Kinetics of Viral Genome Distribution in Swine Peripheral Lymphoid Organs Following Oronasal Infection with Attenuated African swine fever virus strains
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Virus Inoculations
2.3. Sample Collection
2.4. Real-Time PCR
2.5. Histopathology, Immunohistochemistry (IHC) and In Situ Hybridization (ISH)
2.6. Graphical Presentation of Data and Statistical Analysis
3. Results
3.1. Experiment 1 (ASFV Estonia 2014)
3.1.1. Clinical Findings of Experiment 1
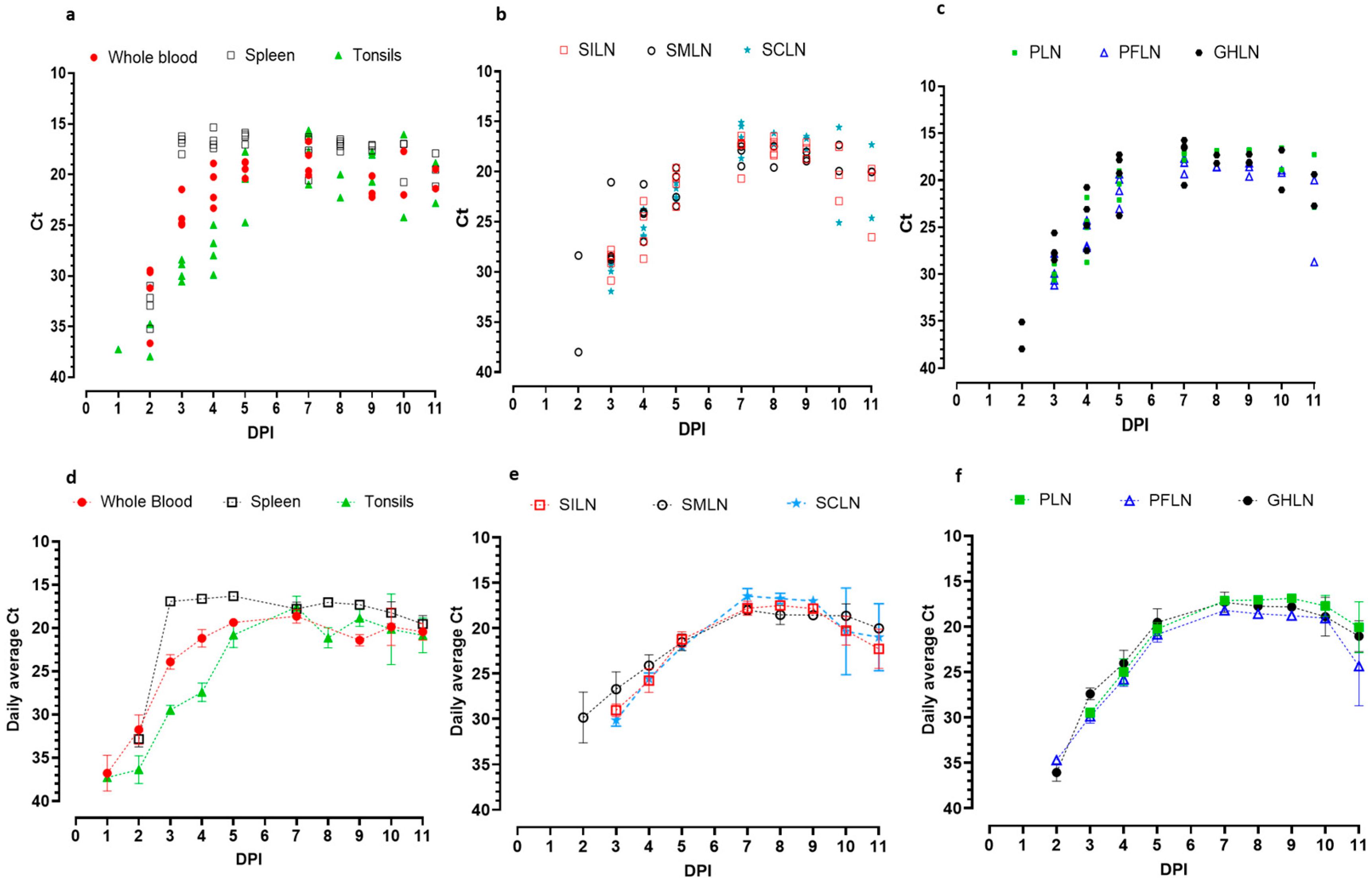
3.1.2. ASFV Genomic Detection Dynamics in Whole Blood, Central Lymphoid Organs, and Peripheral Lymph Nodes
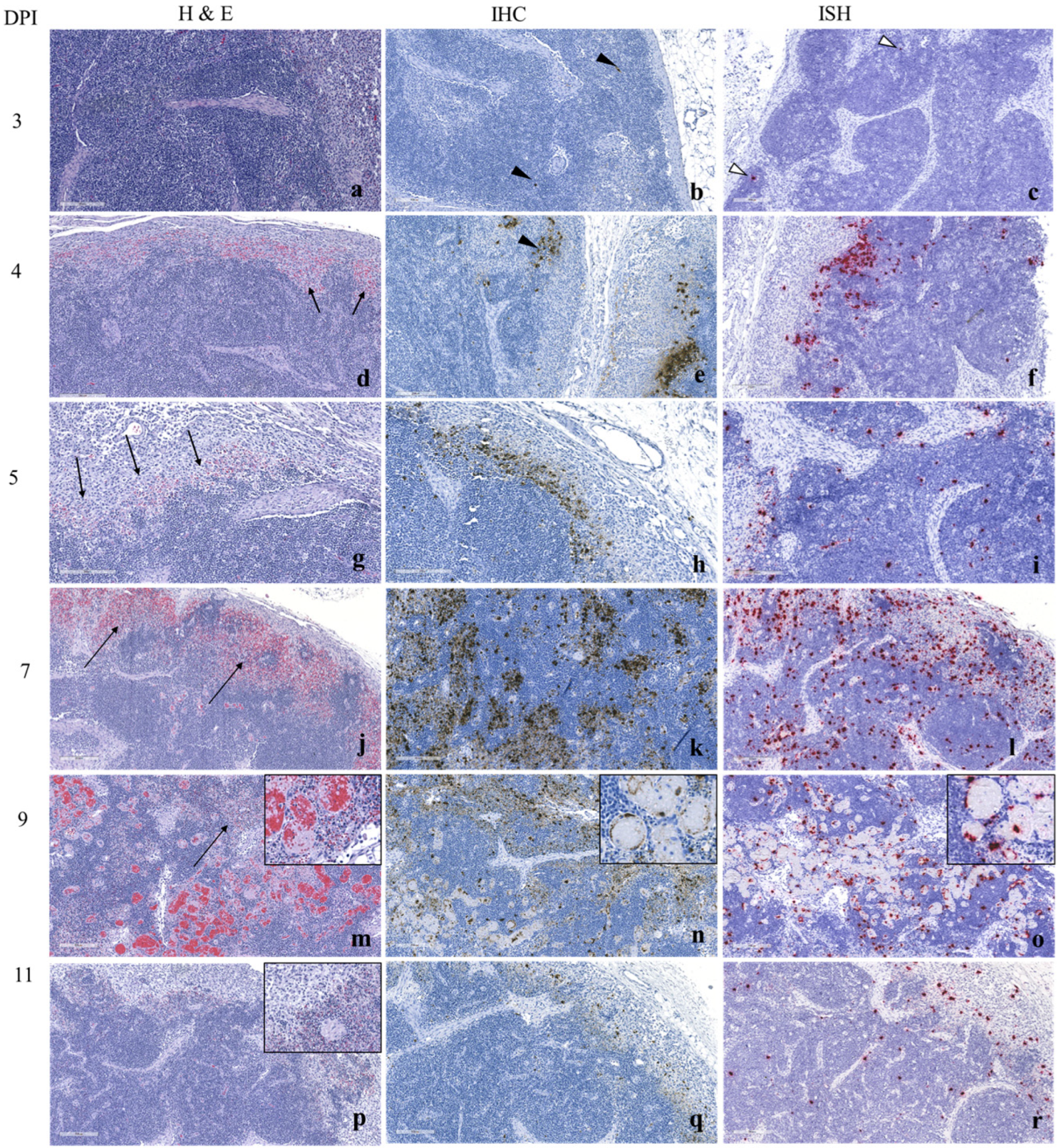
3.1.3. Histopathology and ASFV Detection by Immunohistochemistry (IHC) and In Situ Hybridization (ISH)
3.2. Experiment 2 (ASFV Malta’78)
3.2.1. Clinical Findings of Experiment 2
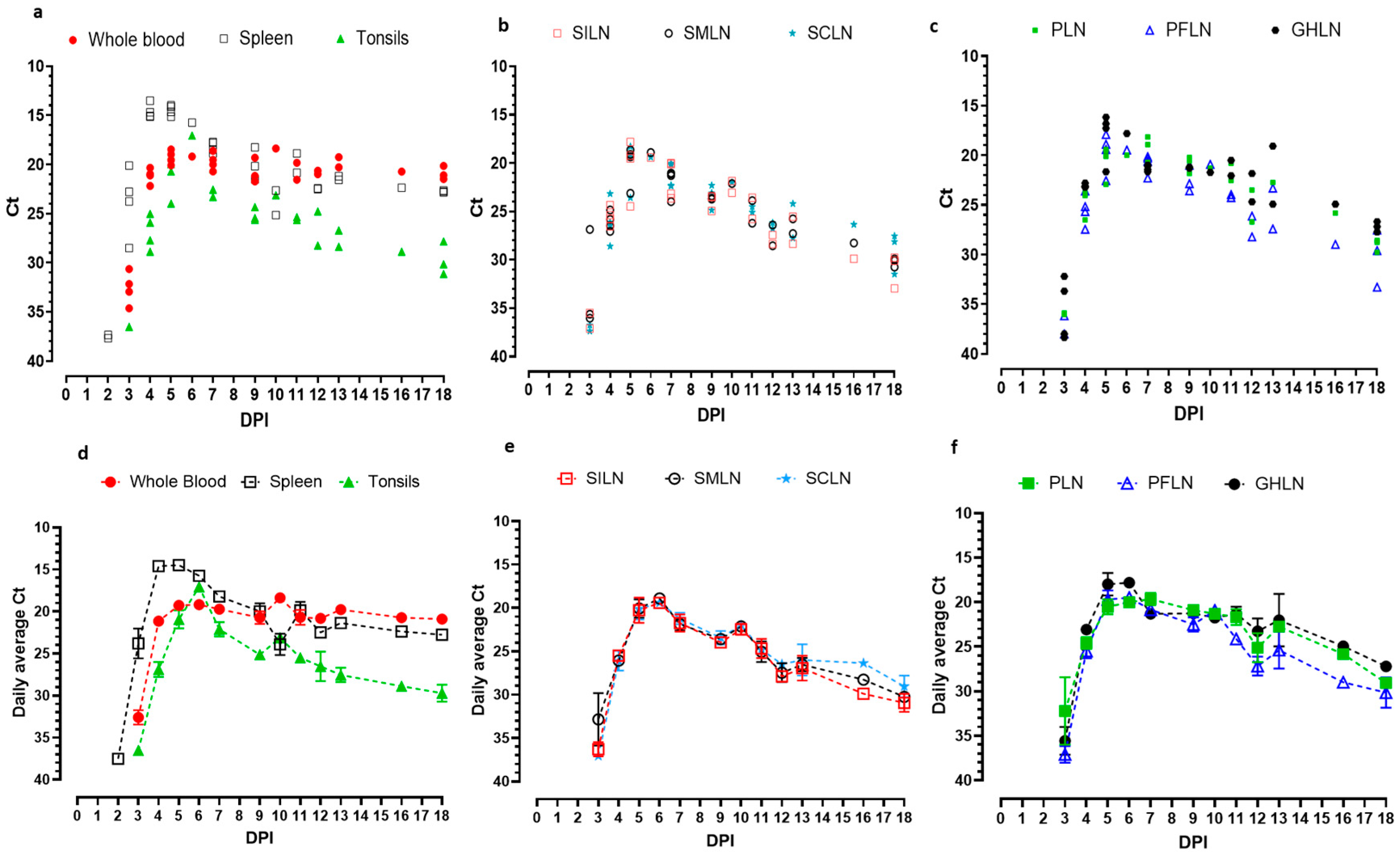
3.2.2. ASFV Genome Detection Dynamics in Whole Blood, Central Lymphoid Organs, and Peripheral Lymph Nodes
3.2.3. Histopathology and ASFV Detection by Immunohistochemistry (IHC) and In Situ Hybridization (ISH)
3.3. End-Point Detection of ASFV Genome in Spleen and SILN of Dead and Euthanized Pigs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WOAH WAHIS. Georgia African Swine Fever Follow-Up Report 1. Available online: https://wahis.woah.org/#/in-review/304 (accessed on 1 January 2025).
- Rowlands, R.J.; Michaud, V.; Heath, L.; Hutchings, G.; Oura, C.; Vosloo, W.; Dwarka, R.; Onashvili, T.; Albina, E.; Dixon, L.K. African swine fever virus isolate, Georgia, 2007. Emerg. Infect. Dis. 2008, 14, 1870–1874. [Google Scholar] [CrossRef] [PubMed]
- Gogin, A.; Gerasimov, V.; Malogolovkin, A.; Kolbasov, D. African swine fever in the North Caucasus region and the Russian Federation in years 2007–2012. Virus Res. 2013, 173, 198–203. [Google Scholar] [CrossRef]
- de la Torre, A.; Bosch, J.; Sánchez-Vizcaíno, J.M.; Ito, S.; Muñoz, C.; Iglesias, I.; Martínez-Avilés, M. African Swine Fever Survey in a European Context. Pathogens 2022, 11, 137. [Google Scholar] [CrossRef]
- Gonzales, W.; Moreno, C.; Duran, U.; Henao, N.; Bencosme, M.; Lora, P.; Reyes, R.; Núñez, R.; De Gracia, A.; Perez, A.M. African swine fever in the Dominican Republic. Transbound. Emerg. Dis. 2021, 68, 3018–3019. [Google Scholar] [CrossRef]
- Blome, S.; Gabriel, C.; Beer, M. Pathogenesis of African swine fever in domestic pigs and European wild boar. Virus Res. 2013, 173, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Izzati, U.Z.; Inanaga, M.; Hoa, N.T.; Nueangphuet, P.; Myint, O.; Truong, Q.L.; Lan, N.T.; Norimine, J.; Hirai, T.; Yamaguchi, R. Pathological investigation and viral antigen distribution of emerging African swine fever in Vietnam. Transbound. Emerg. Dis. 2021, 68, 2039–2050. [Google Scholar] [CrossRef]
- Nga, B.T.T.; Tran Anh Dao, B.; Nguyen Thi, L.; Osaki, M.; Kawashima, K.; Song, D.; Salguero, F.J.; Le, V.P. Clinical and Pathological Study of the First Outbreak Cases of African Swine Fever in Vietnam 2019. Front. Vet. Sci. 2020, 7, 392. [Google Scholar] [CrossRef]
- Salguero, F.J. Comparative Pathology and Pathogenesis of African Swine Fever Infection in Swine. Front. Vet. Sci. 2020, 7, 282. [Google Scholar] [CrossRef]
- Avagyan, H.; Hakobyan, S.; Baghdasaryan, B.; Arzumanyan, H.; Poghosyan, A.; Bayramyan, N.; Semerjyan, A.; Sargsyan, M.; Voskanyan, H.; Vardanyan, T.; et al. Pathology and Clinics of Naturally Occurring Low-Virulence Variants of African Swine Fever Emerged in Domestic Pigs in the South Caucasus. Pathogens 2024, 13, 130. [Google Scholar] [CrossRef]
- Sun, E.; Huang, L.; Zhang, X.; Zhang, J.; Shen, D.; Zhang, Z.; Wang, Z.; Huo, H.; Wang, W.; Huangfu, H.; et al. Genotype I African swine fever viruses emerged in domestic pigs in China and caused chronic infection. Emerg. Microbes Infect. 2021, 10, 2183–2193. [Google Scholar] [CrossRef] [PubMed]
- Depner, K.; Gortazar, C.; Guberti, V.; Masiulis, M.; More, S.; Oļševskis, E.; Thulke, H.-H.; Viltrop, A.; Woźniakowski, G.; Cortiñas Abrahantes, J.; et al. Epidemiological analyses of African swine fever in the Baltic States and Poland. EFSA J. 2017, 15, e05068. [Google Scholar] [CrossRef] [PubMed]
- Gervasi, V.; Marcon, A.; Bellini, S.; Guberti, V. Evaluation of the Efficiency of Active and Passive Surveillance in the Detection of African Swine Fever in Wild Boar. Vet. Sci. 2019, 7, 5. [Google Scholar] [CrossRef] [PubMed]
- Petrov, A.; Schotte, U.; Pietschmann, J.; Dräger, C.; Beer, M.; Anheyer-Behmenburg, H.; Goller, K.V.; Blome, S. Alternative sampling strategies for passive classical and African swine fever surveillance in wild boar. Vet. Microbiol. 2014, 173, 360–365. [Google Scholar] [CrossRef]
- Lamberga, K.; Oļševskis, E.; Seržants, M.; Bērziņš, A.; Viltrop, A.; Depner, K. African Swine Fever in Two Large Commercial Pig Farms in LATVIA-Estimation of the High Risk Period and Virus Spread within the Farm. Vet. Sci. 2020, 7, 105. [Google Scholar] [CrossRef] [PubMed]
- WOAH. African swine fever (infection with African swine fever virus). In Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (Mammals, Birds and Bees); WOAH: Paris, France, 2025. [Google Scholar]
- Penrith, M.L.; van Emmenes, J.; Hakizimana, J.N.; Heath, L.; Kabuuka, T.; Misinzo, G.; Odoom, T.; Wade, A.; Zerbo, H.L.; Luka, P.D. African Swine Fever Diagnosis in Africa: Challenges and Opportunities. Pathogens 2024, 13, 296. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Hu, Z.; Tian, X.; Fan, M.; Liu, Q.; Wang, X. A suitable sampling strategy for the detection of African swine fever virus in living and deceased pigs in the field: A retrospective study. Front. Vet. Sci. 2024, 11, 1419083. [Google Scholar] [CrossRef]
- Pikalo, J.; Deutschmann, P.; Fischer, M.; Roszyk, H.; Beer, M.; Blome, S. African Swine Fever Laboratory Diagnosis—Lessons Learned from Recent Animal Trials. Pathogens 2021, 10, 177. [Google Scholar] [CrossRef]
- Goonewardene, K.B.; Onyilagha, C.; Goolia, M.; Le, V.P.; Blome, S.; Ambagala, A. Superficial Inguinal Lymph Nodes for Screening Dead Pigs for African Swine Fever. Viruses 2022, 14, 83. [Google Scholar] [CrossRef]
- Zani, L.; Forth, J.H.; Forth, L.; Nurmoja, I.; Leidenberger, S.; Henke, J.; Carlson, J.; Breidenstein, C.; Viltrop, A.; Höper, D.; et al. Deletion at the 5′-end of Estonian ASFV strains associated with an attenuated phenotype. Sci. Rep. 2018, 8, 6510. [Google Scholar] [CrossRef]
- Wilkinson, P.J.; Lawman, M.J.; Johnston, R.S. African swine fever in Malta, 1978. Vet. Rec. 1980, 106, 94–97. [Google Scholar] [CrossRef]
- Goonewardene, K.B.; Chung, C.J.; Goolia, M.; Blakemore, L.; Fabian, A.; Mohamed, F.; Nfon, C.; Clavijo, A.; Dodd, K.A.; Ambagala, A. Evaluation of oral fluid as an aggregate sample for early detection of African swine fever virus using four independent pen-based experimental studies. Transbound. Emerg. Dis. 2021, 68, 2867–2877. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, L.; Noll, L.; Stoy, C.; Porter, E.; Fu, J.; Feng, Y.; Peddireddi, L.; Liu, X.; Dodd, K.A.; et al. Development of a real-time PCR assay for detection of African swine fever virus with an endogenous internal control. Transbound. Emerg. Dis. 2020, 67, 2446–2454. [Google Scholar] [CrossRef] [PubMed]
- Embury-Hyatt, C.; Moffat, E.; Zhmendak, D.; Erdelyan, C.N.G.; Collignon, B.; Goonewardene, K.; Ambagala, A.; Yang, M. Generation and characterization of a monoclonal antibody against an African swine fever virus protein encoded by the A137R gene. Front. Vet. Sci. 2023, 10, 1286906. [Google Scholar] [CrossRef] [PubMed]
- Sehl, J.; Pikalo, J.; Schäfer, A.; Franzke, K.; Pannhorst, K.; Elnagar, A.; Blohm, U.; Blome, S.; Breithaupt, A. Comparative Pathology of Domestic Pigs and Wild Boar Infected with the Moderately Virulent African Swine Fever Virus Strain “Estonia 2014”. Pathogens 2020, 9, 662. [Google Scholar] [CrossRef]
- Plowright, W.; Thomson, G.R.; Neser, J.A. African swine fever. In Infectious Diseases of Livestock with Special Reference to Southern Africa; Coetzer, J.A.W., Thomson, G.R., Tustin, R.C., Eds.; Oxford University Press Cape Town: Cape Town, South Africa, 1994; pp. 567–599. [Google Scholar]
- Sánchez-Vizcaíno, J.M.; Martínez-López, B.; Martínez-Avilés, M.; Martins, C.; Boinas, F.; Vial, L.; Michaud, V.; Jori, F.; Etter, E.; Albina, E.; et al. Scientific Report Submitted to EFSA on African Swine Fever; EFSA: Parma, Italy, 2009; pp. 1–141. [Google Scholar]
- Oh, T.; Do, D.T.; Lai, D.C.; Nguyen, L.T.; Lee, J.Y.; Van Le, P.; Chae, C. Chronological expression and distribution of African swine fever virus p30 and p72 proteins in experimentally infected pigs. Sci. Rep. 2022, 12, 4151. [Google Scholar] [CrossRef]
- Oh, S.-I.; Sheet, S.; Bui, V.N.; Dao, D.T.; Bui, N.A.; Kim, T.-H.; Cha, J.; Park, M.-R.; Hur, T.-Y.; Jung, Y.-H.; et al. Transcriptome profiles of organ tissues from pigs experimentally infected with African swine fever virus in early phase of infection. Emerg. Microbes Infect. 2024, 13, 2366406. [Google Scholar] [CrossRef]
- Vu, H.L.X.; McVey, D.S. Recent progress on gene-deleted live-attenuated African swine fever virus vaccines. Npj Vaccines 2024, 9, 60. [Google Scholar] [CrossRef]
- Suh, T.-Y.; Park, J.-H.; Hwang, S.Y.; Park, C.-R.; Kim, J.-E.; Park, J.Y.; Kim, Y.-J.; Kang, H.-E.; Kim, D.-Y.; Choi, J.-G. Safety and efficacy of a Vero-adapted live attenuated vaccine candidate for African swine fever. Vaccine 2025, 56, 127172. [Google Scholar] [CrossRef] [PubMed]
- Diep, N.V.; Ngoc, N.T.; Duc, N.V.; Dang, V.X.; Tiep, T.N.; Quy, C.T.; Tham, B.T.; Doanh, P.N. Safety and Efficacy Profiles of the Live Attenuated Vaccine AVAC ASF LIVE for Preventing African Swine Fever in Pigs. Transbound Emerg. Dis. 2025, 2025, 8623876. [Google Scholar] [CrossRef]
- Fan, J.; Yu, H.; Miao, F.; Ke, J.; Hu, R. Attenuated African swine fever viruses and the live vaccine candidates: A comprehensive review. Microbiol. Spectr. 2024, 12, e03199-23. [Google Scholar] [CrossRef]
- de Carvalho Ferreira, H.C.; Weesendorp, E.; Elbers, A.R.W.; Bouma, A.; Quak, S.; Stegeman, J.A.; Loeffen, W.L.A. African swine fever virus excretion patterns in persistently infected animals: A quantitative approach. Vet. Microbiol. 2012, 160, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Radulovic, E.; Mehinagic, K.; Wüthrich, T.M.; Hilty, M.; Summerfield, A.; Ruggli, N.; Benarafa, C. Development of protective immunity against African swine fever depends on host-environment interactions. Front. Vet. Sci. 2025, 12, 1553310. [Google Scholar] [CrossRef] [PubMed]

| Experiment | ASFV Strain | Found Dead/ Euthanized | Pig Number | DPI at Mortality | Ct in Spleen | Ct in SILN |
|---|---|---|---|---|---|---|
| 1 | ASFV Estonia 2014 | Found dead | 38 | 7 | 17.63 | 17.20 |
| 1 | Found dead | 9 | 8 | 16.53 | 16.49 | |
| 1 | Euthanized | 8 | 9 | 17.61 | 17.76 | |
| 1 | Euthanized | 21 | 9 | 17.09 | 18.73 | |
| 1 | Euthanized | 24 | 9 | 17.18 | 17.08 | |
| 1 | Found dead | 35 | 10 | 16.98 | 20.31 | |
| 1 | Found dead | 18 | 11 | 21.17 | 19.73 | |
| 2 | ASFV Malta’78 | Euthanized | 80 | 6 | 15.74 | 19.41 |
| 2 | Found dead | 77 | 10 | 22.65 | 23.06 |
| Whole Blood | Spleen | Tonsil | SILN | SMLN | SCLN | PFLN | PLN | GHLN | |
|---|---|---|---|---|---|---|---|---|---|
| ASFV Estonia 2014 | |||||||||
| First detection point (DPI) (number of positive pigs) | 2 (4/4) | 2 (4/4) | 1 (1/4) | 3 (4/4) | 2 (2/4) | 3 (4/4) | 3 (4/4) | 3 (4/4) | 2 (3/4) |
| Average Ct at first detection | 31.7 | 32.8 | 37.3 | 29.0 | 33.2 | 30.1 | 29.8 | 29.4 | 35.3 |
| ASFV Malta’78 | |||||||||
| First detection DPI (number of positive pigs) | 3 (4/4) | 2 (2/4) | 3 (1/4) | 3 (2/4) | 3 (3/4) | 3 (2/4) | 3 (2/4) | 3 (3/4) | 3 (4/4) |
| Average Ct at first detection | 32.6 | 37.5 | 36.5 | 36.2 | 32.8 | 37.0 | 37.0 | 35.9 | 35.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goonewardene, K.; Embury-Hyatt, C.; Moffat, E.; Ambagala, A. Kinetics of Viral Genome Distribution in Swine Peripheral Lymphoid Organs Following Oronasal Infection with Attenuated African swine fever virus strains. Viruses 2025, 17, 1472. https://doi.org/10.3390/v17111472
Goonewardene K, Embury-Hyatt C, Moffat E, Ambagala A. Kinetics of Viral Genome Distribution in Swine Peripheral Lymphoid Organs Following Oronasal Infection with Attenuated African swine fever virus strains. Viruses. 2025; 17(11):1472. https://doi.org/10.3390/v17111472
Chicago/Turabian StyleGoonewardene, Kalhari, Carissa Embury-Hyatt, Estella Moffat, and Aruna Ambagala. 2025. "Kinetics of Viral Genome Distribution in Swine Peripheral Lymphoid Organs Following Oronasal Infection with Attenuated African swine fever virus strains" Viruses 17, no. 11: 1472. https://doi.org/10.3390/v17111472
APA StyleGoonewardene, K., Embury-Hyatt, C., Moffat, E., & Ambagala, A. (2025). Kinetics of Viral Genome Distribution in Swine Peripheral Lymphoid Organs Following Oronasal Infection with Attenuated African swine fever virus strains. Viruses, 17(11), 1472. https://doi.org/10.3390/v17111472








