A Limited Structural Modification Results in a Significantly More Efficacious Diazachrysene-Based Filovirus Inhibitor
Abstract
:1. Introduction
2. Results and Discussion
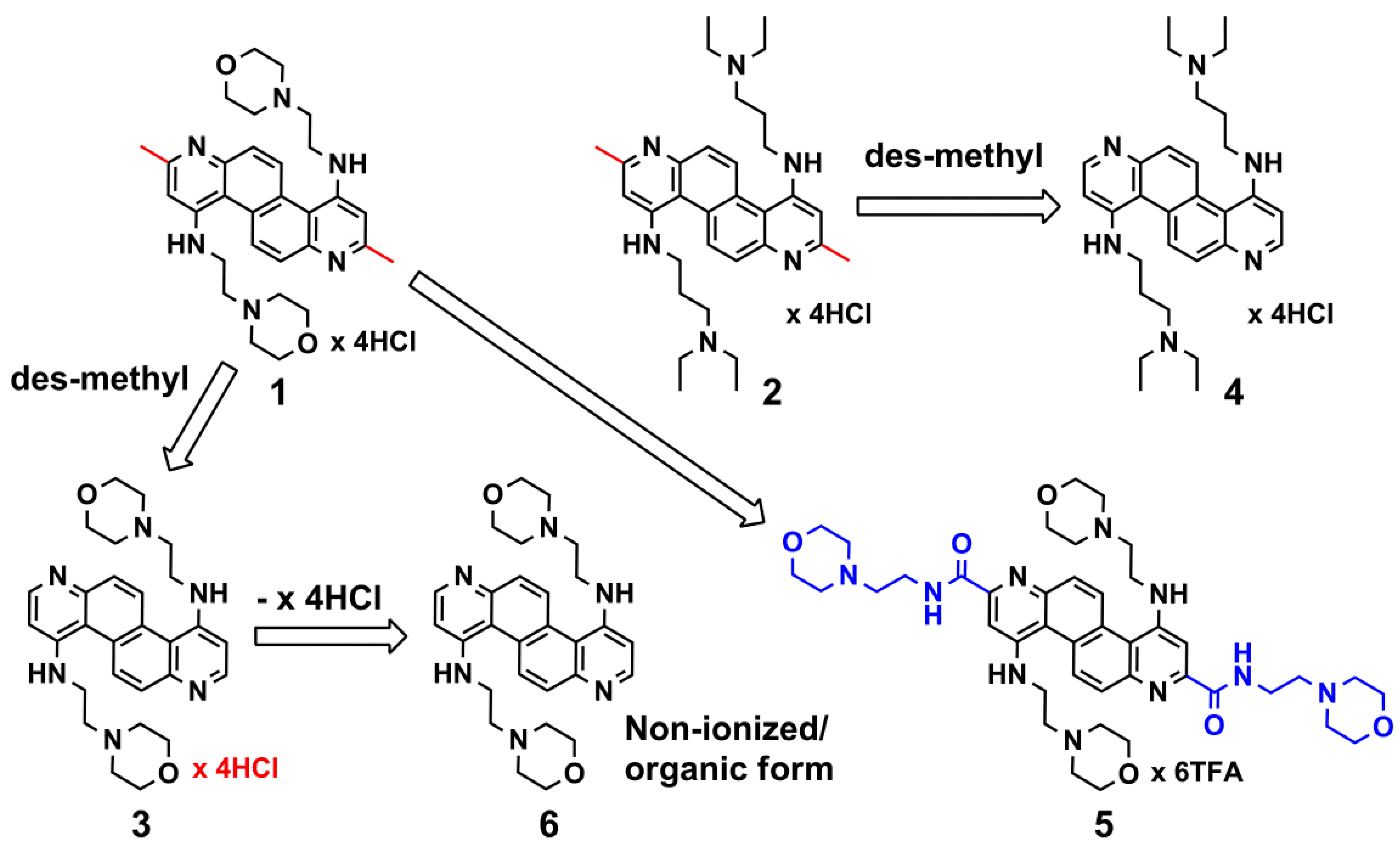
2.1. DAAC Analogs
2.2. Anti-Filovius Activity
2.2.1. Dose-Response Studies: Inhibitors 3 and 5
| Compound | IC50 against EBOV | IC50 against MARV |
|---|---|---|
| 3 | 0.696 µM ± 0.13 µM | 2.76 µM ± 0.21 µM |
| 5 | 12.98 µM ± 0.17 µM | ND * |
| 6 | 1.13 µM ± 0.28 µM | 10.51 µM ± 0.31 µM |
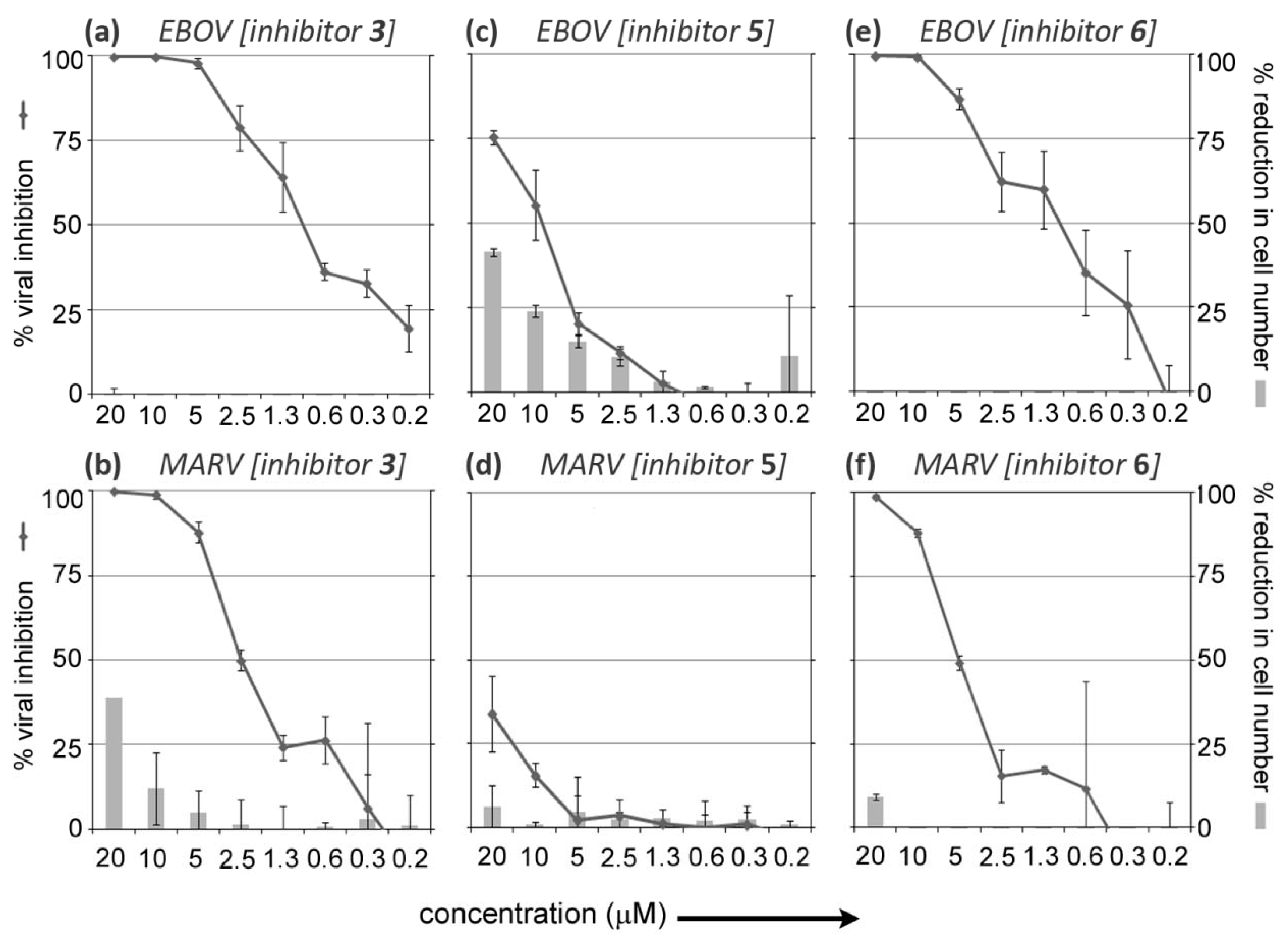
2.2.2. Comparison of the Inhibitory Efficacies and Toxicities of Salt (Cationic/Ionized) form 3 and Basic (Unionized/Non-Salt) form 6
2.3. The Future Development of DAAC-Based Anti-Filovirus Agents
3. Experimental Section
3.1. Synthesis
3.2. Assays to Detect Anti-Filovirus Cellular Efficacy
4. Conclusions
Supplementary Files
Conflict of Interest
Acknowledgments
References
- Bausch, D.G.; Towner, J.S.; Dowell, S.F.; Kaducu, F.; Lukwiya, M.; Sanchez, A.; Nichol, S.T.; Ksiazek, T.G.; Rollin, P.E. Assessment of the risk of ebola virus transmission from bodily fluids and fomites. J. Infect. Dis. 2007, 196, S142–S147. [Google Scholar] [CrossRef]
- Available online: http://www.Bt.Cdc.Gov/agent/agentlist-category.Asp (accessed on 24 June 2012).
- Kuhn, J.H. Filoviruses. A compendium of 40 years of epidemiological, clinical, and laboratory studies. Arch. Virol. Suppl. 2008, 20, 13–360. [Google Scholar] [CrossRef]
- Bradfute, S.B.; Dye, J.M., Jr.; Bavari, S. Filovirus vaccines. Hum. Vaccin 2011, 7, 701–711. [Google Scholar] [CrossRef]
- Sullivan, N.J.; Geisbert, T.W.; Geisbert, J.B.; Shedlock, D.J.; Xu, L.; Lamoreaux, L.; Custers, J.H.; Popernack, P.M.; Yang, Z.Y.; Pau, M.G.; et al. Immune protection of nonhuman primates against ebola virus with single low-dose adenovirus vectors encoding modified gps. PLoS Med. 2006, 3, e177. [Google Scholar]
- Sullivan, N.J.; Sanchez, A.; Rollin, P.E.; Yang, Z.Y.; Nabel, G.J. Development of a preventive vaccine for ebola virus infection in primates. Nature 2000, 408, 605–609. [Google Scholar]
- Warren, T.K.; Warfield, K.L.; Wells, J.; Swenson, D.L.; Donner, K.S.; van Tongeren, S.A.; Garza, N.L.; Dong, L.; Mourich, D.V.; Crumley, S.; et al. Advanced antisense therapies for postexposure protection against lethal filovirus infections. Nat. Med. 2010, 16, 991–994. [Google Scholar]
- Warfield, K.L.; Panchal, R.G.; Aman, M.J.; Bavari, S. Antisense treatments for biothreat agents. Curr. Opin. Mol. Ther. 2006, 8, 93–103. [Google Scholar]
- Warren, T.K.; Shurtleff, A.C.; Bavari, S. Advanced morpholino oligomers: A novel approach to antiviral therapy. Antivir. Res. 2012, 94, 80–88. [Google Scholar]
- Swenson, D.L.; Warfield, K.L.; Warren, T.K.; Lovejoy, C.; Hassinger, J.N.; Ruthel, G.; Blouch, R.E.; Moulton, H.M.; Weller, D.D.; Iversen, P.L.; et al. Chemical modifications of antisense morpholino oligomers enhance their efficacy against ebola virus infection. Antimicrob. Agents Chemother. 2009, 53, 2089–2099. [Google Scholar]
- Panchal, R.G.; Reid, S.P.; Tran, J.P.; Bergeron, A.A.; Wells, J.; Kota, K.P.; Aman, J.; Bavari, S. Identification of an antioxidant small-molecule with broad-spectrum antiviral activity. Antivir. Res. 2012, 93, 23–29. [Google Scholar]
- Reid, S.P.; Shurtleff, A.C.; Bavari, S. Emerging therapeutic options against filoviruses. Drugs Future 2012, 37, 343–352. [Google Scholar]
- Aman, M.J.; Kinch, M.S.; Warfield, K.; Warren, T.; Yunus, A.; Enterlein, S.; Stavale, E.; Wang, P.; Chang, S.; Tang, Q.; et al. Development of a broad-spectrum antiviral with activity against ebola virus. Antivir. Res. 2009, 83, 245–251. [Google Scholar]
- Opsenica, I.; Burnett, J.C.; Gussio, R.; Opsenica, D.; Todorovic, N.; Lanteri, C.A.; Sciotti, R.J.; Gettayacamin, M.; Basilico, N.; Taramelli, D.; et al. A chemotype that inhibits three unrelated pathogenic targets: The botulinum neurotoxin serotype a light chain, p. Falciparum malaria, and the ebola filovirus. J. Med. Chem. 2011, 54, 1157–1169. [Google Scholar]
- Panchal, R.G.; Kota, K.P.; Spurgers, K.B.; Ruthel, G.; Tran, J.P.; Boltz, R.C.; Bavari, S. Development of high-content imaging assays for lethal viral pathogens. J. Biomol. Screen 2010, 15, 755–765. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Selaković, Ž.; Opsenica, D.; Eaton, B.; Retterer, C.; Bavari, S.; Burnett, J.C.; Šolaja, B.A.; Panchal, R.G. A Limited Structural Modification Results in a Significantly More Efficacious Diazachrysene-Based Filovirus Inhibitor. Viruses 2012, 4, 1279-1288. https://doi.org/10.3390/v4081279
Selaković Ž, Opsenica D, Eaton B, Retterer C, Bavari S, Burnett JC, Šolaja BA, Panchal RG. A Limited Structural Modification Results in a Significantly More Efficacious Diazachrysene-Based Filovirus Inhibitor. Viruses. 2012; 4(8):1279-1288. https://doi.org/10.3390/v4081279
Chicago/Turabian StyleSelaković, Života, Dejan Opsenica, Brett Eaton, Cary Retterer, Sina Bavari, James C. Burnett, Bogdan A. Šolaja, and Rekha G. Panchal. 2012. "A Limited Structural Modification Results in a Significantly More Efficacious Diazachrysene-Based Filovirus Inhibitor" Viruses 4, no. 8: 1279-1288. https://doi.org/10.3390/v4081279
APA StyleSelaković, Ž., Opsenica, D., Eaton, B., Retterer, C., Bavari, S., Burnett, J. C., Šolaja, B. A., & Panchal, R. G. (2012). A Limited Structural Modification Results in a Significantly More Efficacious Diazachrysene-Based Filovirus Inhibitor. Viruses, 4(8), 1279-1288. https://doi.org/10.3390/v4081279





