Anti-Obesity Drug Delivery Systems: Recent Progress and Challenges
Abstract
1. Introduction
- Maintaining constant drug levels within the therapeutic range.
- When drugs are targeted to specific tissues/organs, they have less toxicity and fewer side effects.
- Administration is made easier, which increases patient compliance.
- Defence against the degradation of biologically active drug particles such as proteins and peptides.
- Small doses of the drug and a reduction in the number of dosages.
2. Conventional Anti-Obesity Drugs
| Action Principle | Delivery Method | Name of Drug | Drawbacks | Reference |
|---|---|---|---|---|
| Reduce appetite | Oral administration | Phentermine/Topiramate ER | Taste disorders, insomnia, dizziness and constipation | [43] |
| Naltrexone SR/Bupropion SR | Headache, diarrhoea and constipation | [43] | ||
| Lorcaserin | Nausea, dizziness and constipation | [44] | ||
| Rimonabant | Discomfort, nausea and gastrointestinal distress | [43] | ||
| Fenfluramine | Hypertension and heart valve damage | [43] | ||
| Hypodermic injection | Liraglutide | Neuropsychiatric diseases, depression and dizziness | [38,39] | |
| Block the absorption of fat | Oral administration | Orlistat | Flatulence and diarrhoea | [42] |
| Increase energy consumption and reduce appetite | Sibutramine | Cerebrovascular diseases and cardiovascular | [43] |
3. Advanced Treatments of Obesity
| Action Principle | Delivery Mode | Name of Drug | References |
|---|---|---|---|
| Activation of brown adipocytes | Transdermal and hypodermic injection | β3-adrenoceptor agonist (CL316243) | [67,75] |
| thyroid hormone (T3) | [76,77] | ||
| Transdermal and oral administration | ROSI | [73,78] | |
| curcumin | [79,80] | ||
| Oral administration | fucoxanthin | [81] | |
| bile acid | [82] | ||
| capsaicin | [83] | ||
| olive oil | [84] | ||
| Hypodermic injection | GLP1 analogue | [65] | |
| Oral administration | resveratrol | [48] | |
| Fat decomposition | Transdermal and oral administration | gelatine | [62] |
| caffeine | [64,85] | ||
| Transdermal administration | gold NPs | [63,86] |
4. Natural Anti-Obesity Extracts
| Principle of Action | Natural Agent | Active Constituent | Reference |
|---|---|---|---|
| Pancreatic lipase inhibitor | Panax japonicus | Chikusetsusaponins | [109] |
| Thea sinensis (oolong tea) | Crude aqueous extract (caffeine) | [110] | |
| Cassia mimosoides | Proanthocyanidin | [111] | |
| Trigonella foenum graecum L. (seed) | Crude ethanolic extract | [112] | |
| Salix matsudana (leaf) | Polyphenol | [113] | |
| Vitis vinifera | Crude ethanolic extract | [114] | |
| Salvia officinalis L. (leaf) | Methanolic extract (carnosic acid) | [115] | |
| Cassia nomame | Flavan dimers | [116] | |
| Citrus unshiu | Hesperidin | [117] | |
| Chitosan-chitin | Chitosan (80%), chitin (20%) | [118] | |
| Streptomyces toxytricini (fungus) | Lipistatin | [119] | |
| Actinomycetes sp. | Valilactone | [120] | |
| Caulerpa taxifolia (marine algae) | Caulerpenyne | [121] | |
| Appetite suppressant | Panax ginseng (root) | Crude saponins | [122] |
| Camellia sinensis (leaf) | (-)-Epigallocatechin gallate (EGCG) | [123] | |
| Hoodia gordonii and H. pilifera | Steroidal glycoside | [124] | |
| Haseolus vulgaris and Robiniapseudoacacia | Lectins | [125] | |
| Pinus koraiensis (pine nut) | Pine nut fatty acids | [126] | |
| Ephedra species | Ephedrine | [127] | |
| Citrus aurantium | Synephrine | [128] | |
| Hypericum perforatum | Total extract | [129] | |
| Adipocyte differentiation inhibitor | Chili pepper (capsicum) | Capsaicin | [130] |
| Fish oil | Docosahexaenoic acid | [131] | |
| Palm oil | Ɣ-tocotrienol | [132] | |
| Camellia sinensis (green tea) | (-)-Epigallocatechin gallate | [133] | |
| Panax ginseng | Ginsenosides | [134] | |
| Silybum marianum | Silibinin | [135] | |
| Garlic | Ajoene | [136] | |
| Rosmarinus officinalis | Carnosic acid | [137] | |
| Curcuma longa | Curcumin | [138] | |
| Humulus lupulus | Xanthohumol | [139] | |
| Lipid metabolism regulator | Morus albam, Melissa officinalis, Artemisia capillaries | Crude aqueous extract | [140] |
| Curcuma longa L. | Curcumin and curcuminoids | [141] | |
| Glycyrrhiza glabra L. | Liquorice flavonoid | [142] | |
| Panax ginseng | Crude aqueous extract | [143] | |
| Zea mays L. | Purple corn colour (anthocyanins) | [144] | |
| Soybean | Genistein and L-carnitine (soy isoflavone) | [145] | |
| Energy expenditure stimulant | Solanum tuberosum | ethanolic extract | [146] |
| Lipid metabolism regulator and pancreatic lipase inhibitor | Coffea canephora | Caffeine and chlorogenic, neochlorogenic, and feruloyquinic acids | [147,148] |
| Appetite suppressant and adipocyte differentiation inhibitor | Garcinia cambogia | (-)-Hydroxycitric acid (HCA) | [149,150] |
5. Advanced DDSs for the Treatment of Obesity
5.1. Preparation and Characterization of Anti-Obesity DDSs
5.1.1. Polymer Conjugates
5.1.2. Hydrogels
Hydrogel Synthesis Methods
| Characterization Technique | Abbreviation | Liposome Characteristics | References |
|---|---|---|---|
| Laser scanning confocal microscopy | LSCM | Pore dimensions and shape | [212] |
| Scanning electron microscopy | SEM | Morphological characterization, pore formation and pore size, and crosslinking status | [213] |
| Infrared spectroscopic analysis | FTIR | Chemical composition | [214] |
| XRD | Phase behaviour | [214] | |
| Differential scanning calorimetry | DSC | Thermal characteristics of hydrogels | [215] |
| Thermogravimetric analysis | TGA | Thermal stability | [215] |
| Atomic force microscopy | AFM | Topology and roughness | [216] |
| Swelling behaviour | To determine the swell-ability of these polymeric networks, the hydrogels are immersed in aqueous media or medium with a particular pH. These polymers exhibit swelling-related increases in dimensions | [217] |
5.1.3. Microneedles (MNs)
5.1.4. Micro- and Nanoparticles
5.1.5. Liposomes
5.2. Drug Loading and In Vitro Drug Release Profile from Drug Delivery
5.2.1. Polymer Conjugate
5.2.2. Hydrogel
5.2.3. MNs
5.2.4. NPs
| Delivery Method of NPs | Materials | Disease | Reference |
|---|---|---|---|
| Injection | PLGA | Obesity | [313] |
| Egg yolk phosphatidylcholine (EPC), cholesterol, and peptide-conjugated PEG-lipid | [287] | ||
| PLGA and PEG | [311] | ||
| Egg yolk phosphatidylcholine, PEG, and peptide | [285] | ||
| MSN and PCL | [316] | ||
| PLGA and PVA | Obesity and inflammation | [308] | |
| LITA | Obesity and liver lipid accumulation | [317] | |
| YSK05, cholesterol and mPEG-DMG | Type 2 diabetes | [318] | |
| Oligopeptide (ATS-9R) | [319] | ||
| Zinc oxide | [320] | ||
| Egg yolk phosphatidylcholine and cholesterol | [286] | ||
| Dextran | Type 2 diabetes and heart disease | [180] | |
| PLGA | Heart disease | [321] | |
| CHC | Diabetes | [322] | |
| Oral | GLP-1 | Type 2 diabetes | [323] |
| Chitosan, gamma-PGA | Diabetes | [324] |
5.2.5. Liposomes
5.3. Clinical Study Involving DDSs
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Abbreviations | Proper Name |
| DDS | Drug delivery system |
| WHO | World Health Organization |
| BMI | Body mass index |
| CNS | Central nervous system |
| MNs | Microneedles |
| NPs | Nanoparticles |
| FDA | US Food and Drug Administration |
| AT | Adipose tissue |
| WAT | White adipose tissue |
| BAT | Brown adipose tissue |
| UCP1 | Uncoupling protein 1 |
| ROSI | Rosiglitazone |
| GLP1 | Glucagon-like peptide 1 |
| PPAR | Peroxisome proliferator-activated receptor |
| EGCG | (-)-Epigallocatechin-3-gallate |
| GTE | Green tea extract |
| VAT | Visceral adipose tissue |
| PEG | Poly (ethylene glycol) |
| RAFT | Reversible addition–fragmentation transfer polymerization |
| ROP | Ring-opening polymerization |
| ROMP | Ring-opening metathesis polymerization |
| BBB | Blood–brain barrier |
| PK | Pharmacokinetics |
| PLGA | Poly(lactic-co-glycolic acid) |
| HFD | High-fat diet |
| LDL | Low-density lipoprotein |
| HDL | High-density lipoprotein |
| PYP | Polypyrrole |
| HA | Hyaluronic acid |
| DIO | Diet-induced obese |
| epiWAT | Epididymal white adipose tissue |
| igWAT | Inguinal white adipose tissue |
| DMNs | Dissolving microneedles |
| PCL | Polycaprolactone |
| MSH | Melanocyte-stimulating hormone |
| DBZ | Dibenzoazepine |
| AuNPs | Gold nanoparticles |
| NIR | Near-infrared |
| PA imaging | Photoacoustic imaging |
| RPE | Reverse-phase evaporation |
| TFH | Thin-film hydration |
| DLS | Dynamic light scattering |
| SEM | Scanning electron microscopy |
| TEM | Transmission electron microscopy |
| AFM | Atomic force microscopy |
| XRD | X-ray diffraction |
| DSC | Differential scanning calorimetry |
| TGA | Thermogravimetric analysis |
| SIF | Simulated intestinal fluid |
| PBS | Phosphate-buffered saline |
| MNA | Microneedle arrays |
| PVA | Polyvinyl alcohol |
| EPC | Egg yolk phosphatidylcholine |
| LITA | Liposome-encapsulated acetate |
| CHC | Carboxymethyl-hexanoyl chitosan |
References
- Haslam, D.W.; James, W.P.T. Obesity. Lancet 2005, 366, 1197–1209. [Google Scholar] [CrossRef]
- Lau, D.C.; Douketis, J.D.; Morrison, K.M.; Hramiak, I.M.; Sharma, A.M.; Ur, E.; Obesity Canada Clinical Practice Guidelines Expert, P. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 2007, 176, S1–S13. [Google Scholar] [CrossRef]
- WHO. The World Health Report 2000: Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- WHO. Obesity and Overweight. 9 June 2021. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 September 2021).
- Masuzaki, H.; Paterson, J.; Shinyama, H.; Morton, N.M.; Mullins, J.J.; Seckl, J.R.; Flier, J.S. A transgenic model of visceral obesity and the metabolic syndrome. Science 2001, 294, 2166–2170. [Google Scholar] [CrossRef] [PubMed]
- Kopelman, P.G. Obesity as a medical problem. Nature 2000, 404, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Spiegelman, B.M.; Flier, J.S. Obesity and the regulation of energy balance. Cell 2001, 104, 531–543. [Google Scholar] [CrossRef] [PubMed]
- Fontaine, K.R.; Redden, D.T.; Wang, C.; Westfall, A.O.; Allison, D.B. Years of life lost due to obesity. JAMA 2003, 289, 187–193. [Google Scholar] [CrossRef]
- Quek, Y.H.; Tam, W.W.; Zhang, M.W.; Ho, R.C. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef]
- Newcombe, E.A.; Camats-Perna, J.; Silva, M.L.; Valmas, N.; Huat, T.J.; Medeiros, R. Inflammation: The link between comorbidities, genetics, and Alzheimer’s disease. J. Neuroinflammation 2018, 15, 1–26. [Google Scholar] [CrossRef]
- O‘Brien, P.D.; Hinder, L.M.; Callaghan, B.C.; Feldman, E.L. Neurological consequences of obesity. Lancet Neurol. 2017, 16, 465–477. [Google Scholar] [CrossRef]
- Saint-Maurice, P.F.; Troiano, R.P.; Bassett, D.R.; Graubard, B.I.; Carlson, S.A.; Shiroma, E.J.; Fulton, J.E.; Matthews, C.E. Association of daily step count and step intensity with mortality among US adults. JAMA 2020, 323, 1151–1160. [Google Scholar] [CrossRef]
- Sanchis-Gomar, F.; Lavie, C.J.; Mehra, M.R.; Henry, B.M.; Lippi, G. Obesity and outcomes in COVID-19: When an epidemic and pandemic collide. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2020; pp. 1445–1453. [Google Scholar]
- Fuster, J.J.; Ouchi, N.; Gokce, N.; Walsh, K. Obesity-induced changes in adipose tissue microenvironment and their impact on cardiovascular disease. Circ. Res. 2016, 118, 1786–1807. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef] [PubMed]
- Iliev, I.D.; Funari, V.A.; Taylor, K.D.; Nguyen, Q.; Reyes, C.N.; Strom, S.P.; Brown, J.; Becker, C.A.; Fleshner, P.R.; Dubinsky, M. Interactions between commensal fungi and the C-type lectin receptor Dectin-1 influence colitis. Science 2012, 336, 1314–1317. [Google Scholar] [CrossRef] [PubMed]
- Okamura, T.; Hashimoto, Y.; Hamaguchi, M.; Obora, A.; Kojima, T.; Fukui, M. Ectopic fat obesity presents the greatest risk for incident type 2 diabetes: A population-based longitudinal study. Int. J. Obes. 2019, 43, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.A.; Heisel, W.E.; Afshin, A.; Jensen, M.D.; Dietz, W.H.; Long, M.; Kushner, R.F.; Daniels, S.R.; Wadden, T.A.; Tsai, A.G. The science of obesity management: An endocrine society scientific statement. Endocr. Rev. 2018, 39, 79–132. [Google Scholar] [CrossRef]
- Shamloul, R.; Ghanem, H. Erectile dysfunction. Lancet 2013, 381, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, B.K.; Knutsen, S.F.; Oda, K.; Fraser, G.E. Obesity at age 20 and the risk of miscarriages, irregular periods and reported problems of becoming pregnant: The Adventist Health Study-2. Eur. J. Epidemiol. 2012, 27, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Steele, C.B.; Thomas, C.C.; Henley, S.J.; Massetti, G.M.; Galuska, D.A.; Agurs-Collins, T.; Puckett, M.; Richardson, L.C. Vital signs: Trends in incidence of cancers associated with overweight and obesity—United States, 2005–2014. Morb. Mortal. Wkly. Rep. 2017, 66, 1052. [Google Scholar] [CrossRef]
- Avgerinos, K.I.; Spyrou, N.; Mantzoros, C.S.; Dalamaga, M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism 2019, 92, 121–135. [Google Scholar] [CrossRef]
- Quail, D.F.; Dannenberg, A.J. The obese adipose tissue microenvironment in cancer development and progression. Nat. Rev. Endocrinol. 2019, 15, 139–154. [Google Scholar] [CrossRef]
- Ogrodnik, M.; Zhu, Y.; Langhi, L.G.; Tchkonia, T.; Krüger, P.; Fielder, E.; Victorelli, S.; Ruswhandi, R.A.; Giorgadze, N.; Pirtskhalava, T. Obesity-induced cellular senescence drives anxiety and impairs neurogenesis. Cell Metab. 2019, 29, 1061–1077. e1068. [Google Scholar] [CrossRef] [PubMed]
- Behl, T.; Kaur, I.; Sehgal, A.; Singh, S.; Zengin, G.; Negrut, N.; Nistor-Cseppento, D.C.; Pavel, F.M.; Corb Aron, R.A.; Bungau, S. Exploring the genetic conception of obesity via the dual role of FoxO. Int. J. Mol. Sci. 2021, 22, 3179. [Google Scholar] [CrossRef] [PubMed]
- Shick, S.M.; Wing, R.R.; Klem, M.L.; McGuire, M.T.; Hill, J.O.; Seagle, H. Persons successful at long-term weight loss and maintenance continue to consume a low-energy, low-fat diet. J. Am. Diet. Assoc. 1998, 98, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Tate, D.F.; Jeffery, R.W.; Sherwood, N.E.; Wing, R.R. Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? Am. J. Clin. Nutr. 2007, 85, 954–959. [Google Scholar] [CrossRef]
- Strychar, I. Diet in the management of weight loss. CMAJ 2006, 174, 56–63. [Google Scholar] [CrossRef]
- Wing, R.; Phelan, S. Long-term weight loss maintenance. Am. J. Clin. Nutr. 2005, 82, 222S–225S. [Google Scholar] [CrossRef]
- Jacob, J.J.; Isaac, R. Behavioral therapy for management of obesity. Indian J. Endocrinol. Metab. 2012, 16, 28. [Google Scholar] [CrossRef]
- Haskell, W.L.; Lee, I.-M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081. [Google Scholar] [CrossRef]
- Cooke, D.; Bloom, S. The obesity pipeline: Current strategies in the development of anti-obesity drugs. Nat. Rev. Drug Discov. 2006, 5, 919–931. [Google Scholar] [CrossRef]
- Sargent, B.J.; Moore, N.A. New central targets for the treatment of obesity. Br. J. Clin. Pharmacol. 2009, 68, 852–860. [Google Scholar] [CrossRef]
- Padwal, R.S.; Majumdar, S.R. Drug treatments for obesity: Orlistat, sibutramine, and rimonabant. Lancet 2007, 369, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Kokkoli, E. Characterizing particulate drug-delivery carriers with atomic force microscopy. IEEE Eng. Med. Biol. Mag. 2005, 24, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Muller, R.H.; Keck, C.M. Challenges and solutions for the delivery of biotech drugs–a review of drug nanocrystal technology and lipid nanoparticles. J. Biotechnol. 2004, 113, 151–170. [Google Scholar] [CrossRef] [PubMed]
- Langer, R. Drug delivery and targeting. Nature 1998, 392, 5–10. [Google Scholar]
- Srivastava, G.; Apovian, C.M. Current pharmacotherapy for obesity. Nat. Rev. Endocrinol. 2018, 14, 12–24. [Google Scholar] [CrossRef]
- Pilitsi, E.; Farr, O.M.; Polyzos, S.A.; Perakakis, N.; Nolen-Doerr, E.; Papathanasiou, A.-E.; Mantzoros, C.S. Pharmacotherapy of obesity: Available medications and drugs under investigation. Metabolism 2019, 92, 170–192. [Google Scholar] [CrossRef]
- Singh, A.K.; Singh, R. Pharmacotherapy in obesity: A systematic review and meta-analysis of randomized controlled trials of anti-obesity drugs. Expert Rev. Clin. Pharmacol. 2020, 13, 53–64. [Google Scholar] [CrossRef]
- Hankey, C. Session 3 (Joint with the British Dietetic Association): Management of obesity Weight-loss interventions in the treatment of obesity: Symposium on ‘Dietary management of disease’. Proc. Nutr. Soc. 2010, 69, 34–38. [Google Scholar] [CrossRef]
- Bray, G.A.; Frühbeck, G.; Ryan, D.H.; Wilding, J.P. Management of obesity. Lancet 2016, 387, 1947–1956. [Google Scholar] [CrossRef]
- Li, Z.; Fang, X.; Yu, D. Transdermal Drug Delivery Systems and Their Use in Obesity Treatment. Int. J. Mol. Sci. 2021, 22, 12754. [Google Scholar] [CrossRef]
- Tak, Y.J.; Lee, S.Y. Long-term efficacy and safety of anti-obesity treatment: Where do we stand? Curr. Obes. Rep. 2021, 10, 14–30. [Google Scholar] [CrossRef]
- McCreight, L.J.; Bailey, C.J.; Pearson, E.R. Metformin and the gastrointestinal tract. Diabetologia 2016, 59, 426–435. [Google Scholar] [CrossRef]
- Wysham, C.; Blevins, T.; Arakaki, R.; Colon, G.; Garcia, P.; Atisso, C.; Kuhstoss, D.; Lakshmanan, M. Efficacy and safety of dulaglutide added onto pioglitazone and metformin versus exenatide in type 2 diabetes in a randomized controlled trial (AWARD-1). Diabetes Care 2014, 37, 2159–2167. [Google Scholar] [CrossRef]
- Davies, M.J.; Bergenstal, R.; Bode, B.; Kushner, R.F.; Lewin, A.; Skjøth, T.V.; Andreasen, A.H.; Jensen, C.B.; DeFronzo, R.A.; Group, N.-S. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: The SCALE diabetes randomized clinical trial. JAMA 2015, 314, 687–699. [Google Scholar] [CrossRef] [PubMed]
- Zou, T.; Chen, D.; Yang, Q.; Wang, B.; Zhu, M.J.; Nathanielsz, P.W.; Du, M. Resveratrol supplementation of high-fat diet-fed pregnant mice promotes brown and beige adipocyte development and prevents obesity in male offspring. J. Physiol. 2017, 595, 1547–1562. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Castillo, A.; Fuentes-Romero, R.; Rodriguez-Lopez, L.A.; Torres, N.; Tovar, A.R. Understanding the biology of thermogenic fat: Is browning a new approach to the treatment of obesity? Arch. Med. Res. 2017, 48, 401–413. [Google Scholar] [CrossRef] [PubMed]
- Betz, M.J.; Enerbäck, S. Targeting thermogenesis in brown fat and muscle to treat obesity and metabolic disease. Nat. Rev. Endocrinol. 2018, 14, 77–87. [Google Scholar] [CrossRef]
- Concha, F.; Prado, G.; Quezada, J.; Ramirez, A.; Bravo, N.; Flores, C.; Herrera, J.; Lopez, N.; Uribe, D.; Duarte-Silva, L. Nutritional and non-nutritional agents that stimulate white adipose tissue browning. Rev. Endocr. Metab. Disord. 2019, 20, 161–171. [Google Scholar] [CrossRef]
- Peng, M.; Ping, H.; Chun-Yang, X.; Bi-Yu, H.; Qiang, G.-F.; Guan-Hua, D. Recent developments in natural products for white adipose tissue browning. Chin. J. Nat. Med. 2020, 18, 803–817. [Google Scholar]
- Stanford, K.I.; Middelbeek, R.J.; Townsend, K.L.; An, D.; Nygaard, E.B.; Hitchcox, K.M.; Markan, K.R.; Nakano, K.; Hirshman, M.F.; Tseng, Y.-H. Brown adipose tissue regulates glucose homeostasis and insulin sensitivity. J. Clin. Investig. 2012, 123, 215–223. [Google Scholar] [CrossRef]
- Di Maio, G.; Alessio, N.; Demirsoy, I.H.; Peluso, G.; Perrotta, S.; Monda, M.; Di Bernardo, G. Evaluation of browning agents on the white adipogenesis of bone marrow mesenchymal stromal cells: A contribution to fighting obesity. Cells 2021, 10, 403. [Google Scholar] [CrossRef]
- Longo, M.; Zatterale, F.; Naderi, J.; Parrillo, L.; Formisano, P.; Raciti, G.A.; Beguinot, F.; Miele, C. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int. J. Mol. Sci. 2019, 20, 2358. [Google Scholar] [CrossRef]
- Giralt, M.; Villarroya, F. White, brown, beige/brite: Different adipose cells for different functions? Endocrinology 2013, 154, 2992–3000. [Google Scholar] [CrossRef] [PubMed]
- Bartelt, A.; Heeren, J. Adipose tissue browning and metabolic health. Nat. Rev. Endocrinol. 2014, 10, 24–36. [Google Scholar] [CrossRef]
- Giordano, A.; Frontini, A.; Cinti, S. Convertible visceral fat as a therapeutic target to curb obesity. Nat. Rev. Drug Discov. 2016, 15, 405–424. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Yuan, J.-P.; Wu, C.-F.; Wang, J.-H. Fucoxanthin, a marine carotenoid present in brown seaweeds and diatoms: Metabolism and bioactivities relevant to human health. Mar. Drugs 2011, 9, 1806–1828. [Google Scholar] [CrossRef] [PubMed]
- Hiradate, R.; Khalil, I.A.; Matsuda, A.; Sasaki, M.; Hida, K.; Harashima, H. A novel dual-targeted rosiglitazone-loaded nanoparticle for the prevention of diet-induced obesity via the browning of white adipose tissue. J. Control. Release 2021, 329, 665–675. [Google Scholar] [CrossRef]
- Nishikawa, S.; Kamiya, M.; Aoyama, H.; Nomura, M.; Hyodo, T.; Ozeki, A.; Lee, H.; Takahashi, T.; Imaizumi, A.; Tsuda, T. Highly Dispersible and Bioavailable Curcumin but not Native Curcumin Induces Brown-Like Adipocyte Formation in Mice. Mol. Nutr. Food Res. 2018, 62, 1700731. [Google Scholar] [CrossRef]
- An, S.M.; Seong, K.Y.; Yim, S.G.; Hwang, Y.J.; Bae, S.H.; Yang, S.Y.; An, B.S. Intracutaneous delivery of gelatins induces lipolysis and suppresses lipogenesis of adipocytes. Acta Biomater. 2018, 67, 238–247. [Google Scholar] [CrossRef]
- Han, S.; Kim, Y. Polypyrrole-coated hollow gold nanoshell exerts anti-obesity effects via photothermal lipolysis. Colloids Surf. A Physicochem. Eng. Asp. 2019, 570, 414–419. [Google Scholar] [CrossRef]
- Pires-de-Campos, M.S.M.; De Almeida, J.; Wolf-Nunes, V.; Souza-Francesconi, E.; Grassi-Kassisse, D.M. Ultrasound associated with caffeine increases basal and beta-adrenoceptor response in adipocytes isolated from subcutaneous adipose tissue in pigs. J. Cosmet. Laser Ther. 2016, 18, 116–123. [Google Scholar] [CrossRef] [PubMed]
- González-García, I.; Milbank, E.; Diéguez, C.; López, M.; Contreras, C. Glucagon, GLP-1 and thermogenesis. Int. J. Mol. Sci. 2019, 20, 3445. [Google Scholar] [CrossRef] [PubMed]
- Milton-Laskíbar, I.; Gómez-Zorita, S.; Arias, N.; Romo-Miguel, N.; González, M.; Fernández-Quintela, A.; Portillo, M. Effects of resveratrol and its derivative pterostilbene on brown adipose tissue thermogenic activation and on white adipose tissue browning process. J. Physiol. Biochem. 2020, 76, 269–278. [Google Scholar] [CrossRef]
- Xiao, C.; Goldgof, M.; Gavrilova, O.; Reitman, M.L. Anti-obesity and metabolic efficacy of the β3-adrenergic agonist, CL316243, in mice at thermoneutrality compared to 22 °C. Obesity 2015, 23, 1450–1459. [Google Scholar] [CrossRef]
- Michel, M.C.; Gravas, S. Safety and tolerability of β3-adrenoceptor agonists in the treatment of overactive bladder syndrome–insight from transcriptosome and experimental studies. Expert Opin. Drug Saf. 2016, 15, 647–657. [Google Scholar] [CrossRef] [PubMed]
- Weiner, J.; Hankir, M.; Heiker, J.T.; Fenske, W.; Krause, K. Thyroid hormones and browning of adipose tissue. Mol. Cell. Endocrinol. 2017, 458, 156–159. [Google Scholar] [CrossRef]
- Brent, G.A. Mechanisms of thyroid hormone action. J. Clin. Investig. 2012, 122, 3035–3043. [Google Scholar] [CrossRef]
- Sharma, K.; Arya, R.; Mehta, R.; Sharma, R.; Sharma, K.A. Hypothyroidism and cardiovascular disease: Factors, mechanism and future perspectives. Curr. Med. Chem. 2013, 20, 4411–4418. [Google Scholar] [CrossRef]
- Qiang, L.; Wang, L.; Kon, N.; Zhao, W.; Lee, S.; Zhang, Y.; Rosenbaum, M.; Zhao, Y.; Gu, W.; Farmer, S.R. Brown remodeling of white adipose tissue by SirT1-dependent deacetylation of Pparγ. Cell 2012, 150, 620–632. [Google Scholar] [CrossRef]
- Kolli, V.; Stechschulte, L.A.; Dowling, A.R.; Rahman, S.; Czernik, P.J.; Lecka-Czernik, B. Partial agonist, telmisartan, maintains PPARγ serine 112 phosphorylation, and does not affect osteoblast differentiation and bone mass. PLoS ONE 2014, 9, e96323. [Google Scholar] [CrossRef]
- Liu, J.; Huang, Z.; Ma, W.; Peng, S.; Li, Y.; Miranda, K.M.; Tian, J.; Zhang, Y. Design and synthesis of rosiglitazone-ferulic acid-nitric oxide donor trihybrids for improving glucose tolerance. Eur. J. Med. Chem. 2019, 162, 650–665. [Google Scholar] [CrossRef]
- Than, A.; Duong, P.K.; Zan, P.; Liu, J.; Leow, M.K.S.; Chen, P. Lancing drug reservoirs into subcutaneous fat to combat obesity and associated metabolic diseases. Small 2020, 16, 2002872. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, R.C.; Mohan, S. Thyroid hormone acting via TRβ induces expression of browning genes in mouse bone marrow adipose tissue. Endocrine 2017, 56, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Than, A.; Liang, K.; Xu, S.; Sun, L.; Duan, H.; Xi, F.; Xu, C.; Chen, P. Transdermal delivery of anti-obesity compounds to subcutaneous adipose tissue with polymeric microneedle patches. Small Methods 2017, 1, 1700269. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, Q.; Yu, J.; Yu, S.; Wang, J.; Qiang, L.; Gu, Z. Locally Induced Adipose Tissue Browning by Microneedle Patch for Obesity Treatment. ACS Nano 2017, 11, 9223–9230. [Google Scholar] [CrossRef]
- Wang, S.; Liang, X.; Yang, Q.; Fu, X.; Rogers, C.J.; Zhu, M.; Rodgers, B.D.; Jiang, Q.; Dodson, M.V.; Du, M. Resveratrol induces brown-like adipocyte formation in white fat through activation of AMP-activated protein kinase (AMPK) alpha1. Int. J. Obes. 2015, 39, 967–976. [Google Scholar] [CrossRef] [PubMed]
- Ariamoghaddam, A.R.; Ebrahimi-Hosseinzadeh, B.; Hatamian-Zarmi, A.; Sahraeian, R. In vivo anti-obesity efficacy of curcumin loaded nanofibers transdermal patches in high-fat diet induced obese rats. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 92, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Ojulari, O.V.; Lee, S.G.; Nam, J.-O. Therapeutic effect of seaweed derived xanthophyl carotenoid on obesity management; overview of the last decade. Int. J. Mol. Sci. 2020, 21, 2502. [Google Scholar] [CrossRef]
- Moreno-Navarrete, J.M.; Fernandez-Real, J.M. The gut microbiota modulates both browning of white adipose tissue and the activity of brown adipose tissue. Rev. Endocr. Metab. Disord. 2019, 20, 387–397. [Google Scholar] [CrossRef]
- Kida, R.; Yoshida, H.; Murakami, M.; Shirai, M.; Hashimoto, O.; Kawada, T.; Matsui, T.; Funaba, M. Direct action of capsaicin in brown adipogenesis and activation of brown adipocytes. Cell Biochem. Funct. 2016, 34, 34–41. [Google Scholar] [CrossRef]
- Melguizo Rodriguez, L.; Illescas-Montes, R.; Costela-Ruiz, V.; Garcia-Martinez, O. Stimulation of brown adipose tissue by polyphenols in extra virgin olive oil. Crit. Rev. Food Sci. Nutr. 2021, 61, 3481–3488. [Google Scholar] [CrossRef] [PubMed]
- Dangol, M.; Kim, S.; Li, C.G.; Lahiji, S.F.; Jang, M.; Ma, Y.; Huh, I.; Jung, H. Anti-obesity effect of a novel caffeine-loaded dissolving microneedle patch in high-fat diet-induced obese C57BL/6J mice. J. Control. Release 2017, 265, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Jeong, H.S.; Lee, D.H.; Beack, S.; Kim, T.; Lee, G.H.; Park, W.C.; Kim, C.; Kim, K.S.; Hahn, S.K. Targeted Hyaluronate-Hollow Gold Nanosphere Conjugate for Anti-Obesity Photothermal Lipolysis. ACS Biomater. Sci. Eng. 2017, 3, 3646–3653. [Google Scholar] [CrossRef]
- Fu, C.; Jiang, Y.; Guo, J.; Su, Z. Natural products with anti-obesity effects and different mechanisms of action. J. Agric. Food. Chem. 2016, 64, 9571–9585. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, H.; Shimada, Y.; Zang, L.; Terasawa, M.; Nishiura, K.; Matsuda, K.; Toombs, C.; Langdon, C.; Nishimura, N. Novel anti-obesity properties of palmaria mollis in zebrafish and mouse models. Nutrients 2018, 10, 1401. [Google Scholar] [CrossRef]
- Karu, N.; Reifen, R.; Kerem, Z. Weight gain reduction in mice fed Panax ginseng saponin, a pancreatic lipase inhibitor. J. Agric. Food. Chem. 2007, 55, 2824–2828. [Google Scholar] [CrossRef]
- Arai, T.; Kim, H.-J.; Chiba, H.; Matsumoto, A. Anti-obesity effect of fish oil and fish oil-fenofibrate combination in female KK mice. J. Atheroscler. Thromb. 2009, 16, 674–683. [Google Scholar] [CrossRef]
- Lyznicki, J.M.; Young, D.C.; Riggs, J.A.; Davis, R.M. Obesity: Assessment and management in primary care. Am. Fam. Physician 2001, 63, 2185. [Google Scholar]
- Perva-Uzunalić, A.; Škerget, M.; Knez, Ž.; Weinreich, B.; Otto, F.; Grüner, S. Extraction of active ingredients from green tea (Camellia sinensis): Extraction efficiency of major catechins and caffeine. Food Chem. 2006, 96, 597–605. [Google Scholar] [CrossRef]
- Prasanth, M.I.; Sivamaruthi, B.S.; Chaiyasut, C.; Tencomnao, T. A review of the role of green tea (Camellia sinensis) in antiphotoaging, stress resistance, neuroprotection, and autophagy. Nutrients 2019, 11, 474. [Google Scholar] [CrossRef]
- Bailey, H.H.; Mukhtar, H. Green tea polyphenols and cancer chemoprevention of genitourinary cancer. Am. Soc. Clin. Oncol. Educ. Book 2013, 33, 92–96. [Google Scholar] [CrossRef]
- Saleem, M.; Adhami, V.M.; Siddiqui, I.A.; Mukhtar, H. Tea beverage in chemoprevention of prostate cancer: A mini-review. Nutr. Cancer 2003, 47, 13–23. [Google Scholar] [CrossRef]
- Yang, C.S.; Wang, H. Cancer preventive activities of tea catechins. Molecules 2016, 21, 1679. [Google Scholar] [CrossRef] [PubMed]
- Legeay, S.; Rodier, M.; Fillon, L.; Faure, S.; Clere, N. Epigallocatechin gallate: A review of its beneficial properties to prevent metabolic syndrome. Nutrients 2015, 7, 5443–5468. [Google Scholar] [CrossRef] [PubMed]
- Thielecke, F.; Boschmann, M. The potential role of green tea catechins in the prevention of the metabolic syndrome—A review. Phytochemistry 2009, 70, 11–24. [Google Scholar] [CrossRef]
- Suzuki, T.; Pervin, M.; Goto, S.; Isemura, M.; Nakamura, Y. Beneficial effects of tea and the green tea catechin epigallocatechin-3-gallate on obesity. Molecules 2016, 21, 1305. [Google Scholar] [CrossRef]
- Kaihatsu, K.; Yamabe, M.; Ebara, Y. Antiviral mechanism of action of epigallocatechin-3-O-gallate and its fatty acid esters. Molecules 2018, 23, 2475. [Google Scholar] [CrossRef] [PubMed]
- Furushima, D.; Ide, K.; Yamada, H. Effect of tea catechins on influenza infection and the common cold with a focus on epidemiological/clinical studies. Molecules 2018, 23, 1795. [Google Scholar] [CrossRef]
- Tijburg, L.; Mattern, T.; Folts, J.; Weisgerber, U.; Katan, M. Tea flavonoids and cardiovascular diseases: A review. Crit. Rev. Food Sci. Nutr. 1997, 37, 771–785. [Google Scholar] [CrossRef]
- Pervin, M.; Unno, K.; Ohishi, T.; Tanabe, H.; Miyoshi, N.; Nakamura, Y. Beneficial effects of green tea catechins on neurodegenerative diseases. Molecules 2018, 23, 1297. [Google Scholar] [CrossRef]
- Zang, L.; Shimada, Y.; Nakayama, H.; Kim, Y.; Chu, D.-C.; Juneja, L.R.; Kuroyanagi, J.; Nishimura, N. RNA-seq based transcriptome analysis of the anti-obesity effect of green tea extract using zebrafish obesity models. Molecules 2019, 24, 3256. [Google Scholar] [CrossRef] [PubMed]
- Kajimoto, O.; Kajimoto, Y.; Yabune, M.; Nakamura, T.; Kotani, K.; Suzuki, Y.; Nozawa, A.; Nagata, K.; Unno, T.; Sagesaka, Y.M. Tea catechins with a galloyl moiety reduce body weight and fat. J. Health Sci. 2005, 51, 161–171. [Google Scholar] [CrossRef]
- Nagao, T.; Hase, T.; Tokimitsu, I. A green tea extract high in catechins reduces body fat and cardiovascular risks in humans. Obesity 2007, 15, 1473–1483. [Google Scholar] [CrossRef] [PubMed]
- Auvichayapat, P.; Prapochanung, M.; Tunkamnerdthai, O.; Sripanidkulchai, B.-O.; Auvichayapat, N.; Thinkhamrop, B.; Kunhasura, S.; Wongpratoom, S.; Sinawat, S.; Hongprapas, P. Effectiveness of green tea on weight reduction in obese Thais: A randomized, controlled trial. Physiol. Behav. 2008, 93, 486–491. [Google Scholar] [CrossRef]
- Sun, N.-N.; Wu, T.-Y.; Chau, C.-F. Natural dietary and herbal products in anti-obesity treatment. Molecules 2016, 21, 1351. [Google Scholar] [CrossRef] [PubMed]
- Han, L.-K.; Zheng, Y.-N.; Yoshikawa, M.; Okuda, H.; Kimura, Y. Anti-obesity effects of chikusetsusaponins isolated from Panax japonicus rhizomes. BMC Complement. Altern. Med. 2005, 5, 1–10. [Google Scholar] [CrossRef]
- Han, L.; Takaku, T.; Li, J.; Kimura, Y.; Okuda, H. Anti-obesity action of oolong tea. Int. J. Obes. 1999, 23, 98–105. [Google Scholar] [CrossRef]
- Yamamoto, M.; Shimura, S.; Itoh, Y.; Ohsaka, T.; Egawa, M.; Inoue, S. Anti-obesity effects of lipase inhibitor CT-II, an extract from edible herbs, Nomame Herba, on rats fed a high-fat diet. Int. J. Obes. 2000, 24, 758–764. [Google Scholar] [CrossRef]
- Handa, T.; Yamaguchi, K.; Sono, Y.; Yazawa, K. Effects of fenugreek seed extract in obese mice fed a high-fat diet. Biosci. Biotechnol. Biochem. 2005, 69, 1186–1188. [Google Scholar] [CrossRef]
- Han, L.K.; Sumiyoshi, M.; Zhang, J.; Liu, M.X.; Zhang, X.F.; Zheng, Y.N.; Okuda, H.; Kimura, Y. Anti-obesity action of Salix matsudana leaves (Part 1). Anti-obesity action by polyphenols of Salix matsudana in high fat-diet treated rodent animals. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2003, 17, 1188–1194. [Google Scholar]
- Moreno, D.A.; Ilic, N.; Poulev, A.; Brasaemle, D.L.; Fried, S.K.; Raskin, I. Inhibitory effects of grape seed extract on lipases. Nutrition 2003, 19, 876–879. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, K.; Matsuda, H.; Shimoda, H.; Nishida, N.; Kasajima, N.; Yoshino, T.; Morikawa, T.; Yoshikawa, M. Carnosic acid, a new class of lipid absorption inhibitor from sage. Biorg. Med. Chem. Lett. 2004, 14, 1943–1946. [Google Scholar] [CrossRef] [PubMed]
- Hatano, T.; Yamashita, A.; Hashimoto, T.; Ito, H.; Kubo, N.; Yoshiyama, M.; Shimura, S.; Itoh, Y.; Okuda, T.; Yoshida, T. Flavan dimers with lipase inhibitory activity from Cassia nomame. Phytochemistry 1997, 46, 893–900. [Google Scholar] [CrossRef]
- Kawaguchi, K.; Mizuno, T.; Aida, K.; Uchino, K. Hesperidin as an inhibitor of lipases from porcine pancreas and Pseudomonas. Biosci. Biotechnol. Biochem. 1997, 61, 102–104. [Google Scholar] [CrossRef]
- Gades, M.D.; Stern, J.S. Chitosan supplementation and fecal fat excretion in men. Obes. Res. 2003, 11, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Mutoh, M.; Nakada, N.; Matsukuma, S.; Ohshima, S.; Yoshinri, K.; Watanabe, J.; Arisawa, M. Panclicins, novel pancreatic lipase inhibitors I. Taxonomy, fermentation, isolation and biological activity. J. Antibiot. 1994, 47, 1369–1375. [Google Scholar] [CrossRef]
- Kitahara, M.; Asano, M.; Naganawa, H.; Maeda, K.; Hamada, M.; Aoyagi, T.; Umezawa, H.; Iitaka, Y.; Nakamura, H. Valilactone, an inhibitor of esterase, produced by actinomycetes. J. Antibiot. 1987, 40, 1647–1650. [Google Scholar] [CrossRef][Green Version]
- de la Garza, A.L.; Milagro, F.I.; Boque, N.; Campión, J.; Martínez, J.A. Natural inhibitors of pancreatic lipase as new players in obesity treatment. Planta Med. 2011, 77, 773–785. [Google Scholar] [CrossRef]
- Kim, J.H.; Hahm, D.H.; Yang, D.C.; Kim, J.H.; Lee, H.J.; Shim, I. Effect of crude saponin of Korean Red Ginseng on high fat diet-induced obesity in the rat. J. Pharmacol. Sci. 2005, 97, 124–131. [Google Scholar] [CrossRef]
- Moon, H.-S.; Lee, H.-G.; Choi, Y.-J.; Kim, T.-G.; Cho, C.-S. Proposed mechanisms of (−)-epigallocatechin-3-gallate for anti-obesity. Chem. Biol. Interact. 2007, 167, 85–98. [Google Scholar] [CrossRef]
- MacLean, D.B.; Luo, L.-G. Increased ATP content/production in the hypothalamus may be a signal for energy-sensing of satiety: Studies of the anorectic mechanism of a plant steroidal glycoside. Brain Res. 2004, 1020, 1–11. [Google Scholar] [PubMed]
- Baintner, K.; Kiss, P.; Pfüller, U.; Bardocz, S.; Pusztai, A. Effect of orally and intraperitoneally administered plant lectins on food consumption of rats. Acta Physiol. Hung. 2003, 90, 97–107. [Google Scholar] [CrossRef]
- Pasman, W.J.; Heimerikx, J.; Rubingh, C.M.; van den Berg, R.; O‘Shea, M.; Gambelli, L.; Hendriks, H.F.; Einerhand, A.W.; Scott, C.; Keizer, H.G. The effect of Korean pine nut oil on in vitro CCK release, on appetite sensations and on gut hormones in post-menopausal overweight women. Lipids Health Dis. 2008, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Fleming, R. The effect of ephedra and high fat dieting: A cause for concern! A case report. Angiology 2007, 58, 102–105. [Google Scholar] [CrossRef]
- Klontz, K.C.; Timbo, B.B.; Street, D. Consumption of dietary supplements containing citrus aurantium (bitter orange)—2004 California behavioral risk factor surveillance survey (BRFSS). Ann. Pharmacother. 2006, 40, 1747–1751. [Google Scholar] [CrossRef]
- Husain, G.M.; Chatterjee, S.S.; Singh, P.N.; Kumar, V. Hypolipidemic and antiobesity-like activity of standardised extract of Hypericum perforatum L. in rats. Int. Sch. Res. Not. 2011, 2011, 505247. [Google Scholar] [CrossRef]
- Hsu, H.-K.; Yang, Y.-C.; Hwang, J.-H.; Hong, S.-J. Effects of Toona sinensis leaf extract on lipolysis in differentiated 3T3-L1 adipocytes. Kaohsiung J. Med. Sci. 2003, 19, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Takahashi, M.; Ezaki, O. Fish oil feeding decreases mature sterol regulatory element-binding protein 1 (SREBP-1) by down-regulation of SREBP-1c mRNA in mouse liver: A possible mechanism for down-regulation of lipogenic enzyme mRNAs. J. Biol. Chem. 1999, 274, 25892–25898. [Google Scholar] [CrossRef]
- Uto-Kondo, H.; Ohmori, R.; Kiyose, C.; Kishimoto, Y.; Saito, H.; Igarashi, O.; Kondo, K. Tocotrienol suppresses adipocyte differentiation and Akt phosphorylation in 3T3-L1 preadipocytes. J. Nutr. 2009, 139, 51–57. [Google Scholar] [CrossRef]
- Ku, H.-C.; Chang, H.-H.; Liu, H.-C.; Hsiao, C.-H.; Lee, M.-J.; Hu, Y.-J.; Hung, P.-F.; Liu, C.-W.; Kao, Y.-H. Green tea (−)-epigallocatechin gallate inhibits insulin stimulation of 3T3-L1 preadipocyte mitogenesis via the 67-kDa laminin receptor pathway. Am. J. Physiol.-Cell Physiol. 2009, 297, C121–C132. [Google Scholar] [CrossRef]
- Hwang, J.T.; Lee, M.S.; Kim, H.J.; Sung, M.J.; Kim, H.Y.; Kim, M.S.; Kwon, D.Y. Antiobesity effect of ginsenoside Rg3 involves the AMPK and PPAR-γ signal pathways. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2009, 23, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Ka, S.-O.; Kim, K.-A.; Kwon, K.-B.; Park, J.-W.; Park, B.-H. Silibinin attenuates adipogenesis in 3T3-L1 preadipocytes through a potential upregulation of the insig pathway. Int. J. Mol. Med. 2009, 23, 633–637. [Google Scholar] [PubMed]
- Ambati, S.; Yang, J.Y.; Rayalam, S.; Park, H.J.; Della-Fera, M.A.; Baile, C.A. Ajoene exerts potent effects in 3T3-L1 adipocytes by inhibiting adipogenesis and inducing apoptosis. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2009, 23, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Tabuchi, T.; Tamaki, Y.; Kosaka, K.; Takikawa, Y.; Satoh, T. Carnosic acid and carnosol inhibit adipocyte differentiation in mouse 3T3-L1 cells through induction of phase2 enzymes and activation of glutathione metabolism. Biochem. Biophys. Res. Commun. 2009, 382, 549–554. [Google Scholar] [CrossRef]
- Ejaz, A.; Wu, D.; Kwan, P.; Meydani, M. Curcumin inhibits adipogenesis in 3T3-L1 adipocytes and angiogenesis and obesity in C57/BL mice. J. Nutr. 2009, 139, 919–925. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-Y.; Della-Fera, M.A.; Rayalam, S.; Baile, C.A. Effect of xanthohumol and isoxanthohumol on 3T3-L1 cell apoptosis and adipogenesis. Apoptosis 2007, 12, 1953–1963. [Google Scholar] [CrossRef]
- Lee, J.; Chae, K.; Ha, J.; Park, B.-Y.; Lee, H.S.; Jeong, S.; Kim, M.-Y.; Yoon, M. Regulation of obesity and lipid disorders by herbal extracts from Morus alba, Melissa officinalis, and Artemisia capillaris in high-fat diet-induced obese mice. J. Ethnopharmacol. 2008, 115, 263–270. [Google Scholar] [CrossRef]
- Weisberg, S.P.; Leibel, R.; Tortoriello, D.V. Dietary curcumin significantly improves obesity-associated inflammation and diabetes in mouse models of diabesity. Endocrinology 2008, 149, 3549–3558. [Google Scholar] [CrossRef]
- Birari, R.B.; Gupta, S.; Mohan, C.G.; Bhutani, K.K. Antiobesity and lipid lowering effects of Glycyrrhiza chalcones: Experimental and computational studies. Phytomedicine 2011, 18, 795–801. [Google Scholar] [CrossRef]
- Park, M.-Y.; Lee, K.-S.; Sung, M.-K. Effects of dietary mulberry, Korean red ginseng, and banaba on glucose homeostasis in relation to PPAR-α, PPAR-γ, and LPL mRNA expressions. Life Sci. 2005, 77, 3344–3354. [Google Scholar] [CrossRef]
- Tsuda, T.; Horio, F.; Uchida, K.; Aoki, H.; Osawa, T. Dietary cyanidin 3-O-β-D-glucoside-rich purple corn color prevents obesity and ameliorates hyperglycemia in mice. J. Nutr. 2003, 133, 2125–2130. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-Y.; Lee, S.-J.; Park, H.-W.; Cha, Y.-S. Effect of genistein with carnitine administration on lipid parameters and obesity in C57Bl/6J mice fed a high-fat diet. J. Med. Food 2006, 9, 459–467. [Google Scholar] [CrossRef]
- Yoon, S.-S.; Rhee, Y.-H.; Lee, H.-J.; Lee, E.-O.; Lee, M.-H.; Ahn, K.-S.; Lim, H.-T.; Kim, S.-H. Uncoupled protein 3 and p38 signal pathways are involved in anti-obesity activity of Solanum tuberosum L. cv. Bora Valley. J. Ethnopharmacol. 2008, 118, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Shimoda, H.; Seki, E.; Aitani, M. Inhibitory effect of green coffee bean extract on fat accumulation and body weight gain in mice. BMC Complement. Altern. Med. 2006, 6, 1–9. [Google Scholar] [CrossRef]
- Shimada, T.; Hiramatsu, N.; Kasai, A.; Mukai, M.; Okamura, M.; Yao, J.; Huang, T.; Tamai, M.; Takahashi, S.; Nakamura, T. Suppression of adipocyte differentiation by Cordyceps militaris through activation of the aryl hydrocarbon receptor. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E859–E867. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saito, M.; Ueno, M.; Ogino, S.; Kubo, K.; Nagata, J.; Takeuchi, M. High dose of Garcinia cambogia is effective in suppressing fat accumulation in developing male Zucker obese rats, but highly toxic to the testis. Food Chem. Toxicol. 2005, 43, 411–419. [Google Scholar] [CrossRef]
- Kim, M.S.; Kim, J.K.; Kwon, D.Y.; Park, R. Anti-adipogenic effects of Garcinia extract on the lipid droplet accumulation and the expression of transcription factor. Biofactors 2004, 22, 193–196. [Google Scholar] [CrossRef]
- Zhang, W.; Sheng, T.; Gu, Z.; Zhang, Y. Strategies for Browning Agent Delivery. Pharm. Res. 2021, 38, 1327–1334. [Google Scholar] [CrossRef]
- Fenton, O.S.; Olafson, K.N.; Pillai, P.S.; Mitchell, M.J.; Langer, R. Advances in biomaterials for drug delivery. Adv. Mater. 2018, 30, 1705328. [Google Scholar] [CrossRef]
- Park, Y.S.; David, A.E.; Huang, Y.; Park, J.-B.; He, H.; Byun, Y.; Yang, V.C. In vivo delivery of cell-permeable antisense hypoxia-inducible factor 1α oligonucleotide to adipose tissue reduces adiposity in obese mice. J. Control. Release 2012, 161, 1–9. [Google Scholar] [CrossRef]
- Kuss, M.; Kim, J.; Qi, D.; Wu, S.; Lei, Y.; Chung, S.; Duan, B. Effects of tunable, 3D-bioprinted hydrogels on human brown adipocyte behavior and metabolic function. Acta Biomater. 2018, 71, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Kuang, L.; Merkel, M.P.; Yue, F.; Cano-Vega, M.A.; Narayanan, N.; Kuang, S.; Deng, M. Biodegradable Polymeric Microsphere-Based Drug Delivery for Inductive Browning of Fat. Front. Endocrinol. 2015, 6, 169. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Han, D.; Kang, H.-G.; Jeong, S.J.; Jo, J.-E.; Shin, J.; Kim, D.K.; Park, H.-W. Intravenous sustained-release nifedipine ameliorates nonalcoholic fatty liver disease by restoring autophagic clearance. Biomaterials 2019, 197, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zu, Y.; Overby, H.; Ren, G.; Fan, Z.; Zhao, L.; Wang, S. Resveratrol liposomes and lipid nanocarriers: Comparison of characteristics and inducing browning of white adipocytes. Colloids Surf. B Biointerfaces 2018, 164, 414–423. [Google Scholar] [CrossRef]
- Akgönüllü, S.; Özgür, E.; Denizli, A. Recent Advances in Quartz Crystal Microbalance Biosensors Based on the Molecular Imprinting Technique for Disease-Related Biomarkers. Chemosensors 2022, 10, 106. [Google Scholar] [CrossRef]
- McDaid, W.J.; Lissin, N.; Pollheimer, E.; Greene, M.; Leach, A.; Smyth, P.; Bossi, G.; Longley, D.; Cole, D.K.; Scott, C.J. Enhanced target-specific delivery of docetaxel-loaded nanoparticles using engineered T cell receptors. Nanoscale 2021, 13, 15010–15020. [Google Scholar] [CrossRef]
- Kumari, M.; Acharya, A.; Krishnamurthy, P.T. Antibody-conjugated nanoparticles for target-specific drug delivery of chemotherapeutics. Beilstein J. Nanotechnol. 2023, 14, 912–926. [Google Scholar] [CrossRef]
- Goddard, Z.R.; Marín, M.J.; Russell, D.A.; Searcey, M. Active targeting of gold nanoparticles as cancer therapeutics. Chem. Soc. Rev. 2020, 49, 8774–8789. [Google Scholar] [CrossRef]
- Singh, G.; Chawla, P.A.; Faruk, A.; Chawla, V.; Kaur, A. Computational Design of Molecularly Imprinted Polymers in Drug Delivery Systems: A Comprehensive Review. Curr. Drug Deliv. 2023, 20, 75–88. [Google Scholar]
- Feng, Q.; Tong, R. Anticancer nanoparticulate polymer-drug conjugate. Bioeng. Transl. Med. 2016, 1, 277–296. [Google Scholar] [CrossRef]
- Delplace, V.; Couvreur, P.; Nicolas, J. Recent trends in the design of anticancer polymer prodrug nanocarriers. Polym. Chem. 2014, 5, 1529–1544. [Google Scholar] [CrossRef]
- Liao, L.; Liu, J.; Dreaden, E.C.; Morton, S.W.; Shopsowitz, K.E.; Hammond, P.T.; Johnson, J.A. A convergent synthetic platform for single-nanoparticle combination cancer therapy: Ratiometric loading and controlled release of cisplatin, doxorubicin, and camptothecin. JACS 2014, 136, 5896–5899. [Google Scholar] [CrossRef] [PubMed]
- Gao, A.X.; Liao, L.; Johnson, J.A. Synthesis of acid-labile PEG and PEG-doxorubicin-conjugate nanoparticles via Brush-First ROMP. ACS Macro Lett. 2014, 3, 854–857. [Google Scholar] [CrossRef]
- Hu, X.; Hu, J.; Tian, J.; Ge, Z.; Zhang, G.; Luo, K.; Liu, S. Polyprodrug amphiphiles: Hierarchical assemblies for shape-regulated cellular internalization, trafficking, and drug delivery. JACS 2013, 135, 17617–17629. [Google Scholar] [CrossRef]
- Liu, J.; Liu, W.; Weitzhandler, I.; Bhattacharyya, J.; Li, X.; Wang, J.; Qi, Y.; Bhattacharjee, S.; Chilkoti, A. Ring-opening polymerization of prodrugs: A versatile approach to prepare well-defined drug-loaded nanoparticles. Angew. Chem. 2015, 127, 1016–1020. [Google Scholar] [CrossRef]
- Shree, D.; Patra, C.N.; Sahoo, B.M. Applications of nanotechnology-mediated herbal nanosystems for ophthalmic drug. Pharm. Nanotechnol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Alven, S.; Aderibigbe, B.; Balogun, M.O.; Matshe, W.M.; Ray, S.S. Polymer-drug conjugates containing antimalarial drugs and antibiotics. J. Drug Deliv. Sci. Technol. 2019, 53, 101171. [Google Scholar] [CrossRef]
- Srivastava, A.; Yadav, T.; Sharma, S.; Nayak, A.; Kumari, A.A.; Mishra, N. Polymers in drug delivery. J. Biosci. Med. 2015, 4, 69–84. [Google Scholar] [CrossRef]
- Sanchis, J.; Canal, F.; Lucas, R.; Vicent, M.J. Polymer–drug conjugates for novel molecular targets. Nanomedicine 2010, 5, 915–935. [Google Scholar] [CrossRef]
- Pasut, G.; Veronese, F. Polymer–drug conjugation, recent achievements and general strategies. Prog. Polym. Sci. 2007, 32, 933–961. [Google Scholar] [CrossRef]
- Myers, M.G., Jr.; Leibel, R.L.; Seeley, R.J.; Schwartz, M.W. Obesity and leptin resistance: Distinguishing cause from effect. Trends Endocrinol. Metab. 2010, 21, 643–651. [Google Scholar] [CrossRef]
- Yi, X.; Yuan, D.; Farr, S.A.; Banks, W.A.; Poon, C.D.; Kabanov, A.V. Pluronic modified leptin with increased systemic circulation, brain uptake and efficacy for treatment of obesity. J. Control. Release 2014, 191, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Yuan, D.; Yi, X.; Zhao, Y.; Poon, C.D.; Bullock, K.M.; Hansen, K.M.; Salameh, T.S.; Farr, S.A.; Banks, W.A.; Kabanov, A.V. Intranasal delivery of N-terminal modified leptin-pluronic conjugate for treatment of obesity. J. Control. Release 2017, 263, 172–184. [Google Scholar] [CrossRef]
- Yan, C.; Zhang, J.; Huang, M.; Xiao, J.; Li, N.; Wang, T.; Ling, R. Design, strategies, and therapeutics in nanoparticle-based siRNA delivery systems for breast cancer. J. Mater. Chem. B 2023, 11, 8096–8116. [Google Scholar] [CrossRef]
- Saltiel, A.R.; Olefsky, J.M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Investig. 2017, 127, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Graversen, J.H.; Svendsen, P.; Dagnaes-Hansen, F.; Dal, J.; Anton, G.; Etzerodt, A.; Petersen, M.D.; Christensen, P.A.; Moller, H.J.; Moestrup, S.K. Targeting the hemoglobin scavenger receptor CD163 in macrophages highly increases the anti-inflammatory potency of dexamethasone. Mol. Ther. 2012, 20, 1550–1558. [Google Scholar] [CrossRef]
- Ma, L.; Liu, T.W.; Wallig, M.A.; Dobrucki, I.T.; Dobrucki, L.W.; Nelson, E.R.; Swanson, K.S.; Smith, A.M. Efficient Targeting of Adipose Tissue Macrophages in Obesity with Polysaccharide Nanocarriers. ACS Nano 2016, 10, 6952–6962. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.-J.; Rahman, A.; Kim, S.-W.; Baek, Y.-M.; Hwang, H.-J.; Oh, J.-Y.; Hwang, H.-S.; Lee, S.-H.; Yun, J.-W. Chitosan oligosaccharides inhibit adipogenesis in 3T3-L1 adipocytes. J. Microbiol. Biotechnol. 2008, 18, 80–87. [Google Scholar] [PubMed]
- Cui, J.; Li, M.; Wei, Y.; Li, H.; He, X.; Yang, Q.; Li, Z.; Duan, J.; Wu, Z.; Chen, Q. Inhalation aromatherapy via brain-targeted nasal delivery: Natural volatiles or essential oils on mood disorders. Front. Pharmacol. 2022, 13, 860043. [Google Scholar] [CrossRef]
- Li, J.; Mooney, D.J. Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 2016, 1, 1–17. [Google Scholar] [CrossRef]
- Ahmed, E.M. Hydrogel: Preparation, characterization, and applications: A review. J. Adv. Res. 2015, 6, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Gulrez, S.K.; Al-Assaf, S.; Phillips, G.O. Hydrogels: Methods of preparation, characterisation and applications. In Progress in Molecular and Environmental Bioengineering–From Analysis and Modeling to Technology Applications; IntechOpen: Rijeka, Croatiap, 2011; p. 117150. [Google Scholar]
- Schacht, E. Polymer chemistry and hydrogel systems. J. Phys. Conf. Ser. 2004, 3, 22. [Google Scholar] [CrossRef]
- Schmidt, B.V. Hydrophilic polymers. Polymers 2019, 11, 693. [Google Scholar] [CrossRef] [PubMed]
- Liechty, W.B.; Kryscio, D.R.; Slaughter, B.V.; Peppas, N.A. Polymers for drug delivery systems. Annu. Rev. Chem. Biomol. Eng. 2010, 1, 149. [Google Scholar] [CrossRef]
- Mitchell, H.; Hamilton, T.; Steggerda, F.; Bean, H. The chemical composition of the adult human body and its bearing on the biochemistry of growth. J. Biol. Chem. 1945, 158, 625–637. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, A. Study on superabsorbent composites. IX: Synthesis, characterization and swelling behaviors of polyacrylamide/clay composites based on various clays. React. Funct. Polym. 2007, 67, 737–745. [Google Scholar] [CrossRef]
- Maitra, J.; Shukla, V.K. Cross-linking in hydrogels—A review. Am. J. Polym. Sci 2014, 4, 25–31. [Google Scholar]
- Mishra, B.; Upadhyay, M.; Reddy Adena, S.; Vasant, B.; Muthu, M. Hydrogels: An introduction to a controlled drug delivery device, synthesis and application in drug delivery and tissue engineering. Austin J Biomed Eng 2017, 4, 1037–1049. [Google Scholar]
- Hennink, W.E.; van Nostrum, C.F. Novel crosslinking methods to design hydrogels. Adv. Drug Deliv. Rev. 2012, 64, 223–236. [Google Scholar] [CrossRef]
- Wei, M.; Gao, Y.; Li, X.; Serpe, M.J. Stimuli-responsive polymers and their applications. Polym. Chem. 2017, 8, 127–143. [Google Scholar] [CrossRef]
- Shin, J.; Braun, P.V.; Lee, W. Fast response photonic crystal pH sensor based on templated photo-polymerized hydrogel inverse opal. Sens. Actuators B Chem. 2010, 150, 183–190. [Google Scholar] [CrossRef]
- Liu, S.; Oderinde, O.; Hussain, I.; Yao, F.; Fu, G. Dual ionic cross-linked double network hydrogel with self-healing, conductive, and force sensitive properties. Polymer 2018, 144, 111–120. [Google Scholar] [CrossRef]
- Raeburn, J.; Mendoza-Cuenca, C.; Cattoz, B.N.; Little, M.A.; Terry, A.E.; Cardoso, A.Z.; Griffiths, P.C.; Adams, D.J. The effect of solvent choice on the gelation and final hydrogel properties of Fmoc–diphenylalanine. Soft Matter 2015, 11, 927–935. [Google Scholar] [CrossRef]
- Liu, C.B.; Gong, C.Y.; Huang, M.J.; Wang, J.W.; Pan, Y.F.; Zhang, Y.D.; Li, G.Z.; Gou, M.L.; Wang, K.; Tu, M.J. Thermoreversible gel–sol behavior of biodegradable PCL-PEG-PCL triblock copolymer in aqueous solutions. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 84, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Li, H. Kinetics of smart hydrogels responding to electric field: A transient deformation analysis. Int. J. Solids Struct. 2009, 46, 1326–1333. [Google Scholar] [CrossRef][Green Version]
- Namdeo, M.; Bajpai, S.; Kakkar, S. Preparation of a magnetic-field-sensitive hydrogel and preliminary study of its drug release behavior. J. Biomater. Sci. Polym. Ed. 2009, 20, 1747–1761. [Google Scholar] [CrossRef]
- Ono, K.; Saito, Y.; Yura, H.; Ishikawa, K.; Kurita, A.; Akaike, T.; Ishihara, M. Photocrosslinkable chitosan as a biological adhesive. J. Biomed. Mater. Res. Off. J. Soc. Biomater. Jpn. Soc. Biomater. 2000, 49, 289–295. [Google Scholar] [CrossRef]
- Lin, G.; Chang, S.; Hao, H.; Tathireddy, P.; Orthner, M.; Magda, J.; Solzbacher, F. Osmotic swelling pressure response of smart hydrogels suitable for chronically implantable glucose sensors. Sens. Actuators B Chem. 2010, 144, 332–336. [Google Scholar] [CrossRef]
- Chandrawati, R. Enzyme-responsive polymer hydrogels for therapeutic delivery. Exp. Biol. Med. 2016, 241, 972–979. [Google Scholar] [CrossRef]
- Zhang, R.; Bowyer, A.; Eisenthal, R.; Hubble, J. A smart membrane based on an antigen-responsive hydrogel. Biotechnol. Bioeng. 2007, 97, 976–984. [Google Scholar] [CrossRef]
- Murakami, Y.; Maeda, M. DNA-responsive hydrogels that can shrink or swell. Biomacromolecules 2005, 6, 2927–2929. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wang, W.; Veiseh, O.; Appel, E.A.; Xue, K.; Webber, M.J.; Tang, B.C.; Yang, X.-W.; Weir, G.C.; Langer, R. Injectable and glucose-responsive hydrogels based on boronic acid–glucose complexation. Langmuir 2016, 32, 8743–8747. [Google Scholar] [CrossRef]
- Klaus, S.; Pultz, S.; Thone-Reineke, C.; Wolfram, S. Epigallocatechin gallate attenuates diet-induced obesity in mice by decreasing energy absorption and increasing fat oxidation. Int. J. Obes. 2005, 29, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Gao, C.; Yan, P.; Zhang, M.; Wang, Y.; Hu, Y.; Wu, X.; Wang, X.; Sheng, J. EGCG reduces obesity and white adipose tissue gain partly through AMPK activation in mice. Front. Pharmacol. 2018, 9, 1366. [Google Scholar] [CrossRef]
- Zhang, X.-Z.; Guan, J.; Cai, S.-L.; Du, Q.; Guo, M.-L. Polymeric in situ hydrogel implant of epigallocatechin gallate (EGCG) for prolonged and improved antihyperlipidemic and anti-obesity activity: Preparation and characterization. J. Biomater. Tissue Eng. 2015, 5, 813–817. [Google Scholar] [CrossRef]
- Liao, Z.X.; Liu, M.C.; Kempson, I.M.; Fa, Y.C.; Huang, K.Y. Light-triggered methylcellulose gold nanoparticle hydrogels for leptin release to inhibit fat stores in adipocytes. Int. J. Nanomed. 2017, 12, 7603–7611. [Google Scholar] [CrossRef]
- An, Y.-H.; Lee, J.; Son, D.U.; Kang, D.H.; Park, M.J.; Cho, K.W.; Kim, S.; Kim, S.-H.; Ko, J.; Jang, M.-H. Facilitated transdermal drug delivery using nanocarriers-embedded electroconductive hydrogel coupled with reverse electrodialysis-driven iontophoresis. ACS Nano 2020, 14, 4523–4535. [Google Scholar] [CrossRef]
- Rahman, M.S.; Islam, M.M.; Islam, M.S.; Zaman, A.; Ahmed, T.; Biswas, S.; Sharmeen, S.; Rashid, T.U.; Rahman, M.M. Morphological characterization of hydrogels. In Cellulose-Based Superabsorbent Hydrogels; Springer: Berlin/Heidelberg, Germany, 2019; pp. 819–863. [Google Scholar]
- Soares, P.A.; de Seixas, J.R.C.; Albuquerque, P.B.; Santos, G.R.; Mourão, P.A.; Barros, W., Jr.; Correia, M.T.; Carneiro-da-Cunha, M.G. Development and characterization of a new hydrogel based on galactomannan and κ-carrageenan. Carbohydr. Polym. 2015, 134, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Saima, A.; Saeid, R.; Kanchan, K. Hydrogels as potential drug delivery systems. Sci. Res. Essays 2009, 4, 1175–1183. [Google Scholar]
- Thürmer, M.B.; Diehl, C.E.; Brum, F.J.B.; Santos, L.A.D. Preparation and characterization of hydrogels with potential for use as biomaterials. Mater. Res. 2014, 17, 109–113. [Google Scholar] [CrossRef]
- Onaciu, A.; Munteanu, R.A.; Moldovan, A.I.; Moldovan, C.S.; Berindan-Neagoe, I. Hydrogels based drug delivery synthesis, characterization and administration. Pharmaceutics 2019, 11, 432. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Xiao, C. Synthesis and properties of novel hydrogels from oxidized konjac glucomannan crosslinked gelatin for in vitro drug delivery. Carbohydr. Polym. 2008, 72, 479–489. [Google Scholar] [CrossRef]
- Prausnitz, M.R. Engineering Microneedle Patches for Vaccination and Drug Delivery to Skin. Annu. Rev. Chem. Biomol. Eng. 2017, 8, 177–200. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, J.; Wen, D.; Chen, G.; Gu, Z. The potential of a microneedle patch for reducing obesity. Expert Opin. Drug Deliv. 2018, 15, 431–433. [Google Scholar] [CrossRef] [PubMed]
- Henry, S.; McAllister, D.V.; Allen, M.G.; Prausnitz, M.R. Microfabricated microneedles: A novel approach to transdermal drug delivery. J. Pharm. Sci. 1998, 87, 922–925. [Google Scholar] [CrossRef]
- Chen, X.; Prow, T.W.; Crichton, M.L.; Jenkins, D.W.; Roberts, M.S.; Frazer, I.H.; Fernando, G.J.; Kendall, M.A. Dry-coated microprojection array patches for targeted delivery of immunotherapeutics to the skin. J. Control. Release 2009, 139, 212–220. [Google Scholar] [CrossRef]
- Indermun, S.; Luttge, R.; Choonara, Y.E.; Kumar, P.; Du Toit, L.C.; Modi, G.; Pillay, V. Current advances in the fabrication of microneedles for transdermal delivery. J. Control. Release 2014, 185, 130–138. [Google Scholar] [CrossRef]
- Daddona, P.E.; Matriano, J.; Mandema, J.; Maa, Y.-F. Parathyroid hormone (1-34)-coated microneedle patch system: Clinical pharmacokinetics and pharmacodynamics for treatment of osteoporosis. Pharm. Res. 2011, 28, 159–165. [Google Scholar] [CrossRef]
- McAllister, D.V.; Wang, P.M.; Davis, S.P.; Park, J.-H.; Canatella, P.J.; Allen, M.G.; Prausnitz, M.R. Microfabricated needles for transdermal delivery of macromolecules and nanoparticles: Fabrication methods and transport studies. Proc. Natl. Acad. Sci. USA 2003, 100, 13755–13760. [Google Scholar] [CrossRef]
- Tu, K.-T.; Chung, C.-K. Fabrication of biodegradable polymer microneedle array via CO2 laser ablation. In Proceedings of the 10th IEEE International Conference on Nano/Micro Engineered and Molecular Systems, Xi‘an, China, 7–11 April 2015; pp. 494–497. [Google Scholar]
- Lee, J.W.; Han, M.-R.; Park, J.-H. Polymer microneedles for transdermal drug delivery. J. Drug Target. 2013, 21, 211–223. [Google Scholar] [CrossRef]
- Rouphael, N.G.; Paine, M.; Mosley, R.; Henry, S.; McAllister, D.V.; Kalluri, H.; Pewin, W.; Frew, P.M.; Yu, T.; Thornburg, N.J. The safety, immunogenicity, and acceptability of inactivated influenza vaccine delivered by microneedle patch (TIV-MNP 2015): A randomised, partly blinded, placebo-controlled, phase 1 trial. Lancet 2017, 390, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Gittard, S.D.; Ovsianikov, A.; Chichkov, B.N.; Doraiswamy, A.; Narayan, R.J. Two-photon polymerization of microneedles for transdermal drug delivery. Expert Opin. Drug Deliv. 2010, 7, 513–533. [Google Scholar] [CrossRef]
- Dobrzyńska, E.; Kondej, D.; Kowalska, J.; Szewczyńska, M. Exposure to chemical substances and particles emitted during additive manufacturing. Environ. Sci. Pollut. Res. 2022, 29, 40273–40278. [Google Scholar] [CrossRef] [PubMed]
- Aldawood, F.K.; Andar, A.; Desai, S. A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications. Polymers 2021, 13, 2815. [Google Scholar] [CrossRef] [PubMed]
- Eslick, S.; Williams, E.J.; Berthon, B.S.; Wright, T.; Karihaloo, C.; Gately, M.; Wood, L.G. Weight loss and short-chain fatty acids reduce systemic inflammation in monocytes and adipose tissue macrophages from obese subjects. Nutrients 2022, 14, 765. [Google Scholar] [CrossRef]
- Lopez, Y.R.; Perez-Torres, I.; Zuniga-Munoz, A.; Lans, V.G.; Diaz-Diaz, E.; Castro, E.S.; Espejel, R.V. Effect of Glycine on Adipocyte Hypertrophy in a Metabolic Syndrome Rat Model. Curr. Drug Deliv. 2016, 13, 158–169. [Google Scholar] [CrossRef]
- Yang, H.; Kim, S.; Huh, I.; Kim, S.; Lahiji, S.F.; Kim, M.; Jung, H. Rapid implantation of dissolving microneedles on an electrospun pillar array. Biomaterials 2015, 64, 70–77. [Google Scholar] [CrossRef]
- Xie, Y.; Shao, R.; Lin, Y.; Wang, C.; Tan, Y.; Xie, W.; Sun, S. Improved therapeutic efficiency against obesity through transdermal drug delivery using microneedle arrays. Pharmaceutics 2021, 13, 827. [Google Scholar] [CrossRef]
- Martanto, W.; Davis, S.P.; Holiday, N.R.; Wang, J.; Gill, H.S.; Prausnitz, M.R. Transdermal delivery of insulin using microneedles in vivo. Pharm. Res. 2004, 21, 947–952. [Google Scholar] [CrossRef]
- Liu, S.; Jin, M.-N.; Quan, Y.-S.; Kamiyama, F.; Katsumi, H.; Sakane, T.; Yamamoto, A. The development and characteristics of novel microneedle arrays fabricated from hyaluronic acid, and their application in the transdermal delivery of insulin. J. Control. Release 2012, 161, 933–941. [Google Scholar] [CrossRef]
- Wu, X.-M.; Todo, H.; Sugibayashi, K. Enhancement of skin permeation of high molecular compounds by a combination of microneedle pretreatment and iontophoresis. J. Control. Release 2007, 118, 189–195. [Google Scholar] [CrossRef]
- Chen, H.; Zhu, H.; Zheng, J.; Mou, D.; Wan, J.; Zhang, J.; Shi, T.; Zhao, Y.; Xu, H.; Yang, X. Iontophoresis-driven penetration of nanovesicles through microneedle-induced skin microchannels for enhancing transdermal delivery of insulin. J. Control. Release 2009, 139, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Ye, R.; Yang, J.; Li, Y.; Zheng, Y.; Yang, J.; Li, Y.; Liu, B.; Jiang, L. Fabrication of tip-hollow and tip-dissolvable microneedle arrays for transdermal drug delivery. ACS Biomater. Sci. Eng. 2020, 6, 2487–2494. [Google Scholar] [CrossRef] [PubMed]
- Gupta, J.; Felner, E.I.; Prausnitz, M.R. Minimally invasive insulin delivery in subjects with type 1 diabetes using hollow microneedles. Diabetes Technol. Ther. 2009, 11, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Kochba, E.; Levin, Y.; Raz, I.; Cahn, A. Improved insulin pharmacokinetics using a novel microneedle device for intradermal delivery in patients with type 2 diabetes. Diabetes Technol. Ther. 2016, 18, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Ripolin, A.; Quinn, J.; Larrañeta, E.; Vicente-Perez, E.M.; Barry, J.; Donnelly, R.F. Successful application of large microneedle patches by human volunteers. Int. J. Pharm. 2017, 521, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Choi, S.O.; Felner, E.I.; Prausnitz, M.R. Dissolving microneedle patch for transdermal delivery of human growth hormone. Small 2011, 7, 531–539. [Google Scholar] [CrossRef]
- Kohane, D.S. Microparticles and nanoparticles for drug delivery. Biotechnol. Bioeng. 2007, 96, 203–209. [Google Scholar] [CrossRef]
- Whiting, S.; Derbyshire, E.; Tiwari, B.K. Capsaicinoids and capsinoids. A potential role for weight management? A systematic review of the evidence. Appetite 2012, 59, 341–348. [Google Scholar] [CrossRef]
- Almeida, M.A.; Nadal, J.M.; Grassiolli, S.; Paludo, K.S.; Zawadzki, S.F.; Cruz, L.; Paula, J.P.; Farago, P.V. Enhanced gastric tolerability and improved anti-obesity effect of capsaicinoids-loaded PCL microparticles. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 40, 345–356. [Google Scholar] [CrossRef]
- Tan, S.; Gao, B.; Tao, Y.; Guo, J.; Su, Z.Q. Antiobese effects of capsaicin-chitosan microsphere (CCMS) in obese rats induced by high fat diet. J. Agric. Food. Chem. 2014, 62, 1866–1874. [Google Scholar] [CrossRef] [PubMed]
- Lucas, N.; Legrand, R.; Breton, J.; Dechelotte, P.; Edwards-Levy, F.; Fetissov, S.O. Chronic delivery of alpha-melanocyte-stimulating hormone in rat hypothalamus using albumin-alginate microparticles: Effects on food intake and body weight. Neuroscience 2015, 290, 445–453. [Google Scholar] [CrossRef]
- Hsieh, Y.-W.; Tsai, Y.-W.; Lai, H.-H.; Lai, C.-Y.; Lin, C.-Y.; Her, G.M. Depletion of alpha-melanocyte-stimulating hormone induces insatiable appetite and gains in energy reserves and body weight in zebrafish. Biomedicines 2021, 9, 941. [Google Scholar] [CrossRef]
- Bi, P.; Shan, T.; Liu, W.; Yue, F.; Yang, X.; Liang, X.R.; Wang, J.; Li, J.; Carlesso, N.; Liu, X.; et al. Inhibition of Notch signaling promotes browning of white adipose tissue and ameliorates obesity. Nat. Med. 2014, 20, 911–918. [Google Scholar] [CrossRef] [PubMed]
- Bi, P.; Kuang, S. Notch signaling as a novel regulator of metabolism. Trends Endocrinol. Metab. 2015, 26, 248–255. [Google Scholar] [CrossRef]
- Barten, D.M.; Meredith, J.E.; Zaczek, R.; Houston, J.G.; Albright, C.F. γ-Secretase inhibitors for Alzheimer’s disease. Drugs RD 2006, 7, 87–97. [Google Scholar] [CrossRef]
- Tsou, Y.H.; Wang, B.; Ho, W.; Hu, B.; Tang, P.; Sweet, S.; Zhang, X.Q.; Xu, X. Nanotechnology-Mediated Drug Delivery for the Treatment of Obesity and Its Related Comorbidities. Adv. Healthcare Mater. 2019, 8, e1801184. [Google Scholar] [CrossRef] [PubMed]
- Govender, T.; Stolnik, S.; Garnett, M.C.; Illum, L.; Davis, S.S. PLGA nanoparticles prepared by nanoprecipitation: Drug loading and release studies of a water soluble drug. J. Control. Release 1999, 57, 171–185. [Google Scholar] [CrossRef]
- Zambaux, M.F.; Bonneaux, F.; Gref, R.; Maincent, P.; Dellacherie, E.; Alonso, M.; Labrude, P.; Vigneron, C. Influence of experimental parameters on the characteristics of poly (lactic acid) nanoparticles prepared by a double emulsion method. J. Control. Release 1998, 50, 31–40. [Google Scholar] [CrossRef]
- Singh, Y.; Meher, J.G.; Raval, K.; Khan, F.A.; Chaurasia, M.; Jain, N.K.; Chourasia, M.K. Nanoemulsion: Concepts, development and applications in drug delivery. J. Control. Release 2017, 252, 28–49. [Google Scholar] [CrossRef]
- Yang, J.; Bahreman, A.; Daudey, G.; Bussmann, J.; Olsthoorn, R.C.; Kros, A. Drug delivery via cell membrane fusion using lipopeptide modified liposomes. ACS Cent. Sci. 2016, 2, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Lentz, B.R.; Lee, J. Poly (ethylene glycol)(PEG)-mediated fusion between pure lipid bilayers: A mechanism in common with viral fusion and secretory vesicle release? Mol. Membr. Biol. 1999, 16, 279–296. [Google Scholar] [CrossRef] [PubMed]
- Sancho-Albero, M.; del Mar Encabo-Berzosa, M.; Beltran-Visiedo, M.; Fernandez-Messina, L.; Sebastian, V.; Sanchez-Madrid, F.; Arruebo, M.; Santamaria, J.; Martin-Duque, P. Efficient encapsulation of theranostic nanoparticles in cell-derived exosomes: Leveraging the exosomal biogenesis pathway to obtain hollow gold nanoparticle-hybrids. Nanoscale 2019, 11, 18825–18836. [Google Scholar] [CrossRef] [PubMed]
- Knaack, D.A.; Chang, J.; Thomas, M.J.; Sorci-Thomas, M.; Chen, Y.; Sahoo, D. Scavenger receptor class B type I is required for efficient glucose uptake and metabolic homeostasis in adipocytes. bioRxiv 2023. [Google Scholar] [CrossRef]
- Li, B.; Fu, Y.; Xie, M.; Feng, L.; Niu, X.; Que, L.; You, Z. Gold-based nanoparticles realize photothermal and photodynamic synergistic treatment of liver cancer and improve the anaerobic tumor microenvironment under near-infrared light. Front. Bioeng. Biotechnol. 2022, 10, 957349. [Google Scholar] [CrossRef] [PubMed]
- Hari, S.K.; Gauba, A.; Shrivastava, N.; Tripathi, R.M.; Jain, S.K.; Pandey, A.K. Polymeric micelles and cancer therapy: An ingenious multimodal tumor-targeted drug delivery system. Drug Deliv. Transl. Res. 2023, 13, 135–163. [Google Scholar] [CrossRef]
- Sercombe, L.; Veerati, T.; Moheimani, F.; Wu, S.Y.; Sood, A.K.; Hua, S. Advances and Challenges of Liposome Assisted Drug Delivery. Front. Pharmacol. 2015, 6, 286. [Google Scholar] [CrossRef]
- Ash, G.I.; Kim, D.; Choudhury, M. Promises of Nanotherapeutics in Obesity. Trends Endocrinol. Metab. 2019, 30, 369–383. [Google Scholar] [CrossRef]
- Bai, J.; Yang, E.; Chang, P.-S.; Ryu, S. Preparation and characterization of endolysin-containing liposomes and evaluation of their antimicrobial activities against gram-negative bacteria. Enzym. Microb. Technol. 2019, 128, 40–48. [Google Scholar] [CrossRef]
- Yaroslavov, A.; Efimova, A.; Smirnova, N.; Erzunov, D.; Lukashev, N.; Grozdova, I.; Melik-Nubarov, N. A novel approach to a controlled opening of liposomes. Colloids Surf. B Biointerfaces 2020, 190, 110906. [Google Scholar] [CrossRef]
- Clark, S.T.; Arras, M.M.; Sarles, S.A.; Frymier, P.D. Modeling the saturation of detergent association in mixed liposome systems. Colloids Surf. B Biointerfaces 2021, 206, 111927. [Google Scholar] [CrossRef] [PubMed]
- Cressey, P.; Amrahli, M.; So, P.-W.; Gedroyc, W.; Wright, M.; Thanou, M. Image-guided thermosensitive liposomes for focused ultrasound enhanced co-delivery of carboplatin and SN-38 against triple negative breast cancer in mice. Biomaterials 2021, 271, 120758. [Google Scholar] [CrossRef]
- Chen, M.-H.; Chiang, B.-H. Modification of curcumin-loaded liposome with edible compounds to enhance ability of crossing blood brain barrier. Colloids Surf. A Physicochem. Eng. Asp. 2020, 599, 124862. [Google Scholar] [CrossRef]
- Romero-Arrieta, M.R.; Uria-Canseco, E.; Perez-Casas, S. Simultaneous encapsulation of hydrophilic and lipophilic molecules in liposomes of DSPC. Thermochim. Acta 2020, 687, 178462. [Google Scholar] [CrossRef]
- Yuan, Z.; Das, S.; Lazenby, R.A.; White, R.J.; Park, Y.C. Repetitive drug releases from light-activatable micron-sized liposomes. Colloids Surf. A: Physicochem. Eng. Asp. 2021, 625, 126778. [Google Scholar] [CrossRef] [PubMed]
- Vitor, M.T.; Bergami-Santos, P.C.; Zômpero, R.H.F.; Cruz, K.S.P.; Pinho, M.P.; Barbuto, J.A.M.; de la Torre, L.G. Cationic liposomes produced via ethanol injection method for dendritic cell therapy. J. Liposome Res. 2017, 27, 249–263. [Google Scholar] [CrossRef]
- Chaudhry, G.-E.-S.; Akim, A.; Sung, Y.Y.; Muhammad, T.S.T. Polymeric nanoparticles methods of preparation and drug release models: Effectiveness towards drug delivery systems. Res. J. Pharm. Technol. 2022, 15, 2883–2887. [Google Scholar] [CrossRef]
- Sala, M.; Miladi, K.; Agusti, G.; Elaissari, A.; Fessi, H. Preparation of liposomes: A comparative study between the double solvent displacement and the conventional ethanol injection—From laboratory scale to large scale. Colloids Surf. A Physicochem. Eng. Asp. 2017, 524, 71–78. [Google Scholar] [CrossRef]
- Shaker, S.; Gardouh, A.R.; Ghorab, M.M. Factors affecting liposomes particle size prepared by ethanol injection method. Res. Pharm. Sci. 2017, 12, 346. [Google Scholar] [CrossRef]
- Vemuri, S.; Rhodes, C. Preparation and characterization of liposomes as therapeutic delivery systems: A review. Pharm. Acta Helv. 1995, 70, 95–111. [Google Scholar] [CrossRef]
- Jiskoot, W.; Teerlink, T.; Beuvery, E.C.; Crommelin, D.J. Preparation of liposomes via detergent removal from mixed micelles by dilution. Pharm. Weekbl. 1986, 8, 259–265. [Google Scholar] [CrossRef]
- Milsmann, M.H.; Schwendener, R.A.; Weder, H.-G. The preparation of large single bilayer liposomes by a fast and controlled dialysis. Biochim. Biophys. Acta (BBA)-Biomembr. 1978, 512, 147–155. [Google Scholar] [CrossRef]
- Schwendener, R.; Asanger, M.; Weder, H. n-alkyl-glucosides as detergents for the preparation of highly homogeneous bilayer liposomes of variable sizes (60–240 nm φ) applying defined rates of detergent removal by dialysis. Biochem. Biophys. Res. Commun. 1981, 100, 1055–1062. [Google Scholar] [CrossRef]
- Enoch, H.G.; Strittmatter, P. Formation and properties of 1000-A-diameter, single-bilayer phospholipid vesicles. Proc. Natl. Acad. Sci. USA 1979, 76, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Ueno, M.; Tanford, C.; Reynolds, J.A. Phospholipid vesicle formation using nonionic detergents with low monomer solubility. Kinetic factors determine vesicle size and permeability. Biochemistry 1984, 23, 3070–3076. [Google Scholar] [CrossRef]
- Schurtenberger, P.; Mazer, N.; Waldvogel, S.; Känzig, W. Preparation of monodisperse vesicles with variable size by dilution of mixed micellar solutions of bile salt and phosphatidylcholine. Biochim. Biophys. Acta (BBA)-Biomembr. 1984, 775, 111–114. [Google Scholar] [CrossRef]
- Schubert, R. Liposome preparation by detergent removal. Methods Enzymol. 2003, 367, 46–70. [Google Scholar] [PubMed]
- Hossen, M.N.; Kajimoto, K.; Akita, H.; Hyodo, M.; Ishitsuka, T.; Harashima, H. Ligand-based targeted delivery of a peptide modified nanocarrier to endothelial cells in adipose tissue. J. Control. Release 2010, 147, 261–268. [Google Scholar] [CrossRef]
- Hossen, M.N.; Kajimoto, K.; Akita, H.; Hyodo, M.; Harashima, H. Vascular-targeted nanotherapy for obesity: Unexpected passive targeting mechanism to obese fat for the enhancement of active drug delivery. J. Control. Release 2012, 163, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Hossen, N.; Kajimoto, K.; Akita, H.; Hyodo, M.; Harashima, H. A comparative study between nanoparticle-targeted therapeutics and bioconjugates as obesity medication. J. Control. Release 2013, 171, 104–112. [Google Scholar] [CrossRef]
- Hossen, M.N.; Kajimoto, K.; Akita, H.; Hyodo, M.; Ishitsuka, T.; Harashima, H. Therapeutic assessment of cytochrome C for the prevention of obesity through endothelial cell-targeted nanoparticulate system. Mol. Ther. 2013, 21, 533–541. [Google Scholar] [CrossRef]
- Mahmood, S.; Mandal, U.K.; Chatterjee, B.; Taher, M. Advanced characterizations of nanoparticles for drug delivery: Investigating their properties through the techniques used in their evaluations. Nanotechnol. Rev. 2017, 6, 355–372. [Google Scholar] [CrossRef]
- Senn, A.; Pilet, P.-E. Electrophoretic mobility, zeta potential and surface charges of maize root protoplasts. Z. Pflanzenphysiol. 1981, 102, 19–32. [Google Scholar] [CrossRef]
- Zhao, Z.; Katai, H.; Higashi, K.; Ueda, K.; Kawakami, K.; Moribe, K. Cryo-TEM and AFM observation of the time-dependent evolution of amorphous probucol nanoparticles formed by the aqueous dispersion of ternary solid dispersions. Mol. Pharm. 2019, 16, 2184–2198. [Google Scholar] [CrossRef]
- Byrn, S.; Zografi, G.; Chen, X. Differential scanning calorimetry and thermogravimetric analysis. In Solid State Properties of Pharmaceutical Materials; Wiley: Hoboken, NJ, USA, 2017; pp. 124–141. [Google Scholar]
- Panwar, P.; Pandey, B.; Lakhera, P.; Singh, K. Preparation, characterization, and in vitro release study of albendazole-encapsulated nanosize liposomes. Int. J. Nanomed. 2010, 5, 101. [Google Scholar]
- Florence, A.T.; Jani, P.U. Novel oral drug formulations. Drug Saf. 1994, 10, 233–266. [Google Scholar] [CrossRef]
- Ashley, G.W.; Henise, J.; Reid, R.; Santi, D.V. Hydrogel drug delivery system with predictable and tunable drug release and degradation rates. Proc. Natl. Acad. Sci. USA 2013, 110, 2318–2323. [Google Scholar] [CrossRef]
- Larson, N.; Ghandehari, H. Polymeric conjugates for drug delivery. Chem. Mater. 2012, 24, 840–853. [Google Scholar] [CrossRef] [PubMed]
- Patil, J.P. A review on polymer drug conjugate-what, why and how? IJPSR 2015, 6, 4611–4621. [Google Scholar]
- Maeda, H.; Wu, J.; Sawa, T.; Matsumura, Y.; Hori, K. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: A review. J. Control. Release 2000, 65, 271–284. [Google Scholar] [CrossRef]
- Islam, F.; Mitra, S.; Emran, T.B.; Khan, Z.; Nath, N.; Das, R.; Sharma, R.; Awadh, A.A.A.; Park, M.N.; Kim, B. Natural Small Molecules in Gastrointestinal Tract and Associated Cancers: Molecular Insights and Targeted Therapies. Molecules 2022, 27, 5686. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, T.M.; Aimetti, A.A.; Kim, E.; Yesilyurt, V.; Langer, R. Synthesis and characterization of a library of in-situ curing, nonswelling ethoxylated polyol thiol-ene hydrogels for tailorable macromolecule delivery. Adv. Mater. 2015, 27, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Purcell, B.P.; Lobb, D.; Charati, M.B.; Dorsey, S.M.; Wade, R.J.; Zellars, K.N.; Doviak, H.; Pettaway, S.; Logdon, C.B.; Shuman, J.A. Injectable and bioresponsive hydrogels for on-demand matrix metalloproteinase inhibition. Nat. Mater. 2014, 13, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Hong, W.; Zhao, X.; Zhou, J.; Suo, Z. A theory of coupled diffusion and large deformation in polymeric gels. J. Mech. Phys. Solids 2008, 56, 1779–1793. [Google Scholar] [CrossRef]
- Huebsch, N.; Kearney, C.J.; Zhao, X.; Kim, J.; Cezar, C.A.; Suo, Z.; Mooney, D.J. Ultrasound-triggered disruption and self-healing of reversibly cross-linked hydrogels for drug delivery and enhanced chemotherapy. Proc. Natl. Acad. Sci. USA 2014, 111, 9762–9767. [Google Scholar] [CrossRef]
- Wei-Ze, L.; Mei-Rong, H.; Jian-Ping, Z.; Yong-Qiang, Z.; Bao-Hua, H.; Ting, L.; Yong, Z. Super-short solid silicon microneedles for transdermal drug delivery applications. Int. J. Pharm. 2010, 389, 122–129. [Google Scholar] [CrossRef]
- Li, S.; Li, W.; Prausnitz, M. Individually coated microneedles for co-delivery of multiple compounds with different properties. Drug Deliv. Transl. Res. 2018, 8, 1043–1052. [Google Scholar] [CrossRef]
- Agrawal, S.; Gandhi, S.N.; Gurjar, P.; Saraswathy, N. Microneedles: An advancement to transdermal drug delivery system approach. J. Appl. Pharm. Sci. 2020, 10, 149–159. [Google Scholar]
- Kurz, A.; Farlow, M.; Lefevre, G. Pharmacokinetics of a novel transdermal rivastigmine patch for the treatment of Alzheimer’s disease: A review. Int. J. Clin. Pract. 2009, 63, 799–805. [Google Scholar] [CrossRef]
- Suh, J.; Choy, K.-L.; Lai, S.K.; Suk, J.S.; Tang, B.C.; Prabhu, S.; Hanes, J. PEGylation of nanoparticles improves their cytoplasmic transport. Int. J. Nanomed. 2007, 2, 735. [Google Scholar]
- Di Mascolo, D.; Lyon, C.J.; Aryal, S.; Ramirez, M.R.; Wang, J.; Candeloro, P.; Guindani, M.; Hsueh, W.A.; Decuzzi, P. Rosiglitazone-loaded nanospheres for modulating macrophage-specific inflammation in obesity. J. Control. Release 2013, 170, 460–468. [Google Scholar] [CrossRef]
- Cao, Y. Angiogenesis modulates adipogenesis and obesity. J. Clin. Investig. 2007, 117, 2362–2368. [Google Scholar] [CrossRef]
- Cao, Y. Adipose tissue angiogenesis as a therapeutic target for obesity and metabolic diseases. Nat. Rev. Drug Discov. 2010, 9, 107–115. [Google Scholar] [CrossRef]
- Xue, Y.; Xu, X.; Zhang, X.Q.; Farokhzad, O.C.; Langer, R. Preventing diet-induced obesity in mice by adipose tissue transformation and angiogenesis using targeted nanoparticles. Proc. Natl. Acad. Sci. USA 2016, 113, 5552–5557. [Google Scholar] [CrossRef] [PubMed]
- Marrache, S.; Dhar, S. Engineering of blended nanoparticle platform for delivery of mitochondria-acting therapeutics. Proc. Natl. Acad. Sci. USA 2012, 109, 16288–16293. [Google Scholar] [CrossRef]
- Jiang, C.; Cano-Vega, M.A.; Yue, F.; Kuang, L.; Narayanan, N.; Uzunalli, G.; Merkel, M.P.; Kuang, S.; Deng, M. Dibenzazepine-Loaded Nanoparticles Induce Local Browning of White Adipose Tissue to Counteract Obesity. Mol. Ther. 2017, 25, 1718–1729. [Google Scholar] [CrossRef]
- Vashisth, P.; Srivastava, A.K.; Nagar, H.; Raghuwanshi, N.; Sharan, S.; Nikhil, K.; Pruthi, P.A.; Singh, R.P.; Roy, P.; Pruthi, V. Drug functionalized microbial polysaccharide based nanofibers as transdermal substitute. Nanomedicine 2016, 12, 1375–1385. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, T. Curcumin as a functional food-derived factor: Degradation products, metabolites, bioactivity, and future perspectives. Food Funct. 2018, 9, 705–714. [Google Scholar] [CrossRef] [PubMed]
- de Jesus Felismino, C.; Helal-Neto, E.; Portilho, F.L.; Pinto, S.R.; Sancenon, F.; Martínez-Máñez, R.; de Assis Ferreira, A.; da Silva, S.V.; Barja-Fidalgo, T.C.; Santos-Oliveira, R. Effect of obesity on biodistribution of nanoparticles. J. Control. Release 2018, 281, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Sahuri-Arisoylu, M.; Brody, L.; Parkinson, J.; Parkes, H.; Navaratnam, N.; Miller, A.D.; Thomas, E.; Frost, G.; Bell, J. Reprogramming of hepatic fat accumulation and ’browning’ of adipose tissue by the short-chain fatty acid acetate. Int. J. Obes. 2016, 40, 955–963. [Google Scholar] [CrossRef]
- Hayashi, Y.; Suemitsu, E.; Kajimoto, K.; Sato, Y.; Akhter, A.; Sakurai, Y.; Hatakeyama, H.; Hyodo, M.; Kaji, N.; Baba, Y. Hepatic monoacylglycerol O-acyltransferase 1 as a promising therapeutic target for steatosis, obesity, and type 2 diabetes. Mol. Ther. -Nucleic Acids 2014, 3, e154. [Google Scholar] [CrossRef] [PubMed]
- Yong, S.-B.; Song, Y.; Kim, Y.-H. Visceral adipose tissue macrophage-targeted TACE silencing to treat obesity-induced type 2 diabetes. Biomaterials 2017, 148, 81–89. [Google Scholar] [CrossRef]
- El-Gharbawy, R.M.; Emara, A.M.; Abu-Risha, S.E.-S. Zinc oxide nanoparticles and a standard antidiabetic drug restore the function and structure of beta cells in Type-2 diabetes. Biomed. Pharmacother. 2016, 84, 810–820. [Google Scholar] [CrossRef]
- Segura-Ibarra, V.; Cara, F.E.; Wu, S.; Iruegas-Nunez, D.A.; Wang, S.; Ferrari, M.; Ziemys, A.; Valderrabano, M.; Blanco, E. Nanoparticles administered intrapericardially enhance payload myocardial distribution and retention. J. Control. Release 2017, 262, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Chou, H.-S.; Larsson, M.; Hsiao, M.-H.; Chen, Y.-C.; Röding, M.; Nydén, M.; Liu, D.-M. Injectable insulin-lysozyme-loaded nanogels with enzymatically-controlled degradation and release for basal insulin treatment: In vitro characterization and in vivo observation. J. Control. Release 2016, 224, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Nurunnabi, M.; Lee, S.-A.; Revuri, V.; Hwang, Y.H.; Kang, S.H.; Lee, M.; Cho, S.; Cho, K.J.; Byun, Y.; Bae, Y.H. Oral delivery of a therapeutic gene encoding glucagon-like peptide 1 to treat high fat diet-induced diabetes. J. Control. Release 2017, 268, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Su, F.-Y.; Lin, K.-J.; Sonaje, K.; Wey, S.-P.; Yen, T.-C.; Ho, Y.-C.; Panda, N.; Chuang, E.-Y.; Maiti, B.; Sung, H.-W. Protease inhibition and absorption enhancement by functional nanoparticles for effective oral insulin delivery. Biomaterials 2012, 33, 2801–2811. [Google Scholar] [CrossRef] [PubMed]
- Gubernator, J. Active methods of drug loading into liposomes: Recent strategies for stable drug entrapment and increased in vivo activity. Expert Opin. Drug Deliv. 2011, 8, 565–580. [Google Scholar] [CrossRef]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef]
- Fenske, D.B.; Cullis, P.R. Liposomal nanomedicines. Expert Opin. Drug Deliv. 2008, 5, 25–44. [Google Scholar] [CrossRef]
- Nsairat, H.; Khater, D.; Sayed, U.; Odeh, F.; Al Bawab, A.; Alshaer, W. Liposomes: Structure, composition, types, and clinical applications. Heliyon 2022, 8, e09394. [Google Scholar] [CrossRef]
- Alshaer, W.; Zraikat, M.; Amer, A.; Nsairat, H.; Lafi, Z.; Alqudah, D.A.; Al Qadi, E.; Alsheleh, T.; Odeh, F.; Alkaraki, A. Encapsulation of echinomycin in cyclodextrin inclusion complexes into liposomes: In vitro anti-proliferative and anti-invasive activity in glioblastoma. RSC Adv. 2019, 9, 30976–30988. [Google Scholar] [CrossRef]
- Nkanga, C.I.; Bapolisi, A.M.; Okafor, N.I.; Krause, R.W.M. General perception of liposomes: Formation, manufacturing and applications. In Liposomes—Advances and Perspectives; IntechOpen: Rijeka, Croatia, 2019. [Google Scholar]
- Pattni, B.S.; Chupin, V.V.; Torchilin, V.P. New developments in liposomal drug delivery. Chem. Rev. 2015, 115, 10938–10966. [Google Scholar] [CrossRef]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol. Pharm. 2010, 67, 217–223. [Google Scholar]
- Liu, X.; Powell, C.A.; Wang, X. Forward single-cell sequencing into clinical application: Understanding of cancer microenvironment at single-cell solution. Clin. Transl. Med. 2022, 12, e782. [Google Scholar] [CrossRef]
- Gelesis, I. inVentiv Health Clinical, Gelesis Glycemic Index Study. 2017. Available online: https://ClinicalTrials.gov/show/NCT03124134 (accessed on 25 February 2023).
- Neurovalens Ltd.; S.D. University of California; University of Ulster, Exploristics; Compliance Solutions Ltd. Vestibular Stimulation to Trigger Adipose Loss (VeSTAL) Clinical Trial. 2019. Available online: https://ClinicalTrials.gov/show/NCT03640286 (accessed on 25 February 2023).
- Liposomal Amphotericin B (AmBisome) Pharmacokinetics Given as a Single Intravenous Dose to Obese Patients (ASPEN), (n.d.). Available online: https://ClinicalTrials.gov/show/NCT02320604 (accessed on 25 February 2023).
- Transversus Abdominis Plane (TAP) Block Using Liposomal Bupivacaine in Metabolic and Bariatric Surgery Patients, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT05537883 (accessed on 25 February 2023).
- Pain Control in Bariatric Patients: EXPAREL(R) vs. the On-Q(R) Pain Ball, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT02142829 (accessed on 25 February 2023).
- Effects of Glutathione (an Antioxidant) and N-Acetylcysteine on Inflammation, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT01550432 (accessed on 25 February 2023).
- The Effect of Curcumin on the Development of Prednisolone-induced Hepatic Insulin Resistance, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT04315350 (accessed on 25 February 2023).
- Validation of Circulating Endothelial Cells and Microparticles in Youth, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT01508598 (accessed on 25 February 2023).
- Embolization of Arterial Gastric Supply in Obesity, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT04207424 (accessed on 25 February 2023).
- Bariatric Embolization Trial for the Obese Nonsurgical, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT03601273 (accessed on 25 February 2023).
- TIFACT Study—Tissue Factor Expression by Adipose Tissue in Extremely Obese Subjects, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT00379704 (accessed on 25 February 2023).
- Metabolic Effects of Duodenal Jejunal Bypass Liner for Type 2 Diabetes Mellitus, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT02800668 (accessed on 25 February 2023).
- Beetroot Supplementation in Women Enjoying Exercise Together, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT04370756 (accessed on 25 February 2023).
- Homocysteine After Laparoscopic Roux-enY Gastric Bypass, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT03489538 (accessed on 25 February 2023).
- Efficacy of Oral Vitamin D Supplementation in Adolescents and Young Adults, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT04377386 (accessed on 25 February 2023).
- Emory University, Thrasher Research Fund, Insulin Delivery Using Microneedles in Type 1 Diabetes. 2008. Available online: https://ClinicalTrials.gov/show/NCT00837512 (accessed on 25 February 2023).
- Emory University, Glucose Measurement Using Microneedle Patches. 2017. Available online: https://ClinicalTrials.gov/show/NCT02682056 (accessed on 25 February 2023).
- Cardiff University, Enhanced Epidermal Antigen Specific Immunotherapy Trial-1. 2016. Available online: https://ClinicalTrials.gov/show/NCT02837094 (accessed on 25 February 2023).
- Massachusetts General Hospital, Pharmacokinetic Comparison of Intradermal Versus Sub-cutaneous Insulin and Glucagon Delivery in Type 1 Diabetes. 2012. Available online: https://ClinicalTrials.gov/show/NCT01684956 (accessed on 25 February 2023).
- Becton, D. Company, Multi-day (3) In-Patient Evaluation of Intradermal Versus Subcutaneous Basal and Bolus Insulin Infusion. 2012. Available online: https://ClinicalTrials.gov/show/NCT01557907 (accessed on 25 February 2023).
- Becton, D. Company, Pharmacokinetics/Dynamics of Basal (Continuous) Insulin Infusion Administered Either Intradermally or Subcutaneously. 2010. Available online: https://ClinicalTrials.gov/show/NCT01061216 (accessed on 25 February 2023).
- Biomedical, I.C. Suprachoroidal Injection of CLS-TA Alone or with Aflibercept in Subjects with Diabetic Macular Edema. 2016. Available online: https://ClinicalTrials.gov/show/NCT02949024 (accessed on 25 February 2023).
- Imaging Inflammation in Autoimmune Diabetes, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT00585936 (accessed on 25 February 2023).
- Capsaicin Nanoparticle in Patient with Painful Diabetic Neuropathy, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT01125215 (accessed on 25 February 2023).
- Host-Microbiota-Environment Interactions, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT05176795 (accessed on 25 February 2023).
- Clinical Application of Mesenchymal Stem Cells Seeded in Chitosan Scaffold for Diabetic Foot Ulcers, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT03259217 (accessed on 25 February 2023).
- The Role of Eicosanoids in the Cardiovascular Actions of Inhaled Nanoparticles, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT03659864 (accessed on 25 February 2023).
- The Accuracy and Safety of Coronary Artery Contrast-enhanced Magnetic Resonance Imaging with Polysaccharide Superparamagnetic Iron Oxide Nanoparticle, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT05032937 (accessed on 25 February 2023).
- Prevention of Restenosis Following Revascularization, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT00518284 (accessed on 25 February 2023).
- Use of Nanoparticle Paclitaxel (ABI-007) for the Prevention of In-Stent Restenosis, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT00124943 (accessed on 25 February 2023).
- Treatment of Patients with Atherosclerotic Disease with Methotrexate-associated to LDL Like Nanoparticles, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT04616872 (accessed on 25 February 2023).
- Treatment of Patients with Atherosclerotic Disease with Paclitaxel-associated to LDL Like Nanoparticles, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT04148833 (accessed on 25 February 2023).
- Transforming Nanoparticle Dressing for Management of Chronic Venous Ulcers, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT04793074 (accessed on 25 February 2023).
- Magnetic Nanoparticles System in Acute Coronary Syndrome, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT02226523 (accessed on 25 February 2023).
- Plasmonic Nanophotothermal Therapy of Atherosclerosis, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT01270139 (accessed on 25 February 2023).
- Paclitaxel Albumin-Stabilized Nanoparticle Formulation in Treating Patients with Relapsed or Refractory Multiple Myeloma, (n.d.). Available online: https://ClinicalTrials.gov/show/NCT01646762 (accessed on 25 February 2023).
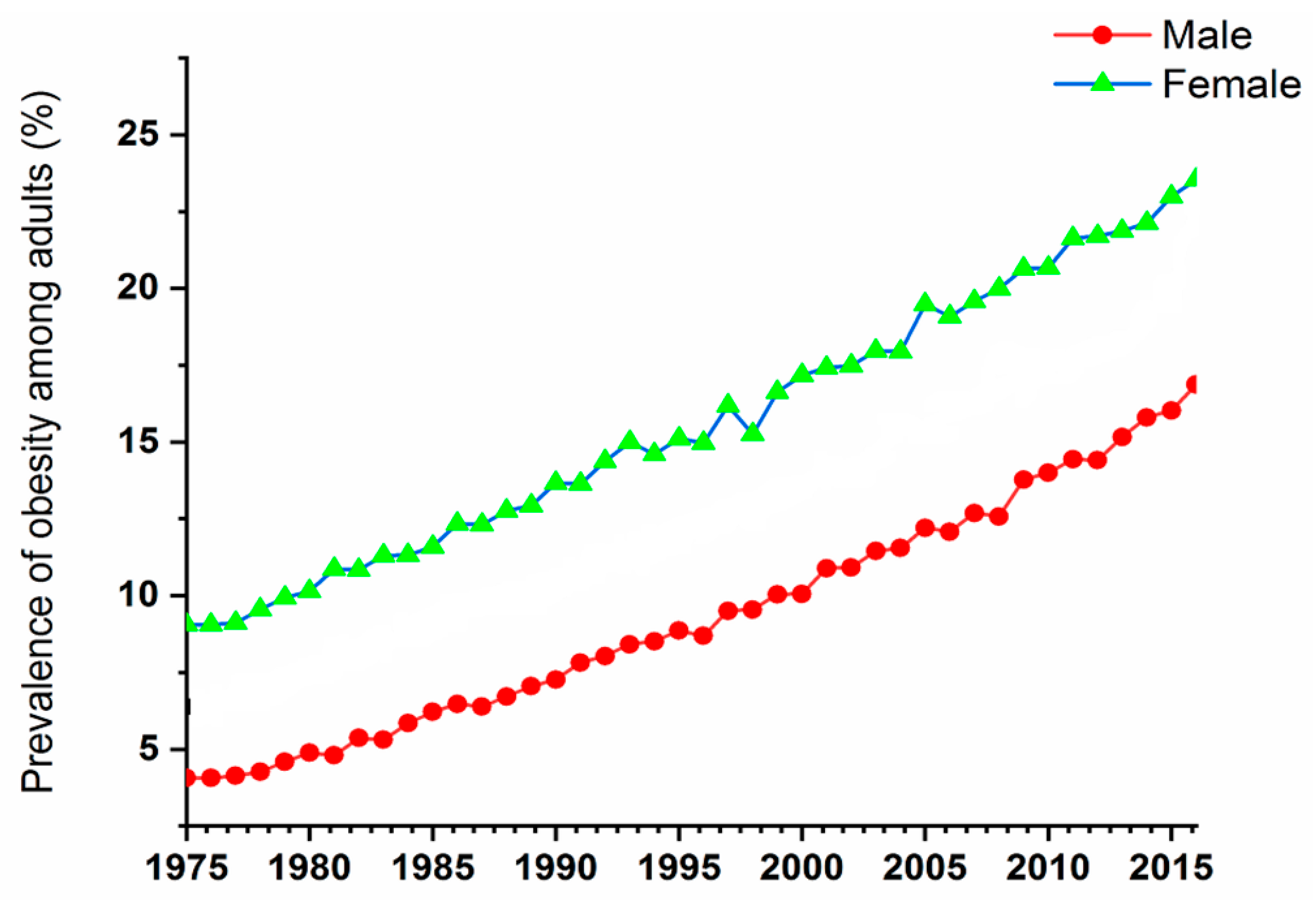
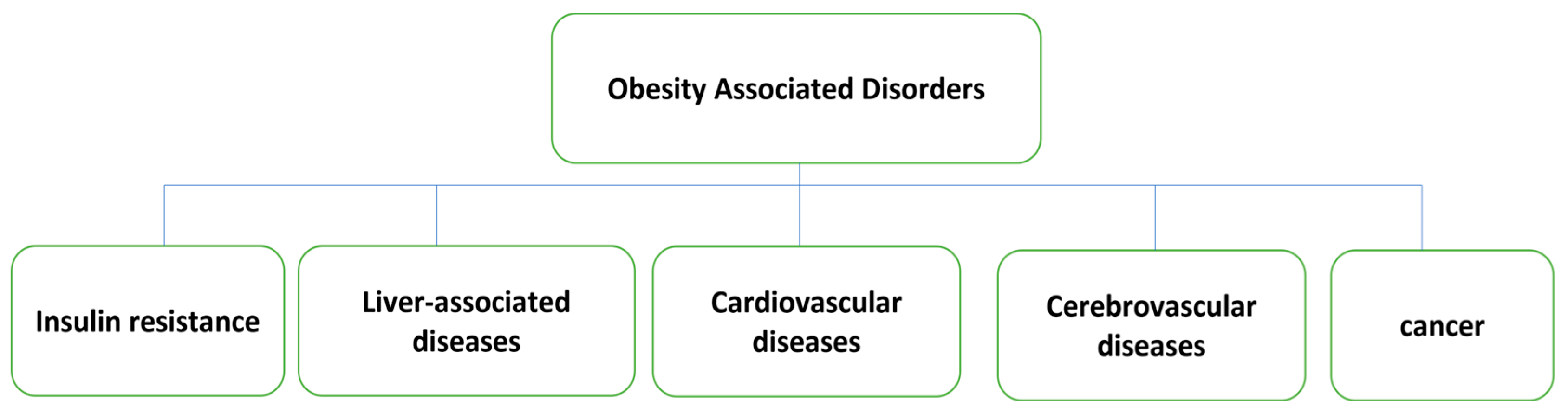
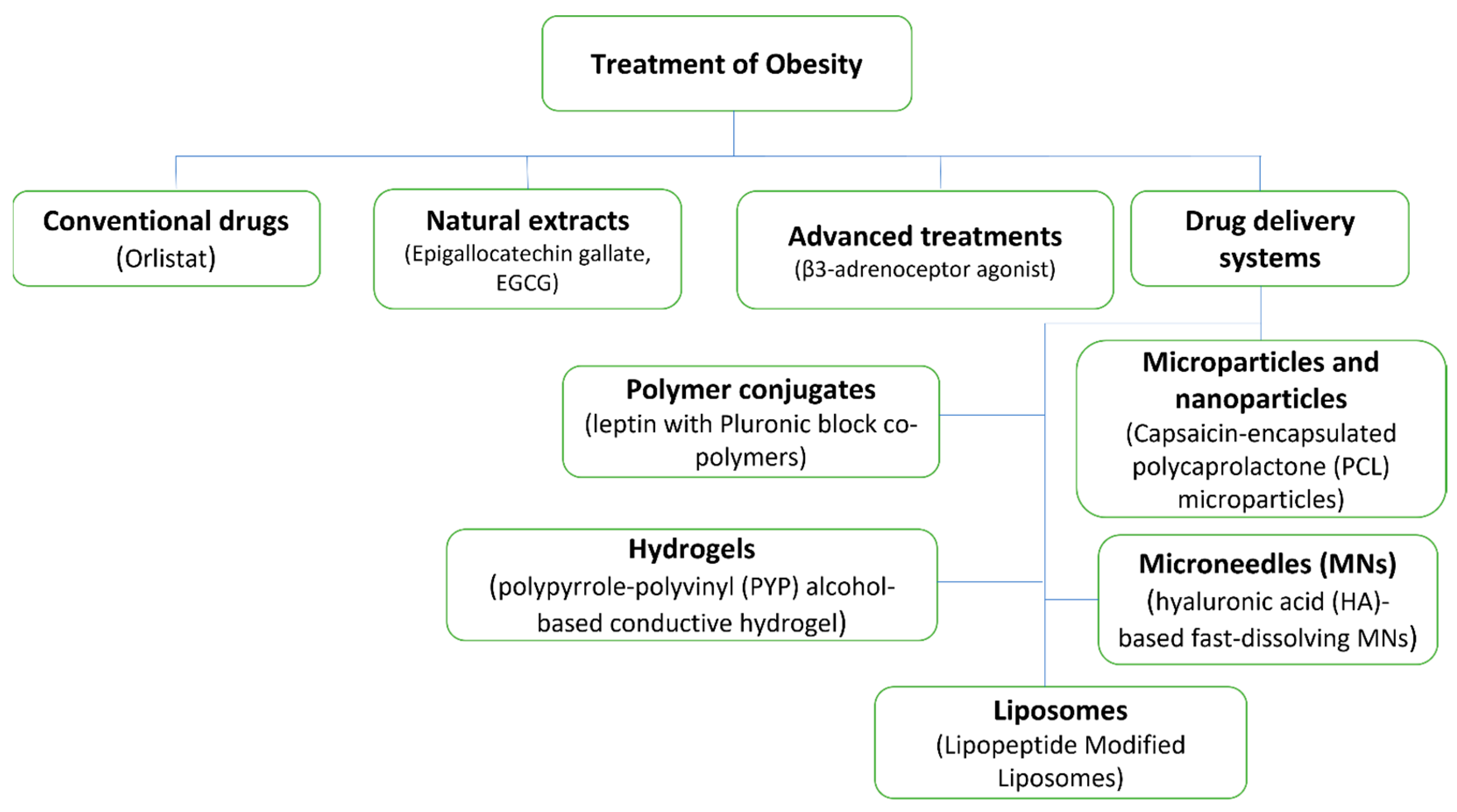
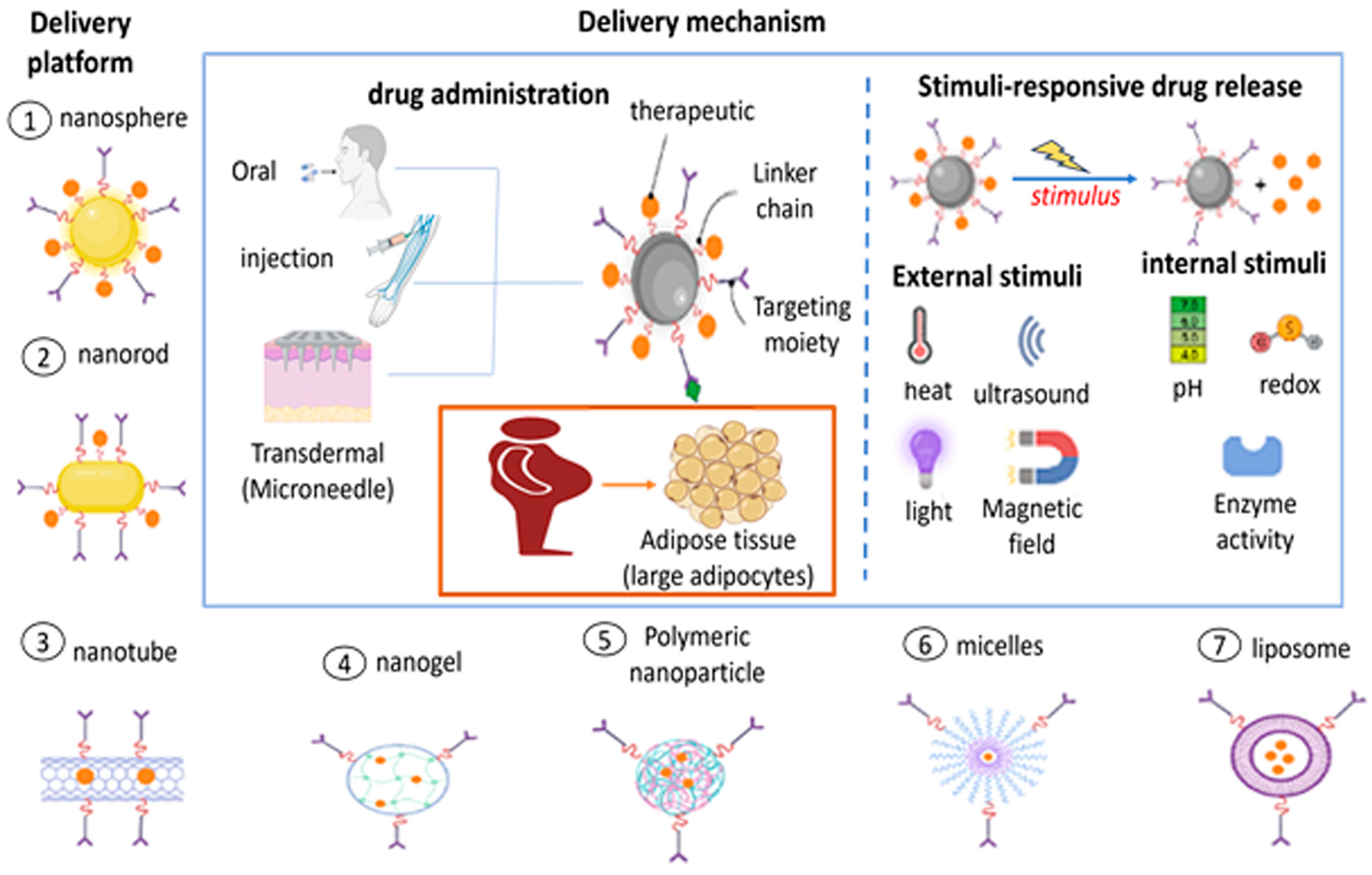

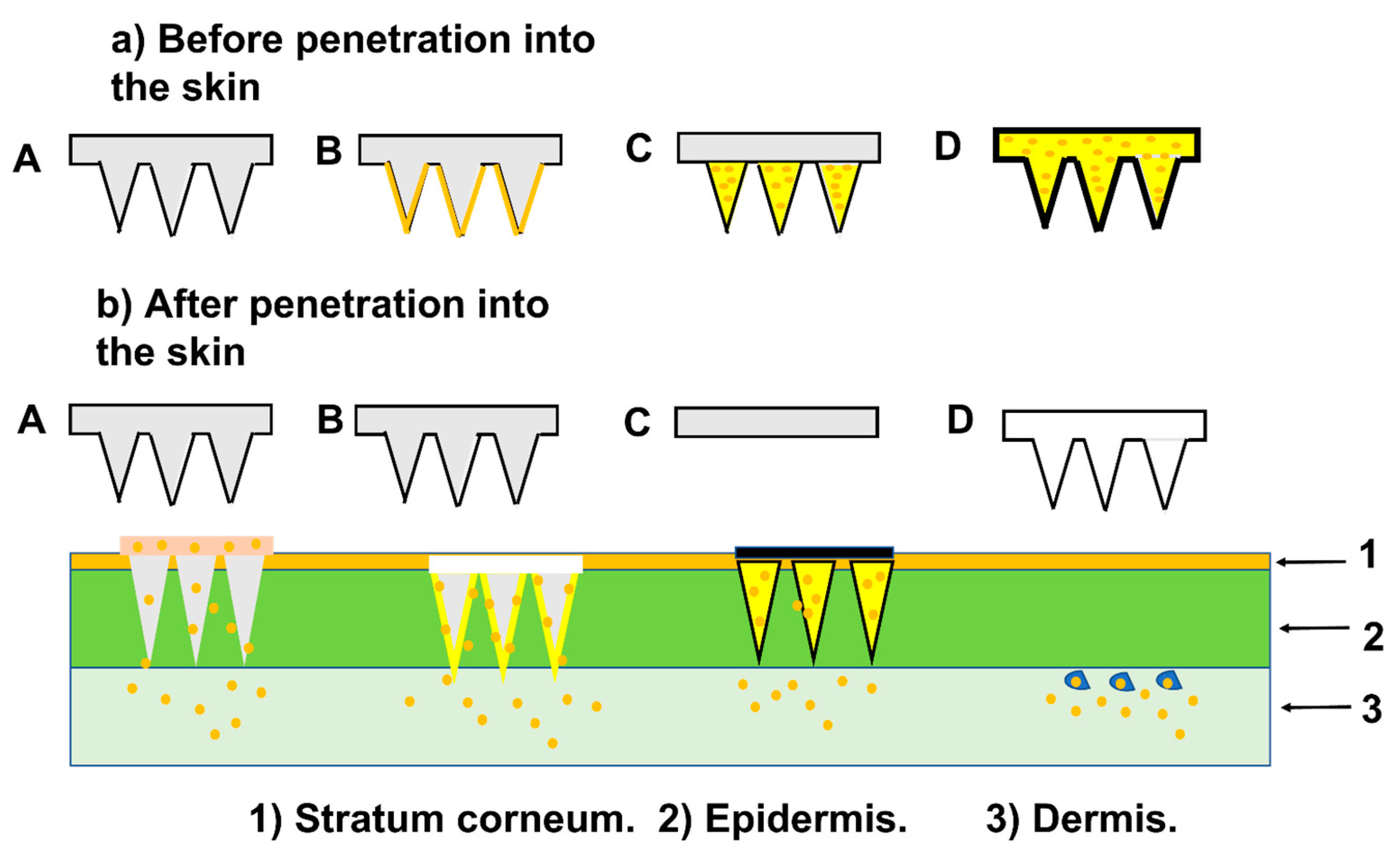
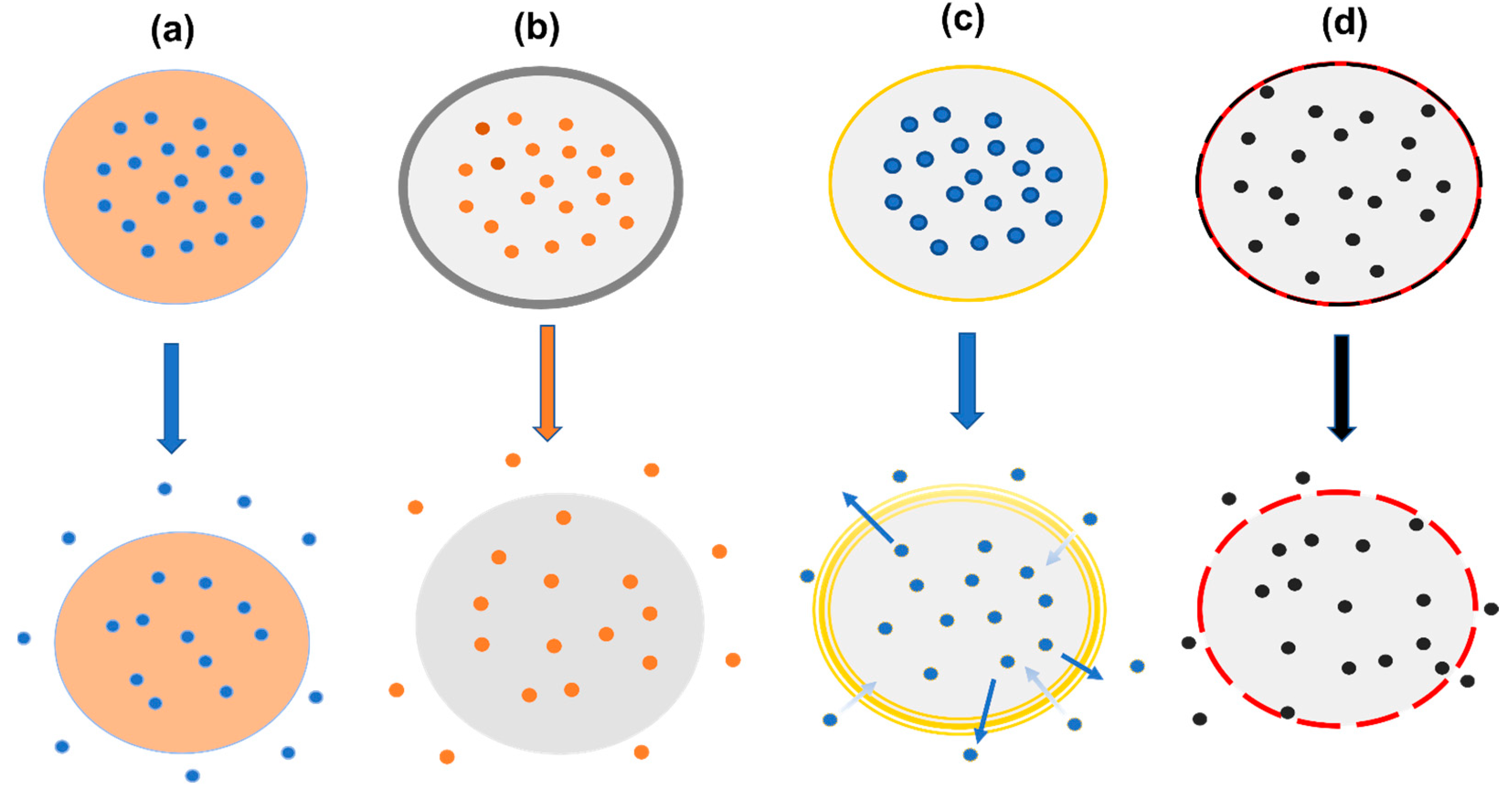
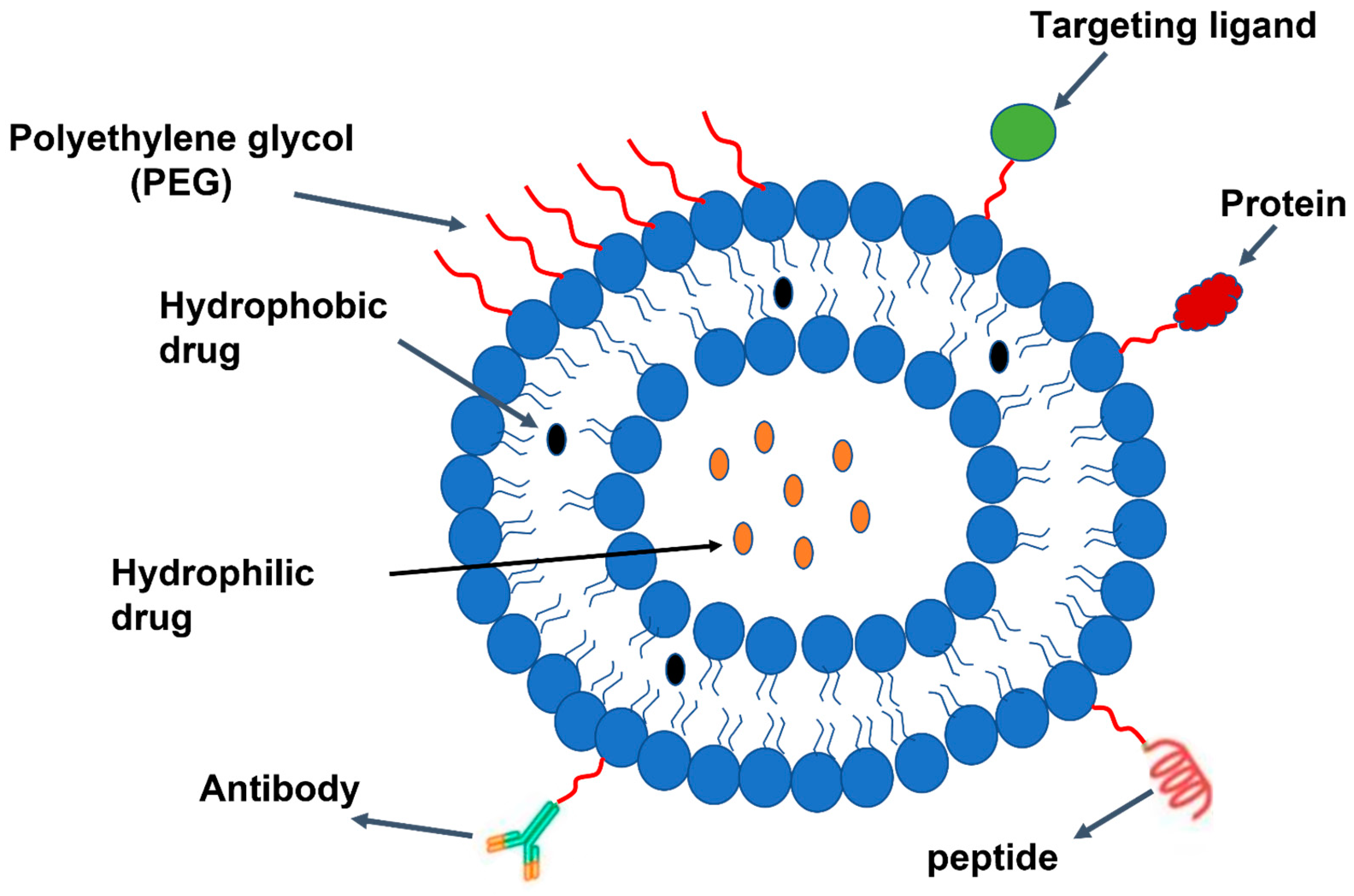
| Characterization Technique | Description | Characteristics of MNs | Reference |
|---|---|---|---|
| Axial force | apply force to the needle’s tip in a vertical direction | determine the failure force of the needle tip | [242] |
| Transverse force | apply force into the needle base in parallel direction | determine the failure force of the needle base | [243] |
| Insertion test | apply the needles into rat, pig, or human skin | determine the actual force on skin and check the ability to release the drug | [85] |
| Liposome Characteristics | Characterization Technique | References |
|---|---|---|
| Average particle | Dynamic light scattering (DLS) and microscope technology: scanning and transmission electron microscopy (SEM/TEM), cryogenic TEM (Cryo-TEM), and atomic force microscopy (AFM) | [288] |
| Zeta potential/surface charge | Electrophoretic mobility, DLS | [289] |
| Particle shape/morphology | TEM, Cryo-TEM, and AFM | [290] |
| Lamellarity | Cryo-TEM and 31P-NMR | [290] |
| Phase behaviour | X-ray diffraction (XRD), differential scanning calorimetry (DSC), and thermogravimetric analysis (TGA) | [291] |
| Encapsulation efficiency/drug release | Centrifugation, dialysis followed by drug content determination using chromatographic and/or spectrophotometric methods | [292] |
| Delivery Approach | Description | Type of MNs | Reference |
|---|---|---|---|
| Poke and patch | Drug releases through micropores generated by MNs | Solid MNs | [303] |
| Coat and poke | Detachment of coating from the MN | Drug-coated MN | [304] |
| Poke and release | Drug diffuses and dissolves through the pores | Dissolving MN | [305] |
| Poke and flow | Drug flows out through the bore | Hollow MN | [306] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashour, M.M.; Mabrouk, M.; Aboelnasr, M.A.; Beherei, H.H.; Tohamy, K.M.; Das, D.B. Anti-Obesity Drug Delivery Systems: Recent Progress and Challenges. Pharmaceutics 2023, 15, 2635. https://doi.org/10.3390/pharmaceutics15112635
Ashour MM, Mabrouk M, Aboelnasr MA, Beherei HH, Tohamy KM, Das DB. Anti-Obesity Drug Delivery Systems: Recent Progress and Challenges. Pharmaceutics. 2023; 15(11):2635. https://doi.org/10.3390/pharmaceutics15112635
Chicago/Turabian StyleAshour, Mohamed M., Mostafa Mabrouk, Mohamed A. Aboelnasr, Hanan H. Beherei, Khairy M. Tohamy, and Diganta B. Das. 2023. "Anti-Obesity Drug Delivery Systems: Recent Progress and Challenges" Pharmaceutics 15, no. 11: 2635. https://doi.org/10.3390/pharmaceutics15112635
APA StyleAshour, M. M., Mabrouk, M., Aboelnasr, M. A., Beherei, H. H., Tohamy, K. M., & Das, D. B. (2023). Anti-Obesity Drug Delivery Systems: Recent Progress and Challenges. Pharmaceutics, 15(11), 2635. https://doi.org/10.3390/pharmaceutics15112635








