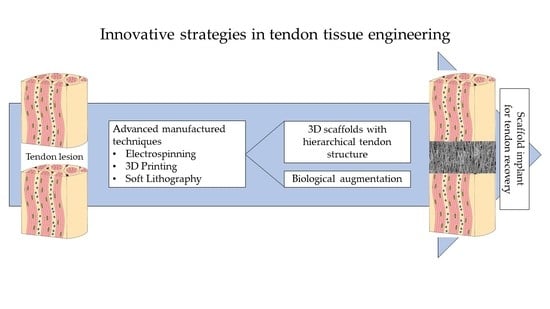
Innovative Strategies in Tendon Tissue Engineering
Abstract
1. Introduction
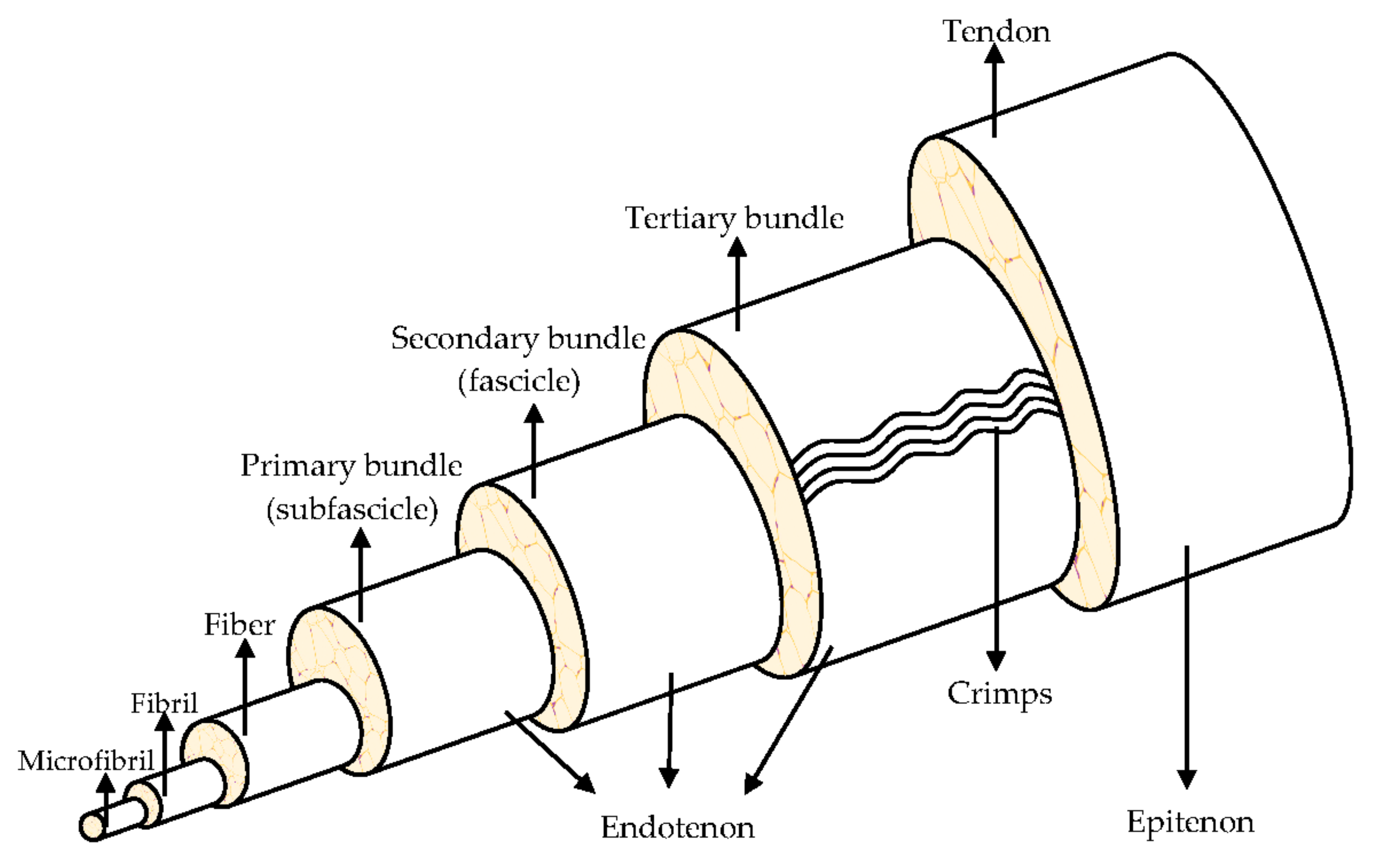
2. Tendon Structure and Metabolism
3. Tendon Cellular Component and ECM
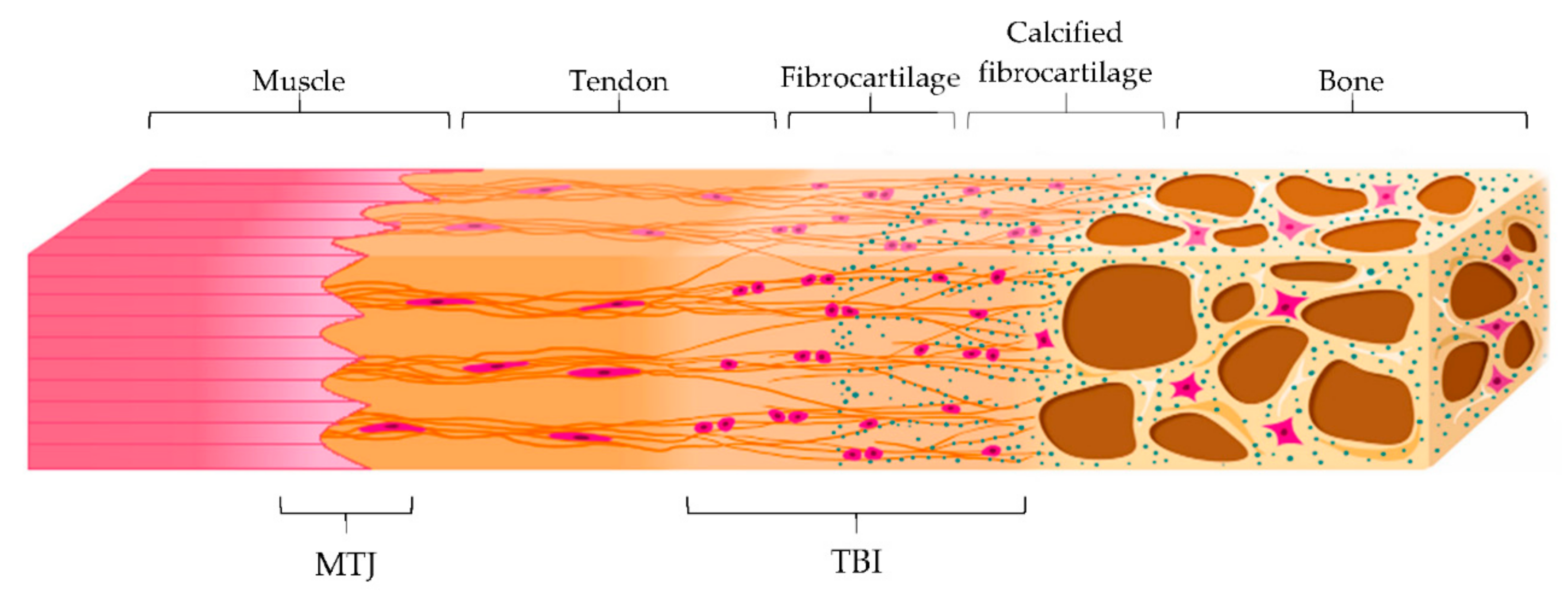
4. Tendon-Bone Insertion (TBI) and Myotendinous Junction (MTJ)
5. Tendon Mechanical Properties
6. Tendon Injuries
7. Traditional Approaches for the Treatment of Injuries
8. New Strategies for the Treatment of Injuries: Tissue Engineering
8.1. Tendon-Specific Stem and Progenitor Cells (TSPCs) Therapy
8.2. 3D Scaffolds
8.2.1. Emerging Manufacturing Methods
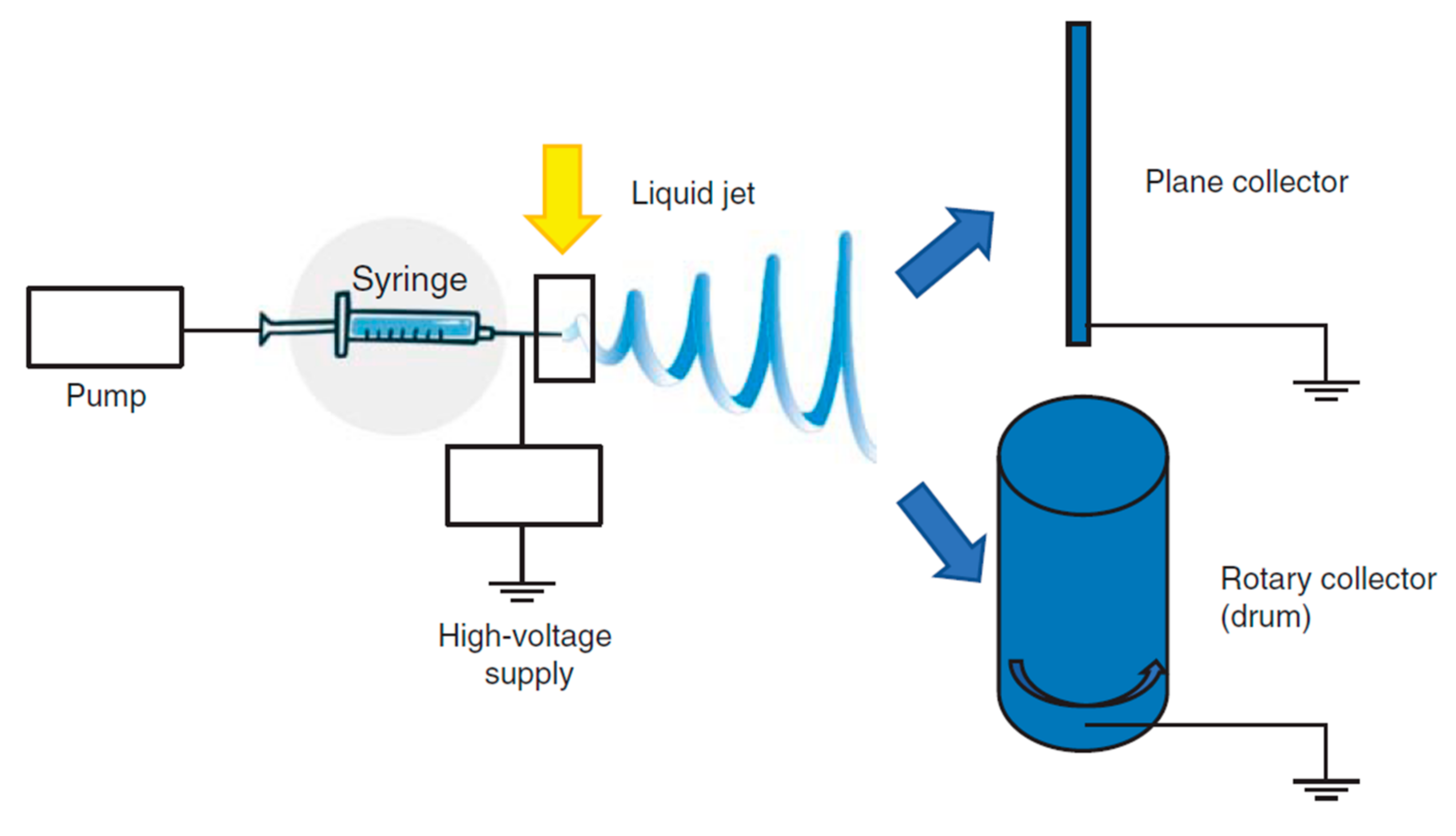
Electrospinning
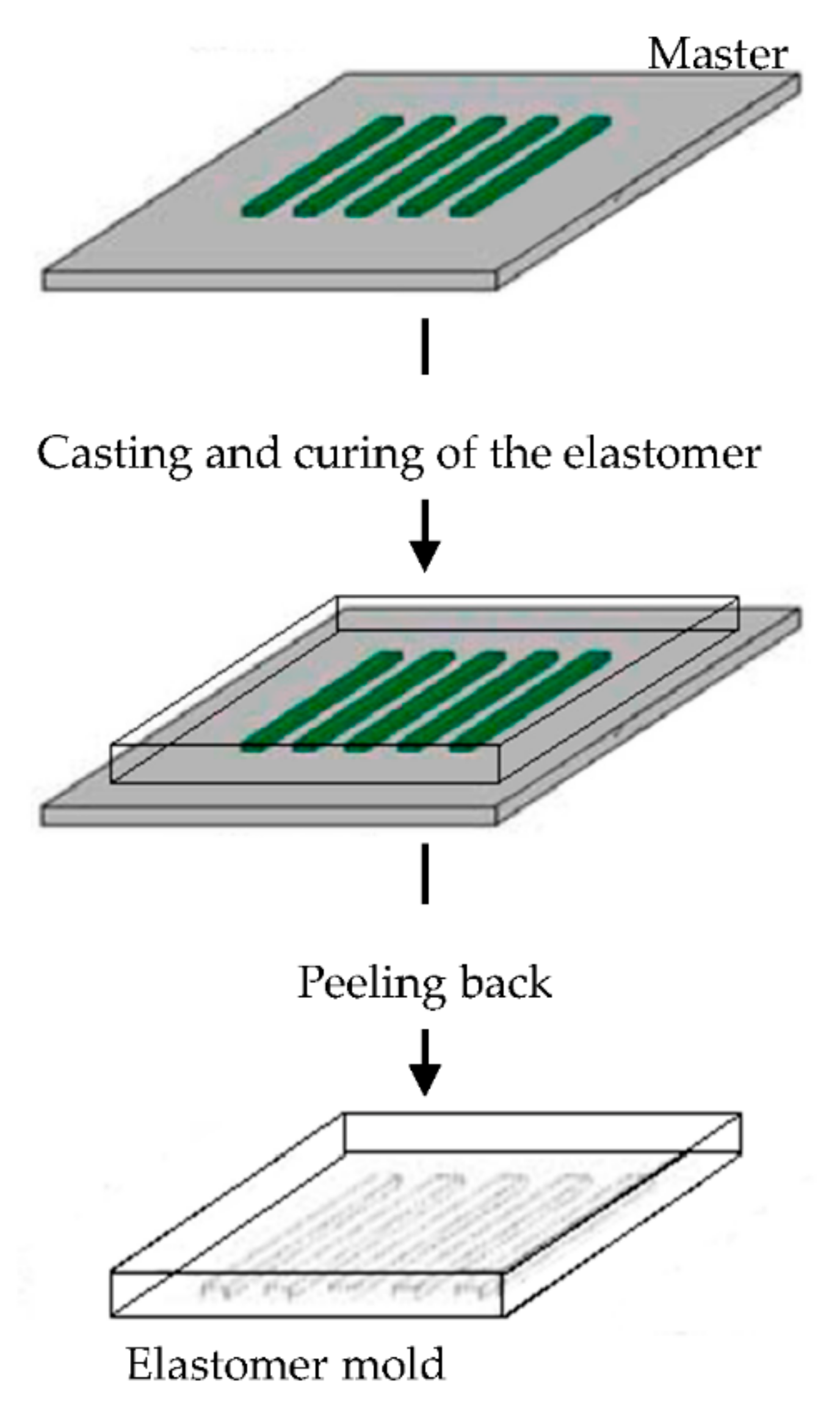
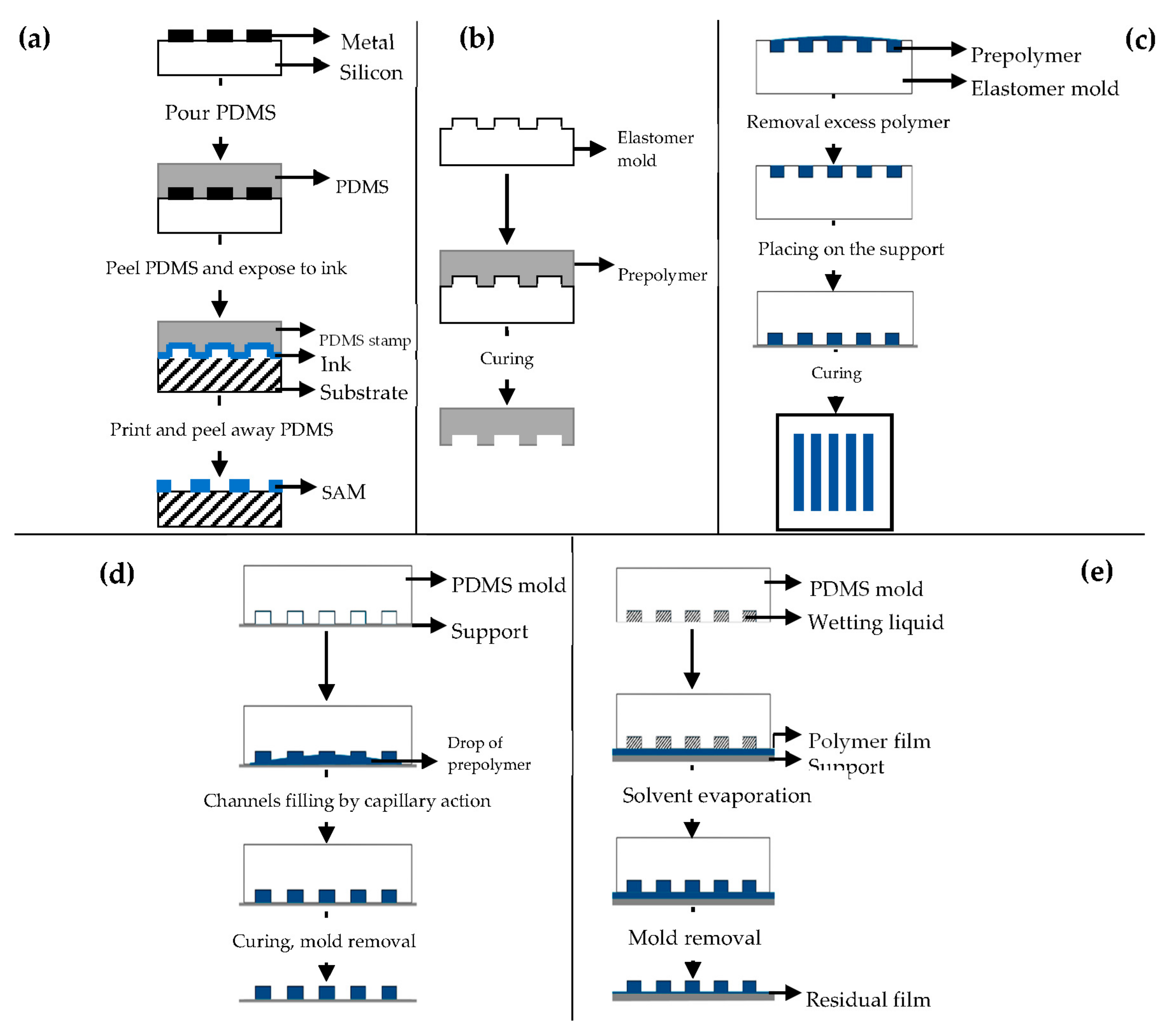
Soft Lithography
3D Printing
8.2.2. Materials
9. Biological Augmentation for Tendon Healing
10. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sigal, I.R.; Grande, D.A.; Dines, D.M.; Dines, J.; Drakos, M. Biologic and Tissue Engineering Strategies for Tendon Repair. Regen. Eng. Transl. Med. 2016, 2, 107–125. [Google Scholar] [CrossRef]
- Wu, F.; Nerilich, M.; Docheva, D. Tendon injuries: Basic science and new repair proposals. Effort. Open Rev. 2017, 2, 332–342. [Google Scholar] [CrossRef] [PubMed]
- Lian, Ø.B.; Engebretsen, L.; Bahr, R. Prevalence of jumper’s knee among elite athletes from different sports: A cross-sectional study. Am. J. Sports Med. 2005, 33. [Google Scholar] [CrossRef] [PubMed]
- Peers, K.H.E.; Lysens, R.J.J. Patellar tendinopathy in athletes. Sports Med. 2005, 35, 71–87. [Google Scholar] [CrossRef] [PubMed]
- Tonoli, C.; Cumps, E.; Aerts, I.; Meeusen, R. Incidence, risk factors and prevention of running related injuries in long distance running: A systematic review. Sport Geneeskd. 2010, 43, 12–18. [Google Scholar] [CrossRef]
- Min, H.K.; Oh, S.H.; Lee, J.M.; Im, G.I.; Lee, J.H. Porous membrane with reverse gradients of PDGF-BB and BMP-2 for tendon-to-bone repair: In vitro evaluation on adipose-derived stem cell differentiation. Acta Biomater. 2014, 10, 1272–1279. [Google Scholar] [CrossRef]
- Zumstein, M.A.; Jost, B.; Hempel, J.; Hodler, J.; Gerber, C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J. Bone Jt. Surg. 2008, 90, 2423–2431. [Google Scholar] [CrossRef]
- Benjamin, M.; Ralphs, J.R. The cell and developmental biology of tendons and ligaments. Int. Rev. Cytol. 2000, 196, 85–130. [Google Scholar] [CrossRef]
- Kannus, P. Structure of the tendon connective tissue. Scand J. Med. Sci. Sports 2000, 10, 312–320. [Google Scholar] [CrossRef]
- Tempfer, H.; Lehner, C.; Grütz, M.; Gehwolf, R.; Traweger, A. Biological Augmentation for Tendon Repair: Lessons to be Learned from Development, Disease, and Tendon Stem Cell Research. Cell Eng. Regen. 2017, 1–31. [Google Scholar] [CrossRef]
- Canty, E.G.; Kadler, K. Collagen fibril biosynthesis in tendon: A review and recent insights. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2002, 133, 979–985. [Google Scholar] [CrossRef]
- Sharma, P.; Maffulli, N. Basic biology of tendon injury and healing. Surg. J. R Coll. Surg. E 2005, 3, 309–316. [Google Scholar] [CrossRef]
- Franchi, M.; Trirè, A.; Quaranta, M.; Orsini, E.; Ottani, V. Collagen Structure of Tendon Relates to Function. Sci. World J. 2007, 7, 404–420. [Google Scholar] [CrossRef] [PubMed]
- Roshan, J.; Kesturu, S.G.; Balian, G.; Chhabra, B. Tendon: Biology, Biomechanics, Repair, Growth Factors, and Evolving Treatment Options. J. Hand Surg. 2008, 33, 102–112. [Google Scholar] [CrossRef]
- Zhang, C.; Zhu, J.; Zhou, Y.; Thampatty, B.P.; Wang, J.H.-C. Tendon Stem/Progenitor Cells and Their Interactions with Extracellular Matrix and Mechanical Loading. Stem Cells Int. 2019, 2019. [Google Scholar] [CrossRef]
- Bi, Y.; Ehirchiou, D.; Kilts, T.M.; Inkson, C.A.; Embree, M.C.; Sonoyama, W.; Li, L.; Leet, A.I.; Seo, B.M.; Zhang, L.; et al. Identification of tendon stem/progenitor cells and the role of the extracellular matrix in their niche. Nat. Med. 2007, 13, 1219–1227. [Google Scholar] [CrossRef]
- Salingcarnboriboon, R.; Yoshitake, H.; Tsuji, K.; Obinata, M.; Amagasa, T.; Nifuji, A.; Noda, M. Establishment of tendon-derived cell lines exhibiting pluripotent mesenchymal stem cell-like property. Exp. Cell Res. 2003, 287, 289–300. [Google Scholar] [CrossRef]
- Tempfer, H.; Wagner, A.; Gehwolf, R.; Lehner, C.; Tauber, M.; Resch, H.; Bauer, H.C. Perivascular cells of the supraspinatus tendon express both tendon- and stem cell-related markers. Histochem. Cell Biol. 2009, 131, 733–741. [Google Scholar] [CrossRef]
- Stanley, R.L.; Fleck, R.A.; Becker, D.L.; Goodship, A.E.; Ralphs, J.R.; Patterson-Kane, J.C. Gap junction protein expression and cellularity: Comparison of immature and adult equine digital tendons. J. Anat. 2007, 211, 325–334. [Google Scholar] [CrossRef]
- Schiele, N.R.; Marturano, J.E.; Kuo, C.K. Mechanical factors in embryonic tendon development: Potential cues for stem cell tenogenesis. Curr. Opin. Biotechnol. 2013, 24, 834–840. [Google Scholar] [CrossRef]
- Schwartz, M.A. Integrins and Extracellular Matrix in Mechanotransduction. Cold Spring Harb. Perspect Biol. 2010, 2, a005066. [Google Scholar] [CrossRef] [PubMed]
- Popov, C.; Burggraf, M.; Kreja, L.; Ignatius, A.; Schieker, M.; Docheva, D. Mechanical stimulation of human tendon stem/progenitor cells results in upregulation of matrix proteins, integrins and MMPs, and activation of p38 and ERK1/2 kinases. BMC Mol. Biol. 2015, 16. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, J.H. Mechanobiological response of tendon stem cells: Implications of tendon homeostasis and pathogenesis of tendinopathy. J. Orthop. Res. 2010, 28, 639–643. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, C.T.; Birch, H.L.; Clegg, P.D.; Screen, H.R. The role of the non-collagenous matrix in tendon function. Int. J. Exp. Pathol. 2013, 94, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Pajala, A.; Melkko, J.; Leppilahti, J.; Ohtonen, P.; Soini, Y.; Risteli, J. Tenascin-C and type I and III collagen expression in total Achilles tendon rupture. An immunohistochemical study. Histol. Histopathol. 2009, 24, 1207–1211. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, H.F.; Felisbino, S.L.; Covizi, D.Z.; Della Colleta, H.H.; Gomes, L. Structure and proteoglycan composition of specialized regions of the elastic tendon of the chicken wing. Cell Tissue Res. 2000, 300, 435–446. [Google Scholar] [CrossRef]
- Smith, R.K.; Zunino, L.; Webbon, P.M.; Heinegard, D. The distribution of cartilage oligomeric matrix protein (COMP) in tendon and its variation with tendon site, age and load. Matrix Biol. 1997, 16, 255–271. [Google Scholar] [CrossRef]
- Matos, A.M.; Gonçalves, A.I.; El Haj, A.J.; Gomes, M.E. Magnetic biomaterials and nano-instructive tools as mediators of tendon mechanotransduction. Nanoscale Adv. 2020, 2, 140. [Google Scholar] [CrossRef]
- Felsenthal, N.; Zelzer, E. Mechanical regulation of musculoskeletal system development. Development 2017, 144, 4271–4283. [Google Scholar] [CrossRef]
- Friese, N.; Gierschner, M.B.; Schadzek, P.; Roger, Y.; Hoffmann, A. Regeneration of damaged tendon-bone junctions (entheses)—TAK1 as a potential node factor. Int. J. Mol. Sci. 2020, 21, 5177. [Google Scholar] [CrossRef]
- Apostolakos, J.; Durant, T.J.S.; Dwyer, C.R.; Russell, R.P.; Weinreb, J.H.; Alaee, F.; Beitzel, K.; McCarthy, M.B.; Cote, M.P.; Mazzocca, A.D. The enthesis: A review of the tendon-to-bone insertion. Muscle Ligaments Tendons J. 2014, 4, 333–342. [Google Scholar] [CrossRef]
- Snedeker, J.G.; Foolen, J. Tendon injury and repair—A perspective on the basic mechanisms of tendon disease and future clinical therapy. Acta Biomater. 2017, 63, 18–36. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, P.; Hansen, P.; Kjær, M. Tendon properties in relation to muscular activity and physical training. Scand J. Med. Sci. Sports 2002, 13, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.L.; Liau, L.L.; Ng, M.H.; Chowdhury, S.R.; Law, J.X. Current progress in tendon and ligament tissue engineering. Tissue Eng. Regen. Med. 2019, 16, 549–571. [Google Scholar] [CrossRef]
- Screen, H.R.C.; Bader, D.L.; Lee, D.A.; Shelton, J.C. Local Strain Measurement within Tendon. Strain 2004, 40, 157–163. [Google Scholar] [CrossRef]
- Tero, A.H.J.; Teppo, L.N.J.; Pekka, K.; Làszò, J.; Markku, J. Collagen fibres of the spontaneously ruptured human tendons display decreased thickness and crimp angle. J. Orthop. 2006, 22, 1303–1309. [Google Scholar] [CrossRef]
- Andrades, J.A.; Claros, S.; Jiménez-Palomo, P.; López-Puertas, J.M.; Zamora-Navas, P.; Guerado, E.; Monleón, M.; Araque, M.C.; Becerra, J. Skeletal Regeneration by Mesenchymal Stem Cells: What Else? Regen. Med. Tissue Eng. Cells Biomater. 2011. Available online: https://www.intechopen.com/books/regenerative-medicine-and-tissue-engineering-cells-and-biomaterials/skeletal-regeneration-by-mesenchymal-stem-cells-what-else-?cid=social_20150505_45207456&adbid=595591418732683264&adbpl=tw&adbpr=38225654 (accessed on 24 September 2020). [CrossRef]
- Lin, T.W.; Cardenas, L.; Soslowsky, L.J. Biomechanics of tendon injury and repair. J. Biomech. 2004, 37, 865–877. [Google Scholar] [CrossRef]
- Voleti, P.B.; Buckley, M.R.; Soslowsky, L.J. Tendon Healing: Repair and Regeneration. Annu. Rev. Biomed. Eng. 2012, 14, 47–71. [Google Scholar] [CrossRef]
- Rees, J.D.; Stride, M.; Scott, A. Tendons—Time to revisit inflammation. Br. J. Sports Med. 2014, 48, 1553–1557. [Google Scholar] [CrossRef]
- D’Addona, A.; Maffulli, N.; Formisano, S.; Rosa, D. Inflammation in tendinopathy. Surgeon 2017, 15, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Morita, W.; Snelling, S.J.; Dakin, S.G.; Carr, A.J. Profibrotic mediators in tendon disease: A systematic review. Arthritis Res. 2016, 18, 269. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.K.H.; Ng, G.Y.F.; Mak, A.F.T. Effects of knee bracing on the sensorimotor function of subjects with Anterior Cruciate Ligament reconstruction. Am. J. Sports Med. 2001, 29, 641–645. [Google Scholar] [CrossRef] [PubMed]
- Abate, M.; Silbernagel, K.G.; Siljeholm, C.; Di Iorio, A.; De Amicis, D.; Salini, V.; Werner, S.; Paganelli, R. Pathogenesis of tendinopathies: Inflammation or degeneration? Arthritis Res. 2009, 11, 235. [Google Scholar] [CrossRef]
- Weiler, A.; Scheffler, S.; Apreleva, M. Healing of Ligament and Tendon to Bone. In Repair and Regeneration of Ligaments, Tendons, and Joint Capsule; Humana Press: Totowa, NJ, USA, 2006; pp. 201–231. [Google Scholar]
- Szczeny, S.E.; Peloquin, J.M.; Cortes, D.H.; Kadlowec, J.A.; Soslowky, L.J.; Elliott, D.M. Biaxial Tensile Testing and Constitutive Modeling of Human Supraspinatus Tendon. J. Biomech. Eng. 2012, 134, 21004. [Google Scholar] [CrossRef] [PubMed]
- Weiler, A.; Hoffmann, R.F.G.; Bail, H.J.; Rehm, O.; Südkamp, N.P. Tendon healing in a bone tunnel. Part II: Histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy 2002, 18, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Walden, G.; Liao, X.; Donell, S.; Raxworthy, M.J.; Riley, G.P.; Saeed, A.A. Clinical, Biological, and Biomaterials Perspective into Tendon Injuries and Regeneration. Tissue Eng. Part B Rev. 2017, 23, 44–58. [Google Scholar] [CrossRef]
- Butler, D.L.; Juncosa, N.; Dressler, M.R. Functional Efficacy of Tendon Repair Processes. Annu. Rev. Biomed. Eng. 2004, 6, 303–329. [Google Scholar] [CrossRef]
- Reed, S.A.; Leahy, E.R. Growth and development symposium: Stem cell therapy in equine tendon injury. J. Anim. Sci. 2013, 91, 59–65. [Google Scholar] [CrossRef]
- Xie, R.G.; Zhang, S.; Tang, J.B.; Chen, F. Biomechanical studies of 3 different 6-strand flexor tendon repair techniques. J. Hand Surg. 2002, 27, 621–627. [Google Scholar] [CrossRef]
- Tang, J.B.; Wang, B.; Chen, F.; Pan, C.Z.; Xie, R.G. Biomechanical evaluation of flexor tendon repair techniques. Clin. Orthop. Relat. Res. 2001, 386, 252–259. [Google Scholar] [CrossRef]
- Veitch, A.; Firoozbakhsh, K.; Pribyl, C.R.; McNally, T. In vitro biomechanical evaluation of the double loop suture for flexor tendon repair. Clin. Orthop. 2000, 377, 228–234. [Google Scholar] [CrossRef]
- Silva, M.J.; Boyer, M.I.; Ditsios, K.; Burns, M.E.; Harwood, F.L.; Amiel, D.; Gelberman, R.H. The insertion site of the canine flexor digitorum profundus tendon heals slowly following injury and suture repair. J. Orthop. Res. 2002, 20, 447–453. [Google Scholar] [CrossRef]
- Zhao, C.; Amadio, P.C.; Momose, T.; Couvreur, P.; Zobitz, M.E.; An, K.N. The effect of suture technique on adhesion formation after flexor tendon repair for partial lacerations in a canine model. J. Trauma 2001, 51, 917–921. [Google Scholar] [CrossRef]
- Deng, S.; Sun, Z.; Zhang, C.; Chen, G.; Li, J. Surgical Treatment Versus Conservative Management for Acute Achilles Tendon Rupture: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Foot Ankle Surg. 2017, 56, 1236–1243. [Google Scholar] [CrossRef]
- Wang, J.H.-C.; Nirmala, X. Application of Tendon Stem/Progenitor Cells and Platelet-Rich Plasma to Treat Tendon Injuries. Oper. Tech. Orthop. 2016, 26, 68–72. [Google Scholar] [CrossRef][Green Version]
- Malgarim Cordenonsi, L.; Faccendini, A.; Rossi, S.; Bonferoni, M.C.; Malavasi, L.; Raffin, R.; Scherman Schapoval, E.E.; del Fante, C.; Vigani, B.; Miele, D.; et al. Platelet lysate loaded electrospun scaffolds: Effect of nanofiber types on wound healing. Eur. J. Pharm. Biopharm. 2019, 142, 247–257. [Google Scholar] [CrossRef]
- Rui, Y.F.; Lui, P.P.; Li, G.; Fu, S.C.; Lee, Y.W.; Chan, K.M. Isolation and characterization of multipotent rat tendon-derived stem cells. Tissue Eng. Part A 2010, 16, 1549–1558. [Google Scholar] [CrossRef]
- Ni, M.; Lui, P.P.Y.; Rui, Y.F.; Lee, Y.W.; Lee, Y.W.; Tan, Q.; Wong, Y.M.; Kong, S.K.; Lau, P.M.; Li, G.; et al. Tendon-derived stem cells (TDSCs) promote tendon repair in a rat patellar tendon window defect model. J. Orthop. Res. 2011, 30, 613–619. [Google Scholar] [CrossRef]
- Chen, J.; Yu, Q.; Wu, B.; Lin, Z.; Pavlos, N.J.; Xu, J.; Ouyang, H.; Wang, A.; Zheng, M.H. Autologous Tenocyte Therapy for Experimental Achilles Tendinopathy in a Rabbit Model. Tissue Eng. Part A 2011, 17, 2037–2048. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, J.H. Prostaglandin E2 (PGE2) exerts biphasic effects on human tendon stem cells. PLoS ONE 2014, 9, e87706. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Akinbiyi, T.; Xu, L.; Ramcharan, M.; Leong, D.J.; Ros, S.J.; Colvin, A.C.; Schaffler, M.B.; Majeska, R.J.; Flatow, E.L.; et al. Tendon-derived stem/progenitor cell aging: Defective self-renewal and altered fate. Aging Cell 2010, 9, 911–915. [Google Scholar] [CrossRef] [PubMed]
- Butler, D.; Goldstein, S.; Guilak, F. Functional tissue engineering: The role of biomechanics. J. Biomech. Eng. 2000, 122, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Guilak, F.; Butler, D.L.; Goldstein, S.A.; Mooney, D. (Eds.) Functional Tissue Engineering; Springer: New York, NY, USA, 2003. [Google Scholar]
- Lanza, R.P.; Langer, R.S.; Vacanti, J. (Eds.) Principles of Tissue Engineering; Academic Press: San Diego, CA, USA, 2000. [Google Scholar]
- O’Brien, F.J. Biomaterials & scaffolds for tissue engineering. Mater. Today 2011, 14, 88–95. [Google Scholar] [CrossRef]
- Caramella, C.; Conti, B.; Modena, T.; Ferrari, F.; Bonferoni, M.C.; Genta, I.; Rossi, S.; Torre, M.L.; Sandri, G.; Sorrenti, M.; et al. Controlled delivery systems for tissue repair and regeneration. J. Drug. Deliv. Sci. Technol. 2016, 32, 206–228. [Google Scholar] [CrossRef]
- Verdiyeva, G.; Koshy, K.; Glibbery, N.; Mann, H.; Seifalian, A.M. Tendon Reconstruction with Tissue Engineering Approach: A Review. J. Biomed. Nanotechnol. 2015, 11, 1495–1523. [Google Scholar] [CrossRef]
- Sandri, G.; Bonferoni, M.C.; Rossi, S.; Ferrari, F.; Aguzzi, C.; Viseras, C.; Caramella, C. Clay minerals for tissue regeneration, repair, and engineering. Wound Health Biomater. 2016, 2, 385–402. [Google Scholar]
- Sensini, A.; Cristofolini, L. Biofabrication of Electrospun Scaffolds for the Regeneration of Tendons and Ligaments. Materials 2018, 11, 1963. [Google Scholar] [CrossRef]
- Sandri, G.; Rossi, S.; Bonferoni, M.C.; Caramella, C.; Ferrari, F. Electrospinning Technologies in Wound Dressing Applications. In Therapeutic Dressings and Wound Healing Applications, 1st ed.; Boateng, J., Ed.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2020; Volume 14, pp. 315–336. [Google Scholar] [CrossRef]
- Ruggeri, M.; Bianchi, E.; Rossi, S.; Vigani, B.; Bonferoni, M.C.; Caramella, C.; Sandri, G.; Ferrari, F. Nanotechnology-Based Medical Devices for the Treatment of Chronic Skin Lesions: From Research to the Clinic. Pharmaceutics 2020, 12, 815. [Google Scholar] [CrossRef]
- Baji, A.; Mai, Y.-W.; Wang, S.-C.; Abtahi, M.; Pei, C. Electrospinning of Polymer Nanofibers: Effects on Oriented Morphology, Structures and Tensile Properties. Compos. Sci. Technol. 2010, 70, 703–718. [Google Scholar] [CrossRef]
- Ding, B.; Kim, H.-Y.; Lee, S.-C.; Shao, C.-L.; Lee, D.-R.; Park, S.-J.; Kwag, G.-B.; Choi, K.-J. Preparation and characterization of a nanoscale poly(vinyl alcohol) fiber aggregate produced by an electrospinning method. J. Polym. Sci. Part B Polym. Phys. 2002, 40, 1261–1268. [Google Scholar] [CrossRef]
- Li, D.; Wang, Y.; Xia, Y. Electrospinning Nanofibers as Uniaxially Aligned Arrays and Layer-by-Layer Stacked Films. Adv. Mater. 2004, 16, 361–366. [Google Scholar] [CrossRef]
- Li, D.; Xia, Y. Electrospinning of nanofibers: Reinventing the wheel? Adv. Mater. 2004, 16, 1151–1170. [Google Scholar] [CrossRef]
- Dan, L.; McCann, J.T.; Younan, X.; Marquez, M. Electrospinning: A Simple and Versatile Technique for Producing Ceramic Nanofibers and Nanotubes. J. Am. Ceram. Soc. 2006, 89, 1861–1869. [Google Scholar] [CrossRef]
- Mit-uppatham, C.; Nithitanakul, M.; Supaphol, P. Ultrafine electrospun polyamide-6 fibers: Effect of solution conditions on morphology and Mean fiber diameter. Macromol. Chem. Phys. 2004, 205, 2327–2338. [Google Scholar] [CrossRef]
- Kumbar, S.G.; James, R.; Nukavarapu, S.P.; Laurencin, C.T. Electrospun nanofiber scaffolds: Engineering soft tissues. Biomed. Mater. 2008, 3. [Google Scholar] [CrossRef]
- Li, W.-J.; Laurencin, C.T.; Caterson, E.J.; Tuan, R.S.; Ko, F.K. Electrospun nanofibrous structure: A novel scaffold for tissue engineering. J. Biomed. Mater. Res. 2002, 60, 613–621. [Google Scholar] [CrossRef]
- Beachley, V.; Wen, X. Effect of electrospinning parameters on the nanofiber diameter and length. Mater. Sci. Eng. C 2008, 29, 663–668. [Google Scholar] [CrossRef]
- Sandri, G.; Miele, D.; Faccendini, A.; Bonferoni, M.C.; Rossi, S.; Grisoli, P.; Taglietti, A.; Ruggeri, M.; Bruni, G.; Vigani, B.; et al. Chitosan/Glycosaminoglycan Scaffolds: The Role of Silver Nanoparticles to Control Microbial Infections in Wound Healing. Polymers 2019, 11, 1207. [Google Scholar] [CrossRef]
- Smith, L.A.; Ma, P.X. Nano-fibrous scaffolds for tissue engineering. Colloids Surf. B Biointerfaces 2004, 39, 125–131. [Google Scholar] [CrossRef]
- Sheikh, F.A.; Macossay, J.; Cantu, T.; Zhang, X.; Shamshi Hassan, M.; Esther Salinas, M.; Farhangi, C.S.; Ahmad, H.; Kim, H.; Bowlin, G.L. Imaging, spectroscopy, mechanical, alignment and biocompatibility studies of electrospun medical grade polyurethane (Carbothane™ 3575A) nanofibers and composite nanofibers containing multiwalled carbon nanotubes. J. Mech. Behav. Biomed. Mater. 2014, 41, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Wang, X.; Zhang, E.; Wang, L.; Yuan, H.; Tu, W.; Zhang, H.; Yin, Z.; Shen, W.; Chen, X.; et al. An epigenetic bioactive composite scaffold with well-aligned nanofibers for functional tendon tissueengineering. Acta Biomater. 2017, 66, 141–156. [Google Scholar] [CrossRef] [PubMed]
- Domingues, R.M.A.; Goncalves, A.I.; Costa-Almeida, R.; Rodrigues, M.T.; Reis, R.L.; Gomes, M.E. Fabrication of Hierarchical and Biomimetic Fibrous Structures to Support the Regeneration of Tendon Tissues. Tendon Regen. Underst. Tissue Physiol. Dev. Eng. Funct. Substit. 2015, 259–277. [Google Scholar]
- Khademhosseini, A.; Langer, R. Microengineered hydrogels for tissue engineering. Biomaterials 2007, 28, 5087–5092. [Google Scholar] [CrossRef] [PubMed]
- Chung, B.G.; Lee, K.-H.; Khademhosseini, A.; Lee, S.-H. Microfluidic fabrication of microengineered hydrogels and their application in tissue engineering. Lab. Chip 2010, 12, 45–59. [Google Scholar] [CrossRef]
- Vozzi, G.; Flaim, C.; Ahluwalia, A.; Bhatia, S. Fabrication of PLGA scaffolds using soft lithography and microsyringe deposition. Biomaterials 2003, 24, 2533–2540. [Google Scholar] [CrossRef]
- Xia, Y.; Whitesides, G.M. Soft Lithography. Annu. Rev. Mater. Sci. 1998, 28, 153–184. [Google Scholar] [CrossRef]
- Whitesides, G.M.; Ostuni, E.; Takayama, S.; Jiang, X.; Ingber, D.E. Soft Lithography in biology and biochemistry. Annu. Rev. Biomed. Eng. 2001, 3, 335–373. [Google Scholar] [CrossRef]
- Qin, D.; Xin, Y.; Whitesides, G.M. Soft Lithography for micro-and nanoscale patterning. Nat. Protoc. 2010, 5, 491–502. [Google Scholar] [CrossRef]
- Rogers, J.A.; Nuzzo, R.G. Recent progress in Soft Lithography. Mater. Today 2005, 8, 50–56. [Google Scholar] [CrossRef]
- Odom, T.W.; Love, J.C.; Wolfe, D.B.; Paul, K.E.; Whitesides, G.M. Improved pattern transfer in Soft Lithography using composite stamps. Langmuir 2002, 18, 5314–5320. [Google Scholar] [CrossRef]
- Lomas, A.; English, A.; Biggs, M.; Pandit, A.; Zeugolis, D.I. Engineering Anisotropic 2D and 3D Structures for Tendon Repair and Regeneration. Tendon Regen. 2015, 225–242. [Google Scholar] [CrossRef]
- Zhu, J.; Li, J.; Wang, B.; Zhang, W.J.; Zhou, G.; Cao, Y.; Liu, W. The regulation of phenotype of cultured tenocytes by microgrooved surface structure. Biomaterials 2010, 31, 6952–6958. [Google Scholar] [CrossRef]
- Lima, M.J.; Correlo, V.M.; Reis, R.L. Micro/nano replication and 3D assembling techniques for scaffold fabrication. Mater. Sci Eng. C Mater. Biol. Appl. 2014, 42, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Ferdous, K.; Masaru, T.; Sheikh, R.A. Fabrication of polymeric biomaterials: A strategy for tissue engineering and medical devices. J. Mater. Chem. 2015, 3, 8224–8249. [Google Scholar] [CrossRef]
- Borenstein, J.T.; Terai, H.; King, K.R.; Weinberg, E.J.; Kaazempur-Mofrad, M.R.; Vacanti, J.P. Microfabrication Technology for Vascularized Tissue Engineering. Biomed. Microdevices 2002, 4, 167–175. [Google Scholar] [CrossRef]
- Zhao, X.-M.; Xia, Y.; Whitesides, G.M. Soft lithographic methods for nano-fabrication. J. Mater. Chem. 1997, 7, 1069–1074. [Google Scholar] [CrossRef]
- Yu, X.; Wang, Z.; Xing, R.; Luan, S.; Han, Y. Fabrication of structures with tunable morphologies and sizes by soft molding. Appl. Surf. Sci. 2005, 252, 1947–1953. [Google Scholar] [CrossRef]
- Bose, S.; Vahabzadeh, S.; Bandyopadhyay, A. Bone tissue engineering using 3D printing. Mater. Today 2013, 16, 496–504. [Google Scholar] [CrossRef]
- Leukers, B.; Gülkan, H.; Irsen, S.H.; Milz, S.; Tille, C.; Schieker, M.; Seitz, H. Hydroxyapatite scaffolds for bone tissue engineering made by 3D printing. J. Mater. Sci. Mater. Med. 2005, 16, 1121–1124. [Google Scholar] [CrossRef]
- Ahmed, T.A.E.; Dare, E.V.; Hincke, M. Fibrin: A Versatile Scaffold for Tissue Engineering Applications. Tissue Eng. Part B Rev. 2008, 14, 199–215. [Google Scholar] [CrossRef] [PubMed]
- Lima, M.J.; Pirraco, R.P.; Sousa, R.A.; Neves, N.M.; Marques, A.P.; Bhattacharya, M.; Correlo, V.M.; Reis, R.L. Bottom-up approach to construct microfabricated multi-layer scaffolds for bone tissue engineering. Biomed. Microdevices 2014, 16, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Inzana, J.A.; Olvera, D.; Fuller, S.M.; Kelly, J.P.; Graeve, O.A.; Schwarz, E.M.; Kates, S.L.; Awada, H.A. 3D Printing of Composite Calcium Phosphate and Collagen Scaffolds for Bone Regeneration. Biomaterials 2014, 35, 4026–4034. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.J.; West, J.L. Vascularization of Engineered Tissues: Approaches to Promote Angio-genesis in Biomaterials. Curr. Top. Med. Chem. 2008, 8, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wen, F.; Lim, P.N.; Zhang, Q.; Konishi, T.; Wang, D.; Teoh, S.H.; Thian, E.S. Nanomaterial scaffolds to regenerate musculoskeletal tissue: Signals from within for neovessel formation. Drug Discov. Today 2017, 22, 1385–1391. [Google Scholar] [CrossRef] [PubMed]
- Tarafder, S.; Balla, V.K.; Davies, N.M.; Bandyopadhyay, A.; Bose, S. Microwave-sintered 3D printed tricalcium phosphate scaffolds for bone tissue engineering. J. Tissue Eng. Regen. Med. 2012, 7, 631–641. [Google Scholar] [CrossRef]
- Wu, Y.; Fuh, J.Y.H.; Wong, Y.S.; Sun, J. Fabrication of 3D scaffolds via e-jet printing for tendon tissue repair. ASME Int. Manuf. Sci. Eng. Conf. 2015, 56833, V002T03A005. [Google Scholar] [CrossRef]
- Mozdzen, L.C.; Rodgers, R.; Banks, J.M.; Bailey, R.C.; Harley, B.A.C. Increasing the strength and bioactivity of collagen scaffolds using customizable arrays of 3D-printed polymer fibers. Acta Biomater. 2016, 33, 25–33. [Google Scholar] [CrossRef]
- Lin, J.; Zhou, W.; Han, S.; Bunpetch, V.; Zhao, K.; Liu, C.; Yin, Z.; Ouyang, H. Cell-material interactions in tendon tissue engineering. Acta Biomater. 2018, 70, 11. [Google Scholar] [CrossRef]
- Zhao, Z.; Liu, J.; Weir, M.D.; Zhang, N.; Zhang, L.; Xie, X.; Zhang, C.; Zhang, K.; Bai, Y.; Xu, H.H.K. Human periodontal ligament stem cells on calcium phosphate scaffold delivering platelet lysate to enhance bone regeneration. RSC Adv. 2019, 9, 41161–41172. [Google Scholar] [CrossRef]
- Santo, V.E.; Gomes, M.E.; Mano, J.F.; Reis, R.L. Chitosan-chondroitin sulphate nanoparticles for controlled delivery of platelet lysates in bone regenerative medicine. J. Tissue Eng. Regen. Med. 2012, 6, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Babo, P.S.; Cai, X.; Plachokova, A.S.; Reis, R.L.; Jansen, J.A.; Gomes, M.E.; Walboomers, X.F. The role of a platelet lysate-based compartmentalized system as a carrier of cells and platelet-origin cytokines for tissue regeneration. Tissue Eng. Part A 2016, 22, 1164–1175. [Google Scholar] [CrossRef] [PubMed]
- Calejo, I.; Costa-Almeida, R.; Reis, R.L.; Gomes, M.E. Enthesis tissue engineering: Biological requirements meet at the interface. Tissue Eng. Part B Rev. 2019, 25, 330–356. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Lamberti, A.; Maffulli, N.; Denaro, V. Tissue engineered biological augmentation for tendon healing: A systematic review. Br. Med. Bull. 2010, 98, 31–59. [Google Scholar] [CrossRef] [PubMed]
- Gulotta, L.V.; Kovacevic, D.; Ehteshami, J.R.; Dagher, E.; Packer, J.D.; Rodeo, S.A. Application of bone marrow-derived mesenchymal stem cells in a rotator cuff repair model. Am. J. Sports Med. 2009, 37, 2126–2133. [Google Scholar] [CrossRef] [PubMed]
- Gulotta, L.V.; Rodeo, S.A. Growth factors for rotator cuff repair. Clin. Sports Med. 2009, 28, 13–23. [Google Scholar] [CrossRef]
- Ali, I.H.; Brazil, D.P. Bone morphogenetic proteins and their antagonists: Current and emerging clinical uses. Br. J. Pharm. 2014, 171, 3620. [Google Scholar] [CrossRef]
- Sharma, P.; Maffulli, N. Tendinopathy and tendon injury: The future. Disabil. Rehabil. 2008, 30, 1733–1745. [Google Scholar] [CrossRef]
- Sharma, P.; Maffulli, N. Biology of tendon injury: Healing, modeling and remodelling. J. Musculoskelet. Neuronal Interact. 2006, 6, 181–190. [Google Scholar]
- Babo, P.S.; Reis, R.L.; Gomes, M.E. Periodontal tissue engineering: Current strategies and the role of platelet rich hemoderivatives. J. Mater. Chem. B 2017, 5, 3617–3628. [Google Scholar] [CrossRef]
- Mori, M.; Rossi, S.; Ferrari, F.; Bonferoni, M.C.; Sandri, G.; Riva, F.; Tenci, M.; Del Fante, C.; Nicoletti, G.; Caramella, C. Sponge-Like Dressings Based on the Association of Chitosan and Sericin for the Treatment of Chronic Skin Ulcers. II. Loading of the Hemoderivative Platelet Lysate. J. Pharm. Sci. 2016, 105, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, S.P.B.; Domingues, R.M.A.; Shevchuk, M.; Gomes, M.E.; Peppas, N.A.; Reis, R.L. Biomaterials for Sequestration of Growth Factors and Modulation of Cell Behavior. Adv. Funct. Mater. 2020, 30. [Google Scholar] [CrossRef]
- Andia, I.; Maffulli, N. Platelet-rich plasma for managing pain and inflammation in osteoarthritis. Nat. Rev. Rheumatol. 2013, 9, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Burnouf, T.; Chou, M.-L.; Wu, Y.-W.; Su, C.-Y.; Lee, L.-W. Antimicrobial activity of platelet (PLT)-poor plasma, PLT-rich plasma, PLT gel, and solvent/detergent-treated PLT lysate biomaterials against wound bacteria. Transfusion 2013, 53, 138–146. [Google Scholar] [CrossRef]
- Yeaman, M.R.; Bayer, A.S. Antimicrobial peptides from platelets. Drug Resist. Updat. 1999, 2, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Copland, I.B.; Garcia, M.A.; Waller, E.K.; Roback, J.D.; Galipeau, J. The effect of platelet lysate fibrinogen on the functionality of MSCs in immunotherapy. Biomaterials 2013, 34, 7840–7850. [Google Scholar] [CrossRef]
- Mishra, A.; Woodall, J.; Vieira, A. Treatment of tendon and muscle using platelet-rich plasma. Clin. Sports Med. 2009, 28, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.E. Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant. Dent. 2001, 10, 225–228. [Google Scholar] [CrossRef]
- Amable, P.R.; Carias, R.B.; Teixeira, M.V.; da Cruz Pacheco, I.; Correa do Amaral, R.J.; Granjeiro, J.M.; Borojevic, R. Platelet-rich plasma preparation for regenerative medicine: Optimization and quantification of cytokines and growth factors. Stem Cell Res. Ther. 2013, 4, 67. [Google Scholar] [CrossRef]
- Seidel, S.R.T.; Vendruscolo, C.P.; Moreira, J.J.; Fülber, J.; Ottaiano, T.F.; Oliva, M.L.V.; Michelacci, Y.M.; Baccarin, R.Y.A. Does Double Centrifugation Lead to Premature Platelet Aggregation and Decreased TGF-β1 Concentrations in Equine Platelet-Rich Plasma? Vet. Sci. 2019, 6, 68. [Google Scholar] [CrossRef]
- Mendes, B.B.; Gómez-Florit, M.; Babo, P.S.; Domingues, R.M.; Reis, R.L.; Gomes, M.E. Blood derivatives awaken in regenerative medicine strategies to modulate wound healing. Avd. Drug Deliv. Rev. 2018, 129, 376–393. [Google Scholar] [CrossRef] [PubMed]
- Perazzi, A.; Busetto, R.; Martinello, T.; Drigo, M.; Pasotto, D.; Cian, F.; Patruno, M.; Iacopetti, I. Description of a double centrifugation tube method for concentrating canine platelets. BMC Vet. Res. 2013, 9, 146. [Google Scholar] [CrossRef] [PubMed]
- Dohan Ehrenfest, D.M.; Rasmusson, L.; Albrektsson, T. Classification of platelet concentrates: From pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol. 2009, 27, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Dohan Ehrenfest, D.M.; Andia, I.; Zumstein, M.A.; Zhang, C.Q.; Pinto, N.R.; Bielecki, T. Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin- PRF) for topical and infiltrative use in orthopedic and sports medicine: Current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014, 4, 3–9. [Google Scholar] [CrossRef]
- Martineau, I.; Lacoste, E.; Gagnon, G. Effects of calcium and thrombin on growth factor release from platelet concentrates: Kinetics and regulation of endothelial cell proliferation. Biomaterials 2004, 25, 4489–4502. [Google Scholar] [CrossRef]
- Wang, H.-L.; Avila, G. Platelet rich plasma: Myth or reality? Eur. J. Dent. 2007, 1, 192–194. [Google Scholar] [CrossRef]
- Fortunato, T.M.; Beltrami, C.; Emanueli, C.; De Bank, P.A.; Pula, G. Platelet lysate gel and endothelial progenitors stimulate microvascular network formation in vitro: Tissue engineering implications. Sci. Rep. 2016, 6, 25326. [Google Scholar] [CrossRef]
- Crespo-Diaz, R.; Behfar, A.; Butler, G.W.; Padley, D.J.; Sarr, M.G.; Bartunek, J.; Dietz, A.B.; Terzic, A. Platelet lysate consisting of a natural repair proteome supports human mesenchymal stem cell proliferation and chromosomal stability. Cell Transplant. 2011, 20, 797–811. [Google Scholar] [CrossRef]
- Fekete, N.; Gadelorge, M.; Furst, D.; Maurer, C.; Dausend, J.; Fleury-Cappellesso, S.; Mailander, V.; Lotfi, R.; Ignatius, A.; Sensebe, L.; et al. Platelet lysate from whole blood-derived pooled platelet concentrates and apheresis-derived platelet concentrates for the isolation and expansion of human bone marrow mesenchymal stromal cells: Production process, content and identification of active components. Cytotherapy 2010, 14, 540–554. [Google Scholar] [CrossRef]
- Brown, A.C.; Barker, T.H. Fibrin-based biomaterials: Modulation of macroscopic properties through rational design at the molecular level. Acta Biomater. 2014, 10, 1502–1514. [Google Scholar] [CrossRef]
- Capila, I.; Linhardt, R.J. Heparin–protein interactions. Angew. Chem. Int. Ed. Eng. 2002, 41, 390–412. [Google Scholar] [CrossRef]
- Macri, L.; Silverstein, D.; Clark, R.A.F. Growth factor binding to the pericellular matrix and its importance in tissue engineering. Adv. Drug Deliv. Rev. 2007, 59, 1366–1381. [Google Scholar] [CrossRef] [PubMed]
- Caliari, S.R.; Weisgerber, D.W.; Grier, W.K.; Mahmassani, Z.; Boppart, M.D.; Harley, B.A.C. Collagen scaffolds incorporating coincident gradations of instructive structural and biochemical cues for osteotendinous junction engineering. Adv. Healthc. Mater. 2015, 4, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Sun, Y.; Xu, P.; Cheng, B. Can patients get better clinical outcomes by using PRP in rotator cuff repair: A metaanalysis of randomized controlled trials. J. Sports Med. Phys. Fit. 2016, 56, 1359–1367. [Google Scholar]
- Mi, B.; Liu, G.; Zhou, W.; Lv, H.; Liu, Y.; Wu, Q.; Liu, J. Platelet rich plasma versus steroid on lateral epicondylitis: Meta-analysis of randomized clinical trials. Phys. Sports Med. 2017, 45, 97–104. [Google Scholar] [CrossRef]
- Costa-Almeida, R.; Babo, P.S.; Reis, R.L.; Gomes, M.E. Platelet-rich Blood Derivatives for Tendon Regeneration. J. Am. Acad Orthop. Surg. 2020, 28, e202–e205. [Google Scholar] [CrossRef]
- Hurley, E.T.; Fat, D.L.; Moran, C.J.; Mullett, H. The Efficacy of Platelet-Rich Plasma and Platelet-Rich Fibrin in Arthroscopic Rotator Cuff Repair: A Meta-analysis of Randomized Controlled Trials. Am. J. Sports Med. 2019, 47, 753–761. [Google Scholar] [CrossRef]
- Yang, F.-A.; Liao, C.-D.; Wu, C.-W.; Shih, Y.-C.; Wu, L.-C.; Chen, H.-C. Effects of applying platelet-rich plasma during arthroscopic rotator cuff repair: A systematic review and meta-analysis of randomised controlled trials. Sci. Rep. 2020, 10, 17171. [Google Scholar] [CrossRef]
- Lee, K.; Silva, E.A.; Mooney, D.J. Growth factor delivery-based tissue engineering: General approaches and a review of recent developments. J. R Soc. Interface 2010, 8, 153–170. [Google Scholar] [CrossRef]
- Mitchell, A.C.; Briquez, P.S.; Hubbell, J.A.; Cochran, J.R. Engineering growth factors for regenerative medicine applications. Acta Biomater. 2016, 30, 1–12. [Google Scholar] [CrossRef]
- Bu, M.; Tang, J.; Wei, Y.; Sun, Y.; Wang, X.; Wu, L.; Liu, H. Enhanced bioavailability of nerve growth factor with phytantriol lipid-based crystalline nanoparticles in cochlea. Int. J. Nanomed. 2015, 10, 6879–6889. [Google Scholar] [CrossRef]
- Liu, S.; Qin, M.; Hu, C.; Wu, F.; Cui, W.; Jin, T.; Fan, C. Tendon healing and anti-adhesion properties of electrospun fibrous membranes containing bFGF loaded nanoparticles. Biomaterials 2013, 34, 4690–4701. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.M.; Willers, C.; Xu, J.; Wang, A.; Zheng, M.H. Autologous tenocyte therapy using porcine derived bioscaffolds for massive rotator cuff defect in rabbits. Tissue Eng. 2007, 13, 1479–1491. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.P.; Lee, C.-H.; Jung, J.W.; Lee, H.-J.; Lee, Y.-S.; Kim, J.-Y.; Park, G.Y.; Choi, J.H.; Chung, S.W. Sustained delivery of transforming growth factor b1 by use of absorbable alginate scaffold enhances rotator cuff healing in a rabbit model. Am. J. Sports Med. 2018, 46, 1441–1450. [Google Scholar] [CrossRef]
- Manning, C.N.; Kim, H.M.; Sakiyama-Elbert, S.; Galatz, L.M.; Havlioglu, N.; Thomopoulos, S. Sustained delivery of transforming growth factor beta three enhances tendon-to-bone healing in a rat model. J. Orthop. Res. 2011, 29, 1099–1105. [Google Scholar] [CrossRef]
- Zhao, S.; Zhao, J.; Dong, S.; Huangfu, X.; Li, B.; Yang, H.; Zhao, J.; Cui, W. Biological augmentation of rotator cuff repair using bFGF-loaded electrospun poly(lactide-co-glycolide) fibrous membranes. Int. J. Nanomed. 2014, 9, 2373–2385. [Google Scholar] [CrossRef]
- Ide, J.; Kikukawa, K.; Hirose, J.; Iyama, K.; Sakamoto, H.; Fujimoto, T.; Mizuta, H. The effect of a local application of fibroblast growth factor-2 on tendon-to-bone remodeling in rats with acute injury and repair of the supraspinatus tendon. J. Shoulder Elb. Surg. 2009, 18, 391–398. [Google Scholar] [CrossRef]
- Rickert, M.; Jung, M.; Adiyaman, M.; Richter, W.; Simank, H.G. A Growth and Differentiation Factor-5 (GDF-5)-coated Suture Stimulates Tendon Healing in an Achilles Tendon Model in Rats. Growth Factors 2001, 19, 115–126. [Google Scholar] [CrossRef]
- Kabuto, Y.; Morihara, T.; Sukenari, T.; Kida, Y.; Oda, R.; Arai, Y.; Sawada, K.; Matsuda, K.-I.; Kawata, M.; Tabata, Y.; et al. Stimulation of Rotator Cuff Repair by Sustained Release of Bone Morphogenetic Protein-7 Using a Gelatin Hydrogel Sheet. Tissue Eng. Part A 2015, 21, 2025–2033. [Google Scholar] [CrossRef]
- Lee, K.-W.; Lee, J.-S.; Kim, Y.-S.; Shim, Y.-B.; Jang, J.-W.; Lee, K.-I. Effective healing of chronic rotator cuff injury using recombinant bone morphogenetic protein-2 coated dermal patch in vivo. J. Biomed. Mater. Res. B 2016, 105, 1840–1846. [Google Scholar] [CrossRef]
- Zhang, J.; Yuan, T.; Zheng, N.; Zhou, Y.; Hogan, M.V.; Wang, J.H.-C. The combined use of kartogenin and platelet-rich plasma promotes fibrocartilage formation in the wounded rat Achilles tendon entheses. Bone Jt. Res. 2017, 6, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.; Zhou, C.; Xu, D.; Bi, F. Combination of platelet-rich plasma and bone marrow mesenchymal stem cells enhances tendon–bone healing in a rabbit model of anterior cruciate ligament reconstruction. J. Orthop. Surg. Res. 2016, 11, 96. [Google Scholar] [CrossRef] [PubMed]
- Okuda, K.; Kawase, T.; Momose, M.; Murata, M.; Saito, Y.; Suzuki, H.; Wolff, L.F.; Yoshie, H. Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factor-beta and modulates the proliferation of periodontally related cells in vitro. J. Periodontol. 2003, 74, 849–857. [Google Scholar] [CrossRef]
- Ranzato, E.; Patrone, M.; Mazzucco, L.; Burlando, B. Platelet lysate stimulates wound repair of HaCaT keratinocytes. Br. J. Derm. 2008, 159, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Backly, R.E.; Ulivi, V.; Tonachini, L.; Cancedda, R.; Descalzi, F.; Mastrogiacomo, M. Platelet lysate induces in vitro wound healing of human keratinocytes associated with a strong proinflammatory response. Tissue Eng. Part A 2011, 17, 1787–1800. [Google Scholar] [CrossRef]
- Witting, M.; Obst, K.; Friess, W.; Hedtrich, S. Recent advances in topical delivery of proteins and peptides mediated by soft matter nanocarriers. Biotechnol. Adv. 2015, 33, 1355–1369. [Google Scholar] [CrossRef]
- Mottaghitalab, F.; Farokhi, M.; Shokrgozar, M.A.; Atyabi, F.; Hosseinkhani, H. Silk fibroin nanoparticle as a novel drug delivery system. J. Control. Release 2015, 206, 161–176. [Google Scholar] [CrossRef]
- Smith, B.D.; Grande, D.A. The current state of scaffolds for musculoskeletal regenerative applications. Nat. Rev. Rheumatol. 2015, 11, 213–222. [Google Scholar] [CrossRef]



| Hemoderivatives | Carrier System | Anatomical Site | Model | Main Outcomes |
|---|---|---|---|---|
| TGF-β1 | Alginate scaffold | Bilateral supraspinatus tendon | Rabbit [157] | More evident formation of fibrocartilage; Better collagen orientation, organization, and continuity; Increase of the ultimate failure load compared to the non-treated groups. |
| TGF-β3 | Heparin/fibrin-based system | Supraspinatus tendon | Rat [158] | Initial increase of proliferation, cellularity, inflammation and vascularity; Subsequent improvement of ultimate force, modulus, failure to stress and toughness. |
| bFGF | PLGA fibrous membranes | Rotator cuff | Rat [159] | Membrane absorption in 2 weeks; Increase of collagen organization and formation of a more mature tissue in compare to groups treated with PLGA membrane alone; Increase in cross-sectional area and consequent reduction of the ultimate stress; Increase of the ultimate load to failure. |
| FGF-2 | Fibrin sealant | Supraspinatus tendon | Rat [160] | Increase in cellularity and vascularity at the tendon-to-bone interface; Increase of the parallel-oriented fibers, bone ingrowth and strength compared to the non-treated group in 2 weeks; Treated and non-treated groups manifested similar strength related to the tendon-to-bone interface maturity in 4 weeks. |
| GDF-5 | Suture | Achilles tendon | Rat [161] | Increase of the tensile strength and maximum failure load in 2 weeks; Increase of the thickness and cell density; Appearance of cartilage-like cells in 4 weeks. |
| BMP-7 | Gelatin hydrogel sheet | Rotator cuff | Rat [162] | At the tendon-to-bone interface, increase of the number of chondrocytes, higher maturity and ultimate load to failure; Higher orientation of the collagen fibers; Higher deposition of collagen matrix compared to the groups treated with BMP-7 alone. |
| rh-BMP-2 | Dermal patch | Rotator cuff | Rabbit [163] | Increase of the ultimate tensile strength and of new bone formation compared to the groups treated with suture and dermal patch alone; Higher cellularity at the tendon-to-bone interface and presence of new fibrochondrocytes. |
| PRP | Local injection | Achilles tendon | Rat [164] | Formation of a collagen fibers transition zone and increase of the mechanical strength; Proteoglycan expression; Complete healing compared to the non-treated groups. |
| PRP | Hamstring tendon grafts | Anterior cruciate ligament | Rabbit [165] | Formation of mineralized tissue, new bone and cartilage at the tendon-to-bone interface; Formation of aligned connective tissue. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianchi, E.; Ruggeri, M.; Rossi, S.; Vigani, B.; Miele, D.; Bonferoni, M.C.; Sandri, G.; Ferrari, F. Innovative Strategies in Tendon Tissue Engineering. Pharmaceutics 2021, 13, 89. https://doi.org/10.3390/pharmaceutics13010089
Bianchi E, Ruggeri M, Rossi S, Vigani B, Miele D, Bonferoni MC, Sandri G, Ferrari F. Innovative Strategies in Tendon Tissue Engineering. Pharmaceutics. 2021; 13(1):89. https://doi.org/10.3390/pharmaceutics13010089
Chicago/Turabian StyleBianchi, Eleonora, Marco Ruggeri, Silvia Rossi, Barbara Vigani, Dalila Miele, Maria Cristina Bonferoni, Giuseppina Sandri, and Franca Ferrari. 2021. "Innovative Strategies in Tendon Tissue Engineering" Pharmaceutics 13, no. 1: 89. https://doi.org/10.3390/pharmaceutics13010089
APA StyleBianchi, E., Ruggeri, M., Rossi, S., Vigani, B., Miele, D., Bonferoni, M. C., Sandri, G., & Ferrari, F. (2021). Innovative Strategies in Tendon Tissue Engineering. Pharmaceutics, 13(1), 89. https://doi.org/10.3390/pharmaceutics13010089