Tadalafil-Loaded Self-Nanoemulsifying Chewable Tablets for Improved Bioavailability: Design, In Vitro, and In Vivo Testing
Abstract
:1. Introduction
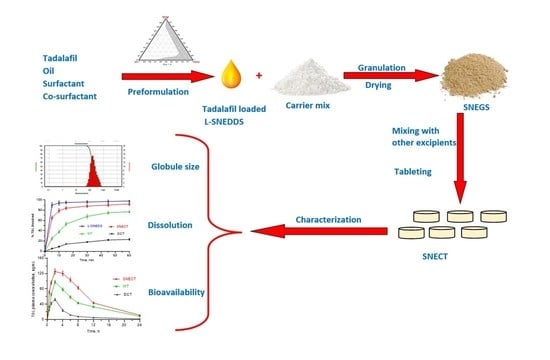
2. Methodology
2.1. Materials
2.2. TDL Quantification
2.3. Solubility Studies
2.4. Screening of Surfactants and Cosurfactants
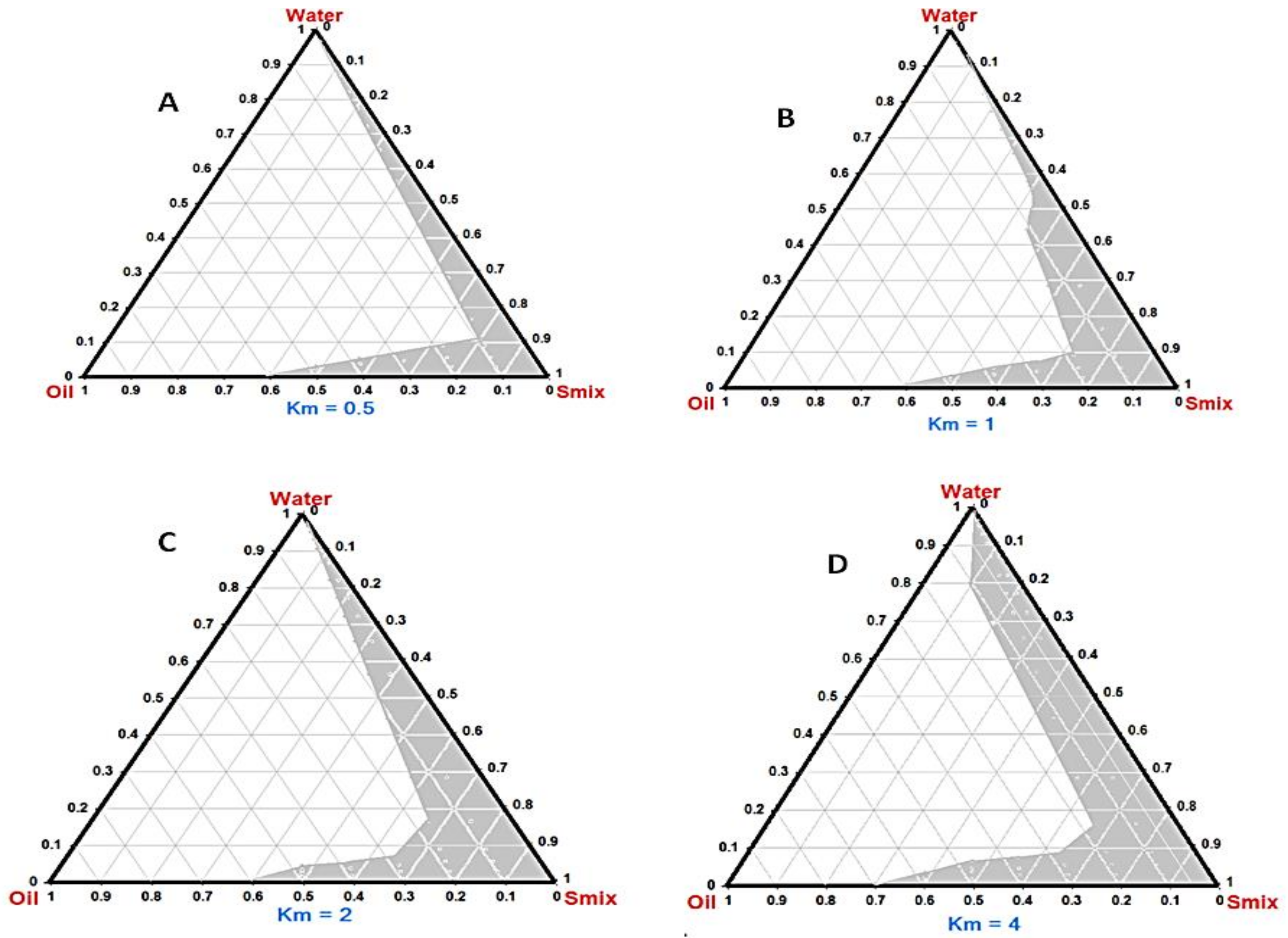
2.5. Construction of Phase Diagrams
2.6. Preparation and Characterization of TDL L-SNEDDS
2.6.1. Dispersibility and Transmittance
2.6.2. Robustness to Dilution
2.6.3. Droplet Size, Polydispersity Index, and Zeta Potential
2.6.4. Thermodynamic Stability Studies
2.7. TDL-Loaded Self-Nanoemulsifying Granules (TDL-SNEG)
2.7.1. Reconstitution Potential
2.7.2. Micromeritic Properties
Angle of Repose
2.7.3. Solid State Characterization
2.8. Tablet Formulations
2.8.1. Tablets Characterization
2.8.2. Dissolution Study
2.8.3. Stability Tests
Stability in Simulated GI Fluids
Dilution Stability in Simulated GI Fluids
Accelerated Stability Tests
2.8.4. Oral Bioavailability Study
Animals and Samples Collection
Processing and Quantification
Pharmacokinetic Analysis
3. Results and Discussion
3.1. Solubility Study
3.2. Phase Diagram
3.3. Tadalafil-Loaded Liquid Self-Nanoemulsifying Delivery Systems (TDL L-SNEDDS)
3.4. Tadalafil-Loaded Self-Nanoemulsifying Granules (TDL-SNEG)
3.5. Tadalafil-Loaded Self-Nanoemulsifying Chewable Tablets (TDL-SNECT)
3.5.1. Characterization and Reconstitution Potential
3.5.2. In Vitro Dissolution
3.5.3. Stability Study
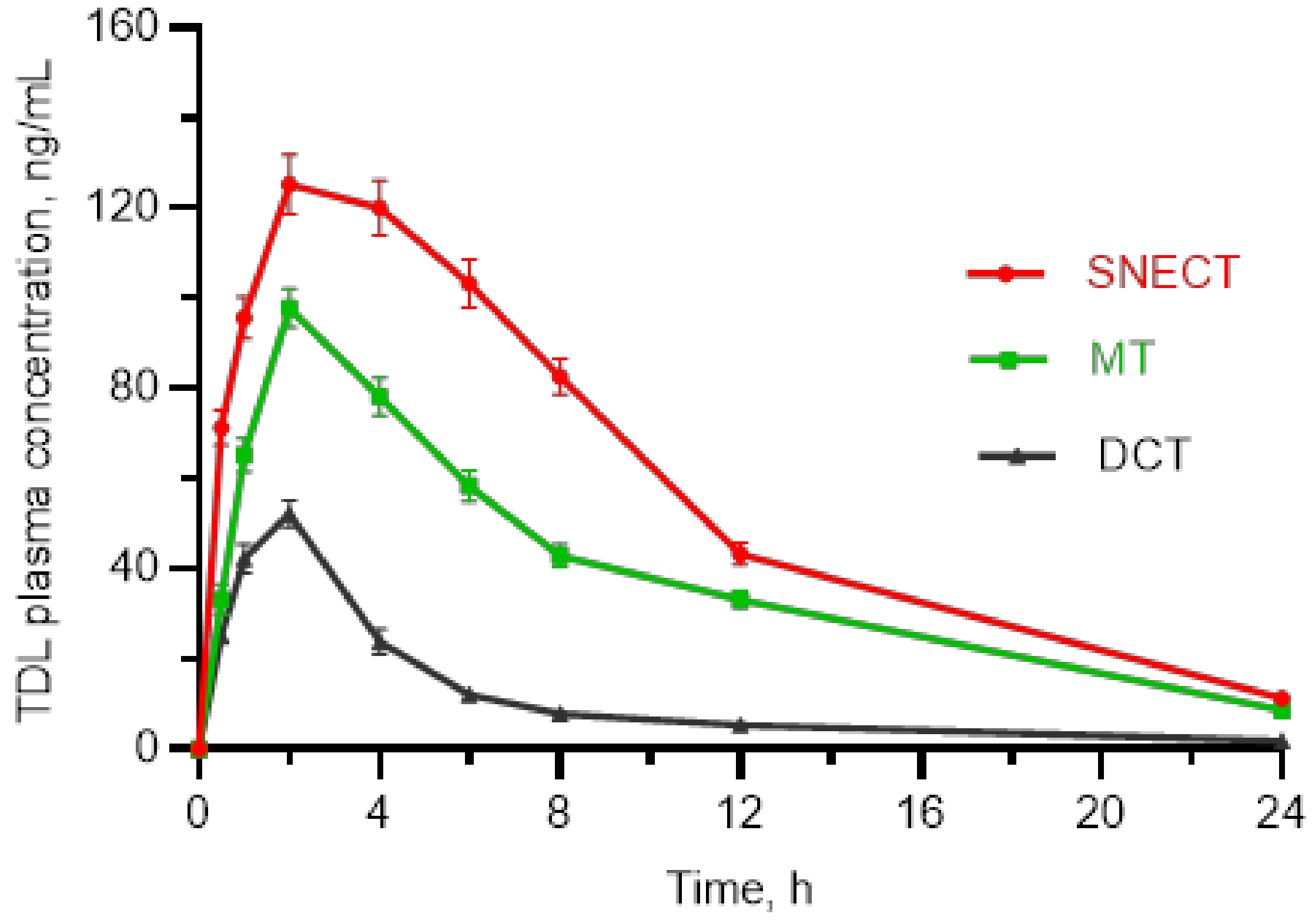
3.5.4. Bioavailability Study
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bolat, M.S.; Akdeniz, E.; Asci, R.; Erdemir, F.; Cinar, O.; Tomak, L. Ureterorenoscopy with stenting and its effect on male sexual function: A controlled randomised prospective study. Andrologia 2017, 49, 23. [Google Scholar] [CrossRef] [PubMed]
- Shamloul, R.; Ghanem, H. Erectile dysfunction. Lancet 2013, 381, 153–165. [Google Scholar] [CrossRef]
- Dong, J.-Y.; Zhang, Y.-H.; Qin, L.-Q. Erectile dysfunction and risk of cardiovascular disease: Meta-analysis of prospective cohort studies. J. Am. Coll. Cardiol. 2011, 58, 1378–1385. [Google Scholar] [CrossRef] [PubMed]
- Velurajah, R.; Brunckhorst, O.; Waqar, M.; McMullen, I.; Ahmed, K. Erectile dysfunction in patients with anxiety disorders: A systematic review. Int. J. Impot. Res. 2022, 34, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Albersen, M.; Linsen, L.; Tinel, H.; Sandner, P.; Van Renterghem, K. Synergistic effects of bay 60-4552 and vardenafil on relaxation of corpus cavernosum tissue of patients with erectile dysfunction and clinical phosphodiesterase type 5 inhibitor failure. J. Sex. Med. 2013, 10, 1268–1277. [Google Scholar] [CrossRef] [PubMed]
- Bella, A.J.; Brock, G.B. Tadalafil in the treatment of erectile dysfunction. Curr. Urol. Rep. 2003, 4, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.-S.; Cho, C.-W. Transdermal delivery of tadalafil using a novel formulation. Drug Deliv. 2016, 23, 1571–1577. [Google Scholar] [CrossRef]
- Carson, C.; Shabsigh, R.; Segal, S.; Murphy, A.; Fredlund, P. Efficacy, safety, and treatment satisfaction of tadalafil versus placebo in patients with erectile dysfunction evaluated at tertiary-care academic centers. Urology 2005, 65, 353–359. [Google Scholar] [CrossRef]
- Coward, R.M.; Carson, C.C. Tadalafil in the treatment of erectile dysfunction. Ther. Clin. Risk Manag. 2008, 4, 1315–1330. [Google Scholar] [CrossRef]
- Mobarak, D.; Salah, S.; Ghorab, M. Improvement of dissolution of a class ii poorly water-soluble drug, by developing a five-component self-nanoemulsifying drug delivery system. J. Drug Deliv. Sci. Technol. 2019, 50, 99–106. [Google Scholar] [CrossRef]
- Badr-Eldin, S.M.; Elkheshen, S.A.; Ghorab, M.M. Improving tadalafil dissolution via surfactant-enriched tablets approach: Statistical optimization, characterization, and pharmacokinetic assessment. J. Drug Deliv. Sci. Technol. 2017, 41, 197–205. [Google Scholar] [CrossRef]
- Fitria, A.; Hanifah, S.; Chabib, L.; Uno, A.M.; Munawwarah, H.; Atsil, N.; Pohara, H.A.; Weuanggi, D.A.; Syukri, Y. Design and characterization of propolis extract loaded self-nano emulsifying drug delivery system as immunostimulant. SJP 2021, 29, 625–634. [Google Scholar] [CrossRef]
- Buya, A.B.; Beloqui, A.; Memvanga, P.B.; Préat, V. Self-nano-emulsifying drug-delivery systems: From the development to the current applications and challenges in oral drug delivery. Pharmaceutics 2020, 12, 1194. [Google Scholar] [CrossRef]
- Dalal, L.; Allaf, A.W.; El-Zein, H. Formulation and in vitro evaluation of self-nanoemulsifying liquisolid tablets of furosemide. Sci. Rep. 2021, 11, 1315. [Google Scholar] [CrossRef]
- Gawin-Mikołajewicz, A.; Nartowski, K.P.; Dyba, A.J.; Gołkowska, A.M.; Malec, K.; Karolewicz, B. Ophthalmic nanoemulsions: From composition to technological processes and quality control. Mol. Pharm. 2021, 18, 3719–3740. [Google Scholar] [CrossRef]
- Dash, R.N.; Mohammed, H.; Humaira, T.; Ramesh, D. Design, optimization and evaluation of glipizide solid self-nanoemulsifying drug delivery for enhanced solubility and dissolution. SJP 2015, 23, 528–540. [Google Scholar] [CrossRef]
- Alwadei, M.; Kazi, M.; Alanazi, F.K. Novel oral dosage regimen based on self-nanoemulsifying drug delivery systems for codelivery of phytochemicals–curcumin and thymoquinone. SJP 2019, 27, 866–876. [Google Scholar] [CrossRef]
- Kim, D.H.; Kim, J.Y.; Kim, R.M.; Maharjan, P.; Ji, Y.-G.; Jang, D.-J.; Min, K.A.; Koo, T.-S.; Cho, K.H. Orlistat-loaded solid snedds for the enhanced solubility, dissolution, and in vivo performance. Int. J. Nanomed. 2018, 13, 7095–7106. [Google Scholar] [CrossRef]
- Parmar, K.; Patel, J.; Sheth, N. Self nano-emulsifying drug delivery system for embelin: Design, characterization and in-vitro studies. Asian J. Pharm. Sci. 2015, 10, 396–404. [Google Scholar] [CrossRef]
- Wang, L.; Dong, J.; Chen, J.; Eastoe, J.; Li, X. Design and optimization of a new self-nanoemulsifying drug delivery system. J. Colloid Interface Sci. 2009, 330, 443–448. [Google Scholar] [CrossRef]
- Subramanian, P. Lipid-based nanocarrier system for the effective delivery of nutraceuticals. Molecules 2021, 26, 5510. [Google Scholar] [CrossRef]
- Soliman, K.A.; Ibrahim, H.K.; Ghorab, M.M. Formulation of avanafil in a solid self-nanoemulsifying drug delivery system for enhanced oral delivery. Eur. J. Pharm. Sci. 2016, 93, 447–455. [Google Scholar] [CrossRef]
- Krstić, M.; Ražić, S.; Djekic, L.; Dobričić, V.; Momčilović, M.; Vasiljevic, D.; Ibrić, S. Application of a mixture experimental design in the optimization of the formulation of solid self-emulsifying drug delivery systems containing carbamazepine. Lat. Am. J. Pharm. 2015, 34, 885–894. [Google Scholar]
- Beg, S.; Katare, O.P.; Saini, S.; Garg, B.; Khurana, R.K.; Singh, B. Solid self-nanoemulsifying systems of olmesartan medoxomil: Formulation development, micromeritic characterization, in vitro and in vivo evaluation. Powder Technol. 2016, 294, 93–104. [Google Scholar] [CrossRef]
- Vohra, A.M.; Patel, C.V.; Kumar, P.; Thakkar, H.P. Development of dual drug loaded solid self microemulsifying drug delivery system: Exploring interfacial interactions using qbd coupled risk based approach. J. Mol. Liq. 2017, 242, 1156–1168. [Google Scholar] [CrossRef]
- Kang, J.H.; Oh, D.H.; Oh, Y.-K.; Yong, C.S.; Choi, H.-G. Effects of solid carriers on the crystalline properties, dissolution and bioavailability of flurbiprofen in solid self-nanoemulsifying drug delivery system (solid snedds). Eur. J. Pharm. Biopharm. 2012, 80, 289–297. [Google Scholar] [CrossRef]
- Tang, B.; Cheng, G.; Gu, J.-C.; Xu, C.-H. Development of solid self-emulsifying drug delivery systems: Preparation techniques and dosage forms. Drug Discov. Today 2008, 13, 606–612. [Google Scholar] [CrossRef]
- Nanda Kishore, R.; Yalavarthi, P.R.; Vadlamudi, H.C.; Vandana, K.R.; Rasheed, A.; Sushma, M. Solid self microemulsification of atorvastatin using hydrophilic carriers: A design. Drug Dev. Ind. Pharm. 2015, 41, 1213–1222. [Google Scholar] [CrossRef]
- Krstic, M.; Djuris, J.; Petrovic, O.; Lazarevic, N.; Cvijic, S.; Ibric, S. Application of the melt granulation technique in development of lipid matrix tablets with immediate release of carbamazepine. J. Drug Deliv. Sci. Technol. 2017, 39, 467–474. [Google Scholar] [CrossRef]
- Tarate, B.; Chavan, R.; Bansal, K.A. Oral solid self-emulsifying formulations: A patent review. Recent Pat. Drug Deliv. Formul. 2014, 8, 126–143. [Google Scholar] [CrossRef]
- Beg, S.; Jena, S.S.; Patra, C.N.; Rizwan, M.; Swain, S.; Sruti, J.; Rao, M.E.B.; Singh, B. Development of solid self-nanoemulsifying granules (ssnegs) of ondansetron hydrochloride with enhanced bioavailability potential. Colloids Surf. B Biointerfaces 2013, 101, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Sun, J.; Wang, Y.; Liu, X.; Liu, Y.; Fu, Q.; Meng, P.; He, Z. Solid self-emulsifying nitrendipine pellets: Preparation and in vitro/in vivo evaluation. Int. J. Pharm. 2010, 383, 1–6. [Google Scholar] [CrossRef] [PubMed]
- El-Badry, M.; Haq, N.; Fetih, G.; Shakeel, F. Solubility and dissolution enhancement of tadalafil using self-nanoemulsifying drug delivery system. J. Oleo Sci. 2014, 63, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Sonawane, P.H.; Panzade, P.S.; Kale, M.A. Rapid estimation of tadalafil by reverse-phase high-performance liquid chromatography method in bulk and tablet formulation. Indian J. Pharm. Sci. 2013, 75, 230–233. [Google Scholar]
- Ahmed, S.A.; Alalawi, A.M.; Shehata, A.M.; Alqurshi, A.A.; Alahmadi, Y.M.; Ali, H.S. Fabric phase sorptive extraction coupled with uplc-esi-ms/ms method for fast and sensitive quantitation of tadalafil in a bioequivalence study. SPJ 2022, in press, corrected proof. [Google Scholar] [CrossRef]
- Abd-Elhakeem, E.; Teaima, M.H.M.; Abdelbary, G.A.; El Mahrouk, G.M. Bioavailability enhanced clopidogrel -loaded solid snedds: Development and in-vitro/in-vivo characterization. J. Drug Deliv. Sci. Technol. 2019, 49, 603–614. [Google Scholar] [CrossRef]
- Choudhury, H.; Gorain, B.; Karmakar, S.; Biswas, E.; Dey, G.; Barik, R.; Mandal, M.; Pal, T.K. Improvement of cellular uptake, in vitro antitumor activity and sustained release profile with increased bioavailability from a nanoemulsion platform. Int. J. Pharm. 2014, 460, 131–143. [Google Scholar] [CrossRef]
- Yen, C.-C.; Chang, C.-W.; Hsu, M.-C.; Wu, Y.-T. Self-nanoemulsifying drug delivery system for resveratrol: Enhanced oral bioavailability and reduced physical fatigue in rats. Int. J. Mol. Sci. 2017, 18, 1853. [Google Scholar] [CrossRef]
- Patel, G.; Shelat, P.; Lalwani, A. Statistical modeling, optimization and characterization of solid self-nanoemulsifying drug delivery system of lopinavir using design of experiment. Drug Deliv. 2016, 23, 3027–3042. [Google Scholar] [CrossRef]
- Nasr, A.; Gardouh, A.; Ghorab, M. Novel solid self-nanoemulsifying drug delivery system (s-snedds) for oral delivery of olmesartan medoxomil: Design, formulation, pharmacokinetic and bioavailability evaluation. Pharmaceutics 2016, 8, 20. [Google Scholar] [CrossRef]
- Nekkanti, V.; Karatgi, P.; Prabhu, R.; Pillai, R. Solid self-microemulsifying formulation for candesartan cilexetil. AAPS PharmSciTech 2010, 11, 9–17. [Google Scholar] [CrossRef]
- Yadav, P.; Rastogi, V.; Verma, A. Application of box–behnken design and desirability function in the development and optimization of self-nanoemulsifying drug delivery system for enhanced dissolution of ezetimibe. Future J. Pharm. Sci. 2020, 6, 7. [Google Scholar] [CrossRef] [Green Version]
- Goh, P.S.; Ng, M.H.; Choo, Y.M.; Amru, N.B.; Chuah, C.H. Production of nanoemulsions from palm-based tocotrienol rich fraction by microfluidization. Molecules 2015, 20, 19936–19946. [Google Scholar] [CrossRef]
- Nair, A.B.; Singh, B.; Shah, J.; Jacob, S.; Aldhubiab, B.; Sreeharsha, N.; Morsy, M.A.; Venugopala, K.N.; Attimarad, M.; Shinu, P. Formulation and evaluation of self-nanoemulsifying drug delivery system derived tablet containing sertraline. Pharmaceutics 2022, 14, 336. [Google Scholar] [CrossRef]
- Mehanna, M.M.; Mneimneh, A.T.; Domiati, S.; Allam, A.N. Tadalafil-loaded limonene-based orodispersible tablets: Formulation, in vitro characterization and in vivo appraisal of gastroprotective activity. Int. J. Nanomed. 2020, 15, 10099–10112. [Google Scholar] [CrossRef]
- Mahmoud, E.A.; Bendas, E.R.; Mohamed, M.I. Preparation and evaluation of self-nanoemulsifying tablets of carvedilol. AAPS PharmSciTech 2009, 10, 183–192. [Google Scholar] [CrossRef]
- Jain, S.; Dongare, K.; Nallamothu, B.; Parkash Dora, C.; Kushwah, V.; Katiyar, S.S.; Sharma, R. Enhanced stability and oral bioavailability of erlotinib by solid self nano emulsifying drug delivery systems. Int. J. Pharm. 2022, 622, 121852. [Google Scholar] [CrossRef]
- Sawatdee, S.; Atipairin, A.; Sae Yoon, A.; Srichana, T.; Changsan, N.; Suwandecha, T. Formulation development of albendazole-loaded self-microemulsifying chewable tablets to enhance dissolution and bioavailability. Pharmaceutics 2019, 11, 134. [Google Scholar] [CrossRef]
- Lee, J.H.; Oh, J.-H.; Lee, Y.-J. Simple and sensitive liquid chromatography–tandem mass spectrometry methods for quantification of tadalafil in rat plasma: Application to pharmacokinetic study in rats. Arch. Pharm. Res. 2013, 36, 457–463. [Google Scholar] [CrossRef]
- Balakumar, K.; Raghavan, C.V.; Selvan, N.T.; Prasad, R.H.; Abdu, S. Self nanoemulsifying drug delivery system (snedds) of rosuvastatin calcium: Design, formulation, bioavailability and pharmacokinetic evaluation. Colloids Surf. B Biointerfaces 2013, 112, 337–343. [Google Scholar] [CrossRef]
- Ali, H.H.; Hussein, A.A. Oral nanoemulsions of candesartan cilexetil: Formulation, characterization and in vitro drug release studies. AAPS Open 2017, 3, 4. [Google Scholar] [CrossRef]
- Akhtar, J.; Siddiqui, H.H.; Fareed, S.; Badruddeen, K.M.; Aqil, M. Nanoemulsion: For improved oral delivery of repaglinide. Drug Deliv. 2016, 23, 2026–2034. [Google Scholar] [CrossRef]
- Onder, A.; Yilmaz-Oral, D.; Jerkovic, I.; Akdemir, A.O.; Gur, S. Evaluation of relaxant responses properties of cinnamon essential oil and its major component, cinnamaldehyde on human and rat corpus cavernosum. Int. Braz. J. Urol. 2019, 45, 1033–1042. [Google Scholar] [CrossRef]
- Patel, J.; Dhingani, A.; Tilala, J.; Raval, M.; Sheth, N. Formulation and development of self-nanoemulsifying granules of olmesartan medoxomil for bioavailability enhancement. Part. Sci. Technol. 2014, 32, 274–290. [Google Scholar] [CrossRef]
- Azeem, A.; Rizwan, M.; Ahmad, F.J.; Iqbal, Z.; Khar, R.K.; Aqil, M.; Talegaonkar, S. Nanoemulsion components screening and selection: A technical note. AAPS PharmSciTech 2009, 10, 69–76. [Google Scholar] [CrossRef]
- Wei, Y.; Ye, X.; Shang, X.; Peng, X.; Bao, Q.; Liu, M.; Guo, M.; Li, F. Enhanced oral bioavailability of silybin by a supersaturatable self-emulsifying drug delivery system (s-sedds). Colloids Surf. A Physicochem. Eng. 2012, 396, 22–28. [Google Scholar] [CrossRef]
- Dixit, R.P.; Nagarsenker, M.S. Self-nanoemulsifying granules of ezetimibe: Design, optimization and evaluation. Eur. J. Pharm. Sci. 2008, 35, 183–192. [Google Scholar] [CrossRef]
- Ke, Z.; Hou, X.; Jia, X.-B. Design and optimization of self-nanoemulsifying drug delivery systems for improved bioavailability of cyclovirobuxine d. Drug Des. Devel. Ther. 2016, 10, 2049–2060. [Google Scholar] [CrossRef]
- Li, P.; Ghosh, A.; Wagner, R.F.; Krill, S.; Joshi, Y.M.; Serajuddin, A.T.M. Effect of combined use of nonionic surfactant on formation of oil-in-water microemulsions. Int. J. Pharm. 2005, 288, 27–34. [Google Scholar] [CrossRef]
- Anton, N.; Vandamme, T.F. Nano-emulsions and micro-emulsions: Clarifications of the critical differences. Pharm. Res. 2011, 28, 978–985. [Google Scholar] [CrossRef]
- Rehman, F.U.; Shah, K.U.; Shah, S.U.; Khan, I.U.; Khan, G.M.; Khan, A. From nanoemulsions to self-nanoemulsions, with recent advances in self-nanoemulsifying drug delivery systems (snedds). Expert Opin. Drug Deliv. 2017, 14, 1325–1340. [Google Scholar] [CrossRef] [PubMed]
- Weerapol, Y.; Limmatvapirat, S.; Nunthanid, J.; Sriamornsak, P. Self-nanoemulsifying drug delivery system of nifedipine: Impact of hydrophilic-lipophilic balance and molecular structure of mixed surfactants. AAPS PharmSciTech 2014, 15, 456–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muqtader Ahmed, M.; Fatima, F.; Abul Kalam, M.; Alshamsan, A.; Soliman, G.A.; Shaikh, A.A.; Alshahrani, S.M.; Aldawsari, M.F.; Bhatia, S.; Khalid Anwer, M. Development of spray-dried amorphous solid dispersions of tadalafil using glycyrrhizin for enhanced dissolution and aphrodisiac activity in male rats. SPJ 2020, 28, 1817–1826. [Google Scholar] [CrossRef] [PubMed]
- Ohwoavworhua, F.O.; Adelakun, T.A.; Okhamafe, A.O. Processing pharmaceutical grade microcrystalline cellulose from groundnut husk: Extraction methods and characterization. Int. J. Green Pharm. 2009, 3, 97–104. [Google Scholar] [CrossRef]
- Wei, Y.; Ling, Y.; Su, M.; Qin, L.; Zhang, J.; Gao, Y.; Qian, S. Characterization and stability of amorphous tadalafil and four crystalline polymorphs. Chem. Pharm. Bull. 2018, 66, 1114–1121. [Google Scholar] [CrossRef]
- Fissan, H.; Ristig, S.; Kaminski, H.; Asbach, C.; Epple, M. Comparison of different characterization methods for nanoparticle dispersions before and after aerosolization. Anal. Methods 2014, 6, 7324–7334. [Google Scholar] [CrossRef]
- Danaei, M.; Dehghankhold, M.; Ataei, S.; Hasanzadeh Davarani, F.; Javanmard, R.; Dokhani, A.; Khorasani, S.; Mozafari, M.R. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics 2018, 10, 57. [Google Scholar] [CrossRef]
- Wlodarski, K.; Tajber, L.; Sawicki, W. Physicochemical properties of direct compression tablets with spray dried and ball milled solid dispersions of tadalafil in pvp-va. Eur. J. Pharm. Biopharm. 2016, 109, 14–23. [Google Scholar] [CrossRef]







| Code | Composition | ||
|---|---|---|---|
| Oil a | S b | CoS c | |
| F1 | 5 | 4 | 1 |
| F2 | 5 | 6 | 1.5 |
| F3 | 5 | 8 | 2 |
| F4 | 5 | 12 | 3 |
| F5 | 5 | 16 | 4 |
| F6 | 5 | 20 | 5 |
| Ingredient (mg/Tablet) | Formulation Codes | |
|---|---|---|
| SNECT | DCT | |
| Tadalafil | 2.5 | 2.5 |
| Cinnamon essential oil | 50 | - |
| Cremophor® RH 40 | 80 | - |
| PEG 400 | 20 | - |
| MCC | 140 | 140 |
| Silicon dioxide | 140 | 140 |
| Mannitol | 250 | 350 |
| PolyplasdoneTM XL 10 | 10 | 10 |
| Steviana | 5 | 5 |
| Magnesium stearate | 2.5 | 2.5 |
| Surfactants/Cosurfactants | No. of Inversions | Transmittance % | |
|---|---|---|---|
| Surfactants | Tween® 80 | 23.33 ± 1.42 | 90.10 ±3.4 |
| Tween® 20 | 27.57 ± 2.42 | 88.22 ± 2.9 | |
| Cremophor® RH 40 | 13.00 ± 1.42 | 94.31 ± 1.8 | |
| LabrasolTM | 36.66 ± 1.42 | 78.97 ± 4.8 | |
| Span® 80 | 33.20 ± 1.42 | 81.70 ± 5.6 | |
| Cosurfactants | PEG 400 | 11.10 ± 1.42 | 98.50 ± 0.9 |
| PEG 200 | 12.80 ± 1.42 | 96.35 ± 1.3 | |
| PG | 29.97± 4.42 | 83.4 ± 2.5 | |
| Glycerin | 33.70 ± 7.42 | 82.8 ± 2.9 | |
| Code | VO | PT (%) | SET (Sec) | Robustness to Dilution | ADS (nm) | PDI | ZP (mV) | Thermodynamic Stability Tests | ||
|---|---|---|---|---|---|---|---|---|---|---|
| H/C | CT | F/T Test | ||||||||
| F1 | B | 90.1 ± 1.7 | 39 ± 0.33 | No | 198 ± 8.7 | 4.5 ± 1.80 | −4.7 ± 0.3 | X | - | - |
| F2 | B | 92.3 ± 2.4 | 37 ± 0.43 | Yes | 222 ± 7.6 | 3.20 ± 0.97 | −5.8 ± 0.27 | √ | X | - |
| F3 | A | 95.7 ± 1.1 | 29 ± 0.37 | Yes | 159 ± 4.7 | 0.24 ± 0.03 | −11.9 ± 0.82 | √ | √ | √ |
| F4 | A | 96.3 ± 1.6 | 25 ± 0.77 | Yes | 132 ± 6.8 | 0.45 ± 0.09 | −17.8 ± 0.18 | √ | √ | √ |
| F5 | A | 97.9 ± 1.3 | 23 ± 0.34 | Yes | 45 ± 6.9 | 1.24 ± 0.16 | −18.1 ± 0.25 | √ | √ | √ |
| F6 | A | 98.8 ± 1.8 | 20 ± 0.29 | Yes | 32 ± 4.6 | 1.35 ± 0.37 | −19.7 ± 0.41 | √ | √ | √ |
| Code | CI | HR | AR | ADS (nm) | (PDI) | ZP (mV) |
|---|---|---|---|---|---|---|
| TDL-SNEGS | 12.2 ± 1.1 | 1.23 ± 0.14 | 28.3 ± 1.6 | 165 ± 3.7 | 0.49 ± 0.1 | −8.7 ± 1.1 |
| Simulated Gastric Fluid (SGF) | Simulated Intestinal Fluid (SIF) | |||
|---|---|---|---|---|
| Initial | After 2 h | Initial | After 6 h | |
| ADS | 163 ± 7.8 | 165 ± 8.3 | 161 ± 4.5 | 169 ± 9.5 |
| PDI | 0.48 ± 0.4 | 0. 49 ± 0.4 | 0.48 ± 0.2 | 0.50 ± 0.03 |
| Formulation | Dilution Fold | SGF | SIF | ||
|---|---|---|---|---|---|
| ADS | PDI | ADS | PDI | ||
| TDL-SNECT | 10 | 165 ± 8.3 | 0.49 ± 0.04 | 166 ± 7.5 | 0.50 ± 0.04 |
| 100 | 169 ± 7.9 | 0.42 ± 0.03 | 169 ± 8.6 | 0.48 ± 0.05 | |
| 200 | 169 ± 6.6 | 0.41 ± 0.02 | 174 ± 9.9 | 0.44 ± 0.03 | |
| 400 | 173 ± 7.1 | 0.46 ± 0.07 | 176 ± 7.7 | 0.49 ± 0.05 | |
| 800 | 174 ± 8.3 | 0.51 ± 0.05 | 179 ± 8.3 | 0.51 ± 0.02 | |
| Formulation | Storage Conditions | Parameter | Initial | After 3 Months |
|---|---|---|---|---|
| TDL-SNECT | 40 °C ±/ 75% RH | Appearance | Light yellow, round tablets | Light yellow, round tablets |
| ADS (nm) | 169 ± 8.70 | 172 ± 6.30 | ||
| PDI | 0.53 ± 0.05 | 0.51 ± 0.09 | ||
| Drug content (%) | 96.42 ± 1.1 | 95.73 ± 2.6 | ||
| Friability (%) | 0.29 ± 0.01 | 0.28 ± 0.01 | ||
| Hardness (kg/cm2) | 4.23 ± 0.33 | 4.25 ± 0.45 | ||
| Disintegration time (Sec) | 49 ± 3.7 | 51 ± 2.9 |
| PK Parameter | SNECT | DCT | MT |
|---|---|---|---|
| Cmax, ng mL−1 | 125.2 ± 6.6 | 54.2 ± 3.2 | 97.8 ± 4.3 |
| tmax (h) | 2.0 ± 0.3 | 2.1 ± 0.2 | 1.90 ± 0.3 |
| AUC 0–24 h (ng × h × mL−1) | 1403.0 ± 70.2 | 263.4 ± 14.7 | 930.0 ± 47.4 |
| t ½ (h) | 6.63 ± 0.8 | 4.90 ± 0.4 | 6.70 ± 0.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, H.S.M.; Ahmed, S.A.; Alqurshi, A.A.; Alalawi, A.M.; Shehata, A.M.; Alahmadi, Y.M. Tadalafil-Loaded Self-Nanoemulsifying Chewable Tablets for Improved Bioavailability: Design, In Vitro, and In Vivo Testing. Pharmaceutics 2022, 14, 1927. https://doi.org/10.3390/pharmaceutics14091927
Ali HSM, Ahmed SA, Alqurshi AA, Alalawi AM, Shehata AM, Alahmadi YM. Tadalafil-Loaded Self-Nanoemulsifying Chewable Tablets for Improved Bioavailability: Design, In Vitro, and In Vivo Testing. Pharmaceutics. 2022; 14(9):1927. https://doi.org/10.3390/pharmaceutics14091927
Chicago/Turabian StyleAli, Hany S. M., Sameh A. Ahmed, Abdulmalik A. Alqurshi, Ali M. Alalawi, Ahmed M. Shehata, and Yaser M. Alahmadi. 2022. "Tadalafil-Loaded Self-Nanoemulsifying Chewable Tablets for Improved Bioavailability: Design, In Vitro, and In Vivo Testing" Pharmaceutics 14, no. 9: 1927. https://doi.org/10.3390/pharmaceutics14091927
APA StyleAli, H. S. M., Ahmed, S. A., Alqurshi, A. A., Alalawi, A. M., Shehata, A. M., & Alahmadi, Y. M. (2022). Tadalafil-Loaded Self-Nanoemulsifying Chewable Tablets for Improved Bioavailability: Design, In Vitro, and In Vivo Testing. Pharmaceutics, 14(9), 1927. https://doi.org/10.3390/pharmaceutics14091927