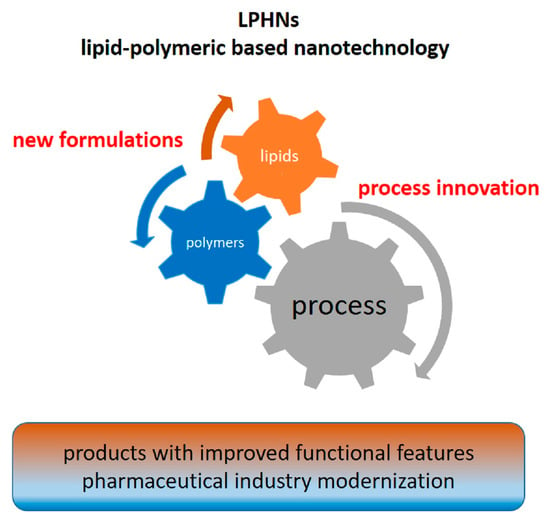
Polymer–Lipid Pharmaceutical Nanocarriers: Innovations by New Formulations and Production Technologies
Abstract
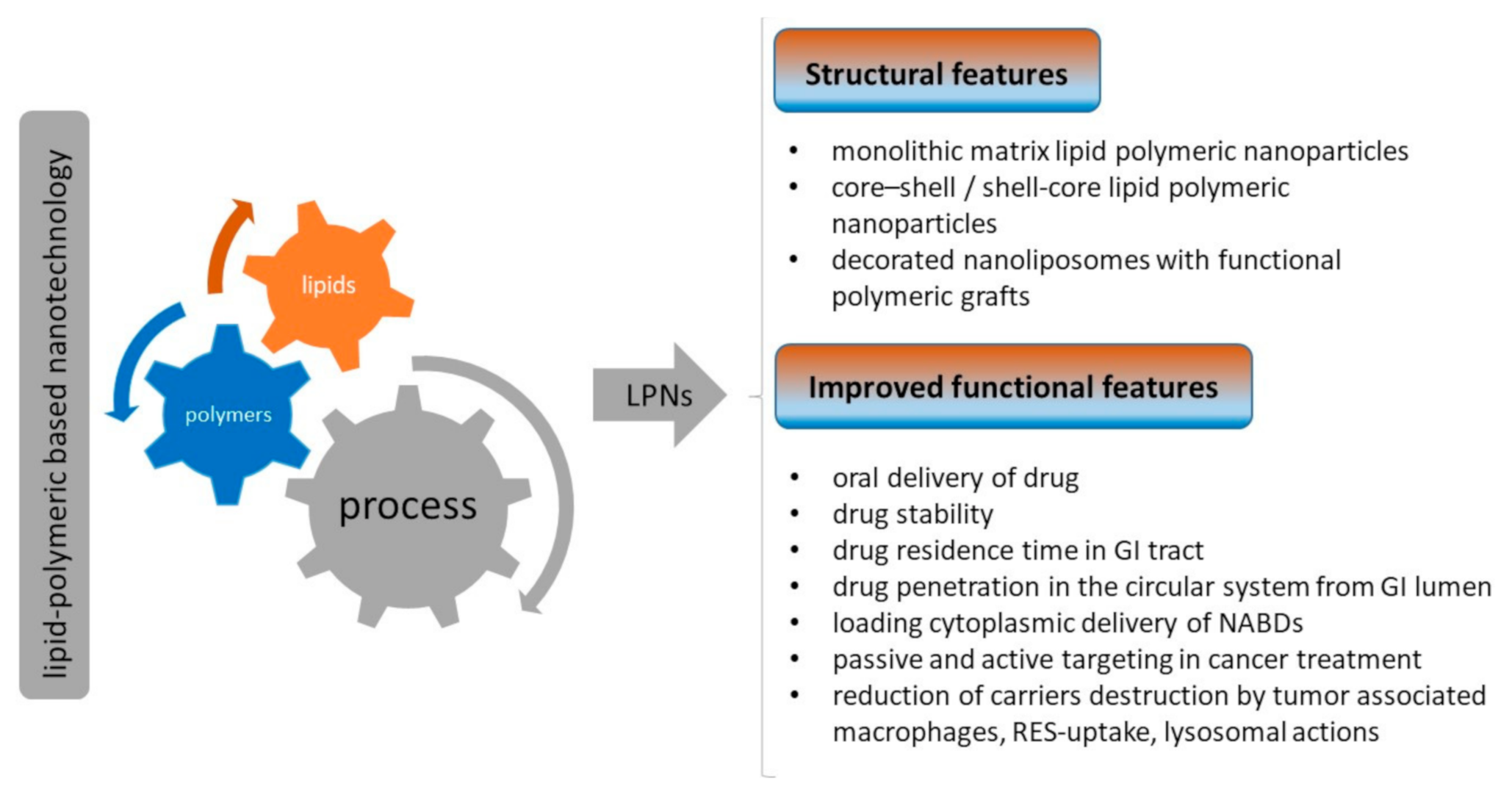
1. Introduction
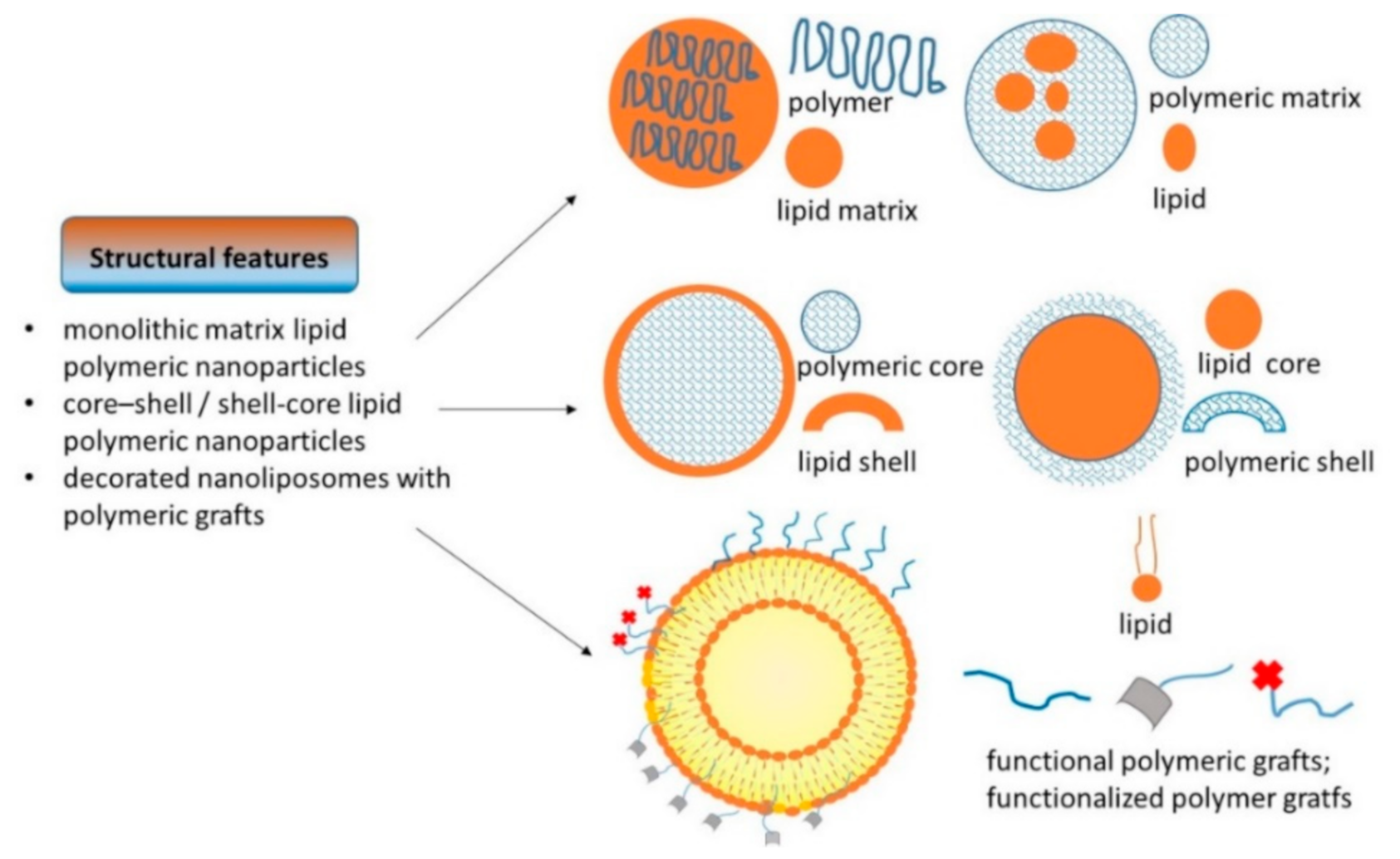
2. Polymeric, Lipid, and Hybrid Nanostructures
| LPHN Composition/Active Ingredient/Preparative Method | Application | Reference |
|---|---|---|
| Lipid, lipoid S75-chitosan, low molecular weight (monolithic nanostructures)/cisplatin/ionic gelation (ethanolic solution dropped in chitosan acidulate solution with cisplatin) | cancer therapies | Khan et al., 2019 [38] |
| Nanoparticles with PLGA core layered by lecithin lipid PEG modified with iRGD peptides/isoliquiritingenin/modified single-step nanoprecipitation | breast tumor therapy | Gao et al., 2017 [39] |
| liver cancer therapies | AlQahtani et al., 2021 [24] |
| Ionizable lipid L319, distearoylphosphatidylcholine, cholesterol, and 1,2-dimyristoyl-rac-glycero-3-methoxy-PEG (nanoliposomes PEGylated)/siRNA/spontaneous vesicle formations method by pumping ethanolic solution with lipids and citrate buffer solution with siRNA within a chromatography tubing | vaccine therapy against SARS-CoV-2 | Polack et al., 2020 [40] Walsh et al., 2020 [41] Maier et al., 2013 [42] Pardi et al., 2015 [43] |
| 1,2-Distearoyl-sn-glycero-3-phosphoethanolamine—PEG, gelucire, PLA, (fructose-tethered phospholipid coated lipophilic polymeric core)/beta carotene and methotrexate/modified single-step nanoprecipitation method | breast cancer therapy | Jain et al. 2017 [44] |
| L-α-Phosphatidylcholine, cholesterol, chitosan (nanoliposomes coated by chitosan)/indomethacin/simil-microfluidic method | cancer therapies | Dalmoro et al., 2018 [45] |
| L-α-Phosphatidylcholine, cholesterol, chitosan (nanoliposomes coated by chitosan)/D3, K2 vitamins/simil-microfluidic method | food supplements | Dalmoro et al., 2019 [46] |
| PLA, soya lecithin, stearylamine (lipid shell, polymer core with antimicrobic)/norfloxacin/emulsification solvent evaporation method | antimicrobial therapies | Dave et al., 2017 [47] |
| PLGA, soybean lecithin, and PEG (polymer core-encapsulating gold crystals, lipid monolayer surrounding, outer lipid PEG)/gold nanocrystals/nanopreciptitation method | bioimaging purposes | Mukherjee et al., 2019 [48] |
Examples of Application
3. Innovations and Performances of Production Technologies
| LPHN Production Techniques/Output Structure | Main Advantages | Main Disadvantages | References |
|---|---|---|---|
| Conventional techniques | |||
| Nanoprecipitation method/monolithic nanosystems | easy to perform, inexpensive | bulk technique (bench-scale), long process times, limited output volumes, poor control | Mukherejee et al., 2019 [48] Dehaini et al., 2016 [62] Zhang et al., 2010 [8] |
| Dropwise (layer-by-layer) method/coated nanosystems | easy to perform, inexpensive | bulk technique (bench-scale), long process times, limited output volumes, poor control | Hasan et al., 2016 [57] Tan et al., 2016 [58] Bochicchio et al., 2018 [77] |
| Emulsification-solvent evaporation method/coated nanosystems | easy to perform, inexpensive | bulk technique (bench-scale), long process times, limited output volumes, poor control | Mukherejee et al., 2019 [48] Zhang et al., 2010 |
| Emerging technologies | |||
| Spray drying/monolithic or layered nanosystems | continuous technique, massive production, precise control | high energy consumption | Dormenval et al., 2019 [70] |
| Microfluidic method/layered polymeric core, outer lipid–PEG | precise control | limited output volumes (bench-scale), expensive apparatus | Wei et al., 2020 [69] Mieszawska et al., 2013 [56] |
| Simil-microfluidic method/chitosan or guar gum-coated nanoliposomes | continuous technique, massive production, precise control, operative room conditions | presence of residual solvent | Bochicchio et al., 2018 [77] Barba et al., 2019 [90] |
| Super critical fluid technique/chitosan-coated liposomes | organic solvent-free preparations | expensive apparatus, high energy consumption | Otake et al., 2006 [88] |
4. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| GI | gastrointestinal (tract, lumen) |
| LNCs | lipid nanocapsules |
| LNs | lipid nanoparticles |
| LPHNs | lipid–polymeric hybrid nanoparticles |
| LPNs | Lipid–polymeric nanoparticles |
| NABDs | nucleic acid-based drugs |
| NCLs | nanostructured lipid carriers |
| NEs | nanoerithrocytes |
| NP | nanoparticle |
| MTT | 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide |
| PNs | lipid nanoparticles |
| RBCs | red blood cells |
| RBC-MCNs | rbc-membrane-camouflaged nanocarriers |
| RES | reticuloendothelial system |
| siRNA | short interfering RNA |
| SLNs | solid lipid nanoparticles |
| SMSLNs | surface-modified solid lipid nanoparticles |
References
- Du, Y.; Chen, B. Combination of drugs and carriers in drug delivery technology and its development. Drug Des. Dev. Ther. 2019, 13, 1401. [Google Scholar] [CrossRef] [PubMed]
- Mandal, B.; Bhattacharjee, H.; Mittal, N.; Sah, H.; Balabathula, P.; Thoma, L.A.; Wood, G.C. Core–shell-type lipid–polymer hybrid nanoparticles as a drug delivery platform. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 474–491. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.X.; Ahmed, T.; Li, L.Y.; Li, J.; Abbasi, A.Z.; Wu, X.Y. Design of nanocarriers for nanoscale drug delivery to enhance cancer treatment using hybrid polymer and lipid building blocks. Nanoscale 2017, 9, 1334–1355. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ayano, E.; Maitani, Y.; Kanazawa, H. Tunable surface properties of temperature-responsive polymer-modified liposomes induce faster cellular uptake. ACS Omega 2017, 2, 316–325. [Google Scholar] [CrossRef]
- Nagase, K.; Hasegawa, M.; Ayano, E.; Maitani, Y.; Kanazawa, H. Effect of polymer phase transition behavior on temperature-responsive polymer-modified liposomes for siRNA transfection. Int. J. Mol. Sci. 2019, 20, 430. [Google Scholar]
- Barve, A.; Jain, A.; Liu, H.; Zhao, Z.; Cheng, K. Enzyme-responsive polymeric micelles of cabazitaxel for prostate cancer targeted therapy. Acta Biomater. 2020, 113, 501–511. [Google Scholar] [CrossRef]
- Ganesan, P.; Ramalingam, P.; Karthivashan, G.; Ko, Y.T.; Choi, D.-K. Recent developments in solid lipid nanoparticle and surface-modified solid lipid nanoparticle delivery systems for oral delivery of phyto-bioactive compounds in various chronic diseases. Int. J. Nanomed. 2018, 13, 1569. [Google Scholar] [CrossRef]
- Zhang, L.; ZHANG, L. Lipid–polymer hybrid nanoparticles: Synthesis, characterization and applications. Nano Life 2010, 1, 163–173. [Google Scholar] [CrossRef]
- Celerino de Moraes Porto, I.C. Polymer biocompatibility. In Polymerization; De Souza Gomes, A., Ed.; InTech Open: Rijeka, Croatia, 2012; pp. 47–62. [Google Scholar] [CrossRef]
- Arif, U.; Haider, S.; Haider, A.; Khan, N.; Alghyamah, A.A.; Jamila, N.; Khan, M.I.; Almasry, W.A.; Kang, I.K. Biocompatible Polymers and their Potential Biomedical Applications: A Review. Curr. Pharm. Des. 2019, 25, 3608–3619. [Google Scholar] [CrossRef]
- Kim, M.W.; Kwon, S.H.; Choi, J.H.; Lee, A. A Promising Biocompatible Platform: Lipid-Based and Bio-Inspired Smart Drug Delivery Systems for Cancer Therapy. Int. J. Mol. Sci. 2018, 19, 3859. [Google Scholar] [CrossRef]
- Sun, M.; Yuan, Y.; Lu, F.; Di Pasqua, A.J. Physicochemical Factors That Influence the Biocompatibility of Cationic Liposomes and Their Ability to Deliver DNA to the Nuclei of Ovarian Cancer SK-OV-3 Cells. Materials 2021, 14, 416. [Google Scholar] [CrossRef] [PubMed]
- Montis, C.; Sostegni, S.; Milani, S.; Baglioni, P.; Berti, D. Biocompatible cationic lipids for the formulation of liposomal DNA vectors. Soft. Matter. 2014, 10, 4287–4297. [Google Scholar] [CrossRef] [PubMed]
- Begines, B.; Ortiz, T.; Pérez-Aranda, M.; Martínez, G.; Merinero, M.; Argüelles-Arias, F.; Alcudia, A. Polymeric nanoparticles for drug delivery: Recent developments and future prospects. Nanomaterials 2020, 10, 1403. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, J.; Vaughan, H.J.; Green, J.J. Biodegradable polymeric nanoparticles for therapeutic cancer treatments. Annu. Rev. Chem. Biomol. Eng. 2018, 9, 105–127. [Google Scholar] [CrossRef] [PubMed]
- George, A.; Shah, P.A.; Shrivastav, P.S. Natural biodegradable polymers based nano-formulations for drug delivery: A review. Int. J. Pharm. 2019, 561, 244–264. [Google Scholar] [CrossRef] [PubMed]
- Venditti, I. Morphologies and functionalities of polymeric nanocarriers as chemical tools for drug delivery: A review. J. King Saud Univ.-Sci. 2019, 31, 398–411. [Google Scholar] [CrossRef]
- Barba, A.A.; Gaetano, L.; Carla, S.; Barbara, D.; Michela, A.; Mario, G.; Rossella, F.; Federica, T.; Giancarlo, F.; Francesco, M.; et al. Novel Lipid and Polymeric Materials as Delivery Systems for Nucleic Acid Based Drugs. Curr. Drug Metab. 2015, 16, 427–452. [Google Scholar] [CrossRef]
- Mufamadi, M.S.; Pillay, V.; Choonara, Y.E.; Du Toit, L.C.; Modi, G.; Naidoo, D.; Ndesendo, V.M. A review on composite liposomal technologies for specialized drug delivery. J. Drug Deliv. 2011, 2011, 939851. [Google Scholar] [CrossRef]
- Jimenez-Jimenez, C.; Manzano, M.; Vallet-Regi, M. Nanoparticles Coated with Cell Membranes for Biomedical Applications. Biology 2020, 9, 406. [Google Scholar] [CrossRef]
- Chen, H.Y.; Deng, J.; Wang, Y.; Wu, C.Q.; Li, X.; Dai, H.W. Hybrid cell membrane-coated nanoparticles: A multifunctional biomimetic platform for cancer diagnosis and therapy. Acta Biomater. 2020, 112, 1–13. [Google Scholar] [CrossRef]
- Xu, C.H.; Ye, P.J.; Zhou, Y.C.; He, D.X.; Wei, H.; Yu, C.Y. Cell membrane-camouflaged nanoparticles as drug carriers for cancer therapy. Acta Biomater. 2020, 105, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.N.; Elsabahy, M.; Khan, S.; Zhang, F.W.; Song, Y.; Dong, M.; Li, R.C.; Smolen, J.; Letteri, R.A.; Su, L.; et al. Erythrocyte-Membrane-Camouflaged Nanocarriers with Tunable Paclitaxel Release Kinetics via Macromolecular Stereocomplexation. ACS Mater. Lett. 2020, 2, 595–601. [Google Scholar] [CrossRef]
- AlQahtani, S.A.; Harisa, G.I.; Alomrani, A.H.; Alanazi, F.K.; Badran, M.M. Improved pharmacokinetic and biodistribution of 5-fluorouracil loaded biomimetic nanoerythrocytes decorated nanocarriers for liver cancer treatment. Colloids Surf. B-Biointerfaces 2021, 197, 111380. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, S.; Ranjan, S.; Dasgupta, N.; Kumar, R.; Thomas, S. Nanocarriers for Drug Delivery: Nanoscience and Nanotechnology in Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Duan, Y.; Dhar, A.; Patel, C.; Khimani, M.; Neogi, S.; Sharma, P.; Kumar, N.S.; Vekariya, R.L. A brief review on solid lipid nanoparticles: Part and parcel of contemporary drug delivery systems. RSC Adv. 2020, 10, 26777–26791. [Google Scholar] [CrossRef]
- Mukherjee, S.; Ray, S.; Thakur, R. Solid lipid nanoparticles: A modern formulation approach in drug delivery system. Indian J. Pharm. Sci. 2009, 71, 349. [Google Scholar] [CrossRef]
- Date, T.; Nimbalkar, V.; Kamat, J.; Mittal, A.; Mahato, R.I.; Chitkara, D. Lipid-polymer hybrid nanocarriers for delivering cancer therapeutics. J. Control. Release 2018, 271, 60–73. [Google Scholar] [CrossRef]
- Bochicchio, S.; Dalmoro, A.; Barba, A.A.; dAmore, M.; Lamberti, G. New preparative approaches for micro and nano drug delivery carriers. Curr. Drug Deliv. 2017, 14, 203–215. [Google Scholar] [CrossRef]
- Rizwanullah, M.; Ahmad, J.; Amin, S.; Mishra, A.; Ain, M.R.; Rahman, M. Polymer-lipid hybrid systems: Scope of intravenous-to-Oral switch in Cancer chemotherapy. Curr. Nanomed. Former. Recent Pat. Nanomed. 2020, 10, 164–177. [Google Scholar] [CrossRef]
- Vargas, K.M.; Shon, Y.-S. Hybrid lipid–nanoparticle complexes for biomedical applications. J. Mater. Chem. B 2019, 7, 695–708. [Google Scholar] [CrossRef]
- Wakaskar, R.R. General overview of lipid–polymer hybrid nanoparticles, dendrimers, micelles, liposomes, spongosomes and cubosomes. J. Drug Target. 2018, 26, 311–318. [Google Scholar] [CrossRef]
- Zangabad, P.S.; Mirkiani, S.; Shahsavari, S.; Masoudi, B.; Masroor, M.; Hamed, H.; Jafari, Z.; Taghipour, Y.D.; Hashemi, H.; Karimi, M. Stimulus-responsive liposomes as smart nanoplatforms for drug delivery applications. Nanotechnol. Rev. 2018, 7, 95–122. [Google Scholar] [CrossRef] [PubMed]
- Campani, V.; Giarra, S.; De Rosa, G. Lipid-based core-shell nanoparticles: Evolution and potentialities in drug delivery. OpenNano 2018, 3, 5–17. [Google Scholar] [CrossRef]
- Majumder, J.; Minko, T. Multifunctional and stimuli-responsive nanocarriers for targeted therapeutic delivery. Expert. Opin. Drug. Deliv. 2020, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Siewert, C.D.; Haas, H.; Cornet, V.; Nogueira, S.S.; Nawroth, T.; Uebbing, L.; Ziller, A.; Al-Gousous, J.; Radulescu, A.; Schroer, M.A. Hybrid Biopolymer and Lipid Nanoparticles with Improved Transfection Efficacy for mRNA. Cells 2020, 9, 2034. [Google Scholar] [CrossRef] [PubMed]
- Garg, N.K.; Tyagi, R.K.; Sharma, G.; Jain, A.; Singh, B.; Jain, S.; Katare, O. Functionalized lipid–polymer hybrid nanoparticles mediated codelivery of methotrexate and aceclofenac: A synergistic effect in breast cancer with improved pharmacokinetics attributes. Mol. Pharm. 2017, 14, 1883–1897. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.M.; Madni, A.; Torchilin, V.; Filipczak, N.; Pan, J.; Tahir, N.; Shah, H. Lipid-chitosan hybrid nanoparticles for controlled delivery of cisplatin. Drug Deliv. 2019, 26, 765–772. [Google Scholar] [CrossRef]
- Gao, F.; Zhang, J.; Fu, C.; Xie, X.; Peng, F.; You, J.; Tang, H.; Wang, Z.; Li, P.; Chen, J. iRGD-modified lipid–polymer hybrid nanoparticles loaded with isoliquiritigenin to enhance anti-breast cancer effect and tumor-targeting ability. Int. J. Nanomed. 2017, 12, 4147. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Walsh, E.E.; Frenck, R.W.; Falsey, A.R.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Neuzil, K.; Mulligan, M.J.; Bailey, R.; et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. N. Engl. J. Med. 2020, 383, 2439–2450. [Google Scholar] [CrossRef]
- Maier, M.A.; Jayaraman, M.; Matsuda, S.; Liu, J.; Barros, S.; Querbes, W.; Tam, Y.K.; Ansell, S.M.; Kumar, V.; Qin, J.; et al. Biodegradable Lipids Enabling Rapidly Eliminated Lipid Nanoparticles for Systemic Delivery of RNAi Therapeutics. Mol. Ther. 2013, 21, 1570–1578. [Google Scholar] [CrossRef]
- Pardi, N.; Tuyishime, S.; Muramatsu, H.; Kariko, K.; Mui, B.L.; Tam, Y.K.; Madden, T.D.; Hope, M.J.; Weissman, D. Expression kinetics of nucleoside-modified mRNA delivered in lipid nanoparticles to mice by various routes. J. Control. Release 2015, 217, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Sharma, G.; Kushwah, V.; Garg, N.K.; Kesharwani, P.; Ghoshal, G.; Singh, B.; Shivhare, U.S.; Jain, S.; Katare, O.P. Methotrexate and beta-carotene loaded-lipid polymer hybrid nanoparticles: A preclinical study for breast cancer. Nanomedicine 2017, 12, 1851–1872. [Google Scholar] [CrossRef] [PubMed]
- Dalmoro, A.; Bochicchio, S.; Nasibullin, S.F.; Bertoncin, P.; Lamberti, G.; Barba, A.A.; Moustafine, R.I. Polymer-lipid hybrid nanoparticles as enhanced indomethacin delivery systems. Eur. J. Pharm. Sci. 2018, 121, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Dalmoro, A.; Bochicchio, S.; Lamberti, G.; Bertoncin, P.; Janssens, B.; Barba, A.A. Micronutrients encapsulation in enhanced nanoliposomal carriers by a novel preparative technology. RSC Adv. 2019, 9, 19800–19812. [Google Scholar] [CrossRef]
- Dave, V.; Yadav, R.B.; Kushwaha, K.; Yadav, S.; Sharma, S.; Agrawal, U. Lipid-polymer hybrid nanoparticles: Development & statistical optimization of norfloxacin for topical drug delivery system. Bioact. Mater. 2017, 2, 269–280. [Google Scholar]
- Mukherjee, A.; Waters, A.K.; Kalyan, P.; Achrol, A.S.; Kesari, S.; Yenugonda, V.M. Lipid–polymer hybrid nanoparticles as a next-generation drug delivery platform: State of the art, emerging technologies, and perspectives. Int. J. Nanomed. 2019, 14, 1937. [Google Scholar] [CrossRef]
- Pardi, N.; Hogan, M.J.; Porter, F.W.; Weissman, D. mRNA vaccines—A new era in vaccinology. Nat. Rev. Drug Discov. 2018, 17, 261–279. [Google Scholar] [CrossRef]
- Goyal, A.K.; Singh, R.; Chauhan, G.; Rath, G. Non-invasive systemic drug delivery through mucosal routes. Artif. Cells Nanomed. Biotechnol. 2018, 46, 539–551. [Google Scholar] [CrossRef]
- Bajracharya, R.; Song, J.G.; Back, S.Y.; Han, H.-K. Recent advancements in non-invasive formulations for protein drug delivery. Comput. Struct. Biotechnol. J. 2019, 17, 1290–1308. [Google Scholar] [CrossRef]
- Guilherme, V.A.; Ribeiro, L.N.; Tofoli, G.R.; Franz-Montan, M.; de Paula, E.; de Jesus, M.B. Current challenges and future of lipid nanoparticles formulations for topical drug application to oral mucosa, skin, and eye. Curr. Pharm. Des. 2017, 23, 6659–6675. [Google Scholar] [CrossRef]
- Teelavath, M.; Patnaik, K.R. Review on Buccal Adhesive Drug Delivery System: A Promising Strategy for Poorly Soluble Drugs. J. Drug Deliv. Ther. 2019, 9, 778–792. [Google Scholar]
- Meraj Anjum, M.; Kanoujia, J.; Parashar, P.; Arya, M.; K Yadav, A.; A Saraf, S. Evaluation of a polymer-lipid-polymer system utilising hybrid nanoparticles of dapsone as a novel antiacne agent. Curr. Drug Ther. 2016, 11, 86–100. [Google Scholar] [CrossRef]
- Helal, N.A.; Eassa, H.A.; Amer, A.M.; Eltokhy, M.A.; Edafiogho, I.; Nounou, M.I. Nutraceuticals’ Novel Formulations: The Good, the Bad, the Unknown and Patents Involved. Recent Pat. Drug Deliv. Formul. 2019, 13, 105–156. [Google Scholar] [PubMed]
- Mieszawska, A.J.; Kim, Y.; Gianella, A.; van Rooy, I.; Priem, B.; Labarre, M.P.; Ozcan, C.; Cormode, D.P.; Petrov, A.; Langer, R.; et al. Synthesis of Polymer–Lipid Nanoparticles for Image-Guided Delivery of Dual Modality Therapy. Bioconjugate Chem. 2013, 24, 1429–1434. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.; Messaoud, G.B.; Michaux, F.; Tamayol, A.; Kahn, C.J.; Belhaj, N.; Linder, M.; Arab-Tehrany, E. Chitosan-coated liposomes encapsulating curcumin: Study of lipid–polysaccharide interactions and nanovesicle behavior. RSC Adv. 2016, 6, 45290–45304. [Google Scholar] [CrossRef]
- Tan, C.; Feng, B.; Zhang, X.; Xia, W.; Xia, S. Biopolymer-coated liposomes by electrostatic adsorption of chitosan (chitosomes) as novel delivery systems for carotenoids. Food Hydrocoll. 2016, 52, 774–784. [Google Scholar] [CrossRef]
- Cuomo, F.; Lopez, F.; Piludu, M.; Miguel, M.G.; Lindman, B.; Ceglie, A. Release of small hydrophilic molecules from polyelectrolyte capsules: Effect of the wall thickness. J. Colloid Interface Sci. 2015, 447, 211–216. [Google Scholar] [CrossRef]
- Van Tran, V.; Moon, J.-Y.; Lee, Y.-C. Liposomes for delivery of antioxidants in cosmeceuticals: Challenges and development strategies. J. Control. Release 2019, 300, 114–140. [Google Scholar] [CrossRef]
- Zhang, L.; Chan, J.M.; Gu, F.X.; Rhee, J.-W.; Wang, A.Z.; Radovic-Moreno, A.F.; Alexis, F.; Langer, R.; Farokhzad, O.C. Self-assembled lipid− polymer hybrid nanoparticles: A robust drug delivery platform. ACS Nano 2008, 2, 1696–1702. [Google Scholar] [CrossRef]
- Dehaini, D.; Fang, R.H.; Luk, B.T.; Pang, Z.; Hu, C.-M.J.; Kroll, A.V.; Yu, C.L.; Gao, W.; Zhang, L. Ultra-small lipid–polymer hybrid nanoparticles for tumor-penetrating drug delivery. Nanoscale 2016, 8, 14411–14419. [Google Scholar] [CrossRef]
- Liu, J.; Cheng, H.; Le Han, Z.Q.; Zhang, X.; Gao, W.; Zhao, K.; Song, Y. Synergistic combination therapy of lung cancer using paclitaxel-and triptolide-coloaded lipid–polymer hybrid nanoparticles. Drug Des. Dev. Ther. 2018, 12, 3199. [Google Scholar] [CrossRef] [PubMed]
- Tahir, N.; Madni, A.; Balasubramanian, V.; Rehman, M.; Correia, A.; Kashif, P.M.; Mäkilä, E.; Salonen, J.; Santos, H.A. Development and optimization of methotrexate-loaded lipid-polymer hybrid nanoparticles for controlled drug delivery applications. Int. J. Pharm. 2017, 533, 156–168. [Google Scholar] [CrossRef] [PubMed]
- Leng, D.; Thanki, K.; Fattal, E.; Foged, C.; Yang, M. Engineering of budesonide-loaded lipid-polymer hybrid nanoparticles using a quality-by-design approach. Int. J. Pharm. 2018, 548, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, A.; Mehta, S.; Yadav, S.; Singh, S.K.; Grobler, A.; Goyal, A.K.; Mehta, A. Pulmonary delivery of antitubercular drugs using spray-dried lipid–polymer hybrid nanoparticles. Artif. Cells Nanomed. Biotechnol. 2016, 44, 1544–1555. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Xue, J.; Hu, Q.; Zhou, M.; Chang, C.; Luo, Y. Synthetic surfactant-and cross-linker-free preparation of highly stable lipid-polymer hybrid nanoparticles as potential oral delivery vehicles. Sci. Rep. 2017, 7, 1–15. [Google Scholar]
- Takami, E.A.; Erogbogbo, F. Microfluidic synthesis of lipid-polymer hybrid nanoparticles for targeted drug delivery. MRS Adv. 2016, 1, 2155–2160. [Google Scholar] [CrossRef]
- Wei, W.; Sun, J.; Guo, X.-Y.; Chen, X.; Wang, R.; Qiu, C.; Zhang, H.-T.; Pang, W.-H.; Wang, J.-C.; Zhang, Q. Microfluidic-Based Holonomic Constraints of siRNA in the Kernel of Lipid/Polymer Hybrid Nanoassemblies for Improving Stable and Safe In Vivo Delivery. ACS Appl. Mater. Inter. 2020, 12, 14839–14854. [Google Scholar] [CrossRef]
- Dormenval, C.; Lokras, A.; Cano-Garcia, G.; Wadhwa, A.; Thanki, K.; Rose, F.; Thakur, A.; Franzyk, H.; Foged, C. Identification of factors of importance for spray drying of small interfering RNA-loaded lipidoid-polymer hybrid nanoparticles for inhalation. Pharm. Res. 2019, 36, 142. [Google Scholar] [CrossRef]
- Bokare, A.; Takami, A.; Kim, J.H.; Dong, A.; Chen, A.; Valerio, R.; Gunn, S.; Erogbogbo, F. Herringbone-Patterned 3D-Printed Devices as Alternatives to Microfluidics for Reproducible Production of Lipid Polymer Hybrid Nanoparticles. ACS Omega 2019, 4, 4650–4657. [Google Scholar] [CrossRef]
- Germain, M.; Caputo, F.; Metcalfe, S.; Tosi, G.; Spring, K.; Åslund, A.K.; Pottier, A.; Schiffelers, R.; Ceccaldi, A.; Schmid, R. Delivering the power of nanomedicine to patients today. J. Control. Release 2020, 326, 164–171. [Google Scholar] [CrossRef]
- Barba, A.A.; Bochicchio, S.; Dalmoro, A.; Lamberti, G. Lipid Delivery Systems for Nucleic-Acid-Based-Drugs: From Production to Clinical Applications. Pharmaceutics 2019, 11, 360. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Ping, Q.; Wei, Y.; Lai, J. Hypoglycemic efficacy of chitosan-coated insulin liposomes after oral administration in mice. Acta Pharm. Sin. 2004, 25, 966–972. [Google Scholar]
- Gradauer, K.; Barthelmes, J.; Vonach, C.; Almer, G.; Mangge, H.; Teubl, B.; Roblegg, E.; Dünnhaupt, S.; Fröhlich, E.; Bernkop-Schnürch, A. Liposomes coated with thiolated chitosan enhance oral peptide delivery to rats. J. Control. Release 2013, 172, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, I.; Smistad, G.; Karlsen, J. Interactions between liposomes and chitosan. Int. J. Pharm. 1994, 101, 227–236. [Google Scholar] [CrossRef]
- Bochicchio, S.; Dalmoro, A.; Bertoncin, P.; Lamberti, G.; Moustafine, R.I.; Barba, A.A. Design and production of hybrid nanoparticles with polymeric-lipid shell–core structures: Conventional and next-generation approaches. RSC Adv. 2018, 8, 34614–34624. [Google Scholar] [CrossRef]
- Tai, K.; Rappolt, M.; Mao, L.; Gao, Y.; Li, X.; Yuan, F. The stabilization and release performances of curcumin-loaded liposomes coated by high and low molecular weight chitosan. Food Hydrocoll. 2020, 99, 105355. [Google Scholar] [CrossRef]
- Badawi, A.A.; El-Laithy, H.M.; El Qidra, R.K.; El Mofty, H.; El Dally, M. Chitosan based nanocarriers for indomethacin ocular delivery. Arch. Pharmacal. Res. 2008, 31, 1040–1049. [Google Scholar] [CrossRef]
- Jøraholmen, M.W.; Vanić, Ž.; Tho, I.; Škalko-Basnet, N. Chitosan-coated liposomes for topical vaginal therapy: Assuring localized drug effect. Int. J. Pharm. 2014, 472, 94–101. [Google Scholar] [CrossRef]
- Park, S.N.; Jo, N.R.; Jeon, S.H. Chitosan-coated liposomes for enhanced skin permeation of resveratrol. J. Ind. Eng. Chem. 2014, 20, 1481–1485. [Google Scholar] [CrossRef]
- Mady, M.M.; Darwish, M.M. Effect of chitosan coating on the characteristics of DPPC liposomes. J. Adv. Res. 2010, 1, 187–191. [Google Scholar] [CrossRef]
- Hao, J.; Guo, B.; Yu, S.; Zhang, W.; Zhang, D.; Wang, J.; Wang, Y. Encapsulation of the flavonoid quercetin with chitosan-coated nano-liposomes. Lwt-Food Sci. Technol. 2017, 85, 37–44. [Google Scholar] [CrossRef]
- Li, Z.; Paulson, A.T.; Gill, T.A. Encapsulation of bioactive salmon protein hydrolysates with chitosan-coated liposomes. J. Funct. Foods 2015, 19, 733–743. [Google Scholar] [CrossRef]
- Rengel, R.G.; Barišić, K.; Pavelić, Ž.; Grubišić, T.Ž.; Čepelak, I.; Filipović-Grčić, J. High efficiency entrapment of superoxide dismutase into mucoadhesive chitosan-coated liposomes. Eur. J. Pharm. Sci. 2002, 15, 441–448. [Google Scholar] [CrossRef]
- Deygen, I.M.; Seidl, C.; Kölmel, D.K.; Bednarek, C.; Heissler, S.; Kudryashova, E.V.; Bräse, S.; Schepers, U. Novel Prodrug of Doxorubicin Modified by Stearoylspermine Encapsulated into PEG-Chitosan-Stabilized Liposomes. Langmuir 2016, 32, 10861–10869. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.X.; Huang, L.; Liu, L.; Abdalla, A.M.E.; Gauthier, M.; Yang, G. Chitosan-coated nano-liposomes for the oral delivery of berberine hydrochloride. J. Mater. Chem. B 2014, 2, 7149–7159. [Google Scholar] [CrossRef]
- Otake, K.; Shimomura, T.; Goto, T.; Imura, T.; Furuya, T.; Yoda, S.; Takebayashi, Y.; Sakai, H.; Abe, M. One-step preparation of chitosan-coated cationic liposomes by an improved supercritical reverse-phase evaporation method. Langmuir 2006, 22, 4054–4059. [Google Scholar] [CrossRef]
- Bochicchio, S.; Dalmoro, A.; Recupido, F.; Lamberti, G.; Barba, A.A. Nanoliposomes production by a protocol based on a simil-microfluidic approach. In Advances in Bionanomaterials; Springer: Berlin/Heidelberg, Germany, 2018; pp. 3–10. [Google Scholar]
- Barba, A.A.; Bochicchio, S.; Bertoncin, P.; Lamberti, G.; Dalmoro, A. Coating of Nanolipid Structures by a Novel Simil-Microfluidic Technique: Experimental and Theoretical Approaches. Coatings 2019, 9, 491. [Google Scholar] [CrossRef]

| Abbreviation | Full Name |
|---|---|
| PLGA | poly(lactic-co-glycolic acid) |
| PLA | poly(lactic acid) |
| PCL | polycaprolactone |
| PEG | polyethylene glycol |
| PHEMA | poly hydroxyethyl methacrylate |
| PHPMA | poly(2-hydroxypropyl methacrylate) |
| PVA | polyvinyl alcohol |
| PNIPAm | poly(N-isopropylacrylamide) |
| PAA | poly(amidoamine) |
| PEI | polyethyleneimine |
| PBAE | poly-(β-amino ester) |
| Abbreviation | Full Name |
|---|---|
| Chol | cholesterol |
| PC | soybean phosphatidylcholine |
| DPPC | 1,2-dipalmitoyl-sn-glycero-3-phosphocholine |
| DSPE | 1,2-distearoyl-sn-glycero-3-phosphoethanolamine |
| DSPC | 1,2-distearoyl-sn-glycero-3-phosphocholine |
| DMPC | 1,2-dimyristoleoyl-sn-glycero-3-ethylphosphocholine |
| DOPE | 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine |
| DOPC | 1,2-dioleoyl-sn-glycero-3-phosphocholine |
| POPC | 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine |
| HSPC | hydrogenated soy phosphatidylcholine |
| PE | phosphor-ethanolamine |
| DOTAP | 1,2-dioleoyl-3-trimethylammonium propane |
| DPTAP | 1,2-dipalmitoyl-3-trimethylammonium-propane |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bochicchio, S.; Lamberti, G.; Barba, A.A. Polymer–Lipid Pharmaceutical Nanocarriers: Innovations by New Formulations and Production Technologies. Pharmaceutics 2021, 13, 198. https://doi.org/10.3390/pharmaceutics13020198
Bochicchio S, Lamberti G, Barba AA. Polymer–Lipid Pharmaceutical Nanocarriers: Innovations by New Formulations and Production Technologies. Pharmaceutics. 2021; 13(2):198. https://doi.org/10.3390/pharmaceutics13020198
Chicago/Turabian StyleBochicchio, Sabrina, Gaetano Lamberti, and Anna Angela Barba. 2021. "Polymer–Lipid Pharmaceutical Nanocarriers: Innovations by New Formulations and Production Technologies" Pharmaceutics 13, no. 2: 198. https://doi.org/10.3390/pharmaceutics13020198
APA StyleBochicchio, S., Lamberti, G., & Barba, A. A. (2021). Polymer–Lipid Pharmaceutical Nanocarriers: Innovations by New Formulations and Production Technologies. Pharmaceutics, 13(2), 198. https://doi.org/10.3390/pharmaceutics13020198