Mucoadhesive Nanocarriers as a Promising Strategy to Enhance Intracellular Delivery against Oral Cavity Carcinoma
Abstract
:1. Introduction
2. Overview of Oral Mucosa
2.1. Anatomy, Physiology, and Permeability of Oral Mucosa
2.2. Permeability Barrier to Oral Mucosal Drug Absorption
2.3. Oral Cavity as a Site for Drug Delivery in Oral Cancer
3. Conventional Treatments and Their Limitations
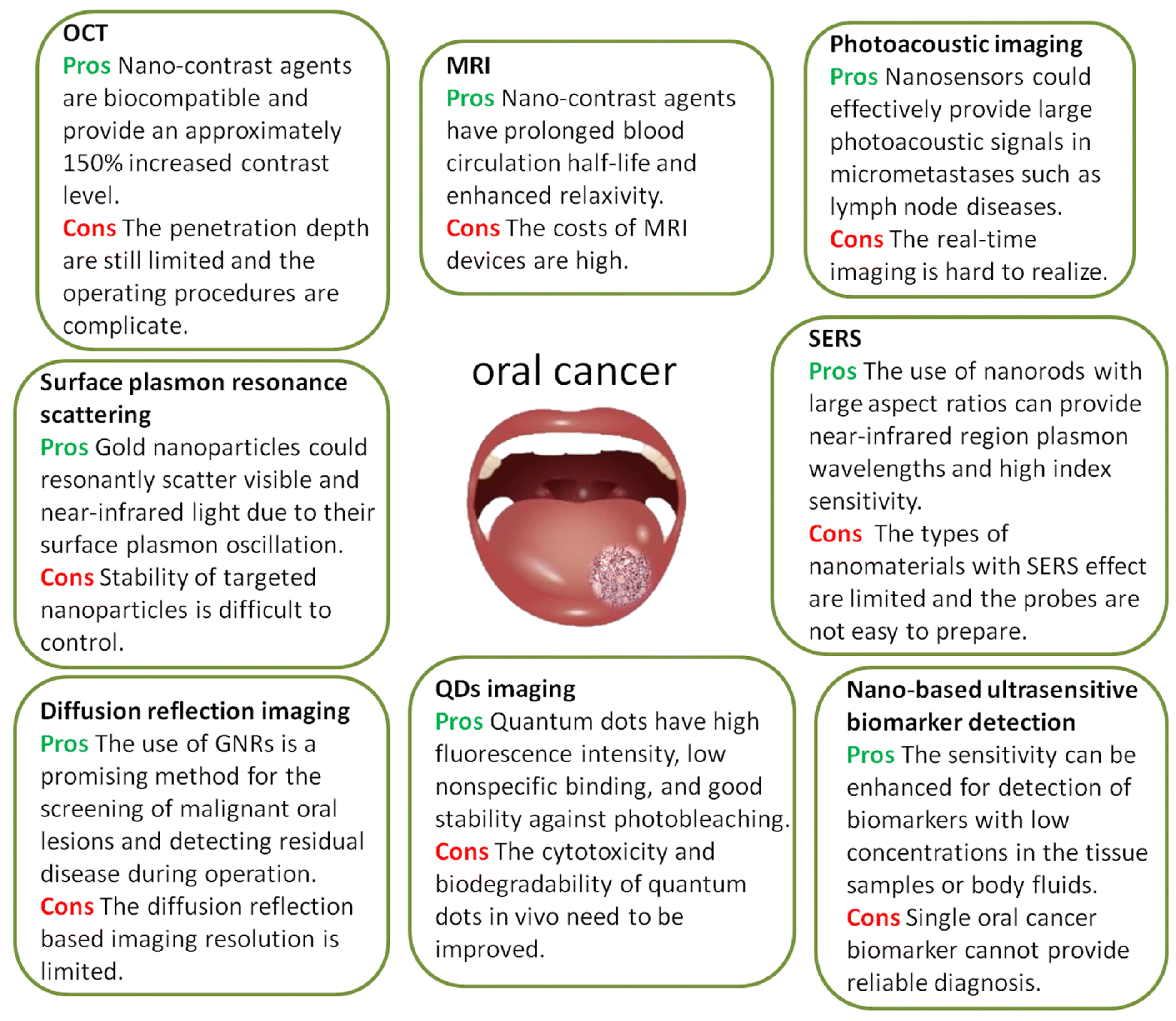
4. Nanocarriers in Oral Cancer Detection and Treatment
5. Mechanism of Cytosolic Delivery of Drugs
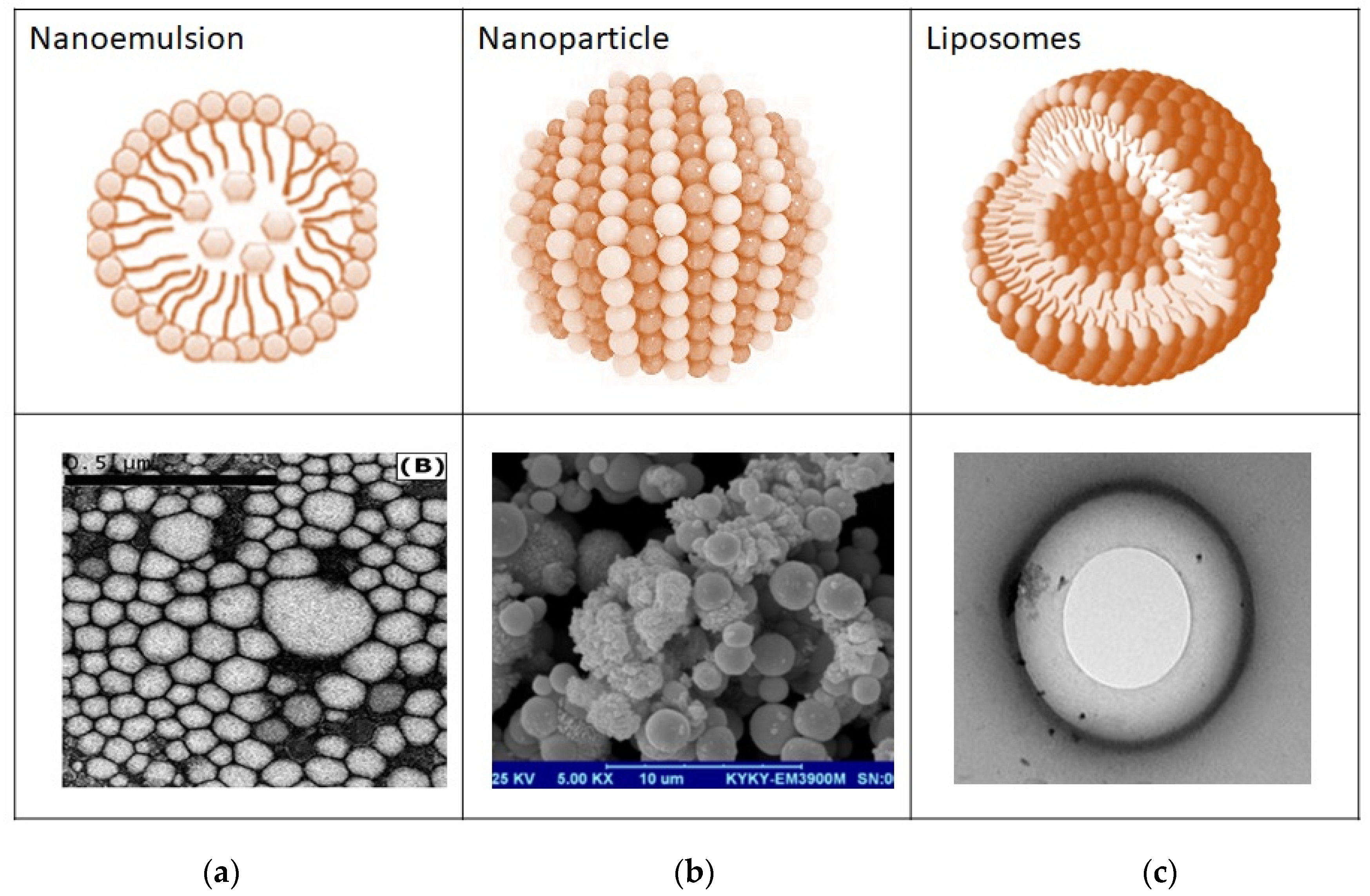
6. Nanocarriers in Drug Delivery
Multifunctional Properties of Nanocarriers
7. Treatment Strategies to Enhance Targeted Delivery to Oral Cancer
7.1. Systemic Delivery of Conventional and Novel Drug Delivery Systems
7.2. Local Delivery of Conventional and Mucoadhesive Novel Drug Delivery Systems for Cytoplasmic Delivery
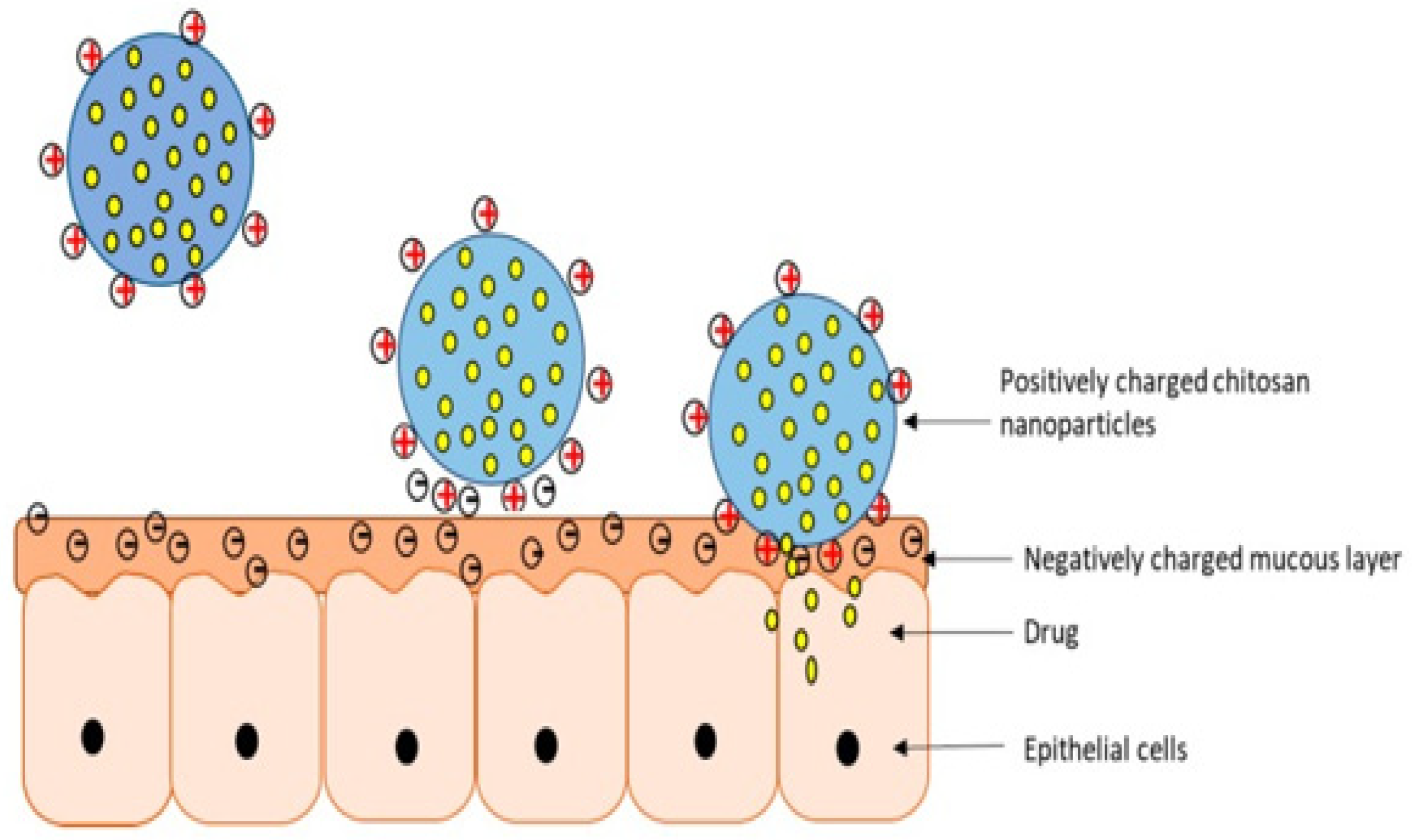
7.2.1. Mucoadhesive Nanoparticles in the Enhanced Treatment of Oral Cancer
7.2.2. Mucoadhesive Liposomes for the Treatment of Oral Cancer
7.2.3. Mucoadhesive Nanoemulsion in the Enhanced Treatment of Oral Cancer
| Types of Nanocarriers | Composition of Nanoparticles | Anticancer Drug | Animal/Ex Vivo/Cell Lines | Outcome | References |
|---|---|---|---|---|---|
| Nanoparticles | Polycaprolactone chitosan | Curcumin | Porcine esophagi |
| [77] |
| Chitosan | Oxaliplatin | Porcine mucosa |
| [21] | |
| Chitosan, hyluronic acid | Doxurubicin | Porcine oral mucosal tissues HN22 cell lines |
| [78] | |
| Liposomes | Chitosan, HPMC, and PVA buccal film | Methotrexate | Human oral squamous carcinoma cell line (HSC-3 cells) |
| [87] |
| Alginate oral paste | Doxorubicin | Human tongue squamous cell carcinoma cell line (CAL-27) |
| [88] | |
| Nanoemulsion | Tween 80 and soya oil, glycerol, water | 5-fluorouracil & curcumin | Oral squamous cells carcinoma (SCC090 and SCC 152) |
| [92] |
| Chia seed oil and α-tocopherol, TPGS, MCC, dextrose | Genistein | FaDu human pharyngeal squamous cell carcinoma |
| [19] |
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Irani, S. New insights into oral cancer—Risk factors and prevention: A review of literature. Int. J. Prev. Med. 2020, 11, 182–190. [Google Scholar] [CrossRef] [PubMed]
- WHO Oral Health. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 11 January 2022).
- Manikandan, M.; Rao, A.K.D.M.; Arunkumar, G.; Manickavasagam, M.; Rajkumar, K.S.; Rajaraman, R.; Munirajan, A.K. Oral squamous cell carcinoma: MicroRNA expression profiling and integrative analyses for elucidation of tumourigenesis mechanism. Mol. Cancer 2016, 15, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nör, J.; Gutkind, J. Head and Neck Cancer in the New Era of Precision Medicine. J. Dent. Res. 2018, 97, 601–602. [Google Scholar] [CrossRef]
- Chi, A.C.; Day, T.A.; Neville, B.W. Oral cavity and oropharyngeal squamous cell carcinoma-an update. CA Cancer J. Clin. 2015, 65, 401–421. [Google Scholar] [CrossRef]
- Li, H.; Shi, L.; Wei, J.; Zhang, C.; Zhou, Z.; Wu, L.; Liu, W. Cellular uptake and anticancer activity of salvianolic acid B phospholipid complex loaded nanoparticles in head and neck cancer and precancer cells. Colloids Surf. B Biointerfaces 2016, 147, 65–72. [Google Scholar] [CrossRef]
- Jiang, X.; Wu, J.; Wang, J.; Huang, R. Tobacco and oral squamous cell carcinoma: A review of carcinogenic pathways. Tob. Induc. Dis. 2019, 17, 29. [Google Scholar] [CrossRef]
- Dhanuthai, K.; Rojanawatsirivej, S.; Thosaporn, W.; Kintarak, S.; Subarnbhesaj, A.; Darling, M.; Kryshtalskyj, E.; Chiang, C.-P.; Shin, H.-I.; Choi, S.-Y.; et al. Oral cancer: A multicenter study. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e23–e29. [Google Scholar] [CrossRef]
- Rivera, C.; Venegas, B. Histological and molecular aspects of oral squamous cell carcinoma (Review). Oncol. Lett. 2014, 8, 7–11. [Google Scholar] [CrossRef] [Green Version]
- Kushima, M.; Tsuda, Y.; Morishita, A.; Fukuda, M.; Akita, H.; Ichihara, M.; Morioka, M. Koilocytosis. J. Jpn. Soc. Clin. Cytol. 2012, 51, 49–52. [Google Scholar] [CrossRef]
- Marcazzan, S.; Varoni, E.M.; Blanco, E.; Lodi, G.; Ferrari, M. Nanomedicine, an emerging therapeutic strategy for oral cancer therapy. Oral Oncol. 2018, 76, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, A.; Madu, C.O.; Lu, Y. Phytochemicals in Chemoprevention: A Cost-Effective Complementary Approach. J. Cancer 2021, 12, 3686–3700. [Google Scholar] [CrossRef] [PubMed]
- Azharuddin, M.; Roberg, K.; Dhara, A.K.; Jain, M.V.; D’Arcy, P.; Hinkula, J.; Slater, N.K.H.; Patra, H.K. Dissecting multi drug resistance in head and neck cancer cells using multicellular tumor spheroids. Sci. Rep. 2019, 9, 20066. [Google Scholar] [CrossRef]
- Blanco, E.; Shen, H.; Ferrari, M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat. Biotechnol. 2015, 33, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.; Wiesenfeld, D. Oral Cancer. Aust. Dent. J. 2018, 63, S91–S99. [Google Scholar] [CrossRef] [PubMed]
- Gomathi, M.; Ayisha Hamna, T.P.; Jijo, A.J.; Saradha Devi, K.M.; Arul, N.; Balachandar, V. Recent advances in radiotherapy and its associated side effects in cancer—A review. J. Basic Appl. Zool. 2019, 80, 14. [Google Scholar] [CrossRef]
- Mariadoss, A.V.A.; Vinayagam, R.; Xu, B.; Venkatachalam, K.; Sankaran, V.; Vijayakumar, S.; Bakthavatsalam, S.R.; Mohamed, S.A.; David, E. Phloretin loaded chitosan nanoparticles enhance the antioxidants and apoptotic mechanisms in DMBA induced experimental carcinogenesis. Chem. Interact. 2019, 308, 11–19. [Google Scholar] [CrossRef]
- Elbayoumi, T.; Gavin, A.; Pham, J.; Wang, D.; Brownlow, B. Layered nanoemulsions as mucoadhesive buccal systems for controlled delivery of oral cancer therapeutics. Int. J. Nanomed. 2015, 10, 1569–1584. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Guillén, M.C.; Montero, M.P. Enhancement of oral bioavailability of natural compounds and probiotics by mucoadhesive tailored biopolymer-based nanoparticles: A review. Food Hydrocoll. 2021, 118, 106772. [Google Scholar] [CrossRef]
- Matos, B.N.; Pereira, M.N.; Bravo, M.D.O.; Filho, M.C.; Saldanha-Araújo, F.; Gratieri, T.; Gelfuso, G.M. Chitosan nanoparticles loading oxaliplatin as a mucoadhesive topical treatment of oral tumors: Iontophoresis further enhances drug delivery ex vivo. Int. J. Biol. Macromol. 2019, 154, 1265–1275. [Google Scholar] [CrossRef]
- Sankar, V.; Hearnden, V.; Hull, K.; Juras, D.V.; Greenberg, M.S.; Kerr, A.R.; Lockhart, P.B.; Patton, L.; Porter, S.; Thornhill, M. Local drug delivery for oral mucosal diseases: Challenges and opportunities. Oral Dis. 2011, 17, 73–84. [Google Scholar] [CrossRef]
- Kurian Mathew, A. Oral local drug delivery: An overview. Pharm. Pharmacol. Res. 2015, 3, 1–6. [Google Scholar]
- Sohi, H.; Ahuja, A.; Ahmad, F.J.; Khar, R.K. Critical evaluation of permeation enhancers for oral mucosal drug de-livery. Drug Dev. Ind. Pharm. 2010, 36, 254–282. [Google Scholar] [CrossRef] [PubMed]
- Macedo, A.; Castro, P.M.; Roque, L.; Thomé, N.G.; Reis, C.; Pintado, M.M.; Fonte, P. Novel and revisited approaches in nanoparticle systems for buccal drug delivery. J. Control. Release 2020, 320, 125–141. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, S.; Hiorth, M. Advanced drug delivery systems for local treatment of the oral cavity. Ther. Deliv. 2015, 6, 595–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roncato, F.; Rruga, F.; Porcù, E.; Casarin, E.; Ronca, R.; Maccarinelli, F.; Realdon, N.; Basso, G.; Alon, R.; Viola, G.; et al. Improvement and extension of anti-EGFR targeting in breast cancer therapy by integration with the Avidin-Nucleic-Acid-Nano-Assemblies. Nat. Commun. 2018, 9, 4070. [Google Scholar] [CrossRef] [Green Version]
- Johnson, D.E.; Burtness, B.; Leemans, C.R.; Lui, V.W.Y.; Bauman, J.E.; Grandis, J.R. Head and neck squamous cell carcinoma. Nat. Rev. Dis. Primers 2020, 6, 92. [Google Scholar] [CrossRef]
- Kato, M.G.; Baek, C.-H.; Chaturvedi, P.; Gallagher, R.; Kowalski, L.P.; Leemans, C.R.; Warnakulasuriya, S.; Nguyen, S.A.; Day, T.A. Update on oral and oropharyngeal cancer staging–International perspectives. World J. Otorhinolaryngol. Head Neck Surg. 2020, 6, 66–75. [Google Scholar] [CrossRef]
- Calixto, G.; Fonseca-Santos, B.; Chorilli, M.; Bernegossi, J. Nanotechnology-based drug delivery systems for treatment of oral cancer: A review. Int. J. Nanomed. 2014, 9, 3719–3735. [Google Scholar] [CrossRef] [Green Version]
- Ketabat, F.; Pundir, M.; Mohabatpour, F.; Lobanova, L.; Koutsopoulos, S.; Hadjiiski, L.; Chen, X.; Papagerakis, P.; Papagerakis, S. Controlled Drug Delivery Systems for Oral Cancer Treatment—Current Status and Future Perspectives. Pharmaceutics 2019, 11, 302. [Google Scholar] [CrossRef] [Green Version]
- Yao, Y.; Zhou, Y.; Liu, L.; Xu, Y.; Chen, Q.; Wang, Y.; Wu, S.; Deng, Y.; Zhang, J.; Shao, A. Nanoparticle-Based Drug Delivery in Cancer Therapy and Its Role in Overcoming Drug Resistance. Front. Mol. Biosci. 2020, 7, 198. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.J.; Zhang, X.Q.; Liu, Q.; Zhang, J.; Zhou, G. Nanotechnology: A promising method for oral cancer detection and diagnosis. J. Nanobiotechnology 2018, 16, 52. [Google Scholar] [CrossRef] [PubMed]
- Gao, A.; Teng, Y.; Seyiti, P.; Yen, Y.; Qian, H.; Xie, C.; Li, R.; Lin, Z. Using Omniscan-Loaded Nanoparticles as a Tumor-Targeted MRI Contrast Agent in Oral Squamous Cell Carcinoma by Gelatinase-Stimuli Strategy. Nanoscale Res. Lett. 2019, 14, 395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, C.S.; Ingato, D.; Wilder-Smith, P.; Chen, Z.; Kwon, Y.J. Stimuli-disassembling gold nanoclusters for diagnosis of early stage oral cancer by optical coherence tomography. Nano Converg. 2018, 5, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yadav, P.; Jain, J.; Sherje, A.P. Recent advances in nanocarriers-based drug delivery for cancer therapeutics: A review. React. Funct. Polym. 2021, 165, 104970. [Google Scholar] [CrossRef]
- Reinholz, J.; Landfester, K.; Mailänder, V. The challenges of oral drug delivery via nanocarriers. Drug Deliv. 2018, 25, 1694–1705. [Google Scholar] [CrossRef]
- Hua, S. Advances in Nanoparticulate Drug Delivery Approaches for Sublingual and Buccal Administration. Front. Pharmacol. 2019, 10, 1328. [Google Scholar] [CrossRef] [Green Version]
- Sivashankari, P.R.; Prabaharan, M. Chitosan/Carbon-Based Nanomaterials as Scaffolds for Tissue Engineering; Elsevier Ltd.: Amsterdam, The Netherlands, 2017; ISBN 9780081019153. [Google Scholar]
- Gao, Z.; Zhang, L.; Sun, Y. Nanotechnology applied to overcome tumor drug resistance. J. Control. Release 2012, 162, 45–55. [Google Scholar] [CrossRef]
- Pathak, C.; Vaidya, F.U.; Pandey, S.M. Mechanism for Development of Nanobased Drug Delivery System. In Applications of Targeted Nano Drugs and Delivery Systems; Elsevier: Amsterdam, The Netherlands, 2019; pp. 35–67. [Google Scholar]
- Caro, C.; Pozo, D. Polysaccharide Colloids as Smart Vehicles in Cancer Therapy. Curr. Pharm. Des. 2015, 21, 4822–4836. [Google Scholar] [CrossRef]
- Battistella, C.; Klok, H.-A. Controlling and Monitoring Intracellular Delivery of Anticancer Polymer Nanomedicines. Macromol. Biosci. 2017, 17, 1700022. [Google Scholar] [CrossRef] [Green Version]
- Parodi, A.; Corbo, C.; Cevenini, A.; Molinaro, R.; Palomba, R.; Pandolfi, L.; Agostini, M.; Salvatore, F.; Tasciotti, E. Enabling cytoplasmic delivery and organelle targeting by surface modification of nanocarriers. Nanomedicine 2015, 10, 1923–1940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Felice, F.; Cavallini, C.; Barlattani, A.; Tombolini, M.; Brugnoletti, O.; Tombolini, V.; Polimeni, A. Nanotechnology in Oral Cavity Carcinoma: Recent Trends and Treatment Opportunities. Nanomaterials 2019, 9, 1546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaikh, R.; Raj Singh, T.; Garland, M.; Woolfson, A.; Donnelly, R. Mucoadhesive drug delivery systems. J. Pharm. Bioallied Sci. 2011, 3, 89–100. [Google Scholar] [PubMed]
- McBain, J.W.; Hopkins, D.G. On Adhesives and Adhesive Action. J. Phys. Chem. 1925, 29, 188–204. [Google Scholar] [CrossRef]
- Jiménez-Castellanos, M.R.; Zia, H.; Rhodes, C.T. Mucoadhesive Drug Delivery Systems. Drug Dev. Ind. Pharm. 1993, 19, 143–194. [Google Scholar] [CrossRef]
- Wakaskar, R.R. Role of Nanoparticles in Drug Delivery Encompassing Cancer Therapeutics. Int. J. Drug Dev. Res. 2017, 93, 3–4. [Google Scholar]
- Gupta, S.; Das, S.; Singh, A.; Ghosh, S. A Brief Review on Bucco-adhesive Drug Delivery System. J. Drug Deliv. Ther. 2021, 11, 231–235. [Google Scholar] [CrossRef]
- Alkhalidi, H.M.; Hosny, K.M.; Rizg, W.Y. Oral Gel Loaded by Fluconazole-Sesame Oil Nanotransfersomes: Development, Optimization, and Assessment of Antifungal Activity. Pharmaceutics 2020, 13, 27. [Google Scholar] [CrossRef]
- Pandey, M.; Choudhury, H.; Aziz, A.B.A.; Bhattamisra, S.; Gorain, B.; Su, J.; Tan, C.; Chin, W.; Yip, K. Potential of Stimuli-Responsive In Situ Gel System for Sustained Ocular Drug Delivery: Recent Progress and Contemporary Research. Polymers 2021, 13, 1340. [Google Scholar] [CrossRef]
- Chin, L.Y.; Tan, J.Y.P.; Choudhury, H.; Pandey, M.; Sisinthy, S.P.; Gorain, B. Development and optimization of chitosan coated nanoemulgel of telmisartan for intranasal delivery: A comparative study. J. Drug Deliv. Sci. Technol. 2021, 62, 102341. [Google Scholar] [CrossRef]
- Pandey, M.; Choudhury, H.; Abdul-Aziz, A.; Bhattamisra, S.K.; Gorain, B.; Carine, T.; Wee Toong, T.; Yi, N.J.; Win Yi, L. Promising Drug Delivery Approaches to Treat Microbial Infections in the Vagina: A Recent Update. Polymers 2020, 13, 26. [Google Scholar] [CrossRef] [PubMed]
- El-Leithy, E.S.; Shaker, D.S.; Ghorab, M.K.; Abdel-Rashid, R.S. Evaluation of Mucoadhesive Hydrogels Loaded with Diclofenac Sodium–Chitosan Microspheres for Rectal Administration. Aaps Pharmscitech 2010, 11, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Yaqoob, A.A.; Ahmad, H.; Parveen, T.; Ahmad, A.; Oves, M.; Ismail, I.M.I.; Qari, H.A.; Umar, K.; Ibrahim, M.N.M. Recent Advances in Metal Decorated Nanomaterials and Their Various Biological Applications: A Review. Front. Chem. 2020, 8, 341. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Sun, Y.; Wang, P.; Zhang, R.; Huo, C.; Gao, T.; Song, C.; Xing, J.; Dong, Y. Mucoadhesive nanoparticles-based oral drug delivery systems enhance ameliorative effects of low molecular weight heparin on experimental colitis. Carbohydr. Polym. 2020, 246, 116660. [Google Scholar] [CrossRef] [PubMed]
- Mahakian, L.M.; Farwell, D.G.; Zhang, H.; Seo, J.W.; Poirier, B.; Tinling, S.P.; Afify, A.M.; Haynam, E.M.; Shaye, D.; Ferrara, K.W. Comparison of PET Imaging with 64Cu-Liposomes and 18F-FDG in the 7,12-Dimethylbenz[a]anthracene (DMBA)-Induced Hamster Buccal Pouch Model of Oral Dysplasia and Squamous Cell Carcinoma. Mol. Imaging Biol. 2014, 16, 284–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, F.; Liao, W.; Xu, Z.; Yang, Y.; Wong, D.T.; Ho, C.-M. Bio/Abiotic Interface Constructed from Nanoscale DNA Dendrimer and Conducting Polymer for Ultrasensitive Biomolecular Diagnosis. Small 2009, 5, 1784–1790. [Google Scholar] [CrossRef] [Green Version]
- Xiong, J.; Feng, J.; Qiu, L.; Gao, Z.; Li, P.; Pang, L.; Zhang, Z. SDF-1-loaded PLGA nanoparticles for the targeted photoacoustic imaging and photothermal therapy of metastatic lymph nodes in tongue squamous cell carcinoma. Int. J. Pharm. 2019, 554, 93–104. [Google Scholar] [CrossRef]
- Yang, S.-J.; Lin, C.-F.; Kuo, M.-L.; Tan, C.-T. Photodynamic Detection of Oral Cancers with High-Performance Chitosan-Based Nanoparticles. Biomacromolecules 2013, 14, 3183–3191. [Google Scholar] [CrossRef]
- Arulmozhi, V.; Pandian, K.; Mirunalini, S. Ellagic acid encapsulated chitosan nanoparticles for drug delivery system in human oral cancer cell line (KB). Colloids Surf. B Biointerfaces 2013, 110, 313–320. [Google Scholar] [CrossRef]
- Cacciotti, I.; Chronopoulou, L.; Palocci, C.; Amalfitano, A.; Cantiani, M.; Cordaro, M.; Lajolo, C.; Callà, C.; Boninsegna, A.; Lucchetti, D.; et al. Controlled release of 18-β-glycyrrhetic acid by nanodelivery systems increases cytotoxicity on oral carcinoma cell line. Nanotechnology 2018, 29, 285101. [Google Scholar] [CrossRef]
- Gupta, P.; Singh, M.; Kumar, R.; Belz, J.; Shanker, R.; Dwivedi, P.D.; Sridhar, S.; Singh, S.P. Synthesis and in vitro studies of PLGA-DTX nanoconjugate as potential drug delivery vehicle for oral cancer. Int. J. Nanomed. 2018, 13, 67–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hejmady, S.; Pradhan, R.; Alexander, A.; Agrawal, M.; Singhvi, G.; Gorain, B.; Tiwari, S.; Kesharwani, P.; Dubey, S.K. Recent advances in targeted nanomedicine as promising antitumor therapeutics. Drug Discov. Today 2020, 25, 2227–2244. [Google Scholar] [CrossRef] [PubMed]
- Pandey, M.; Choudhury, H.; Yeun, O.C.; Yin, H.M.; Lynn, T.W.; Tine, C.L.; Wi, N.S.; Yen, K.C.; Phing, C.S.; Kesharwani, P.; et al. Perspectives of Nanoemulsion Strategies in The Improvement of Oral, Parenteral and Transdermal Chemotherapy. Curr. Pharm. Biotechnol. 2018, 19, 276–292. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, Y.; Ushijima, K.; Noguchi, T.; Okada, N.; Hayasaka, J.-I.; Jinbu, Y.; Ando, H.; Mori, Y.; Kusama, M.; Fujimura, A. Influence of a dosing-time on toxicities induced by docetaxel, cisplatin and 5-fluorouracil in patients with oral squamous cell carcinoma; a cross-over pilot study. Chronobiol. Int. 2018, 35, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, H.; Gorain, B.; Karmakar, S.; Biswas, E.; Dey, G.; Barik, R.; Mandal, M.; Pal, T.K. Improvement of cellular uptake, in vitro antitumor activity and sustained release profile with increased bioavailability from a nanoemulsion platform. Int. J. Pharm. 2014, 460, 131–143. [Google Scholar] [CrossRef]
- Gorain, B.; Choudhury, H.; Pandey, M.; Kesharwani, P. Paclitaxel loaded vitamin E-TPGS nanoparticles for cancer therapy. Mater. Sci. Eng. C 2018, 91, 868–880. [Google Scholar] [CrossRef]
- Chou, P.-L.; Huang, Y.-P.; Cheng, M.-H.; Rau, K.-M.; Fang, Y.-P. Improvement of Paclitaxel-Associated Adverse Reactions (ADRs) via the Use of Nano-Based Drug Delivery Systems: A Systematic Review and Network Meta-Analysis. Int. J. Nanomed. 2020, 15, 1731–1743. [Google Scholar] [CrossRef] [Green Version]
- Nakakaji, R.; Umemura, M.; Mitsudo, K.; Kim, J.-H.; Hoshino, Y.; Sato, I.; Masuda, T.; Yamamoto, M.; Kioi, M.; Koizumi, T.; et al. Treatment of oral cancer using magnetized paclitaxel. Oncotarget 2018, 9, 15591–15605. [Google Scholar] [CrossRef] [Green Version]
- Jaafari, A.; Tilaoui, M.; Mouse, H.A.; M’Bark, L.A.; Aboufatima, R.; Chait, A.; Lepoivre, M.; Zyad, A. Comparative study of the antitumor effect of natural monoterpenes: Relationship to cell cycle analysis. Rev. Bras. Farm. 2012, 22, 534–540. [Google Scholar] [CrossRef] [Green Version]
- Tubtimsri, S.; Limmatvapirat, C.; Limsirichaikul, S.; Akkaramongkolporn, P.; Inoue, Y.; Limmatvapirat, S. Fabrication and characterization of spearmint oil loaded nanoemulsions as cytotoxic agents against oral cancer cell. Asian J. Pharm. Sci. 2018, 13, 425–437. [Google Scholar] [CrossRef]
- Ramalingam, K.; Poonia, M.; Goyal, S.; Sidhu, S.K. Nanotechnology in oral cancer: A comprehensive review. J. Oral Maxillofac. Pathol. 2017, 21, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, M.A.; Syeda, J.T.M.; Wasan, K.M.; Wasan, E.K. An Overview of Chitosan Nanoparticles and Its Application in Non-Parenteral Drug Delivery. Pharmaceutics 2017, 9, 53. [Google Scholar] [CrossRef] [Green Version]
- Garg, U.; Chauhan, S.; Nagaich, U.; Jain, N. Current Advances in Chitosan Nanoparticles Based Drug Delivery and Targeting. Adv. Pharm. Bull. 2019, 9, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Mazzarino, L.; Loch-Neckel, G.; Bubniak, L.D.S.; Mazzucco, S.; Santos-Silva, M.C.; Borsali, R.; Lemos-Senna, E. Curcumin-Loaded Chitosan-Coated Nanoparticles as a New Approach for the Local Treatment of Oral Cavity Cancer. J. Nanosci. Nanotechnol. 2015, 15, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Pornpitchanarong, C.; Rojanarata, T.; Opanasopit, P.; Ngawhirunpat, T.; Patrojanasophon, P. Catechol-modified chitosan/hyaluronic acid nanoparticles as a new avenue for local delivery of doxorubicin to oral cancer cells. Colloids Surf. B Biointerfaces 2020, 196, 111279. [Google Scholar] [CrossRef]
- Wang, Z.-Q.; Liu, K.; Huo, Z.-J.; Li, X.-C.; Wang, M.; Liu, P.; Pang, B.; Wang, S.-J. A cell-targeted chemotherapeutic nanomedicine strategy for oral squamous cell carcinoma therapy. J. Nanobiotechnology 2015, 13, 63. [Google Scholar] [CrossRef] [Green Version]
- Sohail, M.F.; Hussain, S.Z.; Saeed, H.; Javed, I.; Sarwar, H.S.; Nadhman, A.; Huma, Z.-E.; Rehman, M.; Jahan, S.; Hussain, I.; et al. Polymeric nanocapsules embedded with ultra-small silver nanoclusters for synergistic pharmacology and improved oral delivery of Docetaxel. Sci. Rep. 2018, 8, 13304. [Google Scholar] [CrossRef] [Green Version]
- Darwish, W.M.; Abdoon, A.S.; Shata, M.S.; Elmansy, M. Vincristine-loaded polymeric corona around gold nanorods for combination (chemo-photothermal) therapy of oral squamous carcinoma. React. Funct. Polym. 2020, 151, 104575. [Google Scholar] [CrossRef]
- El-Sayed, I.H.; Huang, X.; El-Sayed, M.A. Selective laser photo-thermal therapy of epithelial carcinoma using anti-EGFR antibody conjugated gold nanoparticles. Cancer Lett. 2006, 239, 129–135. [Google Scholar] [CrossRef]
- Karami, N.; Moghimipour, E.; Salimi, A. Liposomes as a novel drug delivery system: Fundamental and pharmaceutical ap-plication. Asian J. Pharm. 2018, 12, S31–S41. [Google Scholar] [CrossRef]
- Sah, A.K.; Vyas, A.; Suresh, P.K.; Gidwani, B. Application of nanocarrier-based drug delivery system in treatment of oral cancer. Artif. Cells Nanomed. Biotechnol. 2018, 46, 650–657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorain, B.; Al-Dhubiab, B.E.; Nair, A.; Kesharwani, P.; Pandey, M.; Choudhury, H. Multivesicular Liposome: A Lipid-based Drug Delivery System for Efficient Drug Delivery. Curr. Pharm. Des. 2021, 27, 4404–4415. [Google Scholar] [CrossRef]
- Erjavec, V.; Pavlica, Z.; Sentjurc, M.; Petelin, M. In vivo study of liposomes as drug carriers to oral mucosa using EPR oximetry. Int. J. Pharm. 2006, 307, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jin, B.; Dong, X.; Xu, X.; Zhang, F. Development and in�vitro evaluation of mucoadhesive patches of methotrexate for targeted delivery in oral cancer. Oncol. Lett. 2017, 15, 2541–2549. [Google Scholar] [CrossRef] [PubMed]
- Shtenberg, Y.; Goldfeder, M.; Prinz, H.; Shainsky, J.; Ghantous, Y.; Abu El-Naaj, I.; Schroeder, A.; Bianco-Peled, H. Mucoadhesive alginate pastes with embedded liposomes for local oral drug delivery. Int. J. Biol. Macromol. 2018, 111, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, M.; Dudhe, R.; Sharma, P.K. Nanoemulsion: An advanced mode of drug delivery system. 3 Biotech 2015, 5, 123–127. [Google Scholar] [CrossRef] [Green Version]
- Chavda, V.P. Nanobased Nano Drug Delivery. In Applications of Targeted Nano Drugs and Delivery Systems; Elsevier: Amsterdam, The Netherlands, 2018; pp. 69–92. [Google Scholar]
- Choudhury, H.; Gorain, B.; Chatterjee, B.; Mandal, U.K.; Sengupta, P.; Tekade, R.K. Pharmacokinetic and Phar-macodynamic Features of Nanoemulsion Following Oral, Intravenous, Topical and Nasal Route. Curr. Pharm. Des. 2016, 23, 2504–2531. [Google Scholar]
- Srivastava, S.; Mohammad, S.; Pant, A.B.; Mishra, P.R.; Pandey, G.; Gupta, S.; Farooqui, S. Co-delivery of 5-Fluorouracil and Curcumin Nanohybrid Formulations for Improved Chemotherapy Against Oral Squamous Cell Carcinoma. J. Maxillofac. Oral Surg. 2018, 17, 597–610. [Google Scholar] [CrossRef]
- Klang, V.; Matsko, N.B.; Valenta, C.; Hofer, F. Electron microscopy of nanoemulsions: An essential tool for characterisation and stability assessment. Micron 2012, 43, 85–103. [Google Scholar] [CrossRef]
- Mohamadi, L.; Bazrafshan, E.; Noroozifar, M.; Ansari-Moghaddam, A.; Barahuie, F.; Balarak, D. Adsorptive Removal of Benzene and Toluene from Aqueous Environments by Cupric Oxide Nanoparticles: Kinetics and Isotherm Studies. J. Chem. 2017, 2017, 2069519. [Google Scholar] [CrossRef] [Green Version]
- Ramana, L.N.; Sethuraman, S.; Ranga, U.; Krishnan, U.M. Development of a liposomal nanodelivery system for nevirapine. J. Biomed. Sci. 2010, 17, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]


 ) paste; (
) paste; (  ) cross-linked paste on porcine tongue. Reprinted from ref. [88] with permission from Elsevier (2018).
) cross-linked paste on porcine tongue. Reprinted from ref. [88] with permission from Elsevier (2018).
 ) paste; (
) paste; (  ) cross-linked paste on porcine tongue. Reprinted from ref. [88] with permission from Elsevier (2018).
) cross-linked paste on porcine tongue. Reprinted from ref. [88] with permission from Elsevier (2018).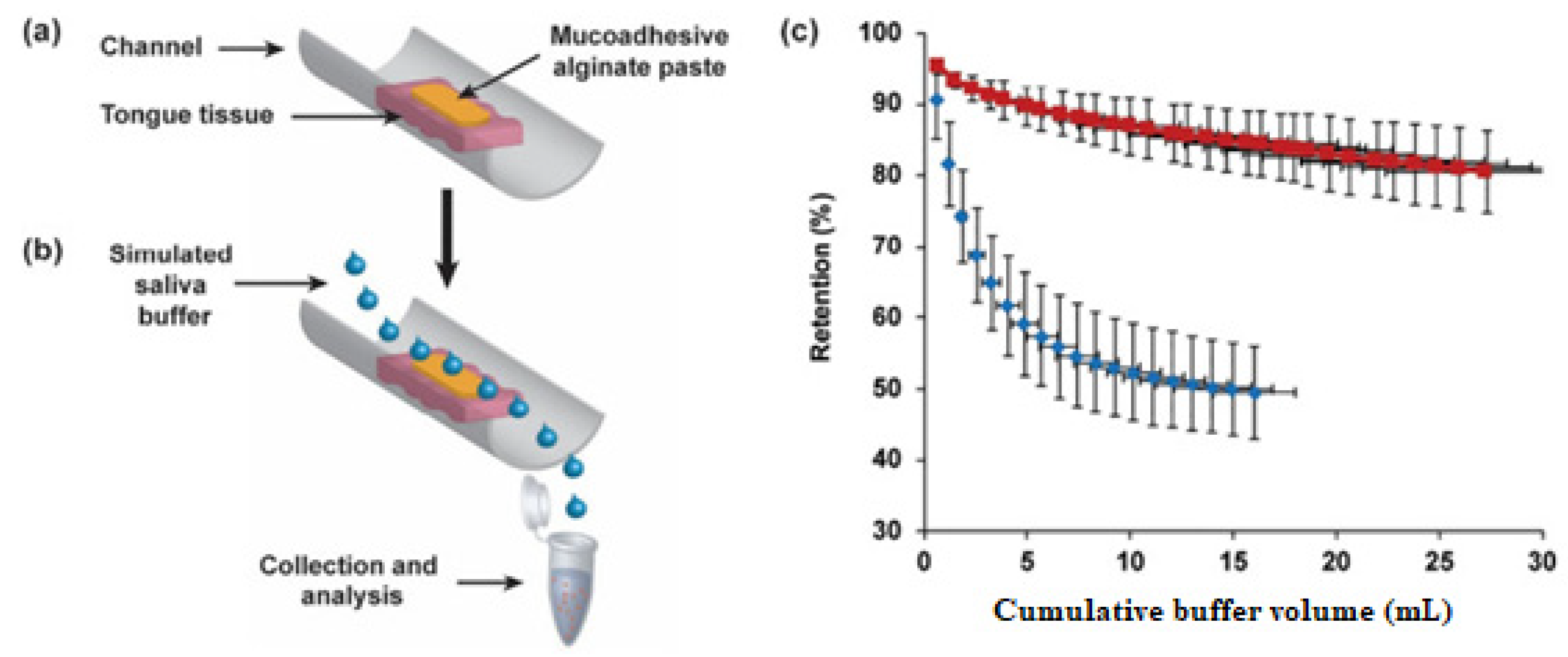
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pandey, M.; Choudhury, H.; Ying, J.N.S.; Ling, J.F.S.; Ting, J.; Ting, J.S.S.; Zhia Hwen, I.K.; Suen, H.W.; Samsul Kamar, H.S.; Gorain, B.; et al. Mucoadhesive Nanocarriers as a Promising Strategy to Enhance Intracellular Delivery against Oral Cavity Carcinoma. Pharmaceutics 2022, 14, 795. https://doi.org/10.3390/pharmaceutics14040795
Pandey M, Choudhury H, Ying JNS, Ling JFS, Ting J, Ting JSS, Zhia Hwen IK, Suen HW, Samsul Kamar HS, Gorain B, et al. Mucoadhesive Nanocarriers as a Promising Strategy to Enhance Intracellular Delivery against Oral Cavity Carcinoma. Pharmaceutics. 2022; 14(4):795. https://doi.org/10.3390/pharmaceutics14040795
Chicago/Turabian StylePandey, Manisha, Hira Choudhury, Jenifer Ngu Shao Ying, Jessica Foo Sze Ling, Jong Ting, Jocelyn Su Szhiou Ting, Ivory Kuek Zhia Hwen, Ho Wan Suen, Hazimah Syazwani Samsul Kamar, Bapi Gorain, and et al. 2022. "Mucoadhesive Nanocarriers as a Promising Strategy to Enhance Intracellular Delivery against Oral Cavity Carcinoma" Pharmaceutics 14, no. 4: 795. https://doi.org/10.3390/pharmaceutics14040795
APA StylePandey, M., Choudhury, H., Ying, J. N. S., Ling, J. F. S., Ting, J., Ting, J. S. S., Zhia Hwen, I. K., Suen, H. W., Samsul Kamar, H. S., Gorain, B., Jain, N., & Mohd Amin, M. C. I. (2022). Mucoadhesive Nanocarriers as a Promising Strategy to Enhance Intracellular Delivery against Oral Cavity Carcinoma. Pharmaceutics, 14(4), 795. https://doi.org/10.3390/pharmaceutics14040795