A Data-Driven Approach for Estimating Type 2 Diabetes-Related Costs in Greece
Abstract
1. Introduction
1.1. Global and National Burden of T2D
1.2. Economic Impact of T2D
1.3. Complications, Aging, and Health System Strain
1.4. The Greek Healthcare System, Cost-Containment Mechanisms, and T2D Expenditure
1.5. Study Rationale and Objectives
2. Material and Methods
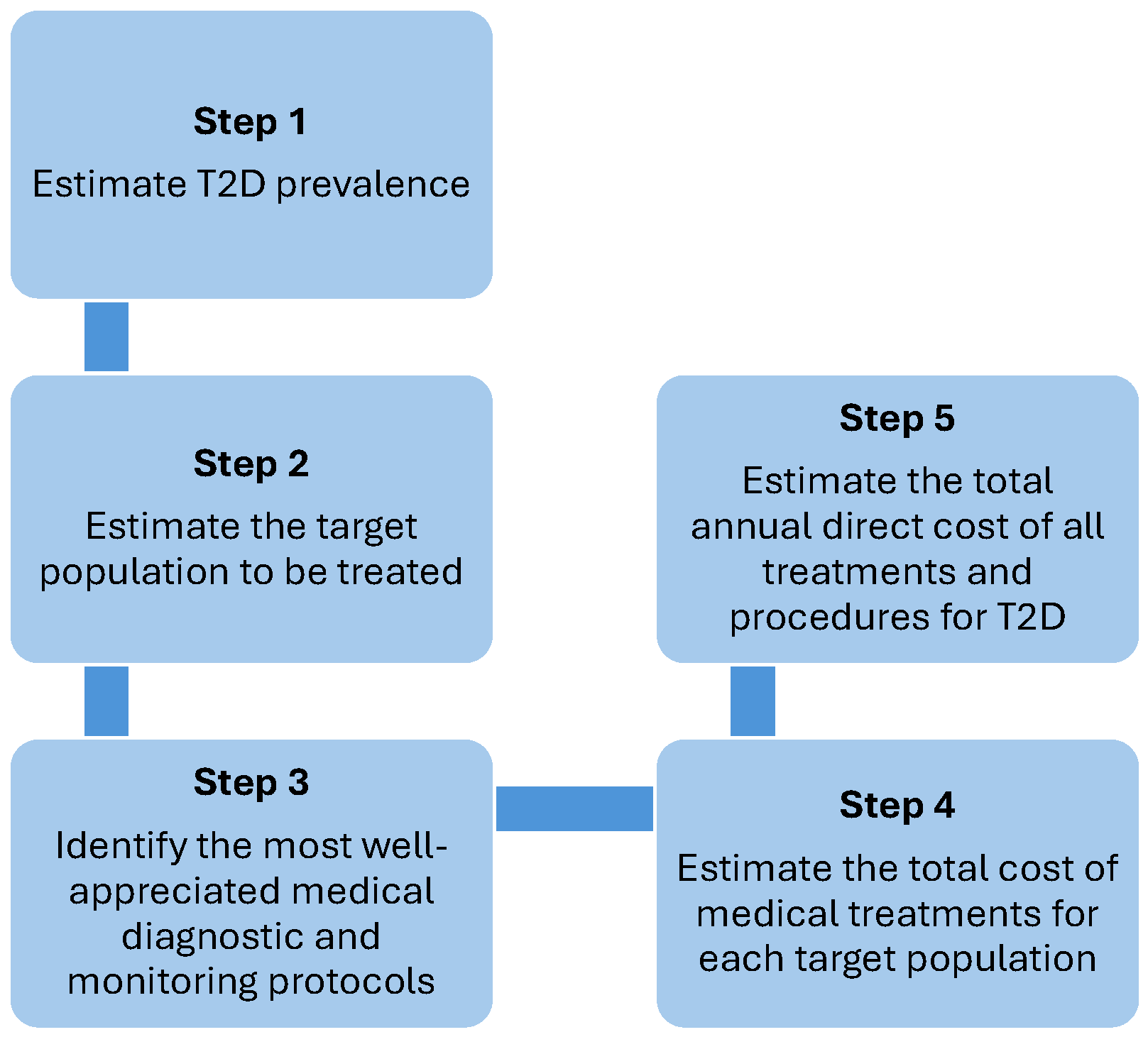
2.1. Application Steps of the Method
- Step 1: Estimate the prevalence of ICD-10 codes related to type 2 diabetes, either through an appropriate sampling method or by conducting a meta-analysis of data from the literature, and calculate the size of the target population requiring treatment in Greece for the years 2021 and 2030, both overall and stratified by age groups (0–9, 10–19, 20–24, 25–49, 50–69, 70+).
- Step 2: Calculate the target population on the basis of census figures or other reliable and validated demographic sources.
- Step 3: Identify the criteria and conditions for initiating drug treatment, the most appropriate treatments, and the strategy for implementing optimal disease management according to the most well-appreciated therapeutic protocols.
- Step 4: Estimate the total cost of medical treatments for each target population, based on the allocation of patients to various treatment options and therapy lines. The distribution of patients between the different treatments and treatment lines can be found by searching PubMed and Google Scholar for randomized clinical trials published in the last 5 years (or any other period the investigators decide).
- Step 5: In line with the established diagnostic and treatment protocols (identified in Step 3), calculate the annual direct costs associated with the cost categories presented above.
2.2. Inputs of the Method
3. Results
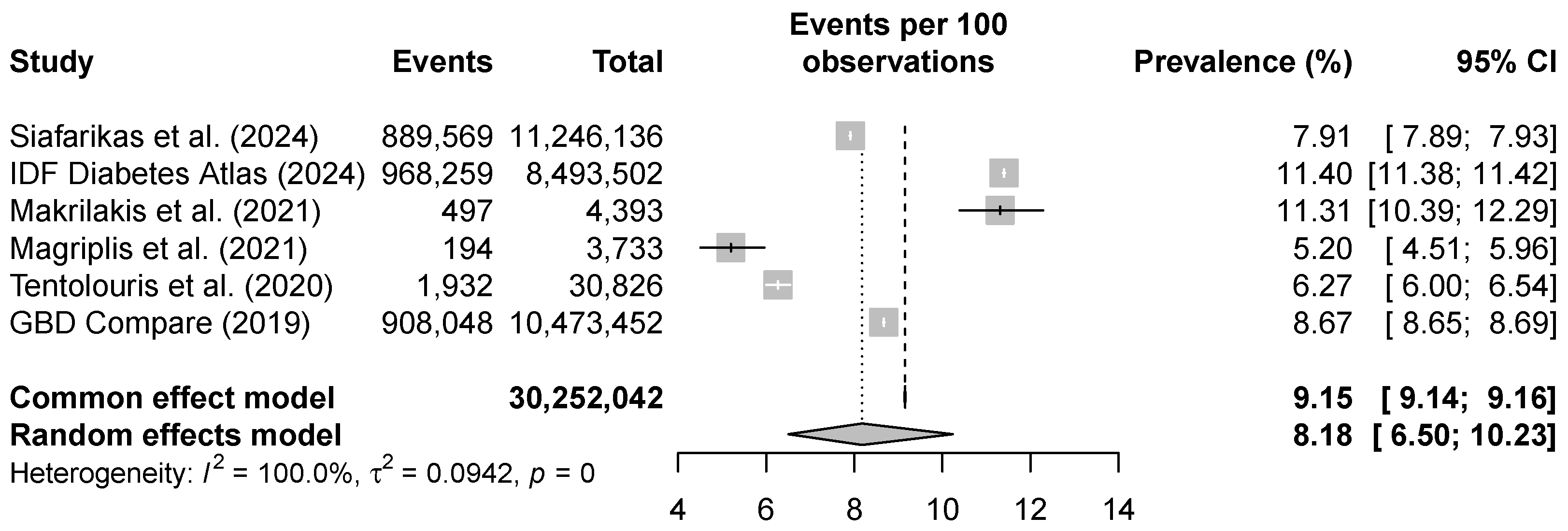
3.1. Prevalence Estimates of T2D
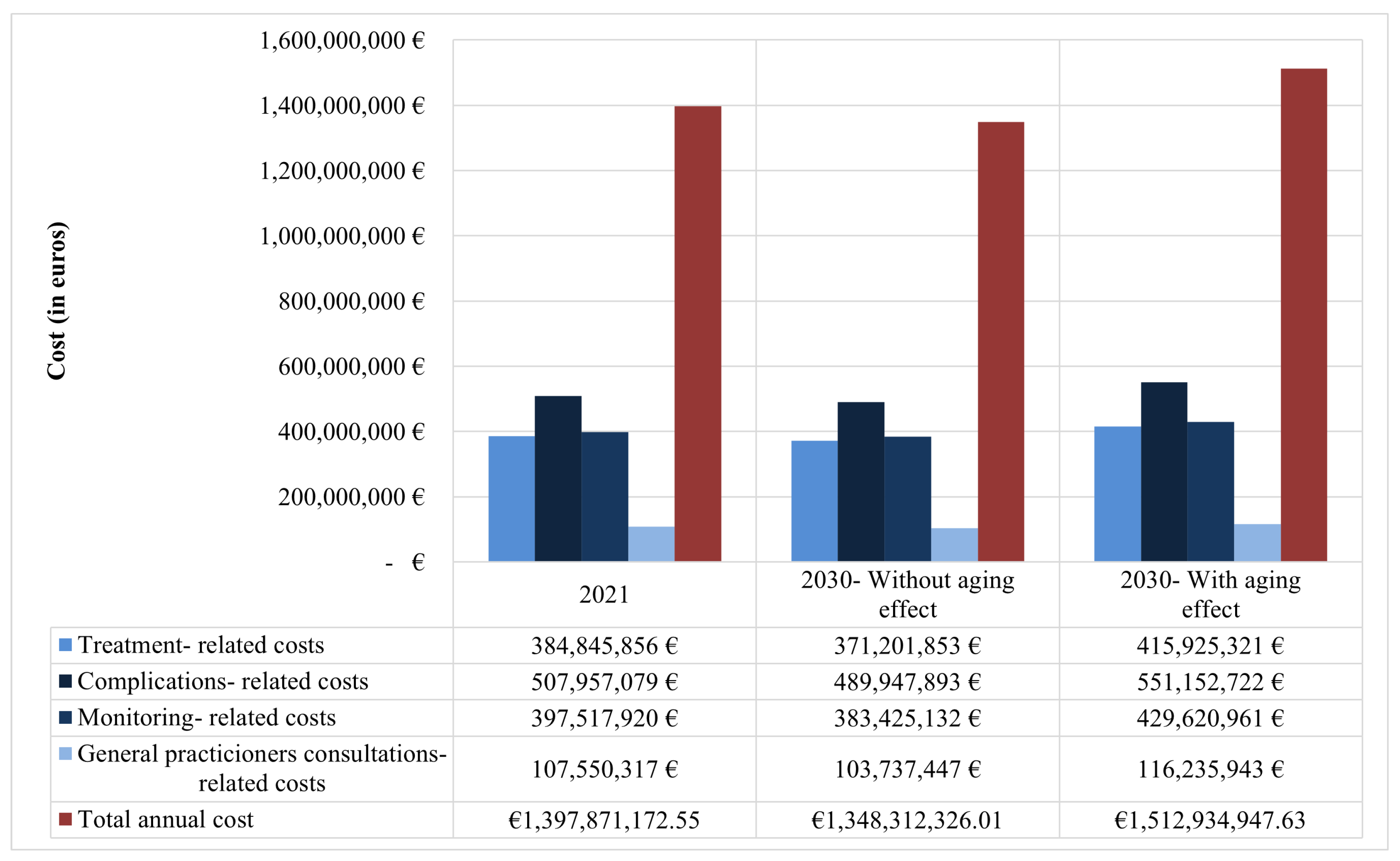
3.2. Estimate of T2D-Related Healthcare Expenditures in 2021
3.3. Sensitivity Analysis Based on RWD
3.4. Projection of Type 2 Diabetes-Related Healthcare Expenditures in 2030
4. Discussion
4.1. Prevalence of T2D
4.2. Cost of T2D
4.3. Dynamics of Type 2 Diabetes and Aging Resilience
4.4. Factors Shaping Type 2 Diabetes Prevalence in Greece
4.5. Economic Implications and Insights from Studies on Estimated Expenses Associated with Type 2 Diabetes
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Forouhi, N.G.; Wareham, N.J. Epidemiology of diabetes. Medicine 2010, 38, 602–606. [Google Scholar] [CrossRef]
- Ong, K.L.; Stafford, L.K.; McLaughlin, S.A.; Boyko, E.J.; Vollset, S.E.; Smith, A.E.; Dalton, B.E.; Duprey, J.; Cruz, J.A.; Hagins, H.; et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef] [PubMed]
- Yang, X. Health expenditure, human capital, and economic growth: An empirical study of developing countries. Int. J. Health Econ. Manag. 2020, 20, 163–176. [Google Scholar] [CrossRef]
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Bommer, C.; Sagalova, V.; Heesemann, E.; Manne-Goehler, J.; Atun, R.; Bärnighausen, T.; Davies, J.; Vollmer, S. Global economic burden of diabetes in adults: Projections from 2015 to 2030. Diabetes Care 2018, 41, 963–970. [Google Scholar] [CrossRef]
- Williams, R.; Karuranga, S.; Malanda, B.; Saeedi, P.; Basit, A.; Besançon, S.; Bommer, C.; Esteghamati, A.; Ogurtsova, K.; Zhang, P.; et al. Global and regional estimates and projections of diabetes-related health expenditure: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2020, 162, 108072. [Google Scholar] [CrossRef]
- Acs, A.; Ludwig, C.; Bereza, B.; Einarson, T.; Panton, U. Prevalence of cardiovascular disease in Type 2 diabetes: A global systematic review. Value Health 2017, 20, A475. [Google Scholar] [CrossRef]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef]
- Ofori, S.N.; Unachukwu, C.N. Holistic approach to prevention and management of type 2 diabetes mellitus in a family setting. Diabetes Metab. Syndr. Obes. Targets Ther. 2014, 7, 159–168. [Google Scholar] [CrossRef]
- Mata-Cases, M.; Casajuana, M.; Franch-Nadal, J.; Casellas, A.; Castell, C.; Vinagre, I.; Mauricio, D.; Bolíbar, B. Direct medical costs attributable to type 2 diabetes mellitus: A population-based study in Catalonia, Spain. Eur. J. Health Econ. 2016, 17, 1001–1010. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, X.; Zhang, P.; Hoerger, T.J. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am. J. Prev. Med. 2013, 45, 253–261. [Google Scholar] [CrossRef]
- Struijs, J.N.; Baan, C.A.; Schellevis, F.G.; Westert, G.P.; Van Den Bos, G.A. Comorbidity in patients with diabetes mellitus: Impact on medical health care utilization. BMC Health Serv. Res. 2006, 6, 84. [Google Scholar] [CrossRef]
- American Diabetes Association. Economic costs of diabetes in the US in 2017. Diabetes Care 2018, 41, 917–928. [Google Scholar] [CrossRef]
- Leung, E.; Wongrakpanich, S.; Munshi, M.N. Diabetes management in the elderly. Diabetes Spectr. Publ. Am. Diabetes Assoc. 2018, 31, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Kalyani, R.R.; Golden, S.H.; Cefalu, W.T. Diabetes and aging: Unique considerations and goals of care. Diabetes Care 2017, 40, 440–443. [Google Scholar] [CrossRef]
- Geyer, J.; Barschkett, M.; Haan, P.; Hammerschmid, A. The effects of an increase in the retirement age on health care costs: Evidence from administrative data. Eur. J. Health Econ. 2023, 24, 1101–1120. [Google Scholar] [CrossRef]
- Andrade, L.; Rapp, T.; Sevilla-Dedieu, C. Quality of diabetes follow-up care and hospital admissions. Int. J. Health Econ. Manag. 2018, 18, 153–167. [Google Scholar] [CrossRef]
- Kalavrezou, N.; Jin, H. Health Care Reform in Greece: Progress and Reform Priorities; International Monetary Fund: Washington, DC, USA, 2021. [Google Scholar]
- Pournara, J. A glance at the evolution of the pharmaceutical clawback in Greece. Int. Tax Rev. 2020. Available online: https://www.internationaltaxreview.com/article/2a68rfy5bw2ycq1wn7os0/a-glance-at-the-evolution-of-the-pharmaceutical-clawback-in-greece (accessed on 10 January 2025).
- Memedovich, K.A.; Manns, B.; Beall, R.; Hollis, A.; Clement, F. The impact of pharmaceutical rebates on patients’ drug expenditures. CMAJ 2019, 191, E308–E312. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Kassab, Y.W.; Taha, N.A.; Zainal, Z.A. Factors impacting pharmaceutical prices and affordability: Narrative review. Pharmacy 2021, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Economou, C.; Kaitelidou, D.; Kentikelenis, A.; Maresso, A.; Sissouras, A. The impact of the crisis on the health system and health in Greece. In Economic Crisis, Health Systems and Health in Europe Country Experience; European Observatory on Health Systems and Policies: Brussels, Belgium, 2015. [Google Scholar]
- Mills, M.; Kanavos, P. Do pharmaceutical budgets deliver financial sustainability in healthcare? Evidence from Europe. Health Policy 2020, 124, 239–251. [Google Scholar] [CrossRef]
- Nika, E.; Tsiampalis, T.; Georgakellos, D. Health budgets using data analytical techniques. In Statistical Methods and Applications in Systems Assurance & Quality; Bersimis, S., Economou, P., Rakitzis, A., Eds.; Advanced Research in Reliability and System Assurance; CRC Press: Boca Raton, FL, USA, 2025; p. 151. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. International Migration Report 2015; United Nations: New York, NY, USA, 2015. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. International Migration Report 2019; United Nations: New York, NY, USA, 2019. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. International Migration Report 2022; United Nations: New York, NY, USA, 2022. [Google Scholar]
- Lee, K.A.; Jin, H.Y.; Kim, Y.J.; Im, Y.J.; Kim, E.Y.; Park, T.S. Treatment patterns of type 2 diabetes assessed using a common data model based on electronic health records of 2000–2019. J. Korean Med. Sci. 2021, 36, e230. [Google Scholar] [CrossRef]
- Deshpande, A.D.; Harris-Hayes, M.; Schootman, M. Epidemiology of diabetes and diabetes-related complications. Phys. Ther. 2008, 88, 1254–1264. [Google Scholar] [CrossRef]
- Tentolouris, A.; Eleftheriadou, I.; Athanasakis, K.; Kyriopoulos, J.; Tsilimigras, D.I.; Grigoropoulou, P.; Doupis, J.; Tentolouris, N. Prevalence of diabetes mellitus as well as cardiac and other main comorbidities in a representative sample of the adult Greek population in comparison with the general population. Hell. J. Cardiol. 2020, 61, 15–22. [Google Scholar] [CrossRef]
- GBD 2019 Ageing Collaborators. Global, regional, and national burden of diseases and injuries for adults 70 years and older: Systematic analysis for the Global Burden of Disease 2019 Study. BMJ 2022, 376, e068208. [Google Scholar] [CrossRef] [PubMed]
- Siafarikas, C.; Karamanakos, G.; Makrilakis, K.; Tsolakidis, A.; Mathioudakis, K.; Liatis, S. Prevalence and incidence of medication-treated diabetes and pattern of glucose-lowering treatment during the COVID-19 pandemic: Real-world data from the electronic Greek Prescription Database. Exp. Clin. Endocrinol. Diabetes 2024, 132, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Makrilakis, K.; Kalpourtzi, N.; Ioannidis, I.; Iraklianou, S.; Raptis, A.; Sotiropoulos, A.; Gavana, M.; Vantarakis, A.; Kantzanou, M.; Hadjichristodoulou, C.; et al. Prevalence of diabetes and pre-diabetes in Greece. Results of the First National Survey of Morbidity and Risk Factors (EMENO) study. Diabetes Res. Clin. Pract. 2021, 172, 108646. [Google Scholar] [CrossRef]
- Magriplis, E.; Panagiotakos, D.; Papakonstantinou, E.; Mitsopoulou, A.V.; Karageorgou, D.; Dimakopoulos, I.; Bakogianni, I.; Chourdakis, M.; Micha, R.; Michas, G.; et al. Prevalence of type 2 diabetes mellitus in a representative sample of Greek adults and its association with modifiable risk factors: Results from the Hellenic National Nutrition and Health Survey. Public Health 2021, 197, 75–82. [Google Scholar] [CrossRef]
- Domeikienė, A.; Vaivadaitė, J.; Ivanauskienė, R.; Padaiga, Ž. Direct cost of patients with type 2 diabetes mellitus healthcare and its complications in Lithuania. Medicina 2014, 50, 54–60. [Google Scholar] [CrossRef]
- Hellenic Statistical Authority (ELSTAT). System of Health Accounts 2010—Health Expenditure in Greece 2010–2021. Available online: https://www.statistics.gr/documents/20181/dd86dbea-fd0d-4243-8c5f-9f6fc0447038 (accessed on 23 August 2025).
- World Bank. GDP (Current US$)—Greece. World Development Indicators. Available online: https://data.worldbank.org/indicator/NY.GDP.MKTP.CD?locations=GR (accessed on 23 August 2025).
- OECD. Health Spending (Indicator). OECD Data. Available online: https://data.oecd.org/healthres/health-spending.htm (accessed on 23 August 2025).
- Bommer, C.; Heesemann, E.; Sagalova, V.; Manne-Goehler, J.; Atun, R.; Bärnighausen, T.; Vollmer, S. The global economic burden of diabetes in adults aged 20–79 years: A cost-of-illness study. Lancet Diabetes Endocrinol. 2017, 5, 423–430. [Google Scholar] [CrossRef]
- Hadley, E.C.; Kuchel, G.A.; Newman, A.B.; Allore, H.G.; Bartley, J.M.; Bergeman, C.S.; Blinov, M.L.; Colon-Emeric, C.S.; Dabhar, F.S.; Dugan, L.L.; et al. Report: NIA workshop on measures of physiologic resiliencies in human aging. J. Gerontol. Ser. A 2017, 72, 980–990. [Google Scholar] [CrossRef] [PubMed]
- Ukraintseva, S.; Yashin, A.; Arbeev, K.; Kulminski, A.; Akushevich, I.; Wu, D.; Joshi, G.; Land, K.C.; Stallard, E. Puzzling role of genetic risk factors in human longevity: “risk alleles" as pro-longevity variants. Biogerontology 2016, 17, 109–127. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, J.L.; Stout, M.B.; Sierra, F. Resilience in aging mice. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2016, 71, 1407–1414. [Google Scholar] [CrossRef] [PubMed]
- Varadhan, R.; Walston, J.D.; Bandeen-Roche, K. Can physical resilience and frailty in older adults be linked by the study of dynamical systems? J. Am. Geriatr. Soc. 2018, 66, 1455–1458. [Google Scholar] [CrossRef]
- Hsueh, M.F.; Önnerfjord, P.; Bolognesi, M.P.; Easley, M.E.; Kraus, V.B. Analysis of “old" proteins unmasks dynamic gradient of cartilage turnover in human limbs. Sci. Adv. 2019, 5, eaax3203. [Google Scholar] [CrossRef]
- Sokol, M.C.; McGuigan, K.A.; Verbrugge, R.R.; Epstein, R.S. Impact of medication adherence on hospitalization risk and healthcare cost. Med. Care 2005, 43, 521–530. [Google Scholar] [CrossRef]
- Lunenfeld, B.; Stratton, P. The clinical consequences of an ageing world and preventive strategies. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 643–659. [Google Scholar] [CrossRef]
- Kyrou, I.; Tsigos, C.; Mavrogianni, C.; Cardon, G.; Van Stappen, V.; Latomme, J.; Kivelä, J.; Wikström, K.; Tsochev, K.; Nanasi, A.; et al. Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: A narrative review with emphasis on data from Europe. BMC Endocr. Disord. 2020, 20, 134. [Google Scholar] [CrossRef]
- Vilar-Compte, M.; Burrola-Méndez, S.; Lozano-Marrufo, A.; Ferré-Eguiluz, I.; Flores, D.; Gaitán-Rossi, P.; Teruel, G.; Pérez-Escamilla, R. Urban poverty and nutrition challenges associated with accessibility to a healthy diet: A global systematic literature review. Int. J. Equity Health 2021, 20, 40. [Google Scholar] [CrossRef]
- Qi, Q.; Hu, F.B. Genetics of type 2 diabetes in European populations. J. Diabetes 2012, 4, 203–212. [Google Scholar] [CrossRef]
- Zheng, Q.; Jiang, J.; Huo, Y.; Chen, D. Genetic predisposition to type 2 diabetes is associated with severity of coronary artery disease in patients with acute coronary syndromes. Cardiovasc. Diabetol. 2019, 18, 131. [Google Scholar] [CrossRef]
- Galicia-Garcia, U.; Benito-Vicente, A.; Jebari, S.; Larrea-Sebal, A.; Siddiqi, H.; Uribe, K.B.; Ostolaza, H.; Martín, C. Pathophysiology of type 2 diabetes mellitus. Int. J. Mol. Sci. 2020, 21, 6275. [Google Scholar] [CrossRef] [PubMed]
- Alzaid, A.; Ladrón de Guevara, P.; Beillat, M.; Lehner Martin, V.; Atanasov, P. Burden of disease and costs associated with type 2 diabetes in emerging and established markets: Systematic review analyses. Expert Rev. Pharmacoeconomics Outcomes Res. 2021, 21, 785–798. [Google Scholar] [CrossRef] [PubMed]
- Seuring, T.; Archangelidi, O.; Suhrcke, M. The economic costs of type 2 diabetes: A global systematic review. Pharmacoeconomics 2015, 33, 811–831. [Google Scholar] [CrossRef] [PubMed]
- Bernfort, L.; Husberg, M.; Wiréhn, A.B.; Rosenqvist, U.; Gustavsson, S.; Karlsdotter, K.; Levin, L.Å. Disease burden and healthcare costs for T2D patients with and without established cardiovascular disease in Sweden: A retrospective cohort study. Diabetes Ther. 2020, 11, 1537–1549. [Google Scholar] [CrossRef]
- Butt, M.D.; Ong, S.C.; Wahab, M.U.; Rasool, M.F.; Saleem, F.; Hashmi, A.; Sajjad, A.; Chaudhry, F.A.; Babar, Z.U.D. Cost of illness analysis of type 2 diabetes mellitus: The findings from a lower-middle income country. Int. J. Environ. Res. Public Health 2022, 19, 12611. [Google Scholar] [CrossRef]
- Williams, R.; Van Gaal, L.; Lucioni, C. Assessing the impact of complications on the costs of Type II diabetes. Diabetologia 2002, 45, S13–S17. [Google Scholar] [CrossRef]
- Leśniowska, J.; Schubert, A.; Wojna, M.; Skrzekowska-Baran, I.; Fedyna, M. Costs of diabetes and its complications in Poland. Eur. J. Health Econ. 2014, 15, 653–660. [Google Scholar] [CrossRef]
- Riley, W.J. Health disparities: Gaps in access, quality and affordability of medical care. Trans. Am. Clin. Climatol. Assoc. 2012, 123, 167. [Google Scholar]
- Mullins, C.D.; Blatt, L.; Gbarayor, C.M.; Yang, H.W.K.; Baquet, C. Health disparities: A barrier to high-quality care. Am. J. Health-Syst. Pharm. 2005, 62, 1873–1882. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Siegel, K.R.; Ng, B.P.; Jawanda, S.; Proia, K.K.; Zhang, X.; Albright, A.L.; Zhang, P. Cost-effectiveness of diabetes prevention interventions targeting high-risk individuals and whole populations: A systematic review. Diabetes Care 2020, 43, 1593–1616. [Google Scholar] [CrossRef]
- Siegel, K.R.; Ali, M.K.; Zhou, X.; Ng, B.P.; Jawanda, S.; Proia, K.; Zhang, X.; Gregg, E.W.; Albright, A.L.; Zhang, P. Cost-effectiveness of interventions to manage diabetes: Has the evidence changed since 2008? Diabetes Care 2020, 43, 1557–1592. [Google Scholar] [CrossRef] [PubMed]
- Waldeyer, R.; Brinks, R.; Rathmann, W.; Giani, G.; Icks, A. Projection of the burden of type 2 diabetes mellitus in Germany: A demographic modelling approach to estimate the direct medical excess costs from 2010 to 2040. Diabet. Med. 2013, 30, 999–1008. [Google Scholar] [CrossRef] [PubMed]
| N | Total population |
| p | Prevalence of T2D |
| T | Number of people suffering from T2D computed as |
| Proportion of patients who receive treatment i | |
| Number of patients who receive treatment i computed as | |
| Cost of treatment i | |
| Total cost of treatment i computed as | |
| Total annual cost computed as the sum of the total costs of all treatments | |
| Cost of complication j related to T2D | |
| Total annual cost of T2D-related complications computed as the sum of the costs of all complications | |
| Cost of medical examination k for monitoring related to T2D | |
| Total annual cost of T2D-related medical examinations computed as the sum of the costs of all medical examinations | |
| Total annual cost of T2D-related general practitioners’ consultations | |
| Total annual cost of T2D computed as |
| Greek Population in 2021 | 10,482,487 | Greek Population in 2030 | 9,721,983 | Greek Population in 2030 | 9,721,983 |
|---|---|---|---|---|---|
| Number of People with T2D | 1,195,004 | Number of People with Type T2D | 1,108,306 | Number of People with T2D, After Considering the Aging Effect | 1,241,837 |
| Distribution of patients into lines of treatments | Distribution of patients into lines of treatments | Distribution of patients into lines of treatments | |||
| First line | 31% | First line | 31% | First line | 31% |
| Second line | 45% | Second line | 45% | Second line | 45% |
| Third line | 23% | Third line | 23% | Third line | 23% |
| Fourth line | 1% | Fourth line | 1% | Fourth line | 1% |
| Number of patients in each line of treatment | Number of patients in each line of treatment | Number of patients in each line of treatment | |||
| First line | 370,451 | First line | 343,575 | First line | 384,969 |
| Second line | 537,752 | Second line | 498,738 | Second line | 558,827 |
| Third line | 274,851 | Third line | 254,910 | Third line | 285,623 |
| Fourth line | 11,950 | Fourth line | 11,083 | Fourth line | 12,418 |
| 30-day cost for each line of treatment | 30-day cost for each line of treatment | 30-day cost for each line of treatment | |||
| First line | EUR 461,211 | First line | EUR 444,861 | First line | EUR 498,458 |
| Second line | EUR 15,284,320 | Second line | EUR 14,742,458 | Second line | EUR 16,518,660 |
| Third line | EUR 15,281,781 | Third line | EUR 14,739,979 | Third line | EUR 16,515,935 |
| Fourth line | EUR 1,043,175 | Fourth line | EUR 1,006,190 | Fourth line | EUR 1,127,390 |
| Total annual cost for diabetes-related treatment lines | EUR 384,845,856 | Total annual cost for diabetes-related treatment lines | EUR 371,201,853 | Total annual cost for diabetes-related treatment lines | EUR 415,925,321 |
| Greek Population in 2021 | 10,482,487 | Greek Population in 2030 | 9,721,983 | Greek Population in 2030 | 9,721,983 |
|---|---|---|---|---|---|
| Number of People with T2D | 857,467 | Number of People with Type T2D | 795,258 | Number of People with T2D, After Considering the Aging Effect | 1,241,837 |
| Distribution of patients into line of treatments | Distribution of patients into line of treatments | Distribution of patients into line of treatments | |||
| First line | 31% | First line | 31% | First line | 31% |
| Second line | 45% | Second line | 45% | Second line | 45% |
| Third line | 23% | Third line | 23% | Third line | 23% |
| Fourth line | 1% | Fourth line | 1% | Fourth line | 1% |
| Number of patients in each line of treatment | Number of patients in each line of treatment | Number of patients in each line of treatment | |||
| First line | 265,815 | First line | 246,530 | First line | 384,969 |
| Second line | 385,860 | Second line | 357,866 | Second line | 558,827 |
| Third line | 197,218 | Third line | 182,909 | Third line | 285,623 |
| Fourth line | 8575 | Fourth line | 7953 | Fourth line | 12,418 |
| 30-day cost for each line of treatment | 30-day cost for each line of treatment | 30-day cost for each line of treatment | |||
| First line | EUR 330,940 | First line | EUR 319,207 | First line | EUR 498,458 |
| Second line | EUR 10,967,152 | Second line | EUR 10,578,349 | Second line | EUR 16,518,660 |
| Third line | EUR 10,965,368 | Third line | EUR 10,576,575 | Third line | EUR 16,515,935 |
| Fourth line | EUR 748,555 | Fourth line | EUR 722,027 | Fourth line | EUR 1,127,390 |
| Total annual cost for diabetes-related treatment lines | EUR 255,975,189.49 | Total annual cost for diabetes-related treatment lines | EUR 266,353,899.84 | Total annual cost for diabetes-related treatment lines | EUR 415,925,321 |
| 2021 | 2030 | 2030 * | ||
|---|---|---|---|---|
| Number of people with T2D | 1,195,004 | 1,108,306 | 1,241,837 | |
| Number of T2D patients with complications | 167,355 | 155,213 | 174,603 | |
| Estimated number of T2D patients with recommended frequency of examinations | 597,502 | 554,153 | 620,919 | |
| T2D-related complications | Cost per T2D-related complication | Total annual cost of T2D-related complications | ||
| Diabetic complications with devastating comorbidities/complications | EUR 6202.00 | EUR 507,957,079 | EUR 489,947,893 | EUR 551,152,722 |
| Diabetic complications without catastrophic comorbidities/complications | EUR 2801.00 | |||
| Endoscopic or exploratory procedures for metabolic dysfunctions on the same day | EUR 297.00 | |||
| Endoscopic or exploratory procedures for metabolic dysfunctions with devastating comorbidities/complications | EUR 4296.00 | |||
| Endoscopic or exploratory procedures for metabolic dysfunctions without catastrophic comorbidities/complications | EUR 1580.00 | |||
| T2D-related medical examinations for monitoring | Cost per T2D-related medical examination for monitoring | Total annual cost of T2D-related medical examinations for monitoring | ||
| SGPT-SGOT levels (2 times/year) | EUR 6.98 | EUR 397,517,920 | EUR 383,425,132 | EUR 429,620,961 |
| HbA1c levels (4 times/year) | EUR 24.64 | |||
| Determination of blood sugar/glucose (GL) (2 times/year) | EUR 4.00 | |||
| Levels of sodium, potassium and phosphorus in blood (2 times/year) | EUR 8.00 | |||
| General blood test (2 times/year) | EUR 5.76 | |||
| Creatinine levels in blood (2 times/year) | EUR 7.60 | |||
| Triglycerides levels in blood (4 times/year) | EUR 13.96 | |||
| Cholesterol levels in blood (4 times/year) | EUR 8.80 | |||
| Urea levels in blood (2 times/year) | EUR 4.00 | |||
| HDL-cholesterol levels in blood (4 times/year) | EUR 16.00 | |||
| Uric acid levels in blood (2 times/year) | EUR 4.00 | |||
| LDL-cholesterol levels in blood (4 times/year) | EUR 16.00 | |||
| General urea test (2 times/year) | EUR 3.52 | |||
| gGt levels in blood (2 times/year) | EUR 8.00 | |||
| TKE erythrocyte sedimentation rate blood test (2 times/year) | EUR 3.52 | |||
| CPK levels in blood (2 times/year) | EUR 10.04 | |||
| ALP levels in blood (2 times/year) | EUR 8.00 | |||
| Calcium levels in blood (2 times/year) | EUR 6.00 | |||
| TSH levels in blood (2 times/year) | EUR 22.00 | |||
| Urine culture (4 times/year) | EUR 20.88 | |||
| Free thyroxine (FT4) (2 times/year) | EUR 24.00 | |||
| Ultrasound (u/s) of upper abdomen (liver, which includes gallbladder, pancreas, spleen) (3 times/year) | EUR 62.70 | |||
| Doppler spectrum ultrasound and color flow imaging (once per year) | EUR 85.00 | |||
| Triplex-ultrasound arteriography: carotid and vertebral arteries in color (once per year) | EUR 60.00 | |||
| Insulin levels (Once per year) | EUR 12.38 | |||
| Triplex-Color ultrasound arteriography of the lower extremities (once per year) | EUR 44.00 | |||
| Free thyroxine (FT3) (2 times/year) | EUR 24.00 | |||
| Ultrasound (u/s) of kidneys, ureters, and bladder, prostate—males (2 times/year) | EUR 12.62 | |||
| Ultrasound (u/s) of thyroid gland/parathyroid (once per year) | EUR 8.28 | |||
| C-peptide levels (2 times/year) | EUR 19.02 | |||
| Ultrasound (u/s) of kidneys, ureters, and bladder, uterus, ovaries, fallopian tubes—females (2 times/year) | EUR 16.56 | |||
| Triplex-color aortic ultrasound arteriography (ascending aorta and aortic arch) (once per year) | EUR 44.00 | |||
| Bottomoscopy with a GOLDMAN tricopter contact lens (once per year) | EUR 7.04 | |||
| Triplex-color ultrasound arteriography of iliac arteries (once per year) | EUR 44.00 | |||
| Total annual cost of T2D-related complications and T2D-related medical examinations for monitoring | EUR 905,475,000 | EUR 873,373,025 | EUR 980,773,683 | |
| 2021 | 2030 | 2030 * | ||
|---|---|---|---|---|
| Number of people with T2D | 857,467 | 795,258 | 1,241,837 | |
| Number of T2D patients with complications | 120,560 | 111,813 | 174,603 | |
| Estimated number of T2D patients with recommended frequency of examinations | 428,734 | 397,629 | 620,919 | |
| T2D-related complications | Cost per T2D-related complication | Total annual cost of T2D-related complications | ||
| Diabetic complications with devastating comorbidities/complications | EUR 6202.00 | EUR 365,923,474 | EUR 352,950,771 | EUR 551,152,722 |
| Diabetic complications without catastrophic comorbidities/complications | EUR 2801.00 | |||
| Endoscopic or exploratory procedures for metabolic dysfunctions on the same day | EUR 297.00 | |||
| Endoscopic or exploratory procedures for metabolic dysfunctions with devastating comorbidities/complications | EUR 4296.00 | |||
| Endoscopic or exploratory procedures for metabolic dysfunctions without catastrophic comorbidities/complications | EUR 1580.00 | |||
| T2D-related medical examinations for monitoring | Cost per T2D-related medical examination for monitoring | Total annual cost of T2D-related medical examinations for monitoring | ||
| SGPT-SGOT levels (2 times/year) | EUR 6.98 | EUR 285,236,543 | EUR 275,124,349 | EUR 429,620,961 |
| HbA1c levels (4 times/year) | EUR 24.64 | |||
| Determination of blood sugar/glucose (GL) (2 times/year) | EUR 4.00 | |||
| Levels of sodium, potassium and phosphorus in blood (2 times/year) | EUR 8.00 | |||
| General blood test (2 times/year) | EUR 5.76 | |||
| Creatinine levels in blood (2 times/year) | EUR 7.60 | |||
| Triglycerides levels in blood (4 times/year) | EUR 13.96 | |||
| Cholesterol levels in blood (4 times/year) | EUR 8.80 | |||
| Urea levels in blood (2 times/year) | EUR 4.00 | |||
| HDL-cholesterol levels in blood (4 times/year) | EUR 16.00 | |||
| Uric acid levels in blood (2 times/year) | EUR 4.00 | |||
| LDL-cholesterol levels in blood (4 times/year) | EUR 16.00 | |||
| General urea test (2 times/year) | EUR 3.52 | |||
| gGt levels in blood (2 times/year) | EUR 8.00 | |||
| TKE erythrocyte sedimentation rate blood test (2 times/year) | EUR 3.52 | |||
| CPK levels in blood (2 times/year) | EUR 10.04 | |||
| ALP levels in blood (2 times/year) | EUR 8.00 | |||
| Calcium levels in blood (2 times/year) | EUR 6.00 | |||
| TSH levels in blood (2 times/year) | EUR 22.00 | |||
| Urine culture (4 times/year) | EUR 20.88 | |||
| Free thyroxine (FT4) (2 times/year) | EUR 24.00 | |||
| Ultrasound (u/s) of upper abdomen (liver, which includes gallbladder, pancreas, spleen) (3 times/year) | EUR 62.70 | |||
| Doppler spectrum ultrasound and color flow imaging (once per year) | EUR 85.00 | |||
| Triplex-Ultrasound arteriography: carotid and vertebral arteries in color (once per year) | EUR 60.00 | |||
| Insulin levels (Once per year) | EUR 12.38 | |||
| Triplex-color ultrasound arteriography of the lower extremities (once per year) | EUR 44.00 | |||
| Free thyroxine (FT3) (2 times/year) | EUR 24.00 | |||
| Ultrasound (u/s) of kidneys, ureters, and bladder, prostate—males (2 times/year) | EUR 12.62 | |||
| Ultrasound (u/s) of thyroid gland/parathyroid (once per year) | EUR 8.28 | |||
| C-peptide levels (2 times/year) | EUR 19.02 | |||
| Ultrasound (u/s) of kidneys, ureters, and bladder, uterus, ovaries, fallopian tubes—females (2 times/year) | EUR 16.56 | |||
| Triplex-Color aortic ultrasound arteriography (ascending aorta and aortic arch) (once per year) | EUR 44.00 | |||
| Bottomoscopy with a GOLDMAN tricopter contact lens (once per year) | EUR 7.04 | |||
| Triplex-color ultrasound arteriography of iliac arteries (once per year) | EUR 44.00 | |||
| Total annual cost of T2D-related complications and T2D-related medical examinations for monitoring | EUR 651,160,013 | EUR 628,075,120 | EUR 980,773,683 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Market Access Society. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nika, E.; Tsiampalis, T.; Sachlas, A.; Liberopoulos, E.; Bersimis, S.; Georgakellos, D. A Data-Driven Approach for Estimating Type 2 Diabetes-Related Costs in Greece. J. Mark. Access Health Policy 2025, 13, 53. https://doi.org/10.3390/jmahp13040053
Nika E, Tsiampalis T, Sachlas A, Liberopoulos E, Bersimis S, Georgakellos D. A Data-Driven Approach for Estimating Type 2 Diabetes-Related Costs in Greece. Journal of Market Access & Health Policy. 2025; 13(4):53. https://doi.org/10.3390/jmahp13040053
Chicago/Turabian StyleNika, Elisavet, Thomas Tsiampalis, Athanasios Sachlas, Evangelos Liberopoulos, Sotirios Bersimis, and Dimitrios Georgakellos. 2025. "A Data-Driven Approach for Estimating Type 2 Diabetes-Related Costs in Greece" Journal of Market Access & Health Policy 13, no. 4: 53. https://doi.org/10.3390/jmahp13040053
APA StyleNika, E., Tsiampalis, T., Sachlas, A., Liberopoulos, E., Bersimis, S., & Georgakellos, D. (2025). A Data-Driven Approach for Estimating Type 2 Diabetes-Related Costs in Greece. Journal of Market Access & Health Policy, 13(4), 53. https://doi.org/10.3390/jmahp13040053






