Prognostic Performance of Inflammatory Biomarkers Based on Complete Blood Counts in COVID-19 Patients
Abstract
:1. Introduction
2. Materials and Methods
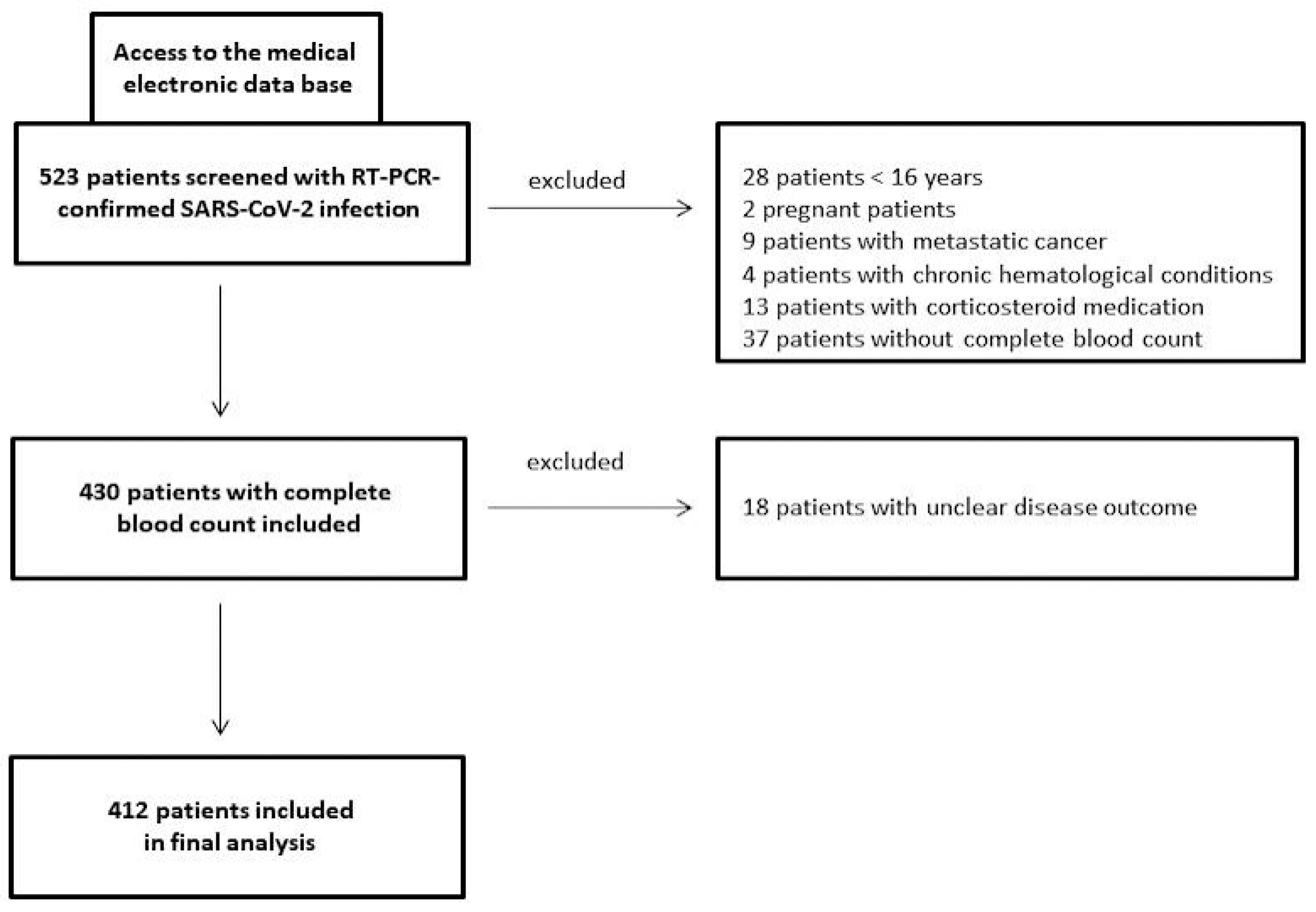
2.1. Patients
2.2. Data Extraction and Outcome Measures
2.3. Laboratory Tests
2.4. Statistics
3. Results
3.1. Patient Characteristics and Outcome Measures
3.2. Univariable Analysis
3.3. Multivariable Analyses
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tian, W.; Jiang, W.; Yao, J.; Nicholson, C.J.; Li, R.H.; Sigurslid, H.H.; Wooster, L.; Rotter, J.I.; Guo, X.; Malhotra, R. Predictors of mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis. J. Med. Virol. 2020, 92, 1875–1883. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Kojima, S.; Kawamoto, A.; Fukushima, M. COVID-19 pathogenesis, prognostic factors, and treatment strategy: Urgent recommendations. J. Med. Virol. 2021, 93, 2694–2704. [Google Scholar] [CrossRef]
- Li, J.; Huang, D.Q.; Zou, B.; Yang, H.; Hui, W.Z.; Rui, F.; Yee, N.T.S.; Liu, C.; Nerurkar, S.N.; Kai, J.C.Y.; et al. Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J. Med. Virol. 2021, 93, 1449–1458. [Google Scholar] [CrossRef]
- Munster, V.J.; Koopmans, M.; van Doremalen, N.; van Riel, D.; de Wit, E. A novel coronavirus emerging in China—key questions for impact assessment. N. Engl. J. Med. 2020, 382, 692–694. [Google Scholar] [CrossRef]
- Chen, Z.; Peng, Y.; Wu, X.; Pang, B.; Yang, F.; Zheng, W.; Liu, C.; Zhang, J. Comorbidities and complications of COVID-19 associated with disease severity, progression, and mortality in China with centralized isolation and hospitalization: A systematic review and meta-analysis. Front. Public Health 2022, 10, 923485. [Google Scholar] [CrossRef] [PubMed]
- Al-Shajlawi, M.; Alsayed, A.R.; Abazid, H.; Awajan, D.; Al-Imam, A.; Basheti, I. Using laboratory parameters as predictors for the severity and mortality of COVID-19 in hospitalized patients. Pharm. Pract. 2022, 20, 2721. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, T.; Raj, A.; Das, N.; Gupta, R.; Gupta, N.; Tiwari, P.; Sahoo, B.; Sagiraju, H.K.R.; Sirohiya, P.; Ratre, B.; et al. The Evaluation of Laboratory Parameters as Predictors of Disease Severity and Mortality in COVID-19 Patients: A Retrospective Study from a Tertiary Care Hospital in India. Cureus 2023, 15, e40273. [Google Scholar] [CrossRef]
- Lippi, G.; Henry, B.M. Eosinophil count in severe coronavirus disease 2019. QJM 2020, 113, 511–512. [Google Scholar] [CrossRef]
- Cazzaniga, M.; Fumagalli, L.A.M.; D’angelo, L.; Cerino, M.; Bonfanti, G.; Fumagalli, R.M.; Schiavo, G.; Lorini, C.; Lainu, E.; Terragni, S.; et al. Eosinopenia is a reliable marker of severe disease and unfavourable outcome in patients with COVID-19 pneumonia. Int. J. Clin. Pract. 2021, 75, e14047. [Google Scholar] [CrossRef]
- Soni, M. Evaluation of eosinopenia as a diagnostic and prognostic indicator in COVID-19 infection. Int. J. Lab. Hematol. 2021, 43, 137–141. [Google Scholar] [CrossRef]
- Ito, A.; Ishida, T.; Nakanishi, Y.; Kobe, H.; Tokioka, F. Eosinopenia is associated with adverse outcomes after COVID-19 infection: A perspective from Japan. Respirology 2023, 28, 677–680. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, H.K.; Mehra, M.R. COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal. J. Heart Lung Transplant. 2020, 39, 405–407. [Google Scholar] [CrossRef]
- WHO Working Group on the Clinical Characterisation and Management of COVID-19 Infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 2020, 20, e192–e197. [Google Scholar] [CrossRef] [PubMed]
- Susok, L.; Said, S.; Reinert, D.; Mansour, R.; Scheel, C.H.; Becker, J.C.; Gambichler, T. The pan-immune-inflammation value and systemic immune-inflammation index in advanced melanoma patients under immunotherapy. J. Cancer Res. Clin. Oncol. 2022, 148, 3103–3108. [Google Scholar] [CrossRef]
- Guven, D.C.; Sahin, T.K.; Erul, E.; Kilickap, S.; Gambichler, T.; Aksoy, S. The Association between the Pan-Immune-Inflammation Value and Cancer Prognosis: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 2675. [Google Scholar] [CrossRef]
- Ramos da Silva, S.; Ju, E.; Meng, W.; Paniz Mondolfi, A.E.; Dacic, S.; Green, A.; Bryce, C.; Grimes, Z.; Fowkes, M.; Sordillo, E.M.; et al. Broad Severe Acute Respiratory Syndrome Coronavirus 2 Cell Tropism and Immunopathology in Lung Tissues from Fatal Coronavirus Disease 2019. J. Infect. Dis. 2021, 223, 1842–1854. [Google Scholar] [CrossRef] [PubMed]
- Karimi, A.; Shobeiri, P.; Kulasinghe, A.; Rezaei, N. Novel Systemic Inflammation Markers to Predict COVID-19 Prognosis. Front. Immunol. 2021, 12, 741061. [Google Scholar] [CrossRef]
- Ballaz, S.J.; Fors, M. Predictive Value of the Platelet Times Neutrophil-to-Lymphocyte Ratio (SII Index) for COVID-19 In-Hospital Mortality. EJIFCC 2023, 34, 167–173. [Google Scholar]
- Haryati, H.; Wicaksono, B.; Syahadatina, M. Complete blood count derived inflammation indexes predict outcome in COVID-19 patients: A study in Indonesia. J. Infect. Dev. Ctries. 2023, 17, 319–326. [Google Scholar] [CrossRef]
- Zein, J.G.; Strauss, R.; Attaway, A.H.; Hu, B.; Milinovich, A.; Jawhari, N.; Chamat, S.S.; Ortega, V.E. Eosinophilia Is Associated with Improved COVID-19 Outcomes in Inhaled Corticosteroid-Treated Patients. J. Allergy Clin. Immunol. Pract. 2022, 10, 742–750.e14. [Google Scholar] [CrossRef]
- Lippi, G.; Sanchis-Gomar, F.; Henry, B.M. COVID-19 and its long-term sequelae: What do we know in 2023? Pol. Arch. Intern. Med. 2023, 133, 16402. [Google Scholar] [CrossRef] [PubMed]
- Notarte, K.I.; de Oliveira, M.H.S.; Peligro, P.J.; Velasco, J.V.; Macaranas, I.; Ver, A.T.; Pangilinan, F.C.; Pastrana, A.; Goldrich, N.; Kavteladze, D.; et al. Age, Sex and Previous Comorbidities as Risk Factors Not Associated with SARS-CoV-2 Infection for Long COVID-19: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 7314. [Google Scholar] [CrossRef] [PubMed]
| (a) | (b) | ||
|---|---|---|---|
| Parameter | Data | Parameter | Data |
| Sex Female/male | 199/213 (48.3%/51.7%) | Obesity no/yes | 324/88 (78.6%/21.4%) |
| Median age (years) | 58 (16–97) | Diabetes mellitus no/yes | 314/97 (76.4%/23.6%) |
| Body mass index (kg/m2) | 27.7 (17.3–50.5) | Smoking no/yes | 359/53 (87.1%/12.9%) |
| Vaccination status No vaccination 1st vaccination 2nd vaccination 1st booster 2nd booster | 367 (89.1%) 19 (4.6%) 23 (5.6%) 3 (0.7%) 0 (0%) | Lung diseases no/yes | 338/74 (82%/18%) |
| Recovery rate no/yes | 409/3 (99.3%/0.7%) | Cardiovascular diseases no/yes | 189/223 (45.9%/54.1%) |
| Median Ct-value (S-gene) (E-gene) (RdRP-gene) (N-gene) | 22 (7–38) 23 (10–37) 24 (7–39) 25 (11–287) | Neuropsychiatric diseases no/yes | 328/84 (79.6%/20.8%) |
| Fever (≥38 °C) no/yes | 319/79 (80.2%/19.8%) | At least two comorbidities no/yes | 198/214 (48.1%/51.9%) |
| Dysnosomie no/yes | 326/86 (79.1%/20.9%) | Staging by Siddiqi and Mehra Stage I Stage IIA Stage IIB Stage III | 89 (21.6%) 52 (12.6%) 223 (54.1%) 49 (11.9%) |
| Breathing rate median | 19 (8–50) | WHO clinical progression scale I II III IV | 93 (22.6%) 211 (51.2%) 54 (13.1%) 55 (13.3%) |
| Oxygen saturation median percentage | 97 (40–100) | COVID-19 pneumonia no/yes | 104/307 (25.3%/74.7%) |
| Days with symptoms before admission median | 6 (1–22) | Intensive care unit (ICU) no/yes median days on ICU | 312/100 (75.7%/24.3%) 9.5 (1–85) |
| In-patient treatment no/yes | 23/389 (5.6%/94.4%) | Deceased with COVID-19 no/yes | 357/55 (86.7%/13.3%) |
| Duration of in-patient treatment median | 10 (1–194) | Duration of in-patient treatment median | 10 (1–194) |
| Breathing support no oxygen via nasal canula high-flow oxygen, non-invasive ventilation intubation ECMO | 140 (34%) 179 (43.4%) 56 (13.6%) 26 (6.3% 11 (2.6%) | ||
| Anti-COVID-19 therapy no dexamethasone remdesivir dexamethasone/remdesivir miscellaneous | 216 (52.4%) 97 (23.5%) 31 (7.5%) 48 (11.7%) 20 (4.9%) | ||
| Parameter | Data |
|---|---|
| C-reactive protein (mg/L) median (range) | 36.3 (1–558) |
| Lactate dehydrogenase (U/L) median (range) | 261.5 (86–1156) |
| Ferritin (ng/mL) median (range) | 409 (5–10,627) |
| Neutrophils (/µL) median (range) | 3955 (900–18,200) |
| Lymphocytes (/µL) median (range) | 1090 (240–5090) |
| Monocytes (/µL) median (range) | 440 (70–7300) |
| Eosinophils (/µL) median (range) Eosinopenia (<40/µL) no/yes Absolute eosinopenia (0/µL) no/yes | 10 (0–480) 105/307 (25.5%/74.5%) 228/184 (55.3%/44.7%) |
| Thrombocytes (/µL) median (range) | 189,000 (24,000–784,000) |
| Neutrophil-to-lymphocyte ratio median (range) healthy controls | 3.7 (0.55–72.6) 1.9 (0.9–11.6) p < 0.0001 |
| Systemic immune-inflammation index median (range) healthy controls | 688 (39.7–14,661) 425 (39.3–5946) p = 0.0002 |
| Pan-immune-inflammation value median (range) healthy controls | 288 (16.8–24,338) 275 (81–1621) p = 0.47 |
| Parameter | Prognostic for Class IIB and III (Siddiqi and Mehra) [12] | Prognostic for Class III and IV (WHO) [13] | Prognostic for COVID-19 Death |
|---|---|---|---|
| Ferritin | AUC 0.77, p < 0.0001 Criterion: >465, Youden index: 0.41 | - | - |
| LDH | AUC 0.81, p < 0.0001 Criterion: >239, Youden index: 0.50 | AUC 0.78, p < 0.0001 Criterion: >371, Youden index: 0.41 | AUC 0.78, p < 0.0001 Criterion: >339, Youden index: 0.45 |
| C-reactive protein | AUC 0.85, p < 0.0001 Criterion: >26, Youden index: 0.54 | AUC 0.81, p < 0.0001 Criterion: >83, Youden index: 0.47 | AUC 0.79, p < 0.0001 Criterion: >47, Youden index: 0.46 |
| Age > 75 years | p < 0.0001 | p < 0.0001 | p < 0.0001 |
| Diabetes | p = 0.014 | - | p < 0.0001 |
| Obesity | - | p = 0.0047 | - |
| Cardiovascular diseases | p < 0.0001 | p = 0.0004 | p < 0.0001 |
| Lung diseases | p = 0.006 | p < 0.0001 | p = 0.0073 |
| Two or more comorbidities | p < 0.0001 | p < 0.0001 | p < 0.0001 |
| Absolute eosinopenia | p < 0.0001 | p < 0.0001 | p < 0.0001 |
| NLR | - | AUC 0.72, p < 0.0001 Criterion: >5.4, Youden index: 0.32 | AUC 0.74, p < 0.0001 Criterion: >7.4, Youden index: 0.47 |
| SII | - | - | AUC 0.70, p < 0.0001 Criterion: >1196, Youden index: 0.37 |
| Parameter | Prognostic for Class IIB and III (Siddiqi and Mehra) [12] | Prognostic for Class III and IV (WHO) [13] | Prognostic for COVID-19 Death |
|---|---|---|---|
| Ferritin | OR 1.0006, 95% CI 1.0001 to 1.0012, p = 0.026 | - | - |
| LDH | - | OR 2.7, 95% CI 1.4 to 5.0, p = 0.027 | OR 4.2, 95% CI 1.8 to 10, p = 0.0012 |
| C-reactive protein | OR 4.5, 95% CI 2.2 to 9, p < 0.0001 | OR 4.4, 95% CI 2.4 to 7.6, p < 0.0001 | - |
| Age | OR 2.3, 95% CI 1.1 to 4.7, p = 0.021 | OR 2.3, 95% CI 1.2 to 4.4, p = 0.011 | OR 8.3, 95% CI 3.5 to 19.8, p < 0.0001 |
| Absence of cardiovascular diseases | OR 0.43, 95% CI 0.20 to 0.88, p = 0.022 | - | - |
| Lung diseases | - | OR 2.3, 95% CI 1.1 to 4.6, p = 0.013 | - |
| Absolute eosinopenia | OR 4.4, 95% CI 2.4 to 7.6, p < 0.0001 | OR 3.2, 95% CI 1.8 to 5.6, p = 0.0001 | OR 2.6, 95% CI 1.2 to 5.7, p = 0.017 |
| NLR | - | OR 2.5, 95% CI 1.3 to 4.9, p = 0.006 | OR 2.8, 95% CI 2.1.1 to 7.4, p = 0.035 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gambichler, T.; Schuleit, N.; Susok, L.; Becker, J.C.; Scheel, C.H.; Torres-Reyes, C.; Overheu, O.; Reinacher-Schick, A.; Schmidt, W. Prognostic Performance of Inflammatory Biomarkers Based on Complete Blood Counts in COVID-19 Patients. Viruses 2023, 15, 1920. https://doi.org/10.3390/v15091920
Gambichler T, Schuleit N, Susok L, Becker JC, Scheel CH, Torres-Reyes C, Overheu O, Reinacher-Schick A, Schmidt W. Prognostic Performance of Inflammatory Biomarkers Based on Complete Blood Counts in COVID-19 Patients. Viruses. 2023; 15(9):1920. https://doi.org/10.3390/v15091920
Chicago/Turabian StyleGambichler, Thilo, Nadine Schuleit, Laura Susok, Jürgen C. Becker, Christina H. Scheel, Christian Torres-Reyes, Oliver Overheu, Anke Reinacher-Schick, and Wolfgang Schmidt. 2023. "Prognostic Performance of Inflammatory Biomarkers Based on Complete Blood Counts in COVID-19 Patients" Viruses 15, no. 9: 1920. https://doi.org/10.3390/v15091920
APA StyleGambichler, T., Schuleit, N., Susok, L., Becker, J. C., Scheel, C. H., Torres-Reyes, C., Overheu, O., Reinacher-Schick, A., & Schmidt, W. (2023). Prognostic Performance of Inflammatory Biomarkers Based on Complete Blood Counts in COVID-19 Patients. Viruses, 15(9), 1920. https://doi.org/10.3390/v15091920









