Phenotypic Consequence of Rearranging the N Gene of RABV HEP-Flury
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses, Plasmids, Cell lines and Animals
2.2. Construction of Full-Length cDNA Clones
2.3. Rescue of the Rearranged Viruses from cDNA
2.4. Quantitative Real-Time PCR
2.5. Western Blot
2.6. Virus Growth and Spread Assays
2.7. Cell Apoptosis by Flow Cytometry
2.8. Lethality in Suckling Mice
2.9. Immunogenicity of the Rescued RABVs
3. Results
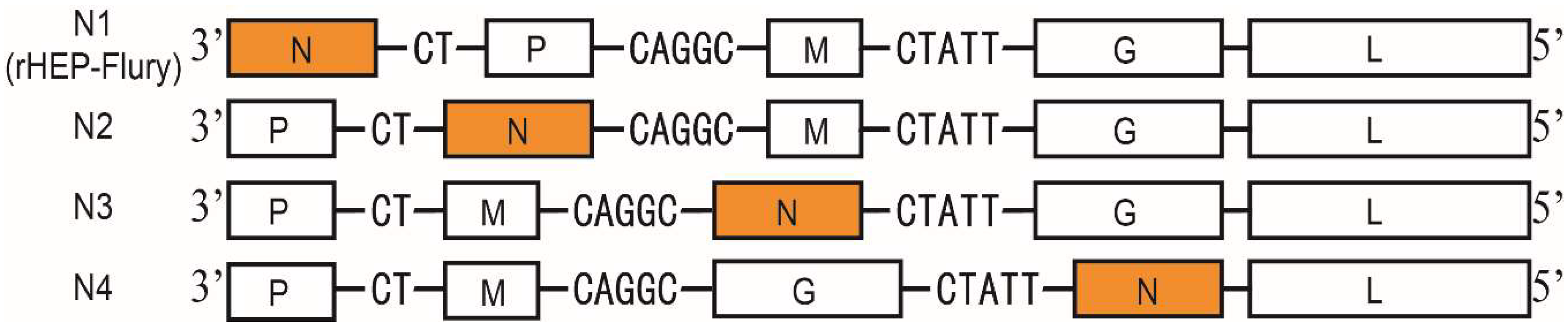
3.1. Structure of the Rearranged RABV
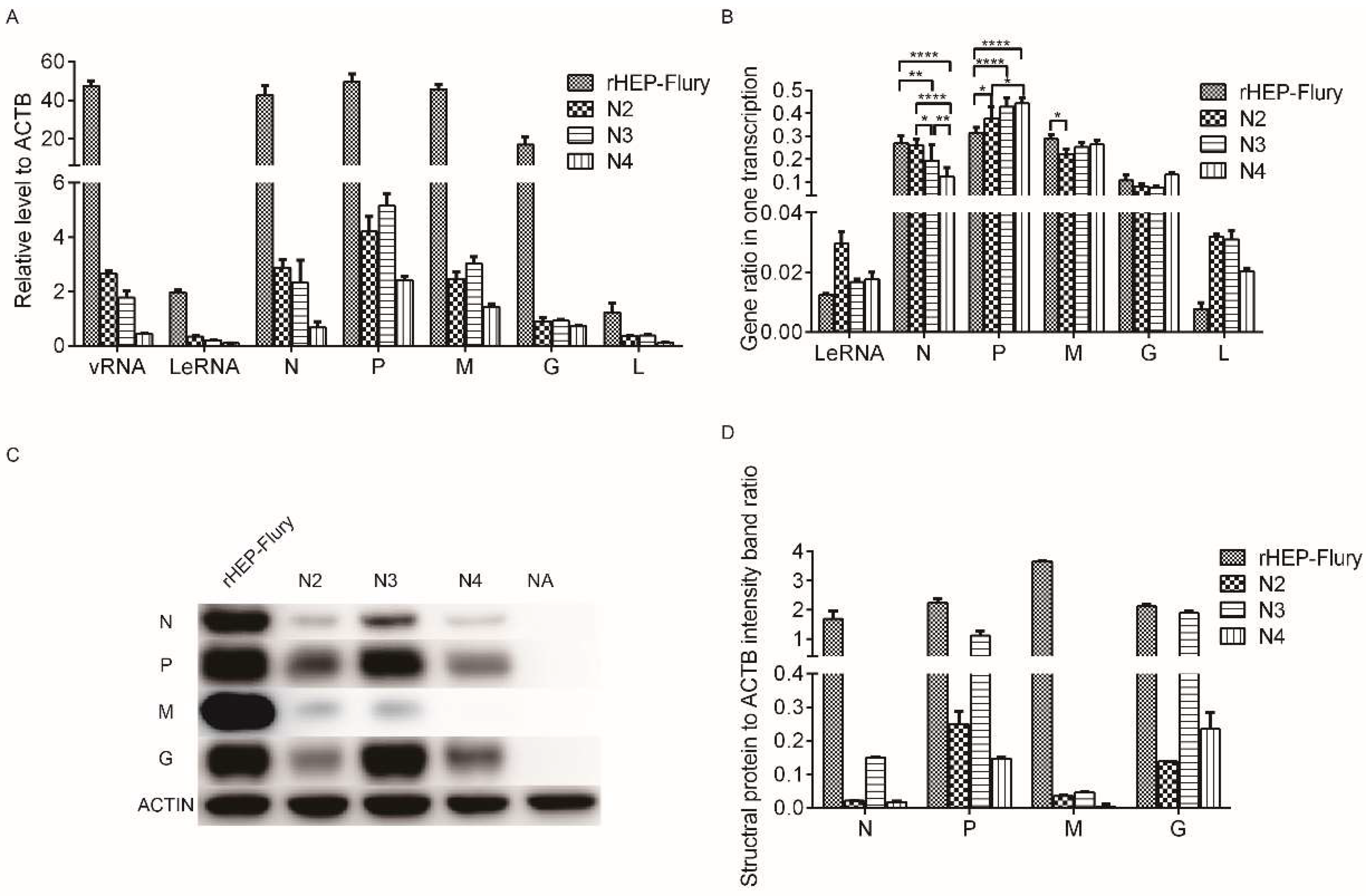
3.2. Effect of Gene Rearrangement on mRNA and Protein Expression
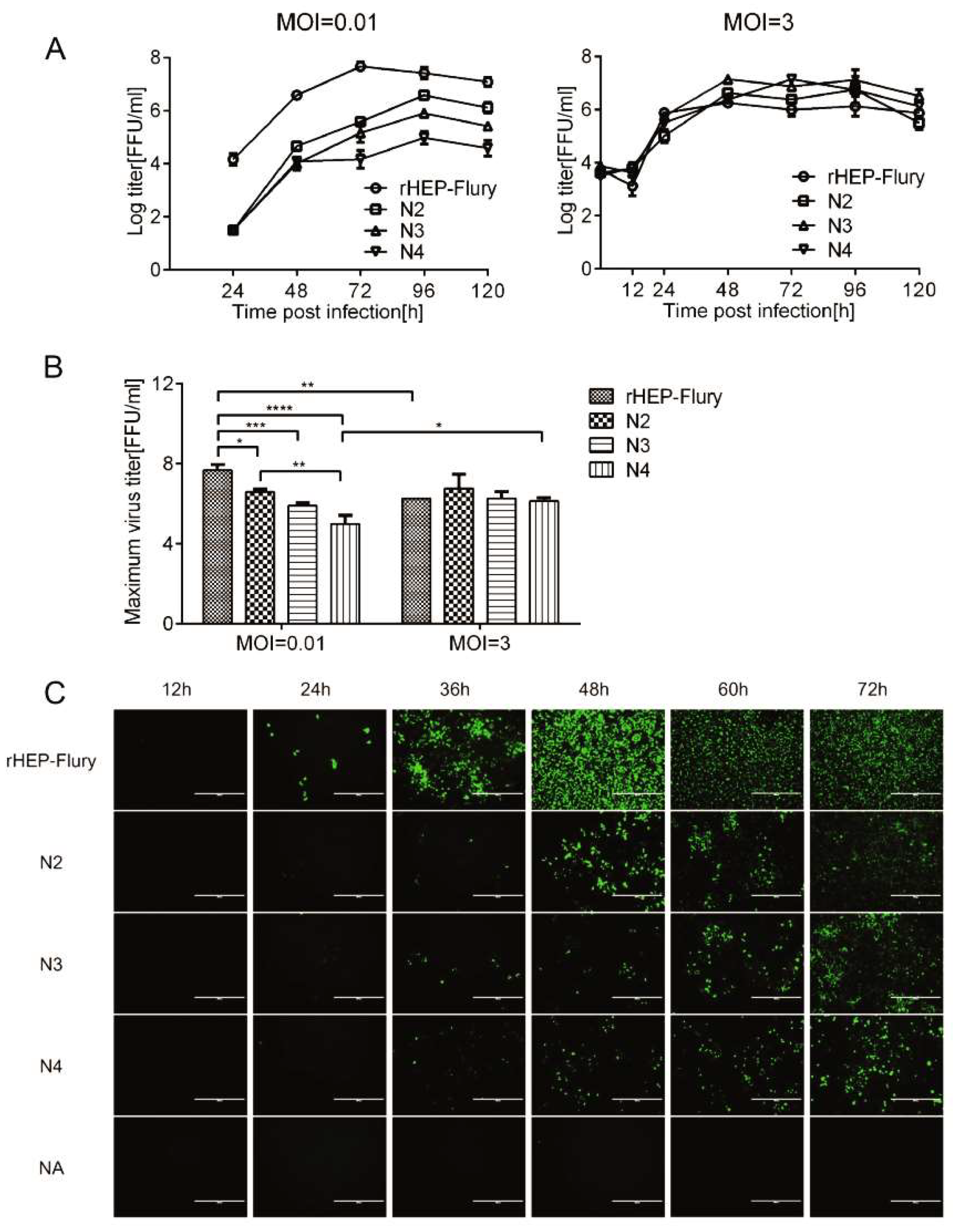
3.3. Replication and Spread of Viruses with Rearranged Genomes
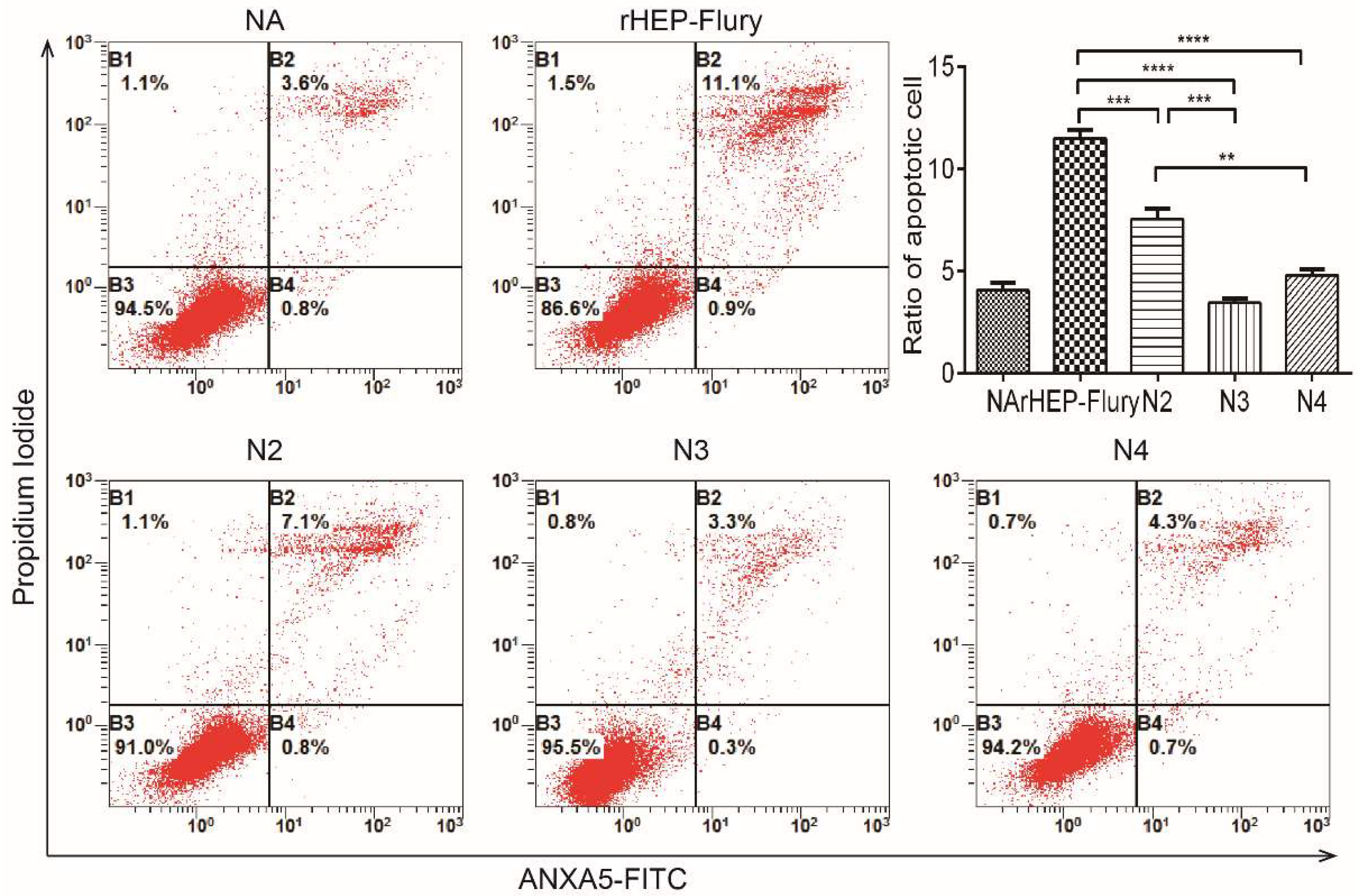
3.4. Cell Apoptosis
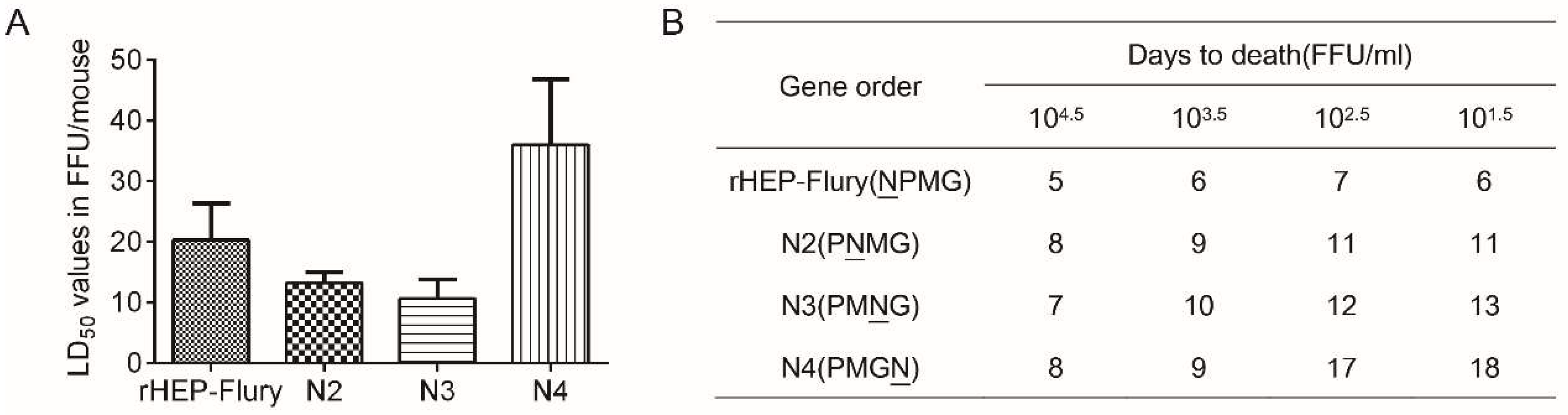
3.5. Lethality in Suckling Mice
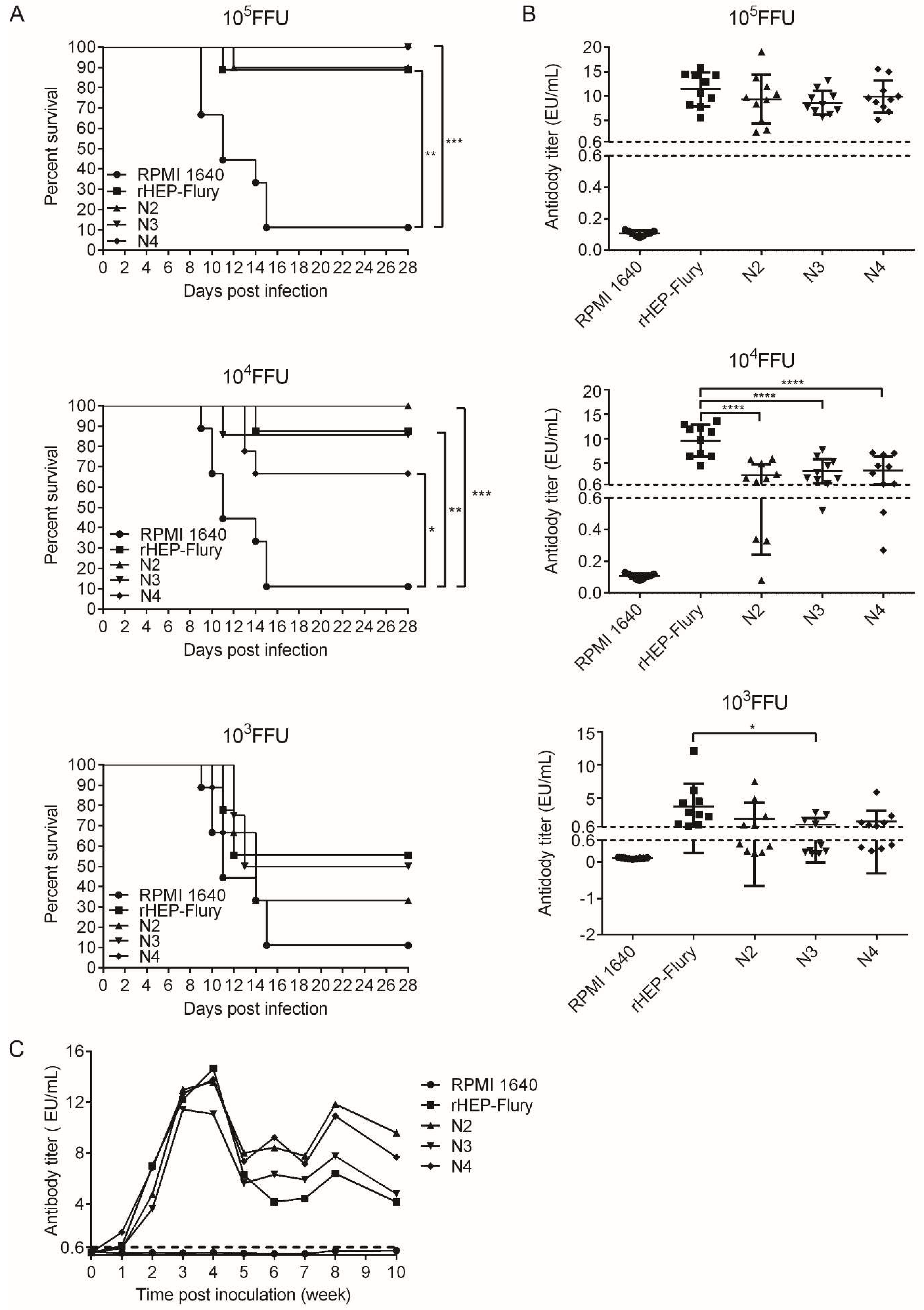
3.6. The Ability of Rearranged Viruses to Protect against Wild-Type Challenge
3.7. The Antibody Level Duration in Mice
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wertz, G.W.; Perepelitsa, V.P.; Ball, L.A. Gene rearrangement attenuates expression and lethality of a nonsegmented negative strand rna virus. Proc. Natl. Acad. Sci. USA 1998, 95, 3501–3506. [Google Scholar] [CrossRef]
- Ball, L.A.; Pringle, C.R.; Flanagan, B.; Perepelitsa, V.P.; Wertz, G.W. Phenotypic consequences of rearranging the p, m, and g genes of vesicular stomatitis virus. J. Virol. 1999, 73, 4705–4712. [Google Scholar]
- Flanagan, E.B.; Ball, L.A.; Wertz, G.W. Moving the glycoprotein gene of vesicular stomatitis virus to promoter-proximal positions accelerates and enhances the protective immune response. J. Virol. 2000, 74, 7895–7902. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ito, N.; Takayama, M.; Yamada, K.; Sugiyama, M.; Minamoto, N. Rescue of rabies virus from cloned cdna and identification of the pathogenicity-related gene: Glycoprotein gene is associated with virulence for adult mice. J. Virol. 2001, 75, 9121–9128. [Google Scholar] [CrossRef] [PubMed]
- Albertini, A.A.; Ruigrok, R.W.; Blondel, D. Rabies virus transcription and replication. Adv. Virus Res. 2011, 79, 1–22. [Google Scholar]
- Davis, B.M.; Rall, G.F.; Schnell, M.J. Everything you always wanted to know about rabies virus (but were afraid to ask). Annu. Rev. Virol. 2015, 2, 451–471. [Google Scholar] [CrossRef] [PubMed]
- Iseni, F.; Barge, A.; Baudin, F.; Blondel, D.; Ruigrok, R.W. Characterization of rabies virus nucleocapsids and recombinant nucleocapsid-like structures. J. Gen. Virol. 1998, 79 Pt 12, 2909–2919. [Google Scholar] [CrossRef]
- Fu, Z.F.; Dietzschold, B.; Schumacher, C.L.; Wunner, W.H.; Ertl, H.C.; Koprowski, H. Rabies virus nucleoprotein expressed in and purified from insect cells is efficacious as a vaccine. Proc. Natl. Acad. Sci. USA 1991, 88, 2001–2005. [Google Scholar] [CrossRef]
- Koser, M.L.; McGettigan, J.P.; Tan, G.S.; Smith, M.E.; Koprowski, H.; Dietzschold, B.; Schnell, M.J. Rabies virus nucleoprotein as a carrier for foreign antigens. Proc. Natl. Acad. Sci. USA 2004, 101, 9405–9410. [Google Scholar] [CrossRef] [PubMed]
- Masatani, T.; Ito, N.; Ito, Y.; Nakagawa, K.; Abe, M.; Yamaoka, S.; Okadera, K.; Sugiyama, M. Importance of rabies virus nucleoprotein in viral evasion of interferon response in the brain. Microbiol. Immunol. 2013, 57, 511–517. [Google Scholar] [CrossRef]
- Masatani, T.; Ito, N.; Shimizu, K.; Ito, Y.; Nakagawa, K.; Abe, M.; Yamaoka, S.; Sugiyama, M. Amino acids at positions 273 and 394 in rabies virus nucleoprotein are important for both evasion of host rig-i-mediated antiviral response and pathogenicity. Virus Res. 2011, 155, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Masatani, T.; Ito, N.; Shimizu, K.; Ito, Y.; Nakagawa, K.; Sawaki, Y.; Koyama, H.; Sugiyama, M. Rabies virus nucleoprotein functions to evade activation of the rig-i-mediated antiviral response. J. Virol. 2010, 84, 4002–4012. [Google Scholar] [CrossRef]
- Wu, X.; Rupprecht, C.E. Glycoprotein gene relocation in rabies virus. Virus Res. 2008, 131, 95–99. [Google Scholar] [CrossRef]
- Brzozka, K.; Finke, S.; Conzelmann, K.K. Identification of the rabies virus alpha/beta interferon antagonist: Phosphoprotein p interferes with phosphorylation of interferon regulatory factor 3. J. Virol. 2005, 79, 7673–7681. [Google Scholar] [CrossRef] [PubMed]
- Marschalek, A.; Finke, S.; Schwemmle, M.; Mayer, D.; Heimrich, B.; Stitz, L.; Conzelmann, K.K. Attenuation of rabies virus replication and virulence by picornavirus internal ribosome entry site elements. J. Virol. 2009, 83, 1911–1919. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, K.; Kawai, A.; Sato, Y.; Ohkubo, A. A unique transcription mode of rabies virus high egg passage-flury strain detected in infected baby hamster kidney-21 cells. Microbiol. Immunol. 2011, 55, 558–564. [Google Scholar] [CrossRef] [PubMed]
- Mei, M.; Long, T.; Zhang, Q.; Zhao, J.; Tian, Q.; Peng, J.; Luo, J.; Wang, Y.; Lin, Y.; Guo, X. Phenotypic consequences in vivo and in vitro of rearranging the p gene of rabv hep-flury. Front. Microbiol. 2017, 8, 120. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yang, X.F.; Peng, J.J.; Liang, H.R.; Yang, Y.T.; Wang, Y.F.; Wu, X.W.; Pan, J.J.; Luo, Y.W.; Guo, X.F. Gene order rearrangement of the m gene in the rabies virus leads to slower replication. Virus Dis. 2014, 25, 365–371. [Google Scholar] [CrossRef]
- Inoue, K.; Shoji, Y.; Kurane, I.; Iijima, T.; Sakai, T.; Morimoto, K. An improved method for recovering rabies virus from cloned cdna. J. Virol. Methods 2003, 107, 229–236. [Google Scholar] [CrossRef]
- National Research Council (US). Committee for the Update of the Guide for the Care and Use of Laboratory Animals. In Guide for the Care and Use of Laboratory Animals, 8th ed.; National Academies Press (US): Washington, DC, USA, 2011. [Google Scholar]
- Luo, J.; Zhao, J.; Tian, Q.; Mo, W.; Wang, Y.; Chen, H.; Guo, X. A recombinant rabies virus carrying gfp between n and p affects viral transcription in vitro. Virus Genes 2016, 52, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liu, W.; Yan, G.; Luo, Y.; Zhao, J.; Yang, X.; Mei, M.; Wu, X.; Guo, X. Itraq protein profile analysis of neuroblastoma (na) cells infected with the rabies viruses rhep-flury and hep-dg. Front. Microbiol. 2015, 6, 691. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peng, J.; Zhu, S.; Hu, L.; Ye, P.; Wang, Y.; Tian, Q.; Mei, M.; Chen, H.; Guo, X. Wild-type rabies virus induces autophagy in human and mouse neuroblastoma cell lines. Autophagy 2016, 12, 1704–1720. [Google Scholar] [CrossRef]
- Wang, Y.; Tian, Q.; Xu, X.; Yang, X.; Luo, J.; Mo, W.; Peng, J.; Niu, X.; Luo, Y.; Guo, X. Recombinant rabies virus expressing ifnalpha1 enhanced immune responses resulting in its attenuation and stronger immunogenicity. Virology 2014, 468–470, 621–630. [Google Scholar] [CrossRef][Green Version]
- Wirblich, C.; Schnell, M.J. Rabies virus (rv) glycoprotein expression levels are not critical for pathogenicity of rv. J. Virol. 2011, 85, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Takayama-Ito, M.; Inoue, K.; Shoji, Y.; Inoue, S.; Iijima, T.; Sakai, T.; Kurane, I.; Morimoto, K. A highly attenuated rabies virus hep-flury strain reverts to virulent by single amino acid substitution to arginine at position 333 in glycoprotein. Virus Res. 2006, 119, 208–215. [Google Scholar] [CrossRef]
- Arnheiter, H.; Davis, N.L.; Wertz, G.; Schubert, M.; Lazzarini, R.A. Role of the nucleocapsid protein in regulating vesicular stomatitis virus rna synthesis. Cell 1985, 41, 259–267. [Google Scholar] [CrossRef]
- Patton, J.T.; Davis, N.L.; Wertz, G.W. N protein alone satisfies the requirement for protein synthesis during rna replication of vesicular stomatitis virus. J. Virol. 1984, 49, 303–309. [Google Scholar] [PubMed]
- Finke, S.; Conzelmann, K.K. Dissociation of rabies virus matrix protein functions in regulation of viral rna synthesis and virus assembly. J. Virol. 2003, 77, 12074–12082. [Google Scholar] [CrossRef] [PubMed]
- Okumura, A.; Harty, R.N. Rabies virus assembly and budding. Adv. Virus Res. 2011, 79, 23–32. [Google Scholar]
- Novella, I.S.; Ball, L.A.; Wertz, G.W. Fitness analyses of vesicular stomatitis strains with rearranged genomes reveal replicative disadvantages. J. Virol. 2004, 78, 9837–9841. [Google Scholar] [CrossRef]
- Novella, I.S.; Ebendick-Corpus, B.E. Molecular basis of fitness loss and fitness recovery in vesicular stomatitis virus. J. Mol. Biol. 2004, 342, 1423–1430. [Google Scholar] [CrossRef]
- Dietzschold, B.; Li, J.; Faber, M.; Schnell, M. Concepts in the pathogenesis of rabies. Future Virol. 2008, 3, 481–490. [Google Scholar] [CrossRef]
- Ohara, S.; Sato, S.; Oyama, K.; Tsutsui, K.; Iijima, T. Rabies virus vector transgene expression level and cytotoxicity improvement induced by deletion of glycoprotein gene. PLoS ONE 2013, 8, e80245. [Google Scholar] [CrossRef]
- Faber, M.; Pulmanausahakul, R.; Hodawadekar, S.S.; Spitsin, S.; McGettigan, J.P.; Schnell, M.J.; Dietzschold, B. Overexpression of the rabies virus glycoprotein results in enhancement of apoptosis and antiviral immune response. J. Virol. 2002, 76, 3374–3381. [Google Scholar] [CrossRef] [PubMed]
- Finke, S.; Conzelmann, K.K. Replication strategies of rabies virus. Virus Res. 2005, 111, 120–131. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Yang, D.K.; Kim, H.H.; Jo, H.Y.; Choi, S.S.; Kim, J.T.; Cho, I.S.; Kim, H.W. Application of recombinant adenoviruses expressing glycoprotein or nucleoprotein of rabies virus to korean raccoon dogs. Clin. Exp. Vaccine Res. 2015, 4, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Kurilla, M.G.; Cabradilla, C.D.; Holloway, B.P.; Keene, J.D. Nucleotide sequence and host la protein interactions of rabies virus leader rna. J. Virol. 1984, 50, 773–778. [Google Scholar]
- Zhang, R.; Liu, C.; Cao, Y.; Jamal, M.; Chen, X.; Zheng, J.; Li, L.; You, J.; Zhu, Q.; Liu, S.; et al. Rabies viruses leader rna interacts with host hsc70 and inhibits virus replication. Oncotarget 2017, 8, 43822–43837. [Google Scholar] [CrossRef] [PubMed]
- Bauer, A.; Nolden, T.; Nemitz, S.; Perlson, E.; Finke, S. A dynein light chain 1 binding motif in rabies virus polymerase l protein plays a role in microtubule reorganization and viral primary transcription. J. Virol. 2015, 89, 9591–9600. [Google Scholar] [CrossRef]
- Ohara, S.; Sota, Y.; Sato, S.; Tsutsui, K.I.; Iijima, T. Increased transgene expression level of rabies virus vector for transsynaptic tracing. PLoS ONE 2017, 12, e0180960. [Google Scholar] [CrossRef][Green Version]
- Liu, X.; Yang, Y.; Sun, Z.; Chen, J.; Ai, J.; Dun, C.; Fu, Z.F.; Niu, X.; Guo, X. A recombinant rabies virus encoding two copies of the glycoprotein gene confers protection in dogs against a virulent challenge. PLoS ONE 2014, 9, e87105. [Google Scholar] [CrossRef] [PubMed]
- Lay, S.; Prehaud, C.; Dietzschold, B.; Lafon, M. Glycoprotein of nonpathogenic rabies viruses is a major inducer of apoptosis in human jurkat t cells. Ann. N. Y. Acad. Sci. 2003, 1010, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Sarmento, L.; Li, X.Q.; Howerth, E.; Jackson, A.C.; Fu, Z.F. Glycoprotein-mediated induction of apoptosis limits the spread of attenuated rabies viruses in the central nervous system of mice. J. Neurovirol. 2005, 11, 571–581. [Google Scholar] [CrossRef]
- Sarmento, L.; Tseggai, T.; Dhingra, V.; Fu, Z.F. Rabies virus-induced apoptosis involves caspase-dependent and caspase-independent pathways. Virus Res. 2006, 121, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Davis, B.M.; Fensterl, V.; Lawrence, T.M.; Hudacek, A.W.; Sen, G.C.; Schnell, M.J. Ifit2 is a restriction factor in rabies virus pathogenicity. J. Virol. 2017, 91. [Google Scholar] [CrossRef]
- Kuang, Y.; Lackay, S.N.; Zhao, L.; Fu, Z.F. Role of chemokines in the enhancement of bbb permeability and inflammatory infiltration after rabies virus infection. Virus Res. 2009, 144, 18–26. [Google Scholar] [CrossRef]
- Niu, X.; Tang, L.; Tseggai, T.; Guo, Y.; Fu, Z.F. Wild-type rabies virus phosphoprotein is associated with viral sensitivity to type i interferon treatment. Arch. Virol. 2013, 158, 2297–2305. [Google Scholar] [CrossRef] [PubMed]
- Kassis, R.; Larrous, F.; Estaquier, J.; Bourhy, H. Lyssavirus matrix protein induces apoptosis by a trail-dependent mechanism involving caspase-8 activation. J. Virol. 2004, 78, 6543–6555. [Google Scholar] [CrossRef]
- Prehaud, C.; Lay, S.; Dietzschold, B.; Lafon, M. Glycoprotein of nonpathogenic rabies viruses is a key determinant of human cell apoptosis. J. Virol. 2003, 77, 10537–10547. [Google Scholar] [CrossRef] [PubMed]
- Thoulouze, M.I.; Lafage, M.; Yuste, V.J.; Baloul, L.; Edelman, L.; Kroemer, G.; Israel, N.; Susin, S.A.; Lafon, M. High level of bcl-2 counteracts apoptosis mediated by a live rabies virus vaccine strain and induces long-term infection. Virology 2003, 314, 549–561. [Google Scholar] [CrossRef]
- Jackson, A.C.; Rasalingam, P.; Weli, S.C. Comparative pathogenesis of recombinant rabies vaccine strain sad-l16 and sad-d29 with replacement of arg333 in the glycoprotein after peripheral inoculation of neonatal mice: Less neurovirulent strain is a stronger inducer of neuronal apoptosis. Acta Neuropathol. 2006, 111, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Kammouni, W.; Wood, H.; Saleh, A.; Appolinario, C.M.; Fernyhough, P.; Jackson, A.C. Rabies virus phosphoprotein interacts with mitochondrial complex i and induces mitochondrial dysfunction and oxidative stress. J. Neurovirol. 2015, 21, 370–382. [Google Scholar] [CrossRef] [PubMed]
| Primer Name | Sequence (5′–3′) | Use |
|---|---|---|
| 3-M-F | 5′-GATATGAAAAAAACTAACACCACTAATAAAATGAAC | Construction for N3 plasmid |
| 3-M-R | 5′-GTAGGGGTGTTGCCTGTTTTTTTCACATCCAAGAGG | |
| 3-N-F | 5′-AGGCAACACCCCTACAATGGATGCCGACAAG | |
| 3-N-R | 5′-TGAGGGATGTTAATAGTTTTTTTCATGATGGATATAC | |
| 4-G-F | 5′-GTGAAAAAAACAGGCAACATCCCTCAAAAGACTTAAGGA | Construction for N4 plasmid |
| 4-G-R | 5′-GTAGGGGTGTTAATAGTTTTTTTCTCGACTGAAATGC | |
| 4-N-F | 5′-TATTAACACCCCTACAATGGATGCCGAC | |
| 4-N-R | 5′-GTTCTTTTGGTATACAGTTTTTTTCATGATGGATATAC |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mei, M.; Long, T.; Zhang, Q.; Zhao, J.; Tian, Q.; Peng, J.; Luo, J.; Jiang, H.; Lin, Y.; Lin, Z.; et al. Phenotypic Consequence of Rearranging the N Gene of RABV HEP-Flury. Viruses 2019, 11, 402. https://doi.org/10.3390/v11050402
Mei M, Long T, Zhang Q, Zhao J, Tian Q, Peng J, Luo J, Jiang H, Lin Y, Lin Z, et al. Phenotypic Consequence of Rearranging the N Gene of RABV HEP-Flury. Viruses. 2019; 11(5):402. https://doi.org/10.3390/v11050402
Chicago/Turabian StyleMei, Mingzhu, Teng Long, Qiong Zhang, Jing Zhao, Qin Tian, Jiaojiao Peng, Jun Luo, He Jiang, Yingyi Lin, Zhixiong Lin, and et al. 2019. "Phenotypic Consequence of Rearranging the N Gene of RABV HEP-Flury" Viruses 11, no. 5: 402. https://doi.org/10.3390/v11050402
APA StyleMei, M., Long, T., Zhang, Q., Zhao, J., Tian, Q., Peng, J., Luo, J., Jiang, H., Lin, Y., Lin, Z., & Guo, X. (2019). Phenotypic Consequence of Rearranging the N Gene of RABV HEP-Flury. Viruses, 11(5), 402. https://doi.org/10.3390/v11050402





