Removal of the N-Glycosylation Sequon at Position N116 Located in p27 of the Respiratory Syncytial Virus Fusion Protein Elicits Enhanced Antibody Responses after DNA Immunization
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells, Virus and Antibodies
2.2. Construction and Expression of Recombinant RSV F Proteins
2.3. Western Blot Analysis
2.4. Immunofluorescence Analysis of Surface Expression
2.5. Flow Cytometric Analysis
2.6. Fusion Assay
2.7. Immunization of Mice with Plasmid DNA and RSV Challenge
2.8. Antibody Responses and Neutralization Assay
2.9. Determination of Lung Viral Titre by qRT-PCR
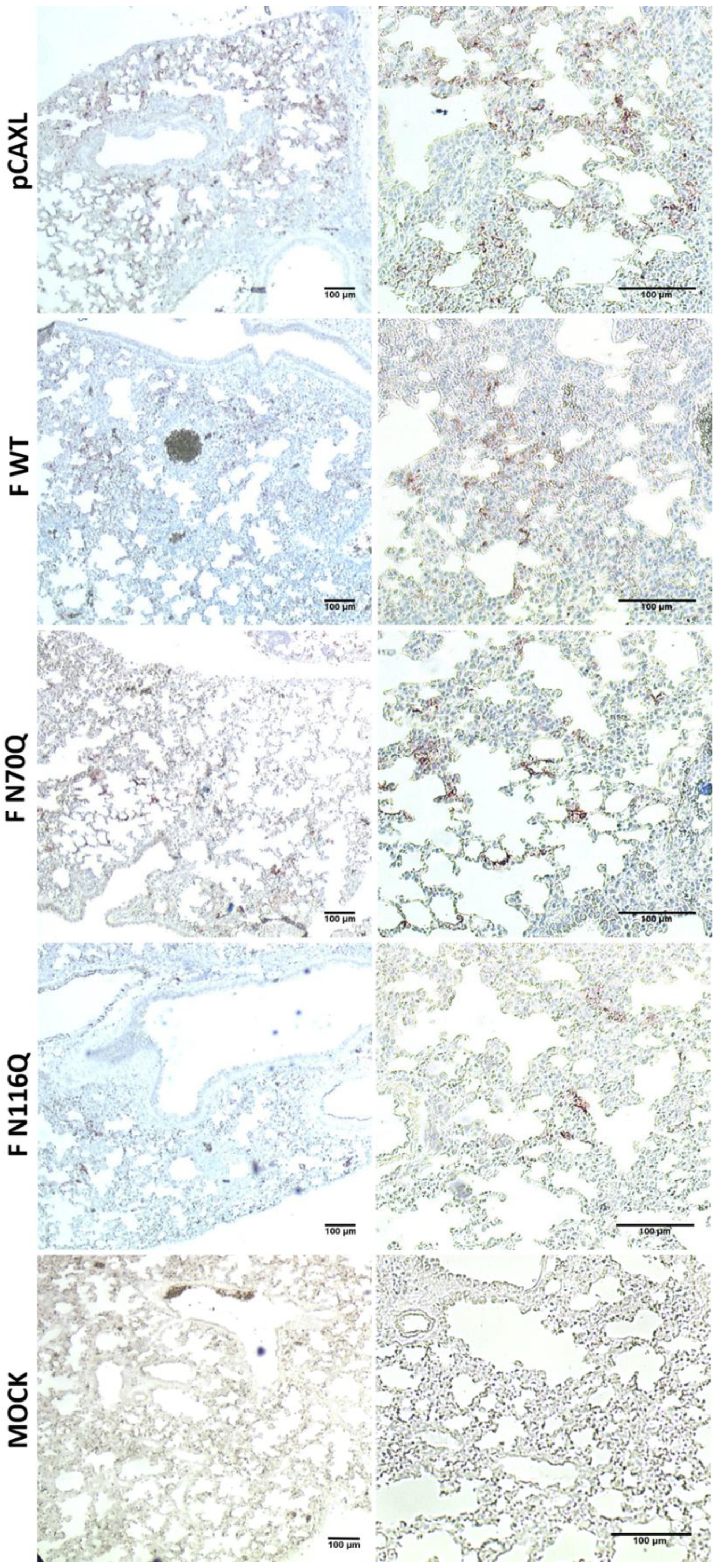
2.10. Immunohistochemistry
2.11. Statistical Analysis
3. Results
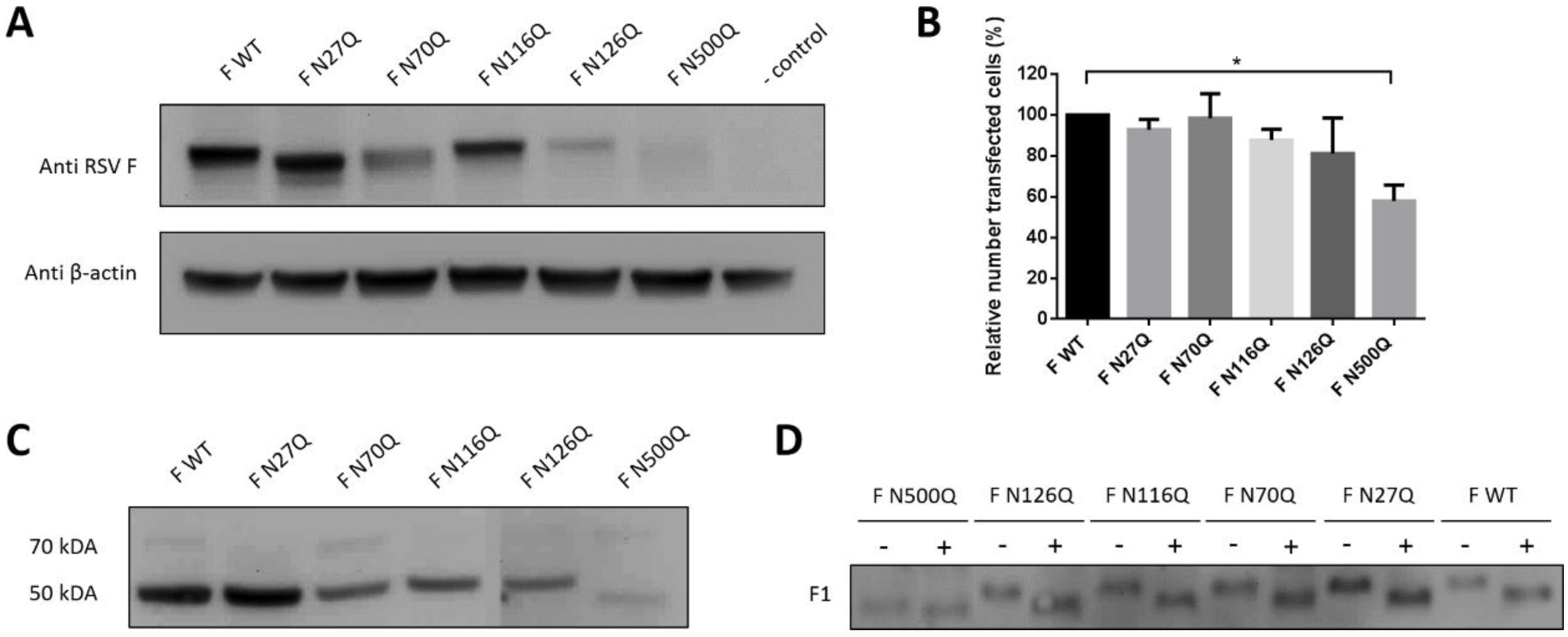
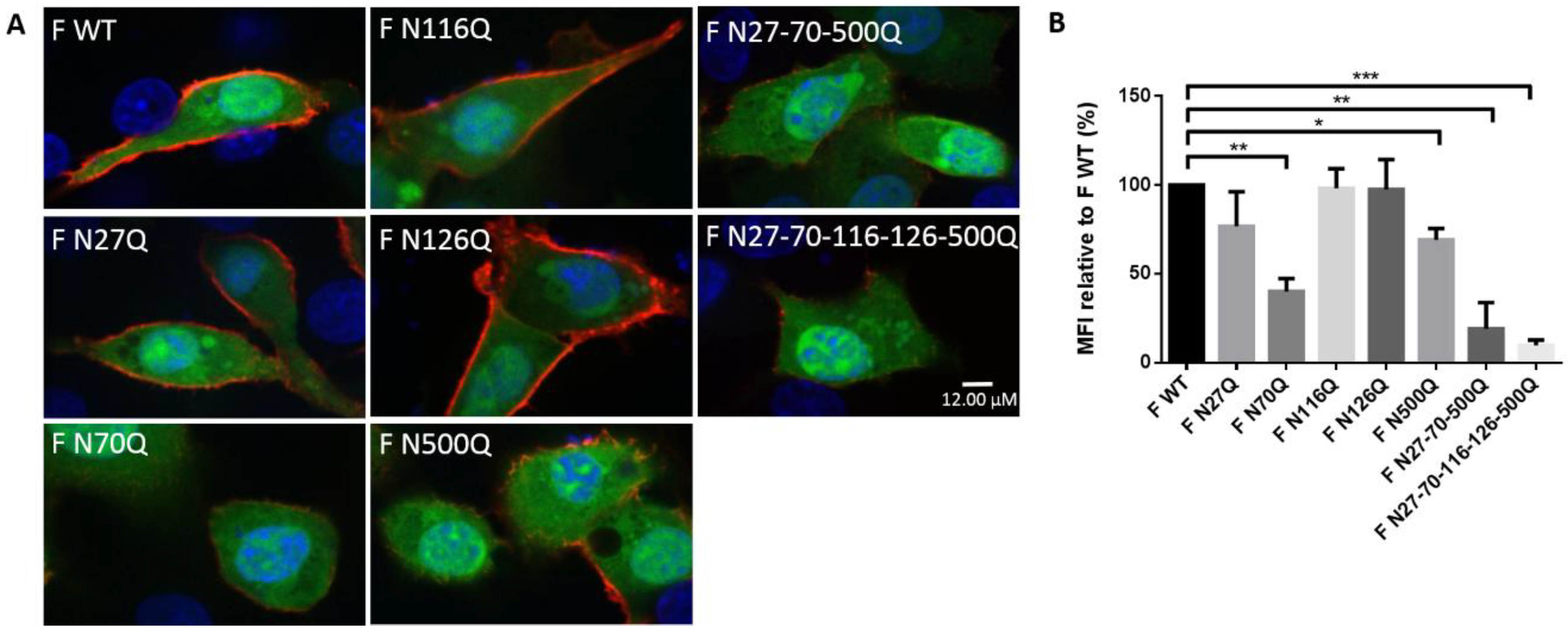
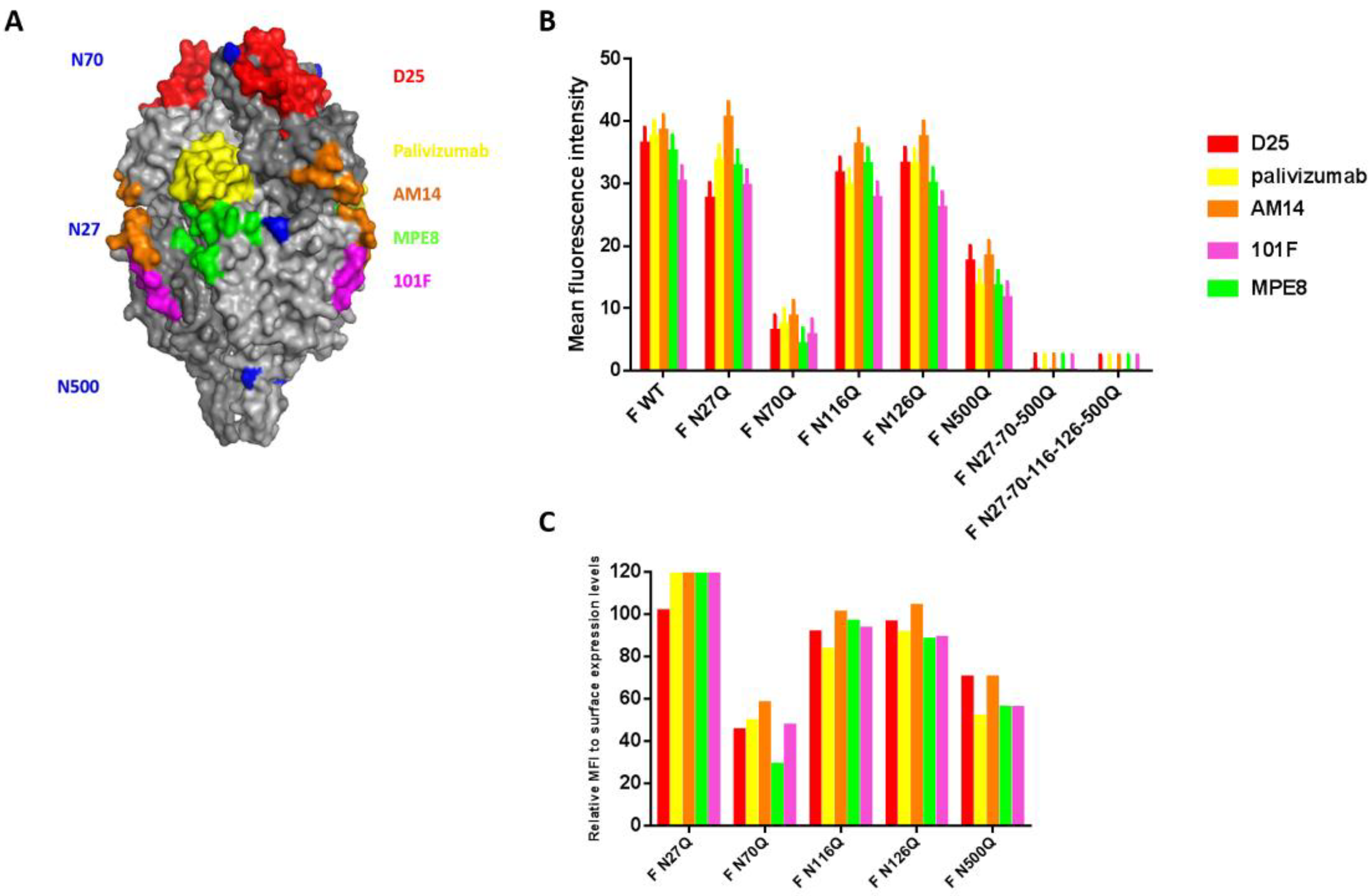
3.1. Expression Analysis of the RSV F Glycomutants and the Effect of N-Sequon Removal on RSV F-Specific mAb Recognition
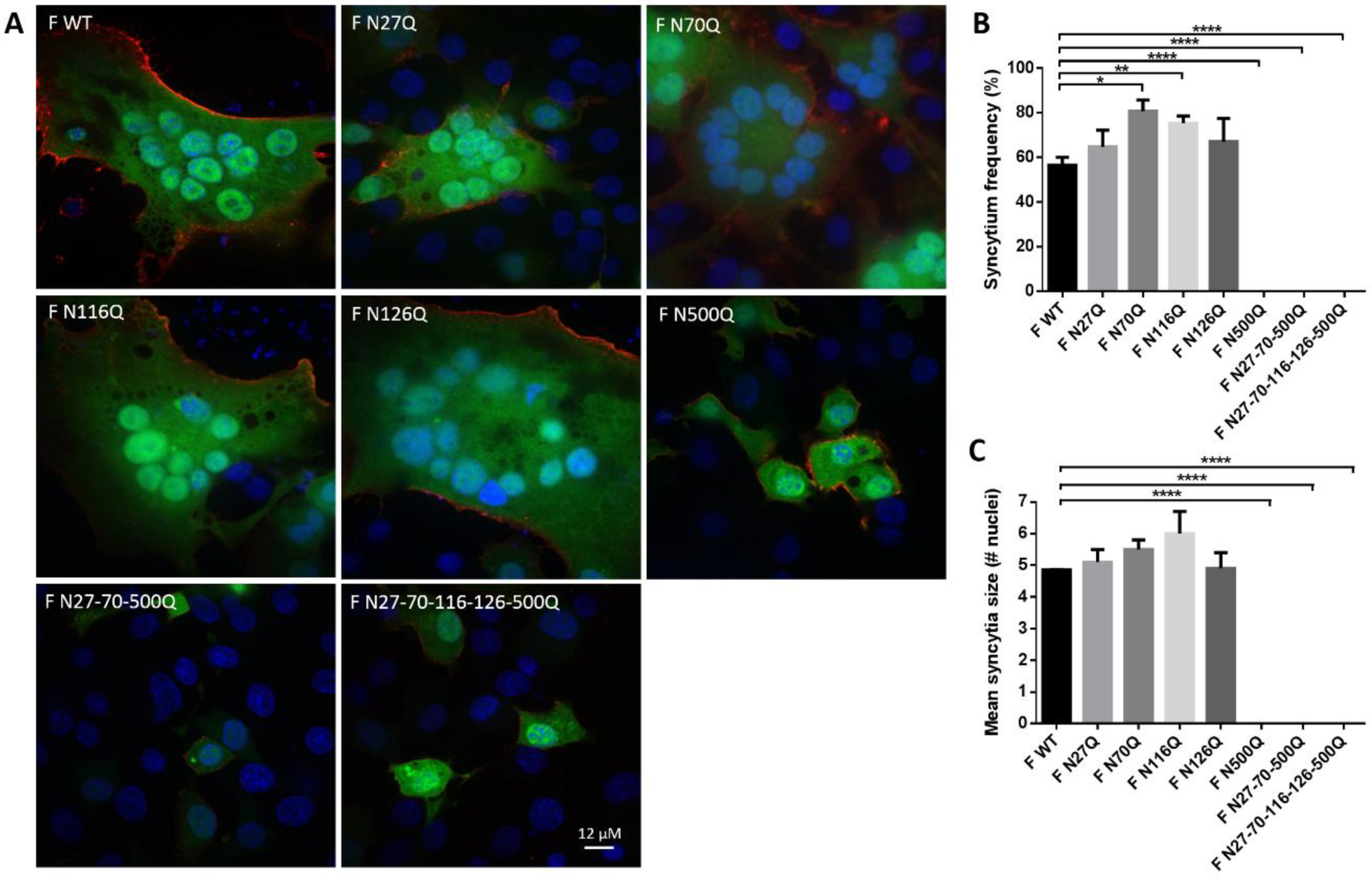
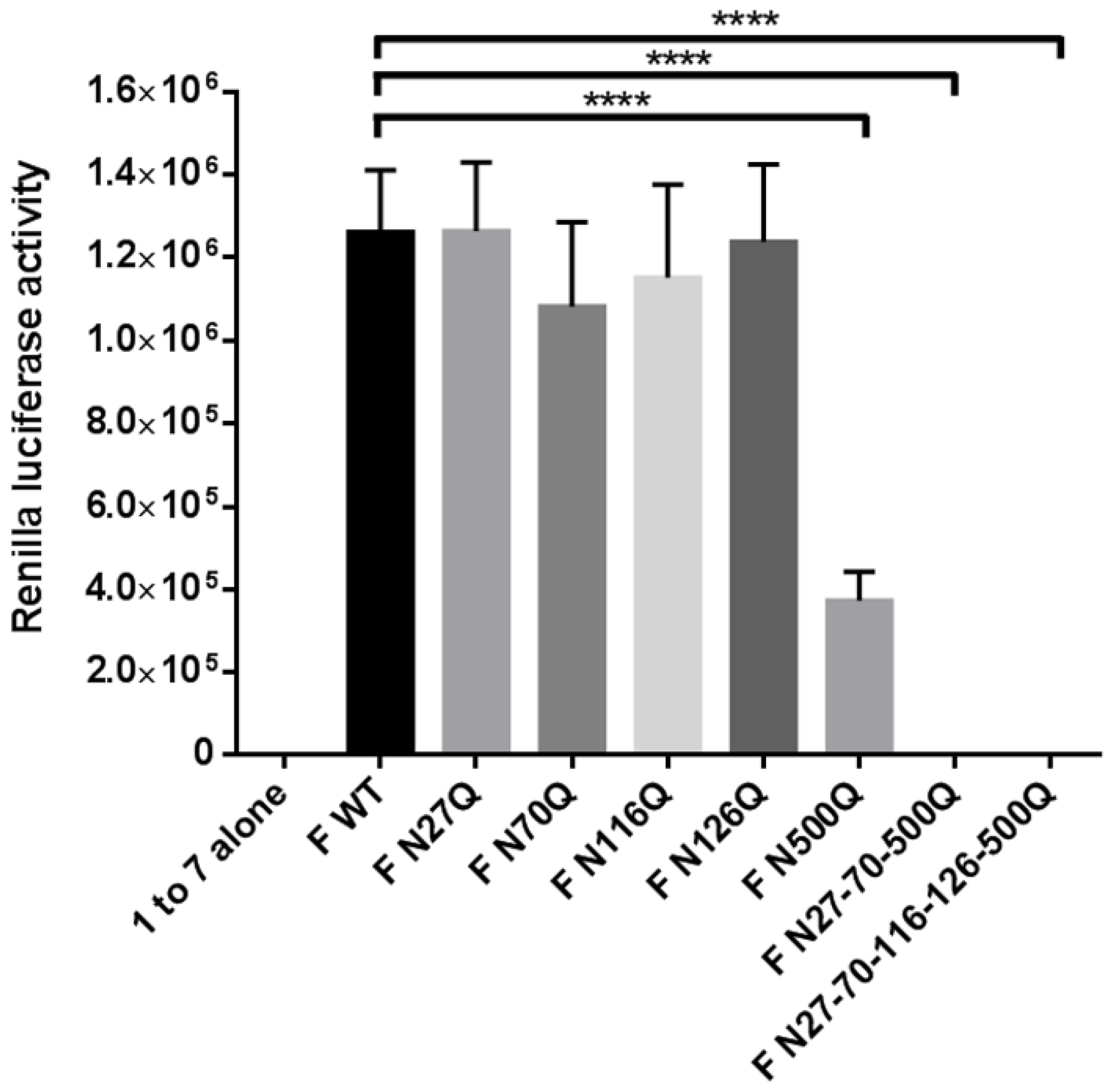
3.2. RSV F Fusion Activity Is Determined by the N-Glycan at Position N500
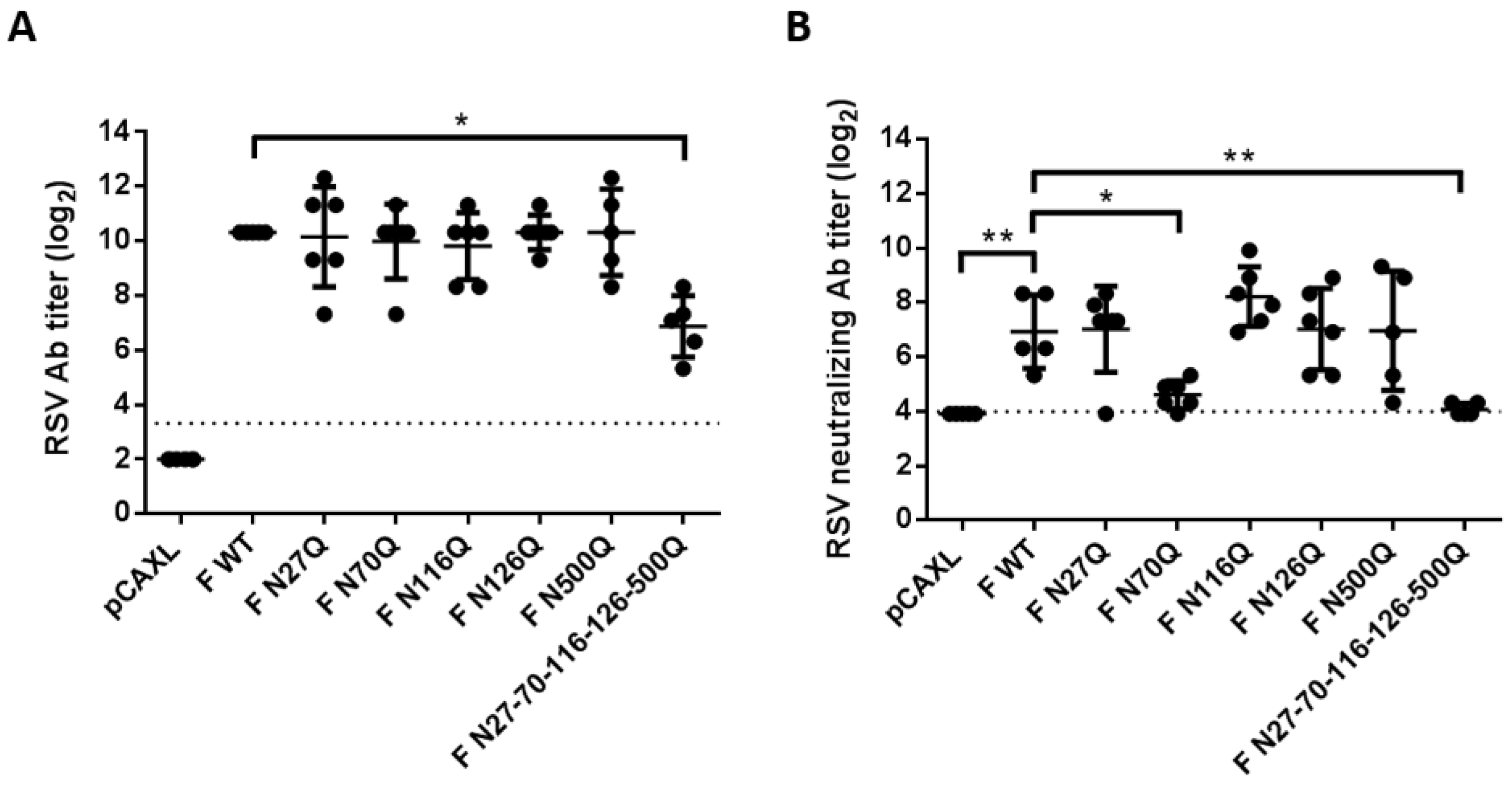
3.3. Effect of Loss of RSV F N-Glycosylation Sites on Antibody Responses
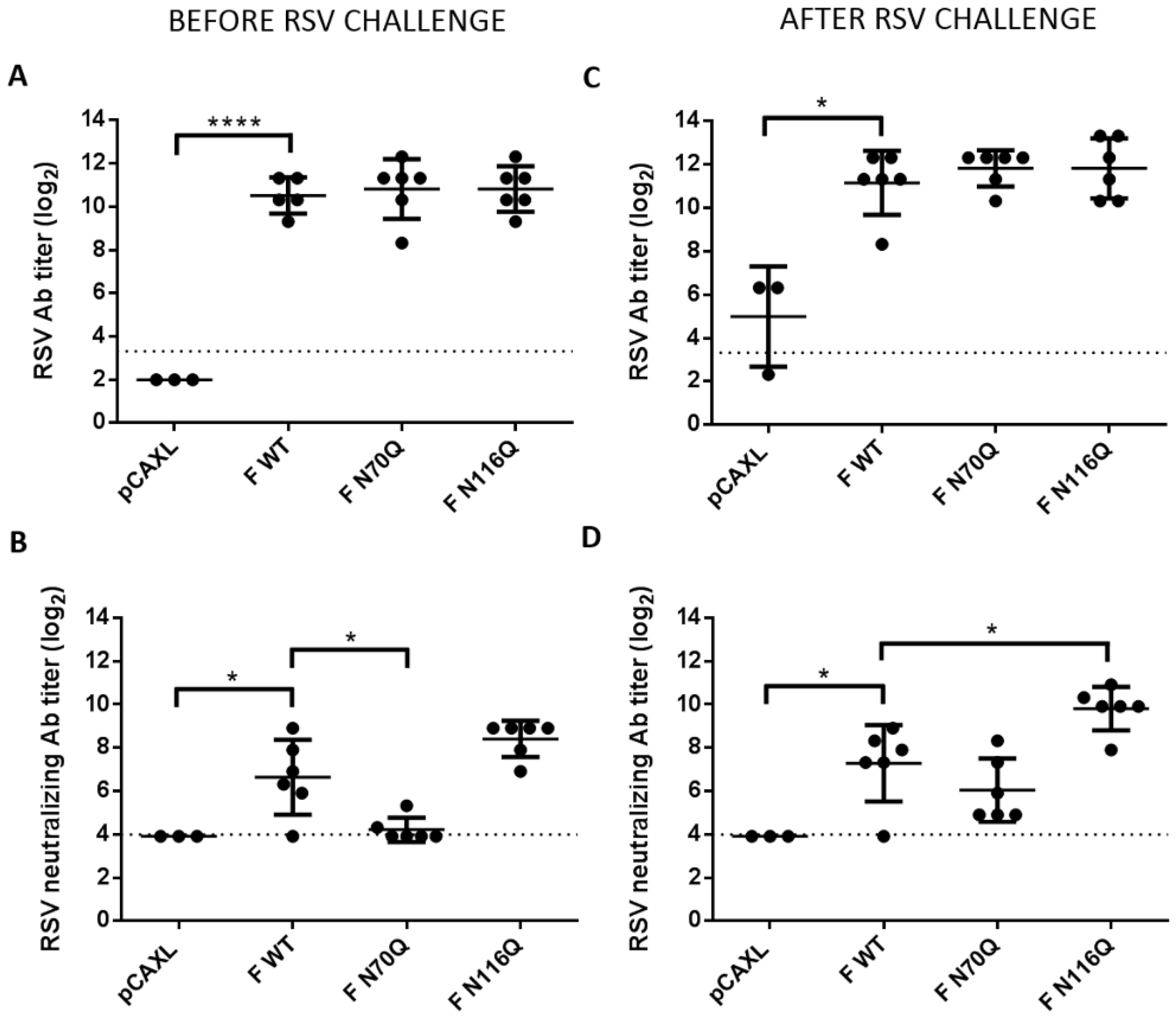
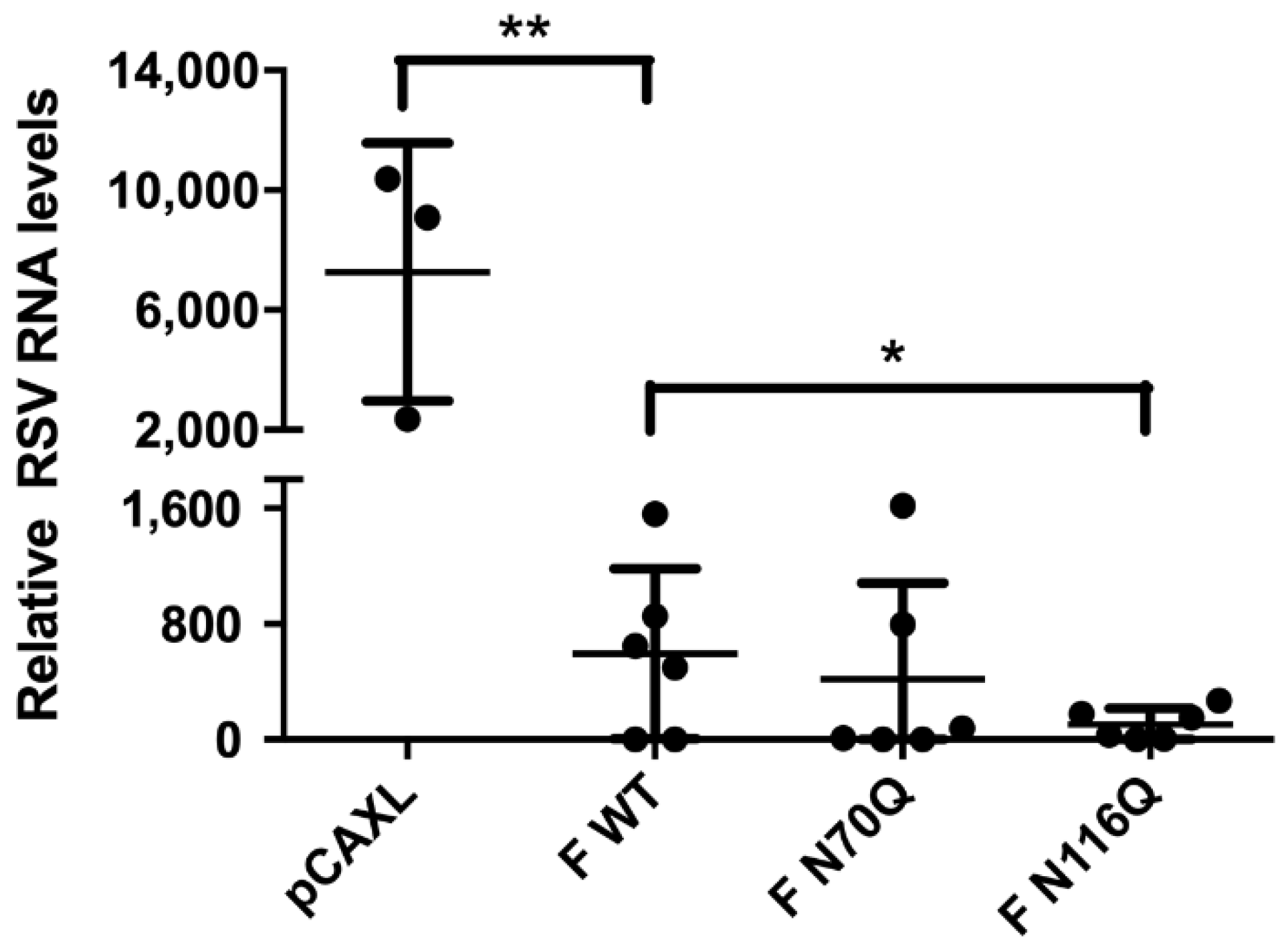
3.4. Immunization with F N116Q DNA Results in Enhanced Neutralizing Antibody Responses and Protection upon Challenge
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Borchers, A.T.; Chang, C.; Gershwin, M.E.; Gershwin, L.J. Respiratory Syncytial Virus—A Comprehensive Review. Clin. Rev. Allergy Immunol. 2013, 45, 331–379. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.L.; Graham, B.S. Viral and Host Factors in Human Respiratory Syncytial Virus Pathogenesis. J. Virol. 2008, 82, 2040–2055. [Google Scholar] [CrossRef] [PubMed]
- Nair, H.; Nokes, D.J.; Gessner, B.D.; Dherani, M.; Madhi, S.A.; Singleton, R.J.; O’Brien, K.L.; Roca, A.; Wright, P.F.; Bruce, N.; et al. Global Burden of Acute Lower Respiratory Infections Due to Respiratory Syncytial Virus in Young Children: A Systematic Review and Meta-Analysis. Lancet 2010, 375, 1545–1555. [Google Scholar] [CrossRef]
- Afonso, C.L.; Amarasinghe, G.K.; Banyai, K.; Bao, Y.; Basler, C.F.; Bavari, S.; Bejerman, N.; Blasdell, K.R.; Briand, F.X.; Briese, T.; et al. Taxonomy of the Order Mononegavirales: Update 2016. Arch. Virol. 2016, 161, 2351–2360. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Barreno, B.; Palomo, C.; Penas, C.; Delgado, T.; Perez-Brena, P.; Melero, J.A. Marked Differences in the Antigenic Structure of Human Respiratory Syncytial Virus F and G Glycoproteins. J. Virol. 1989, 63, 925–932. [Google Scholar] [PubMed]
- Karron, R.A.; Buonagurio, D.A.; Georgiu, A.F.; Whitehead, S.S.; Adamus, J.E.; Clements-Mann, M.L.; Harris, D.O.; Randolph, V.B.; Udem, S.A.; Murphy, B.R.; et al. Respiratory Syncytial Virus (RSV) Sh and G Proteins Are Not Essential for Viral Replication in Vitro: Clinical Evaluation and Molecular Characterization of a Cold-Passaged, Attenuated Rsv Subgroup B Mutant. Proc. Natl. Acad. Sci. USA 1997, 94, 13961–13966. [Google Scholar] [CrossRef] [PubMed]
- Ngwuta, J.O.; Chen, M.; Modjarrad, K.; Joyce, M.G.; Kanekiyo, M.; Kumar, A.; Yassine, H.M.; Moin, S.M.; Killikelly, A.M.; Chuang, G.Y.; et al. Prefusion F-Specific Antibodies Determine the Magnitude of Rsv Neutralizing Activity in Human Sera. Sci. Transl. Med. 2015, 7, 309ra162. [Google Scholar] [CrossRef] [PubMed]
- The Impact-Rsv Study Group. Palivizumab, a Humanized Respiratory Syncytial Virus Monoclonal Antibody, Reduces Hospitalization from Respiratory Syncytial Virus Infection in High-Risk Infants. Pediatrics 1998, 102, 531–537. [Google Scholar] [CrossRef]
- Homaira, N.; Rawlinson, W.; Snelling, T.L.; Jaffe, A. Effectiveness of Palivizumab in Preventing RSV Hospitalization in High Risk Children: A Real-World Perspective. Int. J. Pediatr. 2014, 2014, 571609. [Google Scholar] [CrossRef] [PubMed]
- Neuzil, K.M. Progress toward a Respiratory Syncytial Virus Vaccine. Clin. Vaccine Immunol. 2016, 23, 186–188. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.L.; Mottet, G. Post-Translational Processing and Oligomerization of the Fusion Glycoprotein of Human Respiratory Syncytial Virus. J. Gen. Virol. 1991, 72, 3095–3101. [Google Scholar] [CrossRef] [PubMed]
- Sugrue, R.J.; Brown, C.; Brown, G.; Aitken, J.; Mc, L.R.H.W. Furin Cleavage of the Respiratory Syncytial Virus Fusion Protein is Not a Requirement for Its Transport to the Surface of Virus-Infected Cells. J. Gen. Virol. 2001, 82, 1375–1386. [Google Scholar] [CrossRef] [PubMed]
- Cash, P.; Pringle, C.R.; Preston, C.M. The Polypeptides of Human Respiratory Syncytial Virus: Products of Cell-Free Protein Synthesis and Post-Translational Modifications. Virology 1979, 92, 375–384. [Google Scholar] [CrossRef]
- Kornfeld, R.; Kornfeld, S. Assembly of Asparagine-Linked Oligosaccharides. Annu. Rev. Biochem. 1985, 54, 631–664. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, G.; Trotz, I.; Herrler, G. N-Glycans of F Protein Differentially Affect Fusion Activity of Human Respiratory Syncytial Virus. J. Virol. 2001, 75, 4744–4751. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Reyes, L.; Ruiz-Arguello, M.B.; Garcia-Barreno, B.; Calder, L.; Lopez, J.A.; Albar, J.P.; Skehel, J.J.; Wiley, D.C.; Melero, J.A. Cleavage of the Human Respiratory Syncytial Virus Fusion Protein at Two Distinct Sites Is Required for Activation of Membrane Fusion. Proc. Natl. Acad. Sci. USA 2001, 98, 9859–9864. [Google Scholar] [CrossRef] [PubMed]
- Ellgaard, L.; McCaul, N.; Chatsisvili, A.; Braakman, I. Co- and Post-Translational Protein Folding in the Er. Traffic 2016, 17, 615–638. [Google Scholar] [CrossRef] [PubMed]
- Vigerust, D.J.; Shepherd, V.L. Virus Glycosylation: Role in Virulence and Immune Interactions. Trends Microbiol. 2007, 15, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Doms, R.W.; Lamb, R.A.; Rose, J.K.; Helenius, A. Folding and Assembly of Viral Membrane Proteins. Virology 1993, 193, 545–562. [Google Scholar] [CrossRef] [PubMed]
- Wagner, R.; Wolff, T.; Herwig, A.; Pleschka, S.; Klenk, H.D. Interdependence of Hemagglutinin Glycosylation and Neuraminidase as Regulators of Influenza Virus Growth: A Study by Reverse Genetics. J. Virol. 2000, 74, 6316–6323. [Google Scholar] [CrossRef] [PubMed]
- Beyene, A.; Basu, A.; Meyer, K.; Ray, R. Influence of N-Linked Glycans on Intracellular Transport of Hepatitis C Virus E1 Chimeric Glycoprotein and Its Role in Pseudotype Virus Infectivity. Virology 2004, 324, 273–285. [Google Scholar] [CrossRef] [PubMed]
- Chu, F.L.; Wen, H.L.; Hou, G.H.; Lin, B.; Zhang, W.Q.; Song, Y.Y.; Ren, G.J.; Sun, C.X.; Li, Z.M.; Wang, Z. Role of N-Linked Glycosylation of the Human Parainfluenza Virus Type 3 Hemagglutinin-Neuraminidase Protein. Virus Res. 2013, 174, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Mc, L.R.H.W.; Brown, G.; Sugrue, R.J. Functional Analysis of the N-Linked Glycans within the Fusion Protein of Respiratory Syncytial Virus. Methods Mol. Biol. 2007, 379, 69–83. [Google Scholar] [PubMed]
- Klink, H.A.; Brady, R.P.; Topliff, C.L.; Eskridge, K.M.; Srikumaran, S.; Kelling, C.L. Influence of Bovine Respiratory Syncytial Virus F Glycoprotein N-Linked Glycans on in Vitro Expression and on Antibody Responses in Balb/C Mice. Vaccine 2006, 24, 3388–3395. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, M.; Chen, H.; Luo, F.; Li, P.; Pan, Q.; Xia, B.; Qi, Z.; Ho, W.Z.; Zhang, X.L. Deletion of N-Glycosylation Sites of Hepatitis C Virus Envelope Protein E1 Enhances Specific Cellular and Humoral Immune Responses. Vaccine 2007, 25, 6572–6580. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.C.; Chen, J.R.; Tseng, Y.C.; Hsu, C.H.; Hung, Y.F.; Chen, S.W.; Chen, C.M.; Khoo, K.H.; Cheng, T.J.; Cheng, Y.S.; et al. Glycans on Influenza Hemagglutinin Affect Receptor Binding and Immune Response. Proc. Natl. Acad. Sci. USA 2009, 106, 18137–18142. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, P.; Cao, R.; Gu, J. Mutation of Putative N-Linked Glycosylation Sites in Japanese Encephalitis Virus Premembrane and Envelope Proteins Enhances Humoral Immunity in Balb/C Mice after DNA Vaccination. Virol. J. 2011, 8, 138. [Google Scholar] [CrossRef] [PubMed]
- Reynard, F.; Willkomm, N.; Fatmi, A.; Vallon-Eberhard, A.; Verrier, B.; Bedin, F. Characterization of the Antibody Response Elicited by Hiv-1 Env Glycomutants in Rabbits. Vaccine 2007, 25, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Dowling, W.; Thompson, E.; Badger, C.; Mellquist, J.L.; Garrison, A.R.; Smith, J.M.; Paragas, J.; Hogan, R.J.; Schmaljohn, C. Influences of Glycosylation on Antigenicity, Immunogenicity, and Protective Efficacy of Ebola Virus Gp DNA Vaccines. J. Virol. 2007, 81, 1821–1837. [Google Scholar] [CrossRef] [PubMed]
- Pancera, M.; Zhou, T.; Druz, A.; Georgiev, I.S.; Soto, C.; Gorman, J.; Huang, J.; Acharya, P.; Chuang, G.Y.; Ofek, G.; et al. Structure and Immune Recognition of Trimeric Pre-Fusion HIV-1 Env. Nature 2014, 514, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Whiteman, M.C.; Li, L.; Wicker, J.A.; Kinney, R.M.; Huang, C.; Beasley, D.W.; Chung, K.M.; Diamond, M.S.; Solomon, T.; Barrett, A.D. Development and Characterization of Non-Glycosylated E and Ns1 Mutant Viruses as a Potential Candidate Vaccine for West Nile Virus. Vaccine 2010, 28, 1075–1083. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, C.; Watanabe, S.; Naruse, T.; Kajiwara, E.; Shiino, T.; Umano, N.; Ueda, K.; Sato, H.; Ohgimoto, S.; Hirsch, V.; et al. Protection of Macaques with Diverse Mhc Genotypes against a Heterologous Siv by Vaccination with a Deglycosylated Live-Attenuated Siv. PLoS ONE 2010, 5, e11678. [Google Scholar] [CrossRef] [PubMed]
- Hotard, A.L.; Shaikh, F.Y.; Lee, S.; Yan, D.; Teng, M.N.; Plemper, R.K.; Crowe, J.E., Jr.; Moore, M.L. A Stabilized Respiratory Syncytial Virus Reverse Genetics System Amenable to Recombination-Mediated Mutagenesis. Virology 2012, 434, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Meng, F.; Kondo, N.; Iwamoto, A.; Matsuda, Z. Generation of a Dual-Functional Split-Reporter Protein for Monitoring Membrane Fusion Using Self-Associating Split Gfp. Protein Eng. Des. Sel. 2012, 25, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Payne, R. Genstat Reference Manual (Release 18), Part 3 Procedures; VSN International: Hemel Hempstead, UK, 2015. [Google Scholar]
- McLellan, J.S.; Chen, M.; Leung, S.; Graepel, K.W.; Du, X.; Yang, Y.; Zhou, T.; Baxa, U.; Yasuda, E.; Beaumont, T.; et al. Structure of Rsv Fusion Glycoprotein Trimer Bound to a Prefusion-Specific Neutralizing Antibody. Science 2013, 340, 1113–1117. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Oliver, C.; Prince, G.A.; Hemming, V.G.; Pfarr, D.S.; Wang, S.C.; Dormitzer, M.; O’Grady, J.; Koenig, S.; Tamura, J.K.; et al. Development of a Humanized Monoclonal Antibody (Medi-493) with Potent in Vitro and in Vivo Activity against Respiratory Syncytial Virus. J. Infect. Dis. 1997, 176, 1215–1224. [Google Scholar] [CrossRef] [PubMed]
- Corti, D.; Bianchi, S.; Vanzetta, F.; Minola, A.; Perez, L.; Agatic, G.; Guarino, B.; Silacci, C.; Marcandalli, J.; Marsland, B.J.; et al. Cross-Neutralization of Four Paramyxoviruses by a Human Monoclonal Antibody. Nature 2013, 501, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Gilman, M.S.; Moin, S.M.; Mas, V.; Chen, M.; Patel, N.K.; Kramer, K.; Zhu, Q.; Kabeche, S.C.; Kumar, A.; Palomo, C.; et al. Characterization of a Prefusion-Specific Antibody That Recognizes a Quaternary, Cleavage-Dependent Epitope on the Rsv Fusion Glycoprotein. PLoS Pathog. 2015, 11, e1005035. [Google Scholar] [CrossRef] [PubMed]
- McLellan, J.S.; Chen, M.; Chang, J.S.; Yang, Y.; Kim, A.; Graham, B.S.; Kwong, P.D. Structure of a Major Antigenic Site on the Respiratory Syncytial Virus Fusion Glycoprotein in Complex with Neutralizing Antibody 101f. J. Virol. 2010, 84, 12236–12244. [Google Scholar] [CrossRef] [PubMed]
- Atanasiu, D.; Saw, W.T.; Gallagher, J.R.; Hannah, B.P.; Matsuda, Z.; Whitbeck, J.C.; Cohen, G.H.; Eisenberg, R.J. Dual Split Protein-Based Fusion Assay Reveals That Mutations to Herpes Simplex Virus (HSV) Glycoprotein Gb Alter the Kinetics of Cell-Cell Fusion Induced by HSV Entry Glycoproteins. J. Virol. 2013, 87, 11332–11345. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Meng, F.; Kondo, N.; Iwamoto, A.; Matsuda, Z. Conserved Arginine Residue in the Membrane-Spanning Domain of HIV-1 Gp41 Is Required for Efficient Membrane Fusion. Protein Cell 2011, 2, 369–376. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saw, W.T.; Matsuda, Z.; Eisenberg, R.J.; Cohen, G.H.; Atanasiu, D. Using a Split Luciferase Assay (SLA) to Measure the Kinetics of Cell-Cell Fusion Mediated by Herpes Simplex Virus Glycoproteins. Methods 2015, 90, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Hanna, S.L.; Pierson, T.C.; Sanchez, M.D.; Ahmed, A.A.; Murtadha, M.M.; Doms, R.W. N-Linked Glycosylation of West Nile Virus Envelope Proteins Influences Particle Assembly and Infectivity. J. Virol. 2005, 79, 13262–13274. [Google Scholar] [CrossRef] [PubMed]
- Lambert, D.M. Role of Oligosaccharides in the Structure and Function of Respiratory Syncytial Virus Glycoproteins. Virology 1988, 164, 458–466. [Google Scholar] [CrossRef]
- McDonald, T.P.; Jeffree, C.E.; Li, P.; Rixon, H.W.; Brown, G.; Aitken, J.D.; MacLellan, K.; Sugrue, R.J. Evidence That Maturation of the N-Linked Glycans of the Respiratory Syncytial Virus (RSV) Glycoproteins Is Required for Virus-Mediated Cell Fusion: The Effect of Alpha-Mannosidase Inhibitors on RSV Infectivity. Virology 2006, 350, 289–301. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.L.; Chi, M.H.; Luongo, C.; Lukacs, N.W.; Polosukhin, V.V.; Huckabee, M.M.; Newcomb, D.C.; Buchholz, U.J.; Crowe, J.E., Jr.; Goleniewska, K.; et al. A Chimeric A2 Strain of Respiratory Syncytial Virus (Rsv) with the Fusion Protein of RSV Strain Line 19 Exhibits Enhanced Viral Load, Mucus, and Airway Dysfunction. J. Virol. 2009, 83, 4185–4194. [Google Scholar] [CrossRef] [PubMed]
- Gavrilov, B.K.; Rogers, K.; Fernandez-Sainz, I.J.; Holinka, L.G.; Borca, M.V.; Risatti, G.R. Effects of Glycosylation on Antigenicity and Immunogenicity of Classical Swine Fever Virus Envelope Proteins. Virology 2011, 420, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Hutter, J.; Rodig, J.V.; Hoper, D.; Seeberger, P.H.; Reichl, U.; Rapp, E.; Lepenies, B. Toward Animal Cell Culture-Based Influenza Vaccine Design: Viral Hemagglutinin N-Glycosylation Markedly Impacts Immunogenicity. J. Immunol. 2013, 190, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Ternette, N.; Tippler, B.; Uberla, K.; Grunwald, T. Immunogenicity and Efficacy of Codon Optimized DNA Vaccines Encoding the F-Protein of Respiratory Syncytial Virus. Vaccine 2007, 25, 7271–7279. [Google Scholar] [CrossRef] [PubMed]
- Eroglu, E.; Singh, A.; Bawage, S.; Tiwari, P.M.; Vig, K.; Pillai, S.R.; Dennis, V.A.; Singh, S.R. Immunogenicity of RSV F DNA Vaccine in Balb/C Mice. Adv. Virol. 2016, 2016, 7971847. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Sambhara, S.; Li, C.X.; Ewasyshyn, M.; Parrington, M.; Caterini, J.; James, O.; Cates, G.; Du, R.P.; Klein, M. Protection against Respiratory Syncytial Virus Infection by DNA Immunization. J. Exp. Med. 1998, 188, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Park, E.K.; Soh, B.Y.; Jang, Y.S.; Park, J.H.; Chung, G.H. Immune Induction and Modulation in Mice Following Immunization with DNA Encoding F Protein of Respiratory Syncytial Virus. Mol. Cells 2001, 12, 50–56. [Google Scholar] [PubMed]
- Gilman, M.S.; Castellanos, C.A.; Chen, M.; Ngwuta, J.O.; Goodwin, E.; Moin, S.M.; Mas, V.; Melero, J.A.; Wright, P.F.; Graham, B.S.; et al. Rapid Profiling of RSV Antibody Repertoires from the Memory B Cells of Naturally Infected Adult Donors. Sci. Immunol. 2016, 1, eaaj1879. [Google Scholar] [CrossRef] [PubMed]
- Pancera, M.; Shahzad-Ul-Hussan, S.; Doria-Rose, N.A.; McLellan, J.S.; Bailer, R.T.; Dai, K.; Loesgen, S.; Louder, M.K.; Staupe, R.P.; Yang, Y.; et al. Structural Basis for Diverse N-Glycan Recognition by HIV-1-Neutralizing V1-V2-Directed Antibody Pg16. Nat. Struct. Mol. Biol. 2013, 20, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Decker, J.M.; Wang, S.; Hui, H.; Kappes, J.C.; Wu, X.; Salazar-Gonzalez, J.F.; Salazar, M.G.; Kilby, J.M.; Saag, M.S.; et al. Antibody Neutralization and Escape by HIV-1. Nature 2003, 422, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Helle, F.; Duverlie, G.; Dubuisson, J. The Hepatitis C Virus Glycan Shield and Evasion of the Humoral Immune Response. Viruses 2011, 3, 1909–1932. [Google Scholar] [CrossRef] [PubMed]
- Krzyzaniak, M.A.; Zumstein, M.T.; Gerez, J.A.; Picotti, P.; Helenius, A. Host Cell Entry of Respiratory Syncytial Virus Involves Macropinocytosis Followed by Proteolytic Activation of the F Protein. PLoS Pathog. 2013, 9, e1003309. [Google Scholar] [CrossRef] [PubMed]
- Varki, A.; Lowe, J.B. Biological Roles of Glycans. In Essentials of Glycobiology; Varki, A., Cummings, R.D., Esko, J.D., Freeze, H.H., Stanley, P., Bertozzi, C.R., Hart, G.W., Etzler, M.E., Eds.; Cold Spring Harbor: Long Island, NY, USA, 2009. [Google Scholar]
- Krarup, A.; Truan, D.; Furmanova-Hollenstein, P.; Bogaert, L.; Bouchier, P.; Bisschop, I.J.; Widjojoatmodjo, M.N.; Zahn, R.; Schuitemaker, H.; McLellan, J.S.; et al. A Highly Stable Prefusion RSV F Vaccine Derived from Structural Analysis of the Fusion Mechanism. Nat. Commun. 2015, 6, 8143. [Google Scholar] [CrossRef] [PubMed]
- Cortjens, B.; Yasuda, E.; Yu, X.; Wagner, K.; Claassen, Y.B.; Bakker, A.Q.; van Woensel, J.B.M.; Beaumont, T. Broadly Reactive Anti-Respiratory Syncytial Virus G Antibodies from Exposed Individuals Effectively Inhibit Infection of Primary Airway Epithelial Cells. J. Virol. 2017, 91, e02357-16. [Google Scholar] [CrossRef] [PubMed]
- Schepens, B.; Sedeyn, K.; Ginste, L.V.; de Baets, S.; Schotsaert, M.; Roose, K.; Houspie, L.; van Ranst, M.; Gilbert, B.; van Rooijen, N.; et al. Protection and Mechanism of Action of a Novel Human Respiratory Syncytial Virus Vaccine Candidate Based on the Extracellular Domain of Small Hydrophobic Protein. EMBO Mol. Med. 2014, 6, 1436–1454. [Google Scholar] [CrossRef] [PubMed]
- Doe, B.; Steimer, K.S.; Walker, C.M. Induction of Hiv-1 Envelope (Gp120)-Specific Cytotoxic T Lymphocyte Responses in Mice by Recombinant Cho Cell-Derived Gp120 Is Enhanced by Enzymatic Removal of N-Linked Glycans. Eur. J. Immunol. 1994, 24, 2369–2376. [Google Scholar] [CrossRef] [PubMed]
- Francica, J.R.; Varela-Rohena, A.; Medvec, A.; Plesa, G.; Riley, J.L.; Bates, P. Steric Shielding of Surface Epitopes and Impaired Immune Recognition Induced by the Ebola Virus Glycoprotein. PLoS Pathog. 2010, 6, e1001098. [Google Scholar] [CrossRef] [PubMed]
- Wolfert, M.A.; Boons, G.J. Adaptive Immune Activation: Glycosylation Does Matter. Nat. Chem. Biol. 2013, 9, 776–784. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.L.; Melero, J.A. Progress in Understanding and Controlling Respiratory Syncytial Virus: Still Crazy after All These Years. Virus Res. 2011, 162, 80–99. [Google Scholar] [CrossRef] [PubMed]
- Graham, B.S.; Modjarrad, K.; McLellan, J.S. Novel Antigens for RSV Vaccines. Curr. Opin. Immunol. 2015, 35, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Saade, F.; Petrovsky, N. The Future of Human DNA Vaccines. J. Biotechnol. 2012, 162, 171–182. [Google Scholar] [CrossRef] [PubMed]
| Surface Expression | Total Expression | % Transfected Cells | Fusion Capacity | Total Ab Response | Neutralizing Ab Response | |
|---|---|---|---|---|---|---|
| F N27Q | = | = | = | = | = | = |
| F N70Q | – | – | = | = 1 | = | − |
| F N116Q | = | = | = | = 1 | = | + |
| F N126Q | = | − | = | = | = | = |
| F N500Q | – | − | – | − | = | = |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leemans, A.; Boeren, M.; Van der Gucht, W.; Pintelon, I.; Roose, K.; Schepens, B.; Saelens, X.; Bailey, D.; Martinet, W.; Caljon, G.; et al. Removal of the N-Glycosylation Sequon at Position N116 Located in p27 of the Respiratory Syncytial Virus Fusion Protein Elicits Enhanced Antibody Responses after DNA Immunization. Viruses 2018, 10, 426. https://doi.org/10.3390/v10080426
Leemans A, Boeren M, Van der Gucht W, Pintelon I, Roose K, Schepens B, Saelens X, Bailey D, Martinet W, Caljon G, et al. Removal of the N-Glycosylation Sequon at Position N116 Located in p27 of the Respiratory Syncytial Virus Fusion Protein Elicits Enhanced Antibody Responses after DNA Immunization. Viruses. 2018; 10(8):426. https://doi.org/10.3390/v10080426
Chicago/Turabian StyleLeemans, Annelies, Marlies Boeren, Winke Van der Gucht, Isabel Pintelon, Kenny Roose, Bert Schepens, Xavier Saelens, Dalan Bailey, Wim Martinet, Guy Caljon, and et al. 2018. "Removal of the N-Glycosylation Sequon at Position N116 Located in p27 of the Respiratory Syncytial Virus Fusion Protein Elicits Enhanced Antibody Responses after DNA Immunization" Viruses 10, no. 8: 426. https://doi.org/10.3390/v10080426
APA StyleLeemans, A., Boeren, M., Van der Gucht, W., Pintelon, I., Roose, K., Schepens, B., Saelens, X., Bailey, D., Martinet, W., Caljon, G., Maes, L., Cos, P., & Delputte, P. (2018). Removal of the N-Glycosylation Sequon at Position N116 Located in p27 of the Respiratory Syncytial Virus Fusion Protein Elicits Enhanced Antibody Responses after DNA Immunization. Viruses, 10(8), 426. https://doi.org/10.3390/v10080426







