A Comprehensive Review of the Development and Therapeutic Use of Antivirals in Flavivirus Infection
Abstract
1. Introduction
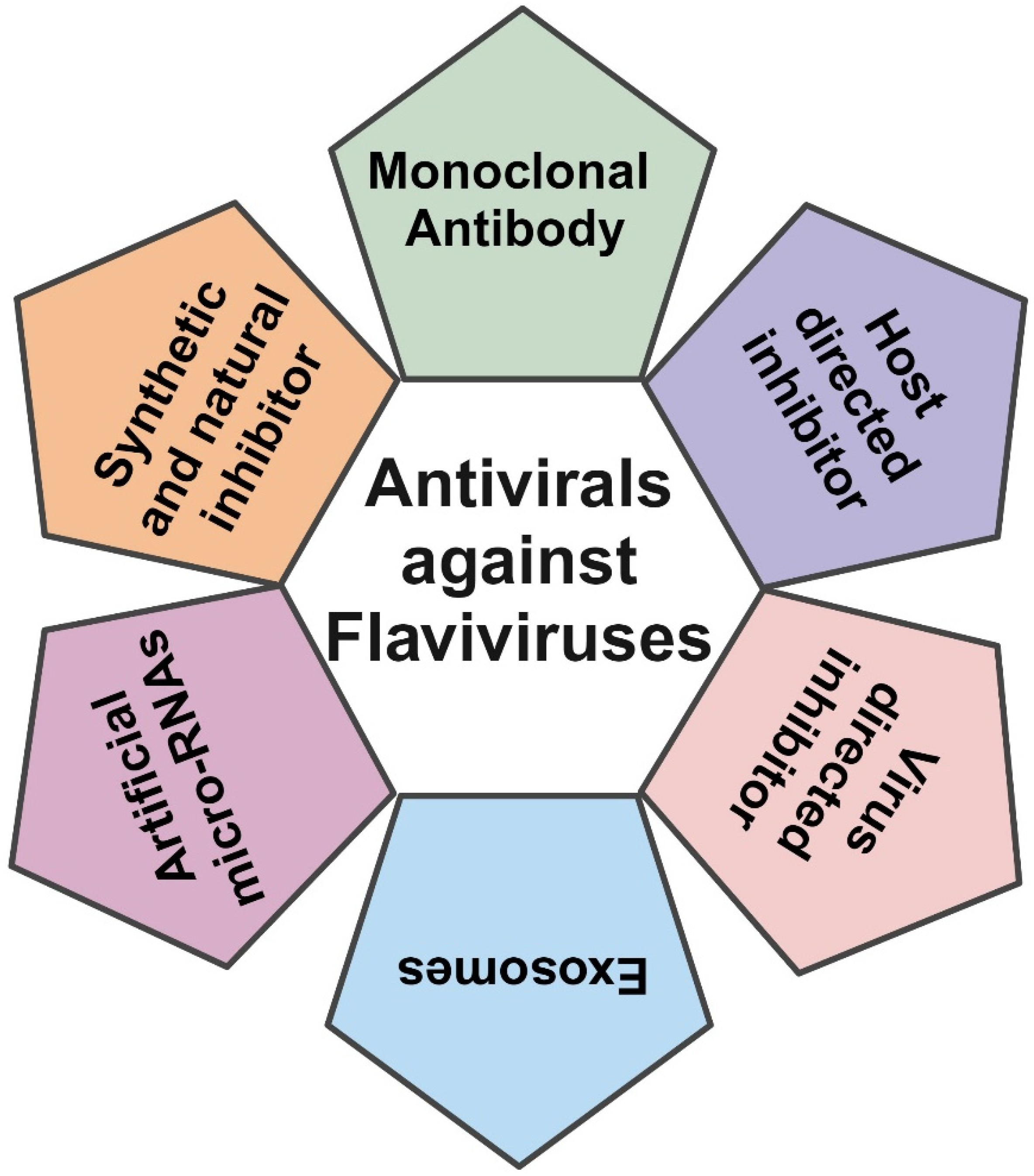
2. Antivirals Against Flavivirus
2.1. Entry Inhibitors
2.1.1. Monoclonal Antibodies (mAbs)
2.1.2. Synthetic and Natural Inhibitors
2.1.3. Host Function Inhibitors
3. Viral Replication and Polyprotein Synthesis and Processing
3.1. NS1 Inhibitors
3.2. NS2A Inhibitors
3.3. NS2B–NS3 Inhibitors
3.4. NS4A and NS4B Inhibitors
3.5. NS5 Inhibitors
3.5.1. Nucleoside Analogs
3.5.2. Non-Nucleoside Inhibitors
3.5.3. MTase Inhibitors
4. Assembly and Egress Inhibitors
C Protein Inhibitors
5. Anti-Flavivirus Drugs with Unidentified Target
6. Artificial microRNAs
7. Exosomes
8. Clinical Trials Against Flaviviruses
9. Discussion and Conclusions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 25HC | 25-Hydroxylcholesterol |
| 4-HPR | 4-Hydroxyphenyl retinamide |
| ACC | Acetyl-coenzyme A carboxylase |
| ADE | Antibody-dependent enhancement |
| AICAR | 5-Aminoimidazole-4-carboxamide ribonucleotide |
| AmiRNAs | Artificial microRNAs |
| AMPK | Adenosine monophosphate-activated protein kinase |
| C | Capsid |
| CHIKV | Chikungunya |
| CMs | Convoluted membranes |
| CQ | Chloroquine |
| CST | Castanospermine |
| D2R | Dopamine D2 receptor |
| DEFA1 | Defensin alpha 1B |
| DENV | Dengue virus |
| DHODH | Dihydroorotate dehydrogenase |
| DNJ | Deoxynojirimycin |
| dsRNA | Double-stranded RNA |
| E | Envelope |
| EDE | E-dimer epitope |
| EDIII | Domain III of envelope proteins |
| ER | Endoplasmic reticulum |
| GTase | Guanylyltransferase |
| HCQ | Hydroxychloroquine |
| HCV | Hepatitis C virus |
| HmAb | Human monoclonal antibody |
| HTS | High-throughput screening |
| IFITM3 | Interferon-induced transmembrane protein 3 |
| JEV | Japanese encephalitis virus |
| LDLR | Low-density lipoprotein receptor |
| LGTV | Langat virus |
| mAb | Monoclonal antibodies |
| MB | Methylene blue |
| MDDCs | Monocyte-derived dendritic cells |
| MERS-CoV | Middle East Respiratory Syndrome coronavirus |
| MODV | Modoc virus |
| MTase | Methyltransferase |
| NDGA | Nordihydroguaiaretic acid |
| Nis | Nucleoside/nucleotide inhibitors |
| NITD | N-sulfonylanthranilic acid derivative |
| NLSs | Nuclear localization sequences |
| NOAEL | No observed adverse effect level |
| NPC | Nuclear pore complex |
| NS | Non-structural |
| NSCs | Neural stem cells |
| PCZ | Prochlorperazine |
| PK | Pharmacokinetic |
| prM/M | Precursor membrane |
| RdRp | RNA-dependent RNA polymerase |
| SAM | S-adenosyl-L-methionine |
| SAR | Structure–activity relationship |
| shRNA | Short hairpin RNA |
| siRNA | Small interfering RNA |
| SLC | Split luciferase complementation |
| SREBP | Sterol regulatory element binding protein |
| TEM | Transmission electron microscopic |
| TGN | Trans-Golgi network |
| UTR | Untranslated region |
| UV-4B | UV-4 hydrochloride |
| VPs | Vesicular packets |
| VRC | Viral replication complex |
| WNV | West Nile virus |
| YFV | Yellow fever virus |
| ZIKV | Zika virus |
| ZIKV-Ig | Human anti-ZIKV immunoglobulin |
References
- Smit, J.M.; Moesker, B.; Rodenhuis-Zybert, I.; Wilschut, J. Flavivirus cell entry and membrane fusion. Viruses 2011, 3, 160–171. [Google Scholar] [CrossRef]
- Allison, S.L.; Stadler, K.; Mandl, C.W.; Kunz, C.; Heinz, F.X. Synthesis and secretion of recombinant tick-borne encephalitis virus protein E in soluble and particulate form. J. Virol. 1995, 69, 5816–5820. [Google Scholar] [CrossRef] [PubMed]
- Lindenbach, B.D.; Rice, C.M. Molecular biology of flaviviruses. Adv. Virus Res. 2003, 59, 23–61. [Google Scholar] [CrossRef]
- Brinton, M.A. The molecular biology of West Nile Virus: A new invader of the western hemisphere. Annu. Rev. Microbiol. 2002, 56, 371–402. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Deng, Y.Q.; Zou, P.; Wang, Q.; Dai, Y.; Yu, F.; Du, L.; Zhang, N.N.; Tian, M.; Hao, J.N.; et al. A peptide-based viral inactivator inhibits Zika virus infection in pregnant mice and fetuses. Nat. Commun. 2017, 8, 15672. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Wu, B.; Tang, H.; Luo, Z.; Xu, Z.; Ouyang, S.; Li, X.; Xie, J.; Yi, Z.; Leng, Q.; et al. Rifapentine is an entry and replication inhibitor against yellow fever virus both in vitro and in vivo. Emerg. Microbes Infect. 2022, 11, 873–884. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Qi, Z. Mosquito-Borne Flaviviruses and Current Therapeutic Advances. Viruses 2022, 14, 1226. [Google Scholar] [CrossRef]
- Mediaty, A.; Neuber, K. Total and specific serum IgE decreases with age in patients with allergic rhinitis, asthma and insect allergy but not in patients with atopic dermatitis. Immun. Ageing 2005, 2, 9. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liu, Y.; Wang, S.; Sun, J.; Wang, P.; Xin, Q.; Zhang, L.; Xiao, G.; Wang, W. Antiviral activity of peptide inhibitors derived from the protein E stem against Japanese encephalitis and Zika viruses. Antivir. Res. 2017, 141, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Alhoot, M.A.; Rathinam, A.K.; Wang, S.M.; Manikam, R.; Sekaran, S.D. Inhibition of dengue virus entry into target cells using synthetic antiviral peptides. Int. J. Med. Sci. 2013, 10, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Isa, D.M.; Chin, S.P.; Chong, W.L.; Zain, S.M.; Rahman, N.A.; Lee, V.S. Dynamics and binding interactions of peptide inhibitors of dengue virus entry. J. Biol. Phys. 2019, 45, 63–76. [Google Scholar] [CrossRef] [PubMed]
- Panya, A.; Bangphoomi, K.; Choowongkomon, K.; Yenchitsomanus, P.T. Peptide inhibitors against dengue virus infection. Chem. Biol. Drug Des. 2014, 84, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Li, P.C.; Jang, J.; Hsia, C.Y.; Groomes, P.V.; Lian, W.; de Wispelaere, M.; Pitts, J.D.; Wang, J.; Kwiatkowski, N.; Gray, N.S.; et al. Small Molecules Targeting the Flavivirus E Protein with Broad-Spectrum Activity and Antiviral Efficacy in Vivo. ACS Infect. Dis. 2019, 5, 460–472. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.N.; Tharakaraman, K.; Rowley, K.J.; Costa, V.V.; Chan, K.R.; Wong, Y.H.; Ong, L.C.; Tan, H.C.; Koch, T.; Cain, D.; et al. Structure-Guided Design of an Anti-dengue Antibody Directed to a Non-immunodominant Epitope. Cell 2015, 162, 493–504. [Google Scholar] [CrossRef]
- Fibriansah, G.; Ibarra, K.D.; Ng, T.S.; Smith, S.A.; Tan, J.L.; Lim, X.N.; Ooi, J.S.; Kostyuchenko, V.A.; Wang, J.; de Silva, A.M.; et al. DENGUE VIRUS. Cryo-EM structure of an antibody that neutralizes dengue virus type 2 by locking E protein dimers. Science 2015, 349, 88–91. [Google Scholar] [CrossRef]
- Komarasamy, T.V.; Adnan, N.A.A.; James, W.; Balasubramaniam, V.R. Finding a chink in the armor: Update, limitations, and challenges toward successful antivirals against flaviviruses. PLoS Negl. Trop. Dis. 2022, 16, e0010291. [Google Scholar] [CrossRef] [PubMed]
- White, J.; Tunga, P.; Anderson, D.M.; Iledan, K.; Loreth, T.; Parrera, G.S.; Astacio, H.; Drobic, B.; Richardson, J.S. Results of a Double-Blind, Randomized, Placebo-Controlled Phase 1 Study to Evaluate the Safety and Pharmacokinetics of Anti-Zika Virus Immunoglobulin. Am. J. Trop. Med. Hyg. 2021, 105, 1552–1562. [Google Scholar] [CrossRef]
- Hrobowski, Y.M.; Garry, R.F.; Michael, S.F. Peptide inhibitors of dengue virus and West Nile virus infectivity. Virol. J. 2005, 2, 49. [Google Scholar] [CrossRef] [PubMed]
- Beigel, J.H.; Nordstrom, J.L.; Pillemer, S.R.; Roncal, C.; Goldwater, D.R.; Li, H.; Holland, P.C.; Johnson, S.; Stein, K.; Koenig, S. Safety and pharmacokinetics of single intravenous dose of MGAWN1, a novel monoclonal antibody to West Nile virus. Antimicrob. Agents Chemother. 2010, 54, 2431–2436. [Google Scholar] [CrossRef]
- de Wispelaere, M.; Lian, W.; Potisopon, S.; Li, P.C.; Jang, J.; Ficarro, S.B.; Clark, M.J.; Zhu, X.; Kaplan, J.B.; Pitts, J.D.; et al. Inhibition of Flaviviruses by Targeting a Conserved Pocket on the Viral Envelope Protein. Cell Chem. Biol. 2018, 25, 1006–1016.e8. [Google Scholar] [CrossRef]
- Wang, J.; Bardelli, M.; Espinosa, D.A.; Pedotti, M.; Ng, T.S.; Bianchi, S.; Simonelli, L.; Lim, E.X.Y.; Foglierini, M.; Zatta, F.; et al. A Human Bi-specific Antibody against Zika Virus with High Therapeutic Potential. Cell 2017, 171, e215. [Google Scholar] [CrossRef]
- Sapparapu, G.; Fernandez, E.; Kose, N.; Bin, C.; Fox, J.M.; Bombardi, R.G.; Zhao, H.; Nelson, C.A.; Bryan, A.L.; Barnes, T.; et al. Neutralizing human antibodies prevent Zika virus replication and fetal disease in mice. Nature 2016, 540, 443–447. [Google Scholar] [CrossRef]
- Barba-Spaeth, G.; Dejnirattisai, W.; Rouvinski, A.; Vaney, M.C.; Medits, I.; Sharma, A.; Simon-Loriere, E.; Sakuntabhai, A.; Cao-Lormeau, V.M.; Haouz, A.; et al. Structural basis of potent Zika-dengue virus antibody cross-neutralization. Nature 2016, 536, 48–53. [Google Scholar] [CrossRef]
- Goo, L.; Debbink, K.; Kose, N.; Sapparapu, G.; Doyle, M.P.; Wessel, A.W.; Richner, J.M.; Burgomaster, K.E.; Larman, B.C.; Dowd, K.A.; et al. A protective human monoclonal antibody targeting the West Nile virus E protein preferentially recognizes mature virions. Nat. Microbiol. 2019, 4, 71–77. [Google Scholar] [CrossRef]
- Gao, Y.; Tai, W.; Wang, N.; Li, X.; Jiang, S.; Debnath, A.K.; Du, L.; Chen, S. Identification of Novel Natural Products as Effective and Broad-Spectrum Anti-Zika Virus Inhibitors. Viruses 2019, 11, 1019. [Google Scholar] [CrossRef] [PubMed]
- Mounce, B.C.; Cesaro, T.; Carrau, L.; Vallet, T.; Vignuzzi, M. Curcumin inhibits Zika and chikungunya virus infection by inhibiting cell binding. Antivir. Res. 2017, 142, 148–157. [Google Scholar] [CrossRef]
- Padilla, S.L.; Rodriguez, A.; Gonzales, M.M.; Gallego, G.J.; Castano, O.J. Inhibitory effects of curcumin on dengue virus type 2-infected cells in vitro. Arch. Virol. 2014, 159, 573–579. [Google Scholar] [CrossRef]
- Yang, C.C.; Hu, H.S.; Lin, H.M.; Wu, P.S.; Wu, R.H.; Tian, J.N.; Wu, S.H.; Tsou, L.K.; Song, J.S.; Chen, H.W.; et al. A novel flavivirus entry inhibitor, BP34610, discovered through high-throughput screening with dengue reporter viruses. Antivir. Res. 2019, 172, 104636. [Google Scholar] [CrossRef]
- Abdul Ahmad, S.A.; Palanisamy, U.D.; Tejo, B.A.; Chew, M.F.; Tham, H.W.; Syed Hassan, S. Geraniin extracted from the rind of Nephelium lappaceum binds to dengue virus type-2 envelope protein and inhibits early stage of virus replication. Virol. J. 2017, 14, 229. [Google Scholar] [CrossRef]
- Abdul Ahmad, S.A.; Palanisamy, U.D.; Khoo, J.J.; Dhanoa, A.; Syed Hassan, S. Efficacy of geraniin on dengue virus type-2 infected BALB/c mice. Virol. J. 2019, 16, 26. [Google Scholar] [CrossRef] [PubMed]
- Jia, F.; Zou, G.; Fan, J.; Yuan, Z. Identification of palmatine as an inhibitor of West Nile virus. Arch. Virol. 2010, 155, 1325–1329. [Google Scholar] [CrossRef] [PubMed]
- Simanjuntak, Y.; Liang, J.J.; Lee, Y.L.; Lin, Y.L. Repurposing of prochlorperazine for use against dengue virus infection. J. Infect. Dis. 2015, 211, 394–404. [Google Scholar] [CrossRef]
- Barrows, N.J.; Campos, R.K.; Powell, S.T.; Prasanth, K.R.; Schott-Lerner, G.; Soto-Acosta, R.; Galarza-Munoz, G.; McGrath, E.L.; Urrabaz-Garza, R.; Gao, J.; et al. A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection. Cell Host Microbe 2016, 20, 259–270. [Google Scholar] [CrossRef]
- Rausch, K.; Hackett, B.A.; Weinbren, N.L.; Reeder, S.M.; Sadovsky, Y.; Hunter, C.A.; Schultz, D.C.; Coyne, C.B.; Cherry, S. Screening Bioactives Reveals Nanchangmycin as a Broad Spectrum Antiviral Active against Zika Virus. Cell Rep. 2017, 18, 804–815. [Google Scholar] [CrossRef] [PubMed]
- Abrams, R.P.M.; Yasgar, A.; Teramoto, T.; Lee, M.H.; Dorjsuren, D.; Eastman, R.T.; Malik, N.; Zakharov, A.V.; Li, W.; Bachani, M.; et al. Therapeutic candidates for the Zika virus identified by a high-throughput screen for Zika protease inhibitors. Proc. Natl. Acad. Sci. USA 2020, 117, 31365–31375. [Google Scholar] [CrossRef]
- Pu, S.Y.; Xiao, F.; Schor, S.; Bekerman, E.; Zanini, F.; Barouch-Bentov, R.; Nagamine, C.M.; Einav, S. Feasibility and biological rationale of repurposing sunitinib and erlotinib for dengue treatment. Antivir. Res. 2018, 155, 67–75. [Google Scholar] [CrossRef]
- Li, C.; Deng, Y.Q.; Wang, S.; Ma, F.; Aliyari, R.; Huang, X.Y.; Zhang, N.N.; Watanabe, M.; Dong, H.L.; Liu, P.; et al. 25-Hydroxycholesterol Protects Host against Zika Virus Infection and Its Associated Microcephaly in a Mouse Model. Immunity 2017, 46, 446–456. [Google Scholar] [CrossRef]
- Savarino, A.; Boelaert, J.R.; Cassone, A.; Majori, G.; Cauda, R. Effects of chloroquine on viral infections: An old drug against today’s diseases? Lancet Infect. Dis. 2003, 3, 722–727. [Google Scholar] [CrossRef]
- Wang, M.; Cao, R.; Zhang, L.; Yang, X.; Liu, J.; Xu, M.; Shi, Z.; Hu, Z.; Zhong, W.; Xiao, G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020, 30, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Tricou, V.; Minh, N.N.; Van, T.P.; Lee, S.J.; Farrar, J.; Wills, B.; Tran, H.T.; Simmons, C.P. A randomized controlled trial of chloroquine for the treatment of dengue in Vietnamese adults. PLoS Negl. Trop. Dis. 2010, 4, e785. [Google Scholar] [CrossRef]
- Dyall, J.; Gross, R.; Kindrachuk, J.; Johnson, R.F.; Olinger, G.G.J.; Hensley, L.E.; Frieman, M.B.; Jahrling, P.B. Middle East Respiratory Syndrome and Severe Acute Respiratory Syndrome: Current Therapeutic Options and Potential Targets for Novel Therapies. Drugs 2017, 77, 1935–1966. [Google Scholar] [CrossRef]
- Michael, F.S.; Isern, S. Flavivirus-Binding, Entry-Obstructing, Protease-Resistant Peptide (RI57). U.S. Patent 10639380 B2, 5 May 2020. [Google Scholar]
- Bailey, M.J.; Broecker, F.; Freyn, A.W.; Choi, A.; Brown, J.A.; Fedorova, N.; Simon, V.; Lim, J.K.; Evans, M.J.; Garcia-Sastre, A.; et al. Human Monoclonal Antibodies Potently Neutralize Zika Virus and Select for Escape Mutations on the Lateral Ridge of the Envelope Protein. J. Virol. 2019, 93, e00405-19. [Google Scholar] [CrossRef]
- Saxena, P.R.; Lawang, A. A comparison of cardiovascular and smooth muscle effects of 5-hydroxytryptamine and 5-carboxamidotryptamine, a selective agonist of 5-HT1 receptors. Arch. Int. Pharmacodyn. Ther. 1985, 277, 235–252. [Google Scholar]
- Badani, H.; Garry, R.F.; Wimley, W.C. Peptide entry inhibitors of enveloped viruses: The importance of interfacial hydrophobicity. Biochim. Biophys. Acta. 2014, 1838, 2180–2197. [Google Scholar] [CrossRef]
- Shoji-Kawata, S.; Sumpter, R.; Leveno, M.; Campbell, G.R.; Zou, Z.; Kinch, L.; Wilkins, A.D.; Sun, Q.; Pallauf, K.; MacDuff, D.; et al. Identification of a candidate therapeutic autophagy-inducing peptide. Nature 2013, 494, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Focosi, D.; McConnell, S.; Casadevall, A.; Cappello, E.; Valdiserra, G.; Tuccori, M. Monoclonal antibody therapies against SARS-CoV-2. Lancet Infect. Dis. 2022, 22, e311–e326. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Du, L. Advances in the research and development of therapeutic antibodies against the Zika virus. Cell. Mol. Immunol. 2019, 16, 96–97. [Google Scholar] [CrossRef]
- Mancini, N. Monoclonal Antibodies and Flaviviruses: A Possible Option? mBio 2022, 13, e0082422. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Smatti, M.K.; Ouhtit, A.; Cyprian, F.S.; Almaslamani, M.A.; Thani, A.A.; Yassine, H.M. Antibody-Dependent Enhancement (ADE) and the role of complement system in disease pathogenesis. Mol. Immunol. 2022, 152, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Lim, L.; Srivastava, S.; Lu, Y.; Song, J. Solution conformations of Zika NS2B-NS3pro and its inhibition by natural products from edible plants. PLoS ONE 2017, 12, e0180632. [Google Scholar] [CrossRef] [PubMed]
- Allard, P.M.; Dau, E.T.; Eydoux, C.; Guillemot, J.C.; Dumontet, V.; Poullain, C.; Canard, B.; Gueritte, F.; Litaudon, M. Alkylated flavanones from the bark of Cryptocarya chartacea as dengue virus NS5 polymerase inhibitors. J. Nat. Prod. 2011, 74, 2446–2453. [Google Scholar] [CrossRef]
- Nawa, M.; Takasaki, T.; Yamada, K.I.; Kurane, I.; Akatsuka, T. Interference in Japanese encephalitis virus infection of Vero cells by a cationic amphiphilic drug, chlorpromazine. J. Gen. Virol. 2003, 84, 1737–1741. [Google Scholar] [CrossRef] [PubMed]
- Jimenez de Oya, N.; Blazquez, A.B.; Casas, J.; Saiz, J.C.; Martin-Acebes, M.A. Direct Activation of Adenosine Monophosphate-Activated Protein Kinase (AMPK) by PF-06409577 Inhibits Flavivirus Infection through Modification of Host Cell Lipid Metabolism. Antimicrob. Agents Chemother. 2018, 62, e00360-18. [Google Scholar] [CrossRef] [PubMed]
- Jimenez de Oya, N.; Esler, W.P.; Huard, K.; El-Kattan, A.F.; Karamanlidis, G.; Blazquez, A.B.; Ramos-Ibeas, P.; Escribano-Romero, E.; Louloudes-Lazaro, A.; Casas, J.; et al. Targeting host metabolism by inhibition of acetyl-Coenzyme A carboxylase reduces flavivirus infection in mouse models. Emerg. Microbes Infect. 2019, 8, 624–636. [Google Scholar] [CrossRef]
- Huang, Y.; Li, Y.; Zhang, H.; Zhao, R.; Jing, R.; Xu, Y.; He, M.; Peer, J.; Kim, Y.C.; Luo, J.; et al. Zika virus propagation and release in human fetal astrocytes can be suppressed by neutral sphingomyelinase-2 inhibitor GW4869. Cell Discov. 2018, 4, 19. [Google Scholar] [CrossRef] [PubMed]
- Martin-Acebes, M.A.; Merino-Ramos, T.; Blazquez, A.B.; Casas, J.; Escribano-Romero, E.; Sobrino, F.; Saiz, J.C. The composition of West Nile virus lipid envelope unveils a role of sphingolipid metabolism in flavivirus biogenesis. J. Virol. 2014, 88, 12041–12054. [Google Scholar] [CrossRef]
- Navarro-Sanchez, E.; Altmeyer, R.; Amara, A.; Schwartz, O.; Fieschi, F.; Virelizier, J.L.; Arenzana-Seisdedos, F.; Despres, P. Dendritic-cell-specific ICAM3-grabbing non-integrin is essential for the productive infection of human dendritic cells by mosquito-cell-derived dengue viruses. EMBO Rep. 2003, 4, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Lee, E.M.; Wen, Z.; Cheng, Y.; Huang, W.K.; Qian, X.; Tcw, J.; Kouznetsova, J.; Ogden, S.C.; Hammack, C.; et al. Identification of small-molecule inhibitors of Zika virus infection and induced neural cell death via a drug repurposing screen. Nat. Med. 2016, 22, 1101–1107. [Google Scholar] [CrossRef]
- Yang, C.F.; Gopula, B.; Liang, J.J.; Li, J.K.; Chen, S.Y.; Lee, Y.L.; Chen, C.S.; Lin, Y.L. Novel AR-12 derivatives, P12-23 and P12-34, inhibit flavivirus replication by blocking host de novo pyrimidine biosynthesis. Emerg. Microbes Infect. 2018, 7, 187. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.J.; Ng, M.L. Infectious entry of West Nile virus occurs through a clathrin-mediated endocytic pathway. J. Virol. 2004, 78, 10543–10555. [Google Scholar] [CrossRef]
- Martin-Acebes, M.A.; Jimenez de Oya, N.; Saiz, J.C. Lipid Metabolism as a Source of Druggable Targets for Antiviral Discovery against Zika and Other Flaviviruses. Pharmaceuticals 2019, 12, 97. [Google Scholar] [CrossRef]
- Farfan-Morales, C.N.; Cordero-Rivera, C.D.; Osuna-Ramos, J.F.; Monroy-Munoz, I.E.; De Jesus-Gonzalez, L.A.; Munoz-Medina, J.E.; Hurtado-Monzon, A.M.; Reyes-Ruiz, J.M.; Del Angel, R.M. The antiviral effect of metformin on zika and dengue virus infection. Sci. Rep. 2021, 11, 8743. [Google Scholar] [CrossRef] [PubMed]
- Htun, H.L.; Yeo, T.W.; Tam, C.C.; Pang, J.; Leo, Y.S.; Lye, D.C. Metformin Use and Severe Dengue in Diabetic Adults. Sci. Rep. 2018, 8, 3344. [Google Scholar] [CrossRef]
- Li, Z.; Brecher, M.; Deng, Y.Q.; Zhang, J.; Sakamuru, S.; Liu, B.; Huang, R.; Koetzner, C.A.; Allen, C.A.; Jones, S.A.; et al. Existing drugs as broad-spectrum and potent inhibitors for Zika virus by targeting NS2B-NS3 interaction. Cell Res. 2017, 27, 1046–1064. [Google Scholar] [CrossRef] [PubMed]
- Akey, D.L.; Brown, W.C.; Jose, J.; Kuhn, R.J.; Smith, J.L. Structure-guided insights on the role of NS1 in flavivirus infection. Bioessays 2015, 37, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Welsch, S.; Miller, S.; Romero-Brey, I.; Merz, A.; Bleck, C.K.; Walther, P.; Fuller, S.D.; Antony, C.; Krijnse-Locker, J.; Bartenschlager, R. Composition and three-dimensional architecture of the dengue virus replication and assembly sites. Cell Host Microbe 2009, 5, 365–375. [Google Scholar] [CrossRef]
- Songprakhon, P.; Thaingtamtanha, T.; Limjindaporn, T.; Puttikhunt, C.; Srisawat, C.; Luangaram, P.; Dechtawewat, T.; Uthaipibull, C.; Thongsima, S.; Yenchitsomanus, P.T.; et al. Peptides targeting dengue viral nonstructural protein 1 inhibit dengue virus production. Sci. Rep. 2020, 10, 12933. [Google Scholar] [CrossRef] [PubMed]
- Sun, E.C.; Ma, J.N.; Liu, N.H.; Yang, T.; Zhao, J.; Geng, H.W.; Wang, L.F.; Qin, Y.L.; Bu, Z.G.; Yang, Y.H.; et al. Identification of two linear B-cell epitopes from West Nile virus NS1 by screening a phage-displayed random peptide library. BMC Microbiol. 2011, 11, 160. [Google Scholar] [CrossRef]
- Raza, S.; Abbas, G.; Azam, S.S. Screening Pipeline for Flavivirus Based Inhibitors for Zika Virus NS1. IEEE/ACM Trans. Comput. Biol. Bioinform. 2020, 17, 1751–1761. [Google Scholar] [CrossRef]
- Bailey, M.J.; Duehr, J.; Dulin, H.; Broecker, F.; Brown, J.A.; Arumemi, F.O.; Bermudez Gonzalez, M.C.; Leyva-Grado, V.H.; Evans, M.J.; Simon, V.; et al. Human antibodies targeting Zika virus NS1 provide protection against disease in a mouse model. Nat. Commun. 2018, 9, 4560. [Google Scholar] [CrossRef]
- Biering, S.B.; Akey, D.L.; Wong, M.P.; Brown, W.C.; Lo, N.T.N.; Puerta-Guardo, H.; Tramontini Gomes de Sousa, F.; Wang, C.; Konwerski, J.R.; Espinosa, D.A.; et al. Structural basis for antibody inhibition of flavivirus NS1-triggered endothelial dysfunction. Science 2021, 371, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Courageot, M.P.; Frenkiel, M.P.; Dos Santos, C.D.; Deubel, V.; Despres, P. Alpha-glucosidase inhibitors reduce dengue virus production by affecting the initial steps of virion morphogenesis in the endoplasmic reticulum. J. Virol. 2000, 74, 564–572. [Google Scholar] [CrossRef]
- Wu, S.F.; Lee, C.J.; Liao, C.L.; Dwek, R.A.; Zitzmann, N.; Lin, Y.L. Antiviral effects of an iminosugar derivative on flavivirus infections. J. Virol. 2002, 76, 3596–3604. [Google Scholar] [CrossRef] [PubMed]
- Edeling, M.A.; Diamond, M.S.; Fremont, D.H. Structural basis of Flavivirus NS1 assembly and antibody recognition. Proc. Natl. Acad. Sci. USA 2014, 111, 4285–4290. [Google Scholar] [CrossRef]
- Halstead, S.B. Stumbles on the path to dengue control. Lancet Infect. Dis. 2014, 14, 661–662. [Google Scholar] [CrossRef] [PubMed]
- Montes-Grajales, D.; Puerta-Guardo, H.; Espinosa, D.A.; Harris, E.; Caicedo-Torres, W.; Olivero-Verbel, J.; Martinez-Romero, E. In silico drug repurposing for the identification of potential candidate molecules against arboviruses infection. Antivir. Res. 2020, 173, 104668. [Google Scholar] [CrossRef]
- Yuan, S.; Chan, J.F.; den-Haan, H.; Chik, K.K.; Zhang, A.J.; Chan, C.C.; Poon, V.K.; Yip, C.C.; Mak, W.W.; Zhu, Z.; et al. Structure-based discovery of clinically approved drugs as Zika virus NS2B-NS3 protease inhibitors that potently inhibit Zika virus infection in vitro and in vivo. Antivir. Res. 2017, 145, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Xu, J.; Lang, Y.; Fan, X.; Kuo, L.; D’Brant, L.; Hu, S.; Samrat, S.K.; Trudeau, N.; Tharappel, A.M.; et al. JMX0207, a Niclosamide Derivative with Improved Pharmacokinetics, Suppresses Zika Virus Infection Both In Vitro and In Vivo. ACS Infect. Dis. 2020, 6, 2616–2628. [Google Scholar] [CrossRef]
- Bhakat, S.; Delang, L.; Kaptein, S.; Neyts, J.; Leyssen, P.; Jayaprakash, V. Reaching beyond HIV/HCV: Nelfinavir as a potential starting point for broad-spectrum protease inhibitors against dengue and chikungunya virus. RSC Adv. 2015, 5, 85938–85949. [Google Scholar] [CrossRef]
- Rassias, G.; Zogali, V.; Swarbrick, C.M.D.; Ki Chan, K.W.; Chan, S.A.; Gwee, C.P.; Wang, S.; Kaplanai, E.; Canko, A.; Kiousis, D.; et al. Cell-active carbazole derivatives as inhibitors of the zika virus protease. Eur. J. Med. Chem. 2019, 180, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Cabarcas-Montalvo, M.; Maldonado-Rojas, W.; Montes-Grajales, D.; Bertel-Sevilla, A.; Wagner-Dobler, I.; Sztajer, H.; Reck, M.; Flechas-Alarcon, M.; Ocazionez, R.; Olivero-Verbel, J. Discovery of antiviral molecules for dengue: In silico search and biological evaluation. Eur. J. Med. Chem. 2016, 110, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Brecher, M.; Li, Z.; Liu, B.; Zhang, J.; Koetzner, C.A.; Alifarag, A.; Jones, S.A.; Lin, Q.; Kramer, L.D.; Li, H. A conformational switch high-throughput screening assay and allosteric inhibition of the flavivirus NS2B-NS3 protease. PLoS Pathog. 2017, 13, e1006411. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Zhou, R.; Huang, C.; Zhang, R.; Wang, J.; Zhang, Y.; Ding, J.; Li, X.; Zhou, J.; Cen, S. Identification of Theaflavin-3,3’-Digallate as a Novel Zika Virus Protease Inhibitor. Front. Pharmacol. 2020, 11, 514313. [Google Scholar] [CrossRef] [PubMed]
- Raut, R.; Beesetti, H.; Tyagi, P.; Khanna, I.; Jain, S.K.; Jeankumar, V.U.; Yogeeswari, P.; Sriram, D.; Swaminathan, S. A small molecule inhibitor of dengue virus type 2 protease inhibits the replication of all four dengue virus serotypes in cell culture. Virol. J. 2015, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Aleshin, A.E.; Shiryaev, S.A.; Strongin, A.Y.; Liddington, R.C. Structural evidence for regulation and specificity of flaviviral proteases and evolution of the Flaviviridae fold. Protein Sci. 2007, 16, 795–806. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Liang, B.; Aarthy, M.; Singh, S.K.; Garg, N.; Mysorekar, I.U.; Giri, R. Hydroxychloroquine Inhibits Zika Virus NS2B-NS3 Protease. ACS Omega 2018, 3, 18132–18141. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.P.; Hu, L.F.; Zheng, H.F.; Mao, C.J.; Hu, W.D.; Xiong, K.P.; Wang, F.; Liu, C.F. Application and interpretation of current autophagy inhibitors and activators. Acta Pharmacol. Sin. 2013, 34, 625–635. [Google Scholar] [CrossRef]
- Li, Z.; Lang, Y.; Sakamuru, S.; Samrat, S.; Trudeau, N.; Kuo, L.; Rugenstein, N.; Tharappel, A.; D’Brant, L.; Koetzner, C.A.; et al. Methylene blue is a potent and broad-spectrum inhibitor against Zika virus in vitro and in vivo. Emerg. Microbes Infect. 2020, 9, 2404–2416. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Xu, J.; Lang, Y.; Wu, X.; Hu, S.; Samrat, S.K.; Tharappel, A.M.; Kuo, L.; Butler, D.; Song, Y.; et al. In vitro and in vivo characterization of erythrosin B and derivatives against Zika virus. Acta Pharm. Sin. B 2022, 12, 1662–1670. [Google Scholar] [CrossRef]
- Li, Z.; Sakamuru, S.; Huang, R.; Brecher, M.; Koetzner, C.A.; Zhang, J.; Chen, H.; Qin, C.F.; Zhang, Q.Y.; Zhou, J.; et al. Erythrosin B is a potent and broad-spectrum orthosteric inhibitor of the flavivirus NS2B-NS3 protease. Antivir. Res. 2018, 150, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Mastrangelo, E.; Pezzullo, M.; De Burghgraeve, T.; Kaptein, S.; Pastorino, B.; Dallmeier, K.; de Lamballerie, X.; Neyts, J.; Hanson, A.M.; Frick, D.N.; et al. Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: New prospects for an old drug. J. Antimicrob. Chemother. 2012, 67, 1884–1894. [Google Scholar] [CrossRef] [PubMed]
- Ketkar, H.; Yang, L.; Wormser, G.P.; Wang, P. Lack of efficacy of ivermectin for prevention of a lethal Zika virus infection in a murine system. Diagn. Microbiol. Infect. Dis. 2019, 95, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Caly, L.; Druce, J.D.; Catton, M.G.; Jans, D.A.; Wagstaff, K.M. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antivir. Res 2020, 178, 104787. [Google Scholar] [CrossRef]
- Ci, Y.; Yao, B.; Yue, K.; Yang, Y.; Xu, C.; Li, D.F.; Qin, C.F.; Shi, L. Bortezomib inhibits ZIKV/DENV by interfering with viral polyprotein cleavage via the ERAD pathway. Cell Chem. Biol. 2023, 30, 527–539.e5. [Google Scholar] [CrossRef] [PubMed]
- Pathak, N.; Lai, M.L.; Chen, W.Y.; Hsieh, B.W.; Yu, G.Y.; Yang, J.M. Pharmacophore anchor models of flaviviral NS3 proteases lead to drug repurposing for DENV infection. BMC Bioinform. 2017, 18, 548. [Google Scholar] [CrossRef]
- Byrd, C.M.; Grosenbach, D.W.; Berhanu, A.; Dai, D.; Jones, K.F.; Cardwell, K.B.; Schneider, C.; Yang, G.; Tyavanagimatt, S.; Harver, C.; et al. Novel benzoxazole inhibitor of dengue virus replication that targets the NS3 helicase. Antimicrob. Agents Chemother. 2013, 57, 1902–1912. [Google Scholar] [CrossRef]
- Yao, Y.; Huo, T.; Lin, Y.L.; Nie, S.; Wu, F.; Hua, Y.; Wu, J.; Kneubehl, A.R.; Vogt, M.B.; Rico-Hesse, R.; et al. Discovery, X-ray Crystallography and Antiviral Activity of Allosteric Inhibitors of Flavivirus NS2B-NS3 Protease. J. Am. Chem. Soc. 2019, 141, 6832–6836. [Google Scholar] [CrossRef]
- Sweeney, N.L.; Hanson, A.M.; Mukherjee, S.; Ndjomou, J.; Geiss, B.J.; Steel, J.J.; Frankowski, K.J.; Li, K.; Schoenen, F.J.; Frick, D.N. Benzothiazole and Pyrrolone Flavivirus Inhibitors Targeting the Viral Helicase. ACS Infect. Dis. 2015, 1, 140–148. [Google Scholar] [CrossRef]
- Basavannacharya, C.; Vasudevan, S.G. Suramin inhibits helicase activity of NS3 protein of dengue virus in a fluorescence-based high throughput assay format. Biochem. Biophys. Res. Commun. 2014, 453, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Shiryaev, S.A.; Farhy, C.; Pinto, A.; Huang, C.T.; Simonetti, N.; Elong Ngono, A.; Dewing, A.; Shresta, S.; Pinkerton, A.B.; Cieplak, P.; et al. Characterization of the Zika virus two-component NS2B-NS3 protease and structure-assisted identification of allosteric small-molecule antagonists. Antivir. Res. 2017, 143, 218–229. [Google Scholar] [CrossRef] [PubMed]
- Nobori, H.; Toba, S.; Yoshida, R.; Hall, W.W.; Orba, Y.; Sawa, H.; Sato, A. Identification of Compound-B, a novel anti-dengue virus agent targeting the non-structural protein 4A. Antivir. Res. 2018, 155, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Kaptein, S.J.F.; Goethals, O.; Kiemel, D.; Marchand, A.; Kesteleyn, B.; Bonfanti, J.F.; Bardiot, D.; Stoops, B.; Jonckers, T.H.M.; Dallmeier, K.; et al. Publisher Correction: A pan-serotype dengue virus inhibitor targeting the NS3-NS4B interaction. Nature 2021, 599, E2. [Google Scholar] [CrossRef] [PubMed]
- Goethals, O.; Voge, N.V.; Kesteleyn, B.; Chaltin, P.; Jinks, T.; De Marez, T.; Koul, A.; Draghia-Akli, R.; Neyts, J.; Van Loock, M. A pan-serotype antiviral to prevent and treat dengue: A journey from discovery to clinical development driven by public-private partnerships. Antivir. Res. 2023, 210, 105495. [Google Scholar] [CrossRef] [PubMed]
- Moquin, S.A.; Simon, O.; Karuna, R.; Lakshminarayana, S.B.; Yokokawa, F.; Wang, F.; Saravanan, C.; Zhang, J.; Day, C.W.; Chan, K.; et al. NITD-688, a pan-serotype inhibitor of the dengue virus NS4B protein, shows favorable pharmacokinetics and efficacy in preclinical animal models. Sci. Transl. Med. 2021, 13, eabb2181. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Liu, Y.; Guo, J.; Wang, P.; Zhang, L.; Xiao, G.; Wang, W. Screening of FDA-Approved Drugs for Inhibitors of Japanese Encephalitis Virus Infection. J. Virol. 2017, 91, e01055-17. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Xie, X.; Ye, N.; Zou, J.; Chen, H.; White, M.A.; Shi, P.Y.; Zhou, J. Design, Synthesis, and Biological Evaluation of Substituted 4,6-Dihydrospiro[[1,2,3]triazolo[4,5-b]pyridine-7,3’-indoline]-2’,5(3H)-dione Analogues as Potent NS4B Inhibitors for the Treatment of Dengue Virus Infection. J. Med. Chem. 2019, 62, 7941–7960. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Zhang, X.; Zhang, L.; Wu, S.; Ma, J.; Wang, F.; Zhou, Y.; Dai, X.; Bullitt, E.; Du, Y.; et al. A yellow fever virus NS4B inhibitor not only suppresses viral replication, but also enhances the virus activation of RIG-I-like receptor-mediated innate immune response. PLoS Pathog. 2022, 18, e1010271. [Google Scholar] [CrossRef] [PubMed]
- Riva, L.; Goellner, S.; Biering, S.B.; Huang, C.T.; Rubanov, A.N.; Haselmann, U.; Warnes, C.M.; De Jesus, P.D.; Martin-Sancho, L.; Terskikh, A.V.; et al. The Compound SBI-0090799 Inhibits Zika Virus Infection by Blocking De Novo Formation of the Membranous Replication Compartment. J. Virol. 2021, 95, e00996-21. [Google Scholar] [CrossRef]
- de Wispelaere, M.; LaCroix, A.J.; Yang, P.L. The small molecules AZD0530 and dasatinib inhibit dengue virus RNA replication via Fyn kinase. J. Virol. 2013, 87, 7367–7381. [Google Scholar] [CrossRef] [PubMed]
- Zmurko, J.; Neyts, J.; Dallmeier, K. Flaviviral NS4b, chameleon and jack-in-the-box roles in viral replication and pathogenesis, and a molecular target for antiviral intervention. Rev. Med. Virol. 2015, 25, 205–223. [Google Scholar] [CrossRef]
- Eyer, L.; Zouharova, D.; Sirmarova, J.; Fojtikova, M.; Stefanik, M.; Haviernik, J.; Nencka, R.; de Clercq, E.; Ruzek, D. Antiviral activity of the adenosine analogue BCX4430 against West Nile virus and tick-borne flaviviruses. Antivir. Res. 2017, 142, 63–67. [Google Scholar] [CrossRef]
- Julander, J.G.; Siddharthan, V.; Evans, J.; Taylor, R.; Tolbert, K.; Apuli, C.; Stewart, J.; Collins, P.; Gebre, M.; Neilson, S.; et al. Efficacy of the broad-spectrum antiviral compound BCX4430 against Zika virus in cell culture and in a mouse model. Antivir. Res. 2017, 137, 14–22. [Google Scholar] [CrossRef]
- Julander, J.G.; Demarest, J.F.; Taylor, R.; Gowen, B.B.; Walling, D.M.; Mathis, A.; Babu, Y.S. An update on the progress of galidesivir (BCX4430), a broad-spectrum antiviral. Antivir. Res. 2021, 195, 105180. [Google Scholar] [CrossRef]
- Escribano-Romero, E.; Jimenez de Oya, N.; Domingo, E.; Saiz, J.C. Extinction of West Nile Virus by Favipiravir through Lethal Mutagenesis. Antimicrob. Agents Chemother. 2017, 61, e01400-17. [Google Scholar] [CrossRef] [PubMed]
- Marlin, R.; Desjardins, D.; Contreras, V.; Lingas, G.; Solas, C.; Roques, P.; Naninck, T.; Pascal, Q.; Behillil, S.; Maisonnasse, P.; et al. Antiviral efficacy of favipiravir against Zika and SARS-CoV-2 viruses in non-human primates. Nat. Commun. 2022, 13, 5108. [Google Scholar] [CrossRef]
- Chen, Y.L.; Abdul Ghafar, N.; Karuna, R.; Fu, Y.; Lim, S.P.; Schul, W.; Gu, F.; Herve, M.; Yokohama, F.; Wang, G.; et al. Activation of peripheral blood mononuclear cells by dengue virus infection depotentiates balapiravir. J. Virol. 2014, 88, 1740–1747. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.Q.; Zhang, N.N.; Li, C.F.; Tian, M.; Hao, J.N.; Xie, X.P.; Shi, P.Y.; Qin, C.F. Adenosine Analog NITD008 Is a Potent Inhibitor of Zika Virus. Open Forum Infect. Dis. 2016, 3, ofw175. [Google Scholar] [CrossRef]
- Hackenbruch, C.; Maringer, Y.; Tegeler, C.M.; Walz, J.S.; Nelde, A.; Heitmann, J.S. Elevated SARS-CoV-2-Specific Antibody Levels in Patients with Post-COVID Syndrome. Viruses 2023, 15, 701. [Google Scholar] [CrossRef]
- Lin, K.; Good, S.S.; Julander, J.G.; Weight, A.E.; Moussa, A.; Sommadossi, J.P. AT-752, a double prodrug of a guanosine nucleotide analog, inhibits yellow fever virus in a hamster model. PLoS Negl. Trop. Dis. 2022, 16, e0009937. [Google Scholar] [CrossRef]
- Good, S.S.; Shannon, A.; Lin, K.; Moussa, A.; Julander, J.G.; La Colla, P.; Collu, G.; Canard, B.; Sommadossi, J.P. Evaluation of AT-752, a Double Prodrug of a Guanosine Nucleotide Analog with In Vitro and In Vivo Activity against Dengue and Other Flaviviruses. Antimicrob. Agents Chemother. 2021, 65, e00988-21. [Google Scholar] [CrossRef]
- Eyer, L.; Fojtikova, M.; Nencka, R.; Rudolf, I.; Hubalek, Z.; Ruzek, D. Viral RNA-Dependent RNA Polymerase Inhibitor 7-Deaza-2’-C-Methyladenosine Prevents Death in a Mouse Model of West Nile Virus Infection. Antimicrob. Agents Chemother. 2019, 63, e02093-18. [Google Scholar] [CrossRef] [PubMed]
- Schul, W.; Liu, W.; Xu, H.Y.; Flamand, M.; Vasudevan, S.G. A dengue fever viremia model in mice shows reduction in viral replication and suppression of the inflammatory response after treatment with antiviral drugs. J. Infect. Dis. 2007, 195, 665–674. [Google Scholar] [CrossRef] [PubMed]
- de Freitas, C.S.; Higa, L.M.; Sacramento, C.Q.; Ferreira, A.C.; Reis, P.A.; Delvecchio, R.; Monteiro, F.L.; Barbosa-Lima, G.; James Westgarth, H.; Vieira, Y.R.; et al. Yellow fever virus is susceptible to sofosbuvir both in vitro and in vivo. PLoS Negl. Trop. Dis. 2019, 13, e0007072. [Google Scholar] [CrossRef]
- Sacramento, C.Q.; de Melo, G.R.; de Freitas, C.S.; Rocha, N.; Hoelz, L.V.; Miranda, M.; Fintelman-Rodrigues, N.; Marttorelli, A.; Ferreira, A.C.; Barbosa-Lima, G.; et al. The clinically approved antiviral drug sofosbuvir inhibits Zika virus replication. Sci. Rep. 2017, 7, 40920. [Google Scholar] [CrossRef]
- Mesci, P.; Macia, A.; LaRock, C.N.; Tejwani, L.; Fernandes, I.R.; Suarez, N.A.; de A. Zanotto, P.M.; Beltrao-Braga, P.C.B.; Nizet, V.; Muotri, A.R. Modeling neuro-immune interactions during Zika virus infection. Hum. Mol. Genet. 2018, 27, 41–52. [Google Scholar] [CrossRef]
- Arora, R.; Liew, C.W.; Soh, T.S.; Otoo, D.A.; Seh, C.C.; Yue, K.; Nilar, S.; Wang, G.; Yokokawa, F.; Noble, C.G.; et al. Two RNA Tunnel Inhibitors Bind in Highly Conserved Sites in Dengue Virus NS5 Polymerase: Structural and Functional Studies. J. Virol. 2020, 94, e01130-20. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.P.; Noble, C.G.; Seh, C.C.; Soh, T.S.; El Sahili, A.; Chan, G.K.; Lescar, J.; Arora, R.; Benson, T.; Nilar, S.; et al. Potent Allosteric Dengue Virus NS5 Polymerase Inhibitors: Mechanism of Action and Resistance Profiling. PLoS Pathog. 2016, 12, e1005737. [Google Scholar] [CrossRef] [PubMed]
- Stefanik, M.; Valdes, J.J.; Ezebuo, F.C.; Haviernik, J.; Uzochukwu, I.C.; Fojtikova, M.; Salat, J.; Eyer, L.; Ruzek, D. FDA-Approved Drugs Efavirenz, Tipranavir, and Dasabuvir Inhibit Replication of Multiple Flaviviruses in Vero Cells. Microorganisms 2020, 8, 599. [Google Scholar] [CrossRef] [PubMed]
- Kamiyama, N.; Soma, R.; Hidano, S.; Watanabe, K.; Umekita, H.; Fukuda, C.; Noguchi, K.; Gendo, Y.; Ozaki, T.; Sonoda, A.; et al. Ribavirin inhibits Zika virus (ZIKV) replication in vitro and suppresses viremia in ZIKV-infected STAT1-deficient mice. Antivir. Res. 2017, 146, 1–11. [Google Scholar] [CrossRef]
- Wagstaff, K.M.; Sivakumaran, H.; Heaton, S.M.; Harrich, D.; Jans, D.A. Ivermectin is a specific inhibitor of importin alpha/beta-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. Biochem. J. 2012, 443, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Suputtamongkol, Y.; Avirutnan, P.; Mairiang, D.; Angkasekwinai, N.; Niwattayakul, K.; Yamasmith, E.; Saleh-Arong, F.A.; Songjaeng, A.; Prommool, T.; Tangthawornchaikul, N.; et al. Ivermectin Accelerates Circulating Nonstructural Protein 1 (NS1) Clearance in Adult Dengue Patients: A Combined Phase 2/3 Randomized Double-blinded Placebo Controlled Trial. Clin. Infect. Dis. 2021, 72, e586–e593. [Google Scholar] [CrossRef] [PubMed]
- Julander, J.G.; Furuta, Y.; Shafer, K.; Sidwell, R.W. Activity of T-1106 in a hamster model of yellow Fever virus infection. Antimicrob. Agents Chemother. 2007, 51, 1962–1966. [Google Scholar] [CrossRef] [PubMed]
- Khandelwal, N.; Chander, Y.; Rawat, K.D.; Riyesh, T.; Nishanth, C.; Sharma, S.; Jindal, N.; Tripathi, B.N.; Barua, S.; Kumar, N. Emetine inhibits replication of RNA and DNA viruses without generating drug-resistant virus variants. Antivir. Res. 2017, 144, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Lao, Z.; Xu, J.; Li, Z.; Long, H.; Li, D.; Lin, L.; Liu, X.; Yu, L.; Liu, W.; et al. Antiviral activity of lycorine against Zika virus in vivo and in vitro. Virology 2020, 546, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Xu, M.; Lee, E.M.; Gorshkov, K.; Shiryaev, S.A.; He, S.; Sun, W.; Cheng, Y.S.; Hu, X.; Tharappel, A.M.; et al. Emetine inhibits Zika and Ebola virus infections through two molecular mechanisms: Inhibiting viral replication and decreasing viral entry. Cell Discov. 2018, 4, 31. [Google Scholar] [CrossRef]
- Pattnaik, A.; Palermo, N.; Sahoo, B.R.; Yuan, Z.; Hu, D.; Annamalai, A.S.; Vu, H.L.X.; Correas, I.; Prathipati, P.K.; Destache, C.J.; et al. Discovery of a non-nucleoside RNA polymerase inhibitor for blocking Zika virus replication through in silico screening. Antivir. Res. 2018, 151, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.P.; Noble, C.G.; Shi, P.Y. The dengue virus NS5 protein as a target for drug discovery. Antivir. Res. 2015, 119, 57–67. [Google Scholar] [CrossRef]
- Chung, K.Y.; Dong, H.; Chao, A.T.; Shi, P.Y.; Lescar, J.; Lim, S.P. Higher catalytic efficiency of N-7-methylation is responsible for processive N-7 and 2’-O methyltransferase activity in dengue virus. Virology 2010, 402, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Noble, C.G.; Li, S.H.; Dong, H.; Chew, S.H.; Shi, P.Y. Crystal structure of dengue virus methyltransferase without S-adenosyl-L-methionine. Antivir. Res. 2014, 111, 78–81. [Google Scholar] [CrossRef]
- Thames, J.E.; Waters, C.D., 3rd; Valle, C.; Bassetto, M.; Aouadi, W.; Martin, B.; Selisko, B.; Falat, A.; Coutard, B.; Brancale, A.; et al. Synthesis and biological evaluation of novel flexible nucleoside analogues that inhibit flavivirus replication in vitro. Bioorg. Med. Chem. 2020, 28, 115713. [Google Scholar] [CrossRef] [PubMed]
- Yates, M.K.; Chatterjee, P.; Flint, M.; Arefeayne, Y.; Makuc, D.; Plavec, J.; Spiropoulou, C.F.; Seley-Radtke, K.L. Probing the Effects of Pyrimidine Functional Group Switches on Acyclic Fleximer Analogues for Antiviral Activity. Molecules 2019, 24, 3184. [Google Scholar] [CrossRef] [PubMed]
- Ci, Y.; Liu, Z.Y.; Zhang, N.N.; Niu, Y.; Yang, Y.; Xu, C.; Yang, W.; Qin, C.F.; Shi, L. Zika NS1-induced ER remodeling is essential for viral replication. J. Cell Biol. 2020, 219, e201903062. [Google Scholar] [CrossRef]
- Avirutnan, P.; Fuchs, A.; Hauhart, R.E.; Somnuke, P.; Youn, S.; Diamond, M.S.; Atkinson, J.P. Antagonism of the complement component C4 by flavivirus nonstructural protein NS1. J. Exp. Med. 2010, 207, 793–806. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, M.; Sharma, N.; Singh, S.K. Flavivirus NS1: A multifaceted enigmatic viral protein. Virol. J. 2016, 13, 131. [Google Scholar] [CrossRef]
- Goldman, A.B.; Abrahams, T.G. Case report 356: Multiple findings of renal osteodystrophy reflected in the vertebral bodies and apophyseal joints of the cervical spine. Skeletal Radiol. 1986, 15, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Rathore, A.P.; Paradkar, P.N.; Watanabe, S.; Tan, K.H.; Sung, C.; Connolly, J.E.; Low, J.; Ooi, E.E.; Vasudevan, S.G. Celgosivir treatment misfolds dengue virus NS1 protein, induces cellular pro-survival genes and protects against lethal challenge mouse model. Antivir. Res. 2011, 92, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Barnard, T.R.; Abram, Q.H.; Lin, Q.F.; Wang, A.B.; Sagan, S.M. Molecular Determinants of Flavivirus Virion Assembly. Trends Biochem. Sci. 2021, 46, 378–390. [Google Scholar] [CrossRef]
- Albulescu, I.C.; Kovacikova, K.; Tas, A.; Snijder, E.J.; van Hemert, M.J. Suramin inhibits Zika virus replication by interfering with virus attachment and release of infectious particles. Antivir. Res. 2017, 143, 230–236. [Google Scholar] [CrossRef]
- Klaitong, P.; Smith, D.R. Roles of Non-Structural Protein 4A in Flavivirus Infection. Viruses 2021, 13, 2077. [Google Scholar] [CrossRef]
- Miller, S.; Kastner, S.; Krijnse-Locker, J.; Buhler, S.; Bartenschlager, R. The non-structural protein 4A of dengue virus is an integral membrane protein inducing membrane alterations in a 2K-regulated manner. J. Biol. Chem. 2007, 282, 8873–8882. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xie, X.; Shi, P.Y. Flavivirus NS4B protein: Structure, function, and antiviral discovery. Antiviral Res. 2022, 207, 105423. [Google Scholar] [CrossRef]
- Chatel-Chaix, L.; Fischl, W.; Scaturro, P.; Cortese, M.; Kallis, S.; Bartenschlager, M.; Fischer, B.; Bartenschlager, R. A Combined Genetic-Proteomic Approach Identifies Residues within Dengue Virus NS4B Critical for Interaction with NS3 and Viral Replication. J. Virol. 2015, 89, 7170–7186. [Google Scholar] [CrossRef] [PubMed]
- Goethals, O.; Kaptein, S.J.F.; Kesteleyn, B.; Bonfanti, J.F.; Van Wesenbeeck, L.; Bardiot, D.; Verschoor, E.J.; Verstrepen, B.E.; Fagrouch, Z.; Putnak, J.R.; et al. Blocking NS3-NS4B interaction inhibits dengue virus in non-human primates. Nature 2023, 615, 678–686. [Google Scholar] [CrossRef]
- Ackaert, O.; Vanhoutte, F.; Verpoorten, N.; Buelens, A.; Lachau-Durand, S.; Lammens, L.; Hoetelmans, R.; Van Loock, M.; Herrera-Taracena, G. Safety, Tolerability, and Pharmacokinetics of JNJ-1802, a Pan-serotype Dengue Direct Antiviral Small Molecule, in a Phase 1, Double-Blind, Randomized, Dose-Escalation Study in Healthy Volunteers. Clin. Infect. Dis. 2023, 77, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Ray, D.; Zhao, Y.; Dong, H.; Ren, S.; Li, Z.; Guo, Y.; Bernard, K.A.; Shi, P.Y.; Li, H. Structure and function of flavivirus NS5 methyltransferase. J. Virol. 2007, 81, 3891–3903. [Google Scholar] [CrossRef]
- Geraghty, R.J.; Aliota, M.T.; Bonnac, L.F. Broad-Spectrum Antiviral Strategies and Nucleoside Analogues. Viruses 2021, 13, 667. [Google Scholar] [CrossRef] [PubMed]
- Abdullah Al Awadh, A. Nucleotide and nucleoside-based drugs: Past, present, and future. Saudi J. Biol. Sci. 2022, 29, 103481. [Google Scholar] [CrossRef] [PubMed]
- Eyer, L.; Nencka, R.; de Clercq, E.; Seley-Radtke, K.; Ruzek, D. Nucleoside analogs as a rich source of antiviral agents active against arthropod-borne flaviviruses. Antivir. Chem. Chemother. 2018, 26, 2040206618761299. [Google Scholar] [CrossRef] [PubMed]
- Kataev, V.E.; Garifullin, B.F. Antiviral nucleoside analogs. Chem. Heterocycl. Compd. 2021, 57, 326–341. [Google Scholar] [CrossRef] [PubMed]
- Stedman, C. Sofosbuvir, a NS5B polymerase inhibitor in the treatment of hepatitis C: A review of its clinical potential. Therap. Adv. Gastroenterol. 2014, 7, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, D.M.; Castillo, E.; Duarte, L.F.; Arriagada, J.; Corrales, N.; Farias, M.A.; Henriquez, A.; Agurto-Munoz, C.; Gonzalez, P.A. Current Antivirals and Novel Botanical Molecules Interfering With Herpes Simplex Virus Infection. Front. Microbiol. 2020, 11, 139. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.; Chen, Y.L.; Schul, W.; Wang, Q.Y.; Gu, F.; Duraiswamy, J.; Kondreddi, R.R.; Niyomrattanakit, P.; Lakshminarayana, S.B.; Goh, A.; et al. An adenosine nucleoside inhibitor of dengue virus. Proc. Natl. Acad. Sci. USA 2009, 106, 20435–20439. [Google Scholar] [CrossRef] [PubMed]
- McMahon, J.H.; Lau, J.S.Y.; Coldham, A.; Roney, J.; Hagenauer, M.; Price, S.; Bryant, M.; Garlick, J.; Paterson, A.; Lee, S.J.; et al. Favipiravir in early symptomatic COVID-19, a randomised placebo-controlled trial. eClinicalMedicine 2022, 54, 101703. [Google Scholar] [CrossRef] [PubMed]
- Guedj, J.; Piorkowski, G.; Jacquot, F.; Madelain, V.; Nguyen, T.H.T.; Rodallec, A.; Gunther, S.; Carbonnelle, C.; Mentre, F.; Raoul, H.; et al. Antiviral efficacy of favipiravir against Ebola virus: A translational study in cynomolgus macaques. PLoS Med. 2018, 15, e1002535. [Google Scholar] [CrossRef] [PubMed]
- Franco, E.J.; Cella, E.; Tao, X.; Hanrahan, K.C.; Azarian, T.; Brown, A.N. Favipiravir Suppresses Zika Virus (ZIKV) through Activity as a Mutagen. Microorganisms 2023, 11, 1342. [Google Scholar] [CrossRef] [PubMed]
- Karuna, R.; Yokokawa, F.; Wang, K.; Zhang, J.; Xu, H.; Wang, G.; Ding, M.; Chan, W.L.; Abdul Ghafar, N.; Leonardi, A.; et al. A Cyclic Phosphoramidate Prodrug of 2’-Deoxy-2’-Fluoro-2’-C-Methylguanosine for the Treatment of Dengue Virus Infection. Antimicrob. Agents Chemother. 2020, 64, e00654-20. [Google Scholar] [CrossRef]
- Toniutto, P.; Fabris, C.; Bitetto, D.; Fumolo, E.; Fornasiere, E.; Pirisi, M. R-1626, a specific oral NS5B polymerase inhibitor of hepatitis C virus. IDrugs 2008, 11, 738–749. [Google Scholar] [PubMed]
- Nguyen, N.M.; Tran, C.N.; Phung, L.K.; Duong, K.T.; Huynh Hle, A.; Farrar, J.; Nguyen, Q.T.; Tran, H.T.; Nguyen, C.V.; Merson, L.; et al. A randomized, double-blind placebo controlled trial of balapiravir, a polymerase inhibitor, in adult dengue patients. J. Infect. Dis. 2013, 207, 1442–1450. [Google Scholar] [CrossRef]
- Lee, M.F.; Wu, Y.S.; Poh, C.L. Molecular Mechanisms of Antiviral Agents against Dengue Virus. Viruses 2023, 15, 705. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.J.; Sharma, S.D.; Feng, J.Y.; Ray, A.S.; Smidansky, E.D.; Kireeva, M.L.; Cho, A.; Perry, J.; Vela, J.E.; Park, Y.; et al. Sensitivity of mitochondrial transcription and resistance of RNA polymerase II dependent nuclear transcription to antiviral ribonucleosides. PLoS Pathog. 2012, 8, e1003030. [Google Scholar] [CrossRef]
- Lim, S.P.; Wang, Q.Y.; Noble, C.G.; Chen, Y.L.; Dong, H.; Zou, B.; Yokokawa, F.; Nilar, S.; Smith, P.; Beer, D.; et al. Ten years of dengue drug discovery: Progress and prospects. Antivir. Res. 2013, 100, 500–519. [Google Scholar] [CrossRef]
- Dragoni, F.; Boccuto, A.; Picarazzi, F.; Giannini, A.; Giammarino, F.; Saladini, F.; Mori, M.; Mastrangelo, E.; Zazzi, M.; Vicenti, I. Evaluation of sofosbuvir activity and resistance profile against West Nile virus in vitro. Antivir. Res. 2020, 175, 104708. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.T.; Colby-Germinario, S.P.; Hassounah, S.A.; Fogarty, C.; Osman, N.; Palanisamy, N.; Han, Y.; Oliveira, M.; Quan, Y.; Wainberg, M.A. Evaluation of Sofosbuvir (beta-D-2’-deoxy-2’-alpha-fluoro-2’-beta-C-methyluridine) as an inhibitor of Dengue virus replication. Sci. Rep. 2017, 7, 6345. [Google Scholar] [CrossRef]
- Appleby, T.C.; Perry, J.K.; Murakami, E.; Barauskas, O.; Feng, J.; Cho, A.; Fox, D., 3rd; Wetmore, D.R.; McGrath, M.E.; Ray, A.S.; et al. Viral replication. Structural basis for RNA replication by the hepatitis C virus polymerase. Science 2015, 347, 771–775. [Google Scholar] [CrossRef] [PubMed]
- Rattanaburee, T.; Junking, M.; Panya, A.; Sawasdee, N.; Songprakhon, P.; Suttitheptumrong, A.; Limjindaporn, T.; Haegeman, G.; Yenchitsomanus, P.T. Inhibition of dengue virus production and cytokine/chemokine expression by ribavirin and compound A. Antivir. Res. 2015, 124, 83–92. [Google Scholar] [CrossRef]
- Noble, C.G.; Lim, S.P.; Chen, Y.L.; Liew, C.W.; Yap, L.; Lescar, J.; Shi, P.Y. Conformational flexibility of the Dengue virus RNA-dependent RNA polymerase revealed by a complex with an inhibitor. J. Virol. 2013, 87, 5291–5295. [Google Scholar] [CrossRef] [PubMed]
- Niyomrattanakit, P.; Chen, Y.L.; Dong, H.; Yin, Z.; Qing, M.; Glickman, J.F.; Lin, K.; Mueller, D.; Voshol, H.; Lim, J.Y.; et al. Inhibition of dengue virus polymerase by blocking of the RNA tunnel. J. Virol. 2010, 84, 5678–5686. [Google Scholar] [CrossRef] [PubMed]
- Pryor, M.J.; Rawlinson, S.M.; Butcher, R.E.; Barton, C.L.; Waterhouse, T.A.; Vasudevan, S.G.; Bardin, P.G.; Wright, P.J.; Jans, D.A.; Davidson, A.D. Nuclear localization of dengue virus nonstructural protein 5 through its importin alpha/beta-recognized nuclear localization sequences is integral to viral infection. Traffic 2007, 8, 795–807. [Google Scholar] [CrossRef] [PubMed]
- Perera, R.; Riley, C.; Isaac, G.; Hopf-Jannasch, A.S.; Moore, R.J.; Weitz, K.W.; Pasa-Tolic, L.; Metz, T.O.; Adamec, J.; Kuhn, R.J. Dengue virus infection perturbs lipid homeostasis in infected mosquito cells. PLoS Pathog. 2012, 8, e1002584. [Google Scholar] [CrossRef]
- Heaton, N.S.; Randall, G. Dengue virus-induced autophagy regulates lipid metabolism. Cell Host Microbe 2010, 8, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Samsa, M.M.; Mondotte, J.A.; Iglesias, N.G.; Assuncao-Miranda, I.; Barbosa-Lima, G.; Da Poian, A.T.; Bozza, P.T.; Gamarnik, A.V. Dengue virus capsid protein usurps lipid droplets for viral particle formation. PLoS Pathog. 2009, 5, e1000632. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, C.M.R.; Sevvana, M.; Kuhn, R.J. Structure-guided paradigm shifts in flavivirus assembly and maturation mechanisms. Adv. Virus Res. 2020, 108, 33–83. [Google Scholar] [CrossRef]
- Chambers, T.J.; Hahn, C.S.; Galler, R.; Rice, C.M. Flavivirus genome organization, expression, and replication. Annu. Rev. Microbiol. 1990, 44, 649–688. [Google Scholar] [CrossRef] [PubMed]
- Crabtree, M.B.; Kinney, R.M.; Miller, B.R. Deglycosylation of the NS1 protein of dengue 2 virus, strain 16681: Construction and characterization of mutant viruses. Arch. Virol. 2005, 150, 771–786. [Google Scholar] [CrossRef] [PubMed]
- Helenius, A.; Aebi, M. Intracellular functions of N-linked glycans. Science 2001, 291, 2364–2369. [Google Scholar] [CrossRef] [PubMed]
- Whitby, K.; Pierson, T.C.; Geiss, B.; Lane, K.; Engle, M.; Zhou, Y.; Doms, R.W.; Diamond, M.S. Castanospermine, a potent inhibitor of dengue virus infection in vitro and in vivo. J. Virol. 2005, 79, 8698–8706. [Google Scholar] [CrossRef]
- Watanabe, S.; Chan, K.W.; Dow, G.; Ooi, E.E.; Low, J.G.; Vasudevan, S.G. Optimizing celgosivir therapy in mouse models of dengue virus infection of serotypes 1 and 2: The search for a window for potential therapeutic efficacy. Antivir. Res. 2016, 127, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Low, J.G.; Sung, C.; Wijaya, L.; Wei, Y.; Rathore, A.P.S.; Watanabe, S.; Tan, B.H.; Toh, L.; Chua, L.T.; Hou, Y.; et al. Efficacy and safety of celgosivir in patients with dengue fever (CELADEN): A phase 1b, randomised, double-blind, placebo-controlled, proof-of-concept trial. Lancet Infect. Dis. 2014, 14, 706–715. [Google Scholar] [CrossRef]
- Callahan, M.; Treston, A.M.; Lin, G.; Smith, M.; Kaufman, B.; Khaliq, M.; Evans DeWald, L.; Spurgers, K.; Warfield, K.L.; Lowe, P.; et al. Randomized single oral dose phase 1 study of safety, tolerability, and pharmacokinetics of Iminosugar UV-4 Hydrochloride (UV-4B) in healthy subjects. PLoS Negl. Trop. Dis. 2022, 16, e0010636. [Google Scholar] [CrossRef]
- Chang, J.; Schul, W.; Butters, T.D.; Yip, A.; Liu, B.; Goh, A.; Lakshminarayana, S.B.; Alonzi, D.; Reinkensmeier, G.; Pan, X.; et al. Combination of alpha-glucosidase inhibitor and ribavirin for the treatment of dengue virus infection in vitro and in vivo. Antivir. Res. 2011, 89, 26–34. [Google Scholar] [CrossRef]
- Evans DeWald, L.; Starr, C.; Butters, T.; Treston, A.; Warfield, K.L. Iminosugars: A host-targeted approach to combat Flaviviridae infections. Antivir. Res. 2020, 184, 104881. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Plummer, E.; Alonzi, D.S.; Wolfe, G.W.; Sampath, A.; Nguyen, T.; Butters, T.D.; Enterlein, S.G.; Stavale, E.J.; Shresta, S.; et al. A Novel Iminosugar UV-12 with Activity against the Diverse Viruses Influenza and Dengue (Novel Iminosugar Antiviral for Influenza and Dengue). Viruses 2015, 7, 2404–2427. [Google Scholar] [CrossRef]
- Merino-Ramos, T.; Vazquez-Calvo, A.; Casas, J.; Sobrino, F.; Saiz, J.C.; Martin-Acebes, M.A. Modification of the Host Cell Lipid Metabolism Induced by Hypolipidemic Drugs Targeting the Acetyl Coenzyme A Carboxylase Impairs West Nile Virus Replication. Antimicrob. Agents Chemother. 2016, 60, 307–315. [Google Scholar] [CrossRef]
- Anwar, A.; Hosoya, T.; Leong, K.M.; Onogi, H.; Okuno, Y.; Hiramatsu, T.; Koyama, H.; Suzuki, M.; Hagiwara, M.; Garcia-Blanco, M.A. The kinase inhibitor SFV785 dislocates dengue virus envelope protein from the replication complex and blocks virus assembly. PLoS ONE 2011, 6, e23246. [Google Scholar] [CrossRef] [PubMed]
- Blazquez, A.B.; Saiz, J.C. Potential for Protein Kinase Pharmacological Regulation in Flaviviridae Infections. Int. J. Mol. Sci. 2020, 21, 9524. [Google Scholar] [CrossRef]
- Martinez-Gutierrez, M.; Correa-Londono, L.A.; Castellanos, J.E.; Gallego-Gomez, J.C.; Osorio, J.E. Lovastatin delays infection and increases survival rates in AG129 mice infected with dengue virus serotype 2. PLoS ONE 2014, 9, e87412. [Google Scholar] [CrossRef] [PubMed]
- Whitehorn, J.; Nguyen, C.V.V.; Khanh, L.P.; Kien, D.T.H.; Quyen, N.T.H.; Tran, N.T.T.; Hang, N.T.; Truong, N.T.; Hue Tai, L.T.; Cam Huong, N.T.; et al. Lovastatin for the Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled Trial. Clin. Infect. Dis. 2016, 62, 468–476. [Google Scholar] [CrossRef]
- Sung, C.; Wei, Y.; Watanabe, S.; Lee, H.S.; Khoo, Y.M.; Fan, L.; Rathore, A.P.; Chan, K.W.; Choy, M.M.; Kamaraj, U.S.; et al. Extended Evaluation of Virological, Immunological and Pharmacokinetic Endpoints of CELADEN: A Randomized, Placebo-Controlled Trial of Celgosivir in Dengue Fever Patients. PLoS Negl. Trop. Dis. 2016, 10, e0004851. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, C.; Lebreton, A.; Young Ng, C.; Lim, J.Y.; Liu, W.; Vasudevan, S.; Labow, M.; Gu, F.; Gaither, L.A. Cholesterol biosynthesis modulation regulates dengue viral replication. Virology 2009, 389, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Osuna-Ramos, J.F.; Farfan-Morales, C.N.; Cordero-Rivera, C.D.; De Jesus-Gonzalez, L.A.; Reyes-Ruiz, J.M.; Hurtado-Monzon, A.M.; Palacios-Rapalo, S.N.; Jimenez-Camacho, R.; Meraz-Rios, M.A.; Del Angel, R.M. Cholesterol-Lowering Drugs as Potential Antivirals: A Repurposing Approach against Flavivirus Infections. Viruses 2023, 15, 1465. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.L.; Sheridan, K.; Parkins, C.J.; Frueh, L.; Jemison, A.L.; Strode, K.; Dow, G.; Nilsen, A.; Hirsch, A.J. Characterization and structure-activity relationship analysis of a class of antiviral compounds that directly bind dengue virus capsid protein and are incorporated into virions. Antivir. Res. 2018, 155, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Xia, H.; Xie, X.; Zou, J.; Noble, C.G.; Russell, W.K.; Holthauzen, L.M.F.; Choi, K.H.; White, M.A.; Shi, P.Y. A cocrystal structure of dengue capsid protein in complex of inhibitor. Proc. Natl. Acad. Sci. USA 2020, 117, 17992–18001. [Google Scholar] [CrossRef] [PubMed]
- Byrd, C.M.; Dai, D.; Grosenbach, D.W.; Berhanu, A.; Jones, K.F.; Cardwell, K.B.; Schneider, C.; Wineinger, K.A.; Page, J.M.; Harver, C.; et al. A novel inhibitor of dengue virus replication that targets the capsid protein. Antimicrob. Agents Chemother. 2013, 57, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.H.; Syu, W.J.; Hu, S.T. Identification of the homotypic interaction domain of the core protein of dengue virus type 2. J. Gen. Virol. 2004, 85, 2307–2314. [Google Scholar] [CrossRef]
- Byk, L.A.; Gamarnik, A.V. Properties and Functions of the Dengue Virus Capsid Protein. Annu. Rev. Virol. 2016, 3, 263–281. [Google Scholar] [CrossRef]
- Sotcheff, S.; Routh, A. Understanding Flavivirus Capsid Protein Functions: The Tip of the Iceberg. Pathogens 2020, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Boonyasuppayakorn, S.; Reichert, E.D.; Manzano, M.; Nagarajan, K.; Padmanabhan, R. Amodiaquine, an antimalarial drug, inhibits dengue virus type 2 replication and infectivity. Antivir. Res. 2014, 106, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Cheung, Y.Y.; Chen, K.C.; Chen, H.; Seng, E.K.; Chu, J.J. Antiviral activity of lanatoside C against dengue virus infection. Antivir. Res. 2014, 111, 93–99. [Google Scholar] [CrossRef]
- Kato, F.; Ishida, Y.; Oishi, S.; Fujii, N.; Watanabe, S.; Vasudevan, S.G.; Tajima, S.; Takasaki, T.; Suzuki, Y.; Ichiyama, K.; et al. Novel antiviral activity of bromocriptine against dengue virus replication. Antivir. Res. 2016, 131, 141–147. [Google Scholar] [CrossRef]
- Zakaria, M.K.; Carletti, T.; Marcello, A. Cellular Targets for the Treatment of Flavivirus Infections. Front. Cell. Infect. Microbiol. 2018, 8, 398. [Google Scholar] [CrossRef]
- Scroggs, S.L.P.; Andrade, C.C.; Chinnasamy, R.; Azar, S.R.; Schirtzinger, E.E.; Garcia, E.I.; Arterburn, J.B.; Hanley, K.A.; Rossi, S.L. Old Drugs with New Tricks: Efficacy of Fluoroquinolones to Suppress Replication of Flaviviruses. Viruses 2020, 12, 1022. [Google Scholar] [CrossRef] [PubMed]
- Haviernik, J.; Stefanik, M.; Fojtikova, M.; Kali, S.; Tordo, N.; Rudolf, I.; Hubalek, Z.; Eyer, L.; Ruzek, D. Arbidol (Umifenovir): A Broad-Spectrum Antiviral Drug That Inhibits Medically Important Arthropod-Borne Flaviviruses. Viruses 2018, 10, 184. [Google Scholar] [CrossRef]
- Puschnik, A.S.; Marceau, C.D.; Ooi, Y.S.; Majzoub, K.; Rinis, N.; Contessa, J.N.; Carette, J.E. A Small-Molecule Oligosaccharyltransferase Inhibitor with Pan-flaviviral Activity. Cell Rep. 2017, 21, 3032–3039. [Google Scholar] [CrossRef] [PubMed]
- Othman, M.A.; Abou-Donia, M.B. Pharmacokinetic profile of (+/−)-gossypol in male Sprague-Dawley rats following single intravenous and oral and subchronic oral administration. Proc. Soc. Exp. Biol. Med. 1988, 188, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Eyre, N.S.; Kirby, E.N.; Anfiteatro, D.R.; Bracho, G.; Russo, A.G.; White, P.A.; Aloia, A.L.; Beard, M.R. Identification of Estrogen Receptor Modulators as Inhibitors of Flavivirus Infection. Antimicrob. Agents Chemother. 2020, 64, e00289. [Google Scholar] [CrossRef]
- Quintana, V.M.; Selisko, B.; Brunetti, J.E.; Eydoux, C.; Guillemot, J.C.; Canard, B.; Damonte, E.B.; Julander, J.G.; Castilla, V. Antiviral activity of the natural alkaloid anisomycin against dengue and Zika viruses. Antivir. Res 2020, 176, 104749. [Google Scholar] [CrossRef] [PubMed]
- Carocci, M.; Hinshaw, S.M.; Rodgers, M.A.; Villareal, V.A.; Burri, D.J.; Pilankatta, R.; Maharaj, N.P.; Gack, M.U.; Stavale, E.J.; Warfield, K.L.; et al. The bioactive lipid 4-hydroxyphenyl retinamide inhibits flavivirus replication. Antimicrob. Agents Chemother. 2015, 59, 85–95. [Google Scholar] [CrossRef]
- Zhou, T.; Tan, L.; Cederquist, G.Y.; Fan, Y.; Hartley, B.J.; Mukherjee, S.; Tomishima, M.; Brennand, K.J.; Zhang, Q.; Schwartz, R.E.; et al. High-Content Screening in hPSC-Neural Progenitors Identifies Drug Candidates that Inhibit Zika Virus Infection in Fetal-like Organoids and Adult Brain. Cell Stem Cell 2017, 21, 274–283.e5. [Google Scholar] [CrossRef] [PubMed]
- Heiss, B.L.; Maximova, O.A.; Pletnev, A.G. Insertion of microRNA targets into the flavivirus genome alters its highly neurovirulent phenotype. J. Virol. 2011, 85, 1464–1472. [Google Scholar] [CrossRef]
- Heiss, B.L.; Maximova, O.A.; Thach, D.C.; Speicher, J.M.; Pletnev, A.G. MicroRNA targeting of neurotropic flavivirus: Effective control of virus escape and reversion to neurovirulent phenotype. J. Virol. 2012, 86, 5647–5659. [Google Scholar] [CrossRef]
- Yen, L.C.; Lin, Y.L.; Sung, H.H.; Liao, J.T.; Tsao, C.H.; Su, C.M.; Lin, C.K.; Liao, C.L. Neurovirulent flavivirus can be attenuated in mice by incorporation of neuron-specific microRNA recognition elements into viral genome. Vaccine 2013, 31, 5915–5922. [Google Scholar] [CrossRef]
- Sharma, H.; Tripathi, A.; Kumari, B.; Vrati, S.; Banerjee, A. Artificial MicroRNA-Mediated Inhibition of Japanese Encephalitis Virus Replication in Neuronal Cells. Nucleic Acid Ther. 2018, 28, 357–365. [Google Scholar] [CrossRef]
- Karothia, D.; Kumar Dash, P.; Parida, M.; Bhagyawant, S.S.; Kumar, J.S. Vector derived artificial miRNA mediated inhibition of West Nile virus replication and protein expression. Gene 2020, 729, 144300. [Google Scholar] [CrossRef] [PubMed]
- Xie, P.W.; Xie, Y.; Zhang, X.J.; Huang, H.; He, L.N.; Wang, X.J.; Wang, S.Q. Inhibition of Dengue virus 2 replication by artificial micrornas targeting the conserved regions. Nucleic Acid Ther. 2013, 23, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Shen, T.; Liu, K.; Miao, D.; Cao, R.; Chen, P. Effective inhibition of Japanese encephalitis virus replication by shRNAs targeting various viral genes in vitro and in vivo. Virology 2014, 454–455, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Xue, Y.; Wang, B.; Du, J.; Jin, Q. Broad-spectrum antiviral activity of RNA interference against four genotypes of Japanese encephalitis virus based on single microRNA polycistrons. PLoS ONE 2011, 6, e26304. [Google Scholar] [CrossRef]
- Brostoff, T.; Pesavento, P.A.; Barker, C.M.; Kenney, J.L.; Dietrich, E.A.; Duggal, N.K.; Bosco-Lauth, A.M.; Brault, A.C. MicroRNA reduction of neuronal West Nile virus replication attenuates and affords a protective immune response in mice. Vaccine 2016, 34, 5366–5375. [Google Scholar] [CrossRef]
- Natekar, J.P.; Rothan, H.A.; Arora, K.; Strate, P.G.; Kumar, M. Cellular microRNA-155 Regulates Virus-Induced Inflammatory Response and Protects against Lethal West Nile Virus Infection. Viruses 2019, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Pacca, C.C.; Severino, A.A.; Mondini, A.; Rahal, P.; D’Avila, S.G.; Cordeiro, J.A.; Nogueira, M.C.; Bronzoni, R.V.; Nogueira, M.L. RNA interference inhibits yellow fever virus replication in vitro and in vivo. Virus Genes 2009, 38, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Fu, Y.; Cheng, M.; Ma, W.; Zheng, N.; Wang, Y.; Wu, Z. sEVs(RVG) selectively delivers antiviral siRNA to fetus brain, inhibits ZIKV infection and mitigates ZIKV-induced microcephaly in mouse model. Mol. Ther. 2022, 30, 2078–2091. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Kordbacheh, R.; Sin, J. Extracellular Vesicles: A Novel Mode of Viral Propagation Exploited by Enveloped and Non-Enveloped Viruses. Microorganisms 2024, 12, 274. [Google Scholar] [CrossRef] [PubMed]
- El Safadi, D.; Mokhtari, A.; Krejbich, M.; Lagrave, A.; Hirigoyen, U.; Lebeau, G.; Viranaicken, W.; Krejbich-Trotot, P. Exosome-Mediated Antigen Delivery: Unveiling Novel Strategies in Viral Infection Control and Vaccine Design. Vaccines 2024, 12, 280. [Google Scholar] [CrossRef]
- Dai, Z.; Cai, R.; Zeng, H.; Zhu, H.; Dou, Y.; Sun, S. Exosome may be the next generation of promising cell-free vaccines. Hum. Vaccin. Immunother. 2024, 20, 2345940. [Google Scholar] [CrossRef] [PubMed]
- Latanova, A.; Karpov, V.; Starodubova, E. Extracellular Vesicles in Flaviviridae Pathogenesis: Their Roles in Viral Transmission, Immune Evasion, and Inflammation. Int. J. Mol. Sci. 2024, 25, 2144. [Google Scholar] [CrossRef]
- Ishikawa, T.; Narita, K.; Matsuyama, K.; Masuda, M. Dissemination of the Flavivirus Subgenomic Replicon Genome and Viral Proteins by Extracellular Vesicles. Viruses 2024, 16, 524. [Google Scholar] [CrossRef]
- Martins, S.T.; Kuczera, D.; Lotvall, J.; Bordignon, J.; Alves, L.R. Characterization of Dendritic Cell-Derived Extracellular Vesicles During Dengue Virus Infection. Front. Microbiol. 2018, 9, 1792. [Google Scholar] [CrossRef] [PubMed]
- Slonchak, A.; Clarke, B.; Mackenzie, J.; Amarilla, A.A.; Setoh, Y.X.; Khromykh, A.A. West Nile virus infection and interferon alpha treatment alter the spectrum and the levels of coding and noncoding host RNAs secreted in extracellular vesicles. BMC Genom. 2019, 20, 474. [Google Scholar] [CrossRef] [PubMed]
- Block, L.N.; Schmidt, J.K.; Keuler, N.S.; McKeon, M.C.; Bowman, B.D.; Wiepz, G.J.; Golos, T.G. Zika virus impacts extracellular vesicle composition and cellular gene expression in macaque early gestation trophoblasts. Sci. Rep. 2022, 12, 7348. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Li, H.; Ye, Z.; Xu, Q.; Fu, Q.; Sun, W.; Qi, W.; Yue, J. Berbamine inhibits Japanese encephalitis virus (JEV) infection by compromising TPRMLs-mediated endolysosomal trafficking of low-density lipoprotein receptor (LDLR). Emerg. Microbes Infect. 2021, 10, 1257–1271. [Google Scholar] [CrossRef]
- Conzelmann, C.; Gross, R.; Zou, M.; Kruger, F.; Gorgens, A.; Gustafsson, M.O.; El Andaloussi, S.; Munch, J.; Muller, J.A. Salivary extracellular vesicles inhibit Zika virus but not SARS-CoV-2 infection. J. Extracell. Vesicles 2020, 9, 1808281. [Google Scholar] [CrossRef]
- Li, S.; Zhu, A.; Ren, K.; Li, S.; Chen, L. DEFA1B inhibits ZIKV replication and retards cell cycle progression through interaction with ORC1. Life Sci. 2020, 263, 118564. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, M.; Xia, X.; Fu, Y.; Wang, Y.; Xu, W.; Wei, H.; Wei, L. Construction of exosome-loaded LL-37 and its protection against zika virus infection. Antivir. Res. 2024, 225, 105855. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Yuan, M.; Zhang, T.; Zheng, N.; Wu, Z. EVs Containing Host Restriction Factor IFITM3 Inhibited ZIKV Infection of Fetuses in Pregnant Mice through Trans-placenta Delivery. Mol. Ther. 2021, 29, 176–190. [Google Scholar] [CrossRef] [PubMed]
- Yenuganti, V.R.; Afroz, S.; Khan, R.A.; Bharadwaj, C.; Nabariya, D.K.; Nayak, N.; Subbiah, M.; Chintala, K.; Banerjee, S.; Reddanna, P.; et al. Milk exosomes elicit a potent anti-viral activity against dengue virus. J. Nanobiotechnology 2022, 20, 317. [Google Scholar] [CrossRef]
- Zhang, Y.; Dai, Y.; Wang, J.; Xu, Y.; Li, Z.; Lu, J.; Xu, Y.; Zhong, J.; Ding, S.W.; Li, Y. Mouse circulating extracellular vesicles contain virus-derived siRNAs active in antiviral immunity. EMBO J. 2022, 41, e109902. [Google Scholar] [CrossRef]
- Ahmed, W.; Neelakanta, G.; Sultana, H. Tetraspanins as Potential Therapeutic Candidates for Targeting Flaviviruses. Front. Immunol. 2021, 12, 630571. [Google Scholar] [CrossRef]
- Santos, P.; Almeida, F. Exosome-Based Vaccines: History, Current State, and Clinical Trials. Front. Immunol. 2021, 12, 711565. [Google Scholar] [CrossRef] [PubMed]
- Aliota, M.T.; Caine, E.A.; Walker, E.C.; Larkin, K.E.; Camacho, E.; Osorio, J.E. Characterization of Lethal Zika Virus Infection in AG129 Mice. PLoS Negl. Trop. Dis. 2016, 10, e0004682. [Google Scholar] [CrossRef] [PubMed]
- Lazear, H.M.; Govero, J.; Smith, A.M.; Platt, D.J.; Fernandez, E.; Miner, J.J.; Diamond, M.S. A Mouse Model of Zika Virus Pathogenesis. Cell Host Microbe 2016, 19, 720–730. [Google Scholar] [CrossRef] [PubMed]
- Kayesh, M.E.H.; Tsukiyama-Kohara, K. Mammalian animal models for dengue virus infection: A recent overview. Arch. Virol. 2022, 167, 31–44. [Google Scholar] [CrossRef]
- Alves Dos Santos, E.; Fink, K. Animal Models for Dengue and Zika Vaccine Development. Adv. Exp. Med. Biol. 2018, 1062, 215–239. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Banerjee, A.; Vrati, S. Development and characterization of an animal model of Japanese encephalitis virus infection in adolescent C57BL/6 mouse. Dis. Model Mech. 2021, 14, dmm.049176. [Google Scholar] [CrossRef]
- Calvert, A.E.; Dixon, K.L.; Delorey, M.J.; Blair, C.D.; Roehrig, J.T. Development of a small animal peripheral challenge model of Japanese encephalitis virus using interferon deficient AG129 mice and the SA14-14-2 vaccine virus strain. Vaccine 2014, 32, 258–264. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhu, B.; Ye, J.; Nie, Y.; Ashraf, U.; Zohaib, A.; Duan, X.; Fu, Z.F.; Song, Y.; Chen, H.; Cao, S. MicroRNA-15b Modulates Japanese Encephalitis Virus-Mediated Inflammation via Targeting RNF125. J. Immunol. 2015, 195, 2251–2262. [Google Scholar] [CrossRef] [PubMed]
- Meier, K.C.; Gardner, C.L.; Khoretonenko, M.V.; Klimstra, W.B.; Ryman, K.D. A mouse model for studying viscerotropic disease caused by yellow fever virus infection. PLoS Pathog. 2009, 5, e1000614. [Google Scholar] [CrossRef]
- Monath, T.P. Treatment of yellow fever. Antivir. Res. 2008, 78, 116–124. [Google Scholar] [CrossRef]
- Mandl, J.N.; Akondy, R.; Lawson, B.; Kozyr, N.; Staprans, S.I.; Ahmed, R.; Feinberg, M.B. Distinctive TLR7 signaling, type I IFN production, and attenuated innate and adaptive immune responses to yellow fever virus in a primate reservoir host. J. Immunol. 2011, 186, 6406–6416. [Google Scholar] [CrossRef] [PubMed]
- Lustig, S.; Olshevsky, U.; Ben-Nathan, D.; Lachmi, B.E.; Malkinson, M.; Kobiler, D.; Halevy, M. A live attenuated West Nile virus strain as a potential veterinary vaccine. Viral Immunol. 2000, 13, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Anderson, J.F.; Magnarelli, L.A.; Wong, S.J.; Koski, R.A.; Fikrig, E. Immunization of mice against West Nile virus with recombinant envelope protein. J. Immunol. 2001, 167, 5273–5277. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.Y.; Guzman, H.; Zhang, H.; Travassos da Rosa, A.P.; Tesh, R.B. West Nile virus infection in the golden hamster (Mesocricetus auratus): A model for West Nile encephalitis. Emerg. Infect. Dis. 2001, 7, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Whitehorn, J.; Yacoub, S. Global warming and arboviral infections. Clin. Med. 2019, 19, 149–152. [Google Scholar] [CrossRef] [PubMed]

| Target | Drug | Viral Specificity | Study Stage | Ref. |
|---|---|---|---|---|
| Envelope | Z2 | DENV, YFV | In vitro | [5,6] |
| ZIKV | In vivo | [5] | ||
| DN59 | DENV-2 | In vitro | [7,8] | |
| WNV | In vitro | |||
| P5 | JEV, ZIKV | In vivo | [9] | |
| DET2 and DET4 | DENV-2 | In vitro | [10,11] | |
| Dipeptide EF | DENV | In vitro | [12] | |
| JBJ-01-162-04 | DENV, JEV, WNV, ZIKV | In vitro | [13] | |
| mAb513 | DENV | In vivo | [14] | |
| 2D22 | DENV | In vivo | [14,15,16] | |
| ZIKV-Ig | ZIKV | Phase 1 clinical trial | [17] | |
| TY014 | YFV | Phase 1 clinical trial | [17] | |
| Tyzivumab | ZIKV | Phase 1 clinical trial | [17] | |
| DN59 | DENV, WNV | In vitro | [18] | |
| MGAWN1 | WNV | Clinical trial withdrawn due to low enrollment | [19] | |
| 3-110-22 (Cyanohydrazone) | DENV, JEV, WNV, ZIKV | In vitro | [20] | |
| ZKA190 and FIT-1 | ZIKV | In vivo | [21] | |
| ZIKV-117 | ZIKV | In vivo | [22] | |
| EDE1 and EDE2 | ZIKV | In vitro | [23] | |
| mAb WNV-86 | WNV | In vivo | [24] | |
| Gossypol | DENV, ZIKV | In vitro | [25] | |
| Curcumin | DENV, ZIKV | In vitro | [26,27] | |
| BP34610 | DNEV-1, 2, 3, 4, and JEV | In vitro | [28] | |
| Viral entry | Geraniin | DENV-2 | In vivo | [29,30] |
| Palmatine | WNV, DENV-2, JEV, YFV, ZIKV | In vitro | [31] | |
| Prochloroperazine (PCZ) | DENV, JEV | In vitro | [32] | |
| Daptomycin | JEV | In vitro | [33,34,35] | |
| Puerto Rico ZIKV | ||||
| Nanchangmycin | CHIKV, DENV, WNV | [34] | ||
| Erlotinib, Sunitinib | DENV | In vivo | [36] | |
| WNV, ZIKV | In vitro | |||
| 25-Hydroxylcholesterol | DENV, YFV, WNV | In vitro | [37] | |
| ZIKV | In vivo | |||
| Chloroquine | ZIKV | In vivo | [38,39] | |
| DENV | Phase 2 clinical trial failed (no viremia reduction) | [33,40] | ||
| Niclosamide | DENV, WNV, YFV, JEV | In vitro | [41] | |
| ZIKV | In vivo | |||
| DET4 and DET2 | DENV | In vitro | [10,11] | |
| EF | DENV | In vitro | [12] | |
| Ri57 | DENV, ZIKV | In vitro | [42] | |
| AC-10 | ZIKV | In vivo | [43] |
| Target | Drug | Viral Specificity | Study Stage | Ref. |
|---|---|---|---|---|
| Dopamine D2 receptor | Prochloroperazine | DENV, JEV | In vitro | [32] |
| Clathrin | Chlorpromazine | JEV, WNV | In vitro | [53] |
| AXL | Nanchangmycin | ZIKV | In vitro | [34] |
| Lipoxygenase-activating protein | MK-591 | ZIKV | In vitro | [35] |
| Receptor tyrosine kinase and epidermal growth factor tyrosine kinase | Sunitinib and erlotinib | DENV | In vivo | [36] |
| Adenosine monophosphate-activated protein kinase | PF-06409577, metformin, and AICAR | WNV, ZIKV and DENV | In vitro | [54] |
| Holesterol-25-hydroxylase | 25-hydroxylcholesterol | ZIKV | In vitro | [37] |
| Coenzyme acetyl | PF-05175157 | WNV | In vivo | [55] |
| Sphingomyelinase-2 | GW4869 | WNV and ZIKV | In vitro | [56,57] |
| Endosome acidification | Chloroquine | DENV | In vitro | [58] |
| Endosomal acidification | Niclosamide | ZIKV | In vitro | [59] |
| De novo pyrimidine biosynthesis pathway | AR-12, P12-23, and P12-34a | DENV, ZIKV, and JEV | In vitro | [60] |
| Target | Drug | Viral Specificity | Study Stage | Ref. |
|---|---|---|---|---|
| NS1 | Peptide 3, 4, 10, 11 | DENV | In vitro | [68,69] |
| Deoxycalyxin-A | ZIKV | In silico | [70] | |
| mAb AA12 | ZIKV | In vivo | [71] | |
| mAb 2B7 | DENV, WNV, ZIKV | In vitro | [72] | |
| Castanospermine and deoxynojirimycin | DENV, ZIKV | In vitro | [73] | |
| N-nonyl-Deoxynojirimycin | DENV-2, JEV | In vitro | [74] | |
| Celgosivir | DENV | Phase 1 clinical trial | [75,76] | |
| NS2A | Novobiocin | DENV, ZIKV | In vivo | [77,78] |
| NS2B–NS3 | Temoporfin | DENV, YFV, WNV, JEV | In vitro | [65] |
| ZIKV | In vivo | [65] | ||
| JMX0207 | DENV-2 | In vitro | [79] | |
| ZIKV | In vivo | [77] | ||
| Nelfinavir | DENV-2 | In vitro | [80] | |
| Compound 4 | ZIKV | In vitro | [81] | |
| Compound 14, Compound 15 | DENV | In vitro | [82] | |
| NSC135618 | DENV, ZIKV, WNV, YFV | In vitro | [83] | |
| ZP10 | ZIKV | In vitro | [84] | |
| MB21 | DENV | In vitro | [85] | |
| Aprotinin | DENV | In vitro | [85,86] | |
| WNV | In silico | |||
| Hydroxychloroquine | ZIKV | In vivo | [87,88] | |
| Methylene blue | ZIKV | In vivo | [89] | |
| DENV | In vitro | [79,90,91] | ||
| Erythrosin B | ZIKV, DENV | In vitro | ||
| Ivermectin | YFV, WNV | In vitro | [92] | |
| ZIKV | In vivo | [93] | ||
| DENV | Phase 2/3 clinical trial | [94] | ||
| Myricetin, quercetin, luteolin, isorhamnetin, apigenin, and curcumin | ZIKV | In vitro | [51] | |
| Bortezomib | ZIKV, DENV | In vitro | [95] | |
| Palmatine | DENV, JEV, WNV, ZIKV | In vitro | [31] | |
| Asunaprevir, Simeprevir | ZIKV | In vitro | [96] | |
| NS3 | ST-610 | DENV | In vivo | [97] |
| SYC-1307 | DENV, JEV, WNV, ZIKV | In vivo | [98] | |
| ML283 | DENV, WNV | In vivo | [99] | |
| Suramin | DENV, ZIKV | In vitro | [100] | |
| NS2B | NSC157058 | WNV | In silico | [101] |
| ZIKV | In vivo | |||
| NS4A | Compound B and SBI-0090799 | DENV, ZIKV | In vitro | [102] |
| NS3-NS4B | JNJ-A07 | DENV | In vivo | [103] |
| JNJ-64281802 | DENV | Phase 2 clinical trial | ||
| JNJ-1802 | DENV | Phase 1 clinical trial | [104] | |
| JEV, WNV, ZIKV | In vitro | |||
| NS4B | NITD-688 | DENV | In vivo | [105] |
| Manidipine | JEV | In vivo | [106] | |
| DENV, ZIKV, WNV | In vitro | |||
| JMX0254 | DENV, YFV | In vivo | [107,108] | |
| SBI-0090799 | ZIKV | In vitro | [109] | |
| AZD0530, dasatinib | DENV-2 | In vitro | [110,111] | |
| NS5 | Galidesivir | WNV, TBEV, ZIKV | In vivo | [112,113] |
| YFV | Phase I clinical trial | [114] | ||
| Favipiravir | WNV, YFV | In vitro | [115] | |
| ZIKV | In vivo | [116] | ||
| Balapiravir | DENV | Phase 1/2 clinical trial | [117] | |
| NITD-008 | ZIKV, TBEV, DENV | In vivo | [118,119] | |
| AT-752 | DENV, YFV | Phase II clinical trial | [120,121] | |
| WNV, ZIKV, JEV | In vitro | |||
| 7DMA | TBEV, ZIKV, WNV, DENV | In vivo | [111,122,123] | |
| Sofosbuvir | YFV | In vivo | [124] | |
| ZIKV | In vivo | [125,126] | ||
| NITD-434, NITD-640 | Pan-flavivirus | In vitro | [127] | |
| NITD-29 | DENV | In vitro | [128] | |
| Efavirenz, tipranavir, dasabuvir | WNV, ZIKV, TBEV | In vitro | [129] | |
| AR-12 | DENV | In vivo | [60] | |
| P12-23, P12-34 | DENV, ZIKV, JEV | In vitro | ||
| Ribavirin | ZIKV | In vivo | [130] | |
| Ivermectin | ZIKV | In vitro | [131] | |
| DENV | Phase 2/3 clinical trial | [132] | ||
| T-1106 | YFV | In vivo | [133] | |
| Rifapentine | YFV | In vivo | [6] | |
| Emetine | ZIKV | In vivo | [134] | |
| Lycorine | ZIKV | In vivo | [135] | |
| Dolutegravir | ZIKV | In vitro | [136] | |
| Compound TPB | ZIKV | In vivo | [137] | |
| Sinefungin | WNV, DENV | In vivo | [138,139,140] | |
| Chartaceones | ZIKV | In vitro | [52] | |
| Fleximers | DENV, ZIKV, YFV | In vitro | [141,142] |
| Target | Drug | Viral Specificity | Study Stage | Ref. |
|---|---|---|---|---|
| Assembly | Deoxynojirimycin (DNJ) | DENV | In vivo | [74] |
| Castanospermine | DENV | In vivo | [187] | |
| Celgosivir | DENV | Phase 1/2 | [188,189,199] | |
| UV-4B | DENV | Phase 1/2 | [190] | |
| UV-12 | DENV | In vivo | [191,192,193] | |
| CM-9-78 | ||||
| CM-10-18 | ||||
| PF-05175157 | WNV, DENV, ZIKV | In vivo | [55] | |
| TOFA | In vitro | [55,194] | ||
| MEDICA 16 | In vitro | |||
| SFV785 | DENV, YFV | In vitro | [195,196] | |
| Lovastatine | DENV | In vivo | [197,198,200] | |
| Atorvastatine, ezetimibe | DENV, ZIKV | In vitro | [201] | |
| Capsid | VGTI-A3 | DENV | In vitro | [194] |
| VGTI-A3-03 | In vitro | [202] | ||
| ST-148 | In vivo | [203,204] |
| Artificial/mi/si/sh RNAs | Viral Specificity | Study Stage | Ref. |
|---|---|---|---|
| amiRNA #1 and amiRNA #2 | JEV | In vitro | [223] |
| amiRNA #1 and amiRNA #2 | WNV | In vitro | [224] |
| amiRNA DENV-128 | DENV | In vitro | [225] |
| miR-124a | WNV | In vivo | [228] |
| miR-155 | WNV | In vivo | [229] |
| shRNA | YFV | In vivo | [230] |
| siRNA | ZIKV | In vivo | [231] |
| Viral Specificity | Study Stage | Ref. |
|---|---|---|
| DENV | In vitro | [237] |
| WNV | In vivo | [238] |
| ZIKV | In vitro | [239] |
| JEV | In vivo | [240] |
| ZIKV | In vivo | [241] |
| ZIKV | In vivo | [242] |
| ZIKV | In vivo | [243] |
| ZIKV | In vivo | [244] |
| ZIKV | In vitro | [241] |
| DENV | In vitro | [245] |
| ZIKV | In vivo | [246] |
| Antiviral | Target | Virus | Clinical Trial Identifier | Clinical Trial | Status | Note | Ref. |
|---|---|---|---|---|---|---|---|
| TY014 | Envelope | YFV | NCT03776786 | Phase 1 | Completed | Safe and abrogate viremia | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Safety and Tolerability of an Antibody Against Yellow Fever Virus (TY014) in Humans/ClinicalTrials.gov/NCT03776786 |
| Zika virus immune globulin (ZIKV-IG) | Envelope | ZIKV | NCT03624946 | Phase 1 | Completed | Safe and well tolerated | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Study in Healthy Volunteers Evaluating Safety and Pharmacokinetics of Zika Virus Immune Globulin (ZIKV-IG)/ClinicalTrials.gov/NCT03624946 |
| Tyzivumab | Envelope | ZIKV | NCT03443830 | Phase 1 | Completed | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Safety and Tolerability of an Antibody Against Zika Virus (Tyzivumab) in Humans/ClinicalTrials.gov/NCT03443830 |
| Intravenous immunoglobulin (IVIG) | Envelope | JEV | NCT01856205 | Phase 2 | Completed | JEV patients had a greater increase in neutralizing antibody titers | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Safety and Efficacy Study of Intravenous Immunoglobulin to Treat Japanese Encephalitis/ClinicalTrials.gov/NCT01856205 |
| Omr-IgG-am | Envelope | WNV | NCT00068055 | Phase 1/2 | Completed | Safe and well-tolerated in patients | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/IVIG—West Nile Encephalitis: Safety and Efficacy/ClinicalTrials.gov/NCT00068055 |
| MGAWN1 | Envelope | WNV | NCT00515385 | Phase 1 | Completed | Safe in healthy subjects | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/A Trial to Evaluate the Safety of a Single Intravenous Infusion of MGAWN1 in Healthy Adults/ClinicalTrials.gov/NCT00515385 |
| Carica papaya leaf extract (CPLE) | NS2B–NS3 | DENV | NCT06121934 | Phase 3 | Completed | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Efficacy and Safety of Carica Papaya in Dengue Fever: A Randomised Clinical Trial//ClinicalTrials.gov/NCT06121934 |
| Ribavirin | NS3 helicase | JEV | NCT00216268 | Phase 2 | Unknown | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Treatment of Japanese Encephalitis/ClinicalTrials.gov/NCT00216268 |
| EYU688 | NS4B | DENV | NCT06006559 | Phase 2 | Ongoing | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/A Study to Assess the Efficacy, Safety and Pharmacokinetics of EYU688 in Patients With Dengue Fever/ClinicalTrials.gov/NCT06006559 |
| Galidesivir | NS5 | YFV | NCT03891420 | Phase 1 | TERMINATED | Withdrawn due to lack of funding | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/A Study to Evaluate the Safety, Pharmacokinetics and Antiviral Effects of Galidesivir in Yellow Fever or COVID-19/ClinicalTrials.gov/NCT03891420 |
| Iron-fortified food | Oxidative stress-mediated signaling | JEV | NCT06027801 | Not Applicable | Recruiting | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Iron Fortified Food to Improve Japanese Encephalitis and Typhoid Fever Vaccine Immunogenicity/ClinicalTrials.gov/NCT06027801 |
| Metformin | AMPK | YFV | NCT04267809 | Phase 2 | Completed | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Modulate Cellular Stress in the Immune Cells to Reduce Rate of Symptomatic Viral Infection/ClinicalTrials.gov/NCT04267809 |
| AVI-4020 injection | Interfere with RNA–RNA duplex structures | WNV | NCT00387283 | Phase 1 | Completed | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Pharmacokinetic Study in Cerebral Spinal Fluid After a Single Dose of AVI-4020/ClinicalTrials.gov/NCT00387283 |
| Ivermectin | IMPα/β (Host) | DENV | NCT02045069 | Phase 2/3 | Unknown | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Efficacy and Safety of Ivermectin Against Dengue Infection/ClinicalTrials.gov/NCT02045069 |
| Ivermectin | IMPα/β (Host) | DENV | NCT03432442 | Phase 2 | Completed | Safe and accelerated NS1 antigen clearance in dengue patients | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Pharmacokinetics and Pharmacodynamics of Ivermectin in Pediatric Dengue Patients/ClinicalTrials.gov/NCT03432442 |
| UV-4B | ER α-glucosidase I and II | DENV | NCT02061358 | Phase 1 | Completed | Safe in healthy subjects | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Study to Determine the Safety, Tolerability and Pharmacokinetics of UV-4B Solution Administered Orally in Healthy Subjects/ClinicalTrials.gov/NCT02061358 |
| Chloroquine | Endosomal acidification | DENV, ZIKV | NCT00849602 | Phase 1/2 | Completed | CQ ameliorated pain and lowered the viral load in dengue patients | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/The Effect of Chloroquine in the Treatment of Patients With Dengue/ClinicalTrials.gov/NCT00849602 |
| Dexamethasone | NF-kB and activator factor-1 | DENV | NCT05631405 | Not Applicable | Ongoing | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Efficacy of Dengue Infection With Warning Signs Treated With Dexamethasone (DengDex Study)/ClinicalTrials.gov/NCT05631405 |
| Anti-d | Fcγ receptor | DENV | NCT01443247 | Not Applicable | Completed | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Role of Andi-d in Dengue Fever: a Pilot Study/ClinicalTrials.gov/NCT01443247 |
| Anakinra | Interleukin-1 receptor (IL-1R) | DENV | NCT05611710 | Phase 2 | Ongoing | No results available | Clinical trials.Gov (accessed on 1 July 2024); available online: Study Details/Anakinra in Dengue With Hyperinflammation (AnaDen)/ClinicalTrials.gov/NCT05611710 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tripathi, A.; Chauhan, S.; Khasa, R. A Comprehensive Review of the Development and Therapeutic Use of Antivirals in Flavivirus Infection. Viruses 2025, 17, 74. https://doi.org/10.3390/v17010074
Tripathi A, Chauhan S, Khasa R. A Comprehensive Review of the Development and Therapeutic Use of Antivirals in Flavivirus Infection. Viruses. 2025; 17(1):74. https://doi.org/10.3390/v17010074
Chicago/Turabian StyleTripathi, Aarti, Shailendra Chauhan, and Renu Khasa. 2025. "A Comprehensive Review of the Development and Therapeutic Use of Antivirals in Flavivirus Infection" Viruses 17, no. 1: 74. https://doi.org/10.3390/v17010074
APA StyleTripathi, A., Chauhan, S., & Khasa, R. (2025). A Comprehensive Review of the Development and Therapeutic Use of Antivirals in Flavivirus Infection. Viruses, 17(1), 74. https://doi.org/10.3390/v17010074





