Polymeric-Micelle-Based Delivery Systems for Nucleic Acids
Abstract
1. Introduction
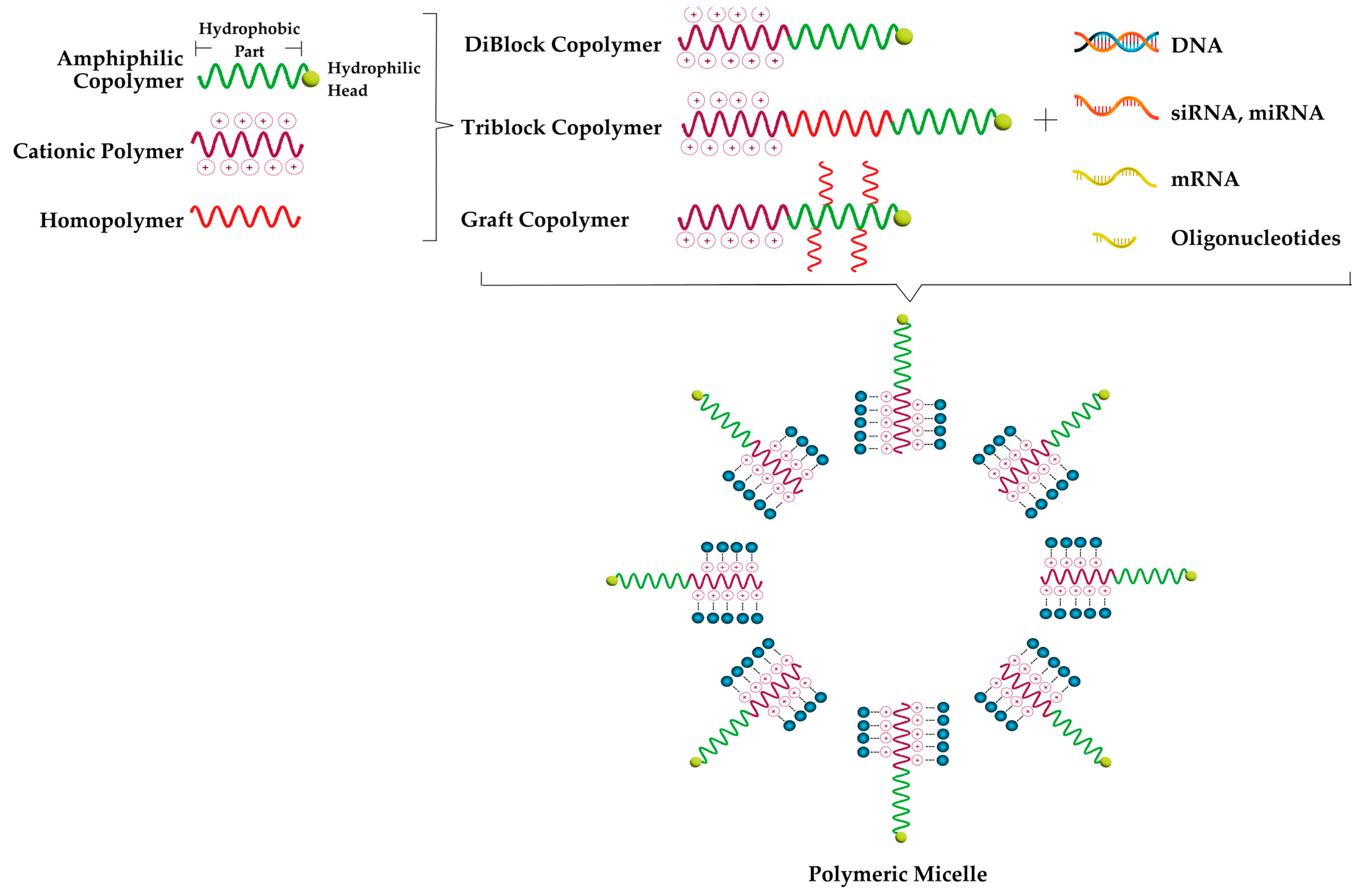
2. Polymeric Micelles
2.1. Preparation of Polymeric Micelles
2.1.1. Preparation Methods of PMs
- -
- Direct Dissolution Method
- -
- Dialysis Method
- -
- Oil-in-Water (O/W) Emulsion
- -
- Thin Film Layer (Solvent Evaporation)
- -
- Lyophilization Method
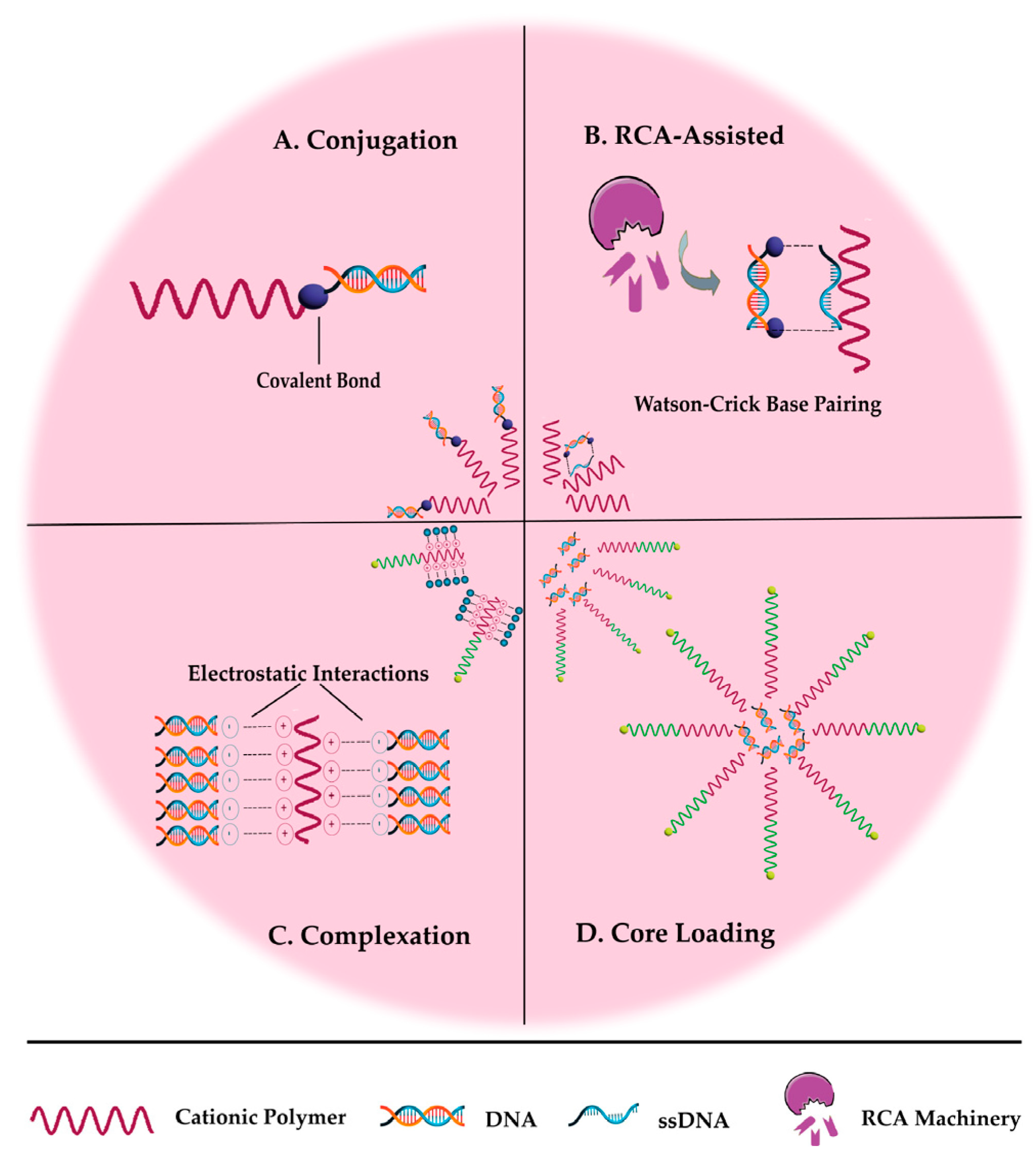
2.1.2. Preparation of Nucleic Acid-Carrying PMs
- -
- Conjugation
- -
- Rolling circle amplification (RCA)-assisted
- -
- Complexation
- -
- Core Loading
2.2. Characteristic Features and Characterization Methods of Polymeric Micelles
2.2.1. Size, Size Distribution, Surface Characteristics and Morphology
2.2.2. Physical Stability
2.2.3. Loading Capacity
2.2.4. Release of Therapeutic Agent
2.2.5. NA Binding
2.3. Functionalization of PMs
2.3.1. pH-Responsive PMs
2.3.2. Reactive Oxygen Species (ROS)-Responsive PMs
2.3.3. Enzyme-Responsive PMs
2.3.4. Thermo-Responsive PMs
2.3.5. ATP-Responsive PMs
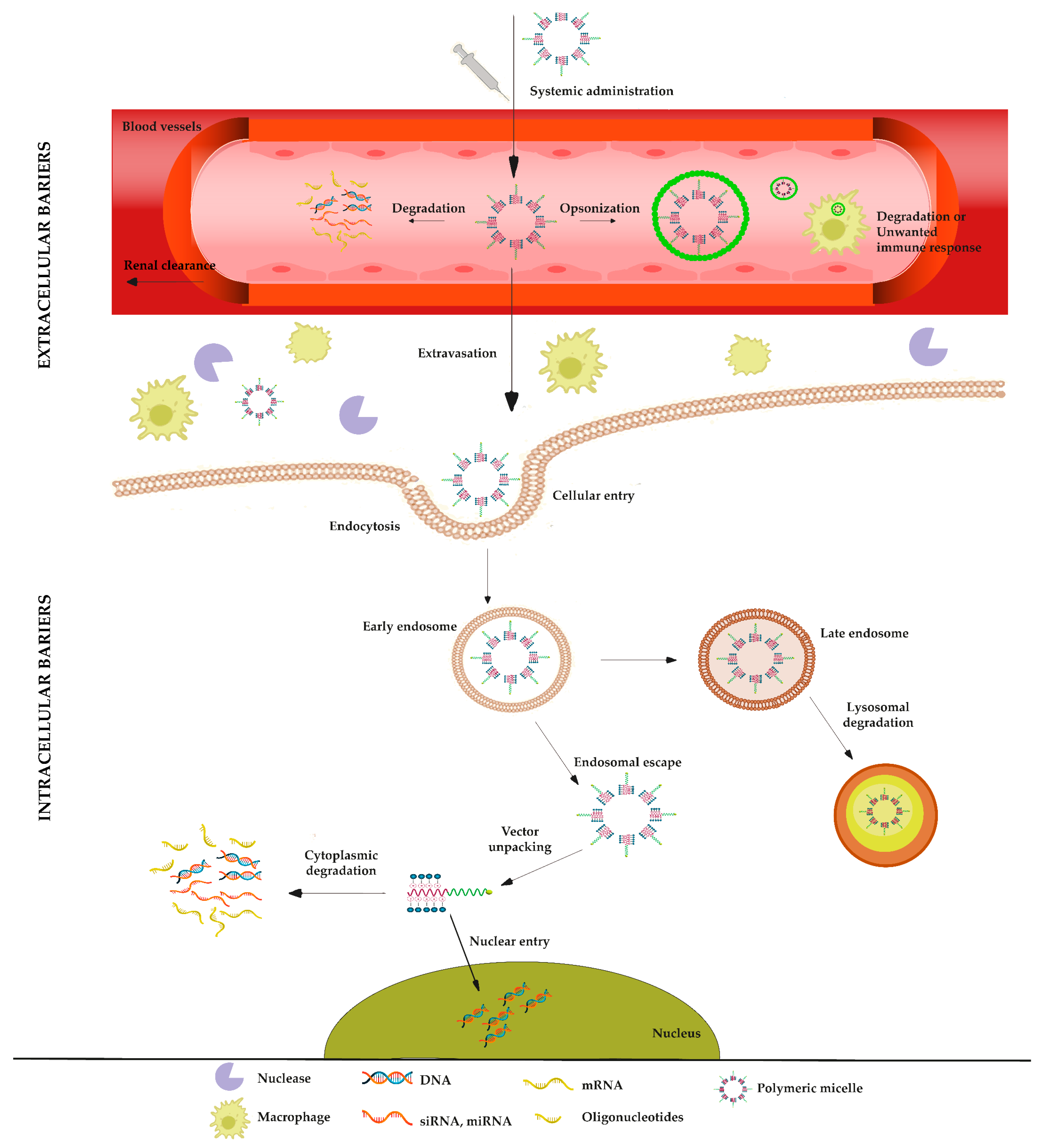
3. Challenges in Delivering Nucleic Acids
3.1. Extracellular Barriers
3.1.1. Nuclease Degradation
3.1.2. Clearance Mechanisms
3.2. Intracellular Barriers
3.2.1. Cellular Uptake
3.2.2. Endosomal Escape
3.2.3. Vector Unpacking
3.2.4. Intracellular Transport
4. Polymeric Micelles for Nucleic Acid Delivery
4.1. Polymers and Modifying Agents in Polymeric Micelles
4.2. Plasmid DNA (pDNA) Delivery
4.3. Messenger RNA (mRNA) Delivery
4.4. Antisense Oligonucleotide (ASO) Delivery
4.5. Small Interfering RNA (siRNA) Delivery
5. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodriguez, A.; Del, A.; Angeles, M. Non-Viral Delivery Systems in Gene Therapy. In Gene Therapy—Tools and Potential Applications; InTech: London, UK, 2013. [Google Scholar]
- Kulkarni, J.A.; Witzigmann, D.; Thomson, S.B.; Chen, S.; Leavitt, B.R.; Cullis, P.R.; van der Meel, R. The current landscape of nucleic acid therapeutics. Nat. Nanotechnol. 2021, 16, 630–643. [Google Scholar] [CrossRef]
- Escors, D.; Breckpot, K. Lentiviral Vectors in Gene Therapy: Their Current Status and Future Potential. Arch. Immunol. Ther. Exp. 2010, 58, 107–119. [Google Scholar] [CrossRef]
- Pan, X.; Veroniaina, H.; Su, N.; Sha, K.; Jiang, F.; Wu, Z.; Qi, X. Applications and developments of gene therapy drug delivery systems for genetic diseases. Asian J. Pharm. Sci. 2021, 16, 687–703. [Google Scholar] [CrossRef]
- Cevher, E.; Demir, A.; Sefik, E. Gene Delivery Systems: Recent Progress in Viral and Non-Viral Therapy. In Recent Advances in Novel Drug Carrier Systems; InTech: London, UK, 2012. [Google Scholar]
- Mirón-Barroso, S.; Domènech, E.B.; Trigueros, S. Nanotechnology-Based Strategies to Overcome Current Barriers in Gene Delivery. Int. J. Mol. Sci. 2021, 22, 8537. [Google Scholar] [CrossRef] [PubMed]
- Sung, Y.; Kim, S. Recent advances in the development of gene delivery systems. Biomater. Res. 2019, 23, 8. [Google Scholar] [CrossRef] [PubMed]
- Jarak, I.; Pereira-Silva, M.; Santos, A.C.; Veiga, F.; Cabral, H.; Figueiras, A. Multifunctional polymeric micelle-based nucleic acid delivery: Current advances and future perspectives. Appl. Mater. Today 2021, 25, 101217. [Google Scholar] [CrossRef]
- Durgun, M.E.; Güngör, S.; Özsoy, Y. Micelles: Promising Ocular Drug Carriers for Anterior and Posterior Segment Diseases. J. Ocul. Pharmacol. Ther. 2020, 36, 323–341. [Google Scholar] [CrossRef]
- U.S. National Library of Medicine PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov (accessed on 25 March 2023).
- Kahraman, E.; Durgun, M.E.; Güngör, S.; Özsoy, Y. Polymeric micellar nanocarriers: Topical treatment of inflammatory diseases. In Polymeric Micelles for Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2022; pp. 115–143. [Google Scholar]
- Kulthe, S.S.; Choudhari, Y.M.; Inamdar, N.N.; Mourya, V. Polymeric micelles: Authoritative aspects for drug delivery. Des. Monomers Polym. 2012, 15, 465–521. [Google Scholar] [CrossRef]
- Pérez, S.E.; Haidar, Z.S. Polymeric micelles: Précis for past, present and future. In Polymeric Micelles for Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2022; pp. 3–14. [Google Scholar]
- Raja, M.A.G. Various polymers in the development of polymeric micelles. In Polymeric Micelles for Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2022; pp. 15–40. [Google Scholar]
- Bodratti, A.M.; Alexandridis, P. Amphiphilic block copolymers in drug delivery: Advances in formulation structure and performance. Expert Opin. Drug Deliv. 2018, 15, 1085–1104. [Google Scholar] [CrossRef]
- Pereira-Silva, M.; Jarak, I.; Alvarez-Lorenzo, C.; Concheiro, A.; Santos, A.C.; Veiga, F.; Figueiras, A. Micelleplexes as nucleic acid delivery systems for cancer-targeted therapies. J. Control. Release 2020, 323, 442–462. [Google Scholar] [CrossRef]
- Özsoy, Y.; Güngör, S.; Kahraman, E.; Durgun, M.E. Polymeric micelles as a novel carrier for ocular drug delivery. In Nanoarchitectonics in Biomedicine; Elsevier: Amsterdam, The Netherlands, 2019; pp. 85–117. [Google Scholar]
- Bai, K.; Wang, A. Polymeric Micelles: Morphology, Synthesis, and Pharmaceutical Application. E3S Web Conf. 2021, 290, 01029. [Google Scholar] [CrossRef]
- Pham, D.T.; Chokamonsirikun, A.; Phattaravorakarn, V.; Tiyaboonchai, W. Polymeric micelles for pulmonary drug delivery: A comprehensive review. J. Mater. Sci. 2021, 56, 2016–2036. [Google Scholar] [CrossRef]
- Ding, J.; Chen, L.; Xiao, C.; Chen, L.; Zhuang, X.; Chen, X. Noncovalent interaction-assisted polymeric micelles for controlled drug delivery. Chem. Commun. 2014, 50, 11274–11290. [Google Scholar] [CrossRef] [PubMed]
- Harada, A.; Kataoka, K. Formation of Polyion Complex Micelles in an Aqueous Milieu from a Pair of Oppositely-Charged Block Copolymers with Poly(ethylene glycol) Segments. Macromolecules 1995, 28, 5294–5299. [Google Scholar] [CrossRef]
- Kabanov, A.V.; Bronich, T.K.; Kabanov, V.A.; Yu, K.; Eisenberg, A. Soluble Stoichiometric Complexes from Poly(N-ethyl-4-vinylpyridinium) Cations and Poly(ethylene oxide)-block-polymethacrylate Anions. Macromolecules 1996, 29, 6797–6802. [Google Scholar] [CrossRef]
- Cohen Stuart, M.A.; Besseling, N.A.M.; Fokkink, R.G. Formation of Micelles with Complex Coacervate Cores. Langmuir 1998, 14, 6846–6849. [Google Scholar] [CrossRef]
- Pergushov, D.V.; Remizova, E.V.; Gradzielski, M.; Lindner, P.; Feldthusen, J.; Zezin, A.B.; Müller, A.H.E.; Kabanov, V.A. Micelles of polyisobutylene-block-poly(methacrylic acid) diblock copolymers and their water-soluble interpolyelectrolyte complexes formed with quaternized poly(4-vinylpyridine). Polymer 2004, 45, 367–378. [Google Scholar] [CrossRef]
- Gohy, J.-F.; Creutz, S.; Garcia, M.; Mahltig, B.; Stamm, M.; Jérôme, R. Aggregates Formed by Amphoteric Diblock Copolymers in Water. Macromolecules 2000, 33, 6378–6387. [Google Scholar] [CrossRef]
- Harada, A.; Kataoka, K. Polyion complex micelle formation from double-hydrophilic block copolymers composed of charged and non-charged segments in aqueous media. Polym. J. 2018, 50, 95–100. [Google Scholar] [CrossRef]
- Kalinova, R.; Dimitrov, I. Functional Polyion Complex Micelles for Potential Targeted Hydrophobic Drug Delivery. Molecules 2022, 27, 2178. [Google Scholar] [CrossRef]
- Pereira-Silva, M.; Jarak, I.; Santos, A.C.; Veiga, F.; Figueiras, A. Micelleplex-based nucleic acid therapeutics: From targeted stimuli-responsiveness to nanotoxicity and regulation. Eur. J. Pharm. Sci. 2020, 153, 105461. [Google Scholar] [CrossRef]
- Kumar, R.; Santa Chalarca, C.F.; Bockman, M.R.; Van Bruggen, C.; Grimme, C.J.; Dalal, R.J.; Hanson, M.G.; Hexum, J.K.; Reineke, T.M. Polymeric Delivery of Therapeutic Nucleic Acids. Chem. Rev. 2021, 121, 11527–11652. [Google Scholar] [CrossRef] [PubMed]
- Mandal, A.; Bisht, R.; Rupenthal, I.D.; Mitra, A.K. Polymeric micelles for ocular drug delivery: From structural frameworks to recent preclinical studies. J. Control. Release 2017, 248, 96–116. [Google Scholar] [CrossRef] [PubMed]
- Hlavatovičová, E.; Fernandez-Alvarez, R.; Byś, K.; Kereïche, S.; Mandal, T.K.; Atanase, L.I.; Štěpánek, M.; Uchman, M. Stimuli-Responsive Triblock Terpolymer Conversion into Multi-Stimuli-Responsive Micelles with Dynamic Covalent Bonds for Drug Delivery through a Quick and Controllable Post-Polymerization Reaction. Pharmaceutics 2023, 15, 288. [Google Scholar] [CrossRef] [PubMed]
- Cagel, M.; Tesan, F.C.; Bernabeu, E.; Salgueiro, M.J.; Zubillaga, M.B.; Moretton, M.A.; Chiappetta, D.A. Polymeric mixed micelles as nanomedicines: Achievements and perspectives. Eur. J. Pharm. Biopharm. 2017, 113, 211–228. [Google Scholar] [CrossRef]
- Schröder, M.; Petrova, M.; Dobrikov, G.M.; Grancharov, G.; Momekova, D.; Petrov, P.D.; Ugrinova, I. Micellar Form of a Ferrocene-Containing Camphor Sulfonamide with Improved Aqueous Solubility and Tumor Curing Potential. Pharmaceutics 2023, 15, 791. [Google Scholar] [CrossRef] [PubMed]
- Debele, T.A.; Chen, C.-K.; Yu, L.-Y.; Lo, C.-L. Lipopolyplex-Mediated Co-Delivery of Doxorubicin and FAK siRNA to Enhance Therapeutic Efficiency of Treating Colorectal Cancer. Pharmaceutics 2023, 15, 596. [Google Scholar] [CrossRef]
- Bryaskova, R.; Georgiev, N.; Philipova, N.; Bakov, V.; Anichina, K.; Argirova, M.; Apostolova, S.; Georgieva, I.; Tzoneva, R. Novel Fluorescent Benzimidazole-Hydrazone-Loaded Micellar Carriers for Controlled Release: Impact on Cell Toxicity, Nuclear and Microtubule Alterations in Breast Cancer Cells. Pharmaceutics 2023, 15, 1753. [Google Scholar] [CrossRef]
- Stancheva, R.; Paunova-Krasteva, T.; Topouzova-Hristova, T.; Stoitsova, S.; Petrov, P.; Haladjova, E. Ciprofloxacin-Loaded Mixed Polymeric Micelles as Antibiofilm Agents. Pharmaceutics 2023, 15, 1147. [Google Scholar] [CrossRef]
- Quartier, J.; Lapteva, M.; Boulaguiem, Y.; Guerrier, S.; Kalia, Y.N. Influence of Molecular Structure and Physicochemical Properties of Immunosuppressive Drugs on Micelle Formulation Characteristics and Cutaneous Delivery. Pharmaceutics 2023, 15, 1278. [Google Scholar] [CrossRef]
- Radeva, L.; Yordanov, Y.; Spassova, I.; Kovacheva, D.; Tzankova, V.; Yoncheva, K. Double-Loaded Doxorubicin/Resveratrol Polymeric Micelles Providing Low Toxicity on Cardiac Cells and Enhanced Cytotoxicity on Lymphoma Cells. Pharmaceutics 2023, 15, 1287. [Google Scholar] [CrossRef]
- Fournier, E.; Dufresne, M.-H.; Smith, D.C.; Ranger, M.; Leroux, J.-C. A Novel One-Step Drug-Loading Procedure for Water-Soluble Amphiphilic Nanocarriers. Pharm. Res. 2004, 21, 962–968. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.E.; Yoon, M.S.; Jo, M.J.; Kim, S.Y.; Lee, J.M.; Kang, S.J.; Park, C.-W.; Kim, J.-S.; Shin, D.H. Synergistic Encapsulation of Paclitaxel and Sorafenib by Methoxy Poly(Ethylene Glycol)-b-Poly(Caprolactone) Polymeric Micelles for Ovarian Cancer Therapy. Pharmaceutics 2023, 15, 1206. [Google Scholar] [CrossRef]
- Algar, W.R. A Brief Introduction to Traditional Bioconjugate Chemistry. In Chemoselective and Bioorthogonal Ligation Reactions; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2017; pp. 1–36. [Google Scholar]
- Nerantzaki, M.; Loth, C.; Lutz, J.-F. Chemical conjugation of nucleic acid aptamers and synthetic polymers. Polym. Chem. 2021, 12, 3498–3509. [Google Scholar] [CrossRef]
- Musacchio, T.; Vaze, O.; D’Souza, G.; Torchilin, V.P. Effective Stabilization and Delivery of siRNA: Reversible siRNA−Phospholipid Conjugate in Nanosized Mixed Polymeric Micelles. Bioconjug. Chem. 2010, 21, 1530–1536. [Google Scholar] [CrossRef] [PubMed]
- Salzano, G.; Riehle, R.; Navarro, G.; Perche, F.; De Rosa, G.; Torchilin, V.P. Polymeric micelles containing reversibly phospholipid-modified anti-survivin siRNA: A promising strategy to overcome drug resistance in cancer. Cancer Lett. 2014, 343, 224–231. [Google Scholar] [CrossRef]
- Jiang, T.; Qiao, Y.; Ruan, W.; Zhang, D.; Yang, Q.; Wang, G.; Chen, Q.; Zhu, F.; Yin, J.; Zou, Y.; et al. Cation-Free siRNA Micelles as Effective Drug Delivery Platform and Potent RNAi Nanomedicines for Glioblastoma Therapy. Adv. Mater. 2021, 33, 2104779. [Google Scholar] [CrossRef]
- Hazekawa, M.; Nishinakagawa, T.; Kawakubo-Yasukochi, T.; Nakashima, M. Glypican-3 gene silencing for ovarian cancer using siRNA-PLGA hybrid micelles in a murine peritoneal dissemination model. J. Pharmacol. Sci. 2019, 139, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Hazekawa, M.; Nishinakagawa, T.; Mori, T.; Yoshida, M.; Uchida, T.; Ishibashi, D. Preparation of siRNA–PLGA/Fab’–PLGA mixed micellar system with target cell-specific recognition. Sci. Rep. 2021, 11, 16789. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xia, X.; Dong, W.; Wang, H.; Li, L.; Ma, P.; Sheng, W.; Xu, X.; Liu, Y. Acid Sensitive Polymeric Micelles Combining Folate and Bioreducible Conjugate for Specific Intracellular siRNA Delivery. Macromol. Biosci. 2016, 16, 759–773. [Google Scholar] [CrossRef]
- Chin, D.D.; Poon, C.; Wang, J.; Joo, J.; Ong, V.; Jiang, Z.; Cheng, K.; Plotkin, A.; Magee, G.A.; Chung, E.J. miR-145 micelles mitigate atherosclerosis by modulating vascular smooth muscle cell phenotype. Biomaterials 2021, 273, 120810. [Google Scholar] [CrossRef] [PubMed]
- Salzano, G.; Costa, D.F.; Sarisozen, C.; Luther, E.; Mattheolabakis, G.; Dhargalkar, P.P.; Torchilin, V.P. Mixed Nanosized Polymeric Micelles as Promoter of Doxorubicin and miRNA-34a Co-Delivery Triggered by Dual Stimuli in Tumor Tissue. Small 2016, 12, 4837–4848. [Google Scholar] [CrossRef] [PubMed]
- Pezzoli, D.; Giupponi, E.; Mantovani, D.; Candiani, G. Size matters for in vitro gene delivery: Investigating the relationships among complexation protocol, transfection medium, size and sedimentation. Sci. Rep. 2017, 7, 44134. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yue, S.; Cao, J.; Zhu, C.; Wang, Y.; Hai, X.; Song, W.; Bi, S. pH-responsive DNA nanomicelles for chemo-gene Synergetic Therapy of Anaplastic Large Cell Lymphoma. Theranostics 2020, 10, 8250–8263. [Google Scholar] [CrossRef]
- Liu, H.; Zhu, Z.; Kang, H.; Wu, Y.; Sefan, K.; Tan, W. DNA-Based Micelles: Synthesis, Micellar Properties and Size-Dependent Cell Permeability. Chem.—A Eur. J. 2010, 16, 3791–3797. [Google Scholar] [CrossRef]
- Ni, Q.; Zhang, F.; Zhang, Y.; Zhu, G.; Wang, Z.; Teng, Z.; Wang, C.; Yung, B.C.; Niu, G.; Lu, G.; et al. In Situ shRNA Synthesis on DNA-Polylactide Nanoparticles to Treat Multidrug Resistant Breast Cancer. Adv. Mater. 2018, 30, 1705737. [Google Scholar] [CrossRef]
- Feldmann, D.P.; Xie, Y.; Jones, S.K.; Yu, D.; Moszczynska, A.; Merkel, O.M. The impact of microfluidic mixing of triblock micelleplexes on in vitro / in vivo gene silencing and intracellular trafficking. Nanotechnology 2017, 28, 224001. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Wang, Y.; Shi, H.; Dong, M.; Han, H.; Li, Q. Nucleolin-Targeting AS1411 Aptamer-Modified Micelle for the Co-Delivery of Doxorubicin and miR-519c to Improve the Therapeutic Efficacy in Hepatocellular Carcinoma Treatment. Int. J. Nanomed. 2021, 16, 2569–2584. [Google Scholar] [CrossRef]
- Jhaveri, A.M.; Torchilin, V.P. Multifunctional polymeric micelles for delivery of drugs and siRNA. Front. Pharmacol. 2014, 5, 77. [Google Scholar] [CrossRef]
- Wautier, J.-L.; Wautier, M.-P. Vascular Permeability in Diseases. Int. J. Mol. Sci. 2022, 23, 3645. [Google Scholar] [CrossRef]
- Cloutier, N.; Paré, A.; Farndale, R.W.; Schumacher, H.R.; Nigrovic, P.A.; Lacroix, S.; Boilard, E. Platelets can enhance vascular permeability. Blood 2012, 120, 1334–1343. [Google Scholar] [CrossRef] [PubMed]
- Park-Windhol, C.; D’Amore, P.A. Disorders of Vascular Permeability. Annu. Rev. Pathol. Mech. Dis. 2016, 11, 251–281. [Google Scholar] [CrossRef] [PubMed]
- Ghezzi, M.; Pescina, S.; Padula, C.; Santi, P.; Del Favero, E.; Cantù, L.; Nicoli, S. Polymeric micelles in drug delivery: An insight of the techniques for their characterization and assessment in biorelevant conditions. J. Control. Release 2021, 332, 312–336. [Google Scholar] [CrossRef]
- Bandi, S.P.; Kumbhar, Y.S.; Venuganti, V.V.K. Effect of particle size and surface charge of nanoparticles in penetration through intestinal mucus barrier. J. Nanopartic. Res. 2020, 22, 62. [Google Scholar] [CrossRef]
- Taipaleenmäki, E.; Brodszkij, E.; Städler, B. Mucopenetrating Zwitterionic Micelles. ChemNanoMat 2020, 6, 744–750. [Google Scholar] [CrossRef]
- Honary, S.; Zahir, F. Effect of Zeta Potential on the Properties of Nano-Drug Delivery Systems—A Review (Part 2). Trop. J. Pharm. Res. 2013, 12, 265–273. [Google Scholar] [CrossRef]
- Jubeh, T.T.; Barenholz, Y.; Rubinstein, A. Differential Adhesion of Normal and Inflamed Rat Colonic Mucosa by Charged Liposomes. Pharm. Res. 2004, 21, 447–453. [Google Scholar] [CrossRef]
- Amjad, M.W.; Kesharwani, P.; Mohd Amin, M.C.I.; Iyer, A.K. Recent advances in the design, development, and targeting mechanisms of polymeric micelles for delivery of siRNA in cancer therapy. Prog. Polym. Sci. 2017, 64, 154–181. [Google Scholar] [CrossRef]
- Huo, H.; Gao, Y.; Wang, Y.; Zhang, J.; Wang, Z.; Jiang, T.; Wang, S. Polyion complex micelles composed of pegylated polyasparthydrazide derivatives for siRNA delivery to the brain. J. Colloid Interface Sci. 2015, 447, 8–15. [Google Scholar] [CrossRef]
- Shim, M.S.; Kwon, Y.J. Stimuli-responsive polymers and nanomaterials for gene delivery and imaging applications. Adv. Drug Deliv. Rev. 2012, 64, 1046–1059. [Google Scholar] [CrossRef]
- Du, F.-S.; Wang, Y.; Zhang, R.; Li, Z.-C. Intelligent nucleic acid delivery systems based on stimuli-responsive polymers. Soft Matter 2010, 6, 835–848. [Google Scholar] [CrossRef]
- Pittella, F.; Kataoka, K. Polymeric Micelles for siRNA Delivery; Springer: Boston, MA, USA, 2013; pp. 161–184. [Google Scholar]
- Bawa, P.; Pillay, V.; Choonara, Y.E.; du Toit, L.C. Stimuli-responsive polymers and their applications in drug delivery. Biomed. Mater. 2009, 4, 022001. [Google Scholar] [CrossRef] [PubMed]
- Forrester, S.J.; Kikuchi, D.S.; Hernandes, M.S.; Xu, Q.; Griendling, K.K. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ. Res. 2018, 122, 877–902. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Qi, H.; Liu, Y.; Duan, C.; Liu, X.; Xia, T.; Chen, D.; Piao, H.; Liu, H.-X. The double-edged roles of ROS in cancer prevention and therapy. Theranostics 2021, 11, 4839–4857. [Google Scholar] [CrossRef]
- Lin, M.; Qi, X. Advances and Challenges of Stimuli-Responsive Nucleic Acids Delivery System in Gene Therapy. Pharmaceutics 2023, 15, 1450. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Zhang, L.; Yang, T.; Wu, H. Stimuli-responsive polymeric micelles for drug delivery and cancer therapy. Int. J. Nanomed. 2018, 13, 2921–2942. [Google Scholar] [CrossRef]
- Kessenbrock, K.; Plaks, V.; Werb, Z. Matrix Metalloproteinases: Regulators of the Tumor Microenvironment. Cell 2010, 141, 52–67. [Google Scholar] [CrossRef]
- Park, J.B.; Lee, C.S.; Jang, J.-H.; Ghim, J.; Kim, Y.-J.; You, S.; Hwang, D.; Suh, P.-G.; Ryu, S.H. Phospholipase signalling networks in cancer. Nat. Rev. Cancer 2012, 12, 782–792. [Google Scholar] [CrossRef]
- Colotta, F.; Allavena, P.; Sica, A.; Garlanda, C.; Mantovani, A. Cancer-related inflammation, the seventh hallmark of cancer: Links to genetic instability. Carcinogenesis 2009, 30, 1073–1081. [Google Scholar] [CrossRef]
- Nakayama, M.; Okano, T.; Miyazaki, T.; Kohori, F.; Sakai, K.; Yokoyama, M. Molecular design of biodegradable polymeric micelles for temperature-responsive drug release. J. Control. Release 2006, 115, 46–56. [Google Scholar] [CrossRef]
- Mastrobattista, E.; Hennink, W.E.; Schiffelers, R.M. Delivery of Nucleic Acids. Pharm. Res. 2007, 24, 1561–1563. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, A.I.S.; Yun, C.-O.; Schiffelers, R.M.; Hennink, W.E. Polymeric delivery systems for nucleic acid therapeutics: Approaching the clinic. J. Control. Release 2021, 331, 121–141. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.H.; Lim, S.; Wong, W.F. Antisense Oligoucleotides: From Design To Therapeutic Application. Clin. Exp. Pharmacol. Physiol. 2006, 33, 533–540. [Google Scholar] [CrossRef]
- Khvorova, A.; Watts, J.K. The chemical evolution of oligonucleotide therapies of clinical utility. Nat. Biotechnol. 2017, 35, 238–248. [Google Scholar] [CrossRef]
- Shen, X.; Corey, D.R. Chemistry, mechanism and clinical status of antisense oligonucleotides and duplex RNAs. Nucleic Acids Res. 2018, 46, 1584–1600. [Google Scholar] [CrossRef] [PubMed]
- Harada-Shiba, M.; Yamauchi, K.; Harada, A.; Takamisawa, I.; Shimokado, K.; Kataoka, K. Polyion complex micelles as vectors in gene therapy—Pharmacokinetics and in vivo gene transfer. Gene Ther. 2002, 9, 407–414. [Google Scholar] [CrossRef]
- Sanati, S.; Taghavi, S.; Abnous, K.; Taghdisi, S.M.; Babaei, M.; Ramezani, M.; Alibolandi, M. Fabrication of anionic dextran-coated micelles for aptamer targeted delivery of camptothecin and survivin-shRNA to colon adenocarcinoma. Gene Ther. 2022, 29, 55–68. [Google Scholar] [CrossRef]
- Chen, Q.; Qi, R.; Chen, X.; Yang, X.; Wu, S.; Xiao, H.; Dong, W. A Targeted and Stable Polymeric Nanoformulation Enhances Systemic Delivery of mRNA to Tumors. Mol. Ther. 2017, 25, 92–101. [Google Scholar] [CrossRef]
- Yen, A.; Cheng, Y.; Sylvestre, M.; Gustafson, H.H.; Puri, S.; Pun, S.H. Serum Nuclease Susceptibility of mRNA Cargo in Condensed Polyplexes. Mol. Pharm. 2018, 15, 2268–2276. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, H.; Chan, D.W.H.; Ma, Y.; Lu, A.; Yu, S.; Zhang, B.; Zhang, G. Strategies for developing long-lasting therapeutic nucleic acid aptamer targeting circulating protein: The present and the future. Front. Cell Dev. Biol. 2022, 10, 1048148. [Google Scholar] [CrossRef]
- Owens, D.E.; Peppas, N.A. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int. J. Pharm. 2006, 307, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, Y.; Nagasaki, Y. Impacts of PEGylation on the gene and oligonucleotide delivery system. J. Appl. Polym. Sci. 2014, 131. [Google Scholar] [CrossRef]
- Miteva, M.; Kirkbride, K.C.; Kilchrist, K.V.; Werfel, T.A.; Li, H.; Nelson, C.E.; Gupta, M.K.; Giorgio, T.D.; Duvall, C.L. Tuning PEGylation of mixed micelles to overcome intracellular and systemic siRNA delivery barriers. Biomaterials 2015, 38, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Tockary, T.A.; Osada, K.; Chen, Q.; Machitani, K.; Dirisala, A.; Uchida, S.; Nomoto, T.; Toh, K.; Matsumoto, Y.; Itaka, K.; et al. Tethered PEG Crowdedness Determining Shape and Blood Circulation Profile of Polyplex Micelle Gene Carriers. Macromolecules 2013, 46, 6585–6592. [Google Scholar] [CrossRef]
- Ge, Z.; Chen, Q.; Osada, K.; Liu, X.; Tockary, T.A.; Uchida, S.; Dirisala, A.; Ishii, T.; Nomoto, T.; Toh, K.; et al. Targeted gene delivery by polyplex micelles with crowded PEG palisade and cRGD moiety for systemic treatment of pancreatic tumors. Biomaterials 2014, 35, 3416–3426. [Google Scholar] [CrossRef]
- Abbasi, S.; Uchida, S.; Toh, K.; Tockary, T.A.; Dirisala, A.; Hayashi, K.; Fukushima, S.; Kataoka, K. Co-encapsulation of Cas9 mRNA and guide RNA in polyplex micelles enables genome editing in mouse brain. J. Control. Release 2021, 332, 260–268. [Google Scholar] [CrossRef]
- Grun, M.K.; Suberi, A.; Shin, K.; Lee, T.; Gomerdinger, V.; Moscato, Z.M.; Piotrowski-Daspit, A.S.; Saltzman, W.M. PEGylation of poly(amine-co-ester) polyplexes for tunable gene delivery. Biomaterials 2021, 272, 120780. [Google Scholar] [CrossRef]
- Shi, D.; Beasock, D.; Fessler, A.; Szebeni, J.; Ljubimova, J.Y.; Afonin, K.A.; Dobrovolskaia, M.A. To PEGylate or not to PEGylate: Immunological properties of nanomedicine’s most popular component, polyethylene glycol and its alternatives. Adv. Drug Deliv. Rev. 2022, 180, 114079. [Google Scholar] [CrossRef]
- Nouri, F.S.; Wang, X.; Chen, X.; Hatefi, A. Reducing the Visibility of the Vector/DNA Nanocomplexes to the Immune System by Elastin-Like Peptides. Pharm. Res. 2015, 32, 3018–3028. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, J.; Meng, F.; Cheng, L.; Feijen, J.; Zhong, Z. Reduction-responsive core-crosslinked hyaluronic acid-b-poly(trimethylene carbonate-co-dithiolane trimethylene carbonate) micelles: Synthesis and CD44-mediated potent delivery of docetaxel to triple negative breast tumor in vivo. J. Mater. Chem. B 2018, 6, 3040–3047. [Google Scholar] [CrossRef]
- Wang, J.; Li, Y.; Wang, L.; Wang, X.; Tu, P. Comparison of hyaluronic acid-based micelles and polyethylene glycol-based micelles on reversal of multidrug resistance and enhanced anticancer efficacy in vitro and in vivo. Drug Deliv. 2018, 25, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhou, S.; Ge, L.; Wu, W.; Jiang, X. Translatable High Drug Loading Drug Delivery Systems Based on Biocompatible Polymer Nanocarriers. Biomacromolecules 2018, 19, 1732–1745. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, A.; Harashima, H. Endocytosis of Gene Delivery Vectors: From Clathrin-dependent to Lipid Raft-mediated Endocytosis. Mol. Ther. 2013, 21, 1118–1130. [Google Scholar] [CrossRef] [PubMed]
- Rennick, J.J.; Johnston, A.P.R.; Parton, R.G. Key principles and methods for studying the endocytosis of biological and nanoparticle therapeutics. Nat. Nanotechnol. 2021, 16, 266–276. [Google Scholar] [CrossRef]
- Billiet, L.; Gomez, J.-P.; Berchel, M.; Jaffrès, P.-A.; Le Gall, T.; Montier, T.; Bertrand, E.; Cheradame, H.; Guégan, P.; Mével, M.; et al. Gene transfer by chemical vectors, and endocytosis routes of polyplexes, lipoplexes and lipopolyplexes in a myoblast cell line. Biomaterials 2012, 33, 2980–2990. [Google Scholar] [CrossRef]
- Manzanares, D.; Ceña, V. Endocytosis: The Nanoparticle and Submicron Nanocompounds Gateway into the Cell. Pharmaceutics 2020, 12, 371. [Google Scholar] [CrossRef]
- Sahay, G.; Batrakova, E.V.; Kabanov, A.V. Different Internalization Pathways of Polymeric Micelles and Unimers and Their Effects on Vesicular Transport. Bioconjug. Chem. 2008, 19, 2023–2029. [Google Scholar] [CrossRef]
- Zhao, J.; Lu, H.; Yao, Y.; Ganda, S.; Stenzel, M.H. Length vs. stiffness: Which plays a dominant role in the cellular uptake of fructose-based rod-like micelles by breast cancer cells in 2D and 3D cell culture models? J. Mater. Chem. B 2018, 6, 4223–4231. [Google Scholar] [CrossRef]
- El Jundi, A.; Morille, M.; Bettache, N.; Bethry, A.; Berthelot, J.; Salvador, J.; Hunger, S.; Bakkour, Y.; Belamie, E.; Nottelet, B. Degradable double hydrophilic block copolymers and tripartite polyionic complex micelles thereof for small interfering ribonucleic acids (siRNA) delivery. J. Colloid Interface Sci. 2020, 580, 449–459. [Google Scholar] [CrossRef]
- Mitchell, M.J.; Billingsley, M.M.; Haley, R.M.; Wechsler, M.E.; Peppas, N.A.; Langer, R. Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discov. 2021, 20, 101–124. [Google Scholar] [CrossRef]
- Lin, W.J.; Lee, W.-C.; Shieh, M.-J. Hyaluronic acid conjugated micelles possessing CD44 targeting potential for gene delivery. Carbohydr. Polym. 2017, 155, 101–108. [Google Scholar] [CrossRef]
- Du, Y.Z.; Cai, L.L.; Li, J.; Zhao, M.D.; Chen, F.Y.; Yuan, H.; Hu, F.Q. Receptor-mediated gene delivery by folic acid-modified stearic acid-grafted chitosan micelles. Int. J. Nanomed. 2011, 6, 1559–1568. [Google Scholar] [CrossRef]
- Dai, J.; Zou, S.; Pei, Y.; Cheng, D.; Ai, H.; Shuai, X. Polyethylenimine-grafted copolymer of poly(l-lysine) and poly(ethylene glycol) for gene delivery. Biomaterials 2011, 32, 1694–1705. [Google Scholar] [CrossRef] [PubMed]
- Qian, Z.M. Targeted Drug Delivery via the Transferrin Receptor-Mediated Endocytosis Pathway. Pharmacol. Rev. 2002, 54, 561–587. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.-A.; Xin, X.; Liu, C.; Liu, Y.; Duan, H.-X.; Qi, L.; Zhang, Y.-Y.; Zhao, H.; Chen, L.-Q.; Jin, M.-J.; et al. Novel brain-targeted nanomicelles for anti-glioma therapy mediated by the ApoE-enriched protein corona in vivo. J. Nanobiotechnol. 2021, 19, 453. [Google Scholar] [CrossRef]
- Choi, M.; Thuy, L.T.; Lee, Y.; Piao, C.; Choi, J.S.; Lee, M. Dual-Functional Dendrimer Micelles with Glycyrrhizic Acid for Anti-Inflammatory Therapy of Acute Lung Injury. ACS Appl. Mater. Interfaces 2021, 13, 47313–47326. [Google Scholar] [CrossRef]
- Jeger, J.L. Endosomes, lysosomes, and the role of endosomal and lysosomal biogenesis in cancer development. Mol. Biol. Rep. 2020, 47, 9801–9810. [Google Scholar] [CrossRef] [PubMed]
- Winkeljann, B.; Keul, D.C.; Merkel, O.M. Engineering poly- and micelleplexes for nucleic acid delivery—A reflection on their endosomal escape. J. Control. Release 2023, 353, 518–534. [Google Scholar] [CrossRef]
- Vermeulen, L.M.P.; De Smedt, S.C.; Remaut, K.; Braeckmans, K. The proton sponge hypothesis: Fable or fact? Eur. J. Pharm. Biopharm. 2018, 129, 184–190. [Google Scholar] [CrossRef]
- Wagner, E.; Kloeckner, J. Gene Delivery Using Polymer Therapeutics. In Polymer Therapeutics I; Springer: Berlin/Heidelberg, Germany, 2006; pp. 135–173. [Google Scholar]
- Wojnilowicz, M.; Glab, A.; Bertucci, A.; Caruso, F.; Cavalieri, F. Super-resolution Imaging of Proton Sponge-Triggered Rupture of Endosomes and Cytosolic Release of Small Interfering RNA. ACS Nano 2019, 13, 187–202. [Google Scholar] [CrossRef]
- Miao, J.; Yang, X.; Shang, X.; Gao, Z.; Li, Q.; Hong, Y.; Wu, J.; Meng, T.; Yuan, H.; Hu, F. Hepatocyte-targeting and microenvironmentally responsive glycolipid-like polymer micelles for gene therapy of hepatitis B. Mol. Ther.—Nucleic Acids 2021, 24, 127–139. [Google Scholar] [CrossRef]
- Ahmad, A.; Khan, J.M.; Haque, S. Strategies in the design of endosomolytic agents for facilitating endosomal escape in nanoparticles. Biochimie 2019, 160, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Butt, A.M.; Abdullah, N.; Rani, N.N.I.M.; Ahmad, N.; Amin, M.C.I.M. Endosomal Escape of Bioactives Deployed via Nanocarriers: Insights Into the Design of Polymeric Micelles. Pharm. Res. 2022, 39, 1047–1064. [Google Scholar] [CrossRef] [PubMed]
- Schaffer, D.V.; Fidelman, N.A.; Dan, N.; Lauffenburger, D.A. Vector unpacking as a potential barrier for receptor-mediated polyplex gene delivery. Biotechnol. Bioeng. 2000, 67, 598–606. [Google Scholar] [CrossRef]
- Sherly, M.C.D.; Rekha, M.R.; Harikrishnan, V.S. Cationised dextran and pullulan modified with diethyl aminoethyl methacrylate for gene delivery in cancer cells. Carbohydr. Polym. 2020, 242, 116426. [Google Scholar] [CrossRef]
- Chen, H.H.; Ho, Y.-P.; Jiang, X.; Mao, H.-Q.; Wang, T.-H.; Leong, K.W. Quantitative Comparison of Intracellular Unpacking Kinetics of Polyplexes by a Model Constructed From Quantum Dot-FRET. Mol. Ther. 2008, 16, 324–332. [Google Scholar] [CrossRef]
- Grigsby, C.L.; Leong, K.W. Balancing protection and release of DNA: Tools to address a bottleneck of non-viral gene delivery. J. R. Soc. Interface 2010, 7, S67–S82. [Google Scholar] [CrossRef]
- Dean, D.A.; Strong, D.D.; Zimmer, W.E. Nuclear entry of nonviral vectors. Gene Ther. 2005, 12, 881–890. [Google Scholar] [CrossRef]
- Remaut, K.; Lucas, B.; Braeckmans, K.; Sanders, N.N.; De Smedt, S.C.; Demeester, J. FRET-FCS as a tool to evaluate the stability of oligonucleotide drugs after intracellular delivery. J. Control. Release 2005, 103, 259–271. [Google Scholar] [CrossRef]
- Krivitsky, A.; Polyak, D.; Scomparin, A.; Eliyahu, S.; Ofek, P.; Tiram, G.; Kalinski, H.; Avkin-Nachum, S.; Feiner Gracia, N.; Albertazzi, L.; et al. Amphiphilic poly(α)glutamate polymeric micelles for systemic administration of siRNA to tumors. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 303–315. [Google Scholar] [CrossRef]
- Kokil, G.R.; Veedu, R.N.; Le, B.T.; Ramm, G.A.; Parekh, H.S. Self-assembling asymmetric peptide-dendrimer micelles—A platform for effective and versatile in vitro nucleic acid delivery. Sci. Rep. 2018, 8, 4832. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, Z.; Lin, C.-Y.; Liu, Y.; Staveley-OCarroll, K.F.; Li, G.; Cheng, K. Silencing PCBP2 normalizes desmoplastic stroma and improves the antitumor activity of chemotherapy in pancreatic cancer. Theranostics 2021, 11, 2182–2200. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Buhrman, J.S.; Liu, Y.; Rayahin, J.E.; Gemeinhart, R.A. Reducible Micelleplexes are Stable Systems for Anti-miRNA Delivery in Cerebrospinal Fluid. Mol. Pharm. 2016, 13, 1791–1799. [Google Scholar] [CrossRef]
- Pittella, F.; Miyata, K.; Maeda, Y.; Suma, T.; Watanabe, S.; Chen, Q.; Christie, R.J.; Osada, K.; Nishiyama, N.; Kataoka, K. Pancreatic cancer therapy by systemic administration of VEGF siRNA contained in calcium phosphate/charge-conversional polymer hybrid nanoparticles. J. Control. Release 2012, 161, 868–874. [Google Scholar] [CrossRef]
- Maeda, Y.; Pittella, F.; Nomoto, T.; Takemoto, H.; Nishiyama, N.; Miyata, K.; Kataoka, K. Fine-Tuning of Charge-Conversion Polymer Structure for Efficient Endosomal Escape of siRNA-Loaded Calcium Phosphate Hybrid Micelles. Macromol. Rapid Commun. 2014, 35, 1211–1215. [Google Scholar] [CrossRef]
- Aji Alex, M.R.; Nehate, C.; Veeranarayanan, S.; Kumar, D.S.; Kulshreshtha, R.; Koul, V. Self assembled dual responsive micelles stabilized with protein for co-delivery of drug and siRNA in cancer therapy. Biomaterials 2017, 133, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zhong, L.; Jiang, Z.; Pan, H.; Zhang, Y.; Zhu, G.; Bai, L.; Tong, R.; Shi, J.; Duan, X. Cationic micelle-based siRNA delivery for efficient colon cancer gene therapy. Nanoscale Res. Lett. 2019, 14, 193. [Google Scholar] [CrossRef]
- Nie, W.; Wang, B.; Mi, X.; Chen, J.; Yu, T.; Miao, J.; Lin, Y.; Yang, T.; Ran, M.; Hong, Z.; et al. Co-Delivery of Paclitaxel and shMCL-1 by Folic Acid-Modified Nonviral Vector to Overcome Cancer Chemotherapy Resistance. Small Methods 2021, 5, 2001132. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.-B.; Uludağ, H.; Lavasanifar, A. Biodegradable amphiphilic poly(ethylene oxide)-block-polyesters with grafted polyamines as supramolecular nanocarriers for efficient siRNA delivery. Biomaterials 2009, 30, 242–253. [Google Scholar] [CrossRef]
- Gao, J.; Zhang, H.; Zhou, F.; Hou, B.; Chen, M.; Xie, Z.; Yu, H. Acid-activatible micelleplex delivering siRNA-PD-L1 for improved cancer immunotherapy of CDK4/6 inhibition. Chin. Chem. Lett. 2021, 32, 1929–1936. [Google Scholar] [CrossRef]
- Sahoo, S.; Kayal, S.; Poddar, P.; Dhara, D. Redox-Responsive Efficient DNA and Drug Co-Release from Micelleplexes Formed from a Fluorescent Cationic Amphiphilic Polymer. Langmuir 2019, 35, 14616–14627. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, C.; Humanes, A.; Coiffier, C.; Gigmes, D.; Verrier, B.; Trimaille, T. Polylactide-Based Reactive Micelles as a Robust Platform for mRNA Delivery. Pharm. Res. 2020, 37, 30. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Guo, C.; Feng, B.; Liu, J.; Chen, X.; Wang, D.; Teng, L.; Li, Y.; Yin, Q.; Zhang, Z.; et al. Triple-Layered pH-Responsive Micelleplexes Loaded with siRNA and Cisplatin Prodrug for NF-Kappa B Targeted Treatment of Metastatic Breast Cancer. Theranostics 2016, 6, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-H.; Lin, M.-W.; Chien, M.-C.; Ke, G.-M.; Wu, I.-E.; Lin, R.-L.; Lin, C.-Y.; Hu, Y.-C. Polyplex nanomicelle delivery of self-amplifying RNA vaccine. J. Control. Release 2021, 338, 694–704. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Chen, X.; Xie, C.; Wang, Y.; Lin, L.; Zhu, K.; Shuai, X. Co-Delivery of Doxorubicin and Anti-BCL-2 siRNA by pH-Responsive Polymeric Vector to Overcome Drug Resistance in In Vitro and In Vivo HepG2 Hepatoma Model. Biomacromolecules 2018, 19, 2248–2256. [Google Scholar] [CrossRef]
- Aini, H.; Itaka, K.; Fujisawa, A.; Uchida, H.; Uchida, S.; Fukushima, S.; Kataoka, K.; Saito, T.; Chung, U.; Ohba, S. Messenger RNA delivery of a cartilage-anabolic transcription factor as a disease-modifying strategy for osteoarthritis treatment. Sci. Rep. 2016, 6, 18743. [Google Scholar] [CrossRef] [PubMed]
- Mondal, G.; Almawash, S.; Chaudhary, A.K.; Mahato, R.I. EGFR-Targeted Cationic Polymeric Mixed Micelles for Codelivery of Gemcitabine and miR-205 for Treating Advanced Pancreatic Cancer. Mol. Pharm. 2017, 14, 3121–3133. [Google Scholar] [CrossRef]
- Cao, Z.; Xiao, H.; Li, L.; Liu, M.; Lin, G.; Zhai, P.; Yong, K.-T.; Wang, X.; Xu, G. The Codelivery of siRNA and QDs by pH-Responsive Micelle for Hepatoma Cancer Cells. Front. Pharmacol. 2019, 10, 1194. [Google Scholar] [CrossRef]
- Zhu, C.; Jung, S.; Luo, S.; Meng, F.; Zhu, X.; Park, T.G.; Zhong, Z. Co-delivery of siRNA and paclitaxel into cancer cells by biodegradable cationic micelles based on PDMAEMA–PCL–PDMAEMA triblock copolymers. Biomaterials 2010, 31, 2408–2416. [Google Scholar] [CrossRef]
- Endres, T.; Zheng, M.; Kılıç, A.; Turowska, A.; Beck-Broichsitter, M.; Renz, H.; Merkel, O.M.; Kissel, T. Amphiphilic Biodegradable PEG-PCL-PEI Triblock Copolymers for FRET-Capable in Vitro and in Vivo Delivery of siRNA and Quantum Dots. Mol. Pharm. 2014, 11, 1273–1281. [Google Scholar] [CrossRef]
- Kanazawa, T.; Morisaki, K.; Suzuki, S.; Takashima, Y. Prolongation of Life in Rats with Malignant Glioma by Intranasal siRNA/Drug Codelivery to the Brain with Cell-Penetrating Peptide-Modified Micelles. Mol. Pharm. 2014, 11, 1471–1478. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Chen, L.; Qi, R.; Zhou, Z.; Deng, Z.; Shi, J.; Qin, T.; Zhao, S.; Qian, Y.; Shen, J. Simultaneous delivery of gene and chemotherapeutics via copolymeric micellar nanoparticles to overcome multiple drug resistance to promote synergistic tumor suppression. J. Biomater. Appl. 2019, 34, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.-M.; Du, J.-Z.; Yan, L.-F.; Mao, H.-Q.; Wang, J. Self-assembled biodegradable micellar nanoparticles of amphiphilic and cationic block copolymer for siRNA delivery. Biomaterials 2008, 29, 4348–4355. [Google Scholar] [CrossRef]
- Liu, X.-Q.; Xiong, M.-H.; Shu, X.-T.; Tang, R.-Z.; Wang, J. Therapeutic Delivery of siRNA Silencing HIF-1 Alpha with Micellar Nanoparticles Inhibits Hypoxic Tumor Growth. Mol. Pharm. 2012, 9, 2863–2874. [Google Scholar] [CrossRef]
- Omedes Pujol, M.; Coleman, D.J.L.; Allen, C.D.; Heidenreich, O.; Fulton, D.A. Determination of key structure–activity relationships in siRNA delivery with a mixed micelle system. J. Control. Release 2013, 172, 939–945. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shi, S.; Shi, K.; Tan, L.; Qu, Y.; Shen, G.; Chu, B.; Zhang, S.; Su, X.; Li, X.; Wei, Y.; et al. The use of cationic MPEG-PCL-g-PEI micelles for co-delivery of Msurvivin T34A gene and doxorubicin. Biomaterials 2014, 35, 4536–4547. [Google Scholar] [CrossRef]
- Yi, H.; Liu, L.; Sheng, N.; Li, P.; Pan, H.; Cai, L.; Ma, Y. Synergistic Therapy of Doxorubicin and miR-129-5p with Self-Cross-Linked Bioreducible Polypeptide Nanoparticles Reverses Multidrug Resistance in Cancer Cells. Biomacromolecules 2016, 17, 1737–1747. [Google Scholar] [CrossRef]
- Wang, X.; Liow, S.S.; Wu, Q.; Li, C.; Owh, C.; Li, Z.; Loh, X.J.; Wu, Y.-L. Codelivery for Paclitaxel and Bcl-2 Conversion Gene by PHB-PDMAEMA Amphiphilic Cationic Copolymer for Effective Drug Resistant Cancer Therapy. Macromol. Biosci. 2017, 17, 1700186. [Google Scholar] [CrossRef] [PubMed]
- Góis, J.R.; Reis, F.; Almeida, A.M.; Pereira, P.; Sousa, F.; Serra, A.C.; Coelho, J.F.J. Preparation of well-defined brush-like block copolymers for gene delivery applications under biorelevant reaction conditions. Colloids Surf. B Biointerfaces 2018, 169, 107–117. [Google Scholar] [CrossRef]
- Hossain, M.S.; Nakane, K. Development of a high-performance heat dissipation sheet with three-dimensional alumina fibrous structure fabricated by freeze-drying. Results Mater. 2022, 13, 100241. [Google Scholar] [CrossRef]
- Wu, J.; Wang, Q.; Dong, X.; Xu, M.; Yang, J.; Yi, X.; Chen, B.; Dong, X.; Wang, Y.; Lou, X.; et al. Biocompatible AIEgen/p-glycoprotein siRNA@reduction-sensitive paclitaxel polymeric prodrug nanoparticles for overcoming chemotherapy resistance in ovarian cancer. Theranostics 2021, 11, 3710–3724. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, M.; Patil, R.; Ren, Y.; Shyam, R.; Wong, P.; Mao, H.-Q. Enhanced Stability and Knockdown Efficiency of Poly(ethylene glycol)-b-polyphosphoramidate/siRNA Micellar Nanoparticles by Co-condensation with Sodium Triphosphate. Pharm. Res. 2011, 28, 1723–1732. [Google Scholar] [CrossRef] [PubMed]
- Al-Abd, A.M.; Lee, S.H.; Kim, S.H.; Cha, J.-H.; Park, T.G.; Lee, S.J.; Kuh, H.-J. Penetration and efficacy of VEGF siRNA using polyelectrolyte complex micelles in a human solid tumor model in-vitro. J. Control. Release 2009, 137, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Yu, H.; Sun, Y.; Zhu, M.; Duan, Y. A mPEG-PLGA-b-PLL copolymer carrier for adriamycin and siRNA delivery. Biomaterials 2012, 33, 4403–4412. [Google Scholar] [CrossRef] [PubMed]
- Raisin, S.; Morille, M.; Bony, C.; Noël, D.; Devoisselle, J.-M.; Belamie, E. Tripartite polyionic complex (PIC) micelles as non-viral vectors for mesenchymal stem cell siRNA transfection. Biomater. Sci. 2017, 5, 1910–1921. [Google Scholar] [CrossRef]
- Hossian, A.K.M.N.; Jois, S.D.; Jonnalagadda, S.C.; Mattheolabakis, G. Nucleic Acid Delivery with α-Tocopherol-Polyethyleneimine-Polyethylene Glycol Nanocarrier System. Int. J. Nanomed. 2020, 15, 6689–6703. [Google Scholar] [CrossRef]
- Lee, S.H.; Mok, H.; Lee, Y.; Park, T.G. Self-assembled siRNA–PLGA conjugate micelles for gene silencing. J. Control. Release 2011, 152, 152–158. [Google Scholar] [CrossRef]
- Wang, Y.; Zheng, X.; Liu, J.; Chen, Q.; Zhao, Y. Tumor-Targeted Anti-VEGF RNAi Capable of Sequentially Responding to Intracellular Microenvironments for Potent Systemic Tumor Suppression. ACS Appl. Bio Mater. 2020, 3, 9145–9155. [Google Scholar] [CrossRef]
- Benns, J.M.; Choi, J.-S.; Mahato, R.I.; Park, J.-S.; Kim, S.W. pH-Sensitive Cationic Polymer Gene Delivery Vehicle: N-Ac-poly(l-histidine)-graft-poly(l-lysine) Comb Shaped Polymer. Bioconjug. Chem. 2000, 11, 637–645. [Google Scholar] [CrossRef]
- Benoit, D.S.W.; Henry, S.M.; Shubin, A.D.; Hoffman, A.S.; Stayton, P.S. pH-Responsive Polymeric siRNA Carriers Sensitize Multidrug Resistant Ovarian Cancer Cells to Doxorubicin via Knockdown of Polo-like Kinase 1. Mol. Pharm. 2010, 7, 442–455. [Google Scholar] [CrossRef]
- Kim, Y.H.; Park, J.H.; Lee, M.; Kim, Y.-H.; Park, T.G.; Kim, S.W. Polyethylenimine with acid-labile linkages as a biodegradable gene carrier. J. Control. Release 2005, 103, 209–219. [Google Scholar] [CrossRef]
- Oishi, M.; Nagasaki, Y.; Itaka, K.; Nishiyama, N.; Kataoka, K. Lactosylated Poly(ethylene glycol)-siRNA Conjugate through Acid-Labile β-Thiopropionate Linkage to Construct pH-Sensitive Polyion Complex Micelles Achieving Enhanced Gene Silencing in Hepatoma Cells. J. Am. Chem. Soc. 2005, 127, 1624–1625. [Google Scholar] [CrossRef] [PubMed]
- Shim, M.S.; Kwon, Y.J. Acid-Responsive Linear Polyethylenimine for Efficient, Specific, and Biocompatible siRNA Delivery. Bioconjug. Chem. 2009, 20, 488–499. [Google Scholar] [CrossRef]
- Miyata, K.; Kakizawa, Y.; Nishiyama, N.; Harada, A.; Yamasaki, Y.; Koyama, H.; Kataoka, K. Block Catiomer Polyplexes with Regulated Densities of Charge and Disulfide Cross-Linking Directed To Enhance Gene Expression. J. Am. Chem. Soc. 2004, 126, 2355–2361. [Google Scholar] [CrossRef]
- Matsumoto, S.; Christie, R.J.; Nishiyama, N.; Miyata, K.; Ishii, A.; Oba, M.; Koyama, H.; Yamasaki, Y.; Kataoka, K. Environment-Responsive Block Copolymer Micelles with a Disulfide Cross-Linked Core for Enhanced siRNA Delivery. Biomacromolecules 2009, 10, 119–127. [Google Scholar] [CrossRef]
- Meyer, M.; Dohmen, C.; Philipp, A.; Kiener, D.; Maiwald, G.; Scheu, C.; Ogris, M.; Wagner, E. Synthesis and Biological Evaluation of a Bioresponsive and Endosomolytic siRNA−Polymer Conjugate. Mol. Pharm. 2009, 6, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Carlisle, R.C.; Etrych, T.; Briggs, S.S.; Preece, J.A.; Ulbrich, K.; Seymour, L.W. Polymer-coated polyethylenimine/DNA complexes designed for triggered activation by intracellular reduction. J. Gene Med. 2004, 6, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Ooya, T.; Choi, H.S.; Yamashita, A.; Yui, N.; Sugaya, Y.; Kano, A.; Maruyama, A.; Akita, H.; Ito, R.; Kogure, K.; et al. Biocleavable polyrotaxane-plasmid DNA polyplex for enhanced gene delivery. J. Am. Chem. Soc. 2006, 128, 3852–3853. [Google Scholar] [CrossRef]
- Zhou, Z.; Li, C.; Zhang, M.; Zhang, Q.; Qian, C.; Oupicky, D.; Sun, M. Charge and Assembly Reversible Micelles Fueled by Intracellular ATP for Improved siRNA Transfection. ACS Appl. Mater. Interfaces 2018, 10, 32026–32037. [Google Scholar] [CrossRef]
- Wang, H.-X.; Yang, X.-Z.; Sun, C.-Y.; Mao, C.-Q.; Zhu, Y.-H.; Wang, J. Matrix metalloproteinase 2-responsive micelle for siRNA delivery. Biomaterials 2014, 35, 7622–7634. [Google Scholar] [CrossRef]
- Zhu, L.; Perche, F.; Wang, T.; Torchilin, V.P. Matrix metalloproteinase 2-sensitive multifunctional polymeric micelles for tumor-specific co-delivery of siRNA and hydrophobic drugs. Biomaterials 2014, 35, 4213–4222. [Google Scholar] [CrossRef]
- Zintchenko, A.; Ogris, M.; Wagner, E. Temperature Dependent Gene Expression Induced by PNIPAM-Based Copolymers: Potential of Hyperthermia in Gene Transfer. Bioconjug. Chem. 2006, 17, 766–772. [Google Scholar] [CrossRef] [PubMed]
- Naito, M.; Yoshinaga, N.; Ishii, T.; Matsumoto, A.; Miyahara, Y.; Miyata, K.; Kataoka, K. Enhanced Intracellular Delivery of siRNA by Controlling ATP-Responsivity of Phenylboronic Acid-Functionalized Polyion Complex Micelles. Macromol. Biosci. 2018, 18, 1700357. [Google Scholar] [CrossRef]
- Yoshinaga, N.; Uchida, S.; Dirisala, A.; Naito, M.; Osada, K.; Cabral, H.; Kataoka, K. mRNA loading into ATP-responsive polyplex micelles with optimal density of phenylboronate ester crosslinking to balance robustness in the biological milieu and intracellular translational efficiency. J. Control. Release 2021, 330, 317–328. [Google Scholar] [CrossRef]
- Lara, A.R.; Ramírez, O.T. Plasmid DNA Production for Therapeutic Applications; Humana Press: Totowa, NJ, USA, 2012; pp. 271–303. [Google Scholar]
- Phillips, A.J. The challenge of gene therapy and DNA delivery. J. Pharm. Pharmacol. 2010, 53, 1169–1174. [Google Scholar] [CrossRef]
- Kabanov, A.V.; Astafyeva, I.V.; Chikindas, M.L.; Rosenblat, G.F.; Kiselev, V.I.; Severin, E.S.; Kabanov, V.A. DNA interpolyelectrolyte complexes as a tool for efficient cell transformation. Biopolymers 1991, 31, 1437–1443. [Google Scholar] [CrossRef] [PubMed]
- Kabanov, A.V.; Astafieva, I.V.; Maksimova, I.V.; Lukanidin, E.M.; Georgiev, G.P.; Kabanov, V.A. Efficient transformation of mammalian cells using DNA interpolyelectrolyte complexes with carbon chain polycations. Bioconjug. Chem. 1993, 4, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Abedi, K.; Shi, J. Polymeric nanoparticles for RNA delivery. In Encyclopedia of Nanomaterials; Elsevier: Amsterdam, The Netherlands, 2023; pp. 555–573. [Google Scholar]
- Bieber, T.; Elsässer, H.-P. Preparation of a Low Molecular Weight Polyethylenimine for Efficient Cell Transfection. Biotechniques 2001, 30, 74–81. [Google Scholar] [CrossRef]
- Tang, G.P.; Zeng, J.M.; Gao, S.J.; Ma, Y.X.; Shi, L.; Li, Y.; Too, H.-P.; Wang, S. Polyethylene glycol modified polyethylenimine for improved CNS gene transfer: Effects of PEGylation extent. Biomaterials 2003, 24, 2351–2362. [Google Scholar] [CrossRef]
- Velluto, D.; Thomas, S.N.; Simeoni, E.; Swartz, M.A.; Hubbell, J.A. PEG-b-PPS-b-PEI micelles and PEG-b-PPS/PEG-b-PPS-b-PEI mixed micelles as non-viral vectors for plasmid DNA: Tumor immunotoxicity in B16F10 melanoma. Biomaterials 2011, 32, 9839–9847. [Google Scholar] [CrossRef]
- Abd Elhameed, H.A.H.; Ungor, D.; Igaz, N.; Gopisetty, M.K.; Kiricsi, M.; Csapó, E.; Gyurcsik, B. High Molecular Weight Poly(ethylenimine)-Based Water-Soluble Lipopolymer for Transfection of Cancer Cells. Macromol. Biosci. 2020, 20, 2000040. [Google Scholar] [CrossRef] [PubMed]
- Xun, M.-M.; Huang, Z.; Xiao, Y.-P.; Liu, Y.-H.; Zhang, J.; Zhang, J.-H.; Yu, X.-Q. Synthesis and Properties of Low-Molecular-Weight PEI-Based Lipopolymers for Delivery of DNA. Polymers 2018, 10, 1060. [Google Scholar] [CrossRef] [PubMed]
- Kara, A.; Ozturk, N.; Esendagli, G.; Ozkose, U.U.; Gulyuz, S.; Yilmaz, O.; Telci, D.; Bozkir, A.; Vural, I. Development of novel self-assembled polymeric micelles from partially hydrolysed poly(2-ethyl-2-oxazoline)-co-PEI-b-PCL block copolymer as non-viral vectors for plasmid DNA in vitro transfection. Artif. Cells Nanomed. Biotechnol. 2018, 46, 264–273. [Google Scholar] [CrossRef]
- Afrouz, M.; Ahmadi-Nouraldinvand, F.; Amani, A.; Zahedian, H.; Elias, S.G.; Arabnejad, F.; Yaghoubi, H.; Farshad, O.; Farazi, N.; Jalali, A.; et al. Preparation and characterization of magnetic PEG-PEI-PLA-PEI-PEG/Fe3O4-PCL/DNA micelles for gene delivery into MCF-7 cells. J. Drug Deliv. Sci. Technol. 2023, 79, 104016. [Google Scholar] [CrossRef]
- Garg, C.; Priyam, A.; Kumar, P.; Sharma, A.K.; Gupta, A. In Vitro Assessment of Core-Shell Micellar Nanostructures of Amphiphilic Cationic Polymer-Peptide Conjugates as Efficient Gene and Drug Carriers. J. Pharm. Sci. 2020, 109, 2847–2853. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.H.; Park, T.G. Poly(l-lysine)-g-poly(d,l-lactic-co-glycolic acid) micelles for low cytotoxic biodegradable gene delivery carriers. J. Control. Release 2002, 82, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Ueno, M.; Yamauchi, S.; Kumekawa, D.; Yamasaki, Y. Peptide Sequence-Dependent Gene Expression of PEGylated Peptide/DNA Complexes. Mol. Pharm. 2019, 16, 3072–3082. [Google Scholar] [CrossRef]
- Takeda, K.M.; Yamasaki, Y.; Dirisala, A.; Ikeda, S.; Tockary, T.A.; Toh, K.; Osada, K.; Kataoka, K. Effect of shear stress on structure and function of polyplex micelles from poly(ethylene glycol)-poly(l-lysine) block copolymers as systemic gene delivery carrier. Biomaterials 2017, 126, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Abedi-Gaballu, F.; Dehghan, G.; Ghaffari, M.; Yekta, R.; Abbaspour-Ravasjani, S.; Baradaran, B.; Ezzati Nazhad Dolatabadi, J.; Hamblin, M.R. PAMAM dendrimers as efficient drug and gene delivery nanosystems for cancer therapy. Appl. Mater. Today 2018, 12, 177–190. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.-T.; Chen, G.; Nie, X.; Wang, L.-H.; Ding, S.-G.; You, Y.-Z. Low generation PAMAM-based nanomicelles as ROS-responsive gene vectors with enhanced transfection efficacy and reduced cytotoxicity in vitro. New J. Chem. 2017, 41, 3273–3279. [Google Scholar] [CrossRef]
- Piao, C.; Zhuang, C.; Choi, M.; Ha, J.; Lee, M. A RAGE-antagonist peptide potentiates polymeric micelle-mediated intracellular delivery of plasmid DNA for acute lung injury gene therapy. Nanoscale 2020, 12, 13606–13617. [Google Scholar] [CrossRef]
- Kim, G.; Piao, C.; Oh, J.; Lee, M. Combined delivery of curcumin and the heme oxygenase-1 gene using cholesterol-conjugated polyamidoamine for anti-inflammatory therapy in acute lung injury. Phytomedicine 2019, 56, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Yan, S.; Zhu, Q.; Chen, J.; Deng, L.; Zheng, Y.; Xue, W.; Guo, R. Targeted multifunctional redox-sensitive micelle co-delivery of DNA and doxorubicin for the treatment of breast cancer. J. Mater. Chem. B 2018, 6, 3372–3386. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Lian, K.; Meng, T.; Liu, X.; Miao, J.; Tan, Y.; Yuan, H.; Hu, F. Immune Adjuvant Targeting Micelles Allow Efficient Dendritic Cell Migration to Lymph Nodes for Enhanced Cellular Immunity. ACS Appl. Mater. Interfaces 2018, 10, 33532–33544. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Kong, N.; Zhang, X.; Cao, Y.; Langer, R.; Tao, W. The landscape of mRNA nanomedicine. Nat. Med. 2022, 28, 2273–2287. [Google Scholar] [CrossRef] [PubMed]
- Shuai, Q.; Zhu, F.; Zhao, M.; Yan, Y. mRNA delivery via non-viral carriers for biomedical applications. Int. J. Pharm. 2021, 607, 121020. [Google Scholar] [CrossRef]
- Yang, W.; Chen, P.; Boonstra, E.; Hong, T.; Cabral, H. Polymeric Micelles with pH-Responsive Cross-Linked Core Enhance In Vivo mRNA Delivery. Pharmaceutics 2022, 14, 1205. [Google Scholar] [CrossRef]
- Ren, J.; Cao, Y.; Li, L.; Wang, X.; Lu, H.; Yang, J.; Wang, S. Self-assembled polymeric micelle as a novel mRNA delivery carrier. J. Control. Release 2021, 338, 537–547. [Google Scholar] [CrossRef]
- Yang, X.; Chen, Q.; Yang, J.; Wu, S.; Liu, J.; Li, Z.; Liu, D.; Chen, X.; Qiu, Y. Tumor-Targeted Accumulation of Ligand-Installed Polymeric Micelles Influenced by Surface PEGylation Crowdedness. ACS Appl. Mater. Interfaces 2017, 9, 44045–44052. [Google Scholar] [CrossRef]
- Baba, M.; Itaka, K.; Kondo, K.; Yamasoba, T.; Kataoka, K. Treatment of neurological disorders by introducing mRNA in vivo using polyplex nanomicelles. J. Control. Release 2015, 201, 41–48. [Google Scholar] [CrossRef]
- Cheng, C.; Convertine, A.J.; Stayton, P.S.; Bryers, J.D. Multifunctional triblock copolymers for intracellular messenger RNA delivery. Biomaterials 2012, 33, 6868–6876. [Google Scholar] [CrossRef] [PubMed]
- Joubert, F.; Munson, M.J.; Sabirsh, A.; England, R.M.; Hemmerling, M.; Alexander, C.; Ashford, M.B. Precise and systematic end group chemistry modifications on PAMAM and poly(l-lysine) dendrimers to improve cytosolic delivery of mRNA. J. Control. Release 2023, 356, 580–594. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.Y.; Khung, Y.L.; Lin, C.-Y. Preparation of Messenger RNA Nanomicelles via Non-Cytotoxic PEG-Polyamine Nanocomplex for Intracerebroventicular Delivery: A Proof-of-Concept Study in Mouse Models. Nanomaterials 2019, 9, 67. [Google Scholar] [CrossRef]
- Crowley, S.T.; Fukushima, Y.; Uchida, S.; Kataoka, K.; Itaka, K. Enhancement of Motor Function Recovery after Spinal Cord Injury in Mice by Delivery of Brain-Derived Neurotrophic Factor mRNA. Mol. Ther.—Nucleic Acids 2019, 17, 465–476. [Google Scholar] [CrossRef]
- Zhao, M.; Li, M.; Zhang, Z.; Gong, T.; Sun, X. Induction of HIV-1 gag specific immune responses by cationic micelles mediated delivery of gag mRNA. Drug Deliv. 2016, 23, 2596–2607. [Google Scholar] [CrossRef]
- Yang, W.; Miyazaki, T.; Nakagawa, Y.; Boonstra, E.; Masuda, K.; Nakashima, Y.; Chen, P.; Mixich, L.; Barthelmes, K.; Matsumoto, A.; et al. Block catiomers with flanking hydrolyzable tyrosinate groups enhance in vivo mRNA delivery via π–π stacking-assisted micellar assembly. Sci. Technol. Adv. Mater. 2023, 24, 2170164. [Google Scholar] [CrossRef]
- Patel, A.K.; Kaczmarek, J.C.; Bose, S.; Kauffman, K.J.; Mir, F.; Heartlein, M.W.; DeRosa, F.; Langer, R.; Anderson, D.G. Inhaled Nanoformulated mRNA Polyplexes for Protein Production in Lung Epithelium. Adv. Mater. 2019, 31, 1805116. [Google Scholar] [CrossRef]
- Li, J.; Men, K.; Gao, Y.; Wu, J.; Lei, S.; Yang, Y.; Pan, H. Single Micelle Vectors based on Lipid/Block Copolymer Compositions as mRNA Formulations for Efficient Cancer Immunogene Therapy. Mol. Pharm. 2021, 18, 4029–4045. [Google Scholar] [CrossRef] [PubMed]
- Prieve, M.G.; Harvie, P.; Monahan, S.D.; Roy, D.; Li, A.G.; Blevins, T.L.; Paschal, A.E.; Waldheim, M.; Bell, E.C.; Galperin, A.; et al. Targeted mRNA Therapy for Ornithine Transcarbamylase Deficiency. Mol. Ther. 2018, 26, 801–813. [Google Scholar] [CrossRef] [PubMed]
- Kakizawa, Y.; Harada, A.; Kataoka, K. Glutathione-Sensitive Stabilization of Block Copolymer Micelles Composed of Antisense DNA and Thiolated Poly(ethylene glycol)-b lock-poly(l-lysine): A Potential Carrier for Systemic Delivery of Antisense DNA. Biomacromolecules 2001, 2, 491–497. [Google Scholar] [CrossRef]
- Kim, B.S.; Kim, H.J.; Osawa, S.; Hayashi, K.; Toh, K.; Naito, M.; Min, H.S.; Yi, Y.; Kwon, I.C.; Kataoka, K.; et al. Dually Stabilized Triblock Copolymer Micelles with Hydrophilic Shell and Hydrophobic Interlayer for Systemic Antisense Oligonucleotide Delivery to Solid Tumor. ACS Biomater. Sci. Eng. 2019, 5, 5770–5780. [Google Scholar] [CrossRef]
- Hanson, M.G.; Grimme, C.J.; Santa Chalarca, C.F.; Reineke, T.M. Cationic Micelles Outperform Linear Polymers for Delivery of Antisense Oligonucleotides in Serum: An Exploration of Polymer Architecture, Cationic Moieties, and Cell Addition Order. Bioconjug. Chem. 2022, 33, 2121–2131. [Google Scholar] [CrossRef] [PubMed]
- Min, H.S.; Kim, H.J.; Naito, M.; Ogura, S.; Toh, K.; Hayashi, K.; Kim, B.S.; Fukushima, S.; Anraku, Y.; Miyata, K.; et al. Systemic Brain Delivery of Antisense Oligonucleotides across the Blood–Brain Barrier with a Glucose-Coated Polymeric Nanocarrier. Angew. Chemie Int. Ed. 2020, 59, 8173–8180. [Google Scholar] [CrossRef] [PubMed]
- Fakhoury, J.J.; Edwardson, T.G.; Conway, J.W.; Trinh, T.; Khan, F.; Barłóg, M.; Bazzi, H.S.; Sleiman, H.F. Antisense precision polymer micelles require less poly(ethylenimine) for efficient gene knockdown. Nanoscale 2015, 7, 20625–20634. [Google Scholar] [CrossRef]
- Kim, B.S.; Osawa, S.; Naito, M.; Ogura, S.; Kamegawa, R.; Ishida, H.; Kim, H.J.; Uchida, S.; Miyata, K. A 50-nm-Sized Micellar Assembly of Thermoresponsive Polymer-Antisense Oligonucleotide Conjugates for Enhanced Gene Knockdown in Lung Cancer by Intratracheal Administration. Adv. Ther. 2020, 3, 1900123. [Google Scholar] [CrossRef]
- Lin, B.; Lu, L.; Wang, Y.; Zhang, Q.; Wang, Z.; Cheng, G.; Duan, X.; Zhang, F.; Xie, M.; Le, H.; et al. Nanomedicine Directs Neuronal Differentiation of Neural Stem Cells via Silencing Long Noncoding RNA for Stroke Therapy. Nano Lett. 2021, 21, 806–815. [Google Scholar] [CrossRef]
- Liao, L.-Y.; Lau, B.-M.; Sánchez-Vidaña, D.; Gao, Q. Exogenous neural stem cell transplantation for cerebral ischemia. Neural Regen. Res. 2019, 14, 1129. [Google Scholar] [CrossRef]
- Alshaer, W.; Zureigat, H.; Al Karaki, A.; Al-Kadash, A.; Gharaibeh, L.; Hatmal, M.M.; Aljabali, A.A.A.; Awidi, A. siRNA: Mechanism of action, challenges, and therapeutic approaches. Eur. J. Pharmacol. 2021, 905, 174178. [Google Scholar] [CrossRef]
- Kim, S.H.; Jeong, J.H.; Lee, S.H.; Kim, S.W.; Park, T.G. Local and systemic delivery of VEGF siRNA using polyelectrolyte complex micelles for effective treatment of cancer. J. Control. Release 2008, 129, 107–116. [Google Scholar] [CrossRef]
- Navarro, G.; Sawant, R.R.; Essex, S.; Tros de ILarduya, C.; Torchilin, V.P. Phospholipid–polyethylenimine conjugate-based micelle-like nanoparticles for siRNA delivery. Drug Deliv. Transl. Res. 2011, 1, 25–33. [Google Scholar] [CrossRef]
- Capelôa, L.; Yazdi, M.; Zhang, H.; Chen, X.; Nie, Y.; Wagner, E.; Lächelt, U.; Barz, M. Cross-Linkable Polyion Complex Micelles from Polypept(o)ide-Based ABC-Triblock Copolymers for siRNA Delivery. Macromol. Rapid Commun. 2022, 43, 2100698. [Google Scholar] [CrossRef]
- Elsabahy, M.; Wazen, N.; Bayó-Puxan, N.; Deleavey, G.; Servant, M.; Damha, M.J.; Leroux, J.-C. Delivery of Nucleic Acids through the Controlled Disassembly of Multifunctional Nanocomplexes. Adv. Funct. Mater. 2009, 19, 3862–3867. [Google Scholar] [CrossRef]
- Pan, J.; Mendes, L.P.; Yao, M.; Filipczak, N.; Garai, S.; Thakur, G.A.; Sarisozen, C.; Torchilin, V.P. Polyamidoamine dendrimers-based nanomedicine for combination therapy with siRNA and chemotherapeutics to overcome multidrug resistance. Eur. J. Pharm. Biopharm. 2019, 136, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Du, L.; Zhou, J.; Meng, L.; Wang, X.; Wang, C.; Huang, Y.; Zheng, S.; Deng, L.; Cao, H.; Liang, Z.; et al. The pH-Triggered Triblock Nanocarrier Enabled Highly Efficient siRNA Delivery for Cancer Therapy. Theranostics 2017, 7, 3432–3445. [Google Scholar] [CrossRef]
- Li, C.; Zhou, J.; Wu, Y.; Dong, Y.; Du, L.; Yang, T.; Wang, Y.; Guo, S.; Zhang, M.; Hussain, A.; et al. Core Role of Hydrophobic Core of Polymeric Nanomicelle in Endosomal Escape of siRNA. Nano Lett. 2021, 21, 3680–3689. [Google Scholar] [CrossRef] [PubMed]
- Ibaraki, H.; Hatakeyama, N.; Arima, N.; Takeda, A.; Seta, Y.; Kanazawa, T. Systemic delivery of siRNA to the colon using peptide modified PEG-PCL polymer micelles for the treatment of ulcerative colitis. Eur. J. Pharm. Biopharm. 2022, 170, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Feng, H.; Jin, L.; Zhang, Y.; Tian, X.; Li, J. Polymeric micelle with pH-induced variable size and doxorubicin and siRNA co-delivery for synergistic cancer therapy. Appl. Nanosci. 2020, 10, 1903–1913. [Google Scholar] [CrossRef]
- Muddineti, O.S.; Shah, A.; Rompicharla, S.V.K.; Ghosh, B.; Biswas, S. Cholesterol-grafted chitosan micelles as a nanocarrier system for drug-siRNA co-delivery to the lung cancer cells. Int. J. Biol. Macromol. 2018, 118, 857–863. [Google Scholar] [CrossRef]
- Ganesh, S.; Iyer, A.K.; Morrissey, D.V.; Amiji, M.M. Hyaluronic acid based self-assembling nanosystems for CD44 target mediated siRNA delivery to solid tumors. Biomaterials 2013, 34, 3489–3502. [Google Scholar] [CrossRef]
- Mousazadeh, H.; Pilehvar-Soltanahmadi, Y.; Dadashpour, M.; Zarghami, N. Cyclodextrin based natural nanostructured carbohydrate polymers as effective non-viral siRNA delivery systems for cancer gene therapy. J. Control. Release 2021, 330, 1046–1070. [Google Scholar] [CrossRef]
- Sinani, G.; Sessevmez, M.; Gök, M.K.; Özgümüş, S.; Alpar, H.O.; Cevher, E. Modified chitosan-based nanoadjuvants enhance immunogenicity of protein antigens after mucosal vaccination. Int. J. Pharm. 2019, 569, 118592. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Zhang, Y.; Li, F.; Bei, S.; Pan, M.; Feng, L. Precise engineering of cholesterol-loaded chitosan micelles as a promising nanocarrier system for co-delivery drug-siRNA for the treatment of gastric cancer therapy. Process Biochem. 2022, 120, 265–274. [Google Scholar] [CrossRef]
- Song, P.; Wang, B.; Pan, Q.; Jiang, T.; Chen, X.; Zhang, M.; Tao, J.; Zhao, X. GE11-modified carboxymethyl chitosan micelles to deliver DOX·PD-L1 siRNA complex for combination of ICD and immune escape inhibition against tumor. Carbohydr. Polym. 2023, 312, 120837. [Google Scholar] [CrossRef] [PubMed]

| Polymer/Modifying Agent | Characteristic | Nucleic Acid | Disease Category | References |
|---|---|---|---|---|
| Aliphatic chain | Hydrophobic | siRNA | Oncology | [130] |
| Amines | Cationic | siRNA | Oncology | [130] |
| APA | Amphiphilic | siRNA | Oncology | [130] |
| APD | Cationic | pDNA | Oncology | [131] |
| Cholic acid | Hydrophobic | pDNA | Oncology | [131] |
| CCP | Anionic | siRNA | Oncology | [132] |
| CPP | Cationic | miRNA | Oncology | [133] |
| siRNA | Oncology | [134,135] | ||
| Cys-bridged His-Arg | Cationic | siRNA | Oncology | [136] |
| DOTAP | Cationic | siRNA | Oncology | [137] |
| pDNA | Oncology | [138] | ||
| DP | Cationic | siRNA | Oncology | [139] |
| EMA | Cationic | siRNA | Oncology | [140] |
| MAODCA | Hydrophobic | pDNA | Oncology | [141] |
| NVP | Cationic | mRNA | - | [142] |
| PAGA | Cationic | siRNA | Oncology | [143] |
| pAsp | Cationic/Hydrophobic | mRNA | Neurology | [95] |
| siRNA | Viral | [144] | ||
| siRNA | Oncology | [134,135,145] | ||
| - | Orthopedia | [146] | ||
| PCC | Cationic | miRNA | Oncology | [147] |
| PCL | Hydrophobic | siRNA | Oncology | [137,139,148,149,150,151,152,153,154,155] |
| pDNA | Oncology | [138,156] | ||
| pCys | Hydrophobic | miRNA | Oncology | [157] |
| PDMAEMA | Cationic | siRNA | Oncology | [148,149,155,158] |
| pDNA | - | [141,159] | ||
| PDPA | Cationic/Hydrophobic | siRNA | Oncology | [143] |
| pDNA | Oncology | [159] | ||
| PE | Hydrophobic | siRNA | Oncology | [43] |
| PEG/mPEG/PEO | Hydrophilic | pDNA | Oncology | [138,156,160] |
| siRNA | Oncology | [43,134,135,136,137,140,143,145,150,151,152,153,154,155,161,162,163,164,165] | ||
| miRNA | Oncology | [133,147,157] | ||
| mRNA | Neurology | [95] | ||
| - | Orthopedia | [146] | ||
| PEI | Cationic | pDNA | Neurology | [147] |
| pDNA | Oncology | [156,166] | ||
| siRNA | Oncology | [150,163,167] | ||
| PGA | Hydrophobic | siRNA | Oncology | [140] |
| PHB | Amphiphilic | siRNA | Oncology | [158] |
| PHis | Hydrophobic | |||
| PLA | Hydrophobic | mRNA | - | [142] |
| miRNA | Oncology | [133] | ||
| PLGA | Hydrophobic | pDNA | Neurology | [147] |
| siRNA | Oncology | [164,167] | ||
| PLL | Cationic/Hydrophobic | siRNA | Oncology | [152,164] |
| miRNA | Oncology | [157] | ||
| siRNA | Oncology | [145,168] | ||
| PMPMC | Hydrophobic | siRNA | Oncology | [161] |
| P(NAS-co-NVP) | Amphiphilic | mRNA | - | [142] |
| POEOMA | Hydrophobic | pDNA | Oncology | [159] |
| Polystyrene | Hydrophobic | siRNA | Oncology | [136] |
| PPA | Cationic | siRNA | Oncology | [162] |
| PPEEA | Cationic | siRNA | Oncology | [153,154] |
| PSMA | Amphiphilic | siRNA | Oncology | [136] |
| RGD | Amphiphilic | siRNA | Oncology | [168] |
| SP | Cationic | siRNA | Oncology | [139] |
| TAT | Cationic | siRNA | Oncology | [151] |
| TEPA | Hydrophobic | miRNA | Oncology | [147] |
| TP | Cationic | siRNA | Oncology | [139] |
| TPP | Hydrophobic | pDNA | Oncology | [166] |
| Stimuli-Responsiveness | Functional Vector | Nucleic Acid | References |
|---|---|---|---|
| pH-responsive | PLL-polyhistidine | siRNA | [169] |
| Poly(styrene-alt-maleic anhydride) | DNA | [170] | |
| Cross-linked low Mw PEI by imine linkers | DNA | [171] | |
| Lactosylated PEG–PLL | siRNA | [172] | |
| Ketalized PEI | DNA/siRNA | [173] | |
| ROS-responsive | PEG–thiolated PLL | DNA | [174] |
| PEG–thiolated PLL | siRNA | [175] | |
| PEG–thiolated PLL–melittin–siRNA | siRNA | [176] | |
| PEI–PHPMA | DNA | [177] | |
| Cyclodextrins threaded onto PEG | DNA | [178] | |
| Enzyme-responsive | PEI-FPBA/Chol-DOPA | siRNA | [179] |
| PEG-PLG∗LAGr9–PCL | siRNA | [180] | |
| PEG-pp-PEI-PE | siRNA | [181] | |
| Temperature-responsive | PEI–poly(NIPAM–acrylamide)/PEI–poly(NIPAMvinylpyrrolidone) | DNA | [182] |
| ATP-responsive | FPBA-functionalized/PEG-PLL | siRNA | [183] |
| PEG-PBA | mRNA | [184] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sinani, G.; Durgun, M.E.; Cevher, E.; Özsoy, Y. Polymeric-Micelle-Based Delivery Systems for Nucleic Acids. Pharmaceutics 2023, 15, 2021. https://doi.org/10.3390/pharmaceutics15082021
Sinani G, Durgun ME, Cevher E, Özsoy Y. Polymeric-Micelle-Based Delivery Systems for Nucleic Acids. Pharmaceutics. 2023; 15(8):2021. https://doi.org/10.3390/pharmaceutics15082021
Chicago/Turabian StyleSinani, Genada, Meltem Ezgi Durgun, Erdal Cevher, and Yıldız Özsoy. 2023. "Polymeric-Micelle-Based Delivery Systems for Nucleic Acids" Pharmaceutics 15, no. 8: 2021. https://doi.org/10.3390/pharmaceutics15082021
APA StyleSinani, G., Durgun, M. E., Cevher, E., & Özsoy, Y. (2023). Polymeric-Micelle-Based Delivery Systems for Nucleic Acids. Pharmaceutics, 15(8), 2021. https://doi.org/10.3390/pharmaceutics15082021








