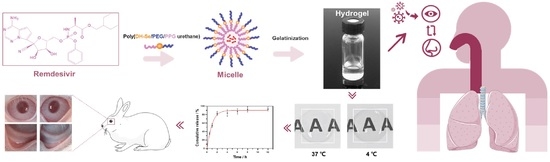
Thermosensitive Poly(DHSe/PEG/PPG Urethane)-Based Hydrogel Extended Remdesivir Application in Ophthalmic Medication
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Synthesis of Poly(DHSe/PEG/PPG Urethane)
2.3. Molecular Characterization
2.4. Determination of Thermal Properties
2.5. Determination of Rheological Properties
2.6. Determination of Sol-Gel Phase Transition
2.7. Cryo-Scanning Electron Microscopy
2.8. Preparation of RDV-Loaded Poly(DHSe/PEG/PPG Urethane) Hydrogel
2.9. Determination of Light Transmittance
2.10. In Vitro Drug Release Study
2.11. Determination of Precorneal Fluorescent Dye Retention
2.12. Imaging of Optical Coherence Tomography
2.13. Measurement of RDV Penetration in Ocular Tissues
2.14. Cell Culture
2.15. Evaluation of Cytotoxicity
2.16. Evaluation of Rabbit Eye Irritation
2.17. Histological Analysis
2.18. Assay of Surface Plasmon Resonance
3. Results and Discussion
3.1. Synthesis and Characterization of Poly(DHSe/PEG/PPG Urethane)
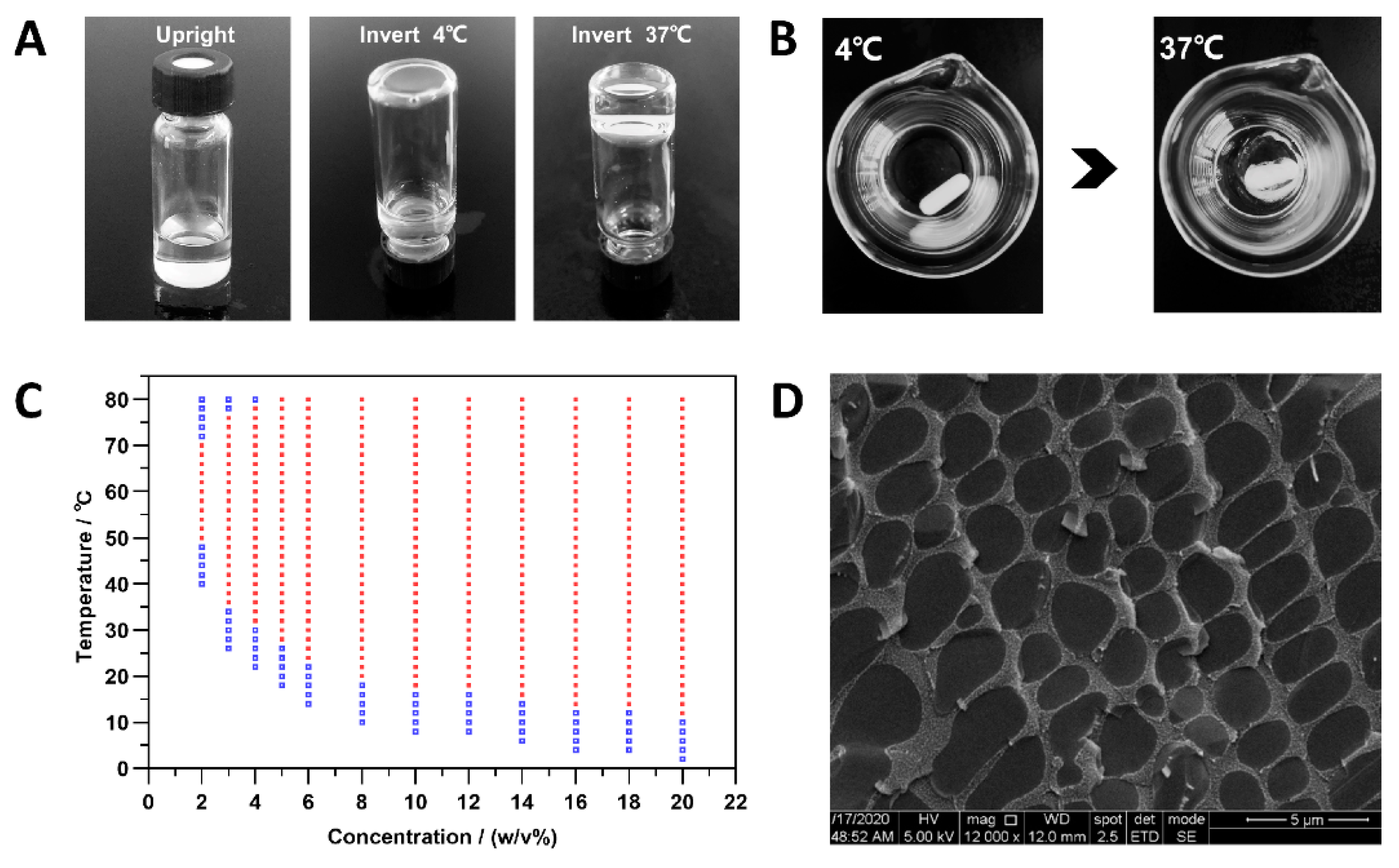
3.2. Sol-Gel Phase Transition
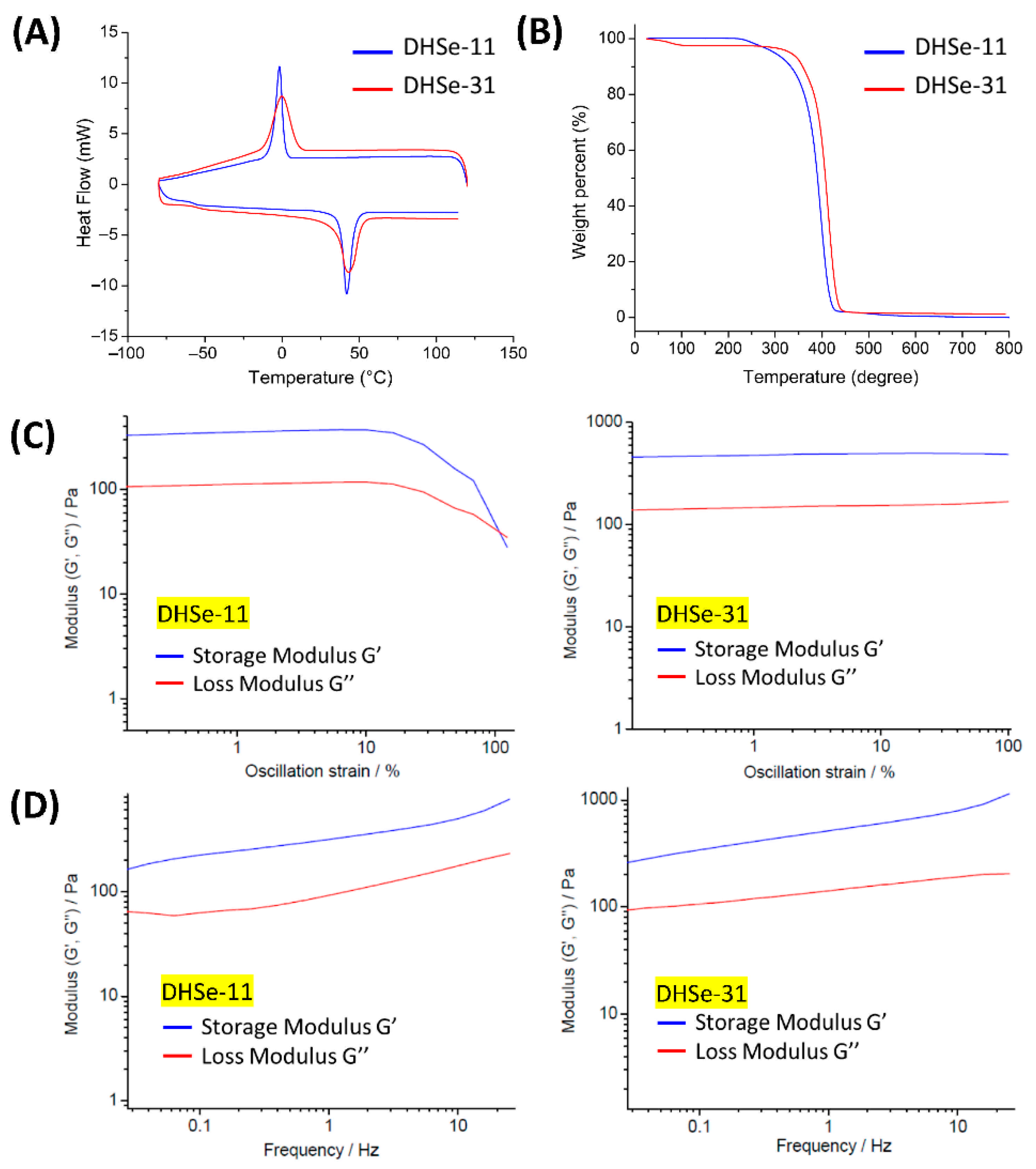
3.3. Thermal and Rheological Properties
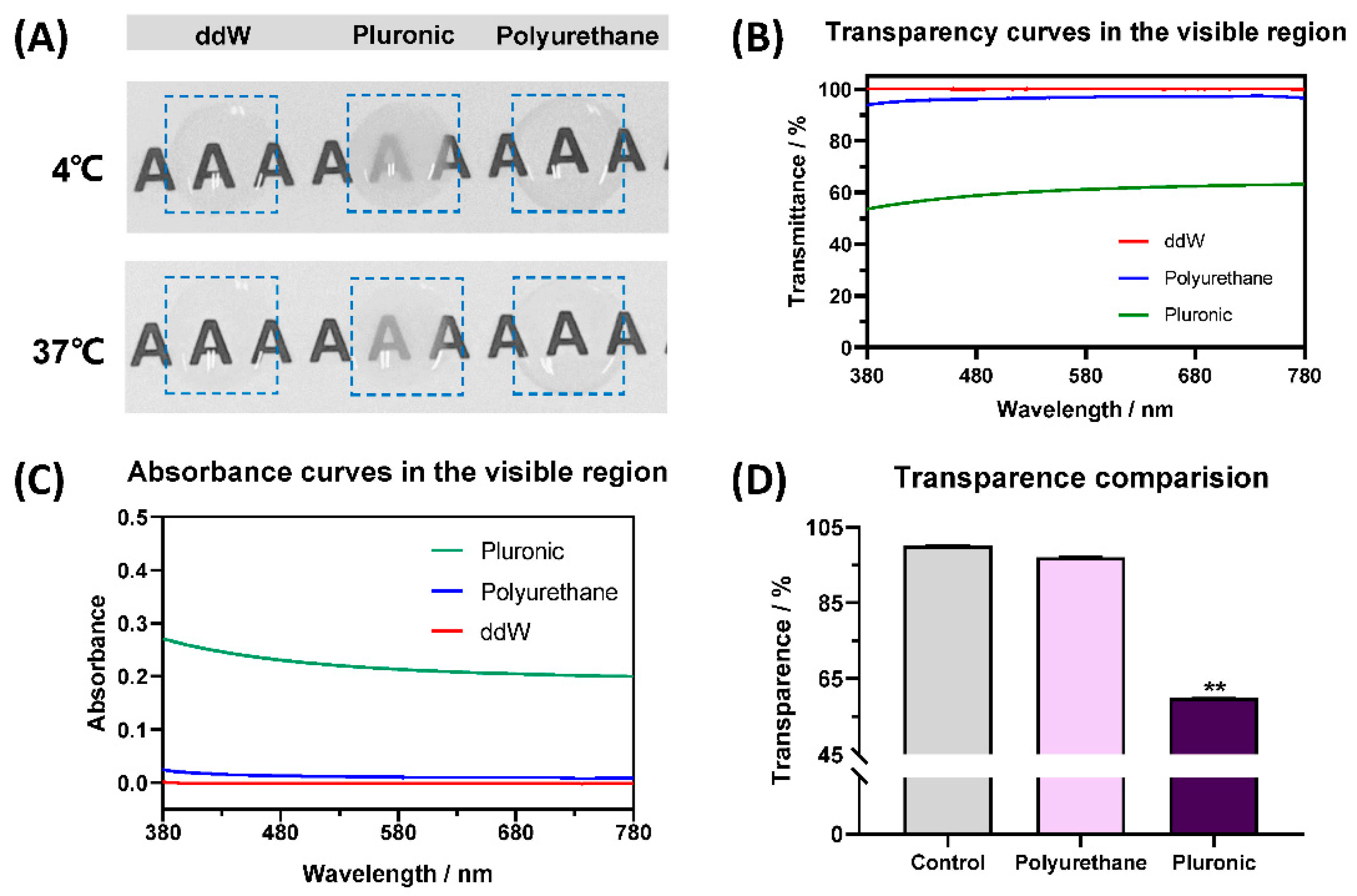
3.4. Transparency of RDV/Poly(DHSe/PEG/PPG Urethane) Hydrogel
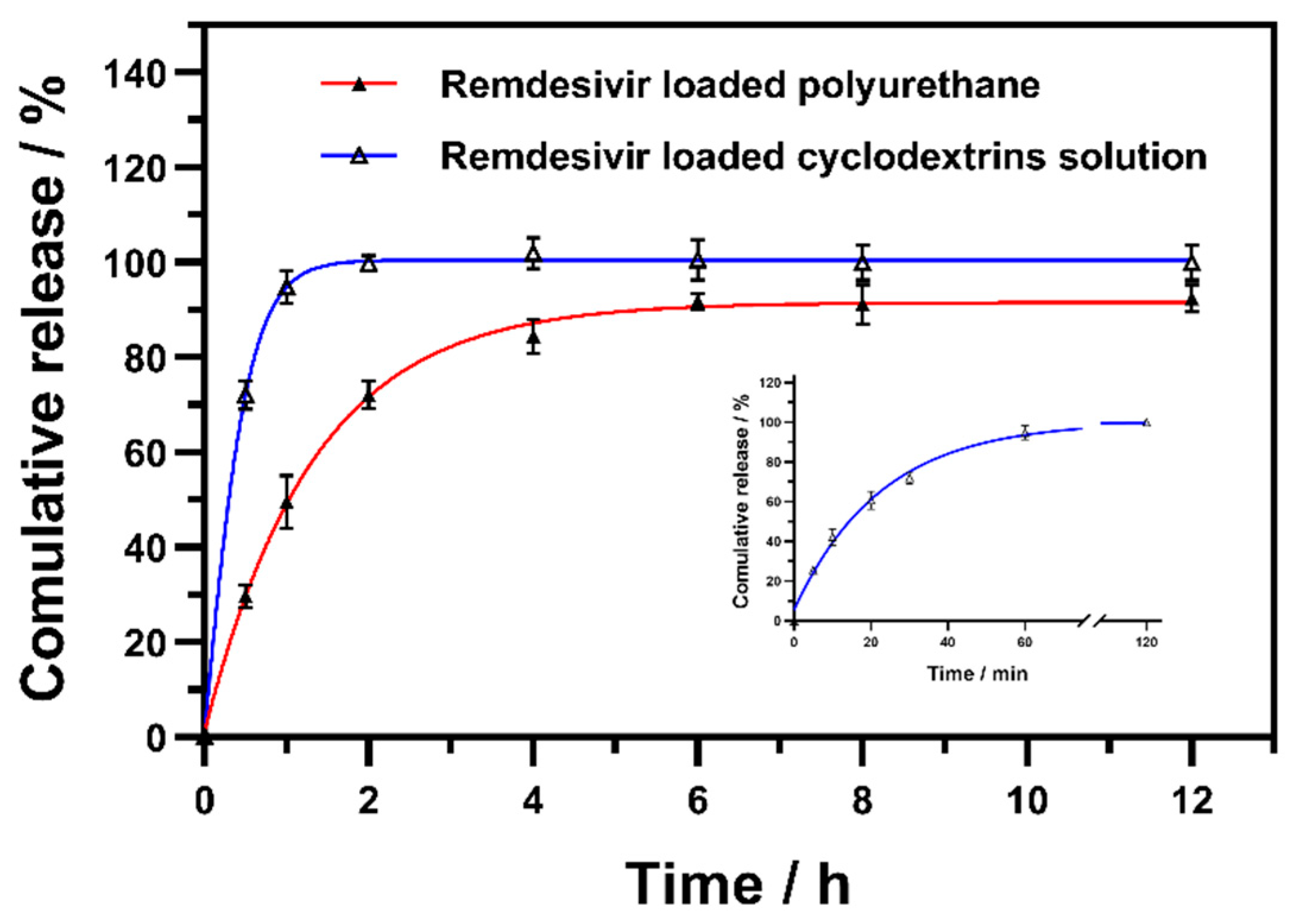
3.5. In Vitro RDV Release Behavior
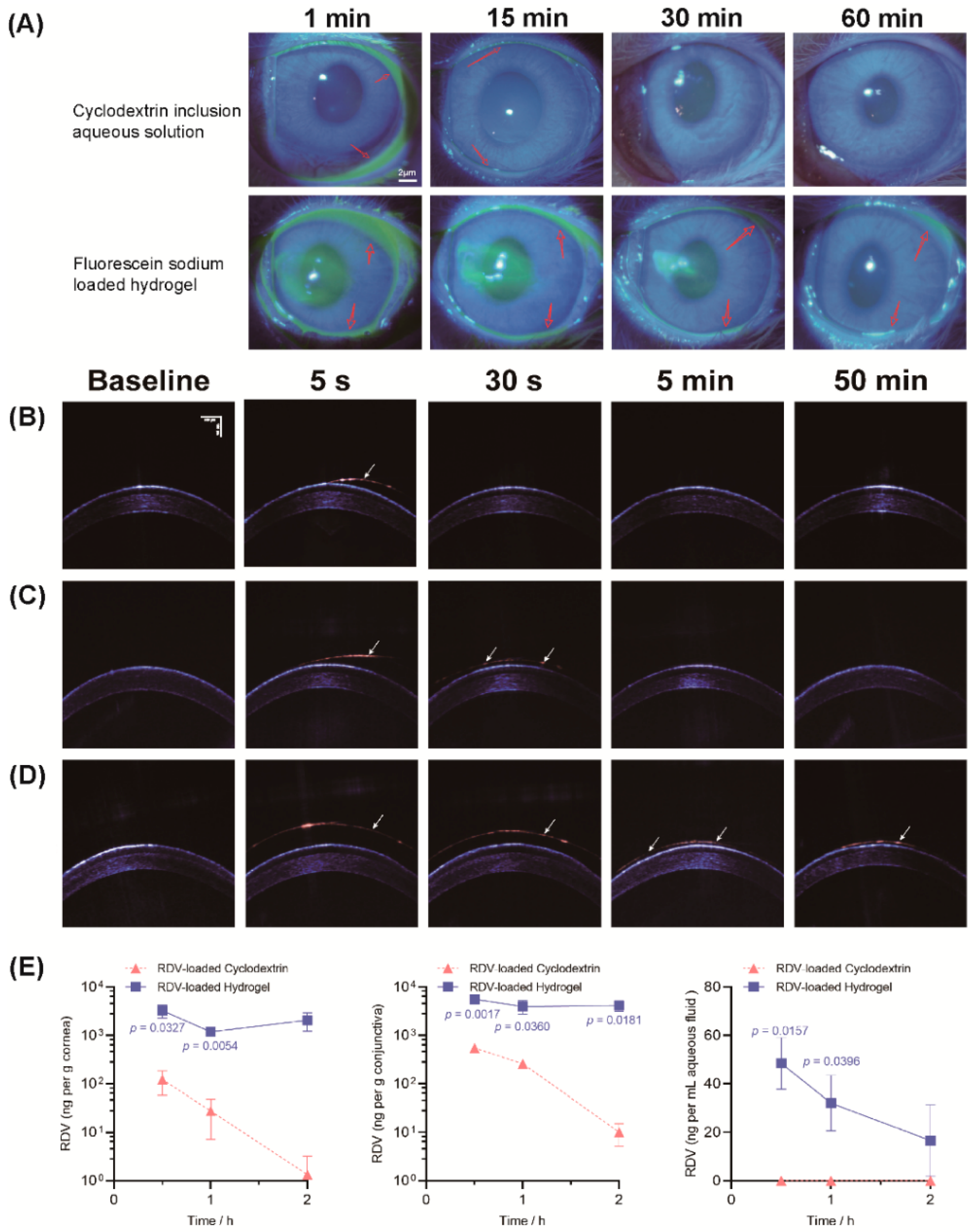
3.6. Drug Retention and Penetration Test
3.7. In Vitro Cytotoxicity
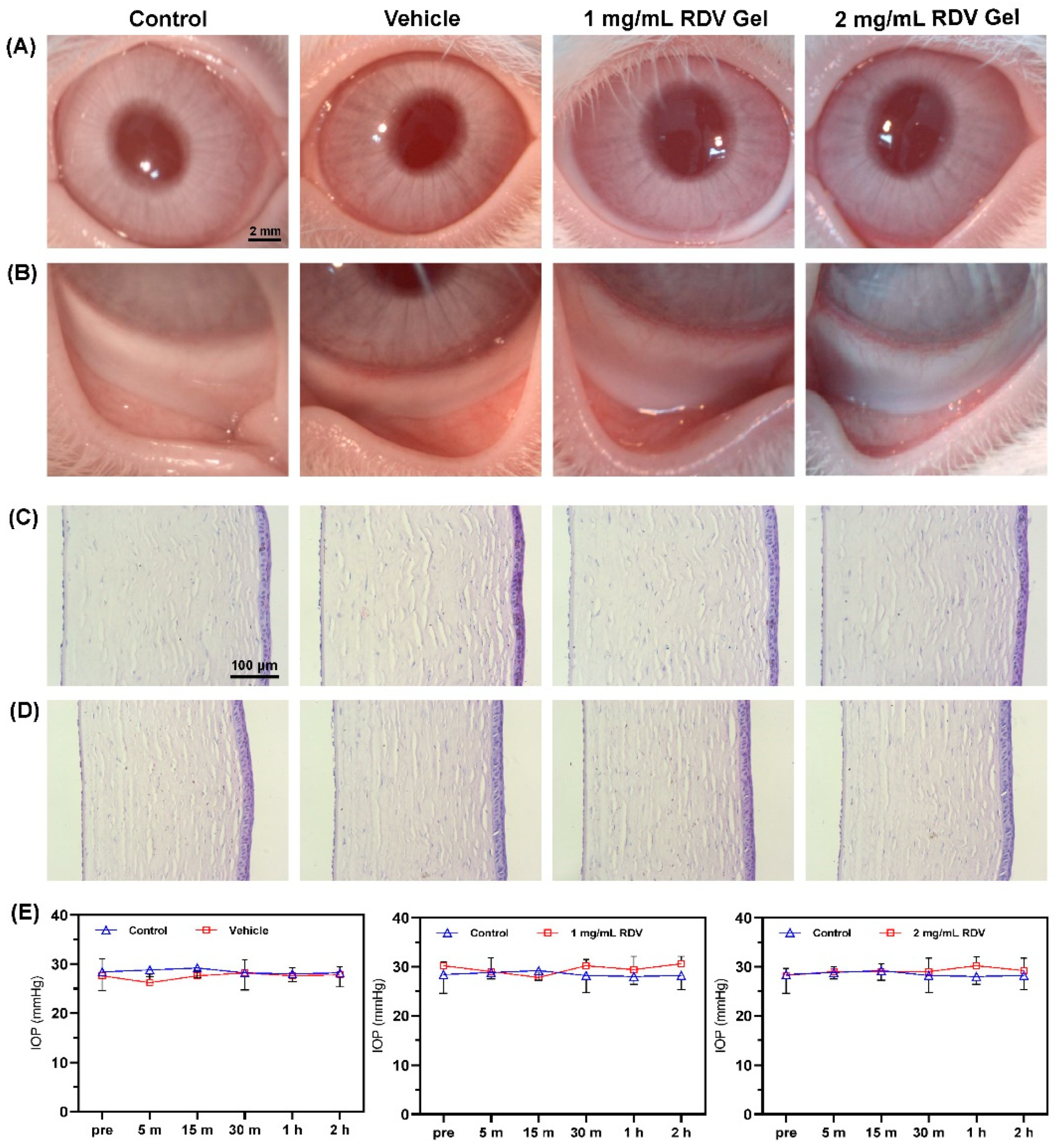
3.8. Ocular Irritation and Histological Evaluation
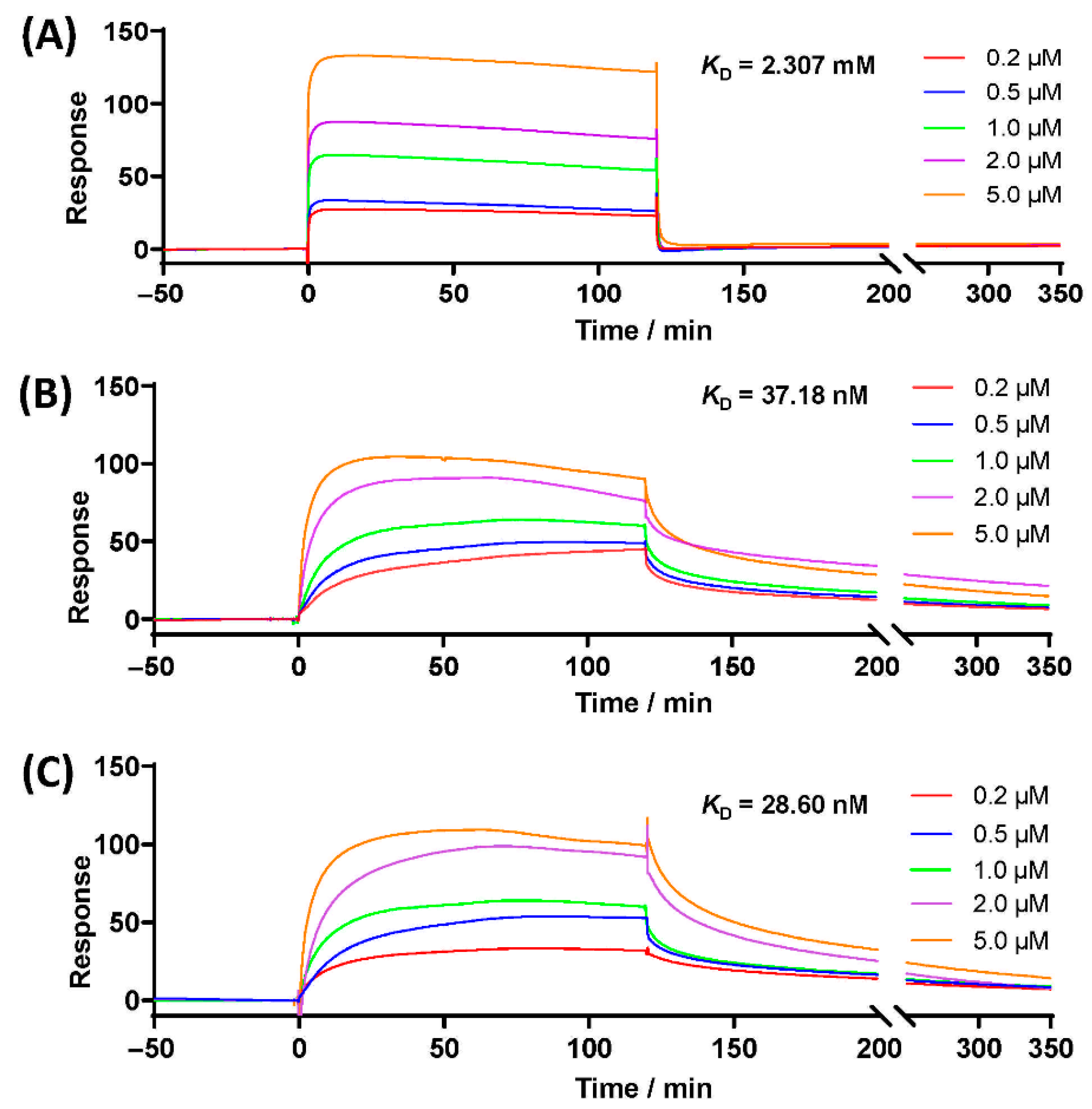
3.9. SPR Analysis with Spike Glycoprotein
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guo, Y.-R.; Cao, Q.-D.; Hong, Z.-S.; Tan, Y.-Y.; Chen, S.-D.; Jin, H.-J.; Tan, K.-S.; Wang, D.-Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status. Mil. Med. Res. 2020, 7, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kesson, A. Respiratory virus infections. Paediatr. Respir. Rev. 2007, 8, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Belser, J.A.; Maines, T.R.; Tumpey, T.M.; Katz, J.M. Influenza A virus transmission: Contributing factors and clinical implications. Expert Rev. Mol. Med. 2010, 12, e39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belser, J.; Rota, P.; Tumpey, T. Ocular tropism of respiratory viruses. Microbiol. Mol. Biol. Rev. 2013, 77, 144–156. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Yu, H.; Mei, T.; Chen, B.; Chen, L.; Li, S.; Zhang, X.; Sun, X. SARS-CoV-2 on the ocular surface: Is it truly a novel transmission route? Br. J. Ophthalmol. 2020, 105, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Napoli, P.; Nioi, M.; D’Aloja, E.; Fossarello, M. The Ocular Surface and the Coronavirus Disease 2019: Does a Dual ‘Ocular Route’ Exist? J. Clin. Med. 2020, 9, 1269. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Xu, Z.; Castiglione, G.M.; Soiberman, U.S.; Eberhart, C.G.; Duh, E.J. ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection. Ocul. Surf. 2020, 18, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.M.; Parab, S.R.; Paranjape, M. Repurposing 0.5% povidone iodine solution in otorhinolaryngology practice in Covid 19 pandemic. Am. J. Otolaryngol. 2020, 41, 102618. [Google Scholar] [CrossRef] [PubMed]
- Kronbichler, A.; Effenberger, M.; Eisenhut, M.; Lee, K.H.; Shin, J.I. Seven recommendations to rescue the patients and reduce the mortality from COVID-19 infection: An immunological point of view. Autoimmun. Rev. 2020, 19, 102570. [Google Scholar] [CrossRef]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; Mehta, A.K.; Zingman, B.S.; Kalil, A.C.; Hohmann, E.; Chu, H.Y.; Luetkemeyer, A.; Kline, S.; et al. Remdesivir for the Treatment of COVID-19—Preliminary report. N. Engl. J. Med. 2020, 383, 1813–1826. [Google Scholar] [CrossRef]
- Choy, K.T.; Wong, A.Y.; Kaewpreedee, P.; Sia, S.F.; Chen, D.; Hui, K.P.Y.; Chu, D.K.W.; Chan, M.C.W.; Cheung, P.P.; Huang, X.; et al. Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro. Antivir. Res. 2020, 178, 104786. [Google Scholar] [CrossRef]
- Choi, S.W.; Shin, J.S.; Park, S.J.; Jung, E.; Park, Y.G.; Lee, J.; Kim, S.J.; Park, H.J.; Lee, J.H.; Park, S.M.; et al. Antiviral activity and safety of remdesivir against SARS-CoV-2 infection in human pluripotent stem cell-derived cardiomyocytes. Antivir. Res. 2020, 184, 104955. [Google Scholar] [CrossRef]
- Xie, J.; Wang, Z. Can remdesivir and its parent nucleoside GS-441524 be potential oral drugs? An in vitro and in vivo DMPK assessment. Acta Pharm. Sin. B 2021, 11, 1607–1616. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhao, H.; Okeke, C.I.; Li, L.; Liu, Z.; Yin, Z.; Zhuang, P.; Sun, J.; Wu, T.; Wang, M.; et al. Comparison of systemic absorption between ofloxacin ophthalmic in situ gels and ofloxacin conventional ophthalmic solutions administration to rabbit eyes by HPLC–MS/MS. Int. J. Pharm. 2013, 450, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, A.; Takahashi, K.; Hirashima, M.; Kawakita, T.; Tsubota, K. Selenoprotein P Controls Oxidative Stress in Cornea. PLoS ONE 2010, 5, e9911. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, A. Development of New Pharmaceutical Candidates with Antioxidant Activity for the Treatment of Corneal Disorders. Cornea 2019, 38, S45–S49. [Google Scholar] [CrossRef] [PubMed]
- Loh, X.J.; Tan, Y.X.; Li, Z.; Teo, L.S.; Goh, S.H.; Li, J. Biodegradable thermogelling poly(ester urethane)s consisting of poly(lactic acid)—Thermodynamics of micellization and hydrolytic degradation. Biomaterials 2008, 29, 2164–2172. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.; Jiang, L.; Yang, S.; Li, Z.; Soh, W.M.W.; Zheng, L.; Loh, X.J.; Wu, Y. Light-Induced Redox-Responsive Smart Drug Delivery System by Using Selenium-Containing Polymer@MOF Shell/Core Nanocomposite. Adv. Heal. Mater. 2019, 8, e1900406. [Google Scholar] [CrossRef]
- Gao, J.; Wu, S.; Emge, T.J.; Rogers, M.A. Nanoscale and microscale structural changes alter the critical gelator concentration of self-assembled fibrillar networks. CrystEngComm 2013, 15, 4507–4515. [Google Scholar] [CrossRef]
- Qi, H.; Chen, W.; Huang, C.; Li, L.; Chen, C.; Li, W.; Wu, C. Development of a poloxamer analogs/carbopol-based in situ gelling and mucoadhesive ophthalmic delivery system for puerarin. Int. J. Pharm. 2007, 337, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Wang, Y.; Bao, Z.; Lin, D.; Liu, H.; Yu, A.; Lei, L.; Li, X.; Xu, X. Thermosensitive glycol chitosan-based hydrogel as a topical ocular drug delivery system for enhanced ocular bioavailability. Int. J. Pharm. 2019, 570, 118688. [Google Scholar] [CrossRef] [PubMed]
- Hua, S. Comparison of in vitro dialysis release methods of loperamide-encapsulated liposomal gel for topical drug delivery. Int. J. Nanomed. 2014, 9, 735–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, Y.; Xu, C.; Shi, H.; Yu, F.; Zhong, Y.; Liu, Z.; Loh, X.J.; Wu, Y.-L.; Li, Z.; Li, C. Engineered bio-adhesive polyhedral oligomeric silsesquioxane hybrid nanoformulation of amphotericin B for prolonged therapy of fungal keratitis. Chem. Eng. J. 2021, 421, 129734. [Google Scholar] [CrossRef]
- Avataneo, V.; de Nicolò, A.; Cusato, J.; Antonucci, M.; Manca, A.; Palermiti, A.; Waitt, C.; Walimbwa, S.; Lamorde, M.; di Perri, G.; et al. Development and validation of a UHPLC-MS/MS method for quantification of the prodrug remdesivir and its metabolite GS-441524: A tool for clinical pharmacokinetics of SARS-CoV-2/COVID-19 and Ebola virus disease. J. Antimicrob. Chemother. 2020, 75, 1772–1777. [Google Scholar] [CrossRef]
- Liu, B.; Zhao, Y.; Zhu, T.; Gao, S.; Ye, K.; Zhou, F.; Qiu, D.; Wang, X.; Tian, Y.; Qu, X. Biphasic Double-Network Hydrogel With Compartmentalized Loading of Bioactive Glass for Osteochondral Defect Repair. Front. Bioeng. Biotechnol. 2020, 8, 752. [Google Scholar] [CrossRef] [PubMed]
- Aston, R.; Sewell, K.; Klein, T.; Lawrie, G.; Grøndahl, L. Evaluation of the impact of freezing preparation techniques on the characterisation of alginate hydrogels by cryo-SEM. Eur. Polym. J. 2016, 82, 1–15. [Google Scholar] [CrossRef] [Green Version]


| Sample | Feed Ratio | Thermal Analysis | GPC | ||||
|---|---|---|---|---|---|---|---|
| PEG | PPG | Tma/°C | Tga/°C | Tdb/°C | Mn/Da | Đ | |
| DHSe-11 | 1 | 1 | 41.85 | −57.11 | 298 | 32,018 | 1.14 |
| DHSe-31 | 3 | 1 | 43.26 | −55.77 | 332 | 25,523 | 1.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, S.; Ke, L.; Zhao, S.; Li, Z.; Xiao, Y.; Wu, Y.; Ren, J.; Qiu, Y. Thermosensitive Poly(DHSe/PEG/PPG Urethane)-Based Hydrogel Extended Remdesivir Application in Ophthalmic Medication. Pharmaceutics 2022, 14, 50. https://doi.org/10.3390/pharmaceutics14010050
Xu S, Ke L, Zhao S, Li Z, Xiao Y, Wu Y, Ren J, Qiu Y. Thermosensitive Poly(DHSe/PEG/PPG Urethane)-Based Hydrogel Extended Remdesivir Application in Ophthalmic Medication. Pharmaceutics. 2022; 14(1):50. https://doi.org/10.3390/pharmaceutics14010050
Chicago/Turabian StyleXu, Sennan, Lingjie Ke, Sichen Zhao, Zhiguo Li, Yang Xiao, Yunlong Wu, Jie Ren, and Yan Qiu. 2022. "Thermosensitive Poly(DHSe/PEG/PPG Urethane)-Based Hydrogel Extended Remdesivir Application in Ophthalmic Medication" Pharmaceutics 14, no. 1: 50. https://doi.org/10.3390/pharmaceutics14010050
APA StyleXu, S., Ke, L., Zhao, S., Li, Z., Xiao, Y., Wu, Y., Ren, J., & Qiu, Y. (2022). Thermosensitive Poly(DHSe/PEG/PPG Urethane)-Based Hydrogel Extended Remdesivir Application in Ophthalmic Medication. Pharmaceutics, 14(1), 50. https://doi.org/10.3390/pharmaceutics14010050