Clinical Efficacy and Nephrotoxicity of the Loading Dose Colistin for the Treatment of Carbapenem-Resistant Acinetobacter baumannii in Critically Ill Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Outcome Measurement
2.2. Antimicrobial Susceptibility Testing
2.3. Statistical Analysis
3. Results
Risk Factors Associated with Nephrotoxicity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Munoz-Price, L.S.; Weinstein, R.A. Acinetobacter infection. N. Engl. J. Med. 2008, 358, 1271–1281. [Google Scholar] [CrossRef] [PubMed]
- Peleg, A.Y.; Seifert, H.; Paterson, D.L. Acinetobacter baumannii: Emergence of a Successful Pathogen. Clin. Microbiol. Rev. 2008, 21, 538–582. [Google Scholar] [CrossRef]
- Kohlenberg, A.; Brümmer, S.; Higgins, P.; Sohr, D.; Piening, B.C.; De Grahl, C.; Halle, E.; Rüden, H.; Seifert, H. Outbreak of carbapenem-resistant Acinetobacter baumannii carrying the carbapenemase OXA-23 in a German university medical centre. J. Med. Microbiol. 2009, 58, 1499–1507. [Google Scholar] [CrossRef] [PubMed]
- Garlantézec, R.; Bourigault, C.; Boles, J.; Prat, G.; Baron, R.; Tonnelier, J.; Cosse, M.; Lefèvre, M.; Jourdain, S.; Lelay, G.; et al. Cost-analysis of an intensive care unit closure due to an imipenem-resistant oxa-23 Acinetobacter baumannii outbreak. J. Hosp. Infect. 2011, 77, 174–175. [Google Scholar] [CrossRef]
- Ayraud-Thévenot, S.; Huart, C.; Mimoz, O.; Taouqi, M.; Laland, C.; Bousseau, A.; Castel, O. Control of multi-drug-resistant Acinetobacter baumannii outbreaks in an intensive care unit: Feasibility and economic impact of rapid unit closure. J. Hosp. Infect. 2012, 82, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Molter, G.; Seifert, H.; Mandraka, F.; Kasper, G.; Weidmann, B.; Hornei, B.; Öhler, M.; Schwimmbeck, P.G.; Kröschel, P.; Higgins, P.; et al. Outbreak of carbapenem-resistant Acinetobacter baumannii in the intensive care unit: A multi-level strategic management approach. J. Hosp. Infect. 2016, 92, 194–198. [Google Scholar] [CrossRef]
- Blot, S.; Vandewoude, K.; Colardyn, F. Nosocomial bacteremia involving Acinetobacter baumannii in critically ill patients: A matched cohort study. Intensiv. Care Med. 2003, 29, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Garnacho, J.; Sole-Violan, J.; Sa-Borges, M.; Diaz, E.; Rello, J. Clinical impact of pneumonia caused by Acinetobacter baumannii in intubated patients: A matched cohort study. Crit. Care Med. 2003, 31, 2478–2482. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Kopterides, P.; Siempos, I.I. Attributable mortality of Acinetobacter baumannii infection among critically ill patients. Clin. Infect. Dis. 2006, 43, 389. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.L.; Clancy, M.; Honnold, C.; Singh, S.; Snesrud, E.; Onmus-Leone, F.; Mc Gann, P.; Ong, A.C.; Kwak, Y.; Waterman, P.; et al. Fatal Outbreak of an Emerging Clone of Extensively Drug-Resistant Acinetobacter baumannii With Enhanced Virulence. Clin. Infect. Dis. 2015, 61, 145–154. [Google Scholar] [CrossRef]
- Grégoire, N.; Mimoz, O.; Mégarbane, B.; Comets, E.; Chatelier, D.; Lasocki, S.; Gauzit, R.; Balayn, D.; Gobin, P.; Marchand, S.; et al. New Colistin population pharmacokinetic data in critically Ill patients suggesting an alternative loading dose rationale. Antimicrob. Agents Chemother. 2014, 58, 7324–7330. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.F.; Karaiskos, I.; Plachouras, D.; Karvanen, M.; Pontikis, K.; Jansson, B.; Papadomichelakis, E.; Antoniadou, A.; Giamarellou, H.; Armaganidis, A.; et al. Application of a Loading Dose of Colistin Methanesulfonate in Critically Ill Patients: Population Pharmacokinetics, Protein Binding, and Prediction of Bacterial Kill. Antimicrob. Agents Chemother. 2012, 56, 4241–4249. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, B.T.; Pogue, J.M.; Zavascki, A.P.; Paul, M.; Daikos, G.L.; Forrest, A.; Giacobbe, D.R.; Viscoli, C.; Giamarellou, H.; Karaiskos, I.; et al. International Consensus Guidelines for the Optimal Use of the Polymyxins: Endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy 2019, 39, 10–39. [Google Scholar] [CrossRef] [PubMed]
- Horan, T.C.; Andrus, M.; Dudeck, M.A. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am. J. Infect. Control 2008, 36, 309–332. [Google Scholar] [CrossRef]
- Ricci, Z.; Cruz, D.; Ronco, C. The RIFLE criteria and mortality in acute kidney injury: A systematic review. Kidney Int. 2008, 73, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: Twentieth Informational Supplement M100-S20; CLSI: Wayne, PA, USA, 2010. [Google Scholar]
- Ece, G.; Samlioglu, P.; Atalay, S.; Kose, S. Evaluation of the in vitro colistin susceptibility of Pseudomonas aeruginosa and Acinetobacter baumannii strains at a tertiary care centre in Western Turkey. Infez. Med. 2014, 22, 36–40. [Google Scholar]
- Bergen, P.J.; Bulitta, J.B.; Forrest, A.; Tsuji, B.T.; Li, J.; Nation, R.L. Pharmacokinetic/Pharmacodynamic Investigation of Colistin against Pseudomonas aeruginosa Using an In Vitro Model. Antimicrob. Agents Chemother. 2010, 54, 3783–3789. [Google Scholar] [CrossRef] [PubMed]
- Owen, R.J.; Li, J.; Nation, R.L.; Spelman, D. In vitro pharmacodynamics of colistin against Acinetobacter baumannii clinical isolates. J. Antimicrob. Chemother. 2007, 59, 473–477. [Google Scholar] [CrossRef]
- Zhou, Y.-F.; Liu, P.; Zhang, C.-J.; Liao, X.-P.; Sun, J.; Liu, Y.-H. Colistin combined with tigecycline: A promising alternative strategy to combat escherichia coli harboring blaNDM–5 and mcr-1. Front. Microbiol. 2020, 10, 2957. [Google Scholar] [CrossRef]
- Garonzik, S.M.; Li, J.; Thamlikitkul, V.; Paterson, D.; Shoham, S.; Jacob, J.; Silveira, F.P.; Forrest, A.; Nation, R.L. Population Pharmacokinetics of Colistin Methanesulfonate and Formed Colistin in Critically Ill Patients from a Multicenter Study Provide Dosing Suggestions for Various Categories of Patients. Antimicrob. Agents Chemother. 2011, 55, 3284–3294. [Google Scholar] [CrossRef]
- Dudhani, R.V.; Turnidge, J.D.; Coulthard, K.; Milne, R.W.; Rayner, C.R.; Li, J.; Nation, R.L. Elucidation of the pharmacokinetic/pharmacodynamic determinant of colistin activity against Pseudomonas aeruginosa in murine thigh and lung infection models. Antimicrob. Agents Chemother. 2010, 54, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Dalfino, L.; Puntillo, F.; Mosca, A.; Monno, R.; Spada, M.L.; Coppolecchia, S.; Miragliotta, G.; Bruno, F.; Brienza, N. High-Dose, Extended-Interval Colistin Administration in Critically Ill Patients: Is This the Right Dosing Strategy? A Preliminary Study. Clin. Infect. Dis. 2012, 54, 1720–1726. [Google Scholar] [CrossRef]
- Moni, M.; Sudhir, A.S.; Dipu, T.S.; Mohamed, Z.; Prabhu, B.P.; Edathadathil, F.; Balachandran, S.; Singh, S.K.; Prasanna, P.; Menon, V.P.; et al. Clinical efficacy and pharmacokinetics of colistimethate sodium and colistin in critically ill patients in an Indian hospital with high endemic rates of multidrug-resistant Gram-negative bacterial infections: A prospective observational study. Int. J. Infect. Dis. 2020, 100, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Trifi, A.; Abdellatif, S.; Daly, F.; Mahjoub, K.; Nasri, R.; Oueslati, M.; Mannai, R.; Bouzidi, M.; Ben Lakhal, S. Efficacy and Toxicity of High-Dose Colistin in Multidrug-Resistant Gram-Negative Bacilli Infections: A Comparative Study of a Matched Series. Chemotherapy 2016, 61, 190–196. [Google Scholar] [CrossRef]
- Gibson, G.A.; Bauer, S.R.; Neuner, E.A.; Bass, S.N.; Lam, S.W. Influence of colistin dose on global cure in patients with bacteremia due to carbapenem-resistant gram-negative bacilli. Antimicrob. Agents Chemother. 2016, 60, 431–436. [Google Scholar] [CrossRef][Green Version]
- Jung, S.; Chung, E.K.; Jun, M.S.; Son, E.S.; Rhie, S.J. Differences in Colistin Administration and Bacterial and Treatment Outcomes in Critically Ill Patients. Sci. Rep. 2019, 9, 1–11. [Google Scholar] [CrossRef]
- Bellos, I.; Pergialiotis, V.; Frountzas, M.; Kontzoglou, K.; Daskalakis, G.; Perrea, D.N. Efficacy and safety of colistin loading dose: A meta-analysis. J. Antimicrob. Chemother. 2020, 75, 1689–1698. [Google Scholar] [CrossRef]
- Falagas, M.E.; Rafailidis, P.I.; Ioannidou, E.; Alexiou, V.G.; Matthaiou, D.K.; Karageorgopoulos, D.E.; Kapaskelis, A.; Nikita, D.; Michalopoulos, A. Colistin therapy for microbiologically documented multidrug-resistant Gram-negative bacterial infections: A retrospective cohort study of 258 patients. Int. J. Antimicrob. Agents 2010, 35, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Karaiskos, I.; Giamarellou, H. Multidrug-resistant and extensively drug-resistant Gram-negative pathogens: Current and emerging therapeutic approaches. Expert Opin. Pharmacother. 2014, 15, 1351–1370. [Google Scholar] [CrossRef]
- Pogue, J.M.; Lee, J.; Marchaim, D.; Yee, V.; Zhao, J.J.; Chopra, T.; Lephart, P.; Kaye, K.S. Incidence of and Risk Factors for Colistin-Associated Nephrotoxicity in a Large Academic Health System. Clin. Infect. Dis. 2011, 53, 879–884. [Google Scholar] [CrossRef]
- Katip, W.; Meechoui, M.; Thawornwittayakom, P.; Chinwong, D.; Oberdorfer, P. Efficacy and Safety of High Loading Dose of Colistin in Multidrug-Resistant Acinetobacter baumannii: A Prospective Cohort Study. J. Intensiv. Care Med. 2019, 34, 996–1002. [Google Scholar] [CrossRef]
- Katip, W.; Uitrakul, S.; Oberdorfer, P. Clinical outcomes and nephrotoxicity of colistin loading dose for treatment of extensively drug-resistant Acinetobacter baumannii in cancer patients. Infect. Drug. Resist. 2017, 10, 293–298. [Google Scholar] [CrossRef]
- Giacobbe, D.R.; Saffioti, C.; Losito, A.R.; Rinaldi, M.; Aurilio, C.; Bolla, C.; Boni, S.; Borgia, G.; Carannante, N.; Cassola, G.; et al. Use of colistin in adult patients: A cross-sectional study. J. Glob. Antimicrob. Resist. 2020, 20, 43–49. [Google Scholar] [CrossRef]
| Characteristic | Non-LD CMS (n = 124) | LD CMS (n = 259) | p-Value |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 50 (40.32) | 94 (36.29) | 0.499 |
| Female | 74 (59.68) | 165 (63.71) | |
| Age, mean ± SD (year) | 65.71 ± 16.19 | 66.35 ± 16.06 | 0.717 |
| Duration of treatment ± SD (days) | 9.95 ± 6.22 | 8.91 ± 7.00 | 0.161 |
| Comorbidities * n (%) | 109 (87.90) | 234(90.35) | 0.478 |
| Hypertension | 66 (53.23) | 108(41.70) | 0.038 |
| Cardiovascular disease | 51 (41.13) | 76(29.46) | 0.028 |
| Diabetes mellitus | 37 (29.84) | 38 (14.67) | 0.001 |
| Chronic kidney disease | 56 (45.16) | 36(13.95) | 0.001 |
| Chronic obstructive pulmonary disease | 16(12.90) | 50(19.31) | 0.148 |
| Malignancy | 26 (20.97) | 70 (27.03) | 0.211 |
| Chronic liver disease | 8(6.45) | 17(6.59) | 1.000 |
| Septic shock, n (%) | 120 (96.77) | 242 (93.44) | 0.233 |
| Mechanical ventilation, n (%) | 115 (92.74) | 223 (86.10) | 0.063 |
| Charlson Score, mean ± SD | 4.88 ± 2.41 | 4.42 ± 2.20 | 0.066 |
| APACHE II score, mean ± SD | 13.57± 4.03 | 12.69 ± 4.22 | 0.054 |
| Baseline SCr, mg/dl, median (IQR) | 1.6 (0.9–2.7) | 1.0(0.5–1.9) | 0.003 |
| Baseline GFR, ml/min, median (IQR) | 38.75 (16.5–65.09) | 65.45 (29.08–100.47) | 0.001 |
| Total CMS dose, mean ± SD (g) | 1.61 ± 1.38 | 2.19 ± 1.49 | 0.001 |
| Type of nephrotoxic medications #, n (%) | |||
| Aminoglycosides | 4 (3.23) | 6 (2.32) | 0.733 |
| Diuretics | 91 (73.39) | 224 (86.49) | 0.003 |
| Amphotericin B | 14 (11.29) | 24 (9.27) | 0.585 |
| Vasopressor | 120 (96.77) | 242 (93.44) | 0.233 |
| Vancomycin | 88 (70.97) | 167 (64.48) | 0.247 |
| Length of hospital stay, mean ± SD (day) | 39.33 ± 26.69 | 37.66 ± 28.51 | 0.582 |
| Site of CRAB infection | |||
| Pneumonia | 108 (87.10) | 210 (81.08) | 0.149 |
| Bacteremia | 4 (3.23) | 14 (5.41) | 0.444 |
| UTI | 11 (8.87) | 36 (13.90) | 0.185 |
| Other | 5 (4.03) | 15 (5.79) | 0.625 |
| Colistin MICs, µg/mL, median (min-max) | 0.25 (0.084–1.5) | 0.25 (0.064–1.5) | 0.868 |
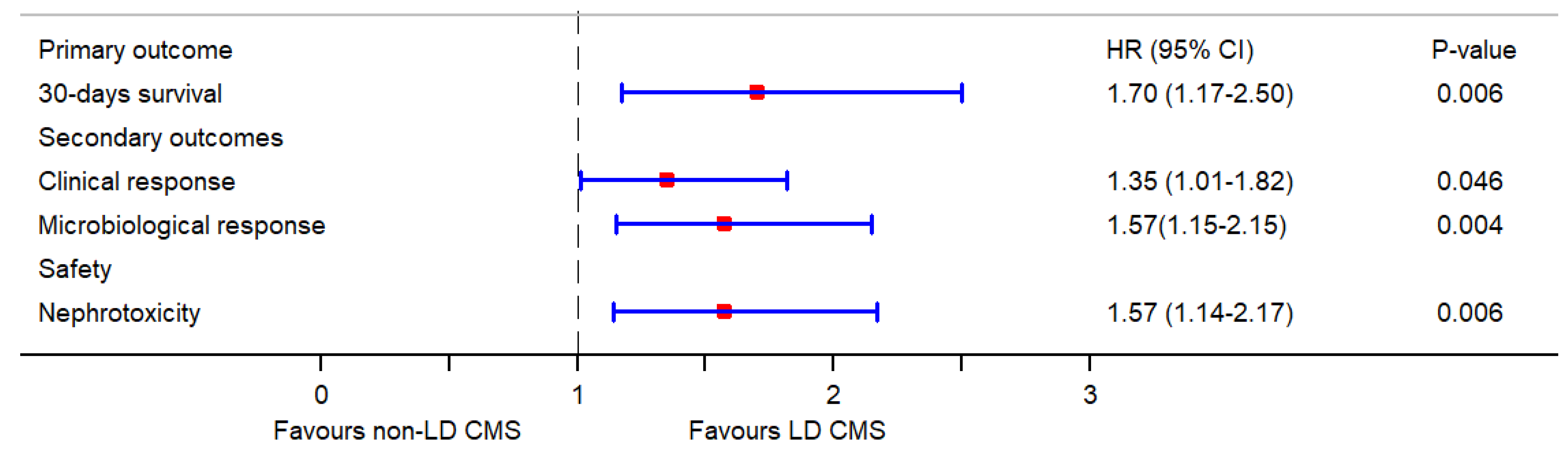
| Variable | Non-LD CMS (n = 124) | LD CMS (n = 259) | Crude HR (95% CI) | p-Value | Adjusted HR * (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Efficacy Primary outcome | ||||||
| 30 days survival | 47 (37.90) | 109 (42.08) | 1.35 (0.96–1.91) | 0.082 | 1.70 (1.17–2.50) | 0.006 |
| Secondary outcomes | ||||||
| Clinical response | 68 (54.84) | 143 (54.83) | 1.21 (0.91–1.62) | 0.189 | 1.35 (1.01–1.82) | 0.046 |
| Microbiological response | 67 (54.03) | 150 (57.91) | 1.30 (0.97–1.73) | 0.073 | 1.57(1.15–2.15) | 0.004 |
| Safety | ||||||
| Nephrotoxicity (RIFLE criteria) | 40 (32.26) | 147 (56.76) | 2.01 (1.47–2.85) | 0.001 | 1.57 (1.14–2.17) | 0.006 |
| 19 (15.32) | 44 (16.98) | ||||
| 9 (7.25) | 46 (17.76) | ||||
| 10 (8.06) | 56 (21.62) | ||||
| 1 (0.80) | 1 (0.38) | ||||
| 1(0.80) | 0 (0.00) |
| Variable a | Non-Nephrotoxicity (n = 188) | Nephrotoxicity (n = 187) | aHR (95% CI) | p Value |
|---|---|---|---|---|
| LD CMS | 112 (59.57) | 147 (78.61) | 1.70 (1.07–2.70) | 0.026 |
| Age ≥ 60 | 118 (62.77) | 141 (75.40) | 2.06 (1.96–2.17) | 0.001 |
| Male | 63 (33.51) | 77 (41.18) | 1.45 (1.29–1.63) | 0.001 |
| Vasopressor | 173 (92.02) | 181 (96.79) | 1.22 (1.11–1.34) | 0.001 |
| Amphotericin B | 16 (8.51) | 21 (11.23) | 1.08 (1.02–1.16) | 0.016 |
| APACHE II score | 14 (13–19) | 19 (15–22) | 1.03 (1.01–1.04) | 0.001 |
| Baseline GFR | 52.14 ± 25.66 | 46.20 ± 26.06 | 1.00 (1.00–1.01) | 0.144 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katip, W.; Uitrakul, S.; Oberdorfer, P. Clinical Efficacy and Nephrotoxicity of the Loading Dose Colistin for the Treatment of Carbapenem-Resistant Acinetobacter baumannii in Critically Ill Patients. Pharmaceutics 2022, 14, 31. https://doi.org/10.3390/pharmaceutics14010031
Katip W, Uitrakul S, Oberdorfer P. Clinical Efficacy and Nephrotoxicity of the Loading Dose Colistin for the Treatment of Carbapenem-Resistant Acinetobacter baumannii in Critically Ill Patients. Pharmaceutics. 2022; 14(1):31. https://doi.org/10.3390/pharmaceutics14010031
Chicago/Turabian StyleKatip, Wasan, Suriyon Uitrakul, and Peninnah Oberdorfer. 2022. "Clinical Efficacy and Nephrotoxicity of the Loading Dose Colistin for the Treatment of Carbapenem-Resistant Acinetobacter baumannii in Critically Ill Patients" Pharmaceutics 14, no. 1: 31. https://doi.org/10.3390/pharmaceutics14010031
APA StyleKatip, W., Uitrakul, S., & Oberdorfer, P. (2022). Clinical Efficacy and Nephrotoxicity of the Loading Dose Colistin for the Treatment of Carbapenem-Resistant Acinetobacter baumannii in Critically Ill Patients. Pharmaceutics, 14(1), 31. https://doi.org/10.3390/pharmaceutics14010031






