Cognitive Training for the Treatment of Addictions Mediated by Information and Communication Technologies (ICT)
Abstract
1. Introduction
Theoretical Basis
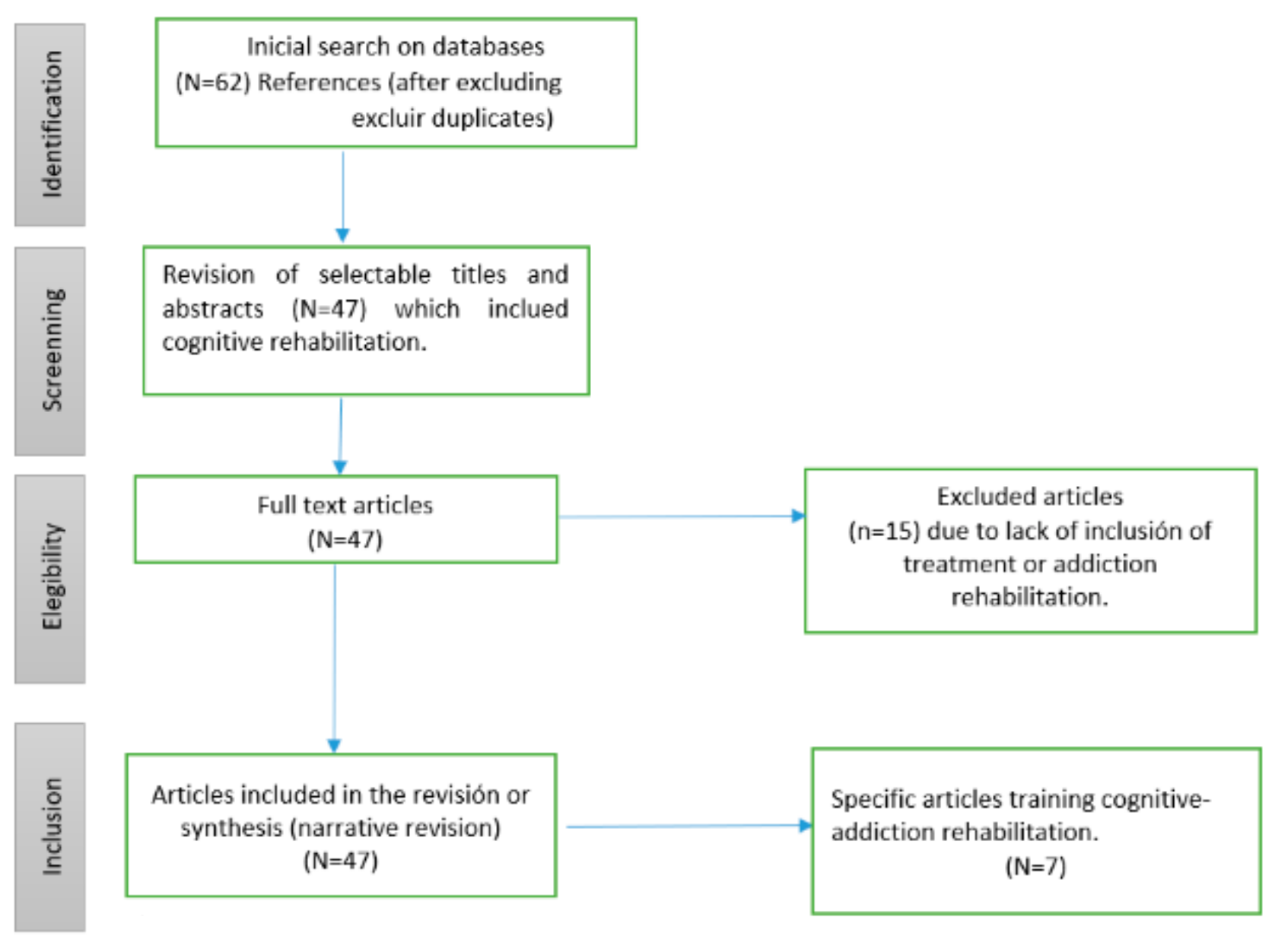
2. Materials and Methods
2.1. Criteria to Select Revision Studies
2.2. Revision Methods
2.3. Cognitive Training and ICT
2.4. Neuropsychological Rehabilitation for Addictions
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- UNODC. Informe Mundial Sobre las Drogas 2011; Naciones Unidas: New York, NY, USA, 2011. (In Spanish) [Google Scholar]
- Ministerio de la Protección Social. Decreto 3039 de 2007, Por el Cual se Adopta el Plan Nacional de Salud Pública 2007–2010; No. 46716; Diario Oficial: Bogotá, Colombia, 2007. (In Spanish)
- Ministerio de Justicia, Ministerio de Salud y Protección Social. Estudio Nacional de Consumo de Sustancias Psicoactivas en Colombia; Ministerio de Justicia, Ministerio de Salud y Protección Social: Bogotá, Colombia, 2013. (In Spanish)
- García Fernández, G.; García Rodríguez, O.; Secades Villa, R. Neuropsicología y Adicción a Drogas. Grupo de Conductas Adictivas. Pap. Psicól. 2011, 32, 159–165. (In Spanish) [Google Scholar]
- Goodman, A. Neurobiology of addiction. An integrative review. Biochem. Pharm. 2008, 75, 266–322. [Google Scholar] [CrossRef]
- Garavan, H.; Stout, J.C. Neurocognitive insights into substance abuse. Trends Cogn. Sci. 2005, 9, 195–201. [Google Scholar] [CrossRef]
- Yucel, M.; Lubman, D.I. Neurocognitive and neuroimaging evidence of behavioural dysregulation in human drug addiction: Implications for diagnosis, treatment and prevention. Drug Alcohol Rev. 2007, 26, 33–39. [Google Scholar] [CrossRef]
- Pedrero-Pérez, E.J.; López-Durán, A.; Olivar-Arroyo, A. Addiction: Frontal personality change but not personality disorder comorbidity. Implications for treatment of addictive disorders. In Personality Traits Theory, Testing and Influences; Jordan, M.E., Ed.; Nova Science Publishers: New York, NY, USA, 2010; pp. 1–36. [Google Scholar]
- Sinha, R. How does stress increase risk of drug abuse and relapse? Psychopharmacology 2001, 158, 343–359. [Google Scholar] [CrossRef]
- Tice, D.M.; Bratslavsky, E.; Baumeister, R.F. Emotional distress regulation takes precedence over impulse control: If you feel bad, do it! J. Pers. Soc. Psychol. 2001, 80, 53–67. [Google Scholar] [CrossRef]
- Yücel, M.; Lubman, D.I.; Solowij, N.; Brewer, W.J. Understanding drug addiction: A neuropsychological perspective. Aust. N. Z. J. Psychiatry 2007, 41, 957–968. [Google Scholar] [CrossRef]
- Bolla, K.; Ernst, M.; Kiehl, K.; Mouratidis, M.; Eldreth, B.A.; Contoreggi, M.D.; Matochik, J.; Kurian, M.S.; Cadet, J.; Kimes, A.; et al. Prefrontal Cortical Dysfunction in Abstinent Cocaine Abusers. J. Neuropsychiatry Clin. Neurosci. 2004, 16, 456–464. [Google Scholar] [CrossRef]
- Robinson, T.E.; Berridge, K.C. Addiction. Annu. Rev. Psychol. 2003, 54, 25–53. [Google Scholar] [CrossRef]
- Verdejo-García, A.; Bechara, A. Neuropsicología y Drogodependencias: Evaluación, Impacto Clínico y Aplicaciones Para la Rehabilitación. In Manual de neuropsicología clínica; En, M., Pérez, G., Eds.; Madrid Pirámide: Madrid, Spain, 2009; pp. 179–208. (In Spanish) [Google Scholar]
- Verdejo García, A.; Pérez García, M.; Bechara, A. Emotion, decision-making and substance dependence: A somatic-marker model of addiction. Curr. Neuropharmacol. 2006, 4, 17–31. [Google Scholar] [CrossRef]
- Rojo-Mota, G.; Pedrero Pérez, E.J.; Ruiz Sánchez de León, J.M.; Llanero-Luque, M.; Olivar-Arroyo, Á.; Puerta-García, C. Terapia Ocupacional en la rehabilitación de la disfunción ejecutiva en adictos a sustancias. Trastor. Adict. 2009, 11, 96–105. (In Spanish) [Google Scholar] [CrossRef]
- Stetler, C.B.; Morsi, D.; Rucki, S. Utilization-focused integrative reviews in a nursing service. Appl. Nurs. Res. 1998, 11, 195–206. [Google Scholar] [CrossRef]
- Mateer, C.A.; Sira, C.S. Cognitive and emotional consequences of TBI: Intervention strategies for vocational rehabilitation. NeuroRehabilitation 2006, 21, 315–326. [Google Scholar] [CrossRef] [PubMed]
- Sohlberg, M.M.; Mateer, C.A. Cognitive Rehabilitation: An Integrative Neuropsychological Approach; Guilford Press: New York, NY, USA, 2001. [Google Scholar]
- Suárez-Yepes, N.; Quiroz-Molinares, N.; Monachello-Fuentes, F.M.; De-los-Reyes-Aragón, C.J. Rehabilitación neuropsicológica infantil: De la teoría a la práctica clínica. Arch. Med. 2016, 16, 455–466. (In Spanish) [Google Scholar] [CrossRef]
- Woods, B.; Thorgrimsen, L.; Spector ARoyan, L.; Orrell, M. Improved quality of life and cognitive stimulation therapy in dementia. Aging Ment. Health 2006, 10, 219–226. [Google Scholar] [CrossRef]
- Clare, L.; Woods, R.T. Cognitive rehabilitation and cognitive training for early stage Alzheimer’s disease and vascular dementia. Neuropsychol. Rehabil. 2004, 14, 385–401. [Google Scholar] [CrossRef]
- Holderbaum, C.S.; Rinaldi, J.; Brandão, L.; Parente, M.A.M.P. A intervenção cognitiva para pacientes portadores de demência do tipo Alzheimer. In Cognição e Envelhecimento; Parente, M.A.M.P., Ed.; Artmed: Porto Alegre, Brasil, 2006; pp. 260–273. (In Spanish) [Google Scholar]
- Lopes, R.M.F.; Argimon, I.I.L. Cognitive training in the elderly and its effect on the executive functions. Acta Colomb. Psicol. 2016, 19, 177–197. [Google Scholar] [CrossRef]
- Salthouse, T.A. The processing-speed theory of adult age differences in cognition. Psychol. Rev. 1996, 103, 403–428. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, L.; Giovanello, K. Executive function in daily life: Age-related influences of executive processes on instrumental activities of daily living. Psychol. Aging 2010, 25, 343–355. [Google Scholar]
- Fernández-Calvo, B.; Rodríguez-Pérez, R.; Contador, I.; Rubio-Santorum, A.; Ramos, F. Eficacia del entrenamiento cognitivo basado en nuevas tecnologías en pacientes con demencia tipo Alzheimer. Psicothema 2011, 23, 44–50. (In Spanish) [Google Scholar] [PubMed]
- Muñoz González, D.A. La estimulación cognitiva como estrategia para la atención psicogerontológica a los adultos mayores con demencia. Rev. Cuba. Salud Pública 2018, 44, 1–8. (In Spanish) [Google Scholar]
- Muñoz-Céspedes, J.; Tirapu-Ustárroz, J. Rehabilitación de las funciones ejecutivas. Rev. Neurol. 2004, 38, 656–663. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Lubrini, G.; Periáñez, J.; Ríos-Lago, M. Introducción a la estimulación cognitiva y la rehabilitación neuropsicológica. In Estimulación Cognitiva y Rehabilitación Neuropsicológica; Editorial UOC: Barcelona, Spain, 2009; pp. 13–32. (In Spanish) [Google Scholar]
- Portellano, J. Cómo desarrollar la inteligencia. In Entrenamiento Neuropsicológico de la Atención y Las Funciones Ejecutivas; Somos Psicología: Madrid, Spain, 2005. (In Spanish) [Google Scholar]
- Elliott, M.; Parente, F. Efficacy of memory rehabilitation therapy: A meta-analysis of TBI and stroke cognitive rehabilitation literature. Brain Inj. 2014, 28, 1610–1616. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.H.; Kim, K.M. Virtual reality for cognitive rehabilitation after brain injury: A systematic review. J. Phys. Ther. Sci. 2015, 27, 2999–3002. [Google Scholar] [CrossRef]
- Coyle, H.; Traynor, V.; Solowij, N. Computerized and virtual reality cognitive training for individuals at high risk of cognitive decline: Systematic review of the literature. Am. J. Geriatr. Psychiatry 2015, 23, 335–359. [Google Scholar] [CrossRef]
- Al Ayubi, S.; Parmanto, B.; Branch, R.; Ding, D. A persuasive andsocial mHealth application for physical activity: A usability andfeasibility study. JMU 2014, 2, 17. [Google Scholar]
- Depompei, R.; Gillette, Y.; Goetz, E.; Xenopoulos, O.; Bryen, D.; Dowds, M. Practical applications for use of PDAs and smartphonewith children and adolescents who have traumatic brain injury. Neurorehabilitation 2008, 23, 487–499. [Google Scholar] [CrossRef]
- Migo, E.M.; Haynes, B.I.; Harris, L.; Friedner, K.; Humphreys, K.; Kopelman, M.D. mHealth and memory aids: Levels ofsmartphone ownersphip in patients. J. Ment. Health 2014, 4, 1–18. [Google Scholar]
- Cicerone, K.D.; Dahlberg, C.; Kalmar, K.; Langenbahn, D.M.; Malec, J.F.; Bergquist, T.F. Evidence-based cognitive rehabilitation: Recommendations for clinical practice. Arch. Phys. Med. Rehabil. 2000, 81, 1596–1615. [Google Scholar] [CrossRef]
- Schutz, L.E.; Trainor, K. Evaluation of cognitive rehabilitation as a treatment paradigm. Brain Inj. 2007, 31, 545–557. [Google Scholar] [CrossRef]
- Laatsch, L.; Harrington, D.; Hotz, G.; Marcantuono, J.; Mozzoni, M.P.; Wals, V.; Hersey, K.P. An evidence-based review of cognitive and behavioral rehabilitation treatment studies in children with acquired brain injury. J. Head Trauma Rehabil. 2007, 22, 248–256. [Google Scholar] [CrossRef] [PubMed]
- McGurk, S.R.; Twamley, E.W.; Sitzer, D.I.; McHugo, G.J.; Mueser, K.T. A meta-analysis of cognitive remediation in schizophrenia. Am. J. Psychiatry 2007, 164, 1791–1802. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, A.R.; Chiaravalloti, N.; Goverover, Y.; DeLuca, J. Evidenced-based cognitive rehabilitation for persons with multiple sclerosis: A review of the literature. Arch. Phys. Med. Rehabil. 2008, 89, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Wykes, T.; Brammer, M.; Mellers, J.; Bray, P.; Reeder, C.; Williams, C.; Corner, J. Effects on the brain of a psychological treatment: Cognitive remediation therapy. Functional magnetic resonance imaging in schizophrenia. Br. J. Psychiatry 2002, 181, 144–152. [Google Scholar] [CrossRef]
- Goldstein, R.Z.; Leskovjan, A.C.; Hoff, A.L.; Hitzemann, R.; Bashan, F.; Khalsa, S.S.; Wang, G.J.; Fowler, J.S.; Volkow, N.D. Severity of neuropsychological impairment in cocaine and alcohol addiction: Association with metabolism in the prefrontal cortex. Neuropsychologia 2004, 42, 1447–1458. [Google Scholar] [CrossRef]
- Roehrich, L.; Goldman, M.S. Experience-dependent neuropsychological recovery and the treatment of alcoholism. J. Consult. Clin. Psychol. 1993, 61, 812–821. [Google Scholar] [CrossRef]
- Allen, D.N.; Goldstein, G.; Seaton, B.E. Cognitive rehabilitation of chronic alcohol abusers. Neuropsychol. Rev. 1997, 7, 21–39. [Google Scholar] [CrossRef]
- Fals-Stewart, W.; Lam, W.K.K. Computer-assisted cognitive rehabilitation for the treatment of patients with substance use disorders: A randomized clinical trial. Exp. Clin. Psychopharmacol. 2010, 18, 87–98. [Google Scholar] [CrossRef]
- Fei, Y.; Jörg, A.; Tian, G.; Minghao, W.; Arne, B.; Elsebeth, S. A smartphone application of alcohol resilience treatment for behavioral self-control training. In En 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society; IEEE: Piscataway, PA, USA, 2012; pp. 1976–1979. [Google Scholar]
- Bickel, W.K.; Moody, L.; Quisenberry, A. Computerized working-memory training as a candidate adjunctive treatment for addiction. Alcohol Res. Curr. Rev. 2014, 36, 123. [Google Scholar]
- Ahn, W.Y.; Vasilev, G.; Lee, S.-H.; Busemeyer, J.R.; Kruschke, J.K.; Bechara, A.; Vassileva, J. Decision-making in stimulant and opiate addicts in protracted abstinence: Evidence from computational modeling with pure users. Front. Psychol. 2014, 5, 849. [Google Scholar] [CrossRef]
- Ruiz-Manrique, G.; Tajima-Pozo, K.; Montañes-Rada, F. Case Report: “ADHD Trainer”: The mobile application that enhances cognitive skills in ADHD patients. F1000 Res. 2014, 3, 283. [Google Scholar] [CrossRef]
- Kapitány-Fövény, M. Potential of an Interactive Drug Prevention Mobile Phone App (Once Upon a High): Questionnaire Study Among Students. JMIR Serious Games 2018, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.A. Newly Designed Mobile-Based Computerized Cognitive Addiction Therapy APP for the Improvement of Cognition Impairments and Risk Decision Making in Methamphetamine Use Disorder: Randomized Controlled Trial. JMIR mHealth uHealth 2018, 6, e10292. [Google Scholar] [CrossRef] [PubMed]
- Kiluk, B.D.; Ray, L.A.; Walthers, J.; Bernstein, M.; Tonigan, J.S.; Magill, M. Technology-Delivered Cognitive-Behavioral Interventions for Alcohol Use: A Meta-Analysis. Alcoholism. Clin. Exp. Res. 2019, 43, 2285–2295. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Rodríguez, M.T.; Collado-Vázquez, S.; Martín-Casas, P.; de la Cuerda, C. APPs en neurorrehabilitación. Una revisión sistemática de aplicaciones móviles. Neurología 2018, 33, 313–326. (In Spanish) [Google Scholar] [CrossRef]
- Fernández-Salazar, S.; Ramos-Morcillo, A.J. Nuevas tecnologías, apps y su aplicación en la práctica clínica basada en evidencias. Enferm. Clin. 2014, 24, 99–101. (In Spanish) [Google Scholar] [CrossRef]
- Shuren, J. The FDA’s role in the development of medical mobile applications. Clin. Pharmacol. Ther. 2014, 95, 485–488. [Google Scholar] [CrossRef]
- FDA. La FDA Expide Guía Final Sobre las Aplicaciones Médicas Móviles. 2013. Available online: https://www.fda.gov/media/80958/download (accessed on 18 November 2019).
- Meulendijk, M.; Meulendijks, J.; Paul, A.; Edwin, N.; Mattijs, E.; Marco, R. What Concerns Users of Medical APPs? Exploring non-Functional Requirements of Medical Mobile Applications. Available online: https://pdfs.semanticscholar.org/5a8c/d9dd8e5175eb0b7a8f52e315ae46b62e762a.pdf (accessed on 18 November 2019).
- Pedrero-Pérez, E.J.; Rojo-Mota, G.; Ruiz-Sánchez de León, J.M.; Llanero-Luque, M.; Puerta-García, C. Rehabilitación cognitiva en el tratamiento de las adicciones. Rev. Neurol. 2011, 52, 163–172. (In Spanish) [Google Scholar] [CrossRef]
| Authors | Year | Method | Key Findings | Conclusions |
|---|---|---|---|---|
| Mateer et al. [18] | 2006 | Case studies and Literature review | Cognitive rehabilitation strategies that address attention, memory and executive deficits can improve clients’ abilities to manage workplace tasks and demands. | Cognitive behavioural therapy is well suited for improving coping skills, helping clients to manage cognitive difficulties and addressing more generalized anxiety and depression in the context of a brain injury. |
| Sohlberg et al. [19] | 2001 | Literature review | The rehabilitation is a group of treatments that include cognitive process training, environmental manipulations and psychotherapy. | Approaches covered encompass behavioral interventions, process-oriented therapies, including cognitive process training, environmental manipulations and psychotherapy. |
| Suárez-Yepes et al. [20] | 2016 | Literature review | From the theoretical review, it was found that the restorative approach is the predominant in the vast majority of interventions reported in the literature. | It was found that very few studies reported clearly and precisely whether there existed improvements in the functionality of the participants. Similarly, few studies reported the inclusion of the family in rehabilitation. |
| Woods et al. [21] | 2006 | Randomized controlled trial of Cognitive Stimulation Therapy (CST) groups, significant improvements in self-reported QoL 201 people with dementia living in residential homes or attending day centres were assessed using the Quality of Life-Alzheimer’s Disease (QOL-AD) scale and a range of measures of cognition, dementia level, mood, dependency and communication. | At baseline, higher QoL in dementia was significantly correlated with lower levels of dependency and depression, but not with cognitive function or dementia severity. Improvement in quality of life was associated with being female, low quality of life at baseline, reduced depression and increased cognitive function. | Changes in cognitive function mediated the effects of treatment in improving QoL. These results suggest that while QoL in dementia appears to be independent of level of cognitive function, interventions aimed at improving cognitive function can, nonetheless, have a direct effect on QoL. |
| Clare et al. [22] | 2004 | Literature review | Six studies reporting cognitive training interventions were included. None of studies demonstrated any statistically significant effects in any domain, although there were indications of some modest, non-significant effects in various domains of cognitive functioning. | Data from a single, high-quality trial provide preliminary positive Results regarding the use of contextualised individual cognitive rehabilitation. |
| Holderbaum et al. [23] | 2006 | This is a quantitative research that used a quasi-experimental design; it is correlational and comparative, involving pre- and post-testing and intervention. The sample was formed by 83 elders, split into an Experimental Group (EG) (45 people) and a Control Group (GC) (38 people). | The results from the comparison between groups showed that there was a significant difference regarding the number of errors in the Sternberg Paradigm and Completed Categories of the WCST. Intragroup comparisons showed that the EG had better results after the intervention on the following tests: GDS, RAVLT, Rey Complex Figures (memory), Digit Span and Vocabulary. | Aging is commonly associated to cognitive decline and loss of other abilities, which leads to the need of researching elements that may contribute to preventive cognitive rehabilitation interventions aiming to guarantee the elderly quality of life. |
| Lopes et al. [24] | 2016 | Quantitative research that used a quasi-experimental design; it is correlational and comparative, involving pre- and posttesting and intervention. The sample was formed by 83 elders, split into an Experimental Group (EG) (45 people) and a Control Group (GC) (38 people). | Significant differences were evidenced between the groups regarding health problems (p = 0.048) and physical activity (p = 0.033). People older in the experimental group were more prone to present diseases, but they also practiced more physical activities that the control group.The GC reduces the number of errors in the paradigm more than the GE, and also significantly changes the weighted score of the Search for Symbols. | The results presented here show the effect of executive training in improving executive function (FE [acronym in Spanish]), which includes the Processing speed. Both the FE and the speed of processing decrease with age [25] Daily activities are strongly related to these functions [26]. |
| Fernández-Calvo et al. [27] | 2011 | The study aims to assess the effi cacy of the Big Brain Academy (BBA), a computerized cognitive training program (CT) based on video games, compared to the Integrated Psychostimulation Program (IPP), a classical CT tool for patients with Alzheimer’s disease (AD). A total of 45 patients with AD at the mild stage were randomly assigned to three experimental conditions. | The EABB group showed signifi cantly slower rates of cognitive decline compared to the EAPI and EANT groups. Furthermore, the EABB group reported significantly greater decrease in depressive symptoms in comparison with the EAPI and EANT groups. The BBA program was more effective than IPP to reduce cognitive decline and depressive symptoms in patients with AD. | The results obtained show that the BBA cognitive stimulation program has proved more effective than a Traditional CD program (PPI), so that patients stimulated with BBA showed a significant reduction of cognitive decline and depressive symptomatology in relation to a ‘traditional’ stimulation group. |
| Muñoz González [28] | 2018 | Review | The purpose is to inform about the benefit of cognitive stimulation as a preventive, economic and effective strategy for the psychogerontological approach of patients with dementia in primary health care. | Cognitive stimulation will improve the quality of life of older adults with dementia and promote individual and family coping with the disease. |
| Muñoz-Céspedes et al. [29] | 2004 | Literatures review | The aim of this report is to review the main rehabilitation programs of executive functions and to adapt them to our culture and context from a theoretical-practice perspective. | New ones are needed research that helps us determine the differential effectiveness of some techniques and programs in different groups of patients with alterations in executive functioning. However, the initial results of some recent studies in this direction they are promising. |
| Lubrini et al. [30] | 2009 | Compilation | An intervention process is fundamental to know the in-depth basic theoretical aspects about the memory process to be able to design an appropriate intervention plan. | It is necessary for patients to master the characteristics of the possible mnesic alterations, to know how to evaluate them and how to assess those preserved capabilities. |
| Portellano [31] | 2005 | Literature review | The empirical concept of “function executive” derived mainly from study of patients and animals with lesions in the prefrontal cortex, especially in the dorsolateral portion. | Restoration, recovery and retraining are based on the principle that the practice or repetition of exercises can strengthen the basic cognitive process or function, as well as progressively improve those functions that present some difficulty. |
| Elliott et al. [32] | 2014 | Meta-analysis was performed on 26 studies of memory retraining and recovery that were published between the years of 1985 and 2013. | Results indicated a significant average (r = 0.51) in the treatment intervention conditions, as well as a significant average (r = 0.31) in the control conditions, in which participants did not receive any treatment. | Results showed that memory rehabilitation was an effective therapeutic intervention, especially for stroke patients and for working memory as a treatment domain. However, the results also indicated that significant memory improvement occurred spontaneously over time. |
| Shin et al. [33] | 2015 | Literature review | At of 350 titles and abstracts were retrieved, and 17 articles were selected for this review. Selected articles were assessed on the level of evidence using the Physiotherapy Evidence Database (PEDro) scale. | Articles assessing the impact of cognitive impairments in memory were most commonly found, and VR interventions elicited positive effects in patients with brain injury. VR can be considered a new tool for cognitive rehabilitation after brain injury. |
| Coyle et al. [34] | 2015 | Literature review | The aim of this study was to assess the efficacy of cognitive training, specifically computerized cognitive training (CCT) and virtual reality cognitive training (VRCT), programs for individuals living with mild cognitive impairment (MCI) or dementia, and therefore at high risk of cognitive decline. | CCT and VRCT were moderately effective in long-term improvement of cognition for those at high risk of cognitive decline. Total intervention time did not mediate efficacy. Future research needs to improve study design by including larger samples, longitudinal designs, and a greater range of outcome measures, including functional and quality of life measures, to assess the wider effect of cognitive training on individuals at high risk of cognitive decline. |
| Al Ayubi et al. [35] | 2015 | Analytical study to review the fundamental characteristics of the technologies used in physical activity monitoring and promotion. | Advances in smartphones and the wide usage of social networking systems offer opportunities for the development of innovative interventions to promote physical activity. | The usability results suggest that the system is usable and user satisfaction was high. Deploying the application was shown to be feasible for the promotion of daily physical activity. |
| Depompei et al. [36] | 2008 | These trials were conducted with individuals who had memory and organizational problems as a result of cognitive disorders of traumatic brain injury (TBI) or intellectual disability (ID). | Results indicate that the use of electronic devices can enhance independent behavior. Factors influencing success include: student motivation, audible beep of the device; support for programming and troubleshooting, alterations of functions; and selection of features to motivate. | Based on the result of the studies, an intervention plan for use of Personal Digital Assistants was developed for use by clinicians. |
| Migo et al. [37] | 2014 | A questionnaire on smartphone ownership was given to an opportunity sample of consecutive patients attending a neuropsychiatry and memory disorders outpatient clinic. Data were collected in 2012 and repeated 12 months later in 2013 to assess changes over time. | Exploring how smartphones and their APPs could function as memory aids is likely to be useful for a large enough number of patients to be clinically worthwhile. | The use of mobile devices to deliver healthcare has not yet been exploited in neuropsychological rehabilitation. Smartphones have the potential to serve as multi-functional memory aids. |
| Cicerone et al. [38] | 2000 | Literature review | Of the 171 studies evaluated, 29 were rated as Class I, 35 as Class II and 107 as Class III. The overall evidence within each predefined area of intervention was then synthesized, and recommendations were derived based on consideration of the relative strengths of the evidence. The resulting practice parameters were organized into three types of recommendations: Practice Standards, Practice Guidelines and Practice Options. | Overall, support exists for the effectiveness of several forms of cognitive rehabilitation for persons with stroke and TBI. Specific recommendations can be made for remediation of language and perception after left and right hemisphere stroke, respectively, and for the remediation of attention, memory, functional communication and executive functioning after TBI. |
| Schutz et al. [39] | 2007 | Literature review | The construct of ‘cognitive rehabilitation’ has not been defined in a consensual manner and the variations in usage have produced misunderstanding and controversy. At one extreme, it refers to a paradigm of complex, sophisticated and integrated interventions, and at the other to a poorly conceptualized and largely ineffectual service modality. | A treatment selection standard is proposed, specifying the conditions under which a holistic model or the ‘contextualized’ training alternative is likely to be more viable. |
| Laatsch et al. [40] | 2007 | This study was to complete a systematic evidence-based review of published cognitive and behavioral treatment studies with pediatric subjects who have a history of an acquired brain injury (ABI). | The studies, involving 366 children and youth with ABI, were classified as one Class I study, fove Class II studies, six Class III studies and 16 Class IV studies. | Despite a limited number of studies, two treatment recommendations and one option were developed from this systematic literature search. |
| McGurk et al. [41] | 2007 | A meta-analysis was conducted of 26 randomized, controlled trials of cognitive remediation in schizophrenia including 1.151 patients. | Cognitive remediation was associated with significant improvements across all three outcomes, with a medium effect size for cognitive performance (0.41), a slightly lower effect size for psychosocial functioning (0.36) and a small effect size for symptoms (0.28). The effects of cognitive remediation on psychosocial functioning were significantly stronger in studies that provided adjunctive psychiatric rehabilitation than in those that provided cognitive remediation alone. | Cognitive remediation produces moderate improvements in cognitive performance and, when combined with psychiatric rehabilitation, also improves functional outcomes. |
| O’Brien et al. [42] | 2008 | Literature review | Studies were chosen based on criteria from previous evidence-based reviews. | Cognitive rehabilitation in MS is in its relative infancy. More methodologically rigorous research is needed to determine the effectiveness and efficacy of various cognitive rehabilitation interventions. |
| Wykes et al. [43] | 2002 | Three groups (patients receiving control therapy or CRT and a healthy control group) were investigated in a repeated measures design using the two-back test. Functional magnetic resonance imaging (fMRI) data and a broad assessment of executive functioning were completed at baseline and post-treatment. | fMRI analyses indicate that the control group showed decreased activation but the two patient groups showed an increase in activation over time. The patient group that received successful CRT had significantly increased brain activation in regions associated with working memory, particularly the frontocortical areas. | This is the first time that brain activation changes in a seriously disabled group of patients with schizophrenia can be associated clearly with psychological rather than pharmacological therapy. |
| Goldstein et al. [44] | 2004 | Exploratory and confirmatory statistical approaches to study the severity of neuropsychological (NP) impairment in 42 crack/cocaine addicted subjects and in 112 comparison subjects (40 alcoholics and 72 controls). | Results revealed that (1) cocaine addicted individuals had a generalized mild level of neurocognitive impairment (<1 S.D. below control mean); and (2) controlling for age and education, relative metabolism in the dorsolateral prefrontal cortex significantly predicted the Visual Memory and Verbal Memory factors and relative metabolism in the anterior cingulate gyrus significantly predicted the Attention/Executive factor. | Tasks that simulate real-life decision-making or that target specific putative cognitive-behavioral or motivational-emotional mechanisms might offer greater sensitivity in characterizing the changes that accompany addiction to drugs. |
| Roehrich et al. [45] | 1993 | Four groups of male alcoholics received pre- and posttesting. Between the two testing sessions, the groups received neuropsychological remediation tasks (n = 15), ecologically relevant tasks (n = 15), attention-placebo tasks (n = 16) or no intervention (n = 15). | Results showed that exposure to both types of remediation produced significant cognitive recovery, with skills transferring to posttest neuropsychological measures and RP acquisition. Hence, cognitive remediation may facilitate alcoholism treatment. | Accumulating research has shown that some cognitive deficits in recently abstinent alcoholics (e.g., cognitive flexibility, acquisition of novel skills) improve only with remediation in contrast to the spontaneous, time-dependent rebound seen for other tasks. |
| Allen et al. [46] | 1997 | Literature review | Empirical investigations conducted to date indicate that some cognitive deficiencies secondary to alcoholism are amenable to cognitive rehabilitation, and that this remediation is generalizable. | The current literature suggests that individuals who chronically abuse alcohol exhibit a wide variety of cognitive deficits resulting from cerebral dysfunction that is either directly or indirectly related to their alcohol consumption history. |
| Fals-Stewart et al. [47] | 2010 | Patients with substance use disorders entering long-term residential care (N = 160) were randomly assigned to one of two conditions: (a) standard treatment plus computer-assisted cognitive rehabilitation (CACR); (b) an equally intensive attention control condition consisting of standard treatment plus a computer-assisted typing tutorial (CATT). | Mediational analyses revealed the positive comparative effect of CACR on abstinence during the year after treatment was mediated by treatment engagement and length of stay in residence. | |
| Yu et al. [48] | 2012 | Students of two vocational schools and two high schools filled out a questionnaire at a baseline (T0) and a 2-month follow-up (T1) data collection session. Students of one vocational school and one high school downloaded the Once Upon a High app (app group), whereas students from the other vocational school and high school did not (nonapp group). | There were 386 students who participated in the T0 session. After dropout, 246 students took part in T1 data collection procedure. Alcohol was the most frequently consumed psychoactive substance (334/364, 91.8% lifetime use), followed by tobacco (252/386, 65.3%, lifetime use) and cannabis (43/323, 13.3% lifetime use). Decreased self-efficacy (beta = −0.29, p = 0.04) and increased daily physical exercise frequencies (beta = 0.04, p < 0.001) predicted higher frequencies of past month energy drink consumption, whereas elevated past month alcohol consumption was mainly predicted by a decrease in negative attitudes toward substance users (beta = −13, p = 0.04) in the regression models. Once Upon a High was found to be effective only in reducing energy drink consumption (beta = -1.13, p = 0.04) after controlling for design effect, whereas perceived utility of the app showed correlation with a decreasing alcohol use (rS (44) = 0.32, p = 0.03). | The Once Upon a High app can be a useful tool to assist preventive intervention programs by increasing knowledge and self-efficacy; however, its efficacy in reducing or preventing substance use needs to be improved and further studied. Additional potential impacts of the app need further testing. |
| Bickel et al. [49] | 2014 | Forty MUD participants were assigned randomly to either the CCAT group (n = 20), who received 4 weeks of CCAT plus regular detoxification treatment as usual, or the control group (n = 20), who only received the regular detoxification treatment as usual, in drug rehabilitation centers in Shanghai. | Compared to the control group, CCAT improved working memory in the CCAT group (p = 0.01). Group × time interactions were observed among DDT, IGT and BART tasks, with rates of discounting delayed rewards, IGT and BART scores (p < 0.001) being reduced among those who received CCAT, whereas no changes were found in the control group. | The newly designed CCAT can help to improve cognitive impairment and impulsive control in MUD. Further research is needed to understand the underlying brain mechanisms of the cognitive therapy. |
| Ahn et al. [50] | 2014 | We report the case of a 10 years old patient diagnosed with attention deficit hyperactivity disorder (ADHD) and comorbid video game addiction, who was treated with medication combined with a novel cognitive training method based on video games called the TCT method. | The TCT method is a cognitive training method that enhances cognitive skills such as attention, working memory, processing speed, calculation ability, reasoning and visuomotor coordination. | The purpose of reviewing this case is to highlight that regular cognitive computerized training in ADHD patients may improve some of their cognitive symptoms and might be helpful for treating video game addiction. |
| Ruiz-Manrique et al. [51] | 2014 | An ART app for the Android system and an accessory of bilateral tactile stimulation were developed and will be used in a study with behavioral self-control training. | This paper presented the design and realization of the smart phone based ART application. The design of a pilot study, which is to examine the benefits of a smartphone application providing behavioral self-control training, is also reported in this paper. | N/A |
| Kapitány-Fövény et al. [52] | 2018 | Descriptive data were used to characterize the nature of the literature on technology-delivered, CBT-based interventions for alcohol use (“CBT Tech”). | The content of CBT Tech programs varied, ranging from four to 62 sessions/exercises, with many programs combining elements of motivational interviewing (47%). With respect to efficacy, CBT Tech as a stand-alone treatment in contrast to a minimal treatment control showed a positive and statistically significant, albeit small effect (g = 0.20: 95% CI = 0.22, 0.38, kes = 5). When CBT Tech was compared to treatment as usual (TAU), effects were nonsignificant. However, when CBT Tech was tested as an addition to TAU, in contrast to TAU only, the effect size was positive, significant (g = 0.30: 95% CI = 0.10, 0.50, kes = 7), and stable over 12-month follow-up. Only two studies compared CBT Tech to in-person CBT, and this pooled effect size did not suggest superior efficacy. | These Results show a benefit for technology-delivered, CBT-based interventions as a stand-alone therapy for heavy drinking or as an addition to usual care in specialty substance use settings. |
| Zhu et al. [53] | 2018 | This article reviewd emerging evidence for computerized working memory training as an efficacious adjunctive treatment for drug dependence and highlights future challenges and opportunities in the field of working-memory training, including duration of training needed, persistence of improvements and utility of booster sessions, and selection of patients based on degree of deficits. | N/A | N/A |
| Kiluk et al. [54] | 2019 | We used computational modeling to address these questions in a unique sample of relatively “pure” amphetamine-dependent (N = 38) and heroin-dependent individuals (N = 43) who were currently in protracted abstinence, and in 48 healthy controls (HC). A Bayesian model comparison technique, a simulation method, and parameter recovery tests were used to compare three cognitive models: (1) Prospect Valence Learning with decay reinforcement learning rule (PVL-DecayRI), (2) PVL with delta learning rule (PVL-Delta) and (3) Value-Plus-Perseverance (VPP) model based on a Win-Stay-Lose-Switch (WSLS) strategy. | Computational modeling results suggested that overall, all three groups relied more on RL than on a WSLS strategy. Heroin users displayed reduced loss aversion relative to HC across all three models, which suggests that their decision-making deficits are longstanding (or pre-existing) and may be driven by reduced sensitivity to loss. In contrast, amphetamine users showed comparable cognitive functions to HC with the VPP model, whereas the second best-fitting model with relatively good simulation performance (PVL-DecayRI) revealed increased reward sensitivity relative to HC. | These results suggest that some decision-making deficits persist in protracted abstinence and may be mediated by different mechanisms in opiate and stimulant users. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Restrepo, S.; Rincón, D.; Sepulveda, E. Cognitive Training for the Treatment of Addictions Mediated by Information and Communication Technologies (ICT). Future Internet 2020, 12, 38. https://doi.org/10.3390/fi12020038
Restrepo S, Rincón D, Sepulveda E. Cognitive Training for the Treatment of Addictions Mediated by Information and Communication Technologies (ICT). Future Internet. 2020; 12(2):38. https://doi.org/10.3390/fi12020038
Chicago/Turabian StyleRestrepo, Sandra, Dubis Rincón, and Edwin Sepulveda. 2020. "Cognitive Training for the Treatment of Addictions Mediated by Information and Communication Technologies (ICT)" Future Internet 12, no. 2: 38. https://doi.org/10.3390/fi12020038
APA StyleRestrepo, S., Rincón, D., & Sepulveda, E. (2020). Cognitive Training for the Treatment of Addictions Mediated by Information and Communication Technologies (ICT). Future Internet, 12(2), 38. https://doi.org/10.3390/fi12020038




