, D.; Vishnubala, D.; Le Feuvre, P.; Beaney, T.; Korgaonkar, J.; Majeed, A.; McGregor, A.H. Returning to physical activity after covid-19. BMJ 2021, 372, m4721. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC), USA. Post-COVID 19 Conditions. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html (accessed on 20 May 2021).

| Authors | Study Design | Sample of Study | Presenting Symptoms | Cardiac Biomarker | Results | Treatment |
|---|---|---|---|---|---|---|
| Asif and Ali [17] | Case report | 64-year-old man | Dyspnea | Troponin: 0.17 ng/mL NT-proBNP: - | ECG: T Echo: - CMR: NR EMB/PM:NR | Aspirin, clopidogrel, heparin, azithromycin, hydroxychloroquine, meropenem, propofol, fentanyl, atracurium, vasopressin, tocilizumab |
| Asif and Ali [17] | Case report | 71-year-old man | Fever, cough, and dyspnea | Troponin: 1.6 ng/mL NT-proBNP: - | ECG: ST, Q Echo: - CMR: NR EMB/PM:NR | Aspirin, clopidogrel, heparin, azithromycin, cefepime, vancomycin, tocilizumab, fentanyl, midazolam |
| Beri et al. [18] | Case report | 72-year old man | Chest tightness, shortness of breath, cough, fatigue, and intermittent diarrhea | Troponin: - NT-proBNP: - | ECG: ST, TV Echo: ventricular dysfunction, cardiomegaly CMR: NR EMB/PM: NR | NR |
| Bernal-Torres et al. [19] | Case report | 38-year-old woman | Palpitations, general malaise | Troponin: 1190 ng/mL NT-proBNP: 13,000 pg/mL | ECG: ST Echo: LVEF 30%, hypokinesia CMR: Edema+ Injury+ EMB/PM: NR | Methylprednisolone, immunoglobulin, hydroxychloroquine, azithromycin, lopinavir/ritonavir |
| Beşler and Arslan [20] | Case report | 20-year-old man | Febrile sensation and chest pain | Troponin: 0.572 ng/mL NT-proBNP: 127 pg/L | ECG: - Echo: - CMR: Edema+ Injury+ EMB/PM:NR | Hydroxychloroquine, azithromycin, ceftriaxone, tigecycline, favipiravir, colchicine |
| Cizgici et al. [21] | Case report | 78-year-old man | Chest pain and shortness of breath. | Troponin: 998.1 ng/mL NT-proBNP: 127 pg/mL | ECG: FA, ST Echo: - CMR: Edema+ Injury+ EMB/PM:NR | Furosemide, ACE-I, beta-blocker, COVID-19-specific therapy |
| Coyle et al. [22] | Case report | 57-year-old man | Shortness of breath, fevers, cough, myalgia, decreased appetite, nausea, and diarrhea | Troponin: 7.33 ng/mL NT-proBNP: 1300 pg/mL | ECG: - Echo: Hypokinesia, LVEF 35–40% CMR: Edema+ Injury+ EMB/PM:NR | Hydroxychloroquine, methylprednisolone, azithromycin, ceftriaxone, colchicine |
| Craver et al. [23] | Case report | 17-year-old man | Full cardiac arrest after a 2-day history of headache, dizziness, nausea, and vomiting | NR | ECG: NR Echo: NR CMR: NR EMB/PM: Immune cell infiltrate, necrosis | NR |
| Dolhnikoff et al. [24] | Case report | 11-year-old boy | Fever, odynophagia, myalgia, and abdominal pain | Troponin: 0.342 ng/mL NT-proBNP: - | ECG: TV Echo: LVEF 31%, hypokinesia CMR: Edema+ Injury+ EMB/PM: viral particles in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells | Epinephrine, furosemide, ceftriaxone, azithromycin |
| Doyen et al. [25] | Case report | 69-year-old man | Cough, fever, dyspnea | Troponin: 9002 ng/mL NT-proBNP: 22.600 pg/mL | ECG: T Echo: LVH CMR: Edema+ Injury+ EMB/PM: NR | Hydrocortisone, aspirin, fondaparinux |
| Fried et al. [26] | Case report | 64-year-old woman | Chest pressure | Troponin: 18,6 ng/mL NT-proBNP: - | ECG: Sinusal tachy, ST Echo: LVEF 30%, pericardial effusion CMR: NR EMB/PM: NR | Hydroxychloroquine, dobutamine, IABP |
| Hu et al. [27] | Case report | 37-year-old man | Chest pain, dyspnea, and diarrhea | Troponin: 10,000 ng/mL NT-proBNP: 2102 pg/mL | ECG: ST Echo: LVD, LVEF 27% CMR: NR EMB/PM:NR | Methylprednisolone, immunoglobulin, norepinephrine, diuretic, milrinone, pantoprazole, piperacillin/sulbactam |
| Inciardi et al. [28] | Case report | 53-year-old woman | Fever and cough | Troponin: 0,24 ng/mL NT-proBNP: 5647 pg/mL | ECG: ST, T Echo: Hypokinesia, LVEF 40%, pericardial effusion CMR: Edema+ Injury+ EMB/PM: NR | Hydroxychloroquine, lopinavir/ritonavir, methylprednisolone, bisoprolol, kanrenone, furosemide |
| Irabien- Ortiz et al. [29] | Case report | 59-year-old woman | Anginal chest pain in the absence of respiratory symptoms | Troponin: 1100 ng/mL NT-proBNP: 4421 pg/mL | ECG: ST Echo: LVH CMR: Edema+ Injury+ EMB/PM:NR | Immunoglobulins, methylprednisolone, ritonavir/lopinavir, interferon-B |
| Jacobs et al. [30] | Case report | 48-year-old man | Fever, diarrhoea, cough, dysosmia, and dyspnea | Troponin: 14 932 ng/mL NT-proBNP: 9223 pg/mL | ECG: T Echo: LVH, hyperdynamic ventricular function CMR: NR EMB/PM: Immune cell infiltrate, edema, necrosis | Hydroxychloroquine, azithromycin, ECMO |
| Juusela et al. [31] | Case report | 45-year-old woman, pregnant (39 weeks) | Contractions and emesis | Troponin: 0.046 ng/mL NT-proBNP: 114 pg/mL | ECG: - Echo: LVEF 40% CMR: NR EMB/PM:NR | Methylprednisolone, hydroxychloroquine, tocilizumab, cesarean |
| Juusela et al. [31] | Case report | 26-year-old woman, pregnant (33 weeks) | Shortness of breath, dyspnea, | Troponin: 0.046 ng/mL NT-proBNP: <10 pg/mL | ECG: VT Echo: Hypokinesia, LVEF 40% CMR: - EMB/PM:NR | Metoprolol, cesarean |
| Kim et al. [32] | Case report | 21-year-old woman | Coughing, sputum, diarrhea, and shortness of breath | Troponin: 1.26 ng/mL NT-proBNP: 1929 pg/mL | ECG: VE Echo: Severe LV systolic dysfunction CMR: Edema+ Injury+ EMB/PM: NR | NR |
| Luetkens et al. [33] | Case report | 79-year-old man | Fatigue, shortness of breath, recurrent syncopes | Troponin: 63,5 ng/mL NT-proBNP: 1178 pg/mL | ECG: - Echo: Hypokinesia, LVEF 49% CMR: Edema+ Injury+ EMB/PM: NR | NR |
| Naneishvili et al. [34] | Case report | 44-year-old woman | Fever, lethargy, muscle aches and two episodes of syncope | Troponin: 639 ng/mL NT-proBNP: - | ECG: FA Echo: LVEF 37%, LVH, pericardial effusion CMR: NR EMB/PM: NR | Methylprednisolone, remdesvir, amiodarone, milrinone, inotropic support |
| Oberweis et al. [35] | Case report | 8-year-old male | Fever, coughing, weight loss, and severe fatigue | Troponin: 0.044 ng/mL NT-proBNP: 5112 pg/mL | ECG: ST Echo: LVEF 21%, pericardial effusion CMR: Edema+ Injury+ EMB/PM: NR | Heparin, dobutamine, immunoglobulins, milrinone, tocilizumab |
| Oleszak et al. [36] | Case report | 52-year-old man | Cough, fever, shortness of breath, and a single episode of trace hemoptysis | Troponin: 0.017 ng/mL NT-proBNP: 1220 pg/mL | ECG: Sinusal tachy Echo: LVEF 25%, LVH CMR: NR EMB/PM: NR | Ceftriaxone, azithromycin, hydroxychloroquine, furosemide |
| Paul et al. [37] | Case report | 35-year-old man | Chest pain and fatigue | Troponin: 2885 ng/mL NT-proBNP: - | ECG: repolarization changes Echo: - CMR: Edema+ Injury+ EMB/PM:NR | Ramipril, bisoprolol |
| Pavon et al. [38] | Case report | 64-year-old man | Chest pain and dyspnea | Troponin: 1843 ng/L NT-proBNP: - | ECG: - Echo: LVEF 40% CMR: Edema+ Injury+ EMB/PM: NR | Piperacillin/tazobactam |
| Radbel et al. [39] | Case report | 40-year-old man | Fever, dry cough, and dyspnea | Troponin: 30,39 ng/mL NT-proBNP: - | ECG: ST Echo: hypokinesia CMR: NR EMB/PM: NR | Hydroxychloroquine, azithromycin, tocilizumab |
| Rauf et al. [40] | Case report | 5-year-old boy | Fever, abdominal pain and loose stools, bulbar conjunctivitis, and extremity edema | Troponin: 29 ng/mL NT-proBNP: 8000 pg/mL | ECG: - Echo: LVEF 35%, hypokinesia CMR: NR EMB/PM: NR | Inotropic support, immunoglobulins, aspirin, steroids, diuretics |
| Sala et al. [41] | Case report | 43-year-old woman | Chest pain and dyspnea | Troponin: 106 ng/mL NT-proBNP: 512 pg/mL | ECG: ST Echo: Hypokinesia, LVEF 43% CMR: Edema+ Injury+ EMB/PM: Immune cell infiltrate, edema, necrosis | Lopinavir/ritonavir, hydroxychloroquine |
| Sardari et al. [42] | Case report | 31-year-old man | Dyspnea on exertion and low-grade fever | Troponin: <0.03 ng/mL NT-proBNP: - | ECG: - Echo: Mild LV systolic dysfunction CMR: Edema+ Injury+ EMB/PM:NR | Bisoprolol, lisinopril |
| Tavazzi et al. [43] | Case report | 69-year-old woman | Dyspnea, cough, and weakness | Troponin: 4332 ng/mL NT-proBNP: - | ECG: - Echo: LVD, LVEF 27% CMR: NR EMB/PM: viral particles within the interstitial cells of the myocardium, edema, necrosis | IABP, ECMO |
| Trogen et al. [44] | Case report | 17-year-old man | Fever and neck pain, diarrhea | Troponin: 2.97 ng/mL NT-proBNP: 2124 pg/mL | ECG: T Echo: LVEF 40% CMR: Edema+ Injury+ EMB/PM: NR | Hydroxychloroquine, piperacillin-tazobactam, enoxaparin |
| Warchoł et al. [45] | Case report | 74-year-old man | Palpitations, general malaise | Troponin: 102 ng/mL NT-proBNP: 2451 pg/mL | ECG: VT Echo: LVEF 25% CMR: Edema - Injury+ EMB/PM: NR | Metoprolol, amiodarone |
| Yuan et al. [46] | Case report | 33-year-old man | Chest pain, fever, and muscle ache | Troponin: - NT-proBNP: - | ECG: - Echo: VT CMR: Edema+ Injury- EMB/PM:NR | NR |
| Zeng et al. [47] | Case report | 63-year-old man | Shortness of breath and chest tightness after activity | Troponin: 11.37 g/L NT-proBNP: 22.600 pg/mL | ECG: Sinusal tachy Echo: dyskinesia, LVD, LVEF 32% CMR: NR EMB/PM: NR | High-flow oxygen, CCRTlopinavir-ritonavir, interferon α-1b, methylprednisolone, immunoglobulin, piperacillin-tazobactam |
| Cairns et al. [48] | Case report | 58-year-old female | Developed cardiogenic shock after fever, diarrhoea, and vomiting | Troponin 3532.9 ng/L NT-proBNP: NR | ECG: NR Echo: TTE showed 3–4 cm pericardial effusion with evidence of cardiac tamponade CMR: NR EMB/PM: NR | Pericardial drain, vasopressor support, intravenous amoxicillin, oral doxycycline initially, escalated to piperacillin/tazobactam, furosemide, intravenous immunoglobulin (2 g/kg) |
| Beaudry et al. [49] | 15-year-old female | Epigastric pain, nasal congestion, and rhinorrhea. Pyrexia (38.9°C), tachycardia, and worsening respiratory failure | Troponin 2.48 ng/mL NT-proBNP: 8328 pg/mL | ECG: sinus tachycardia Echo: severely diminished LV ejection CMR: NR EMB/PM: cardiomyocytes with interstitial lymphoplasmacytic infiltrate and mixed inflammation surrounding cardiac vessels | Mechanical ventilation (intensive care unit), norepinephrine infusion cefepime, metronidazole, doxycycline | |
| Garot J et al. [50] | 69-year-old man | Fever, asthenia, and abdominal pain, hypotension, hypoxemia, anuria, and multi-organ failure (MOF) | Troponin 8066 pg/mL NT-proBNP: NR | ECG: no signs of ischemia Echo: non-dilated and severe, diffuse LV hypokinesia (LV ejection fraction: 30%) CMR: NR EMB/PM: Abundant myocardial edema, interstitial inflammation (predominance of mononucleated leucocytes) associated with cardiomyocytes dystrophies and strong granular cytoplasmic staining of cardiomyocytes for SARS coronavirus nucleocapsid protein | Veno-arterial unit and extracorporeal membrane oxygenation (VA-ECMO), noradrenalin, dobutamine |
| Authors | Study Design | Sample of Study | Results | Treatment | Conclusion |
|---|---|---|---|---|---|
| Buja et al. [51] | Case series | 23 | Lymphocytic myocarditis, lymphocytic pericarditis, multifocal acute injury of cardiomyocytes without inflammatory cellular infiltrates | N/A | COVID-19 is a systemic disease with major involvement of the lungs and heart. |
| Chen et al. [52] | Retrospective study | 99 | Pneumonia, abnormal CT, cardiac injury, secondary infection | Mechanical respirators and circulatory support systems, including IABP, Impella, and ECMO | COVID-19 infection might deteriorate rapidly, eventually followed by fulminant myocarditis. More attention should be paid to patients with extremely increased cardiac troponin I levels and new-onset arrhythmias. |
| Deng et al. [53] | Retrospective study | 112 | High troponin level and pulmonary hypertension indicating myocardial injury | N/A | Myocardial injury is due to systemic consequences rather than direct injury by Sars-CoV2. |
| Escher et al. [54] | Retrospective study | 104 | EMB: active myocarditis according to the Dallas criteria, necrosis | N/A | Evidence of SARS-CoV-2 genomes detection in EMB. |
| Guo et al. [55] | Retrospective single-center case | 187 | Hypertension, coronary heart disease, cardiomyopathy, elevated TnT level exhibited myocardial injury | Antiviral therapy, antibiotics, respiratory support | Myocardial injury is essentially connected with the lethal outcome. |
| Halushka et al. [56] | Meta-analysis | 22 studies with 277 patients | Macro or microvascular thrombi, inflammation, or intraluminal megakaryocytes | N/A | COVID-19-related cardiac histopathological findings are common, while myocarditis is rare. |
| Han et al. [57] | Single-center study | 273 | High blood levels of CKMB, MYO, Ultra-TnI, NTproBNP indicating acute cardiac injury | Monitoring of the myocardiac enzyme profiles | Higher concentrations of CK-MB, MYO, ultra-TnI, and NT- proBNPin venous blood signified the severity and case fatality rate (CFR) of COVID-19. |
| Khalid et al. [58] | Case series | 2 | Abnormal ECG and Echo, high blood levels of TnI, and NTproBNP | Dual antiplatelet therapy, heparin, dobutamine, norepinephrine, ECMO | Cases of COVID-19 infection with myocardial involvement may have distinct mechanistic pathways and outcomes. |
| Nunes Duarte-Neto et al. [59] | Case series | 10 | Hypertrophy of cardiomyocytes, myocardial fibrosis, interstitial edema fibrin thrombi (2 mild lymphomononuclear myocarditis) | N/A | COVID-19 is a systemic disease with major effects in the lungs and the involvement of various organs including the heart. |
| Puntmann et al. [60] | Cohort study | 100 | hsTnT values significantly elevated, EMB: active lymphocytic inflammation, CMR: myocardial fibrosis and/or edema | Antiviral, antibiotic, steroid, hydrochloroquine | The combination of histological findings as well as the increase relative to age-matched, sex-matched, and risk-factor-matched controls makes this a COVID-19-related inflammatory process. |
| Rajpal et al. [61] | Prospective study | 26 | CMR: myocardial edema and myocardial injury, pericardial effusion | N/A | CMR may provide an excellent risk-stratification assessment for myocarditis in athletes who have recovered from COVID-19. |
| Ruan et al. [62] | Retrospective multi-center study | 150 | Predictors of a fatal outcome included age, underlying diseases, secondary infection, and elevated inflammatory indicators in the blood | N/A | The infection of SARS-CoV-2 may cause fulminant myocarditis, and patients with cardiovascular diseases have a significantly increased risk of death when they are infected with SARS-CoV-2. |
| Shi et al. [63] | Cohort study | 416 | Abnormal ECG, bilateral pneumonia, ground-glass opacity, mottling | Antiviral therapy, oxygen, glucocorticoids, intravenous immunoglobulin therapy, antibiotic therapy | The data and findings support cardiac injury as a complication in COVID-19 patients. |
| Yang et al. [64] | Meta-analysis | 6 studies with 1527 patients | Hypertension, cardiac cerebrovascular disease, and diabetes | N/A | COVID-19 might aggravate the damage to the heart. |
| Types of Post-COVID Conditions | ||
|---|---|---|
| Long COVID-19 | COVID-19 Multiorgan Effects | COVID-19 Treatment or Hospitalization Effects |
| A range of symptoms that can last weeks or months after first being infected or can appear weeks after infection. Can happen to anyone who has had COVID-19, even if the illness was mild, or they had no symptoms. Tiredness or fatigue, difficulty thinking or concentrating (sometimes referred to as “brain fog”), headache, loss of smell or taste, orthostatic dizziness, fast-beating or pounding heart (also known as heart palpitations), chest pain, difficulty breathing or shortness of breath, cough, joint or muscle pain, depression or anxiety, fever, symptoms that get worse after physical or mental activities. | Multiorgan effects can affect most, if not all, body systems, including heart, lung, kidney, skin, and brain functions. Can also include conditions that occur after COVID-19, like multisystem inflammatory syndrome (MIS) and autoimmune condition. | Longer-term effects of COVID-19 treatment or hospitalization (some of these effects are similar to those related to hospitalization for other respiratory infections or other conditions). Can include severe weakness and post-traumatic stress disorder (PTSD involves long-term reactions to a stressful event), and post-intensive care syndrome (PICS). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carretta, D.M.; Silva, A.M.; D’Agostino, D.; Topi, S.; Lovero, R.; Charitos, I.A.; Wegierska, A.E.; Montagnani, M.; Santacroce, L. Cardiac Involvement in COVID-19 Patients: A Contemporary Review. Infect. Dis. Rep. 2021, 13, 494-517. https://doi.org/10.3390/idr13020048
Carretta DM, Silva AM, D’Agostino D, Topi S, Lovero R, Charitos IA, Wegierska AE, Montagnani M, Santacroce L. Cardiac Involvement in COVID-19 Patients: A Contemporary Review. Infectious Disease Reports. 2021; 13(2):494-517. https://doi.org/10.3390/idr13020048
Chicago/Turabian StyleCarretta, Domenico Maria, Aline Maria Silva, Donato D’Agostino, Skender Topi, Roberto Lovero, Ioannis Alexandros Charitos, Angelika Elzbieta Wegierska, Monica Montagnani, and Luigi Santacroce. 2021. "Cardiac Involvement in COVID-19 Patients: A Contemporary Review" Infectious Disease Reports 13, no. 2: 494-517. https://doi.org/10.3390/idr13020048
APA StyleCarretta, D. M., Silva, A. M., D’Agostino, D., Topi, S., Lovero, R., Charitos, I. A., Wegierska, A. E., Montagnani, M., & Santacroce, L. (2021). Cardiac Involvement in COVID-19 Patients: A Contemporary Review. Infectious Disease Reports, 13(2), 494-517. https://doi.org/10.3390/idr13020048









