The Role of Polymeric Biomaterials in the Treatment of Articular Osteoarthritis
Abstract
1. Introduction
2. Polymeric Systems for Pharmacological Treatments
2.1. Local Drug Delivery System Approaches
2.2. Anti-Inflammatory Drugs and Analgesics
2.3. Antioxidants
2.4. Immunosuppressive and Antirheumatic Drugs
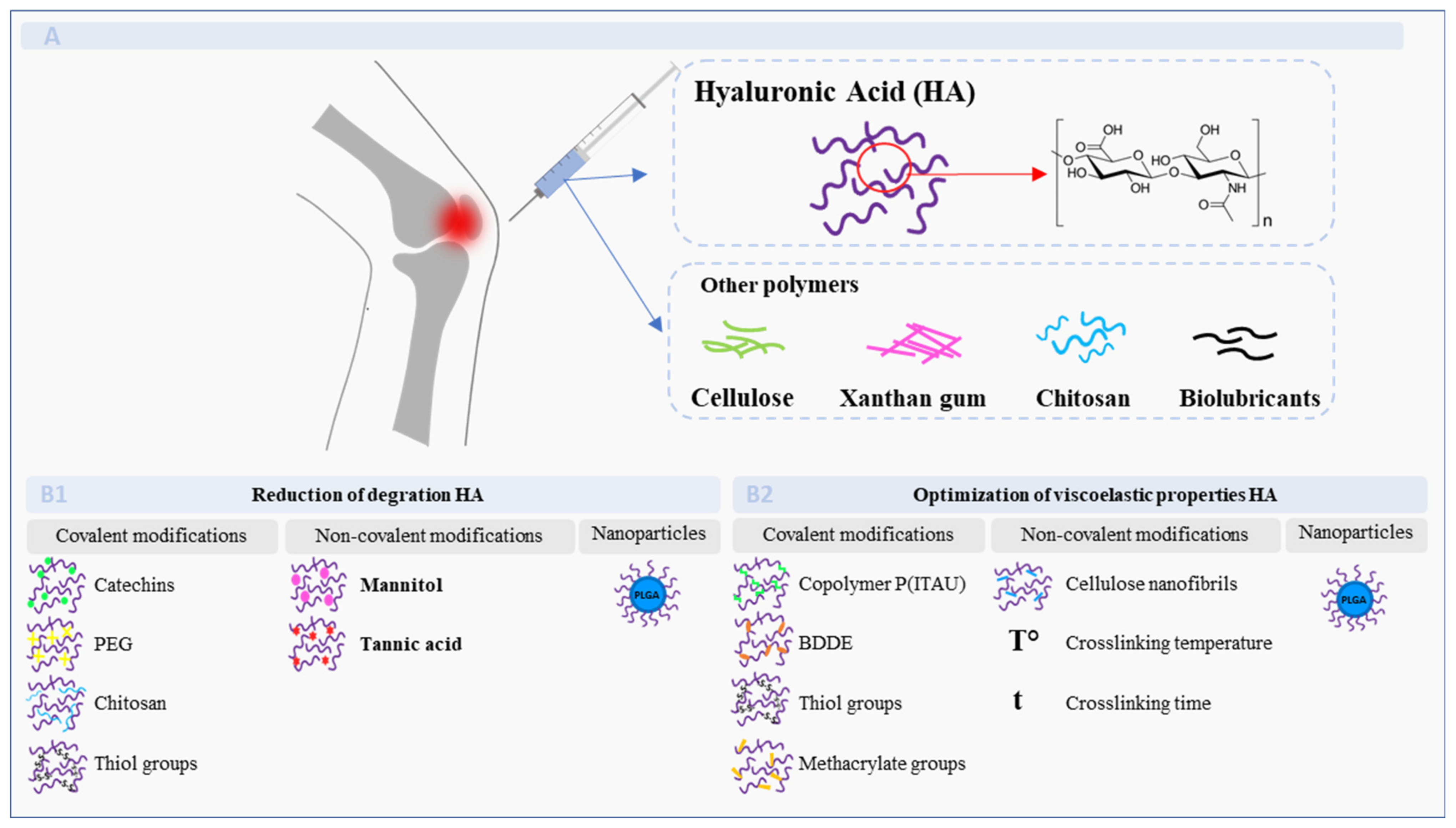
3. Polymers Used in Viscosupplementation
3.1. Natural-Based Polymers
3.2. Hyaluronic Acid
3.3. Cellulose
3.4. Other Polysacharide-Based Materials
4. Cell-Based Therapies for Osteoarthritis
4.1. Polymeric Scaffolds
4.2. Chondrocyte-Loaded Polymeric Scaffolds
4.3. Mesenchymal Stem Cell-Loaded Scaffolds
5. Conclusions and Final Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buckwalter, J.A.; Mankin, H.J.; Grodzinsky, A.J. Articular cartilage and osteoarthritis. Instr. Course Lect. 2005, 54, 465–480. [Google Scholar] [PubMed]
- Guan, V.X.; Mobasheri, A.; Probst, Y.C. A systematic review of osteoarthritis prevention and management with dietary phytochemicals from foods. Maturitas 2019, 122, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Mobasheri, A.; Rayman, M.P.; Gualillo, O.; Sellam, J.; Van Der Kraan, P.; Fearon, U. The role of metabolism in the pathogenesis of osteoarthritis. Nat. Rev. Rheumatol. 2017, 13, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Glyn-Jones, S.; Palmer, A.; Agricola, R.; Price, A.J.; Vincent, T.L.; Weinans, H.; Carr, A.J. Osteoarthritis. Lancet 2015, 386, 376–387. [Google Scholar] [CrossRef]
- Neogi, T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr. Cartil. 2013, 21, 1145–1153. [Google Scholar] [CrossRef]
- Hiligsmann, M.; Cooper, C.; Arden, N.; Boers, M.; Branco, J.C.; Brandi, M.L.; Bruyère, O.; Guillemin, F.; Hochberg, M.C.; Hunter, D.J. Health economics in the field of osteoarthritis: An expert’s consensus paper from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Semin. Arthritis Rheum. 2013, 43, 303–313. [Google Scholar] [CrossRef]
- González-Rodríguez, M.; Fernandez-Romero, A.; Rabasco, A. Towards the antioxidant therapy in Osteoarthritis: Contribution of nanotechnology. J. Drug Deliv. Sci. Technol. 2017, 42, 94–106. [Google Scholar] [CrossRef]
- Grover, A.K.; Samson, S.E. Benefits of antioxidant supplements for knee osteoarthritis: Rationale and reality. Nutr. J. 2015, 15, 1. [Google Scholar] [CrossRef]
- Oo, W.M.; Little, C.; Duong, V.; Hunter, D.J. The development of disease-modifying therapies for osteoarthritis (DMOADs): The evidence to date. Drug Des. Dev. Ther. 2021, 15, 2921. [Google Scholar] [CrossRef]
- Janssen, M.; Mihov, G.; Welting, T.; Thies, J.; Emans, P. Drugs and polymers for delivery systems in OA joints: Clinical needs and opportunities. Polymers 2014, 6, 799–819. [Google Scholar] [CrossRef]
- Gao, J.; Xia, Z.; Mary, H.B.; Joseph, J.; Luo, J.N.; Joshi, N. Overcoming barriers for intra-articular delivery of disease-modifying osteoarthritis drugs. Trends Pharmacol. Sci. 2022, 43, 171–187. [Google Scholar] [CrossRef]
- Pontes-Quero, G.M.; Garcia-Fernandez, L.; Aguilar, M.R.; San Román, J.; Cano, J.P.; Vázquez-Lasa, B. Active viscosupplements for osteoarthritis treatment. Semin. Arthritis Rheum. 2019, 49, 171–183. [Google Scholar] [CrossRef]
- Nicholls, M.; Manjoo, A.; Shaw, P.; Niazi, F.; Rosen, J. A comparison between rheological properties of intra-articular hyaluronic acid preparations and reported human synovial fluid. Adv. Ther. 2018, 35, 523–530. [Google Scholar] [CrossRef]
- Stellavato, A.; Vassallo, V.; La Gatta, A.; Pirozzi, A.V.A.; De Rosa, M.; Balato, G.; D’Addona, A.; Tirino, V.; Ruosi, C.; Schiraldi, C. Novel hybrid gels made of high and low molecular weight hyaluronic acid induce proliferation and reduce inflammation in an osteoarthritis in vitro model based on human synoviocytes and chondrocytes. BioMed Res. Int. 2019, 2019, 4328219. [Google Scholar] [CrossRef]
- Hutmacher, D.W. Scaffolds in tissue engineering bone and cartilage. Biomaterials 2000, 21, 2529–2543. [Google Scholar] [CrossRef]
- Milcovich, G.; Antunes, F.; Golob, S.; Farra, R.; Grassi, M.; Voinovich, D.; Grassi, G.; Asaro, F. Thermo-responsive hydrogels from cellulose-based polyelectrolytes and catanionic vesicles for biomedical application. J. Biomed. Mater. Res. Part A 2016, 104, 1668–1679. [Google Scholar] [CrossRef]
- Milcovich, G.; Antunes, F.E.; Farra, R.; Grassi, G.; Grassi, M.; Asaro, F. Modulating carbohydrate-based hydrogels as viscoelastic lubricant substitute for articular cartilages. Int. J. Biol. Macromol. 2017, 102, 796–804. [Google Scholar] [CrossRef]
- Housman, L.; Arden, N.; Schnitzer, T.J.; Birbara, C.; Conrozier, T.; Skrepnik, N.; Wei, N.; Bockow, B.; Waddell, D.; Tahir, H. Intra-articular hylastan versus steroid for knee osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1684–1692. [Google Scholar] [CrossRef]
- He, Z.; Wang, B.; Hu, C.; Zhao, J. An overview of hydrogel-based intra-articular drug delivery for the treatment of osteoarthritis. Colloids Surf. B Biointerfaces 2017, 154, 33–39. [Google Scholar] [CrossRef]
- Mealy, J.E.; Rodell, C.B.; Burdick, J.A. Sustained small molecule delivery from injectable hyaluronic acid hydrogels through host–guest mediated retention. J. Mater. Chem. B 2015, 3, 8010–8019. [Google Scholar] [CrossRef]
- Ahmad, U.; Sohail, M.; Ahmad, M.; Minhas, M.U.; Khan, S.; Hussain, Z.; Kousar, M.; Mohsin, S.; Abbasi, M.; Shah, S.A. Chitosan based thermosensitive injectable hydrogels for controlled delivery of loxoprofen: Development, characterization and in-vivo evaluation. Int. J. Biol. Macromol. 2019, 129, 233–245. [Google Scholar] [CrossRef]
- Zhang, Z.; Wei, X.; Gao, J.; Zhao, Y.; Zhao, Y.; Guo, L.; Chen, C.; Duan, Z.; Li, P.; Wei, L. Intra-articular injection of cross-linked hyaluronic acid-dexamethasone hydrogel attenuates osteoarthritis: An experimental study in a rat model of osteoarthritis. Int. J. Mol. Sci. 2016, 17, 411. [Google Scholar] [CrossRef]
- Joshi, N.; Yan, J.; Levy, S.; Bhagchandani, S.; Slaughter, K.V.; Sherman, N.E.; Amirault, J.; Wang, Y.; Riegel, L.; He, X. Towards an arthritis flare-responsive drug delivery system. Nat. Commun. 2018, 9, 1275. [Google Scholar] [CrossRef]
- Mohammadi, F.; Samani, S.M.; Tanideh, N.; Ahmadi, F. Hybrid scaffolds of hyaluronic acid and collagen loaded with prednisolone: An interesting system for osteoarthritis. Adv. Pharm. Bull. 2018, 8, 11. [Google Scholar] [CrossRef]
- Kim, T.; Seol, D.R.; Hahm, S.-C.; Ko, C.; Kim, E.-H.; Chun, K.; Kim, J.; Lim, T.-H. Analgesic effect of intra-articular injection of temperature-responsive hydrogel containing bupivacaine on osteoarthritic pain in rats. BioMed Res. Int. 2015, 2015, 812949. [Google Scholar] [CrossRef]
- Barati, M.; Samani, S.M.; Jahromi, L.P.; Ashrafi, H.; Azadi, A. Controlled-release in-situ gel forming formulation of tramadol containing chitosan-based pro-nanogels. Int. J. Biol. Macromol. 2018, 118, 1449–1454. [Google Scholar] [CrossRef]
- dos Santos, A.C.M.; Akkari, A.C.S.; Ferreira, I.R.S.; Maruyama, C.R.; Pascoli, M.; Guilherme, V.A.; de Paula, E.; Fraceto, L.F.; de Lima, R.; da Silva Melo, P. Poloxamer-based binary hydrogels for delivering tramadol hydrochloride: Sol-gel transition studies, dissolution-release kinetics, in vitro toxicity, and pharmacological evaluation. Int. J. Nanomed. 2015, 10, 2391. [Google Scholar]
- Matsuzaki, T.; Matsushita, T.; Tabata, Y.; Saito, T.; Matsumoto, T.; Nagai, K.; Kuroda, R.; Kurosaka, M. Intra-articular administration of gelatin hydrogels incorporating rapamycin–micelles reduces the development of experimental osteoarthritis in a murine model. Biomaterials 2014, 35, 9904–9911. [Google Scholar] [CrossRef]
- Park, J.H.; Park, S.H.; Lee, H.Y.; Lee, J.W.; Lee, B.K.; Lee, B.Y.; Kim, J.H.; Kim, M.S. An injectable, electrostatically interacting drug depot for the treatment of rheumatoid arthritis. Biomaterials 2018, 154, 86–98. [Google Scholar] [CrossRef]
- García Fernández, L.; Olmeda Lozano, M.; Benito Garzón, L.; Pérez Caballer, A.; San Román, J.; Vázquez Lasa, B. Injectable hydrogel-based drug delivery system for cartilage regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 110, 110702. [Google Scholar] [CrossRef]
- Songkroh, T.; Xie, H.; Yu, W.; Liu, X.; Sun, G.; Xu, X.; Ma, X. Injectable in situ forming chitosan-based hydrogels for curcumin delivery. Macromol. Res. 2015, 23, 53–59. [Google Scholar] [CrossRef]
- Mok, S.-W.; Fu, S.-C.; Cheuk, Y.-C.; Chu, I.-M.; Chan, K.-M.; Qin, L.; Yung, S.-H.; Kevin Ho, K.-W. Intra-articular delivery of quercetin using thermosensitive hydrogel attenuate cartilage degradation in an osteoarthritis rat model. Cartilage 2020, 11, 490–499. [Google Scholar] [CrossRef]
- Lu, K.-Y.; Lin, Y.-C.; Lu, H.-T.; Ho, Y.-C.; Weng, S.-C.; Tsai, M.-L.; Mi, F.-L. A novel injectable in situ forming gel based on carboxymethyl hexanoyl chitosan/hyaluronic acid polymer blending for sustained release of berberine. Carbohydr. Polym. 2019, 206, 664–673. [Google Scholar] [CrossRef]
- Boechat, A.L.; de Oliveira, C.P.; Tarragô, A.M.; da Costa, A.G.; Malheiro, A.; Guterres, S.S.; Pohlmann, A.R. Methotrexate-loaded lipid-core nanocapsules are highly effective in the control of inflammation in synovial cells and a chronic arthritis model. Int. J. Nanomed. 2015, 10, 6603. [Google Scholar]
- Dhanaraj, S.A.; Muralidharan, S.; Kanniappan, P.; Hui, W.T.S.; Qi, L.L. Formulation and evaluation of chitosan nanospheres containing methotrexate targeted drug delivery system. J. Young Pharm. 2016, 8, 330. [Google Scholar] [CrossRef]
- Bishnoi, M.; Jain, A.; Hurkat, P.; Jain, S.K. Aceclofenac-loaded chondroitin sulfate conjugated SLNs for effective management of osteoarthritis. J. Drug Target. 2014, 22, 805–812. [Google Scholar] [CrossRef]
- Crivelli, B.; Bari, E.; Perteghella, S.; Catenacci, L.; Sorrenti, M.; Mocchi, M.; Faragò, S.; Tripodo, G.; Prina-Mello, A.; Torre, M.L. Silk fibroin nanoparticles for celecoxib and curcumin delivery: ROS-scavenging and anti-inflammatory activities in an in vitro model of osteoarthritis. Eur. J. Pharm. Biopharm. 2019, 137, 37–45. [Google Scholar] [CrossRef]
- Rao, K.; Roome, T.; Aziz, S.; Razzak, A.; Abbas, G.; Imran, M.; Jabri, T.; Gul, J.; Hussain, M.; Sikandar, B. Bergenin loaded gum xanthan stabilized silver nanoparticles suppress synovial inflammation through modulation of the immune response and oxidative stress in adjuvant induced arthritic rats. J. Mater. Chem. B 2018, 6, 4486–4501. [Google Scholar] [CrossRef]
- Wang, J.; Wang, X.; Cao, Y.; Huang, T.; Song, D.X.; Tao, H.R. Therapeutic potential of hyaluronic acid/chitosan nanoparticles for the delivery of curcuminoid in knee osteoarthritis and an in vitro evaluation in chondrocytes. Int. J. Mol. Med. 2018, 42, 2604–2614. [Google Scholar] [CrossRef]
- El-Gogary, R.I.; Khattab, M.A.; Abd-Allah, H. Intra-articular multifunctional celecoxib loaded hyaluronan nanocapsules for the suppression of inflammation in an osteoarthritic rat model. Int. J. Pharm. 2020, 583, 119378. [Google Scholar] [CrossRef]
- Zhang, H.; Xiong, H.; Ahmed, W.; Yao, Y.; Wang, S.; Fan, C.; Gao, C. Reactive oxygen species-responsive and scavenging polyurethane nanoparticles for treatment of osteoarthritis in vivo. Chem. Eng. J. 2021, 409, 128147. [Google Scholar] [CrossRef]
- Pontes-Quero, G.M.; Benito-Garzón, L.; Pérez Cano, J.; Aguilar, M.R.; Vázquez-Lasa, B. Modulation of inflammatory mediators by polymeric nanoparticles loaded with anti-inflammatory drugs. Pharmaceutics 2021, 13, 290. [Google Scholar] [CrossRef]
- Pontes-Quero, G.M.; Benito-Garzón, L.; Cano, J.P.; Aguilar, M.R.; Vázquez-Lasa, B. Amphiphilic polymeric nanoparticles encapsulating curcumin: Antioxidant, anti-inflammatory and biocompatibility studies. Mater. Sci. Eng. C 2021, 121, 111793. [Google Scholar] [CrossRef]
- Kang, C.; Jung, E.; Hyeon, H.; Seon, S.; Lee, D. Acid-activatable polymeric curcumin nanoparticles as therapeutic agents for osteoarthritis. Nanomed. Nanotechnol. Biol. Med. 2020, 23, 102104. [Google Scholar] [CrossRef]
- Abd-Allah, H.; Kamel, A.O.; Sammour, O.A. Injectable long acting chitosan/tripolyphosphate microspheres for the intra-articular delivery of lornoxicam: Optimization and in vivo evaluation. Carbohydr. Polym. 2016, 149, 263–273. [Google Scholar] [CrossRef]
- Kaur, M.; Sharma, S.; Sinha, V. Polymer based microspheres of aceclofenac as sustained release parenterals for prolonged anti-inflammatory effect. Mater. Sci. Eng. C 2017, 72, 492–500. [Google Scholar] [CrossRef]
- Arunkumar, P.; Indulekha, S.; Vijayalakshmi, S.; Srivastava, R. Synthesis, characterizations, in vitro and in vivo evaluation of Etoricoxib-loaded Poly (Caprolactone) microparticles–a potential Intra-articular drug delivery system for the treatment of Osteoarthritis. J. Biomater. Sci. Polym. Ed. 2016, 27, 303–316. [Google Scholar] [CrossRef]
- Cannavà, C.; Tommasini, S.; Stancanelli, R.; Cardile, V.; Cilurzo, F.; Giannone, I.; Puglisi, G.; Ventura, C.A. Celecoxib-loaded PLGA/cyclodextrin microspheres: Characterization and evaluation of anti-inflammatory activity on human chondrocyte cultures. Colloids Surf. B Biointerfaces 2013, 111, 289–296. [Google Scholar] [CrossRef]
- Janssen, M.; Timur, U.T.; Woike, N.; Welting, T.J.; Draaisma, G.; Gijbels, M.; van Rhijn, L.W.; Mihov, G.; Thies, J.; Emans, P.J. Celecoxib-loaded PEA microspheres as an auto regulatory drug-delivery system after intra-articular injection. J. Control. Release 2016, 244, 30–40. [Google Scholar] [CrossRef]
- Rudnik-Jansen, I.; Colen, S.; Berard, J.; Plomp, S.; Que, I.; van Rijen, M.; Woike, N.; Egas, A.; van Osch, G.; van Maarseveen, E. Prolonged inhibition of inflammation in osteoarthritis by triamcinolone acetonide released from a polyester amide microsphere platform. J. Control. Release 2017, 253, 64–72. [Google Scholar] [CrossRef]
- Cosco, D.; Failla, P.; Costa, N.; Pullano, S.; Fiorillo, A.; Mollace, V.; Fresta, M.; Paolino, D. Rutin-loaded chitosan microspheres: Characterization and evaluation of the anti-inflammatory activity. Carbohydr. Polym. 2016, 152, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Shi, Y.; Zhang, Z.; Yang, Z.; Huang, G. Intra-articular delivery of tetramethylpyrazine microspheres with enhanced articular cavity retention for treating osteoarthritis. Asian J. Pharm. Sci. 2018, 13, 229–238. [Google Scholar] [CrossRef]
- Ratanavaraporn, J.; Soontornvipart, K.; Shuangshoti, S.; Shuangshoti, S.; Damrongsakkul, S. Localized delivery of curcumin from injectable gelatin/Thai silk fibroin microspheres for anti-inflammatory treatment of osteoarthritis in a rat model. Inflammopharmacology 2017, 25, 211–221. [Google Scholar] [CrossRef]
- Sungkhaphan, P.; Ratanavaraporn, J.; Damrongsukkul, S. Development of Thai Silk Fibroin/Hyaluronic Acid Microspheres and the Application on Controlled Release of Curcumin. Eng. J. 2017, 21, 139–153. [Google Scholar] [CrossRef][Green Version]
- El-Setouhy, D.A.; Abdelmalak, N.S.; Anis, S.E.; Louis, D. Leflunomide biodegradable microspheres intended for intra-articular administration: Development, anti-inflammatory activity and histopathological studies. Int. J. Pharm. 2015, 495, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Paik, J.; Duggan, S.T.; Keam, S.J. Triamcinolone acetonide extended-release: A review in osteoarthritis pain of the knee. Drugs 2019, 79, 455–462. [Google Scholar] [CrossRef]
- Han, Y.; Yang, J.; Zhao, W.; Wang, H.; Sun, Y.; Chen, Y.; Luo, J.; Deng, L.; Xu, X.; Cui, W. Biomimetic injectable hydrogel microspheres with enhanced lubrication and controllable drug release for the treatment of osteoarthritis. Bioact. Mater. 2021, 6, 3596–3607. [Google Scholar] [CrossRef]
- Zhang, W.; Xu, W.; Ning, C.; Li, M.; Zhao, G.; Jiang, W.; Ding, J.; Chen, X. Long-acting hydrogel/microsphere composite sequentially releases dexmedetomidine and bupivacaine for prolonged synergistic analgesia. Biomaterials 2018, 181, 378–391. [Google Scholar] [CrossRef]
- Khanal, M.; Gohil, S.V.; Kuyinu, E.; Kan, H.-M.; Knight, B.E.; Baumbauer, K.M.; Lo, K.W.-H.; Walker, J.; Laurencin, C.T.; Nair, L.S. Injectable nanocomposite analgesic delivery system for musculoskeletal pain management. Acta Biomater. 2018, 74, 280–290. [Google Scholar] [CrossRef]
- Naghizadeh, Z.; Karkhaneh, A.; Khojasteh, A. Simultaneous release of melatonin and methylprednisolone from an injectable in situ self-crosslinked hydrogel/microparticle system for cartilage tissue engineering. J. Biomed. Mater. Res. Part A 2018, 106, 1932–1940. [Google Scholar] [CrossRef]
- Qi, X.; Qin, X.; Yang, R.; Qin, J.; Li, W.; Luan, K.; Wu, Z.; Song, L. Intra-articular administration of chitosan thermosensitive in situ hydrogels combined with diclofenac sodium–loaded alginate microspheres. J. Pharm. Sci. 2016, 105, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wei, C.; Chen, X.; Liu, J.; Yu, Q.; Liu, Y.; Liu, J. Drug delivery system based on near-infrared light-responsive molybdenum disulfide nanosheets controls the high-efficiency release of dexamethasone to inhibit inflammation and treat osteoarthritis. ACS Appl. Mater. Interfaces 2019, 11, 11587–11601. [Google Scholar] [CrossRef] [PubMed]
- Mohan, L.; Anandan, C.; Rajendran, N. Drug release characteristics of quercetin-loaded TiO2 nanotubes coated with chitosan. Int. J. Biol. Macromol. 2016, 93, 1633–1638. [Google Scholar] [CrossRef]
- Rivera-Delgado, E.; Djuhadi, A.; Danda, C.; Kenyon, J.; Maia, J.; Caplan, A.I.; von Recum, H.A. Injectable liquid polymers extend the delivery of corticosteroids for the treatment of osteoarthritis. J. Control. Release 2018, 284, 112–121. [Google Scholar] [CrossRef]
- Tamura, T.; Higuchi, Y.; Kitamura, H.; Murao, N.; Saitoh, R.; Morikawa, T.; Sato, H. Novel hyaluronic acid–methotrexate conjugate suppresses joint inflammation in the rat knee: Efficacy and safety evaluation in two rat arthritis models. Arthritis Res. Ther. 2016, 18, 79. [Google Scholar] [CrossRef]
- Kim, S.E.; Lee, J.Y.; Shim, K.-S.; Lee, S.; Min, K.; Bae, J.-H.; Kim, H.-J.; Park, K.; Song, H.-R. Attenuation of inflammation and cartilage degradation by sulfasalazine-containing hyaluronic acid on osteoarthritis rat model. Int. J. Biol. Macromol. 2018, 114, 341–348. [Google Scholar] [CrossRef]
- Chen, L.; Li, X.; Zhang, Y.; Chen, T.; Xiao, S.; Liang, H. Morphological and mechanical determinants of cellular uptake of deformable nanoparticles. Nanoscale 2018, 10, 11969–11979. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.Y.; Yuk, S.H. Polymeric protein delivery systems. Prog. Polym. Sci. 2007, 32, 669–697. [Google Scholar] [CrossRef]
- Sutariya, V.; Tur, J.; Kelly, S.; Halasz, K.; Chapalamadugu, K.C.; Nimbalkar, R.; Pathak, Y.V.; Weigel, R.; Daviau, T.; Webb, T. Nanodrug delivery platform for glucocorticoid use in skeletal muscle injury. Can. J. Physiol. Pharmacol. 2018, 96, 681–689. [Google Scholar] [CrossRef]
- Roux, C. Cartílago articular normal: Anatomía, fisiología, metabolismo y envejecimiento. EMC-Apar. Locomot. 2016, 49, 1–10. [Google Scholar] [CrossRef]
- Luna-Preitschopf, A.D.; Zwickl, H.; Nehrer, S.; Hengstschläger, M.; Mikula, M. Rapamycin maintains the chondrocytic phenotype and interferes with inflammatory cytokine induced processes. Int. J. Mol. Sci. 2017, 18, 1494. [Google Scholar] [CrossRef] [PubMed]
- Takayama, K.; Kawakami, Y.; Kobayashi, M.; Greco, N.; Cummins, J.H.; Matsushita, T.; Kuroda, R.; Kurosaka, M.; Fu, F.H.; Huard, J. Local intra-articular injection of rapamycin delays articular cartilage degeneration in a murine model of osteoarthritis. Arthritis Res. Ther. 2014, 16, 482. [Google Scholar] [CrossRef] [PubMed]
- Emami, A.; Tepper, J.; Short, B.; Yaksh, T.L.; Bendele, A.M.; Ramani, T.; Cisternas, A.F.; Chang, J.H.; Mellon, R.D. Toxicology evaluation of drugs administered via uncommon routes: Intranasal, intraocular, intrathecal/intraspinal, and intra-articular. Int. J. Toxicol. 2018, 37, 4–27. [Google Scholar] [CrossRef] [PubMed]
- Persson, M.S.; Sarmanova, A.; Doherty, M.; Zhang, W. Conventional and biologic disease-modifying anti-rheumatic drugs for osteoarthritis: A meta-analysis of randomized controlled trials. Rheumatology 2018, 57, 1830–1837. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Klein, J. Recent progress in cartilage lubrication. Adv. Mater. 2021, 33, 2005513. [Google Scholar] [CrossRef]
- Chandrasekharan, A.; Seong, K.Y.; Yim, S.G.; Kim, S.; Seo, S.; Yoon, J.; Yang, S.Y. In situ photocrosslinkable hyaluronic acid-based surgical glue with tunable mechanical properties and high adhesive strength. J. Polym. Sci. Part A Polym. Chem. 2019, 57, 522–530. [Google Scholar] [CrossRef]
- Laffleur, F.; Netsomboon, K.; Erman, L.; Partenhauser, A. Evaluation of modified hyaluronic acid in terms of rheology, enzymatic degradation and mucoadhesion. Int. J. Biol. Macromol. 2019, 123, 1204–1210. [Google Scholar] [CrossRef]
- Baek, J.; Fan, Y.; Jeong, S.-H.; Lee, H.-Y.; Jung, H.-D.; Kim, H.-E.; Kim, S.; Jang, T.-S. Facile strategy involving low-temperature chemical cross-linking to enhance the physical and biological properties of hyaluronic acid hydrogel. Carbohydr. Polym. 2018, 202, 545–553. [Google Scholar] [CrossRef]
- Diaconu, A.; Nita, L.; Bercea, M.; Chiriac, A.; Rusu, A.; Rusu, D. Hyaluronic acid gels with tunable properties by conjugating with a synthetic copolymer. Biochem. Eng. J. 2017, 125, 135–143. [Google Scholar] [CrossRef]
- Jia, Y.; Zhu, W.; Zheng, M.; Huo, M.; Zhong, C. Bacterial cellulose/hyaluronic acid composite hydrogels with improved viscoelastic properties and good thermodynamic stability. Plast. Rubber Compos. 2018, 47, 165–175. [Google Scholar] [CrossRef]
- Lee, F.; Chung, J.E.; Xu, K.; Kurisawa, M. Injectable degradation-resistant hyaluronic acid hydrogels cross-linked via the oxidative coupling of green tea catechin. ACS Macro Lett. 2015, 4, 957–960. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-Y.; Hwang, C.-H.; Kim, H.-E.; Jeong, S.-H. Enhancement of bio-stability and mechanical properties of hyaluronic acid hydrogels by tannic acid treatment. Carbohydr. Polym. 2018, 186, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Bae, K.H.; Yamashita, A.; Chung, J.E.; Kurisawa, M. Thiol-mediated synthesis of hyaluronic acid–epigallocatechin-3-O-gallate conjugates for the formation of injectable hydrogels with free radical scavenging property and degradation resistance. Biomacromolecules 2017, 18, 3143–3155. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.-P.; Nguyen, L.V.-H.; Tran, N.M.-P.; Nguyen, D.T.; Nguyen, T.N.-T.; Tran, H.A.; Dang, N.N.-T.; Van Vo, T.; Nguyen, T.-H. The effect of oxidation degree and volume ratio of components on properties and applications of in situ cross-linking hydrogels based on chitosan and hyaluronic acid. Mater. Sci. Eng. C 2019, 103, 109670. [Google Scholar] [CrossRef] [PubMed]
- Rinaudo, M.; Lardy, B.; Grange, L.; Conrozier, T. Effect of mannitol on hyaluronic acid stability in two in vitro models of oxidative stress. Polymers 2014, 6, 1948–1957. [Google Scholar] [CrossRef]
- Mota, A.H.; Direito, R.; Carrasco, M.P.; Rijo, P.; Ascensão, L.; Viana, A.S.; Rocha, J.; Eduardo-Figueira, M.; Rodrigues, M.J.; Custódio, L. Combination of hyaluronic acid and PLGA particles as hybrid systems for viscosupplementation in osteoarthritis. Int. J. Pharm. 2019, 559, 13–22. [Google Scholar] [CrossRef]
- Doench, I.; Torres-Ramos, M.E.; Montembault, A.; Nunes de Oliveira, P.; Halimi, C.; Viguier, E.; Heux, L.; Siadous, R.; Thiré, R.M.; Osorio-Madrazo, A. Injectable and gellable chitosan formulations filled with cellulose nanofibers for intervertebral disc tissue engineering. Polymers 2018, 10, 1202. [Google Scholar] [CrossRef]
- Lapasin, R.; Segatti, F.; Mercuri, D.; De Conti, G.; Spagnul, C.; Fusi, S. Rheological studies dedicated to the development of a novel injectable polymeric blend for viscosupplementation treatment. Chem. Biochem. Eng. Q. 2015, 29, 511–518. [Google Scholar] [CrossRef]
- Shao, H.; Jin, Y.; Han, G.; Jiang, P.; Zhu, X.; Liu, F.; Song, Z.; Li, M.; Ling, P. Viscosupplementation of synovial fluid with xanthan gum for treatment of osteoarthritis and its clearance kinetics in the rabbit knee joint. Biorheology 2014, 51, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Wathier, M.; Lakin, B.A.; Cooper, B.G.; Bansal, P.N.; Bendele, A.M.; Entezari, V.; Suzuki, H.; Snyder, B.D.; Grinstaff, M.W. A synthetic polymeric biolubricant imparts chondroprotection in a rat meniscal tear model. Biomaterials 2018, 182, 13–20. [Google Scholar] [CrossRef]
- Arjmandi, M.; Ramezani, M. Mechanical and tribological assessment of silica nanoparticle-alginate-polyacrylamide nanocomposite hydrogels as a cartilage replacement. J. Mech. Behav. Biomed. Mater. 2019, 95, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Arjmandi, M.; Ramezani, M.; Nand, A.; Neitzert, T. Experimental study on friction and wear properties of interpenetrating polymer network alginate-polyacrylamide hydrogels for use in minimally-invasive joint implants. Wear 2018, 406, 194–204. [Google Scholar] [CrossRef]
- Mäkelä, J.; Cooper, B.; Korhonen, R.; Grinstaff, M.; Snyder, B. Functional effects of an interpenetrating polymer network on articular cartilage mechanical properties. Osteoarthr. Cartil. 2018, 26, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Suo, H.; Zhang, D.; Yin, J.; Qian, J.; Wu, Z.L.; Fu, J. Interpenetrating polymer network hydrogels composed of chitosan and photocrosslinkable gelatin with enhanced mechanical properties for tissue engineering. Mater. Sci. Eng. C 2018, 92, 612–620. [Google Scholar] [CrossRef]
- Comblain, F.; Rocasalbas, G.; Gauthier, S.; Henrotin, Y. Chitosan: A promising polymer for cartilage repair and viscosupplementation. Bio-Med. Mater. Eng. 2017, 28, S209–S215. [Google Scholar] [CrossRef]
- Tiwari, S.; Bahadur, P. Modified hyaluronic acid based materials for biomedical applications. Int. J. Biol. Macromol. 2019, 121, 556–571. [Google Scholar] [CrossRef]
- Zheng, Y.; Yang, J.; Liang, J.; Xu, X.; Cui, W.; Deng, L.; Zhang, H. Bioinspired hyaluronic acid/phosphorylcholine polymer with enhanced lubrication and anti-inflammation. Biomacromolecules 2019, 20, 4135–4142. [Google Scholar] [CrossRef]
- Conrozier, T.; Eymard, F.; Afif, N.; Balblanc, J.-C.; Legré-Boyer, V.; Chevalier, X.; Group, H.S. Safety and efficacy of intra-articular injections of a combination of hyaluronic acid and mannitol (HAnOX-M) in patients with symptomatic knee osteoarthritis: Results of a double-blind, controlled, multicenter, randomized trial. Knee 2016, 23, 842–848. [Google Scholar] [CrossRef]
- Diaz-Rodriguez, P.; Marino, C.; Vázquez, J.A.; Caeiro-Rey, J.R.; Landin, M. Targeting joint inflammation for osteoarthritis management through stimulus-sensitive hyaluronic acid based intra-articular hydrogels. Mater. Sci. Eng. C 2021, 128, 112254. [Google Scholar] [CrossRef]
- Gao, Y.; Vogus, D.; Zhao, Z.; He, W.; Krishnan, V.; Kim, J.; Shi, Y.; Sarode, A.; Ukidve, A.; Mitragotri, S. Injectable hyaluronic acid hydrogels encapsulating drug nanocrystals for long-term treatment of inflammatory arthritis. Bioeng. Transl. Med. 2022, 7, e10245. [Google Scholar] [CrossRef]
- Jin, Y.; Koh, R.H.; Kim, S.-H.; Kim, K.M.; Park, G.K.; Hwang, N.S. Injectable anti-inflammatory hyaluronic acid hydrogel for osteoarthritic cartilage repair. Mater. Sci. Eng. C 2020, 115, 111096. [Google Scholar] [CrossRef] [PubMed]
- Hickey, R.J.; Pelling, A.E. Cellulose biomaterials for tissue engineering. Front. Bioeng. Biotechnol. 2019, 7, 45. [Google Scholar] [CrossRef] [PubMed]
- Szustak, M.; Gendaszewska-Darmach, E. Nanocellulose-Based Scaffolds for Chondrogenic Differentiation and Expansion. Front. Bioeng. Biotechnol. 2021, 9, 736213. [Google Scholar] [CrossRef]
- Boyer, C.; Réthoré, G.; Weiss, P.; d’Arros, C.; Lesoeur, J.; Vinatier, C.; Halgand, B.; Geffroy, O.; Fusellier, M.; Vaillant, G. A self-setting hydrogel of silylated chitosan and cellulose for the repair of osteochondral defects: From in vitro characterization to preclinical evaluation in dogs. Front. Bioeng. Biotechnol. 2020, 8, 23. [Google Scholar] [CrossRef] [PubMed]
- Cooper, B.G.; Lawson, T.; Snyder, B.D.; Grinstaff, M.W. Reinforcement of articular cartilage with a tissue-interpenetrating polymer network reduces friction and modulates interstitial fluid load support. Osteoarthr. Cartil. 2017, 25, 1143–1149. [Google Scholar] [CrossRef]
- Leone, G.; Consumi, M.; Pepi, S.; Pardini, A.; Bonechi, C.; Tamasi, G.; Donati, A.; Lamponi, S.; Rossi, C.; Magnani, A. Enriched Gellan Gum hydrogel as visco-supplement. Carbohydr. Polym. 2020, 227, 115347. [Google Scholar] [CrossRef]
- Scognamiglio, F.; Travan, A.; Donati, I.; Borgogna, M.; Marsich, E. A hydrogel system based on a lactose-modified chitosan for viscosupplementation in osteoarthritis. Carbohydr. Polym. 2020, 248, 116787. [Google Scholar] [CrossRef]
- Salamanna, F.; Giavaresi, G.; Parrilli, A.; Martini, L.; Nicoli Aldini, N.; Abatangelo, G.; Frizziero, A.; Fini, M. Effects of intra-articular hyaluronic acid associated to Chitlac (arty-duo®) in a rat knee osteoarthritis model. J. Orthop. Res. 2019, 37, 867–876. [Google Scholar] [CrossRef]
- Consumi, M.; Leone, G.; Pepi, S.; Pardini, A.; Lamponi, S.; Bonechi, C.; Tamasi, G.; Rossi, C.; Magnani, A. Calcium ions hyaluronan/gellan gum protective shell for delivery of oleuropein in the knee. Int. J. Polym. Mater. Polym. Biomater. 2022, 71, 414–424. [Google Scholar] [CrossRef]
- Jeznach, O.; Kołbuk, D.; Sajkiewicz, P. Injectable hydrogels and nanocomposite hydrogels for cartilage regeneration. J. Biomed. Mater. Res. Part. A 2018, 106, 2762–2776. [Google Scholar] [CrossRef]
- Flégeau, K.; Pace, R.; Gautier, H.; Rethore, G.; Guicheux, J.; Le Visage, C.; Weiss, P. Toward the development of biomimetic injectable and macroporous biohydrogels for regenerative medicine. Adv. Colloid Interface Sci. 2017, 247, 589–609. [Google Scholar] [CrossRef] [PubMed]
- Foyt, D.A.; Norman, M.D.; Yu, T.T.; Gentleman, E. Exploiting advanced hydrogel technologies to address key challenges in regenerative medicine. Adv. Healthc. Mater. 2018, 7, 1700939. [Google Scholar] [CrossRef] [PubMed]
- Fiorica, C.; Palumbo, F.S.; Pitarresi, G.; Gulino, A.; Agnello, S.; Giammona, G. Injectable in situ forming hydrogels based on natural and synthetic polymers for potential application in cartilage repair. RSC Adv. 2015, 5, 19715–19723. [Google Scholar] [CrossRef]
- Hu, D.; Shan, X. Effects of different concentrations of type-I collagen hydrogel on the growth and differentiation of chondrocytes. Exp. Ther. Med. 2017, 14, 5411–5416. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kontturi, L.-S.; Järvinen, E.; Muhonen, V.; Collin, E.C.; Pandit, A.S.; Kiviranta, I.; Yliperttula, M.; Urtti, A. An injectable, in situ forming type II collagen/hyaluronic acid hydrogel vehicle for chondrocyte delivery in cartilage tissue engineering. Drug Deliv. Transl. Res. 2014, 4, 149–158. [Google Scholar] [CrossRef]
- Li, T.; Song, X.; Weng, C.; Wang, X.; Sun, L.; Gong, X.; Yang, L.; Chen, C. Self-crosslinking and injectable chondroitin sulfate/pullulan hydrogel for cartilage tissue engineering. Appl. Mater. Today 2018, 10, 173–183. [Google Scholar] [CrossRef]
- Little, C.J.; Kulyk, W.M.; Chen, X. The effect of chondroitin sulphate and hyaluronic acid on chondrocytes cultured within a fibrin-alginate hydrogel. J. Funct. Biomater. 2014, 5, 197–210. [Google Scholar] [CrossRef]
- Ma, F.; Pang, X.; Tang, B. Alginate/chondroitin sulfate based hybrid hydrogel with different molecular weight and its capacity to regulate chondrocytes activity. Carbohydr. Polym. 2019, 206, 229–237. [Google Scholar] [CrossRef]
- Mahapatra, C.; Jin, G.-Z.; Kim, H.-W. Alginate-hyaluronic acid-collagen composite hydrogel favorable for the culture of chondrocytes and their phenotype maintenance. Tissue Eng. Regen. Med. 2016, 13, 538–546. [Google Scholar] [CrossRef]
- Peng, S.; Wu, C.-W.; Lin, J.-Y.; Yang, C.-Y.; Cheng, M.-H.; Chu, I.-M. Promoting chondrocyte cell clustering through tuning of a poly (ethylene glycol)-poly (peptide) thermosensitive hydrogel with distinctive microarchitecture. Mater. Sci. Eng. C 2017, 76, 181–189. [Google Scholar] [CrossRef]
- Radhakrishnan, J.; Subramanian, A.; Sethuraman, S. Injectable glycosaminoglycan–protein nano-complex in semi-interpenetrating networks: A biphasic hydrogel for hyaline cartilage regeneration. Carbohydr. Polym. 2017, 175, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Wang, H.; Trinh, P.; Heilshorn, S.C.; Yang, F. Elastin-like protein-hyaluronic acid (ELP-HA) hydrogels with decoupled mechanical and biochemical cues for cartilage regeneration. Biomaterials 2017, 127, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Adali, T.; Kalkan, R.; Karimizarandi, L. The chondrocyte cell proliferation of a chitosan/silk fibroin/egg shell membrane hydrogels. Int. J. Biol. Macromol. 2019, 124, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Hou, S.; Wang, X.; Park, S.; Jin, X.; Ma, P.X. Rapid self-integrating, injectable hydrogel for tissue complex regeneration. Adv. Healthc. Mater. 2015, 4, 1491–1495. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Zhu, F.; Li, X.; Liang, Q.; Zhuo, Z.; Huang, J.; Duan, L.; Xiong, J.; Wang, D. Repair of osteochondral defects using injectable chitosan-based hydrogel encapsulated synovial fluid-derived mesenchymal stem cells in a rabbit model. Mater. Sci. Eng. C 2019, 99, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Pascual-Garrido, C.; Aisenbrey, E.A.; Rodriguez-Fontan, F.; Payne, K.A.; Bryant, S.J.; Goodrich, L.R. Photopolymerizable injectable cartilage mimetic hydrogel for the treatment of focal chondral lesions: A proof of concept study in a rabbit animal model. Am. J. Sports Med. 2019, 47, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.-C.; Chang, Y.-H.; Liu, H.-W.; Ding, D.-C. Transplanting human umbilical cord mesenchymal stem cells and hyaluronate hydrogel repairs cartilage of osteoarthritis in the minipig model. Tzu-Chi Med. J. 2019, 31, 11. [Google Scholar]
- Choi, B.; Kim, S.; Lin, B.; Li, K.; Bezouglaia, O.; Kim, J.; Evseenko, D.; Aghaloo, T.; Lee, M. Visible-light-initiated hydrogels preserving cartilage extracellular signaling for inducing chondrogenesis of mesenchymal stem cells. Acta Biomater. 2015, 12, 30–41. [Google Scholar] [CrossRef]
- Deng, Y.; Sun, A.X.; Overholt, K.J.; Gary, Z.Y.; Fritch, M.R.; Alexander, P.G.; Shen, H.; Tuan, R.S.; Lin, H. Enhancing chondrogenesis and mechanical strength retention in physiologically relevant hydrogels with incorporation of hyaluronic acid and direct loading of TGF-β. Acta Biomater. 2019, 83, 167–176. [Google Scholar] [CrossRef]
- Park, M.H.; Subbiah, R.; Kwon, M.J.; Kim, W.J.; Kim, S.H.; Park, K.; Lee, K. The three dimensional cues-integrated-biomaterial potentiates differentiation of human mesenchymal stem cells. Carbohydr. Polym. 2018, 202, 488–496. [Google Scholar] [CrossRef]
- Yao, H.; Xue, J.; Wang, Q.; Xie, R.; Li, W.; Liu, S.; Cai, J.; Qin, D.; Wang, D.-A.; Ren, L. Glucosamine-modified polyethylene glycol hydrogel-mediated chondrogenic differentiation of human mesenchymal stem cells. Mater. Sci. Eng. C 2017, 79, 661–670. [Google Scholar] [CrossRef]
- Zhu, M.; Feng, Q.; Sun, Y.; Li, G.; Bian, L. Effect of cartilaginous matrix components on the chondrogenesis and hypertrophy of mesenchymal stem cells in hyaluronic acid hydrogels. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 2292–2300. [Google Scholar] [CrossRef]
- Mondal, S.; Haridas, N.; Letha, S.S.; Vijith, V.; Rajmohan, G.; Rosemary, M. Development of injectable high molecular weight hyaluronic acid hydrogels for cartilage regeneration. J. Macromol. Sci. Part A 2016, 53, 507–514. [Google Scholar] [CrossRef]
- Sarem, M.; Arya, N.; Heizmann, M.; Neffe, A.T.; Barbero, A.; Gebauer, T.P.; Martin, I.; Lendlein, A.; Shastri, V.P. Interplay between stiffness and degradation of architectured gelatin hydrogels leads to differential modulation of chondrogenesis in vitro and in vivo. Acta Biomater. 2018, 69, 83–94. [Google Scholar] [CrossRef]
- Sun, A.X.; Lin, H.; Fritch, M.R.; Shen, H.; Alexander, P.G.; DeHart, M.; Tuan, R.S. Chondrogenesis of human bone marrow mesenchymal stem cells in 3-dimensional, photocrosslinked hydrogel constructs: Effect of cell seeding density and material stiffness. Acta Biomater. 2017, 58, 302–311. [Google Scholar] [CrossRef]
- Yang, Z.; Denslin, V.; Wu, Y.; Lee, E.H.; Abbas, A.A.; Kamarul, T.; Hui, J.H. Influence of fibrinogen concentration on mesenchymal stem cells and chondrocytes chondrogenesis in fibrin hydrogels. J. Biomater. Tissue Eng. 2017, 7, 1136–1145. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, J.-S. Usage of human mesenchymal stem cells in cell-based therapy: Advantages and disadvantages. Dev. Reprod. 2017, 21, 1–10. [Google Scholar] [CrossRef]
| Therapeutic Class | Encapsulation Systems | Active Ingredient | Methods/Composition | References |
|---|---|---|---|---|
| Anti-inflammatory and analgesic drugs | Hydrogels | Loxoprofen | Chitosan/isopropylacrylamide hydrogel | Ahmad [21] |
| Dexamethasone | Hyaluronic acid hydrogel | Zhang [22] | ||
| Triamcinolone | Enzymatic activities, responsive TG18 hydrogel (correlate with disease severity) | Joshi [23] | ||
| Prednisolone | Hyaluronic acid/collagen hybrid hydrogel | Mohammadi [24] | ||
| Bupivacaine | Temperature-responsive hydrogel | Kim [25] | ||
| Tramadol | Chitosan nanogel | Barati [26] | ||
| Tramadol | Poloxamer-based binary hydrogel | Dos Santos [27] | ||
| Naproxen, Dexamethason | Gelatin and HA semi-IPN | García-Fernández [30] | ||
| Nanoparticles | Aceclofenac | Solid lipid nanoparticles (SLNs) | Bishnoi [36] | |
| Celecoxib | Silk fibroin nanoparticles (SFNs) | Crivelli [37] | ||
| Celecoxib | Hyaluronan nanoparticles | El-Gogary [40] | ||
| Dexamethasone | ROS-responsive polythioketal urethane nanoparticles | Zhang [41] | ||
| Celecoxib, dexamethasone and tenoxicam | Terpolymer NPs based on a methacrylic derivative of vitamin E, vinylpyrrolidone and vinylcaprolactam | Pontes-Quero [42] | ||
| Microparticles | Diclofenac Sodium | Lubricating microspheres | Han [57] | |
| Triamcinolone | Polyester amide microspheres (PEA) | Rudnik-Jansen [50] | ||
| Triamcinolone | PLGA microspheres | Paik [56] | ||
| Celecoxib | Inflammation-responsive polyester amide microspheres (PEA) | Janssen [49] | ||
| Celecoxib | PLGA microspheres with or without cyclodextrin | Cannava [48] | ||
| Etoricoxib | Polycaprolactone microparticles (PCL-MPs) | Arunkumar [47] | ||
| Aceclofenac | PCL or PLGA microspheres | Kaur [46] | ||
| Lornoxicam | Chitosan/tripolyphosphate microspheres (TPP) | Abd-Allah [45] | ||
| Combined systems | Bupivacaine | Microsphere/hydrogel composite (MS/GEL) | Zhang [58] | |
| Ropivacaine | Nanocapsule/hydrogel composite (NC/GEL) | Khanal [59] | ||
| Methylprednisolone | Microparticle/hydrogel composite (MP/GEL) | Naghizadeh [60] | ||
| Diclofenac | Microsphere/hydrogel composite (MS/GEL) | Qi [61] | ||
| Molybdenum surfaces | Dexamethasone | MbS2 nanosheets | Zhao [62] | |
| Solid and liquid polymers | Hydrocortisone, triamcinolone y dexamethasone | Cyclodextrins in a solid disk or polymer fluid form | Rivera-Delgado [64] | |
| Antioxidants | Hydrogels | Curcumin | Chitosan/genipin/sodium salts hydrogels | Songkroh [31] |
| Quercetin | Polyethylene glycol (PEG)/polyalanine (PA) hydrogel | Mok [32] | ||
| Berberine | pH-responsive chitosan/hyaluronic acid gel | Lu [33] | ||
| Nanoparticles | Curcumin | Terpolymer NPs based on a methacrylic derivative of vitamin E, vinylpyrrolidone and vinyl caprolactam | Pontes-Quero [43] | |
| Curcumin | Acid-activable poly(β-amino ester) nanoparticles | Kang [44] | ||
| Curcumin | Silk fibroin nanoparticles (SFNs) | Crivelli [37] | ||
| Curcumin | Hyaluronic acid/chitosan nanoparticles | Wang [39] | ||
| Bergenin | Xanthan stabilized silver nanoparticles | Rao [38] | ||
| Microparticles | Curcumin | Silk fibroin/hyaluronic acid microspheres | Sungkhaphan [54] | |
| Curcumin | Gelatin/silk fibroin microspheres | Ratanavaraporn [53] | ||
| Tetramethylpyrazine | PLGA microspheres | Zhang [52] | ||
| Rutin | Chitosan microspheres | Cosco [51] | ||
| Titanium surfaces | Quercetin | TiO2 nanotubes coated with chitosan | Mohan [63] | |
| Immunosuppressive and antirheumatic drugs | Hydrogel | Minocycline | Methoxy polyethylene glycol/caprolactone hydrogel | Park [29] |
| Rapamycin | Gelatin hydrogel incorporating drug-micelles | Matsuzaki [28] | ||
| Nanoparticles | Methotrexate | Chitosan nanospheres | Dhanaraj [35] | |
| Methotrexate | Lipid nanocapsules | Boechat [34] | ||
| Microparticles | Leflunomide | PDLG microspheres | El-Setouhy [55] | |
| Conjugated systems | Methotrexate | Hyaluronic acid conjugate | Tamura [65] | |
| Sulfasalazine | Hyaluronic acid conjugate | Kim [66] |
| Type of Cell | Modified Characteristics | System Composition | Relevant Components | Type of Study | Results and Comments | References |
|---|---|---|---|---|---|---|
| Chondrocytes | Without modifications | Chitosan/silk fibroin/eggshell membrane hydrogel | - | In vitro | Biocompatible with chondrocytes | Adali [123] |
| Dextran-UPy hydrogel | In vitro and in vivo | Biocompatible with chondrocytes and BMSC | Hou [124] | |||
| Modification of cell environment | Hydrogel with alginate/polyvinyl alcohol semi-IPNs | CS addition | In vitro | Maintenance of chondrocyte phenotype and increased ECM production | Radhakrishnan [121] | |
| Fibrin/alginate hydrogel | HA and/or CS addition | Increased cell proliferation and ECM production | Little [117] | |||
| Alginate/HA hydrogel | Type II collagen addition | Maintenance of chondrocyte phenotype and increased cell proliferation and ECM production | Mahapatra [119] | |||
| Pullulan/CS hydrogel | Growing CS concentrations | Maintenance of chondrocyte phenotype and increased ECM production | Li [116] | |||
| HA hydrogel | Elastin addition | Increased metabolic activity | Fiorica [113] | |||
| Hydrogel with HA/type II collagen IPNs | 1 addition | Increased ECM production | Kontturi [115] | |||
| Elastin/HA hydrogel | Growing HA concentrations | Maintenance of chondrocyte phenotype, increased ECM production and reduced degradation | Zhu [122] | |||
| Type I collagen hydrogel | Type I collagen | Transdifferentiation and hypertrophy of chondrocytes | Hu [114] | |||
| Modification of hydrogel physical properties | Alginate/CS hydrogel | Polymer molecular weight | Increased cartilage production, reduced degradation and decrease of inflammation | Ma [118] | ||
| Mesenchymal Stem Cells (MSC) | Without modifications | HA hydrogel | - | In vitro and in vivo | MSCs differentiation and chondrocytes and cartilage regeneration | Wu [127] |
| PEG/CS hydrogel | MSCs differentiation and chondrocytes and cartilage regeneration | Pascual-Garrido [126] | ||||
| Dextran-UPy hydrogel | Simultaneous encapsulation of chondrocytes and BMSCs | Hou [124] | ||||
| Chitosan hydrogel | MSCs differentiation and chondrocytes and cartilage regeneration | Jia [125] | ||||
| Modification of cell environment | Alginate hydrogel | Adhesion and signaling molecules | In vitro | Increased cell proliferation, chondrogenesis and ECM production | Park [130] | |
| PEG/HA hydrogel | 3 and HA addition | Increased chondrogenesis and ECM production | Deng [129] | |||
| PEG hydrogel | Glucosamine addition | In vitro and in vivo | Increased chondrogenesis and ECM production and cartilage regeneration | Yao [131] | ||
| Methacrylated HA hydrogel | CS and type II collagen addition | Increased chondrogenesis and ECM production, reduced degradation and cartilage regeneration | Zhu [132] | |||
| Methacrylated chitosan hydrogel | 1 and type II colla-gen addition | Increased chondrogenesis and ECM production and cartilage regeneration | Choi [128] | |||
| Modification of hydrogel physical properties | HMW HA hydrogel crosslinked with divinyl sulfone | Crosslinking rate | In vitro | Decreased cell proliferation | Mondal [133] | |
| PEG/PLA hydrogel | Material stiffness | Decreased cell proliferation | Sun [135] | |||
| Gelatin hydrogel | Material stiffness and degradation | In vitro and in vivo | Increased chondrogenesis, slower hydrogel degradation and cartilage regeneration | Sarem [134] | ||
| Methacrylated collagen hydrogel | Reticular microstructure | Increased chondrogenesis and ECM production and cartilage regeneration | Yang [136] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velasco-Salgado, C.; Pontes-Quero, G.M.; García-Fernández, L.; Aguilar, M.R.; de Wit, K.; Vázquez-Lasa, B.; Rojo, L.; Abradelo, C. The Role of Polymeric Biomaterials in the Treatment of Articular Osteoarthritis. Pharmaceutics 2022, 14, 1644. https://doi.org/10.3390/pharmaceutics14081644
Velasco-Salgado C, Pontes-Quero GM, García-Fernández L, Aguilar MR, de Wit K, Vázquez-Lasa B, Rojo L, Abradelo C. The Role of Polymeric Biomaterials in the Treatment of Articular Osteoarthritis. Pharmaceutics. 2022; 14(8):1644. https://doi.org/10.3390/pharmaceutics14081644
Chicago/Turabian StyleVelasco-Salgado, Carmen, Gloria María Pontes-Quero, Luis García-Fernández, María Rosa Aguilar, Kyra de Wit, Blanca Vázquez-Lasa, Luis Rojo, and Cristina Abradelo. 2022. "The Role of Polymeric Biomaterials in the Treatment of Articular Osteoarthritis" Pharmaceutics 14, no. 8: 1644. https://doi.org/10.3390/pharmaceutics14081644
APA StyleVelasco-Salgado, C., Pontes-Quero, G. M., García-Fernández, L., Aguilar, M. R., de Wit, K., Vázquez-Lasa, B., Rojo, L., & Abradelo, C. (2022). The Role of Polymeric Biomaterials in the Treatment of Articular Osteoarthritis. Pharmaceutics, 14(8), 1644. https://doi.org/10.3390/pharmaceutics14081644








