Abstract
Total gastrectomy with D2 lymphadenectomy for gastric cancer is a complex surgical procedure with a moderate complication rate. Sometimes, some complications may have a misleading onset without a clear clinical presentation and blood test changes. In this case report, hiccups were the main symptom of subdiaphragmatic fluid collection after total gastrectomy.
1. Introduction
Gastric cancer (GC) has one of the greatest impacts on public health worldwide, ranking sixth in terms of incidence and seventh in terms of mortality among all cancers. The incidence of GC varies significantly around the world, with the highest rates observed in Eastern Asia and Central and Eastern Europe and, to a lesser extent, in Central and South America. Conversely, the lowest rates are recorded in Oceania, North America, Northern Europe, and Africa. The contrasting incidence rates observed in relation to the diverse clinico-pathological presentations exhibited by Asian and Western populations are indicative of differing pathogenic processes, as well as biological, environmental, and nutritional risk factors [1,2].
In recent decades, there has been a significant advancement in the management of GC, largely as a result of the parallel development of different approaches in the early diagnosis and systemic treatment of the condition. Early diagnosis of gastric cancer has become a global reality. In Japan and South Korea, most such cancers are diagnosed at an early stage, thanks to screening programs. In Western countries, however, a higher proportion of cancers are diagnosed at an advanced stage. Consequently, in Eastern countries, most early cancers are treated with endoscopic procedures, resulting in favorable overall survival rates. The Japanese Society for Gastroenterological Endoscopy defines early gastric cancer (EGC) as an invasive carcinoma involving only the stomach mucosa or submucosa, regardless of lymph node status (T1, any N according to TNM Classification of the eighth edition of the AJCC staging system) [3,4,5].
For cases of resectable gastric cancer that are not suitable for endoscopic treatment, radical surgery is the preferred treatment option. In the context of contemporary multimodal approaches involving different clinical figures such as surgeons, radiotherapists, and oncologists, several therapeutic strategies have been introduced to reduce the risk of recurrence and improve long-term survival. These include perioperative chemotherapy, adjuvant chemotherapy, and adjuvant chemoradiation therapy. Total gastrectomy with D2 lymphadenectomy is the surgical standard procedure of care for patients with resectable proximal gastric cancer and is usually performed as part of a multimodal approach that includes perioperative chemotherapy [6,7].
This surgical procedure is considered to be highly demanding, requiring a high level of experience and technical skill in the specialist field of upper gastrointestinal tract surgery. It is characterized by a high complication rate in both open and minimally invasive surgical approaches [8,9,10]. Postoperative surgical complications can vary widely. These range from conditions such as postoperative gastroparesis, which can be managed conservatively with minimal global consequences, to life-threatening complications such as anastomotic fistulas.
2. Case Report
2.1. Patient History and Staging
A case of a 72-year-old male patient, a non-smoker with no previous surgery, with a history of psoriatic dermatitis, and without any systemic complications or chronic corticosteroid therapy, was chosen for this study. Due to epigastric abdominal pain and dysphagia with solid food, the patient underwent EGDS with evidence of a neoplastic excavated lesion involving the gastric angulus antrum along the lesser curvature (Figure 1). The histological examination of the biopsy specimen revealed a tubular adenocarcinoma G3, HP-negative. Despite initially presenting with dysphagia, the patient did not experience any weight loss at the time of diagnosis.
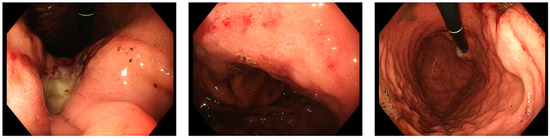
Figure 1.
Diagnostic EGDS showing a deformed antrum with an ulcerated lesion raised and centrally depressed, ulcerated at the level of the angulus, extending distally almost to the pylorus.
The patient underwent oncological staging, which included a thoraco-abdominal CT scan. This investigation revealed a locally advanced gastric tumor characterized by perigastric lymphadenopathy along the lesser gastric curvature, with no distant metastases (Figure 2).
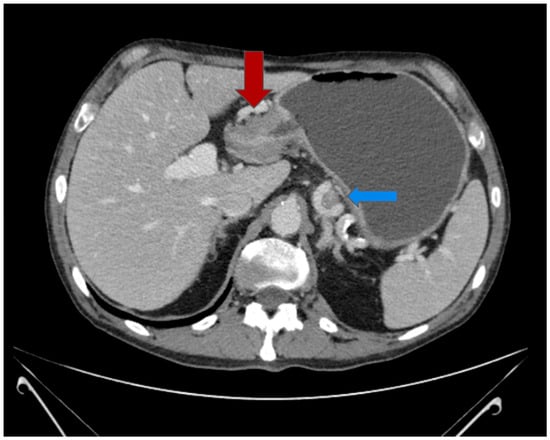
Figure 2.
Preoperative abdominal CT scan with IV contrast: neoplastic sleeve thickening of the gastric antrum (red arrow) with gastrectasia; perigastric lymphadenopathy along the lesser curvature (blue arrow).
2.2. Multimodal Approach and Treatment
This case was discussed at the multidisciplinary team meeting, which included surgeons, oncologists, radiotherapists, and nuclear medicine specialists, all of whom had expertise in upper gastrointestinal tract tumors. The recommendation was made for perioperative chemotherapy using the FLOT (which includes Docetaxel, Oxalilplatin, Leucovorin, and 5-Fluorouracil) regimen. However, the patient only completed the first cycle of chemotherapy due to the onset of anemia, upper limb deep vein thrombosis (DVT), and a worsening of dysphagia. Due to this clinical presentation, it was decided to proceed with upfront surgery.
The patient underwent exploratory laparotomy, which confirmed the locally advanced sub-occluding neoplasm with a single peritoneal nodule localized in the transverse mesocolon. We performed total gastrectomy with D2 lymphadenectomy and esophago-jejunal anastomosis with Roux-en-Y reconstruction, excision of the peritoneal nodule, and feeding jejunostomy. A comprehensive histological evaluation of the surgical specimen was conducted, which resulted in the following pathological diagnosis: low-grade tubular adenocarcinoma with serosal invasion and 7 metastatic lymph nodes out of 71 harvested. The peritoneal nodule was positive for neoplastic localization. pTNM: ypT4a pN3a pM1 according to AJCC 8th edition.
2.3. Postoperative Course
The initial postoperative course was normal, and the NG tube was removed on postoperative day III after a negative methylene blue test. On postoperative day IV, the patient started oral fluid feeding with enteral support through a jejunostomy. On postoperative day V, the patient was started on a soft diet, but during the same day, hiccups occurred in association with nausea. Therefore, we stopped oral feeding and started prokinetic therapy with partial clinical regression of the symptoms. Furthermore, on postoperative day V, laboratory tests showed anemia (Hb 8.6 g/dL vs. 10.6 g/dL), so the patient was transfused with two units of concentrated red blood cells. However, hiccups persisted. On postoperative day VII, the patient presented with fever, which responded to acetaminophen, neutrophilic leukocytosis, and elevated c-reactive protein on laboratory tests. Due to growing suspicions of major complications that could explain the hiccups and anemia, such as internal gastrointestinal bleeding, efferent loop syndrome, or an abdominal fluid collection, we decided to perform a CT scan of the abdomen. This revealed bilateral pleural effusions, two minor hypodense lesions of the spleen (Figure 3), and a subdiaphragmatic perisplenic fluid collection (Figure 4). Blood and urine cultures were also taken, both of which showed no bacterial growth.
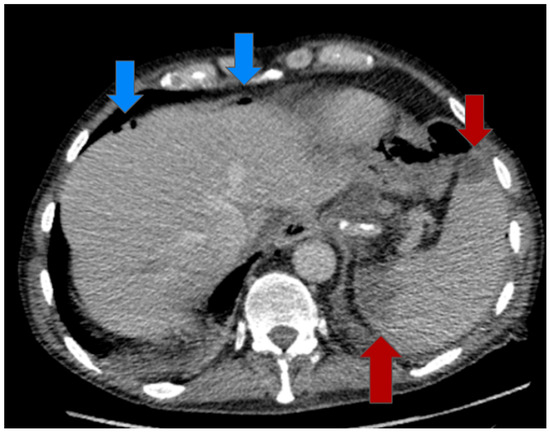
Figure 3.
Postoperative abdominal CT scan with IV contrast: hypodense lesions of the spleen (red arrow), intraperitoneal air microbubbles (blue arrow) compatible with open surgery outcomes; no evidence of air bubbles at the esophago-jejunal anastomosis and downstream jejuno-jejunal anastomosis.
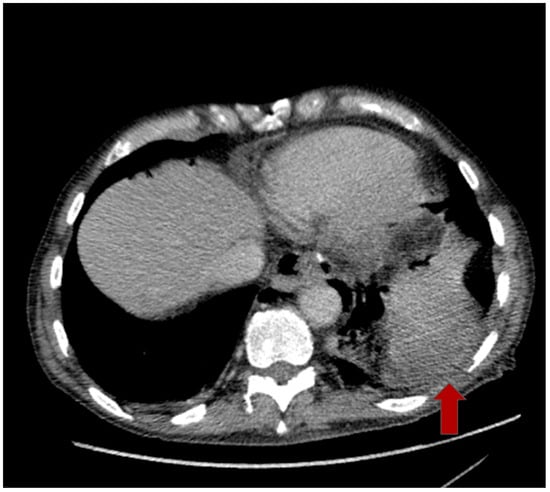
Figure 4.
Postoperative abdominal CT scan with IV contrast: subdiaphragmatic perisplenic fluid collection (red arrow).
Physical examination of the abdomen was negative, with no evidence of abdominal defense reaction or peritonism, and the output from the abdominal drains was consistently serosanguineous fluid. Given the hemodynamic stability, the absence of peritonitis and gastrointestinal leakage, and the haemochrome’s stability following blood transfusion, conservative treatment was considered the optimal approach.
The patient was, therefore, treated with prokinetic drugs and broad-spectrum antibiotic therapy, which resulted in progressive symptom regression and normalization of inflammatory laboratory tests. No surgical or radiological intervention was required. The patient was discharged on postoperative day XIV. Subsequent follow-up was regular; the patient had no further symptoms and continued with oral feeding. Finally, a CT scan of the thorax and abdomen was performed 30 days after surgery (Figure 5), showing a reduction in the subdiaphragmatic fluid collection and stable hypodense lesions in the spleen.
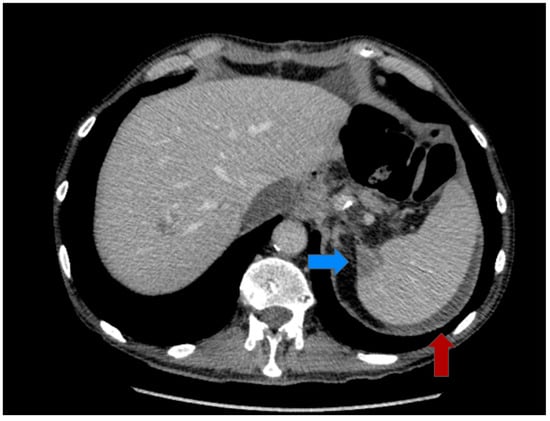
Figure 5.
Abdominal CT scan with IV contrast at 30 days: hypodense lesion of the spleen (blue arrow), subdiaphragmatic perisplenic fluid collection in reduction (red arrow).
3. Discussion
Hiccup, or singultus, originates from the Latin word singultus, which means “the act of catching one’s breath while sobbing” [11].
Hiccups are characterized by involuntary and intermittent contractions of the diaphragm and intercostal muscles, resulting in a sudden inspiration associated with audible closure of the glottis. The hiccup reflex arc is composed of three distinct modules: the afferent limb, which includes the phrenic, vagus, and sympathetic nerves to transmit somatic and visceral sensory signals; the central processing unit in the mid-brain; and the efferent limb, which is conducted in motor fibers of the phrenic nerves to the diaphragm and accessory nerves to the intercostal muscles, respectively. Lesions in the reflex arc components are considered to be the pathophysiological mechanism of hiccups, and the etiology can be distinguished according to the affected arc component and classified as a central or peripheral pathway [12,13].
Regarding the topic of peripheral causes, it is possible to distinguish between different aetiologies originating in the gastrointestinal tract. These include gastro-oesophageal reflux disease, hiatus hernia, stomach volvulus, stomach distension, bowel obstruction, H. pylori infection, peptic ulceration, pancreatitis, hepatitis, abdominal abscesses, gallbladder disease, oesophageal tumors, and abdominal voluminous tumors [14,15,16,17,18,19,20]. In addition, a number of causal factors have been identified in relation to the surgical environment. These include the use of certain anesthetic agents, central venous catheterization, pharyngeal intubation, bronchoscopy, gastric insufflation and sedation during endoscopy, and thoracic and abdominal surgery [21,22,23,24,25,26,27,28].
Total gastrectomy with D2 lymphadenectomy is a surgical procedure with a significant complication rate, even when performed by highly experienced and skilled teams at specialized third-level centers. This applies to both open and minimally invasive surgery. The overall complication rate was found to range from 28.5% to 29.8%, while the 30-day mortality rate was observed to vary between 3.7% and 3.6% in the Netherlands, according to the Dutch Upper gastrointestinal Cancer Audit (DUCA), in comparison to the Gastrectomy Complications Consensus Group (GCCG) in Europe. Distinctions can be made between intraoperative complications, general postoperative complications (e.g., pleural effusion, pneumothorax, or non-surgical infections), and postoperative surgical complications. Several postoperative surgical complications have been identified, the most serious of which are postoperative bleeding requiring invasive treatment (endoscopic hemostasis, radiological embolization, or surgical exploration if previous treatment has failed), postoperative bowel perforation or necrosis, or duodenal leakage or anastomotic leakage. These can cause abdominal contamination that may develop into sepsis if not tamponaded or treated promptly. Further significant complications necessitating re-intervention or other invasive procedures include evisceration, diaphragmatic hernia, feeding jejunostomy-related complications, and other reoperations not attributable to postoperative bleeding, leakage, or bowel necrosis. A number of other postoperative surgical complications were documented, including postoperative bowel obstruction, postoperative pancreatic fistula, postoperative pancreatitis, delayed gastric emptying (by the 10th postoperative day), and other postoperative abnormal fluid from drainage or abdominal collections without gastrointestinal leak, which may require treatment (e.g., abdominal abscess; chylous ascites following extensive lymphadenectomy [29].
In light of the foregoing, it is imperative to recognize postoperative complications at the earliest stage by employing all available means, whether clinical, laboratory, or instrumental. This is essential to ensure timely intervention and to prevent the progression of the condition toward an unfavorable outcome.
In this case report, it was observed that hiccups were the initial and sole symptom and clinical sign of a postoperative surgical complication. This complication was subsequently identified as a subdiaphragmatic collection by means of an abdominal CT scan with an iodinated contrast medium.
In accordance with the established protocol at our institute for the post-surgical period, routine laboratory examinations were conducted on the first and third postoperative days. These examinations encompass a comprehensive assessment of the complete blood count, including the leukocyte count, as well as renal and hepatic function tests. Additionally, inflammatory indices, such as C-reactive protein and procalcitonin, are measured to ensure a comprehensive diagnostic assessment to identify and recognize early signs of complications. In this particular case report, the results of routine laboratory investigations initially failed to reveal any significant alterations on postoperative days I and III; it was only on postoperative day V that the laboratory tests revealed moderate anemia (Hb 8.6 g/dL vs. 10.6 g/dL), although this occurred in the absence of any other symptoms or clinical signs. The only notable manifestation was the onset of hiccups. A significant shift in the patient’s laboratory tests was not observed until postoperative day VII, marked by the presence of neutrophilic leukocytosis and elevated levels of C-reactive protein. These major alterations coincided with a rise in body temperature to 38 °C on the same day.
The presence of hiccups, the sole significant symptom initially presented, in the context of anemia and fever, and in the absence of any other evident clinical findings, led to the hypothesis that the observed symptoms were a result of a self-limiting bleed following the surgical procedures conducted during the D2 lymphadenectomy on the greater curvature of the stomach and the dissection of the gastrosplenic ligament. These procedures resulted in the formation of a peri-splenic blood collection, which led to phrenic nerve irritation and hiccups. In this case, the bleeding was self-limiting, as confirmed by serial CT scans and the subsequent resolution of anemia following limited blood transfusion.
The fever may have been caused by a secondary infection of the collection, which was successfully treated with broad-spectrum antibiotics and did not require invasive intervention, either radiological or surgical. Physical examination of the abdomen consistently yielded negative findings, as the fluid collection was not in contact with the anterior abdominal wall or visceral peritoneum. A CT scan performed one month after surgery, along with the favorable clinical outcome of the patient, confirmed our clinical hypothesis.
In the event of treatment failure, as evidenced by an observed deterioration in inflammatory markers or the clinical picture, the implementation of radiological drainage to address the collection may be considered.
However, surgical exploration to drain the collection, explore the entire abdominal cavity for possible sources of contamination or leakage, and perform a washout and placement of drains would only be indicated in the case of a subsequent uncontrolled septic state with hemodynamic instability.
This clinical presentation is of particular relevance, especially in cancer patients undergoing multimodal treatment or elderly patients. In such cases, clinical signs and symptoms may be reduced, and significant surgical sequelae may initially go unnoticed. This can result in a deterioration of the patient’s general condition due to complications that are not recognized in a timely manner. This can have a negative impact on the patient’s prognosis and oncological outcomes [30,31,32].
In this context, postoperative monitoring is particularly important in cases of suspected bleeding related to injury to the spleen or splenic vessels. If diagnosed early, conservative management may be attempted if the extent of bleeding or lesion is not severe. In fact, it has been observed that patients who have undergone splenectomy in an operation where it was not planned appear to have a worse oncological prognosis, suggesting an altered anti-tumor immunity in patients who have undergone splenectomy [33]. One study found that among patients who underwent colectomy for cancer, those who underwent splenectomy had a significant decrease in 5-year survival (70% vs. 47%) [34]. Similar findings were reported in another study, which found that splenectomy was an independent factor in the risk of recurrence in patients undergoing gastrectomy for cancer (48% vs. 23%) [35].
We performed a literature review carried out on the main scientific portals (PubMed, Google Scholar, Research Gate); hiccups were highlighted as a symptom associated with surgical complications in a few papers. In a recent (2021) case of exploratory laparoscopy and subsequent appendectomy for acute appendicitis, the patient developed persistent hiccups for a few minutes after pneumoperitoneum was established. In this instance, it was hypothesized that the Trendelenburg position provided a direct stimulus to the diaphragm muscle from the inflammatory peritoneal fluid, in addition to the pressure stimulus from the pneumoperitoneum [36]. In 1993, a review was conducted to investigate the occurrence of persistent postoperative hiccups, defined as hiccups lasting more than 48 h. The potential causative factors were identified as postoperative pneumonia, subdiaphragmatic abscess, or gastric distension [37]. A 1968 study of 220 patients treated at the Mayo Clinic between 1935 and 1963 investigated the etiology of hiccups. The study identified various cases of hiccups following surgery, including one case in the thoracic surgery field for a transthoracic resection of the lower part of the esophagus and the upper part of the stomach for cancer of the esophagus and 23 cases following in order of frequency: gastroenterostomy, gastrectomy, or both (5); exploratory laparotomy for carcinomatosis (4); colectomy (4); exploratory laparotomy for cancer of the pancreas (3); cholecystectomy (3); exploratory laparotomy for chronic relapsing pancreatitis (1); closure of perforated jejunal ulcer (1); takedown of jejuno-colonic stoma for Crohn’s disease (1); sympathectomy (1) [28].
4. Conclusions
The distinguishing feature of this paper is that hiccups were the only initially notable symptom exhibited in the context of a surgical complication following a total gastrectomy with D2 lymphadenectomy for gastric cancer in the absence of other discernible clinical manifestations.
Therefore, even the mildest symptoms must not be overlooked, even if there are no significant changes in laboratory or physical examinations. This is because, as illustrated in the present case, they may be the initial manifestation of a major surgical complication, and an early and timely diagnosis would certainly facilitate the management of the complication. This could be achieved by performing a CT scan with contrast to recognize and delineate any ongoing process (e.g., sepsis, leakage, or bleeding), enabling the most appropriate strategy to be chosen.
Author Contributions
Conceptualization, F.L. and G.M.; methodology, F.L.; validation, F.L., G.M., and P.P.; formal analysis, F.L. and G.M.; investigation, F.L., G.M., F.T. and B.M.; data curation, F.L., G.M., F.T. and B.M.; writing—original draft preparation, F.L.; writing—review and editing, F.L., G.M. and P.P.; visualization, F.L. and G.M.; supervision, P.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received ‘Ricerca Corrente’ funding from the Italian Ministry of Health to cover publication costs.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to only one case.
Informed Consent Statement
Written informed consent was obtained from the patient for the surgical procedure.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to patient data confidentiality.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AJCC | American Joint Committee on Cancer |
| CT | Computed Tomography |
| DUCA | Dutch Upper GI Cancer Audit |
| DVT | Deep Vein Thrombosis |
| FLOT | Docetaxel, Oxalilplatin, Leucovorin, 5-Fluorouracil |
| EGDS | Esophagogastroduodenoscopy |
| GC | Gastric Cancer |
| GCCG | Gastrectomy Complications Consensus Group |
| GI | Gastro-Intestinal |
| TNM | Tumor-node-metastasis system |
References
- Ferlay, J.; Laversanne, M.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Tomorrow (Version 1.1). Lyon, France: International Agency for Research on Cancer. 2024. Available online: https://gco.iarc.who.int/tomorrow (accessed on 31 January 2025).
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Chiarello, M.M.; Fico, V.; Pepe, G.; Tropeano, G.; Adams, N.J.; Altieri, G.; Brisinda, G. Early gastric cancer: A challenge in Western countries. World J. Gastroenterol. 2022, 28, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Hirota, W.K.; Zuckerman, M.J.; Adler, D.G.; Davila, R.E.; Egan, J.; Leighton, J.A.; Qureshi, W.A.; Rajan, E.; Fanelli, R.; Wheeler-Harbaugh, J.; et al. ASGE guideline: The role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest. Endosc. 2006, 63, 570–580. [Google Scholar] [CrossRef]
- Ji, X.; Bu, Z.-D.; Yan, Y.; Li, Z.-Y.; Wu, A.-W.; Zhang, L.-H.; Zhang, J.; Wu, X.-J.; Zong, X.-L.; Li, S.-X.; et al. The 8th edition of the American Joint Committee on Cancer tumor-node-metastasis staging system for gastric cancer is superior to the 7th edition: Results from a Chinese mono-institutional study of 1663 patients. Gastric Cancer 2018, 21, 643–652. [Google Scholar] [CrossRef]
- Lordick, F.; Carneiro, F.; Cascinu, S.; Fleitas, T.; Haustermans, K.; Piessen, G.; Vogel, A.; Smyth, E. Gastric cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022, 33, 1005–1020. [Google Scholar] [CrossRef]
- Ajani, J.A.; D’Amico, T.A.; Bentrem, D.J.; Chao, J.; Cooke, D.; Corvera, C.; Das, P.; Enzinger, P.C.; Enzler, T.; Fanta, P.; et al. Gastric Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2022, 20, 167–192. [Google Scholar] [CrossRef] [PubMed]
- Gertsen, E.C.; Goense, L.; Brenkman, H.J.F.; van Hillegersberg, R.; Ruurda, J.P.; Dutch Upper Gastrointestinal Cancer Audit (DUCA) Group. Identification of the clinically most relevant postoperative complications after gastrectomy: A population-based cohort study. Gastric Cancer 2020, 23, 339–348. [Google Scholar] [CrossRef]
- Zhou, J.; Yu, P.; Shi, Y.; Tang, B.; Hao, Y.; Zhao, Y.; Qian, F. Evaluation of Clavien-Dindo classification in patients undergoing total gastrectomy for gastric cancer. Med. Oncol. 2015, 32, 120. [Google Scholar] [CrossRef]
- Siani, L.M.; Ferranti, F.; De Carlo, A.; Quintiliani, A. Completely laparoscopic versus open total gastrectomy in stage I-III/C gastric cancer: Safety, efficacy and five-year oncologic outcome. Minerva Chir. 2012, 67, 319–326. [Google Scholar]
- Hiccup. Available online: http://en.wikipedia.org/wiki/Hiccup (accessed on 18 February 2025).
- He, J.; Guan, A.; Yang, T.; Fu, L.; Wang, Y.; Wang, S.; Ren, H.; Chen, L.; Zhu, Y.; Deng, B. Pathogenesis and treatment of perioperative hiccups: A narrative review. Ann. Med. 2025, 57, 2474173. [Google Scholar] [CrossRef]
- Chang, F.-Y.; Lu, C.-L. Hiccup: Mystery, nature and treatment. J. Neurogastroenterol. Motil. 2012, 18, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Cerezo, E.; Viñuelas-Chicano, M.; Pérez-Vigara, G.; Gomez-Ruiz, C.J.; Sanchez-Manjavacas, N.; Jimeno-Ayllon, C.; Perez-Sola, A. A patient with persistent hiccups and gastro-oesophageal reflux disease. Gut 2008, 57, 763. [Google Scholar] [CrossRef] [PubMed]
- Félix-Téllez, F.A.; Jiménez-Castillo, R.A.; Remes-Troche, J.M. Identifying the hiccup-induced esophagogastric wave form: A case series report using high-resolution manometry. ACG Case Rep. J. 2024, 11, e01541. [Google Scholar] [CrossRef]
- Senior, A.; Hari, C. A rare case of acute on chronic gastric volvulus with Borchardt’s triad. J. Surg. Case Rep. 2014, 2014, rju114. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Shang, Q.; Wei, G.Q.; Guo, Q.H.; Ka, S.Q.; Zhang, Z.Y.; Li, F.W.; Shen, X.P.; Zhang, D.K. Jinghuaweikang capsules combined with Quadruple therapy in the treatment of Helicobacter pylori infection: A multicenter, randomized, controlled, clinical study. Zhonghua Yi Xue Za Zhi 2019, 99, 295–300. [Google Scholar] [CrossRef]
- Kumar, S.; Sharma, P.; Muthu, R.; Mohakund, S. Management of empyema of gallbladder with percutaneous cholecysto-duodenal stenting in a case of hilar cholangiocarcinoma treated with common bile duct metallic stenting. Indian J. Radiol. Imaging 2011, 21, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, C.; Bansari, A.; Ladna, M.; Dideban, B. Prolonged intractable hiccups associated with HSV(I.&II) esophagitis, H. pylori gastritis. Case Rep. Infect. Dis. 2023, 2023, 3561895. [Google Scholar]
- Muraki, N.; Asahina, K.; Hori, K.; Inanaga, R.; Matsui, K.; Shinozaki, M. Intra-abdominal abscess caused by mycobacteroides abscessus in a peritoneal dialysis patient: A case report. Intern. Med. 2024, 10, 232–236. [Google Scholar] [CrossRef]
- McVey, F.K.; Goodman, N.W. Gastro-oesophageal reflux and hiccough on induction of anaesthesia. Anaesthesia 1992, 47, 712. [Google Scholar] [CrossRef]
- Khatri, S.; Hannurkar, P. Understanding and treating laryngeal mask airway-induced intraoperative hiccups. Cureus 2024, 16, e69782. [Google Scholar] [CrossRef]
- Neumann, M.; Lazo, K.G.; Stover, D. Sarcoidosis presenting as hiccups. Respirol. Case Rep. 2020, 8, e00605. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, Y.; Nakajima, Y.; Tokuda, K.; Kidani, R. Recurrent hiccups caused by malposition of the peritoneal catheter of a lumboperitoneal shunt: A case report. No Shinkei Geka 2016, 44, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Arroyo-Cózar, M.; Grau Delgado, J.; Gabaldón Conejos, T. Hiccups induced by midazolam during sedation in flexible bronchoscopy. Arch. Bronconeumol. 2012, 48, 103. [Google Scholar] [CrossRef]
- Tammineedi, S.N.; Singla, R.; Cornejo Leon, M.; Kohli, M.; Saini, C.; Pitiliya, A. Unforeseen effects: Hiccups unveiled by high-dose steroids in demyelination. eNeurologicalSci 2024, 35, 100509. [Google Scholar] [CrossRef]
- Xausa, G.; Escher, M.; Singovski, S.; Hentsch, L. Recurrent persistent hiccups on opioid treatment: A case report and literature review. J. Pain Palliat. Care Pharmacother. 2023, 37, 82–90. [Google Scholar] [CrossRef]
- Visser, M.R.; Voeten, D.M.; Gisbertz, S.S.; Ruurda, J.P.; Henegouwen, M.I.v.B.; van Hillegersberg, R.; The Dutch Upper Gastrointestinal Cancer Audit (DUCA) Group. Outcomes after gastrectomy according to the Gastrectomy Complications Consensus Group (GCCG) in the Dutch Upper GI Cancer Audit (DUCA). Gastric Cancer 2024, 27, 1124–1135. [Google Scholar] [CrossRef]
- Chen, G.; Wang, J.; Chen, K.; Kang, M.; Zhang, H.; Jin, X.; Lin, L.; Chen, J. Relationship Between Postoperative Complications and the Prognosis of Gastric Carcinoma Patients Who Underwent Surgical Resection: A Systematic Review and Meta-Analysis. Cancer Control J. Moffitt Cancer Cent. 2021, 28, 10732748211011955. [Google Scholar] [CrossRef]
- Obana, A.; Iwasaki, K.; Suwa, T. Impact of postoperative complications on gastric cancer survival. Surgery 2025, 178, 108873. [Google Scholar] [CrossRef] [PubMed]
- Buzelé, R.; Barbier, L.; Sauvanet, A.; Fantin, B. Medical complications following splenectomy. J. Visc. Surg. 2016, 153, 277–286. [Google Scholar] [CrossRef]
- Zhang, C.; Shaw, N. A curious case of hiccups during laparoscopic surgery. J. Anaesthesiol. Clin. Pharmacol. 2021, 37, 304–305. [Google Scholar] [CrossRef]
- Wakeman, C.J.; Dobbs, B.R.; Frizelle, F.A.; Bissett, I.P.; Dennett, E.R.; Hill, A.G.; Thompson-Fawcett, M.W. The impact of splenectomy on outcome after resection for colorectal cancer: A multicenter, nested, paired cohort study. Dis. Colon Rectum 2008, 51, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.G.; Cheong, J.H.; Hyung, W.J.; Kim, J.; Choi, S.H.; Noh, S.H. Adverse effect of splenectomy on recurrence in total gastrectomy cancer patients with perioperative transfusion. Am. J. Surg. 2006, 192, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Vallet-Regí, M.; Manzano, M.; Rodriguez-Mañas, L.; Checa López, M.; Aapro, M.; Balducci, L. Management of Cancer in the Older Age Person: An Approach to Complex Medical Decisions. Oncologist 2017, 22, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Hansen, B.J.; Rosenberg, J. Persistent postoperative hiccups: A review. Acta Anaesthesiol. Scand. 1993, 37, 643–646. [Google Scholar] [CrossRef]
- Souadjian, J.V.; Cain, J.C. Intractable hiccup. Etiologic factors in 220 cases. Postgrad. Med. 1968, 43, 72–77. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).