Anti-Melanogenic Mechanism of Tetrahydrocurcumin and Enhancing Its Topical Delivery Efficacy Using a Lecithin-Based Nanoemulsion
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. HaCaT Cell Culture and Cell Viability Studies
2.3. Measurement of Intracellular ROS in HaCaT
2.4. Measurement of α-MSH
2.5. B16F10 Cell Culture and Cytotoxicity Assay
2.6. Measurement of Melanin Content in B16F10 Cells
2.7. Measurement of Tyrosinase Activity in the B16F10 Cells
2.8. Real-Time Polymerase Chain Reaction (RT-PCR)
2.9. Western Blot Analysis
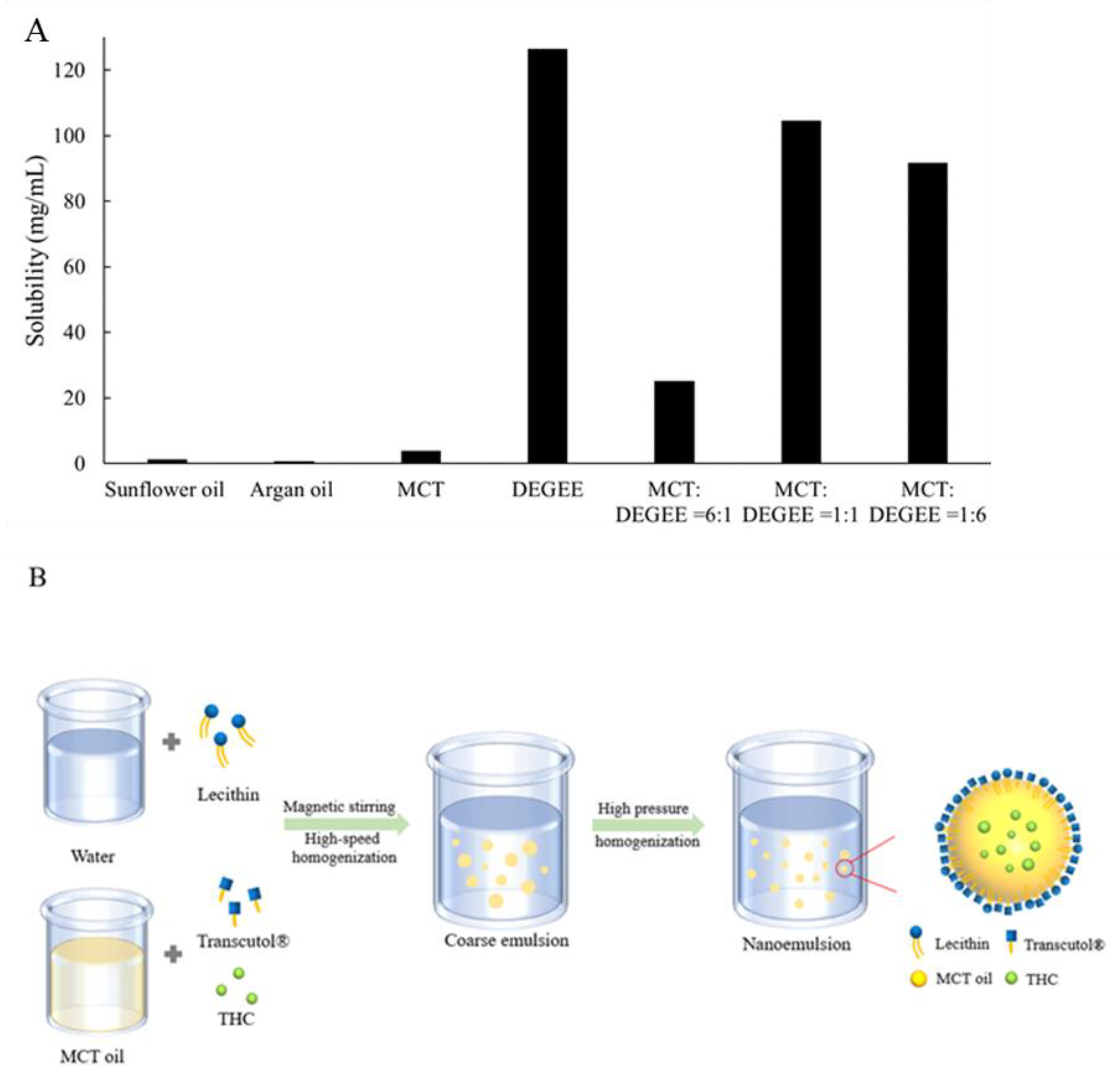
2.10. Determination of THC’s Solubility in Selected Solvents
2.11. Fabrication of the Nanoemulsion
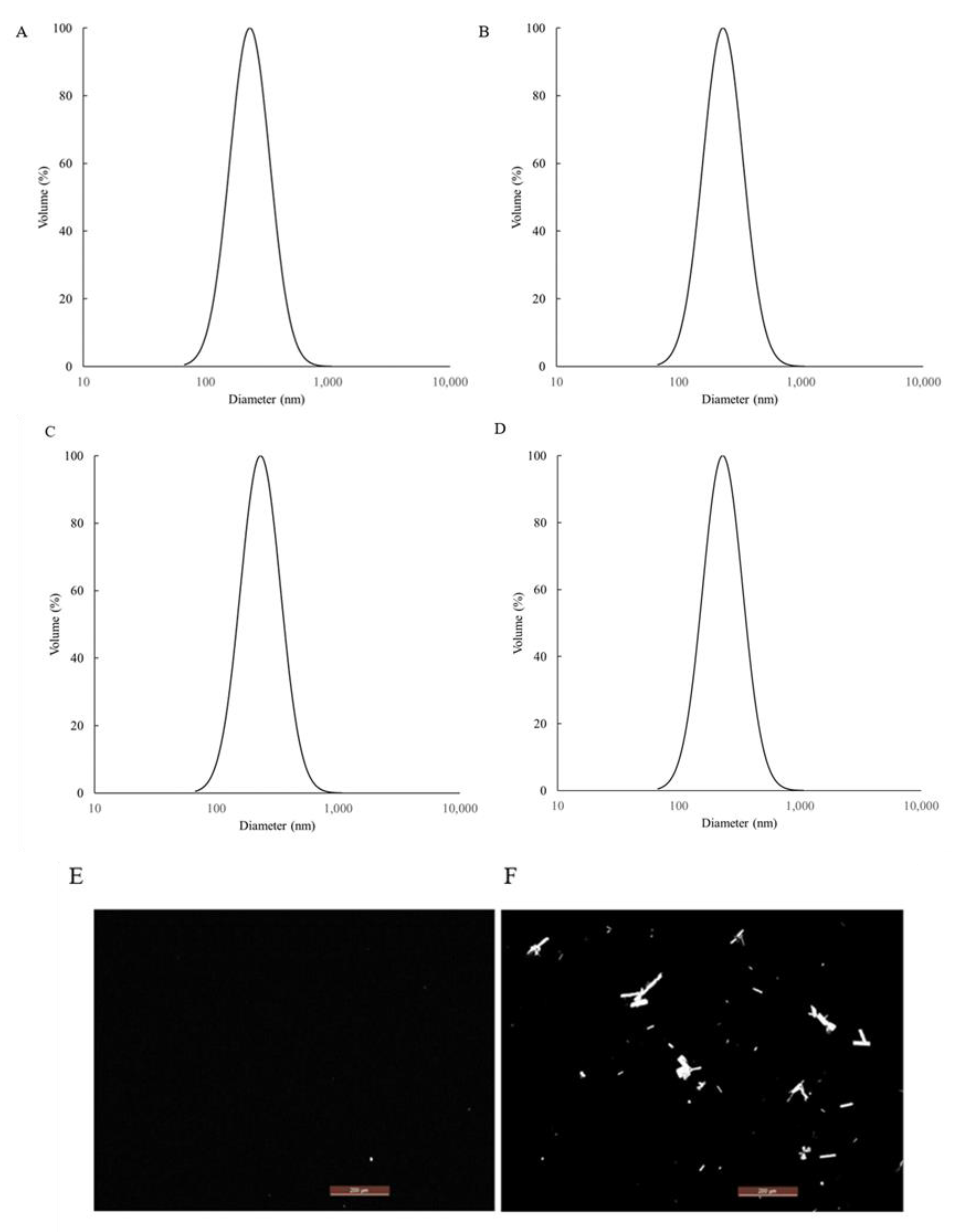
2.12. Particle Size Measurements, LUMiSizer® Test & Polarized Microscopy of the Nanoemulsions
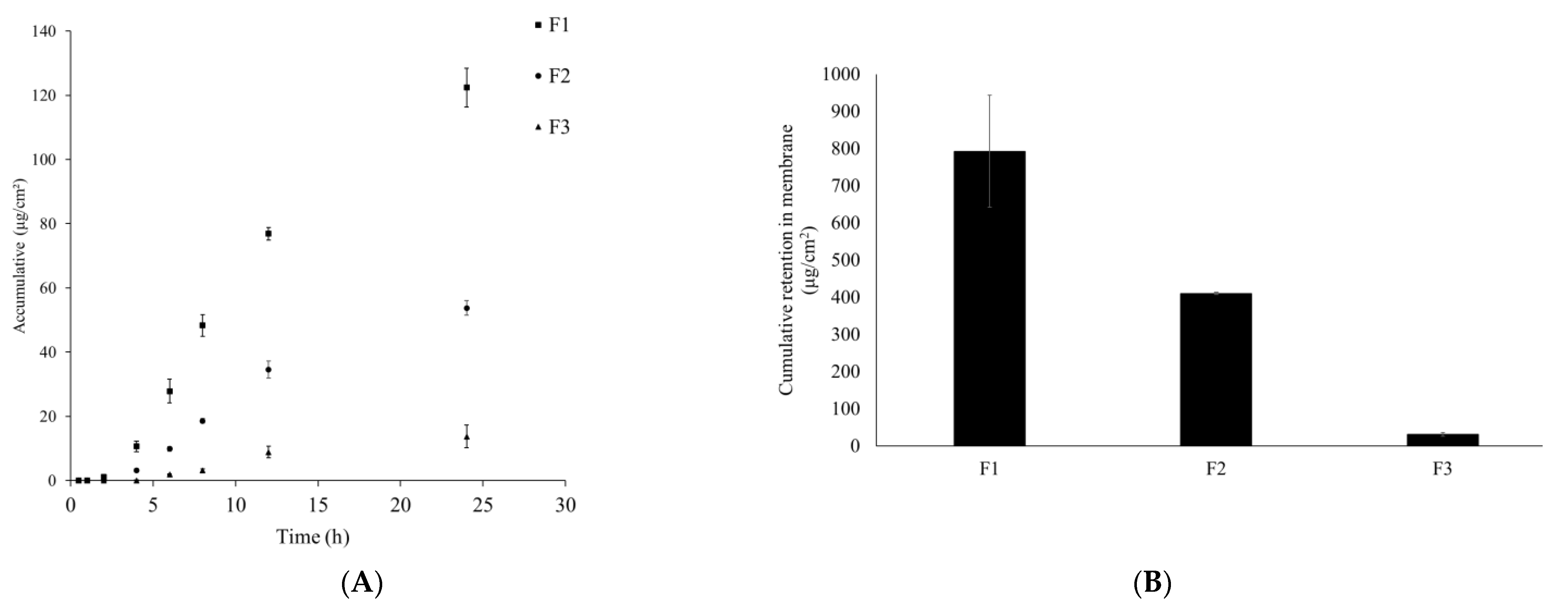
2.13. In Vitro Franz Diffusion Cell Permeation Study
2.14. High Performance Liquid Chromatography (HPLC)
2.15. Statistical Analysis
3. Results
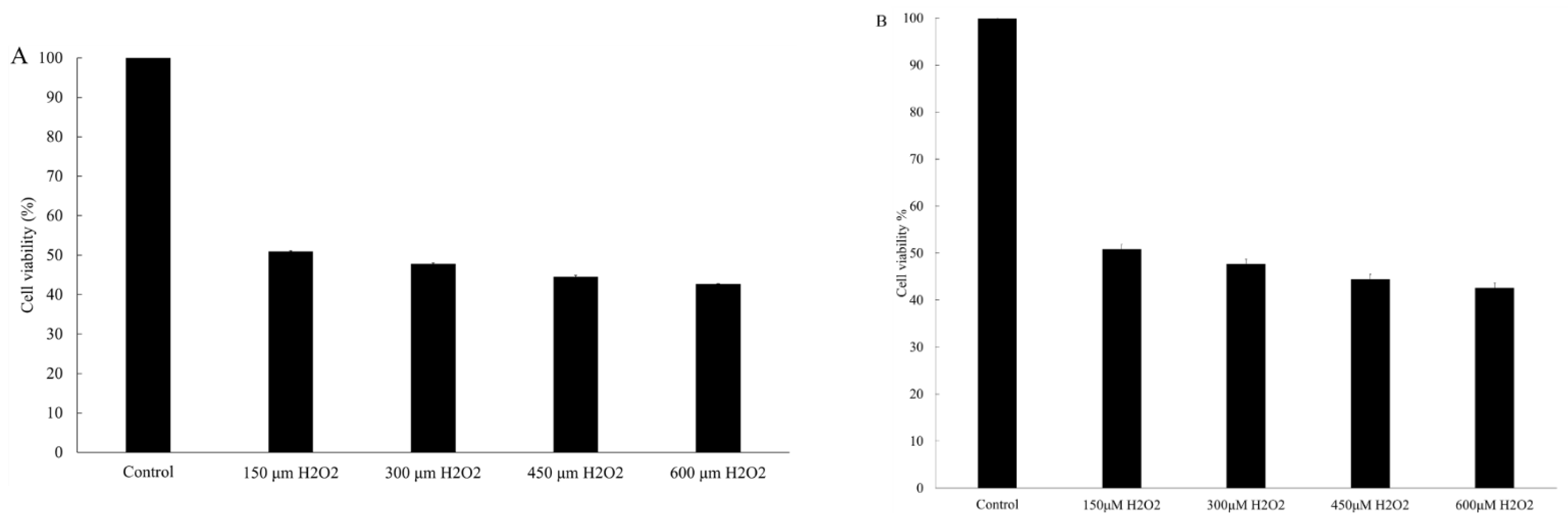
3.1. MTT Assay-HaCaT
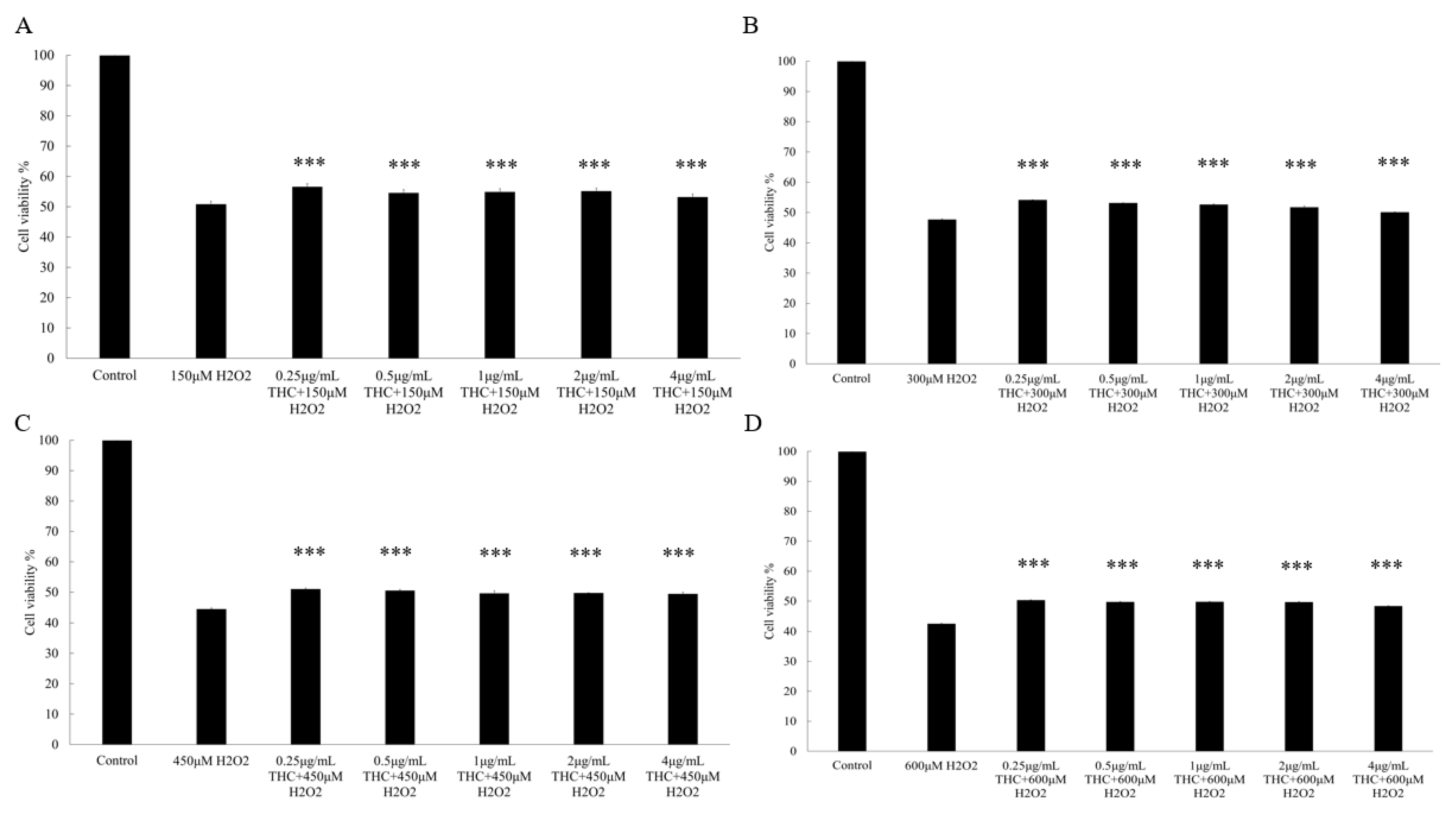
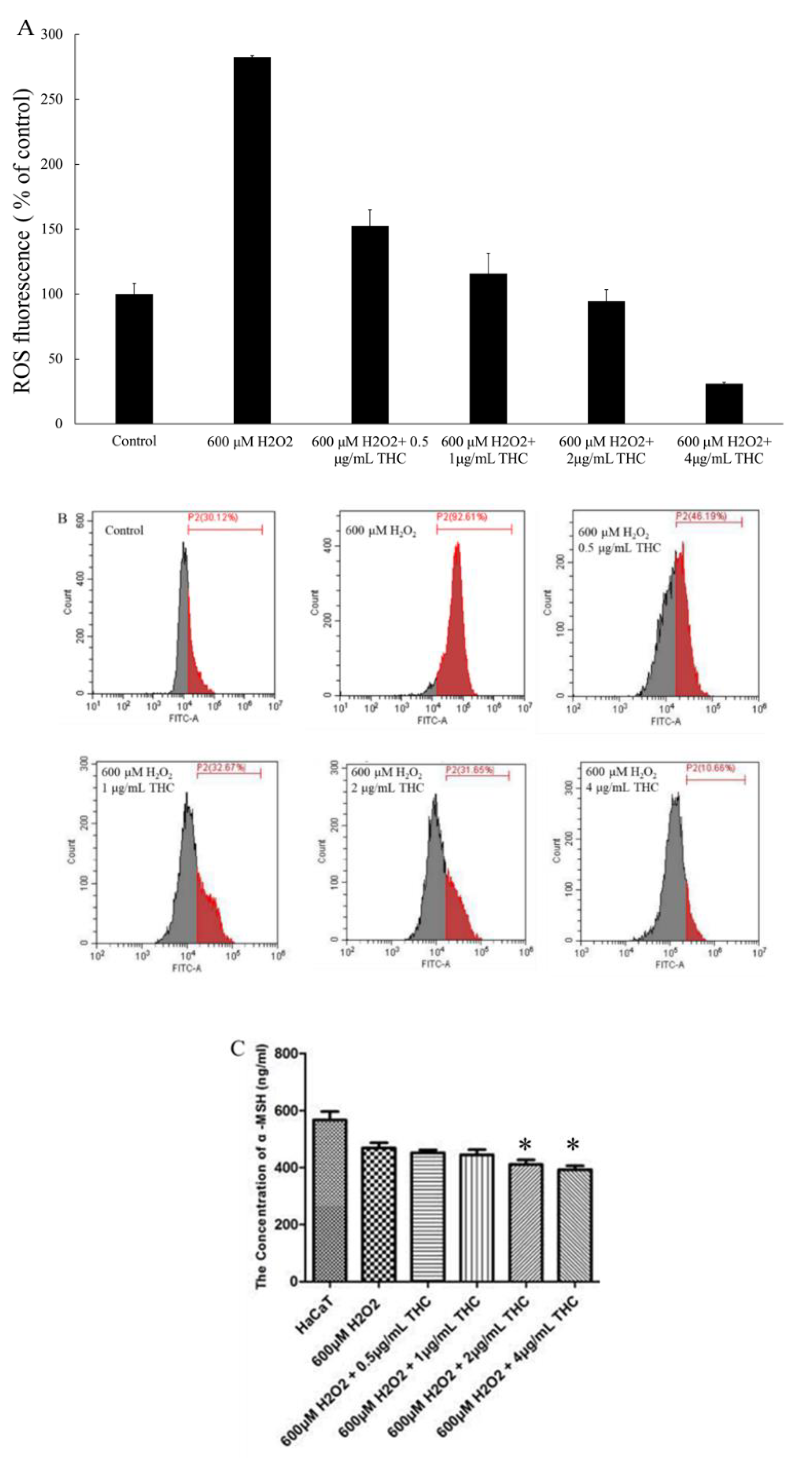
3.2. Measurement of Intracellular ROS in HaCaT and α-MSH
3.3. MTT Assay-B16F10
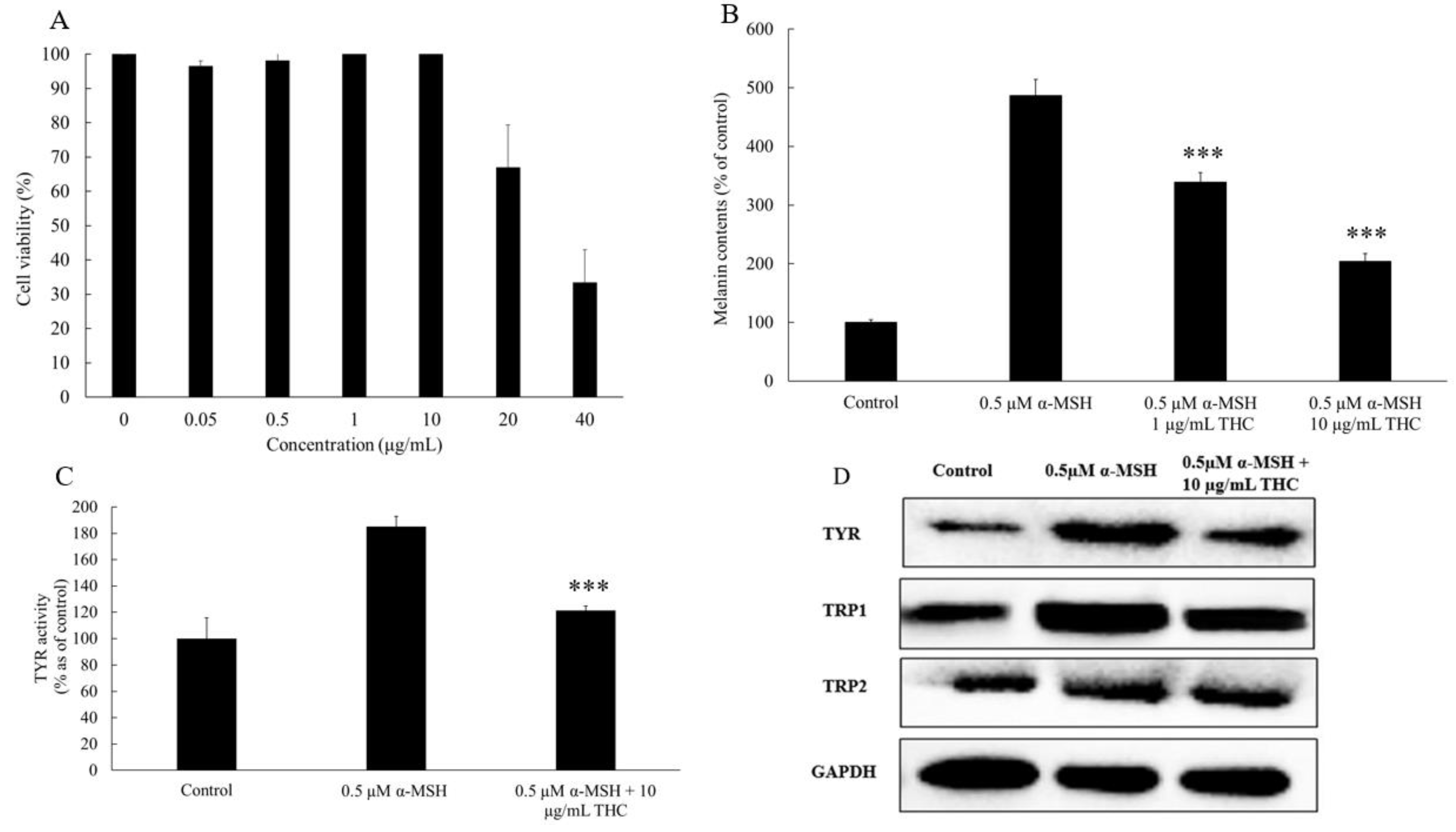
3.4. Melanin Content and Cellular Tyrosinase Activity Assay in B16F10 Cell Model
3.5. Western Blot Analysis
3.6. Realtime Polymerase Chain Reaction
3.7. Determination of THC’s Solubility in Selected Solvents
3.8. Stability Study for the Lecithin Based Nanoemulsions
3.9. In Vitro Franz Diffusion Cell Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dąbrowska, A.K.; Spano, F.; Derler, S.; Adlhart, C.; Spencer, N.D.; Rossi, R.M. The relationship between skin function, barrier properties, and body-dependent factors. Skin Res. Technol. 2018, 24, 165–174. [Google Scholar] [CrossRef] [Green Version]
- Drexler, H. Skin protection and percutaneous absorption of chemical hazards. Int. Arch. Occup. Environ. Health 2003, 76, 359–361. [Google Scholar] [CrossRef]
- Li, X.; He, C.; Chen, Z.; Zhou, C.; Gan, Y.; Jia, Y. A review of the role of sebum in the mechanism of acne pathogenesis. J. Cosmet. Dermatol. 2017, 16, 168–173. [Google Scholar] [CrossRef]
- Jia, Y.; Gan, Y.; He, C.; Chen, Z.; Zhou, C. The mechanism of skin lipids influencing skin status. J. Dermatol. Sci. 2018, 89, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Wang, H.; Yang, M.; He, C.; Yang, M.; Gao, Y.; Jia, Y. Lipidomic analysis of facial skin surface lipids reveals an altered lipid profile in infant acne. Br. J. Dermatol. 2020, 182, 817–818. [Google Scholar] [CrossRef] [PubMed]
- Gan, Y.; Zhou, M.; He, C.; Chen, Z.; Jia, Y. Lipidomics reveals skin surface lipid abnormity in acne in young men. Br. J. Dermatol. 2018, 179, 732–740. [Google Scholar]
- Jia, Y.; Zhou, M.; Huang, H.; Gan, Y.; Yang, M.; Ding, R. Characterization of circadian human facial surface lipid composition. Exp. Dermatol. 2019, 28, 858–862. [Google Scholar] [CrossRef]
- Barygina, V.; Becatti, M.; Lotti, T.; Moretti, S.; Taddei, N.; Fiorillo, C. ROS-challenged keratinocytes as a new model for oxidative stress-mediated skin diseases. J. Cell. Biochem. 2019, 120, 28–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, Y.; Wu, P.Y.; Chen, C.W.; Lyu, J.L.; Liu, Y.J.; Wen, K.C.; Lin, C.Y.; Kuo, Y.H.; Chiang, H.M. Protective effects and mechanisms of N-phenethyl caffeamide from UVA-induced skin damage in human epidermal keratinocytes through Nrf2/HO-1 regulation. Int. J. Mol. Sci. 2019, 20, 164. [Google Scholar] [CrossRef] [Green Version]
- Dalmau, N.; Andrieu-Abadie, N.; Tauler, R.; Bedia, C. Phenotypic and lipidomic characterization of primary human epidermal keratinocytes exposed to simulated solar UV radiation. J. Dermatol. Sci. 2018, 92, 97–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, X.; Mosby, N.; Yang, J.; Xu, A.; Abdel-Malek, Z.; Kadekaro, A.L. α-MSH activates immediate defense responses to UV-induced oxidative stress in human melanocytes. Pigment Cell Melanoma Res. 2009, 22, 809–818. [Google Scholar] [CrossRef]
- Pelle, E.; Mammone, T.; Marenus, K.; Maes, D.; Huang, X.; Frenkel, K. Ultraviolet-B-induced oxidative DNA base damage in primary normal human epidermal keratinocytes and inhibition by a hydroxyl radical scavenger. J. Investig. Dermatol. 2003, 121, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Goh, M.J.; Kim, J.; Choi, T.J.; Lee, H.K.; Na, Y.J.; Cho, K.H. A systems-biological study on the identification of safe and effective molecular targets for the reduction of ultraviolet B-induced skin pigmentation. Sci. Rep. 2015, 5, 10305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, J.Y.; Fisher, D.E. Melanocyte biology and skin pigmentation. Nature 2007, 445, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Holder, G.M.; Plummer, J.L.; Ryan, A.J. The metabolism and excretion of curcumin (1,7-bis-(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione) in the rat. Xenobiotica 1978, 8, 761–768. [Google Scholar] [CrossRef]
- Kukongviriyapan, U.; Apaijit, K.; Kukongviriyapan, V. Oxidative stress and cardiovascular dysfunction associated with cadmium exposure: Beneficial effects of curcumin and tetrahydrocurcumin. Tohoku J. Exp. Med. 2016, 239, 25–38. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.B.; Luo, D.D.; Xie, J.H.; Xian, Y.F.; Lai, Z.Q.; Liu, Y.H.; Liu, W.H.; Chen, J.N.; Lai, X.P.; Lin, Z.X.; et al. Curcumin’s metabolites, tetrahydrocurcumin and octahydrocurcumin, possess superior anti-inflammatory effects in vivo through suppression of TAK1-NF-κB pathway. Front. Pharmacol. 2018, 9, 1181. [Google Scholar] [CrossRef]
- Wu, J.C.; Tsai, M.L.; Lai, C.S.; Wang, Y.J.; Ho, C.T.; Pan, M.H. Chemopreventative effects of tetrahydrocurcumin on human diseases. Food Funct. 2013, 5, 12–17. [Google Scholar] [CrossRef]
- Wikramanayake, T.C.; Stojadinovic, O.; Tomic-Canic, M. Epidermal differentiation in barrier maintenance and wound healing. Adv. Wound Care 2014, 3, 272–280. [Google Scholar] [CrossRef]
- Kakkar, V.; Kaur, I.P.; Kaur, A.P.; Saini, K.; Singh, K.K. Topical delivery of tetrahydrocurcumin lipid nanoparticles effectively inhibits skin inflammation: In vitro and in vivo study. Drug Dev. Ind. Pharm. 2018, 44, 1701–1712. [Google Scholar] [CrossRef]
- Rao, A.B.; Prasad, E.; Deepthi, S.S.; Haritha, V.; Ramakrishna, S.; Madhusudan, K.; Surekha, M.V.; Rao, Y.S.R.V. Wound healing: A new perspective on glucosylated tetrahydrocurcumin. Drug Des. Dev. Ther. 2015, 9, 3579. [Google Scholar]
- Vater, C.; Adamovic, A.; Ruttensteiner, L.; Steiner, K.; Tajpara, P.; Klang, V.; Elbe-Bürger, A.; Wirth, M.; Valenta, C. Cytotoxicity of lecithin-based nanoemulsions on human skin cells and ex vivo skin permeation: Comparison to conventional surfactant types. Int. J. Pharm. 2019, 566, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Yue, Y.; Liu, G.; Li, Y.; Zhang, J.; Gong, Q.; Yan, Z.; Duan, M. Preparation and characterization of a lecithin nanoemulsion as a topical delivery system. Nanoscale Res. Lett. 2010, 5, 224–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pawar, K.R.; Babu, R.J. Lipid materials for topical and transdermal delivery of nanoemulsions. Crit. Rev. Ther. Drug Carr. Syst. 2014, 31, 429–458. [Google Scholar] [CrossRef] [PubMed]
- Su, R.; Fan, W.; Yu, Q.; Dong, X.; Qi, J.; Zhu, Q.; Zhao, W.; Wu, W.; Chen, Z.; Li, Y.; et al. Size-dependent penetration of nanoemulsions into epidermis and hair follicles: Implications for transdermal delivery and immunization. Oncotarget 2017, 8, 38214. [Google Scholar] [CrossRef] [Green Version]
- Zhu, J.; Tang, X.; Jia, Y.; Ho, C.T.; Huang, Q. Applications and delivery mechanisms of hyaluronic acid used for topical/transdermal delivery-A review. Int. J. Pharm. 2020, 578, 119127. [Google Scholar] [CrossRef]
- Nagula, R.L.; Wairkar, S. Recent advances in topical delivery of flavonoids: A review. J. Control Release 2019, 296, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.H.; Lin, Y.S.; Huang, Y.W.; Fang, S.U.; Lin, S.Y.; Hou, W.C. Protective effects of minor components of curcuminoids on hydrogen peroxide-treated human HaCaT keratinocytes. J. Agric. Food Chem. 2016, 64, 3598–3608. [Google Scholar] [CrossRef]
- Jeon, N.J.; Kim, Y.S.; Kim, E.K.; Dong, X.; Lee, J.W.; Park, J.S.; Shin, W.B.; Moon, S.H.; Jeon, B.T.; Park, P.J. Inhibitory effect of carvacrol on melanin synthesis via suppression of tyrosinase expression. J. Funct. Foods 2018, 45, 199–205. [Google Scholar] [CrossRef]
- Goenka, S.; Nagabhushanam, K.; Majeed, M.; Simon, S.R. Calebin-A, a Curcuminoid analog inhibits α-MSH-induced melanogenesis in B16F10 mouse melanoma cells. Cosmetics 2019, 6, 51. [Google Scholar] [CrossRef] [Green Version]
- Zielińska, A.; Martins-Gomes, C.; Ferreira, N.R.; Silva, A.M.; Nowak, I.; Souto, E.B. Anti-inflammatory and anti-cancer activity of citral: Optimization of citral-loaded solid lipid nanoparticles (SLN) using experimental factorial design and LUMiSizer®. Int. J. Pharm. 2018, 553, 428–440. [Google Scholar] [CrossRef]
- Haq, A.; Michniak-Kohn, B. Effects of solvents and penetration enhancers on transdermal delivery of thymoquinone: Permeability and skin deposition study. Drug Deliv. 2018, 25, 1943–1949. [Google Scholar] [CrossRef] [Green Version]
- Nahhas, A.F.; Abdel-Malek, Z.A.; Kohli, I.; Braunberger, T.L.; Lim, H.W.; Hamzavi, I.H. The potential role of antioxidants in mitigating skin hyperpigmentation resulting from ultraviolet and visible light-induced oxidative stress. Photodermatol. Photoimmunol. Photomed. 2019, 35, 420–428. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, H.; Yamane, T.; Iguchi, K.; Tanaka, K.; Iddamalgoda, A.; Unno, K.; Hoshino, M.; Takeda, A. Melanin production through novel processing of proopiomelanocortin in the extracellular compartment of the auricular skin of C57BL/6 mice after UV-irradiation. Sci. Rep. 2015, 5, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Trivedi, M.K.; Panda, P.; Sethi, K.K.; Gangwar, M.; Mondal, S.C.; Jana, S. Solid and liquid state characterization of tetrahydrocurcumin using XRPD, FT-IR, DSC, TGA, LC-MS, GC-MS, and NMR and its biological activities. J. Pharm. Anal. 2020, 10, 334–345. [Google Scholar] [CrossRef]
- Hadgraft, J.; Lane, M.E. Drug crystallization–implications for topical and transdermal delivery. Expert Opin. Drug Deliv. 2016, 13, 817–830. [Google Scholar] [CrossRef]
- Tang, X.; Zhang, M.; Zhang, H.; Pan, Y.; Dong, Q.; Xin, Y.; Ho, C.T.; Huang, Q. Evaluation of the bioaccessibility of tetrahydrocurcumin-hyaluronic acid conjugate using in vitro and ex vivo models. Int. J. Biol. Macromol. 2021, 182, 1322–1330. [Google Scholar] [CrossRef]
- Kung, C.P.; Zhang, Y.; Sil, B.C.; Hadgraft, J.; Lane, M.E.; Patel, B.; McCulloch, R. Investigation of binary and ternary solvent systems for dermal delivery of methadone. Int. J. Pharm. 2020, 586, 119538. [Google Scholar] [CrossRef] [PubMed]
- Villanueva-Martínez, A.; Hernández-Rizo, L.; Ganem-Rondero, A. Evaluating two nanocarrier systems for the transdermal delivery of sodium alendronate. Int. J. Pharm. 2020, 582, 119312. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Xie, H.; Chen, X.; Shi, W.; Xiao, X.; Lei, D.; Li, J. Differential response of normal human epidermal keratinocytes and HaCaT cells to hydrogen peroxide-induced oxidative stress. Clin. Exp. Dermatol. 2012, 37, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Pelle, E.; Mammone, T.; Maes, D.; Frenkel, K. Keratinocytes act as a source of reactive oxygen species by transferring hydrogen peroxide to melanocytes. J. Investig. Dermatol. 2005, 124, 793–797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spencer, J.D.; Gibbons, N.C.; Rokos, H.; Peters, E.M.; Wood, J.M.; Schallreuter, K.U. Oxidative stress via hydrogen peroxide affects proopiomelanocortin peptides directly in the epidermis of patients with vitiligo. J. Investig. Dermatol. 2007, 127, 411–420. [Google Scholar] [CrossRef] [Green Version]
- Sugiyama, Y.; Kawakishi, S.; Osawa, T. Involvement of the β-diketone moiety in the antioxidative mechanism of tetrahydrocurcumin. Biochem. Pharmacol. 1996, 52, 519–525. [Google Scholar] [CrossRef]
- Hundshammer, C.; Schön, C.; Kimura, M.; Furune, T.; Terao, K.; Elgeti, D.; Mohr, R. Enhanced metabolic bioavailability of tetrahydrocurcumin after oral supplementation of a γ-cyclodextrin curcumin complex. J. Funct. Foods 2021, 79, 104410. [Google Scholar] [CrossRef]
- Trivedi, M.K.; Gangwar, M.; Mondal, S.C.; Jana, S. Protective effects of tetrahydrocurcumin (THC) on fibroblast and melanoma cell lines in vitro: It’s implication for wound healing. J. Food Sci. Technol. 2017, 54, 1137–1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirjavainen, M.; Mönkkönen, J.; Saukkosaari, M.; Valjakka-Koskela, R.; Kiesvaara, J.; Urtti, A. Phospholipids affect stratum corneum lipid bilayer fluidity and drug partitioning into the bilayers. J. Control Release 1999, 58, 207–214. [Google Scholar] [CrossRef]
- Elnaggar, Y.S.; El-Refaie, W.M.; El-Massik, M.A.; Abdallah, O.Y. Lecithin-based nanostructured gels for skin delivery: An update on state of art and recent applications. J. Control Release 2014, 180, 10–24. [Google Scholar] [CrossRef]
- Vater, C.; Hlawaty, V.; Werdenits, P.; Cichoń, M.A.; Klang, V.; Elbe-Bürger, A.; Wirth, M.; Valenta, C. Effects of lecithin-based nanoemulsions on skin: Short-time cytotoxicity MTT and BrdU studies, skin penetration of surfactants and additives and the delivery of curcumin. Int. J. Pharm. 2020, 580, 119209. [Google Scholar] [CrossRef]
- Haq, A.; Goodyear, B.; Ameen, D.; Joshi, V.; Michniak-Kohn, B. Strat-M® synthetic membrane: Permeability comparison to human cadaver skin. Int. J. Pharm. 2018, 547, 432–437. [Google Scholar] [CrossRef]
- Dreher, F.; Walde, P.; Walther, P.; Wehrli, E. Interaction of a lecithin microemulsion gel with human stratum corneum and its effect on transdermal transport. J. Control Release 1997, 45, 131–140. [Google Scholar] [CrossRef]
- Shaker, D.S.; Ishak, R.A.; Ghoneim, A.; Elhuoni, M.A. Nanoemulsion: A review on mechanisms for the transdermal delivery of hydrophobic and hydrophilic drugs. Sci. Pharm. 2019, 87, 17. [Google Scholar] [CrossRef] [Green Version]

| GAPDH | Forward | 5′-TGTTTCCTCGTCCCGTAGA-3′ |
| Reverse | 5′-GATGGCAACAATCTCCACTTTG-3′ | |
| Tyrosinase | Forward | 5′-TCCAAGAGTCAGATCCAGGC-3′ |
| Reverse | 5′-TCCTGGGGTTGCTTCTTCTT-3′ | |
| TRP1 | Forward | 5′-AGTGGCTGCGTTGTTACTTG-3′ |
| Reverse | 5′-TGGAGTGGTTAGGATTCGGG-3′ | |
| TRP2 | Forward | 5′-CTTTTGGACCATGTTCGGCA-3′ |
| Reverse | 5′-AGGAGTTGGTGATCATGGCA-3′ |
| A | |||
| Group | tyrosinase | GAPDH | tyrosinase: GAPDH |
| Control | 343144 | 1310392 | 0.262 |
| 0.5 µM α-MSH | 1057134 | 1097892 | 0.963 |
| 0.5 µM α-MSH + 10 µg/mL THC | 641184 | 1157389 | 0.554 |
| B | |||
| Group | trp1 | GAPDH | trp1: GAPDH |
| Control | 705731 | 1310392 | 0.539 |
| 0.5 µM α-MSH | 1695207 | 1097892 | 1.544 |
| 0.5 µM α-MSH + 10 µg/mL THC | 1088834 | 1157389 | 0.941 |
| C | |||
| Group | trp2 | GAPDH | trp2: GAPDH |
| Control | 620056 | 1310392 | 0.473 |
| 0.5 µM α-MSH | 910823 | 1097892 | 0.829 |
| 0.5 µM α-MSH + 10 µg/mL THC | 687519 | 1157389 | 0.594 |
| Ingredients/ID | S1 | S2 | S3 | S4 | S5 | S6 | S7 |
|---|---|---|---|---|---|---|---|
| 8% (w/w) Lecithin dispersion | 20% | 30% | 40% | 50% | 50% | 50% | 50% |
| Water | 49% | 39% | 29% | 19% | 9% | -- | 29% |
| DEGEE | 10% | 10% | 10% | 10% | 10% | 10% | 10% |
| THC | 1% | 1% | 1% | 1% | 1% | 1% | 1% |
| MCT | 20% | 20% | 20% | 20% | 30% | 39% | 10% |
| Instability index | 0.746 | 0.411 | 0.053 | 0.049 | 0.061 | 0.062 | 0.023 |
| Ingredients | F1 | F2 | F3 |
|---|---|---|---|
| (8% w/v) Lecithin dispersion | 50% | 50% | -- |
| Medium Chain Triglyceride | 30% | -- | -- |
| DEGEE | 10% | 10% | -- |
| THC | 1% | 1% | 1% |
| Water | 9% | 39% | 99% |
| Instability index | 0.061 | 0.018 | N/A * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, X.; Dong, Q.; Li, J.; Li, F.; Michniak-Kohn, B.B.; Zhao, D.; Ho, C.-T.; Huang, Q. Anti-Melanogenic Mechanism of Tetrahydrocurcumin and Enhancing Its Topical Delivery Efficacy Using a Lecithin-Based Nanoemulsion. Pharmaceutics 2021, 13, 1185. https://doi.org/10.3390/pharmaceutics13081185
Tang X, Dong Q, Li J, Li F, Michniak-Kohn BB, Zhao D, Ho C-T, Huang Q. Anti-Melanogenic Mechanism of Tetrahydrocurcumin and Enhancing Its Topical Delivery Efficacy Using a Lecithin-Based Nanoemulsion. Pharmaceutics. 2021; 13(8):1185. https://doi.org/10.3390/pharmaceutics13081185
Chicago/Turabian StyleTang, Xudong, Qiaoru Dong, Jun Li, Fang Li, Bozena B. Michniak-Kohn, Denggao Zhao, Chi-Tang Ho, and Qingrong Huang. 2021. "Anti-Melanogenic Mechanism of Tetrahydrocurcumin and Enhancing Its Topical Delivery Efficacy Using a Lecithin-Based Nanoemulsion" Pharmaceutics 13, no. 8: 1185. https://doi.org/10.3390/pharmaceutics13081185
APA StyleTang, X., Dong, Q., Li, J., Li, F., Michniak-Kohn, B. B., Zhao, D., Ho, C.-T., & Huang, Q. (2021). Anti-Melanogenic Mechanism of Tetrahydrocurcumin and Enhancing Its Topical Delivery Efficacy Using a Lecithin-Based Nanoemulsion. Pharmaceutics, 13(8), 1185. https://doi.org/10.3390/pharmaceutics13081185







