Placental Infection Associated with SARS-CoV-2 Wildtype Variant and Variants of Concern
Abstract
:1. Introduction
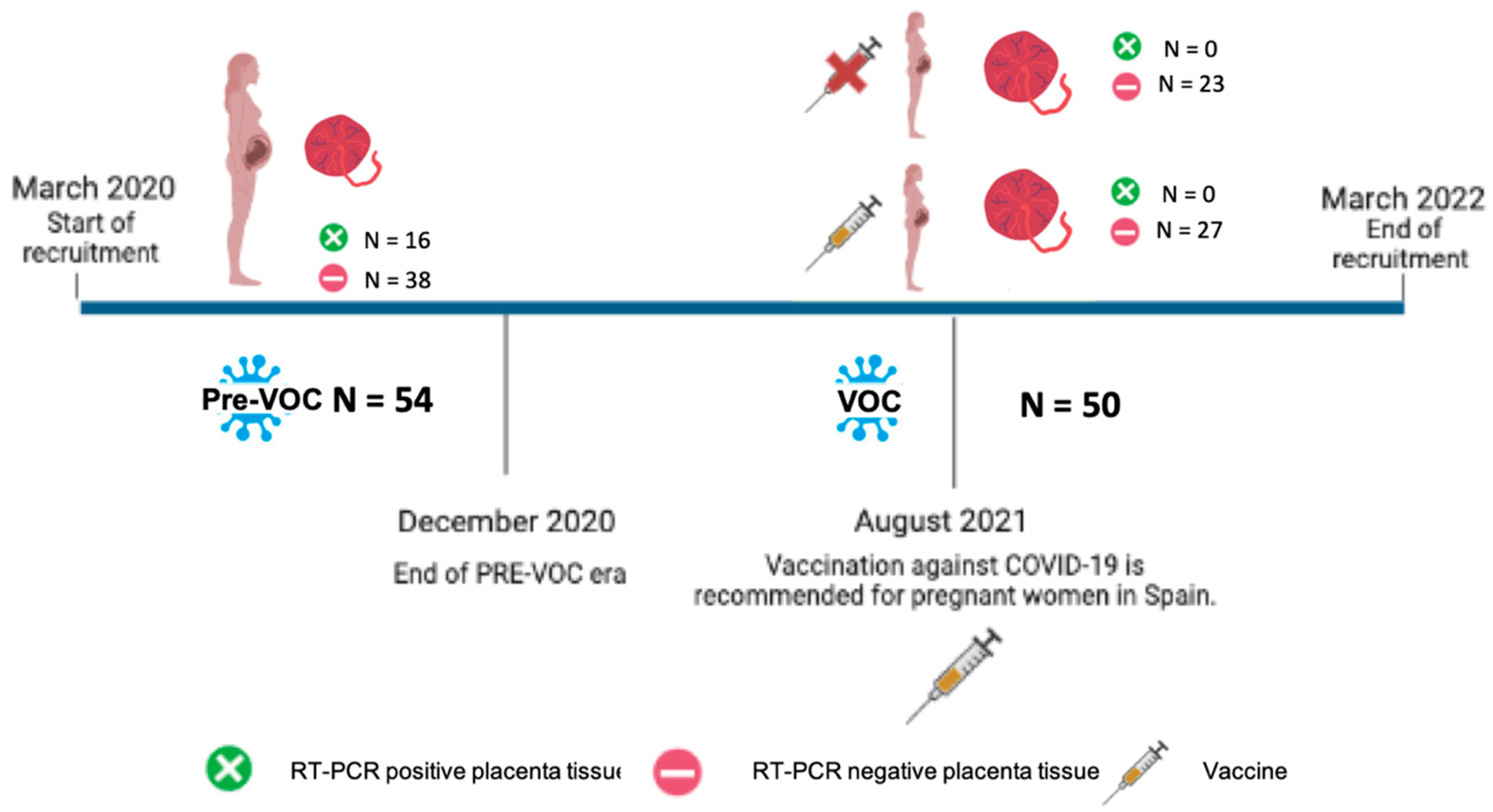
2. Materials and Methods
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Whole genome sequencing
References
- Rambaut, A.; Loman, N.; Pybus, O.; Barclay, W.; Barrett, J.; Carabelli, A.; Connor, T.; Peacock, T.; Robertson, D.L.; Volz, E.; et al. Preliminary genomic characterisation of an emergent SARS-CoV-2 lineage in the UK defined by a novel set of spike mutations. Virological 2020. Available online: https://virological.org/t/preliminary-genomic-characterisation-of-an-emergent-sars-cov-2-lineagein-the-uk-defined-by-a-novel-set-of-spike-mutations/563 (accessed on 10 August 2023).
- European Centre for Disease Prevention and Control. Threat Assessment Brief: Emergence of SARS-CoV-2 B.1.617 Variants in India and Situation in the EU/EEA. 11 May 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/threat-assessment-emergence-sars-cov-2-b1617-variants (accessed on 10 August 2023).
- Cao, Y.; Wang, J.; Jian, F.; Xiao, T.; Song, W.; Yisimayi, A.; Huang, W.; Li, Q.; Wang, P.; An, R.; et al. Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature 2022, 602, 657–663. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed on 10 August 2023).
- Mediavilla, J.R.; Lozy, T.; Lee, A.; Kim, J.; Kan, V.W.; Titova, E.; Amin, A.; Zody, M.C.; Corvelo, A.; Oschwald, D.M.; et al. Molecular and Clinical Epidemiology of SARS-CoV-2 Infection among Vaccinated and Unvaccinated Individuals in a Large Healthcare Organization from New Jersey. Viruses 2023, 15, 1699. [Google Scholar] [CrossRef]
- Esper, F.P.; Adhikari, T.M.; Tu, Z.J.; Cheng, Y.-W.; El-Haddad, K.; Farkas, D.H.; Bosler, D.; Rhoads, D.; Procop, G.W.; Ko, J.S.; et al. Alpha to Omicron: Disease Severity and Clinical Outcomes of Major SARS-CoV-2 Variants. J. Infect. Dis. 2023, 227, 344–352. [Google Scholar] [CrossRef]
- Fiolet, T.; Kherabi, Y.; MacDonald, C.J.; Ghosn, J.; Peiffer-Smadja, N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: A narrative review. Clin. Microbiol. Infect. 2022, 28, 202–221. [Google Scholar] [CrossRef]
- Male, V. SARS-CoV-2 infection and COVID-19 vaccination in pregnancy. Nat. Rev. Immunol. 2022, 22, 277–282. [Google Scholar] [CrossRef]
- Villar, J.; Soto Conti, C.P.; Gunier, R.B.; Ariff, S.; Craik, R.; Cavoretto, P.I.; Rauch, S.; Gandino, S.; Nieto, R.; Winsey, A.; et al. Pregnancy outcomes and vaccine effectiveness during the period of omicron as the variant of concern, INTERCOVID-2022: A multinational, observational study. Lancet 2023, 11, 447–457. [Google Scholar] [CrossRef]
- Villar, J.; Ariff, S.; Gunier, R.B.; Thiruvengadam, R.; Rauch, S.; Kholin, A.; Roggero, P.; Prefumo, F.; do Vale, M.S.; Cardona-Perez, J.A.; et al. Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection: The INTERCOVID Multinational Cohort Study. JAMA Pediatr. 2021, 175, 817–826, Correction in JAMA Pediatr. 2022, 176, 104. [Google Scholar] [CrossRef]
- Savasi, V.M.; Parisi, F.; Patanè, L.; Ferrazzi, E.; Frigerio, L.; Pellegrino, A.; Spinillo, A.; Tateo, S.; Ottoboni, M.; Veronese, P.; et al. Clinical findings and disease severity in hospitalized pregnant women with coronavirus disease 2019 (COVID-19). Obstet. Gynecol. 2020, 136, 252–258. [Google Scholar] [CrossRef]
- Seasely, A.R.; Blanchard, C.T.; Arora, N.; Battarbee, A.N.; Casey, B.M.; Dionne-Odom, J.; Leal, S.M., Jr.; Moates, D.B.; Sinkey, R.G.; Szychowski, J.M.; et al. Maternal and Perinatal Outcomes Associated With the Omicron Variant of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection. Obstet. Gynecol. 2022, 140, 262–265. [Google Scholar] [CrossRef]
- Vousden, N.; Ramakrishnan, R.; Bunch, K.; Morris, E.; Simpson, N.A.B.; Gale, C.; O’Brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J.; et al. Severity of maternal infection and perinatal outcomes during periods of SARS-CoV-2 wildtype, alpha, and delta variant dominance in the UK: Prospective cohort study. BMJ Med. 2022, 1, e000053. [Google Scholar] [CrossRef] [PubMed]
- Mihajlovic, S.; Nikolic, D.; Santric-Milicevic, M.; Milicic, B.; Rovcanin, M.; Acimovic, A.; Lackovic, M. Four Waves of the COVID-19 Pandemic: Comparison of Clinical and Pregnancy Outcomes. Viruses 2022, 14, 2648. [Google Scholar] [CrossRef] [PubMed]
- Taglauer, E.; Benarroch, Y.; Rop, K.; Barnett, E.; Sabharwal, V.; Yarrington, C.; Wachman, E.M. Consistent localization of SARS-CoV-2 spike glycoprotein and ACE2 over TMPRSS2 predominance in placental villi of 15 COVID-19 positive maternal-fetal dyads. Placenta 2020, 100, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.A.; Baldewijns, M.; Benachi, A.; Bugatti, M.; Collins, R.R.J.; De Luca, D.; Facchetti, F.; Linn, R.L.; Marcelis, L.; Morotti, D.; et al. Chronic Histiocytic Intervillositis With Trophoblast Necrosis Is a Risk Factor Associated with Placental Infection from Coronavirus Disease 2019 (COVID-19) and Intrauterine Maternal-Fetal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Transmission in Live-Born and Stillborn Infants. Arch. Pathol. Lab. Med. 2021, 145, 517–528. [Google Scholar] [PubMed]
- Kotlyar, A.M.; Grechukhina, O.; Chen, A.; Popkhadze, S.; Grimshaw, A.; Tal, O.; Taylor, H.S.; Tal, R. Vertical transmission of coronavirus disease 2019: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2021, 224, 35–53.e3. [Google Scholar] [CrossRef]
- Fenizia, C.; Biasin, M.; Cetin, I.; Vergani, P.; Mileto, D.; Spinillo, A.; Gismondo, M.R.; Perotti, F.; Callegari, C.; Mancon, A.; et al. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat. Commun. 2020, 11, 5128. [Google Scholar] [CrossRef]
- Dubucs, C.; Groussolles, M.; Ousselin, J.; Sartor, A.; Van Acker, N.; Vayssière, C.; Pasquier, C.; Reyre, J.; Batlle, L.; Stèphanie Favarel Clinical Research Associate; et al. Severe placental lesions due to maternal SARS-CoV-2 infection associated to intrauterine fetal death. Hum. Pathol. 2022, 121, 46–55. [Google Scholar] [CrossRef]
- Celik, E.; Vatansever, C.; Ozcan, G.; Kapucuoglu, N.; Alatas, C.; Besli, Y.; Palaoglu, E.; Gursoy, T.; Manici, M.; Turgal, M.; et al. Placental deficiency during maternal SARS-CoV-2 infection. Placenta 2022, 117, 47–56. [Google Scholar] [CrossRef]
- Garcia-Flores, V.; Romero, R.; Xu, Y.; Theis, K.R.; Arenas-Hernandez, M.; Miller, D.; Peyvandipour, A.; Galaz, J.; Levenson, D.; Bhatti, G.; et al. Maternal-fetal immune responses in pregnant women infected with SARS-CoV-2. Nat. Commun. 2022, 13, 320. [Google Scholar] [CrossRef]
- Gao, Z.; Xu, Y.; Sun, C.; Wang, X.; Guo, Y.; Qiu, S.; Ma, K. A systematic review of asymptomatic infections with COVID-19. J. Microbiol. Immunol. Infect. 2021, 54, 12–16. [Google Scholar] [CrossRef]
- Evolución Diaria COVID-19 en Aragón. Datos Completes. Available online: https://www.aragon.es/coronavirus/situacion-actual/evolucion-diaria-datos-completos (accessed on 10 August 2023).
- Fabre, M.; Calvo, P.; Ruiz-Martinez, S.; Peran, M.; Oros, D.; Medel-Martinez, A.; Strunk, M.; Benito Ruesca, R.; Schoorlemmer, J.; Paules, C. Frequent Placental SARS-CoV-2 in Patients with COVID-19-Associated Hypertensive Disorders of Pregnancy. Fetal Diagn. Ther. 2021, 48, 801–811. [Google Scholar] [CrossRef] [PubMed]
- Figueras, F.; Meler, E.; Iraola, A.; Eixarch, E.; Coll, O.; Figueras, J.; Francis, A.; Gratacos, E.; Gardosi, J. Customized birthweight standards for a Spanish population. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 136, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Magee, L.A.; Brown, M.A.; Hall, D.R.; Gupte, S.; Hennessy, A.; Karumanchi, S.A.; Kenny, L.C.; McCarthy, F.; Myers, J.; Poon, L.C.; et al. The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2022, 27, 148–169. [Google Scholar] [CrossRef] [PubMed]
- Shanes, E.D.; Miller, E.S.; Otero, S.; Ebbott, R.; Aggarwal, R.; Willnow, A.S.; Ozer, E.A.; Mithal, L.B.; Goldstein, J.A. Placental Pathology After SARS-CoV-2 Infection in the Pre-Variant of Concern, Alpha/Gamma, Delta, or Omicron Eras. Int. J. Surg. Pathol. 2022, 31, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Wierz, M.; Sauerbrei, B.; Wandernoth, P.; Kriegsmann, M.; Casadonte, R.; Kriegsmann, K.; Kriegsmann, J. Detection of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) including Variant Analysis by Mass Spectrometry in Placental Tissue. Viruses 2022, 14, 604. [Google Scholar] [CrossRef]
- Argueta, L.B.; Lacko, L.A.; Bram, Y.; Tada, T.; Carrau, L.; Rendeiro, A.F.; Zhang, T.; Uhl, S.; Lubor, B.C.; Chandar, V.; et al. Inflammatory responses in the placenta upon SARS-CoV-2 infection late in pregnancy. iScience 2022, 25, 104223. [Google Scholar] [CrossRef]
- Dubucs, C.; Groussolles, M.; Brazet, E.; Courtade-Saïdi, M.; Van Acker, N.; Ousselin, J.; Pasquier, C.; Aziza, J. Fetal death and placental lesions after two COVID-19 episodes in single pregnancy in unvaccinated woman. Ultrasound Obstet. Gynecol. 2022, 60, 814–816. [Google Scholar] [CrossRef]
- Heeralall, C.; Ibrahim, U.H.; Lazarus, L.; Gathiram, P.; Mackraj, I. The effects of COVID-19 on placental morphology. Placenta 2023, 138, 88–96. [Google Scholar] [CrossRef]
- Serra, F.E.; Rosa Junior, E.R.; de Rossi, P.; Francisco, R.P.V.; Rodrigues, A.S. COVID-19: Impact of Original, Gamma, Delta, and Omicron Variants of SARS-CoV-2 in Vaccinated and Unvaccinated Pregnant and Postpartum Women. Vaccines 2022, 10, 2172. [Google Scholar] [CrossRef]
- Kourtis, A.P.; Read, J.S.; Jamieson, D.J. Pregnancy and infection. N. Engl. J. Med. 2014, 370, 2211–2218. [Google Scholar] [CrossRef]
- Silasi, M.; Cardenas, I.; Kwon, J.Y.; Racicot, K.; Aldo, P.; Mor, G. Viral infections during pregnancy. Am. J. Reprod. Immunol. 2015, 73, 199–213. [Google Scholar] [CrossRef]
- Mor, G.; Aldo, P.; Alvero, A.B. The unique immunological and microbial aspects of pregnancy. Nat. Rev. Immunol. 2017, 17, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Cribiù, F.M.; Erra, R.; Pugni, L.; Rubio-Perez, C.; Alonso, L.; Simonetti, S.; Croci, G.A.; Serna, G.; Ronchi, A.; Pietrasanta, C.; et al. Severe SARS-CoV-2 placenta infection can impact neonatal outcome in the absence of vertical transmission. J. Clin. Investig. 2021, 131, e145427. [Google Scholar] [CrossRef]
- Smithgall, M.C.; Liu-Jarin, X.; Hamele-Bena, D.; Cimic, A.; Mourad, M.; Debelenko, L.; Chen, X. Third-trimester placentas of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-positive women: Histomorphology, including viral immunohistochemistry and in-situ hybridization. Histopathology 2020, 77, 994–999. [Google Scholar] [CrossRef] [PubMed]
- Salamanna, F.; Veronesi, F.; Martini, L.; Landini, M.P.; Fini, M. Post-COVID-19 Syndrome: The Persistent Symptoms at the Post-viral Stage of the Disease. A Systematic Review of the Current Data. Front. Med. 2021, 8, 653516. [Google Scholar] [CrossRef] [PubMed]
- Glynn, S.M.; Yang, Y.J.; Thomas, C.; Friedlander, R.L.; Cagino, K.A.; Matthews, K.C.; Riley, L.E.; Baergen, R.N.; Prabhu, M. SARS-CoV-2 and Placental Pathology: Malperfusion Patterns Are Dependent on Timing of Infection During Pregnancy. Am. J. Surg. Pathol. 2022, 46, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Papageorghiou, A.T.; Deruelle, P.; Gunier, R.B.; Rauch, S.; García-May, P.K.; Mhatre, M.; Usman, M.A.; Abd-Elsalam, S.; Etuk, S.; Simmons, L.E.; et al. Preeclampsia and COVID-19: Results from the INTERCOVID prospective longitudinal study. Am. J. Obstet. Gynecol. 2021, 225, 289.e1–289.e17. [Google Scholar] [CrossRef]
- Duley, L. The global impact of pre-eclampsia and eclampsia. Semin. Perinatol. 2009, 33, 130–137. [Google Scholar] [CrossRef]
- Cunningham, F.G.; Leveno, K.J.; Dashe, J.S.; Bloom, S.L.; Spong, C.T.; Casey, B.M. Williams obstetrics. In Hypertensive Disorders, 24th ed.; Leveno, K.J., Bloom, S.L., Dashe, J.S., Hoffman, B.L., Eds.; McGraw Hill: New York, NY, USA, 2014; Chapter 40; pp. 728–779. [Google Scholar]
- Stock, S.J.; Moore, E.; Calvert, C.; Carruthers, J.; Denny, C.; Donaghy, J.; Hillman, S.; Hopcroft, L.E.M.; Hopkins, L.; Goulding, A.; et al. Pregnancy outcomes after SARS-CoV-2 infection in periods dominated by delta and omicron variants in Scotland: A population-based cohort study. Lancet Respir. Med. 2022, 10, 1129–1136. [Google Scholar] [CrossRef]
- Menni, C.; Valdes, A.M.; Polidori, L.; Antonelli, M.; Penamakuri, S.; Nogal, A.; Louca, P.; May, A.; Figueiredo, J.C.; Hu, C.; et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: A prospective observational study from the ZOE COVID Study. Lancet 2022, 399, 1618–1624. [Google Scholar] [CrossRef]
- Shoji, K.; Tsuzuki, S.; Akiyama, T.; Matsunaga, N.; Asai, Y.; Suzuki, S.; Iwamoto, N.; Funaki, T.; Yamada, M.; Ozawa, N.; et al. Comparison of clinical characteristics of COVID-19 in pregnant women between the Delta and Omicron variants of concern predominant periods. J. Infect. Chemother. 2023, 29, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, E.H.; SoRelle, J.A.; McIntire, D.D.; Spong, C.Y. Increasing severity of COVID-19 in pregnancy with Delta (B.1.617.2) variant surge. Am. J. Obstet. Gynecol. 2022, 226, 149–151. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidou, A.E.; Angelidou, S.; Havaki, S.; Paparizou, K.; Spanakis, N.; Chatzakis, C.; Sotiriadis, A.; Theodora, M.; Donoudis, C.; Daponte, A.; et al. Stillbirth due to SARS-CoV-2 placentitis without evidence of intrauterine transmission to fetus: Association with maternal risk factors. Ultrasound Obstet. Gynecol. 2022, 59, 813–822. [Google Scholar] [CrossRef]
- Kontovazainitis, C.G.; Katsaras, G.N.; Gialamprinou, D.; Mitsiakos, G. COVID-19 vaccination and pregnancy: A systematic review of maternal and neonatal outcomes. J. Perinat. Med. 2023, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Blakeway, H.; Prasad, S.; Kalafat, E.; Heath, P.T.; Ladhani, S.N.; Le Doare, K.; Magee, L.A.; O’Brien, P.; Rezvani, A.; von Dadelszen, P.; et al. COVID-19 vaccination during pregnancy: Coverage and safety. Am. J. Obstet. Gynecol. 2022, 226, 236.e1–236.e14. [Google Scholar] [CrossRef] [PubMed]
| Pre-VOC (n = 54) | VOC (n = 50) | p | |
|---|---|---|---|
| Demographic maternal data | |||
| Maternal age (SD), years | 31.5 (5.9) | 32.8 (5.4) | 0.311 |
| Maternal weight (SD), kg | 69.5 (12.6) | 67.9 (13.1) | 0.330 |
| Caucasian (%) | 30 (55.5) | 32 (64.0) | 0.381 |
| Primiparous (%) | 24 (44.4) | 18 (36.0) | 0.381 |
| Maternal and neonatal outcome at delivery | |||
| Gestational age at birth mean (SD), days | 272.2 (20.3) | 274 (7.4) | 0.365 |
| Birth weight, mean (SD), grams | 3114.5 (609.3) | 3136.7 (343.6) | 0.224 |
| Small for gestational age neonate (%) | 7 (13.0) | 4 (8.0) | 0.411 |
| Preterm birth (%) | 9 (16.7) | 2 (4.0) | 0.036 |
| Hypertensive disorders of pregnancy (%) | 14 (25.9) | 3 (6.0) | 0.003 |
| Labor induction (%) | 23 (42.6) | 16 (52.0) | 0.338 |
| Cesarean delivery (%) | 8 (14.8) | 12 (24.0) | 0.235 |
| Umbilical artery pH < 7.10 (%) | 2 (3.7) | 2 (4.0) | 0.984 |
| Description of SARS-CoV-2 infection | |||
| Trimester of SARS-CoV-2 infection | 0.083 | ||
| 1° (%) | 4 (7.4) | 0 (0.0) | |
| 2° (%) | 19 (35.2) | 14(28) | |
| 3° (%) | 31 (57.4) | 36 (72) | |
| Time between SARS-CoV-2 diagnosis and delivery, days (%) | 0.001 | ||
| <10 days | 7 (13.0) | 23 (46.0) | |
| 11–84 days | 23 (42.6) | 14 (28.0) | |
| >84 days | 24 (44.4) | 13 (26.0) | |
| Interval from diagnosis of SARS-CoV-2 to delivery (SD), days | 75.0 (54.2) | 50.3 (57.8) | 0.027 |
| COVID-19 Symptoms | 0.184 | ||
| No (%) | 23 (42.6) | 29 (58.0) | 0.085 |
| Mild (%) | 27 (50.0) | 20 (40.0) | 0.204 |
| Severe (%) | 4 (7.4) | 1 (2.0) | 0.206 |
| RT-PCR-positive placenta tissue (CT < 37), (%) | 16 (29.6) | 0 (0.0) | 0.000 |
| Diagnosis SARS-CoV-2 | Delivery and Placenta Tissue Results | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | GA at Diagnosis | PS | SYM | GA at Delivery | Interval SARS-CoV-2—Delivery (d) | RT-PCR Result Nasopharyngeal at Delivery Time | CT RT-PCR Nasopharyngeal | CT RT-PCR Placenta Tissue | Lineage | Correlation between PS and Placenta Tissue |
| 1 | 38 + 3 | Pre-VOC | S | 38 + 4 | 1 | Positive | 33.5 | 15.1 | B.1.177 | Yes |
| 2 | 25 + 1 | Pre-VOC | M | 39 + 2 | 99 | Negative | 33.9 | B.1 | Yes | |
| 3 | 31 + 4 | Pre-VOC | A | 41 + 0 | 74 | Negative | 30.2 | B.1 | Yes | |
| 4 | 24 + 6 | Pre-VOC | M | 37 + 1 | 86 | Negative | 31.7 | B.1.177 | Yes | |
| 5 | 25 + 6 | Pre-VOC | M | 40 + 1 | 100 | Negative | 33.1 | - | - | |
| 6 | 32 + 0 | Pre-VOC | A | 40 + 1 | 85 | Negative | 31.1 | B.1 | Yes | |
| 7 | 21 + 3 | Pre-VOC | A | 36 + 5 | 107 | N/A | 33.4 | B.1.177 | Yes | |
| 8 | 24 + 4 | Pre-VOC | M | 39 + 5 | 106 | Negative | 32.4 | B.1 | Yes | |
| 9 | 36 + 2 | Pre-VOC | A | 38 + 0 | 12 | Positive | 34.8 | 35.2 | B.1.177 | Yes |
| 10 | 30 + 0 | Pre-VOC | A | 40 + 2 | 72 | Negative | 24.5 | B.1 | Yes | |
| 11 | 37 + 6 | Pre-VOC | A | 38 + 1 | 2 | Positive | 35.3 | 33.9 | - | - |
| 12 | 17 + 5 | Pre-VOC | M | 38 + 2 | 151 | Negative | 32.0 | B.1 | Yes | |
| 13 | 27 + 5 | Pre-VOC | M | 37 + 0 | 68 | Negative | 23.3 | B.1.177 | Yes | |
| 14 | 32 + 3 | Pre-VOC | A | 41 + 2 | 64 | Negative | 32.5 | B.1 | Yes | |
| 15 | 8 + 0 | Pre-VOC | A | 35 + 2 | 191 | Negative | 28.7 | B.1.177 | Yes | |
| 16 | 41 + 0 | Pre-VOC | A | 41 + 1 | 8 | Positive | 35.5 | 33.7 | - | - |
| Pre-VOC (n = 54) | VOC Unvaccinated (n = 23) | VOC Vaccinated (n = 27) | p | |
|---|---|---|---|---|
| Hypertensive disorders of pregnancy, (%) | 14 (25.9) | 2 (8.7) | 1 (3.7) | 0.022 |
| Preterm birth, (%) | 9 (16.7) | 1 (4.3) | 1 (3.7) | 0.110 |
| Small for gestational age, (%) | 7 (13.0) | 1 (4.3) | 3 (11.1) | 0.528 |
| Birth weight, mean (SD), g | 3114.5 (609.3) | 3168.3 (308.4) | 3290.7 (367.2) | 0.331 |
| Trimester of SARS-CoV-2 infection | 0.148 | |||
| 1° (%) | 4 (7.4) | 0 (0.0) | 0 (0.0) | |
| 2° (%) | 19 (35.2) | 4 (17.4) | 10 (37) | |
| 3° (%) | 31 (57.4) | 18 (78.3) | 17 (63) | |
| Interval from diagnosis of SARS-CoV-2 to delivery (SD), d | 75.0 | 43.9 | 55.8 | 0.07 |
| COVID-19 Symptoms | 0.370 | |||
| No (%) | 23 (42.6) | 12 (52.2) | 17 (63) | 0.218 |
| Mild (%) | 27 (50) | 10 (43.5) | 10 (37) | 0.534 |
| Severe (%) | 4(7.4) | 1 (4.3) | 0 (0.0) | 0.338 |
| COVID-19 symptomatic, (%) | 31 (57.4) | 11 (47.8) | 10 (37) | 0.218 |
| RT-PCR-positive placenta tissue (CT < 37), (%) | 16 (29.6) | 0 (0.0) | 0 (0.0) | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Medel-Martinez, A.; Paules, C.; Peran, M.; Calvo, P.; Ruiz-Martinez, S.; Ormazabal Cundin, M.; Cebollada-Solanas, A.; Strunk, M.; Schoorlemmer, J.; Oros, D.; et al. Placental Infection Associated with SARS-CoV-2 Wildtype Variant and Variants of Concern. Viruses 2023, 15, 1918. https://doi.org/10.3390/v15091918
Medel-Martinez A, Paules C, Peran M, Calvo P, Ruiz-Martinez S, Ormazabal Cundin M, Cebollada-Solanas A, Strunk M, Schoorlemmer J, Oros D, et al. Placental Infection Associated with SARS-CoV-2 Wildtype Variant and Variants of Concern. Viruses. 2023; 15(9):1918. https://doi.org/10.3390/v15091918
Chicago/Turabian StyleMedel-Martinez, Ana, Cristina Paules, María Peran, Pilar Calvo, Sara Ruiz-Martinez, María Ormazabal Cundin, Alberto Cebollada-Solanas, Mark Strunk, Jon Schoorlemmer, Daniel Oros, and et al. 2023. "Placental Infection Associated with SARS-CoV-2 Wildtype Variant and Variants of Concern" Viruses 15, no. 9: 1918. https://doi.org/10.3390/v15091918
APA StyleMedel-Martinez, A., Paules, C., Peran, M., Calvo, P., Ruiz-Martinez, S., Ormazabal Cundin, M., Cebollada-Solanas, A., Strunk, M., Schoorlemmer, J., Oros, D., & Fabre, M. (2023). Placental Infection Associated with SARS-CoV-2 Wildtype Variant and Variants of Concern. Viruses, 15(9), 1918. https://doi.org/10.3390/v15091918





