Development of an Antiviral Ion-Activated In Situ Gel Containing 18β-Glycyrrhetinic Acid: A Promising Alternative against Respiratory Syncytial Virus
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
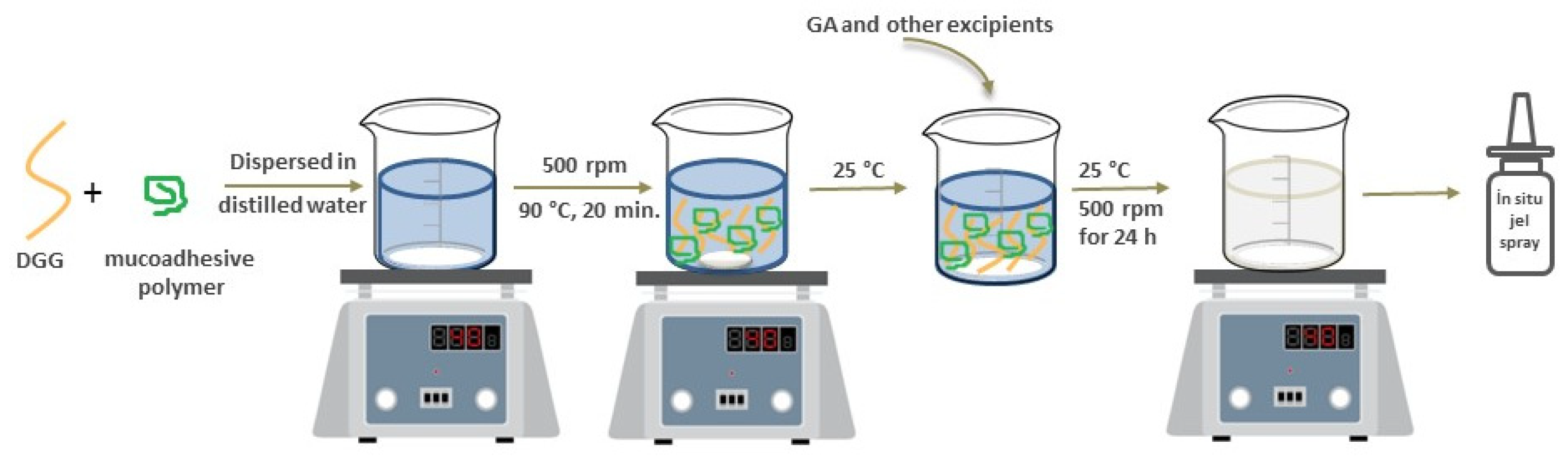
2.2.1. Preparation of GA-Loaded In Situ Gelling Formulations
Preparation of In Situ Gelling Systems Using Only Gellan Gum
Preparation of In Situ Gelling Systems Using Combined Polymers
2.2.2. Characterization of GA-Loaded In Situ Gelling Formulations
Gelation Capacity of In Situ Gelling Formulations with/without Mucoadhesive Polymers
Rheological Evaluation
Mechanical Characteristics of In Situ Gelling Formulations
In Situ Gelling Formulation–Mucin Interaction Study
Ex Vivo Mucoadhesive Strength Test
Sprayability Analysis
Quantitative Determination of 18β-Glycyrrhetinic Acid
Active Substance Content Determination
Fourier Transform Infrared Spectrometry (FTIR) Studies
In Vitro Release Study
Physicochemical Stability
2.2.3. Cell Culture Studies
Cells and Virus
Cytotoxicity Assay
3. Results and Discussion
3.1. Optimization and Characterization of GA-Loaded In Situ Gelling Formulations
3.1.1. Gelation Capacity of In Situ Gelling Formulations
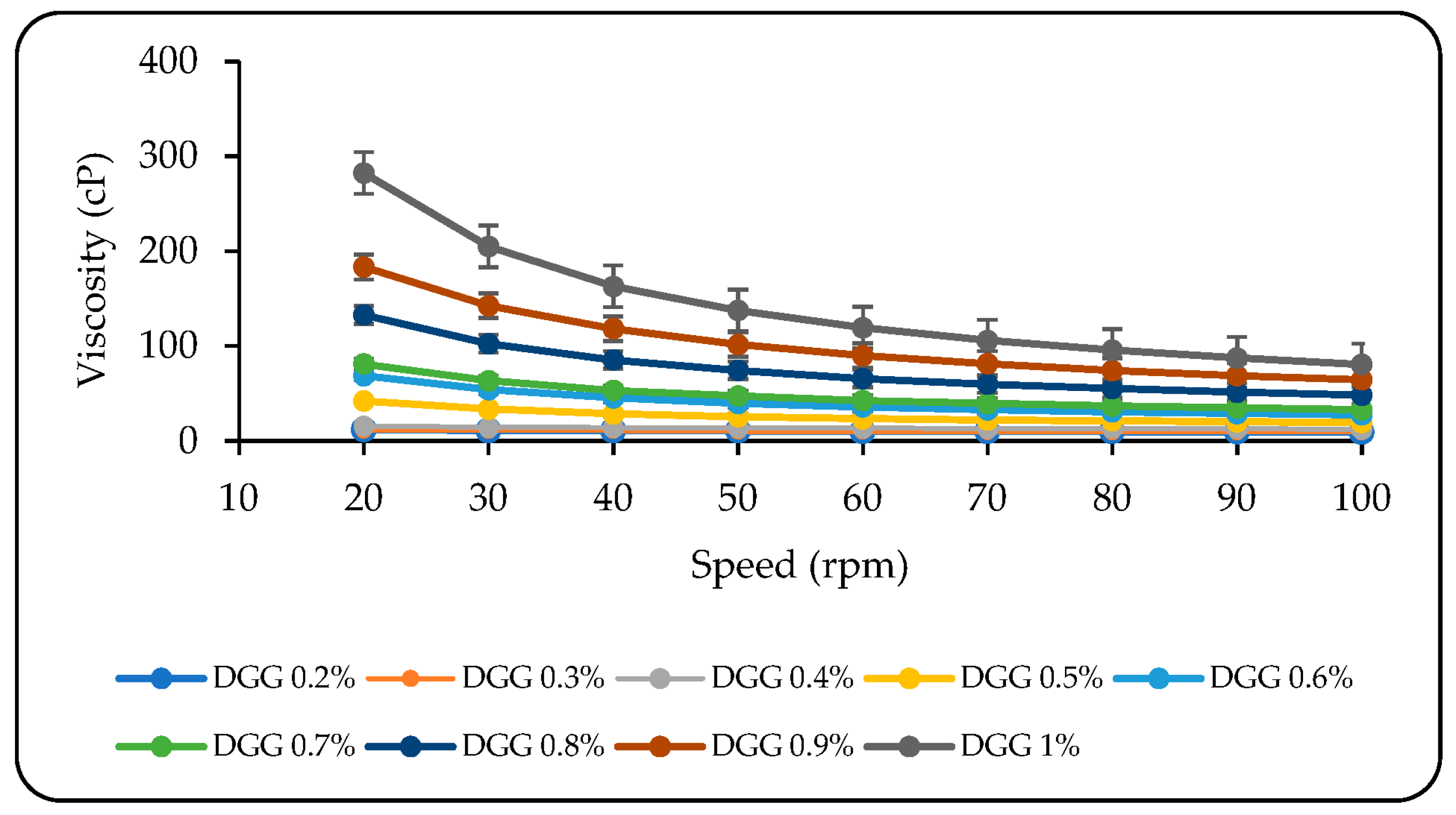
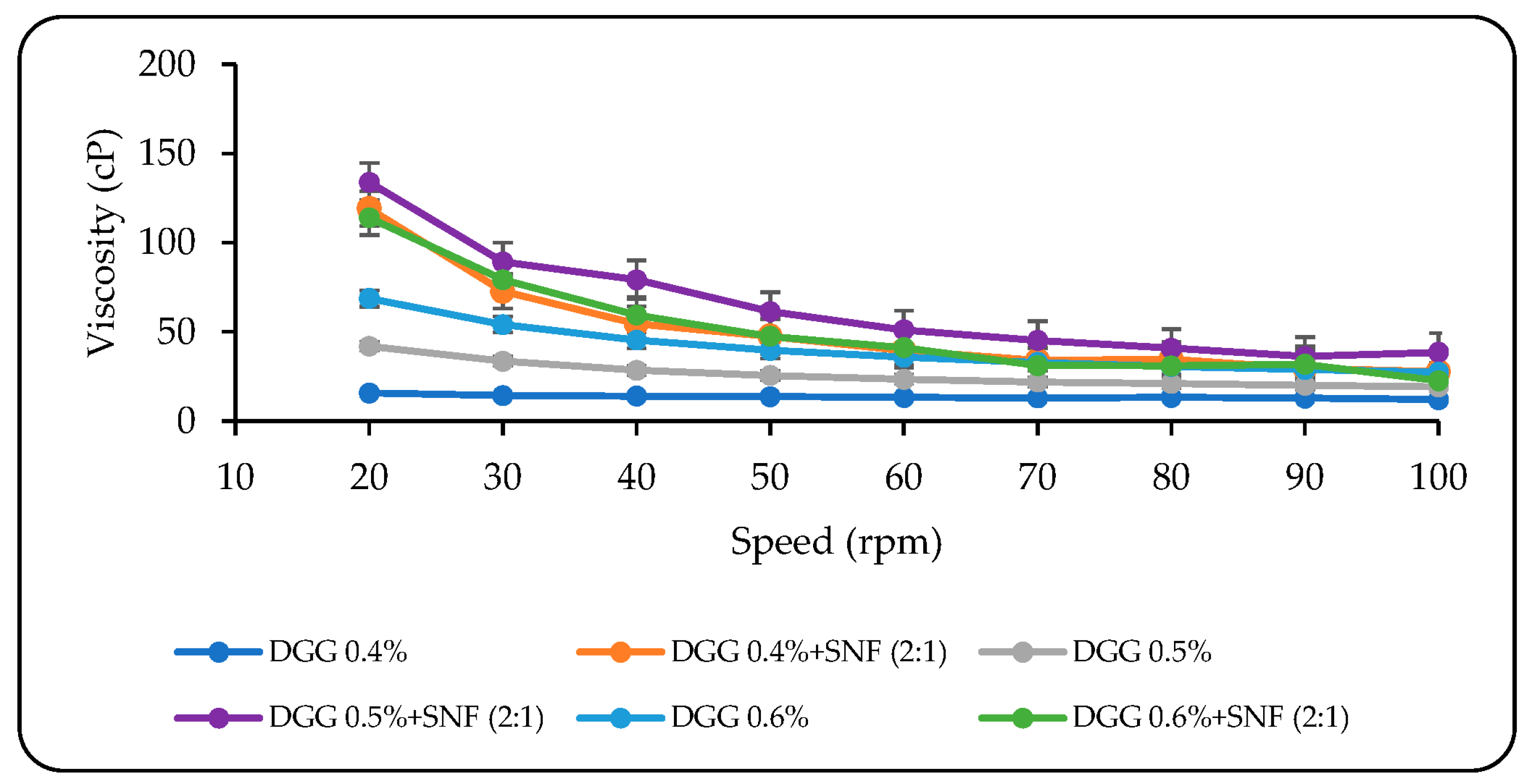
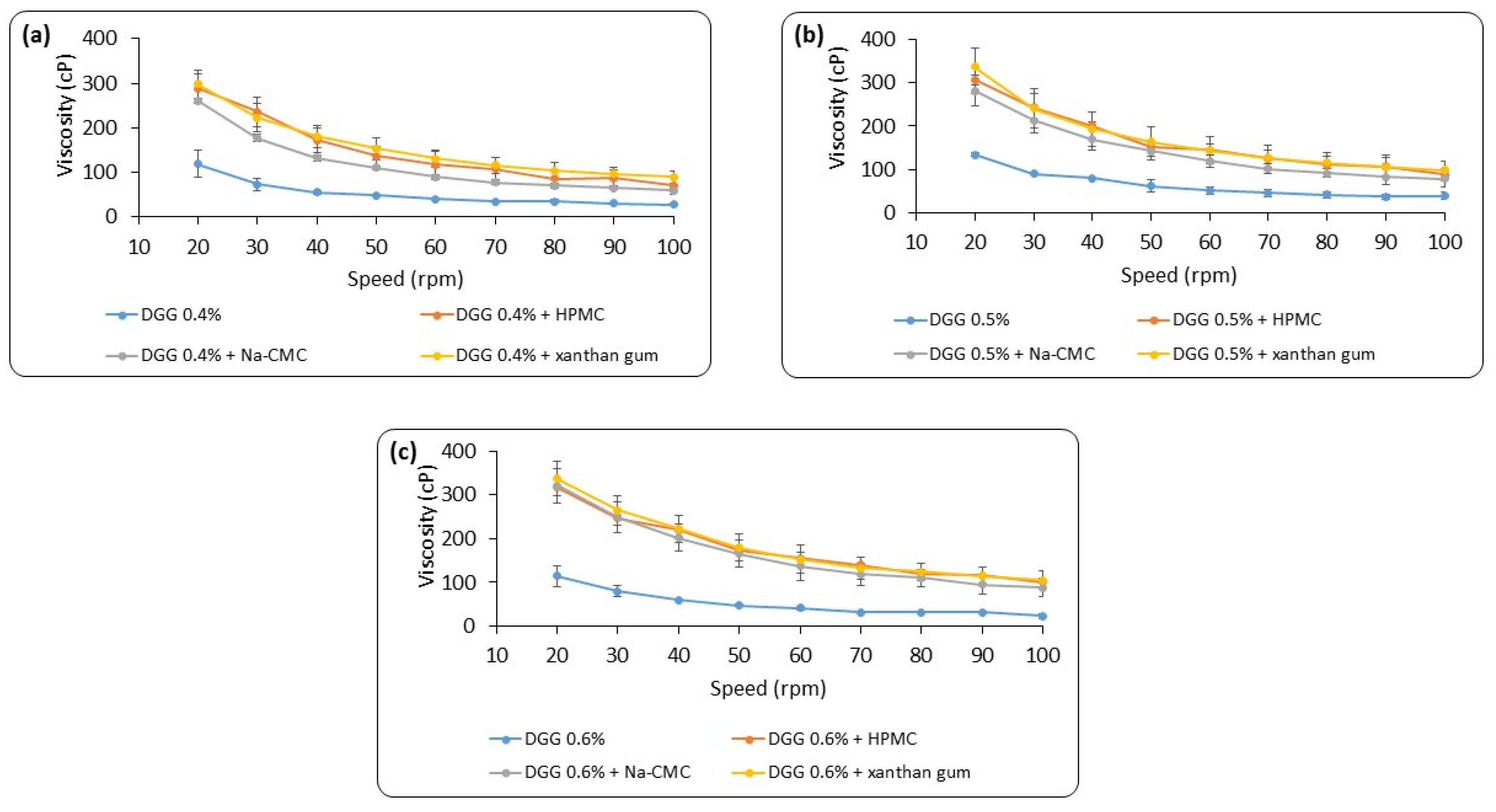
3.1.2. Rheological Evaluation
3.1.3. Mechanical Characteristics of In Situ Gelling Formulations
3.1.4. In Situ Gelling Formulation–Mucin Interaction Study
3.1.5. Ex Vivo Mucoadhesive Strength Test
3.1.6. Sprayability
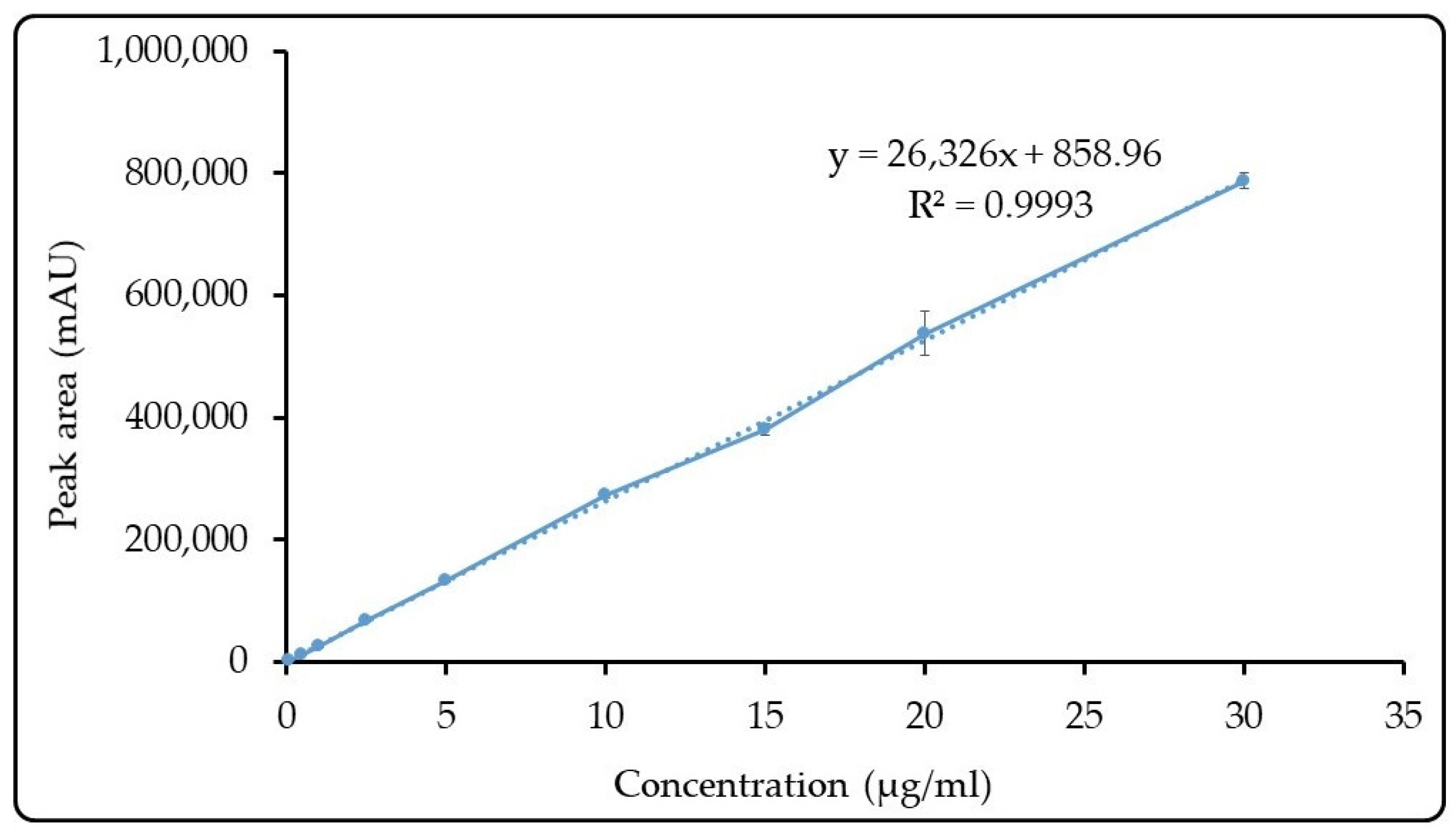
3.1.7. Quantitative Determination of 18β-Glycyrrhetinic Acid
3.1.8. Active Substance Content Determination
3.1.9. Fourier Transform Infrared Spectrometry (FTIR) Studies
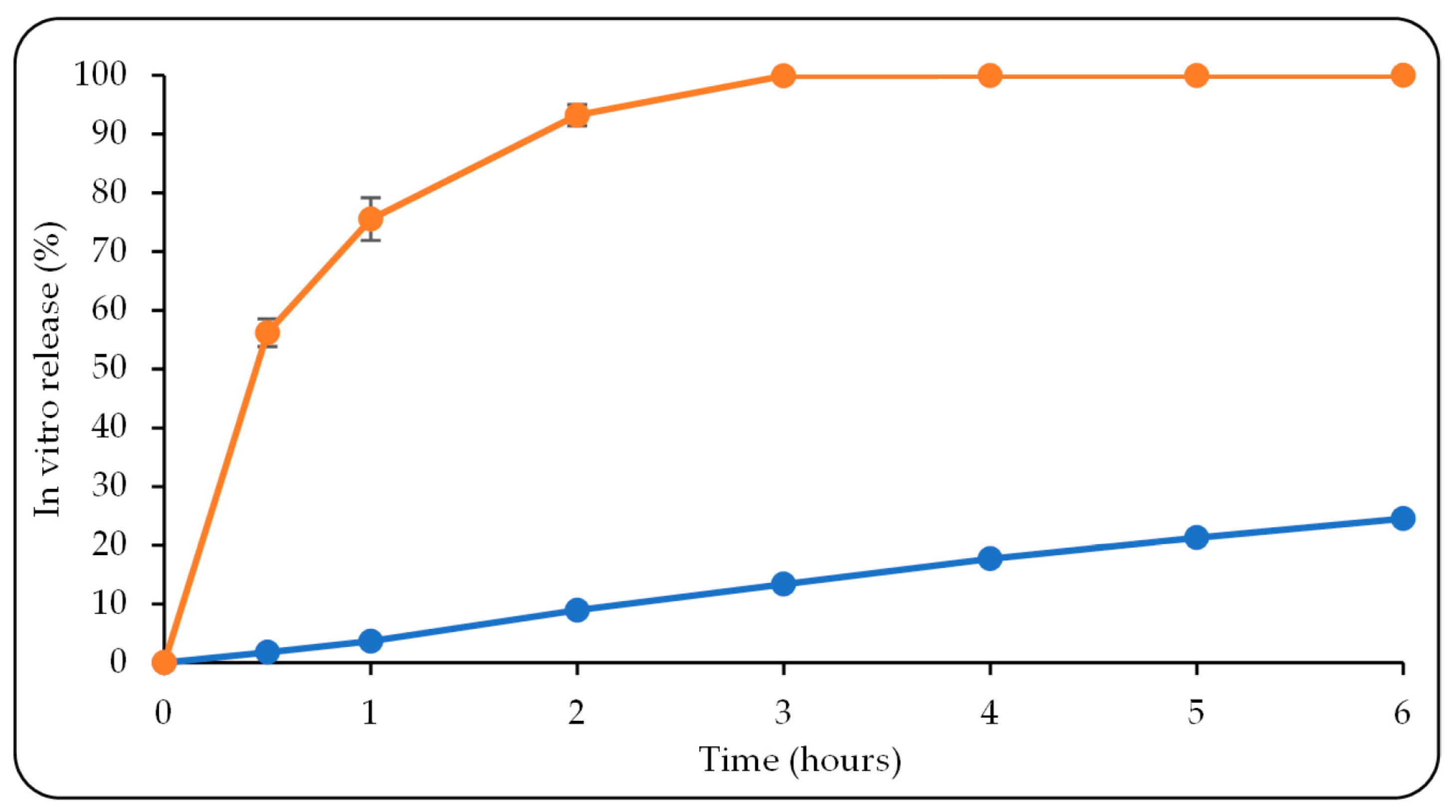
3.1.10. In Vitro Release Study
3.1.11. Physicochemical Stability
3.2. Cell Culture Studies
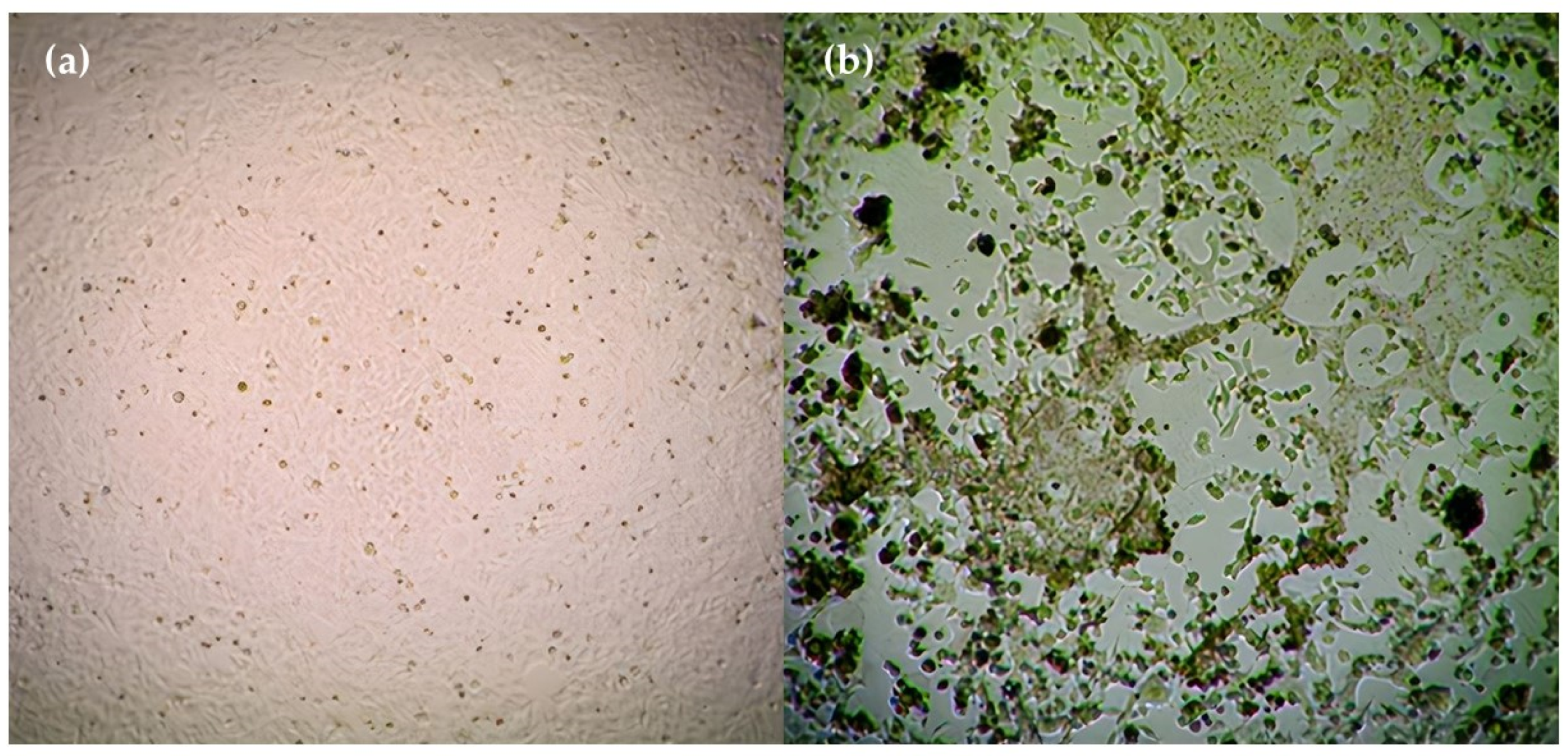
3.2.1. Cytotoxicity Assay
3.2.2. Virus Titration
3.2.3. Antiviral Activity Assay
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, Q.; Zhou, Y.H.; Ye, F.; Yang, Z.Q. Antivirals for respiratory viral infections: Problems and prospects. Semin. Respir. Crit. Care Med. 2016, 37, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Borchardt, R.A.; Rolston, K.V. Respiratory tract infections: Emerging viral pathogens. JAAPA 2012, 25, 19–20. [Google Scholar] [CrossRef]
- Kim, Y.I.; Pareek, R.; Murphy, R.; Harrison, L.; Farrell, E.; Cook, R.; DeVincenzo, J. The antiviral effects of RSV fusion inhibitor, MDT-637, on clinical isolates, vs its achievable concentrations in the human respiratory tract and comparison to ribavirin. Influenza Other Respir. Viruses 2017, 11, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Yeolekar, L.R.; Damle, R.G.; Kamat, A.N.; Khude, M.R.; Simha, V.; Pandit, A.N. Respiratory viruses in acute respiratory tract infections in Western India. Indian J. Pediatr. 2008, 75, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.L.; Fearns, R.; Graham, B.S. Respiratory Syncytial Virus: Virology, Reverse Genetics, and Pathogenesis of Disease. In Challenges and Opportunities for Respiratory Syncytial Virus Vaccines; Anderson, L., Graham, B., Eds.; Current Topics in Microbiology and Immunology; Springer: Berlin/Heidelberg, 2013; Volume 372. [Google Scholar] [CrossRef]
- Shafique, M.; Zahoor, M.A.; Arshad, M.I.; Aslam, B.; Siddique, A.B.; Rasool, M.H.; Qamar, M.U.; Usman, M. Hurdles in vaccine development against respiratory syncytial virus. In The Burden of Respiratory Syncytial Virus Infection in the Young; IntechOpen: London, UK, 2019. [Google Scholar]
- Wat, D. The common cold: A review of the literature. Eur. J. Intern. Med. 2004, 15, 79–88. [Google Scholar] [CrossRef]
- Morris, J.; Blount Jr, R.; Savage, R. Recovery of cytopathogenic agent from chimpanzees with goryza. Proc. Soc. Exp. Biol. Med. 1956, 92, 544–549. [Google Scholar] [CrossRef]
- Chanock, R.; Finberg, L. Recovery from Infants with Respiratory Illness of a Virus related to Chimpanzee Coryza Agent (CCA). II. Epidemiologie Aspects of Infection in Infants and Young Children. Am. J. Hyg. 1957, 66, 291–300. [Google Scholar]
- Glezen, W.P.; Taber, L.H.; Frank, A.L.; Kasel, J.A. Risk of primary infection and reinfection with respiratory syncytial virus. Am. J. Dis. Child. 1986, 140, 543–546. [Google Scholar] [CrossRef]
- Britto, C.J.; Brady, V.; Lee, S.; Cruz, C.S.D. Respiratory viral infections in chronic lung diseases. Clin. Chest Med. 2017, 38, 87–96. [Google Scholar] [CrossRef]
- Peebles Jr, R.S.; Graham, B.S. Pathogenesis of respiratory syncytial virus infection in the murine model. Proc. Am. Thorac. Soc. 2005, 2, 110–115. [Google Scholar] [CrossRef]
- Behzadi, M.A.; Leyva-Grado, V.H. Overview of current therapeutics and novel candidates against influenza, respiratory syncytial virus, and Middle East respiratory syndrome coronavirus infections. Front. Microbiol. 2019, 10, 1327. [Google Scholar] [CrossRef] [PubMed]
- Antonini, T.M.; Coilly, A.; Rossignol, E.; Fougerou-Leurent, C.; Dumortier, J.; Leroy, V.; Veislinger, A.; Radenne, S.; Botta-Fridlund, D.; Durand, F. Sofosbuvir-based regimens in HIV/HCV coinfected patients after liver transplantation: Results from the ANRS CO23 CUPILT study. Transplantation 2018, 102, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-A.; Seong, R.-K.; Kumar, M.; Shin, O.S. Favipiravir and ribavirin inhibit replication of Asian and African strains of Zika virus in different cell models. Viruses 2018, 10, 72. [Google Scholar] [CrossRef] [PubMed]
- Zhurilo, N.I.; Chudinov, M.V.; Matveev, A.V.; Smirnova, O.S.; Konstantinova, I.D.; Miroshnikov, A.I.; Prutkov, A.N.; Grebenkina, L.E.; Pulkova, N.V.; Shvets, V.I. Isosteric ribavirin analogues: Synthesis and antiviral activities. Bioorganic Med. Chem. Lett. 2018, 28, 11–14. [Google Scholar] [CrossRef]
- Bonavia, A.; Franti, M.; Pusateri Keaney, E.; Kuhen, K.; Seepersaud, M.; Radetich, B.; Shao, J.; Honda, A.; Dewhurst, J.; Balabanis, K. Identification of broad-spectrum antiviral compounds and assessment of the druggability of their target for efficacy against respiratory syncytial virus (RSV). Proc. Natl. Acad. Sci. USA 2011, 108, 6739–6744. [Google Scholar] [CrossRef]
- Devincenzo, J.P. Therapy of respiratory syncytial virus infection. Pediatr. Infect. Dis. J. 2000, 19, 786–790. [Google Scholar] [CrossRef]
- Sun, Z.; Pan, Y.; Jiang, S.; Lu, L. Respiratory syncytial virus entry inhibitors targeting the F protein. Viruses 2013, 5, 211–225. [Google Scholar] [CrossRef]
- Trang, T.P.; Whalen, M.; Hilts-Horeczko, A.; Doernberg, S.B.; Liu, C. Comparative effectiveness of aerosolized versus oral ribavirin for the treatment of respiratory syncytial virus infections: A single-center retrospective cohort study and review of the literature. Transpl. Infect. Dis. 2018, 20, e12844. [Google Scholar] [CrossRef]
- Simoes, E.A.; Bont, L.; Manzoni, P.; Fauroux, B.; Paes, B.; Figueras-Aloy, J.; Checchia, P.A.; Carbonell-Estrany, X. Past, present and future approaches to the prevention and treatment of respiratory syncytial virus infection in children. Infect. Dis. Ther. 2018, 7, 87–120. [Google Scholar] [CrossRef]
- Domachowske, J.B.; Anderson, E.J.; Goldstein, M. The future of respiratory syncytial virus disease prevention and treatment. Infect. Dis. Ther. 2021, 10, 47–60. [Google Scholar] [CrossRef]
- Geskey, J.M.; Thomas, N.J.; Brummel, G.L. Palivizumab: A review of its use in the protection of high risk infants against respiratory syncytial virus (RSV). Biol. Targets Ther. 2007, 1, 33–43. [Google Scholar]
- Anderson, E.J.; Carosone-Link, P.; Yogev, R.; Yi, J.; Simões, E.A. Effectiveness of palivizumab in high-risk infants and children: A propensity score weighted regression analysis. Pediatr. Infect. Dis. J. 2017, 36, 699. [Google Scholar] [CrossRef] [PubMed]
- Blanken, M.O.; Rovers, M.M.; Molenaar, J.M.; Winkler-Seinstra, P.L.; Meijer, A.; Kimpen, J.L.; Bont, L. Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. N. Engl. J. Med. 2013, 368, 1791–1799. [Google Scholar] [CrossRef]
- Resch, B. Product review on the monoclonal antibody palivizumab for prevention of respiratory syncytial virus infection. Hum. Vaccines Immunother. 2017, 13, 2138–2149. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Noshita, T.; Yu, T.; Kidachi, Y.; Kamiie, K.; Umetsu, H.; Ryoyama, K. Novel effects of glycyrrhetinic acid on the central nervous system tumorigenic progenitor cells: Induction of actin disruption and tumor cell-selective toxicity. Eur. J. Med. Chem. 2010, 45, 2943–2948. [Google Scholar] [CrossRef] [PubMed]
- Kong, S.-Z.; Chen, H.-M.; Yu, X.-T.; Zhang, X.; Feng, X.-X.; Kang, X.-H.; Li, W.-J.; Huang, N.; Luo, H.; Su, Z.-R. The protective effect of 18β-Glycyrrhetinic acid against UV irradiation induced photoaging in mice. Exp. Gerontol. 2015, 61, 147–155. [Google Scholar] [CrossRef]
- Kalaiarasi, P.; Pugalendi, K. Protective effect of 18β-glycyrrhetinic acid on lipid peroxidation and antioxidant enzymes in experimental diabetes. J. Pharm. Res. 2011, 4, 107–111. [Google Scholar]
- Zhao, C.-h.; Xu, J.; Zhang, Y.-q.; Zhao, L.-x.; Feng, B. Inhibition of human enterovirus 71 replication by pentacyclic triterpenes and their novel synthetic derivatives. Chem. Pharm. Bull. 2014, 62, 764–771. [Google Scholar] [CrossRef]
- Huang, L.-R.; Hao, X.-J.; Li, Q.-J.; Wang, D.-P.; Zhang, J.-X.; Luo, H.; Yang, X.-S. 18β-Glycyrrhetinic acid derivatives possessing a trihydroxylated A ring are potent gram-positive antibacterial agents. J. Nat. Prod. 2016, 79, 721–731. [Google Scholar] [CrossRef] [PubMed]
- Aly, A.M.; Al-Alousi, L.; Salem, H.A. Licorice: A possible anti-inflammatory and anti-ulcer drug. Aaps Pharmscitech 2005, 6, E74–E82. [Google Scholar] [CrossRef] [PubMed]
- Kalaiarasi, P.; Pugalendi, K.V. Antihyperglycemic effect of 18β-glycyrrhetinic acid, aglycone of glycyrrhizin, on streptozotocin-diabetic rats. Eur. J. Pharmacol. 2009, 606, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.G.; You, H.J.; Park, S.J.; Moon, A.R.; Chung, Y.C.; Kang, S.K.; Chun, H.K. Hepatoprotective effects of 18β-glycyrrhetinic acid on carbon tetrachloride-induced liver injury: Inhibition of cytochrome P450 2E1 expression. Pharmacol. Res. 2002, 46, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Pastorino, G.; Cornara, L.; Soares, S.; Rodrigues, F.; Oliveira, M.B.P. Liquorice (Glycyrrhiza glabra): A phytochemical and pharmacological review. Phytother. Res. 2018, 32, 2323–2339. [Google Scholar] [CrossRef] [PubMed]
- Hardy, M.E.; Hendricks, J.M.; Paulson, J.M.; Faunce, N.R. 18 β-glycyrrhetinic acid inhibits rotavirus replication in culture. Virol. J. 2012, 9, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.F.; Wang, K.C.; Chiang, L.C.; Shieh, D.E.; Yen, M.H.; San Chang, J. Water extract of licorice had anti-viral activity against human respiratory syncytial virus in human respiratory tract cell lines. J. Ethnopharmacol. 2013, 148, 466–473. [Google Scholar]
- Higgins, T.S.; Wu, A.W.; Illing, E.A.; Sokoloski, K.J.; Weaver, B.A.; Anthony, B.P.; Hughes, N.; Ting, J.Y. Intranasal antiviral drug delivery and coronavirus disease 2019 (COVID-19): A state of the art review. Otolaryngol.-Head Neck Surg. 2020, 163, 682–694. [Google Scholar] [CrossRef]
- Cao, S.-L.; Ren, X.-W.; Zhang, Q.-Z.; Chen, E.; Xu, F.; Chen, J.; Liu, L.-C.; Jiang, X.-G. In situ gel based on gellan gum as new carrier for nasal administration of mometasone furoate. Int. J. Pharm. 2009, 365, 109–115. [Google Scholar] [CrossRef]
- Andrews, G.P.; Laverty, T.P.; Jones, D.S. Mucoadhesive polymeric platforms for controlled drug delivery. Eur. J. Pharm. Biopharm. 2009, 71, 505–518. [Google Scholar] [CrossRef]
- Phillipson, M.; Johansson, M.E.; Henriksnas, J.; Petersson, J.; Gendler, S.J.; Sandler, S.; Persson, A.E.G.; Hansson, G.C.; Holm, L. The gastric mucus layers: Constituents and regulation of accumulation. Am. J. Physiol.-Gastrointest. Liver Physiol. 2008, 295, G806–G812. [Google Scholar] [CrossRef]
- Salamat-Miller, N.; Chittchang, M.; Johnston, T.P. The use of mucoadhesive polymers in buccal drug delivery. Adv. Drug Deliv. Rev. 2005, 57, 1666–1691. [Google Scholar] [CrossRef]
- Hagesaether, E.; Hiorth, M.; Sande, S.A. Mucoadhesion and drug permeability of free mixed films of pectin and chitosan: An in vitro and ex vivo study. Eur. J. Pharm. Biopharm. 2009, 71, 325–331. [Google Scholar] [CrossRef]
- Musumeci, T.; Bonaccorso, A.; Puglisi, G. Epilepsy disease and nose-to-brain delivery of polymeric nanoparticles: An overview. Pharmaceutics 2019, 11, 118. [Google Scholar] [CrossRef]
- Sosnik, A.; das Neves, J.; Sarmento, B. Mucoadhesive polymers in the design of nano-drug delivery systems for administration by non-parenteral routes: A review. Prog. Polym. Sci. 2014, 39, 2030–2075. [Google Scholar] [CrossRef]
- Shinde, J.V.; Mali, K.K.; Dias, R.J.; Havaldar, V.D.; Mahajan, N.S. In situ mucoadhesive nasal gels of metoclopramide hydrochloride: Preformulation and formulation studies. J. Pharm. Res. 2008, 1, 88–96. [Google Scholar]
- Altuntaş, E.; Yener, G. Formulation and evaluation of thermoreversible in situ nasal gels containing mometasone furoate for allergic rhinitis. AAPS PharmSciTech 2017, 18, 2673–2682. [Google Scholar] [CrossRef]
- Salunke, S.R.; Patil, S.B. Ion activated in situ gel of gellan gum containing salbutamol sulphate for nasal administration. Int. J. Biol. Macromol. 2016, 87, 41–47. [Google Scholar] [CrossRef]
- Jansson, B.; Hägerström, H.; Fransén, N.; Edsman, K.; Björk, E. The influence of gellan gum on the transfer of fluorescein dextran across rat nasal epithelium in vivo. Eur. J. Pharm. Biopharm. 2005, 59, 557–564. [Google Scholar] [CrossRef]
- Morsi, N.; Ibrahim, M.; Refai, H.; El Sorogy, H. Nanoemulsion-based electrolyte triggered in situ gel for ocular delivery of acetazolamide. Eur. J. Pharm. Sci. 2017, 104, 302–314. [Google Scholar] [CrossRef] [PubMed]
- United State Pharmacopeia 44-NF39. 2021. Available online: www.pharmaceuticalsky.com/2022/01/usp-2021-united-state-pharmacopeia-44.html (accessed on 16 June 2023).
- Saindane, N.S.; Pagar, K.P.; Vavia, P.R. Nanosuspension based in situ gelling nasal spray of carvedilol: Development, in vitro and in vivo characterization. Aaps Pharmscitech 2013, 14, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Song, X.; Sun, F.; Yang, Z.; Hou, S.; Liu, Z. Formulation and evaluation of in situ gelling systems for intranasal administration of gastrodin. Aaps Pharmscitech 2011, 12, 1102–1109. [Google Scholar] [CrossRef]
- Hao, J.; Zhao, J.; Zhang, S.; Tong, T.; Zhuang, Q.; Jin, K.; Chen, W.; Tang, H. Fabrication of an ionic-sensitive in situ gel loaded with resveratrol nanosuspensions intended for direct nose-to-brain delivery. Colloids Surf. B Biointerfaces 2016, 147, 376–386. [Google Scholar] [CrossRef]
- Hassan, E.E.; Gallo, J.M. A simple rheological method for the in vitro assessment of mucin-polymer bioadhesive bond strength. Pharm. Res. 1990, 7, 491–495. [Google Scholar] [CrossRef]
- Mayol, L.; Quaglia, F.; Borzacchiello, A.; Ambrosio, L.; La Rotonda, M.I. A novel poloxamers/hyaluronic acid in situ forming hydrogel for drug delivery: Rheological, mucoadhesive and in vitro release properties. Eur. J. Pharm. Biopharm. 2008, 70, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Callens, C.; Ceulemans, J.; Ludwig, A.; Foreman, P.; Remon, J.P. Rheological study on mucoadhesivity of some nasal powder formulations. Eur. J. Pharm. Biopharm. 2003, 55, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Gadhave, D.; Tupe, S.; Tagalpallewar, A.; Gorain, B.; Choudhury, H.; Kokare, C. Nose-to-brain delivery of amisulpride-loaded lipid-based poloxamer-gellan gum nanoemulgel: In vitro and in vivo pharmacological studies. Int. J. Pharm. 2021, 607, 121050. [Google Scholar] [CrossRef]
- Gadhave, D.; Gorain, B.; Tagalpallewar, A.; Kokare, C. Intranasal teriflunomide microemulsion: An improved chemotherapeutic approach in glioblastoma. J. Drug Deliv. Sci. Technol. 2019, 51, 276–289. [Google Scholar] [CrossRef]
- Spray, N.; Solution, I. Suspension, and Spray Drug Products; Chemistry, Manufacturing and Controls Documentation; US Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER): Rockville, MD, USA, 2002; Volume 23.
- Grobuschek, N.; Lecnik, O.; Schmid, M.G.; Gubitz, G. Mass uniformity of nasal sprays. Scientia Pharmaceutica 2003, 71, 151–164. [Google Scholar] [CrossRef][Green Version]
- Zhou, N.; Zou, C.; Qin, M.; Li, Y.; Huang, J. A simple method for evaluation pharmacokinetics of glycyrrhetinic acid and potential drug-drug interaction between herbal ingredients. Sci. Rep. 2019, 9, 11308. [Google Scholar] [CrossRef] [PubMed]
- Nodilo, L.N.; Perkušić, M.; Ugrina, I.; Špoljarić, D.; Brala, C.J.; Klarić, D.A.; Lovrić, J.; Saršon, V.; Kučuk, M.S.; Zadravec, D. In situ gelling nanosuspension as an advanced platform for fluticasone propionate nasal delivery. Eur. J. Pharm. Biopharm. 2022, 175, 27–42. [Google Scholar] [CrossRef]
- Francis, T. Diagnostic Procedures for Virus and Rickettsial Diseases; American Public Health Association: Benjamin, MD, USA, 1956. [Google Scholar]
- Andrighetti-Fröhner, C.; Antonio, R.; Creczynski-Pasa, T.; Barardi, C.; Simões, C. Cytotoxicity and potential antiviral evaluation of violacein produced by Chromobacterium violaceum. MemÓRias Do Inst. Oswaldo Cruz 2003, 98, 843–848. [Google Scholar] [CrossRef]
- Ho, W.S.; Xue, J.Y.; Sun, S.S.; Ooi, V.E.; Li, Y.L. Antiviral activity of daphnoretin isolated from Wikstroemia indica. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2010, 24, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Doğan, H.H.; Duman, R. The Anti Hrsv Activity of Ferula Halophila Peşmen Aqueous and Methanol Extract by Mtt Assay. Trak. Univ. J. Nat. Sci. 2021, 22, 43–48. [Google Scholar] [CrossRef]
- Ozkan, B.; Altuntas, E.; Cakir Koc, R.; Budama-Kilinc, Y. Development of piperine nanoemulsions: An alternative topical application for hypopigmentation. Drug Dev. Ind. Pharm. 2022, 48, 117–127. [Google Scholar] [CrossRef]
- Food and Drug Administration. Guidance for Industry: Drug Stability Guidelines. 2008. Available online: http://www.fda.gov/downloads/AnimalVeterinary/GuidanceComplianceEnforcement/GuidanceforIndustry (accessed on 21 May 2023).
- Pires, P.C.; Rodrigues, M.; Alves, G.; Santos, A.O. Strategies to improve drug strength in nasal preparations for brain delivery of low aqueous solubility drugs. Pharmaceutics 2022, 14, 588. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, D.; Chawla-Sarkar, M.; Chatterjee, T.; Dey, R.S.; Bag, P.; Chakraborti, S.; Khan, M.T.H. Recent advancements for the evaluation of anti-viral activities of natural products. New Biotechnol. 2009, 25, 347–368. [Google Scholar] [CrossRef] [PubMed]
- Faber, T.E. Immunity to Respiratory Syncytial Virus: A Clinical Perspective; Utrecht University: Utrecht, The Netherlands, 2017. [Google Scholar]
- Proença-Módena, J.L.; Acrani, G.O.; Snider, C.B.; Arruda, E. Respiratory Viral Infections. In Tropical Infectious Diseases: Principles, Pathogens and Practice; Saunders: Philadelphia, PA, USA, 2011; pp. 378–391. [Google Scholar] [CrossRef]
- Grabovac, V.; Guggi, D.; Bernkop-Schnürch, A. Comparison of the mucoadhesive properties of various polymers. Adv. Drug Deliv. Rev. 2005, 57, 1713–1723. [Google Scholar] [CrossRef]
- Chatterjee, B.; Amalina, N.; Sengupta, P.; Mandal, U.K. Mucoadhesive polymers and their mode of action: A recent update. J. Appl. Pharm. Sci. 2017, 7, 195–203. [Google Scholar]
- Takeuchi, H.; Thongborisute, J.; Matsui, Y.; Sugihara, H.; Yamamoto, H.; Kawashima, Y. Novel mucoadhesion tests for polymers and polymer coated particles to design optimal mucoadhesion drug delivery systems. Adv. Drug Deliv. Rev. 2005, 57, 1583–1594. [Google Scholar] [CrossRef]
- Wu, Y.; Liu, Y.; Li, X.; Kebebe, D.; Zhang, B.; Ren, J.; Lu, J.; Li, J.; Du, S.; Liu, Z. Research progress of in-situ gelling ophthalmic drug delivery system. Asian J. Pharm. Sci. 2019, 14, 1–15. [Google Scholar] [CrossRef]
- Pal, K.; Paulson, A.T.; Rousseau, D. Biopolymers in controlled-release delivery systems. In Modern Biopolymer Science; Academic Press: Cambridge, MA, USA, 2009; pp. 519–557. [Google Scholar]
- Khouryieh, H.A.; Herald, T.J.; Aramouni, F.; Alavi, S. Intrinsic viscosity and viscoelastic properties of xanthan/guar mixtures in dilute solutions: Effect of salt concentration on the polymer interactions. Food Res. Int. 2007, 40, 883–893. [Google Scholar] [CrossRef]
- Lin, H.-R.; Sung, K. Carbopol/pluronic phase change solutions for ophthalmic drug delivery. J. Control. Release 2000, 69, 379–388. [Google Scholar] [CrossRef]
- Almeida, H.; Amaral, M.H.; Lobão, P.; Lobo, J.M.S. In situ gelling systems: A strategy to improve the bioavailability of ophthalmic pharmaceutical formulations. Drug Discov. Today 2014, 19, 400–412. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.S.; Woolfson, A.D.; Brown, A.F. Textural, viscoelastic and mucoadhesive properties of pharmaceutical gels composed of cellulose polymers. Int. J. Pharm. 1997, 151, 223–233. [Google Scholar] [CrossRef]
- Peppas, N.A.; Buri, P.A. Surface, interfacial and molecular aspects of polymer bioadhesion on soft tissues. J. Control. Release 1985, 2, 257–275. [Google Scholar] [CrossRef]
- Draget, K.; Simensen, M.; Onsøyen, E.; Smidsrød, O. Gel strength of Ca-limited alginate gels made in situ. In Proceedings of the Fourteenth International Seaweed Symposium, Brest, France, 16–21 August 1992; pp. 563–569. [Google Scholar]
- Fini, A.; Bergamante, V.; Ceschel, G.C. Mucoadhesive gels designed for the controlled release of chlorhexidine in the oral cavity. Pharmaceutics 2011, 3, 665–679. [Google Scholar] [CrossRef]
- Tangri, P.; Madhav, N. Oral mucoadhesive drug delivery systems: A review. JBI 2011, 2229, 7499. [Google Scholar]
- USP44-NF39 2021, Inhalation and Nasal Drug Products: Aerosols, Sprays, and Powders—Performance Quality Tests. Available online: https://online.uspnf.com/uspnf/document/1_GUID-FA5F788A-4449-4F16-8435-9B8D5EECB5C9_5_en-US (accessed on 16 June 2023).
- Prasher, P.; Sharma, M. Mucoadhesive nanoformulations and their potential for combating COVID-19. Nanomedicine 2021, 16, 2497–2501. [Google Scholar] [CrossRef]
- Vigani, B.; Rossi, S.; Sandri, G.; Bonferoni, M.C.; Caramella, C.M.; Ferrari, F. Recent advances in the development of in situ gelling drug delivery systems for non-parenteral administration routes. Pharmaceutics 2020, 12, 859. [Google Scholar] [CrossRef]
- Karavasili, C.; Fatouros, D.G. Smart materials: In situ gel-forming systems for nasal delivery. Drug Discov. Today 2016, 21, 157–166. [Google Scholar] [CrossRef]
- Corazza, E.; di Cagno, M.P.; Bauer-Brandl, A.; Abruzzo, A.; Cerchiara, T.; Bigucci, F.; Luppi, B. Drug delivery to the brain: In situ gelling formulation enhances carbamazepine diffusion through nasal mucosa models with mucin. Eur. J. Pharm. Sci. 2022, 179, 106294. [Google Scholar] [CrossRef]

| Ingredients | Composition (% w/w) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| DGG | 0.2 | 0.3 | 0.4 | 0.5 | 0.6 | 0.7 | 0.8 | 0.9 | 1 |
| GA | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 |
| Dexpanthenol | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 |
| Glycerin | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Benzalkonium chloride | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 |
| Distilled water | 98.48 | 98.38 | 98.28 | 98.18 | 98.08 | 97.98 | 97.88 | 97.78 | 97.68 |
| Ingredients | Composition (% w/w) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DGG | 0.4 | 0.5 | 0.6 | 0.4 | 0.5 | 0.6 | 0.4 | 0.5 | 0.6 | 0.4 | 0.5 | 0.6 |
| GA | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 |
| Xanthan gum | 0.5 | 0.5 | 0.5 | - | - | - | - | - | - | - | - | - |
| HPMC | - | - | - | 0.5 | 0.5 | 0.5 | - | - | - | - | - | - |
| Na-CMC | - | - | - | - | - | - | 0.5 | 0.5 | 0.5 | - | - | - |
| Carbopol® 974P NF | - | - | - | - | - | - | - | - | - | 0.5 | 0.5 | 0.5 |
| Dexpanthenol | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 |
| Glycerin | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Benzalkonium chloride | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 |
| Distilled water | 97.78 | 97.68 | 97.58 | 97.78 | 97.68 | 97.58 | 97.78 | 97.68 | 97.58 | 97.78 | 97.68 | 97.58 |
| Ingredients | Composition (% w/w) | |||
|---|---|---|---|---|
| DGG | 0.5 | 0.5 | 0.5 | 0.5 |
| GA | 0.1 | 0.1 | 0.1 | 0.1 |
| Na-CMC | 0.1 | 0.3 | 0.5 | 0.7 |
| Dexpanthenol | 0.2 | 0.2 | 0.2 | 0.2 |
| Glycerin | 1 | 1 | 1 | 1 |
| Benzalkonium chloride | 0.02 | 0.02 | 0.02 | 0.02 |
| Distilled water | 98.08 | 97.88 | 97.68 | 97.48 |
| Formulation | ηp | ηm | ηt | ηb | Fb (Pa) |
|---|---|---|---|---|---|
| DGG 0.4% − HPMC | 125.68 ± 2.84 | 13.95 ± 0.32 | 238.13 ± 11.25 | 98.50 ± 2.76 | 3.94 ± 0.45 |
| DGG 0.5% − HPMC | 168.68 ± 6.23 | 13.95 ± 0.32 | 294.35 ± 14.98 | 111.73 ± 4.87 | 4.47 ± 0.87 |
| DGG 0.6% − HPMC | 251.36 ± 16.89 | 13.95 ± 0.32 | 343.96 ± 10.62 | 78.65 ± 1.34 | 3.15 ± 0.23 |
| DGG 0.4% − Na-CMC | 55.59 ± 2.38 | 13.95 ± 0.32 | 191.82 ± 7.94 | 122.28 ± 8.98 | 4.89 ± 0.98 |
| DGG 0.5% − Na-CMC | 72.48 ± 1.68 | 13.95 ± 0.32 | 321.08 ± 9.15 | 234.65 ± 11.85 | 9.39 ± 0.34 |
| DGG 0.6% − Na-CMC | 74.01 ± 2.24 | 13.95 ± 0.32 | 327.43 ± 12.18 | 239.46 ± 10.37 | 9.58 ± 1.36 |
| DGG 0.4% − xanthan gum | 99.22 ± 3.34 | 13.95 ± 0.32 | 317.51 ± 15.64 | 204.34 ± 8.82 | 8.17 ± 1.67 |
| DGG 0.5% − xanthan gum | 148.83 ± 5.75 | 13.95 ± 0.32 | 317.04 ± 10.21 | 154.26 ± 2.75 | 6.17 ± 1.43 |
| DGG 0.6% − xanthan gum | 188.52 ± 4.90 | 13.95 ± 0.32 | 317.51 ± 6.86 | 115.04 ± 9.46 | 4.60 ± 0.24 |
| Formulation | ηp | ηm | ηt | ηb | Fb (Pa) |
|---|---|---|---|---|---|
| DGG 0.5% − Na-CMC 0.1% | 20.28 ± 0.33 | 16.51 ± 0.49 | 298.84 ± 18.36 | 262.06 ± 13.36 | 8.91 ± 1.21 |
| DGG 0.5% − Na-CMC 0.3% | 54.28 ± 0.71 | 16.51 ± 0.49 | 315.03 ± 18.39 | 244.23 ± 11.36 | 8.30 ± 0.56 |
| DGG 0.5% − Na-CMC 0.5% | 74.23 ± 3.16 | 16.51 ± 0.49 | 371.08 ± 19.17 | 280.34 ± 16.23 | 9.53 ± 0.78 |
| DGG 0.5% − Na-CMC 0.7% | 116.41 ± 5.82 | 16.51 ± 0.49 | 371.37 ± 15.89 | 238.44 ± 10.20 | 8.11 ± 0.43 |
| Formulation | Adhesion Strength (g) |
|---|---|
| DGG 0.5% − Na-CMC 0.1% | 14.33 ± 8.40 |
| DGG 0.5% − Na-CMC 0.3% | 15.67 ± 5.20 |
| DGG 0.5% − Na-CMC 0.5% | 19.67 ± 5.90 |
| DGG 0.5% − Na-CMC 0.7% | 27.67 ± 6.80 |
| Formulation | T1 | T7 | T14 | ||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Weight Deviation (%) | Mean ± SD | Weight Deviation (%) | |
| DGG 0.5% − Na-CMC 0.1% | 0.323 ± 0.003 | 0.319 ± 0.002 | 1.24 | 0.320 ± 0.003 | 0.93 |
| DGG 0.5% − Na-CMC 0.3% | 0.319 ± 0.002 | 0.326 ± 0.001 | 2.19 | 0.323 ± 0.002 | 1.25 |
| DGG 0.5% − Na-CMC 0.5% | 0.306 ± 0.001 | 0.299 ± 0.002 | 2.29 | 0.302 ± 0.001 | 1.30 |
| DGG 0.5% − Na-CMC 0.7% | 0.299 ± 0.003 | 0.287 ± 0.001 | 4.01 | 0.294 ± 0.001 | 1.67 |
| Cytotoxicity | ||
|---|---|---|
| Sample Type | MNTC a (µg/mL) | CC50 b (µg/mL) |
| GA | 8.33 | 47.59 |
| GA in situ gelling formulation | 4.16 | 15.29 |
| Placebo in situ gelling formulation | 4.16 | 14.84 |
| Ribavirin | 0.98 | 117.00 |
| Sample Type | Simultaneous | Pre-Infection | ||
|---|---|---|---|---|
| EC50 a (µg/mL) | SI b | EC50 a (µg/mL) | SI b | |
| GA | 0.435 | 109.65 | 0.115 | 415.00 |
| GA in situ gelling formulation | 0.050 | 306.00 | 0.154 | 100.00 |
| Placebo in situ gelling formulation | 0.790 | 18.83 | 2.005 | 7.40 |
| Ribavirin | 4.189 | 28.00 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Özkan, B.; Altuntaş, E.; Ünlü, Ü.; Doğan, H.H.; Özsoy, Y.; Çakır Koç, R. Development of an Antiviral Ion-Activated In Situ Gel Containing 18β-Glycyrrhetinic Acid: A Promising Alternative against Respiratory Syncytial Virus. Pharmaceutics 2023, 15, 2055. https://doi.org/10.3390/pharmaceutics15082055
Özkan B, Altuntaş E, Ünlü Ü, Doğan HH, Özsoy Y, Çakır Koç R. Development of an Antiviral Ion-Activated In Situ Gel Containing 18β-Glycyrrhetinic Acid: A Promising Alternative against Respiratory Syncytial Virus. Pharmaceutics. 2023; 15(8):2055. https://doi.org/10.3390/pharmaceutics15082055
Chicago/Turabian StyleÖzkan, Burcu, Ebru Altuntaş, Ümmühan Ünlü, Hasan Hüseyin Doğan, Yıldız Özsoy, and Rabia Çakır Koç. 2023. "Development of an Antiviral Ion-Activated In Situ Gel Containing 18β-Glycyrrhetinic Acid: A Promising Alternative against Respiratory Syncytial Virus" Pharmaceutics 15, no. 8: 2055. https://doi.org/10.3390/pharmaceutics15082055
APA StyleÖzkan, B., Altuntaş, E., Ünlü, Ü., Doğan, H. H., Özsoy, Y., & Çakır Koç, R. (2023). Development of an Antiviral Ion-Activated In Situ Gel Containing 18β-Glycyrrhetinic Acid: A Promising Alternative against Respiratory Syncytial Virus. Pharmaceutics, 15(8), 2055. https://doi.org/10.3390/pharmaceutics15082055







