Acute and Prolonged Effects of Dermal Suction on Joint Range of Motion and Passive Muscle Stiffness: A Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
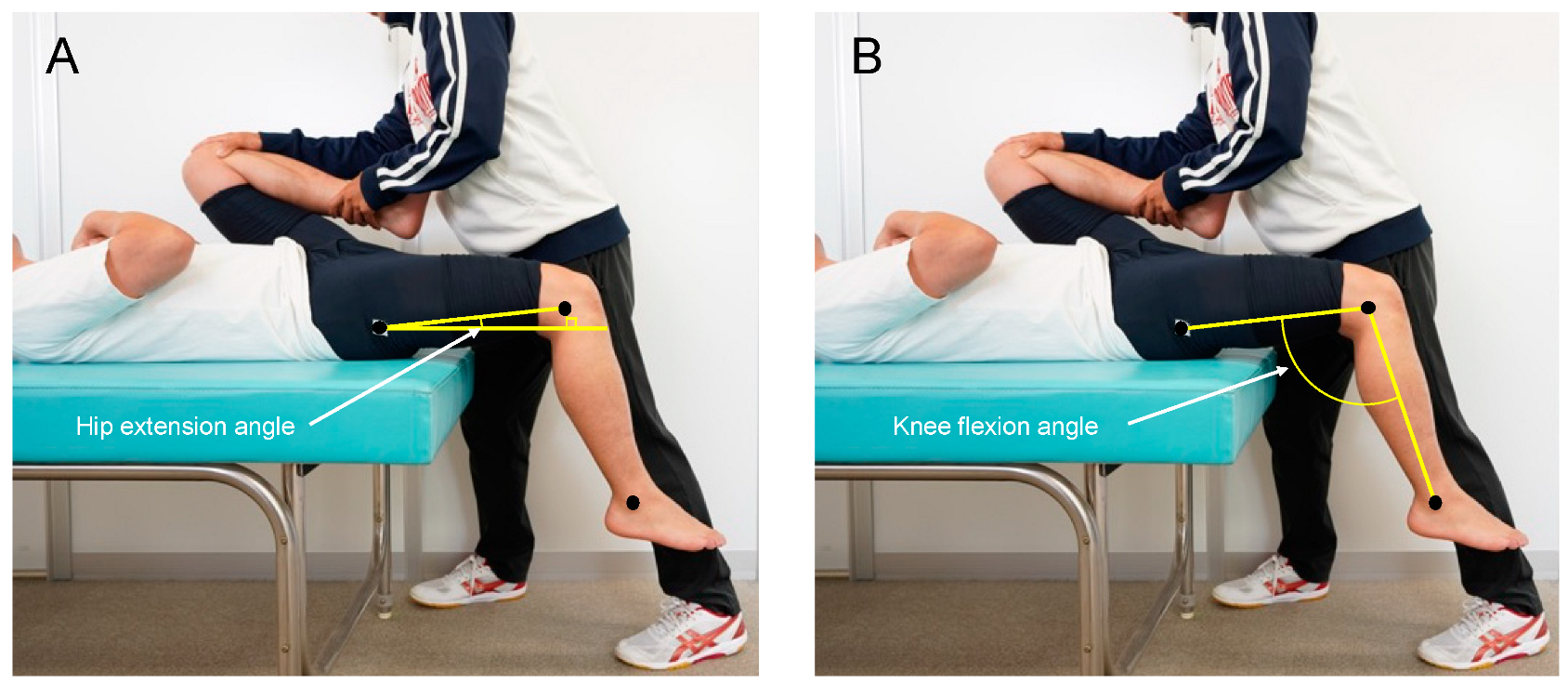
2.3. Joint ROM
2.4. Passive Muscle Stiffness
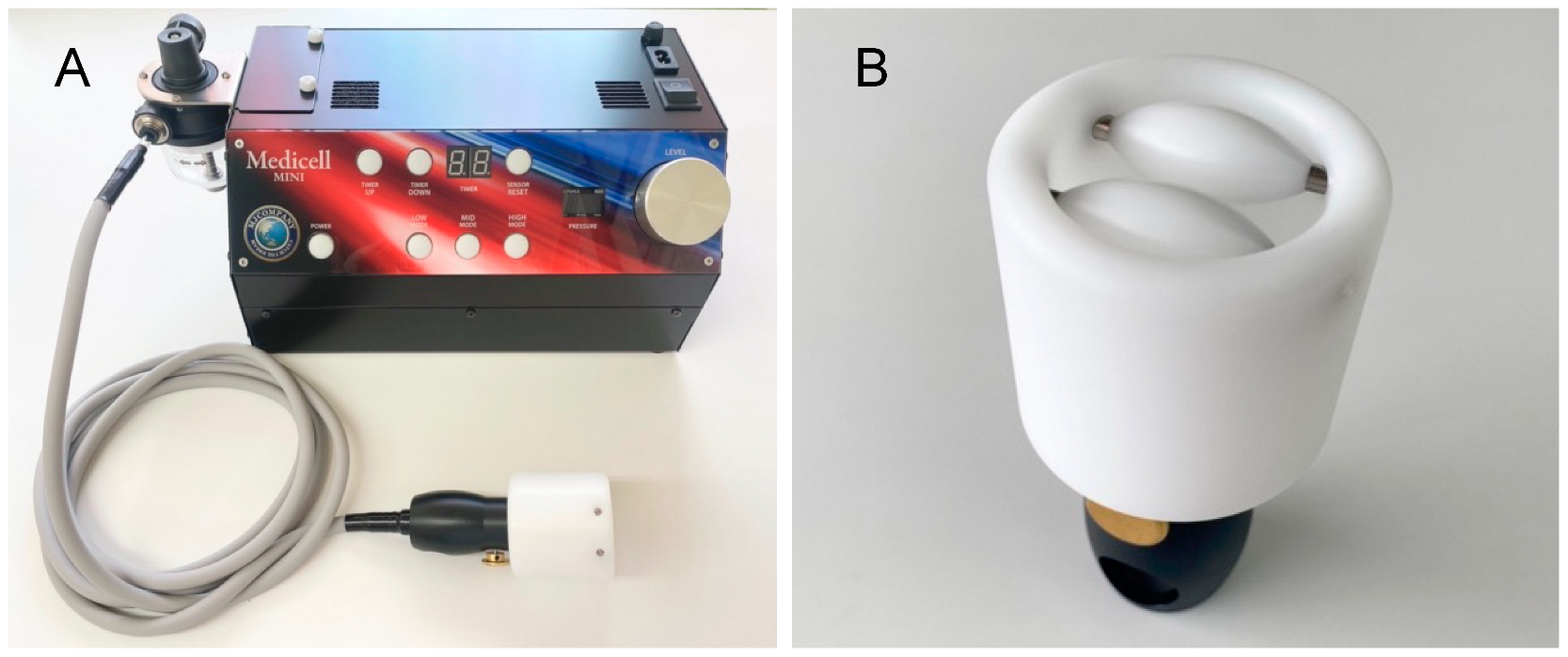
2.5. Dermal Suction
2.6. Reliability
2.7. Statistics
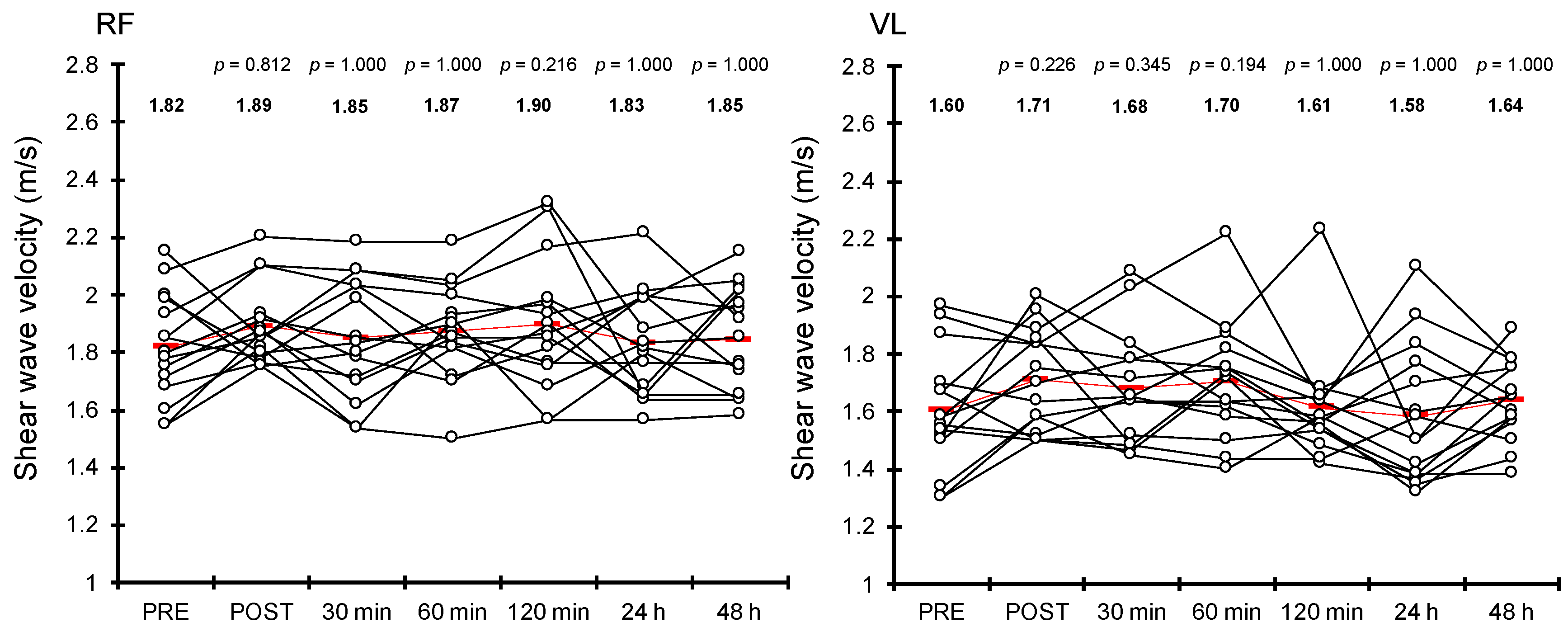
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yoo, S.S.; Tausk, F. Cupping: East meets West. Int. J. Dermatol. 2004, 43, 664–665. [Google Scholar] [CrossRef]
- Kim, J.E.; Cho, J.E.; Do, K.S.; Lim, S.Y.; Kim, H.J.; Yim, J.E. Effect of cupping therapy on range of motion, pain threshold, and muscle activity of the hamstring muscle compared to passive stretching. J. Korean Soc. Phys. Med. 2017, 12, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Markowski, A.; Sanford, S.; Pikowski, J.; Fauvell, D.; Cimino, D.; Caplan, S. A pilot study analyzing the effects of Chinese cupping as an adjunct treatment for patients with subacute low back pain on relieving pain, improving range of motion, and improving function. J. Altern. Complement. Med. 2014, 20, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Murray, D.; Clarkson, C. Effects of moving cupping therapy on hip and knee range of movement and knee flexion power: A preliminary investigation. J. Man. Manip. Ther. 2019, 27, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Ullah, K.; Younis, A.; Wali, M. An investigation into the effect of cupping therapy as a treatment for anterior knee pain and its potential role in health promotion. Internet J. Altern. Med. 2007, 4, 1–9. [Google Scholar]
- Yim, J.; Park, J.; Kim, H.; Woo, J.; Joo, S.; Lee, S.; Song, J. Comparison of the effects of muscle stretching exercises and cupping therapy on pain thresholds, cervical range of motion and angle: A cross-over study. Phys. Ther. Rehab. Sci. 2017, 6, 83–89. [Google Scholar] [CrossRef] [Green Version]
- Schafer, M.D.; Tom, J.C.; Girouard, T.J.; Navalta, J.W.; Turner, C.L.; Radzak, K.N. Cupping therapy does not influence healthy adult’s hamstring range of motion compared to control or sham conditions. Int. J. Exerc. Sci. 2020, 13, 216. [Google Scholar]
- Cobb, S.; Maddox, O.; Seitz, G.; Arnot, C. The effects of stretching versus static and dynamic cupping on lumbar range of motion: A randomized control trial. Orthop. Phys. Ther. Pract. 2022, 34, 276–282. [Google Scholar]
- Johns, R.J.; Wright, V. Relative importance of various tissues in joint stiffness. J. Appl. Physiol. 1962, 17, 824–828. [Google Scholar] [CrossRef]
- Enomoto, S.; Shibutani, T.; Akihara, Y.; Nakatani, M.; Yamada, K.; Oda, T. Acute Effects of Dermal Suction on Passive Muscle and Joint Stiffness. Healthcare 2021, 9, 1483. [Google Scholar] [CrossRef]
- Mizuno, T.; Matsumoto, M.; Umemura, Y. Viscoelasticity of the muscle–tendon unit is returned more rapidly than range of motion after stretching. Scand. J. Med. Sci. Sports 2013, 23, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Power, K.; Behm, D.; Cahill, F.; Carroll, M.; Young, W. An acute bout of static stretching: Effects on force and jumping performance. Med. Sci. Sports Exerc. 2004, 36, 1389–1396. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, M.; Onuma, R.; Kiyono, R.; Yasaka, K.; Sato, S.; Yahata, K.; Fukaya, T.; Konrad, A. The acute and prolonged effects of different durations of foam rolling on range of motion, muscle stiffness, and muscle strength. J. Sports Sci. Med. 2021, 20, 62. [Google Scholar] [CrossRef] [PubMed]
- Harvey, D. Assessment of the flexibility of elite athletes using the modified Thomas test. Br. J. Sports Med. 1998, 32, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reiner, M.M.; Glashüttner, C.; Bernsteiner, D.; Tilp, M.; Guilhem, G.; Morales-Artacho, A.; Konrad, A. A comparison of foam rolling and vibration foam rolling on the quadriceps muscle function and mechanical properties. Eur. J. Appl. Physiol. 2021, 121, 1461–1471. [Google Scholar] [CrossRef]
- Vigotsky, A.D.; Lehman, G.J.; Contreras, B.; Beardsley, C.; Chung, B.; Feser, E.H. Acute effects of anterior thigh foam rolling on hip angle, knee angle, and rectus femoris length in the modified Thomas test. PeerJ 2015, 3, e1281. [Google Scholar] [CrossRef] [Green Version]
- Nagahara, R.; Suganuma, S.; Tsuda, S.; Shibutani, T.; Enomoto, S. Acute effects of dermal suctioning on back pain in racehorses: A pilot study. Comp. Exerc. Physiol. 2022, 18, 339–347. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 28 June 2022).
- Crawley, M.J. The R Book; John Wiley & Sons: Hoboken, NJ, USA, 2007. [Google Scholar]
- Abe, J.; Iritani, R.; Tsuchida, K.; Kamimura, Y.; West, S.A. A solution to a sex ratio puzzle in Melittobia wasps. Proc. Natl. Acad. Sci. USA 2021, 118, e2024656118. [Google Scholar] [CrossRef]
- Enomoto, S.; Oda, T.; Sugisaki, N.; Toeda, M.; Kurokawa, S.; Kaga, M. Muscle stiffness of the rectus femoris and vastus lateralis in children with Osgood–Schlatter disease. Knee 2021, 32, 140–147. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Roostayi, M.M.; Norouzali, T.; Manshadi, F.D.; Abbasi, M.; Baghban, A.A. The effects of cupping therapy on skin’s biomechanical properties in wistar rats. Chin. Med. 2016, 7, 25–30. [Google Scholar] [CrossRef] [Green Version]
- Tasaka, A.; Ono, T.; Oki, S.; Umei, N.; Ishikura, H.; Aihara, K.; Sato, Y.; Otsuka, A.; Muto, N. Effect of skin resection on the improvement of joint contractures in rats. J. Phys. Ther. Sci. 2014, 26, 11–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chino, K.; Takahashi, H. Measurement of gastrocnemius muscle elasticity by shear wave elastography: Association with passive ankle joint stiffness and sex differences. Eur. J. Appl. Physiol. 2016, 116, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Chiacchiero, M.; Dresely, B.; Silva, U.; DeLosReyes, R.; Vorik, B. The relationship between range of movement, flexibility, and balance in the elderly. Top. Geriatr. Rehabil. 2010, 26, 148–155. [Google Scholar] [CrossRef] [Green Version]
- Kerrigan, D.C.; Xenopoulos-Oddsson, A.; Sullivan, M.J.; Lelas, J.J.; Riley, P.O. Effect of a hip flexor [ndash] stretching program on gait in the elderly. Arch. Phys. Med. Rehabil. 2003, 84, 1–6. [Google Scholar] [CrossRef]
- Charles, J.P.; Suntaxi, F.; Anderst, W.J. In vivo human lower limb muscle architecture dataset obtained using diffusion tensor imaging. PLoS ONE 2019, 14, e0223531. [Google Scholar] [CrossRef] [Green Version]
- Toomey, C.; McCreesh, K.; Leahy, S.; Jakeman, P. Technical considerations for accurate measurement of subcutaneous adipose tissue thickness using B-mode ultrasound. Ultrasound 2011, 19, 91–96. [Google Scholar] [CrossRef]
- Xu, J.; Hug, F.; Fu, S.N. Stiffness of individual quadriceps muscle assessed using ultrasound shear wave elastography during passive stretching. J. Sport Health Sci. 2018, 7, 245–249. [Google Scholar] [CrossRef] [Green Version]
- Hirata, K.; Kanehisa, H.; Miyamoto-Mikami, E.; Miyamoto, N. Evidence for intermuscle difference in slack angle in human triceps surae. J. Biomech. 2015, 48, 1210–1213. [Google Scholar] [CrossRef]
- Hirata, K.; Miyamoto-Mikami, E.; Kanehisa, H.; Miyamoto, N. Muscle-specific acute changes in passive stiffness of human triceps surae after stretching. Eur. J. Appl. Physiol. 2016, 116, 911–918. [Google Scholar] [CrossRef]
- Hug, F.; Lacourpaille, L.; Maïsetti, O.; Nordez, A. Slack length of gastrocnemius medialis and Achilles tendon occurs at different ankle angles. J. Biomech. 2013, 46, 2534–2538. [Google Scholar] [CrossRef] [PubMed]
- Evans, S.R. Clinical trial structures. J. Exp. Stroke Transl. Med. 2010, 3, 8–18. [Google Scholar] [CrossRef] [PubMed]

| Sex | Age (Years) | Height (cm) | Body Mass (kg) |
|---|---|---|---|
| Men | 28.0 (4.5) | 172.1 (3.1) | 72.2 (15.0) |
| Women | 22.8 (1.5) | 158.2 (4.5) | 54.9 (8.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enomoto, S.; Shibutani, T.; Akihara, Y.; Yamada, K.; Oda, T. Acute and Prolonged Effects of Dermal Suction on Joint Range of Motion and Passive Muscle Stiffness: A Preliminary Study. Healthcare 2022, 10, 2241. https://doi.org/10.3390/healthcare10112241
Enomoto S, Shibutani T, Akihara Y, Yamada K, Oda T. Acute and Prolonged Effects of Dermal Suction on Joint Range of Motion and Passive Muscle Stiffness: A Preliminary Study. Healthcare. 2022; 10(11):2241. https://doi.org/10.3390/healthcare10112241
Chicago/Turabian StyleEnomoto, Shota, Tomonari Shibutani, Yu Akihara, Kazunori Yamada, and Toshiaki Oda. 2022. "Acute and Prolonged Effects of Dermal Suction on Joint Range of Motion and Passive Muscle Stiffness: A Preliminary Study" Healthcare 10, no. 11: 2241. https://doi.org/10.3390/healthcare10112241
APA StyleEnomoto, S., Shibutani, T., Akihara, Y., Yamada, K., & Oda, T. (2022). Acute and Prolonged Effects of Dermal Suction on Joint Range of Motion and Passive Muscle Stiffness: A Preliminary Study. Healthcare, 10(11), 2241. https://doi.org/10.3390/healthcare10112241






