Effects of Capacitive-Resistive Electric Transfer on Sports Performance in Paralympic Swimmers: A Stopped Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
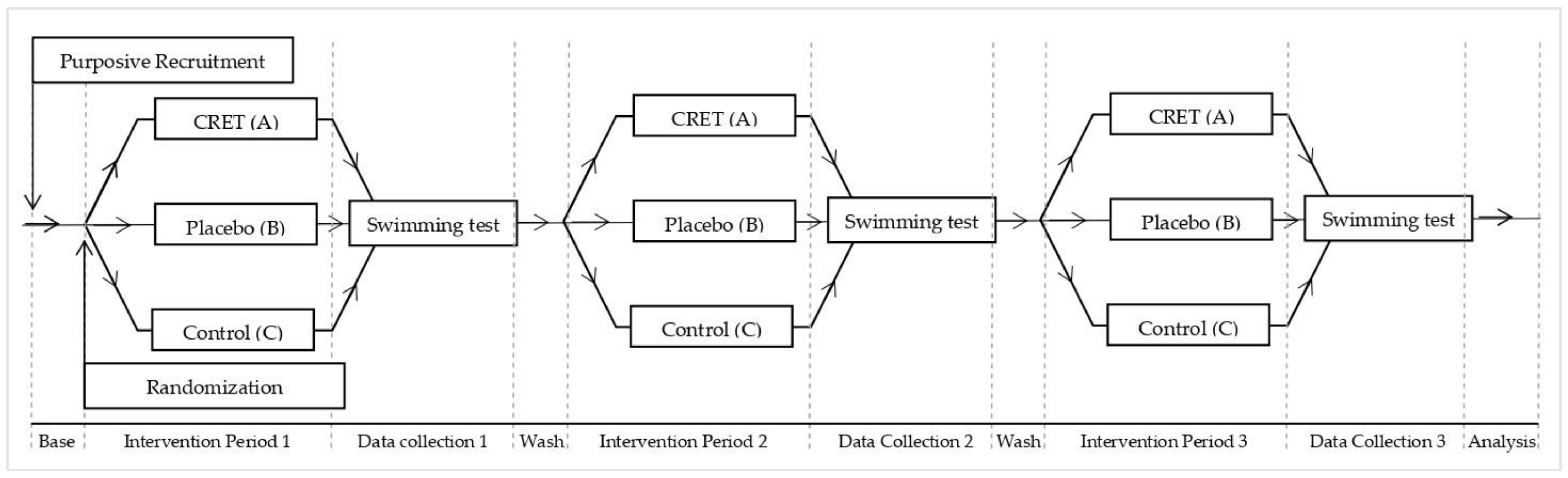
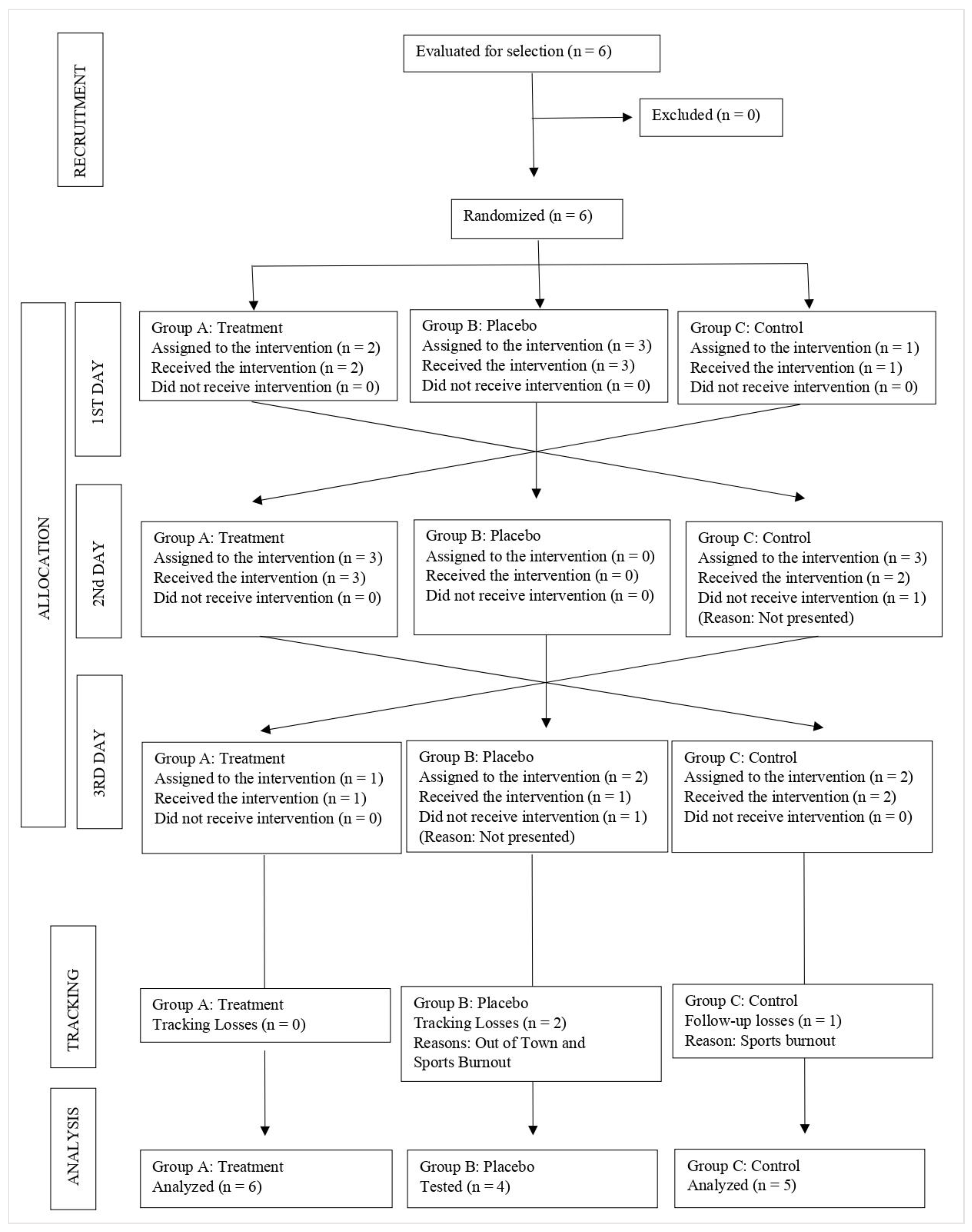
2.1. Study Design and Ethics
2.2. Experimental Design
2.3. Participants
2.4. Intervention
2.5. Outcome
2.6. Swimming Tests and Data Collection
2.7. Statistical Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Practical Applications
- -
- Basing the practical use of CRET on known physiological effects is insufficient. Not knowing its effects on sports performance and their extent might lead to questions about its use, and possible undesirable effects. This paper presents clinicians with information related to the latest proven benefits of CRET, as well as deepening the knowledge into the undesired effect of its application immediately prior to a performance at specific parameters.
- -
- A very detailed protocol was established in this study resulting from the scientific available information. Use of this protocol as a baseline to carry out modifications could be of the utmost interest to the paralympic population, as well as the methodology presented as a tool to prove those future modifications.
- -
- This study opens a broader field of study from clinic use of this technology to the sport/competitive field. The study suggests future lines of investigation, such as real time monitoring of CRET’s physiological effects in sports. There is a current need to deepen the knowledge of the following CRET’s influence on sports performance related to duration of appliance, electrical potential, location of application, temperature threshold, training or competitive frame.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kumaran, B.; Watson, T. Thermal build-up, decay and retention responses to local therapeutic application of 448 kHz capacitive resistive monopolar radiofrequency: A prospective randomised crossover study in healthy adults. Int. J. Hyperth. 2015, 31, 883–895. [Google Scholar] [CrossRef] [PubMed]
- Paolucci, T.; Pezzi, L.; Centra, M.; Porreca, A.; Barbato, C.; Bellomo, R.; Saggini, R. Effects of capacitive and resistive electric transfer therapy in patients with painful shoulder impingement syndrome: A comparative study. J. Int. Med. Res. 2019, 48, 030006051988309. [Google Scholar] [CrossRef]
- Coccetta, C.A.; Sale, P.; Ferrara, P.E.; Specchia, A.; Maccauro, G.; Ferriero, G.; Ronconi, G. Effects of capacitive and resistive electric transfer therapy in patients with knee osteoarthritis: A randomized controlled trial. Int. J. Rehabil. Res. 2019, 42, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Osti, R.; Pari, C.; Salvatori, G.; Massari, L. Tri-length laser therapy associated to tecar therapy in the treatment of low-back pain in adults: A preliminary report of a prospective case series. Lasers Med. Sci. 2014, 30, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, Y.; Hasegawa, S.; Yokota, Y.; Nishiguchi, S.; Fukutani, N.; Shirooka, H.; Tasaka, S.; Matsushita, T.; Matsubara, K.; Nakayama, Y.; et al. Effect of Capacitive and Resistive electric transfer on haemoglobin saturation and tissue temperature. Int. J. Hyperth. 2017, 33, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Clijsen, R.; Leoni, D.; Schneebeli, A.; Cescon, C.; Soldini, E.; Li, L.; Barbero, M. Does the Application of Tecar Therapy Affect Temperature and Perfusion of Skin and Muscle Microcirculation? A Pilot Feasibility Study on Healthy Subjects. J. Altern. Complement. Med. 2020, 26, 147–153. [Google Scholar] [CrossRef] [PubMed]
- van der Veen, P.; Kempenaers, F.; Vermijlen, S.; Van Waeyenberghe, C.; Kerckhofs, E.; Bossuyt, A.; Van den Brande, P.; Lievens, P. Electromagnetic diathermia: A lymphoscintigraphic and light reflection rheographic study of leg lymphatic and venous dynamics in healthy subjects. Lymphology 2000, 33, 12–18. [Google Scholar]
- Yokota, Y.; Sonoda, T.; Tashiro, Y.; Suzuki, Y.; Kajiwara, Y.; Zeidan, H.; Nakayama, Y.; Kawagoe, M.; Shimoura, K.; Tatsumi, M.; et al. Effect of Capacitive and Resistive electric transfer on changes in muscle flexibility and lumbopelvic alignment after fatiguing exercise. J. Phys. Ther. Sci. 2018, 30, 719–725. [Google Scholar] [CrossRef]
- Vikmoen, O.; Raastad, T.; Seynnes, O.; Bergstrøm, K.; Ellefsen, S.; Rønnestad, B.R. Effects of heavy strength training on running performance and determinants of running performance in female endurance athletes. PLoS ONE 2016, 11, e0150799. [Google Scholar] [CrossRef]
- Dankel, S.J.; Mattocks, K.T.; Mouser, J.G.; Buckner, S.L.; Jessee, M.B.; Loenneke, J.P. A critical review of the current evidence examining whether resistance training improves time trial performance. J. Sports Sci. 2018, 36, 1485–1491. [Google Scholar] [CrossRef]
- Bonne, T.C.; Lundby, C.; Jørgensen, S.; Johansen, L.; Mrgan, M.; Bech, S.R.; Sander, M.; Papoti, M.; Nordsborg, N.B. “Live High-Train High” increases hemoglobin mass in Olympic swimmers. Eur. J. Appl. Physiol. 2014, 114, 1439–1449. [Google Scholar] [CrossRef] [PubMed]
- Hellard, P.; Scordia, C.; Avalos, M.; Mujika, I.; Pyne, D.B. Modelling of optimal training load patterns during the 11 weeks preceding major competition in elite swimmers. Appl. Physiol. Nutr. Metab. 2017, 42, 1106–1117. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G.; Hawley, J.A.; Burke, L.M. Design and analysis of research on sport performance enhancement. Med. Sci. Sports Exerc. 1999, 31, 472–485. [Google Scholar] [CrossRef] [PubMed]
- Hainline, B.; Turner, J.A.; Caneiro, J.P.; Stewart, M.; Lorimer Moseley, G. Pain in elite athletes—Neurophysiological, biomechanical and psychosocial considerations: A narrative review. Br. J. Sports Med. 2017, 51, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Cecchi, F.; Pancani, S.; Vannetti, F.; Boni, R.; Castagnoli, C.; Paperini, A.; Pasquini, G.; Sofi, F.; Molino-Lova, R.; Macchi, C.; et al. Hemoglobin concentration is associated with self-reported disability and reduced physical performance in a community dwelling population of nonagenarians: The Mugello Study. Intern. Emerg. Med. 2017, 12, 1167–1173. [Google Scholar] [CrossRef]
- McGowan, C.J.; Pyne, D.B.; Thompson, K.G.; Raglin, J.S.; Osborne, M.; Rattray, B. Elite sprint swimming performance is enhanced by completion of additional warm-up activities. J. Sports Sci. 2017, 35, 1493–1499. [Google Scholar] [CrossRef]
- Connick, M.J.; Beckman, E.; Spathis, J.; Deuble, R.; Tweedy, S.M. How Much Do Range of Movement and Coordination Affect Paralympic Sprint Performance? Med. Sci. Sport. Exerc. 2015, 47, 2216–2223. [Google Scholar] [CrossRef]
- Kilduff, L.P.; Finn, C.V.; Baker, J.S.; Cook, C.J.; West, D.J. Preconditioning Strategies to Enhance Physical Performance on the Day of Competition. Int. J. Sport. Physiol. Perform. 2013, 8, 677–681. [Google Scholar] [CrossRef]
- Ulrich, S.; Hasler, E.D.; Müller-Mottet, S.; Keusch, S.; Furian, M.; Latshang, T.D.; Schneider, S.; Saxer, S.; Bloch, K.E. Mechanisms of Improved Exercise Performance under Hyperoxia. Respiration 2017, 93, 90–98. [Google Scholar] [CrossRef]
- McGowan, C.J.; Thompson, K.G.; Pyne, D.B.; Raglin, J.S.; Rattray, B. Heated jackets and dryland-based activation exercises used as additional warm-ups during transition enhance sprint swimming performance. J. Sci. Med. Sport 2016, 19, 354–358. [Google Scholar] [CrossRef]
- Neiva, H.P.; Marques, M.C.; Barbosa, T.M.; Izquierdo, M.; Marinho, D.A. Warm-Up and Performance in Competitive Swimming. Sport. Med. 2014, 44, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Morriën, F.; Taylor, M.J.D.; Hettinga, F.J. Biomechanics in paralympics: Implications for performance. Int. J. Sports Physiol. Perform. 2017, 12, 578–589. [Google Scholar] [CrossRef] [PubMed]
- Burkett, B.; Payton, C.; Van de Vliet, P.; Jarvis, H.; Daly, D.; Mehrkuehler, C.; Kilian, M.; Hogarth, L. Performance Characteristics of Para Swimmers How Effective Is the Swimming Classification System? Phys. Med. Rehabil. Clin. N. Am. 2018, 29, 333–346. [Google Scholar] [CrossRef] [PubMed]
- Currell, K.; Jeukendrup, A.E. Validity, reliability and sensitivity of measures of sporting performance. Sport. Med. 2008, 38, 297–316. [Google Scholar] [CrossRef] [PubMed]
- Jeukendrup, A.; Saris, W.H.M.; Brouns, F.; Kester, A.D.M. A new validated endurance performance test. Med. Sci. Sports Exerc. 1996, 28, 266–270. [Google Scholar] [CrossRef]
- Simim, M.A.M.; De Mello, M.T.; Silva, B.V.C.; Rodrigues, D.F.; Rosa, J.P.P.; Couto, B.P.; Da Silva, A. Load monitoring variables in training and competition situations: A systematic review applied to wheelchair sports. Adapt. Phys. Act. Q. 2017, 34, 466–483. [Google Scholar] [CrossRef]
- Borg, G.A.V. Psychophysical bases of perceived exertion. Plast. Reconstr. Surg. 1954, 14, 377–381. [Google Scholar] [CrossRef]
- Daly, D.J.; Djobova, S.K.; Malone, L.A.; Vanlandewijck, Y.; Steadward, R.D. Swimming speed patterns and stroking variables in the paralympic100-m freestyle. Adapt. Phys. Act. Q. 2003, 20, 260–278. [Google Scholar] [CrossRef]
- Fulton, S.K.; Pyne, D.B.; Hopkins, W.G.; Burkett, B. Training Characteristics of Paralympic Swimmers. J. Strength Cond. Res. 2010, 24, 471–478. [Google Scholar] [CrossRef]
- Dingley, A.; Pyne, D.B.; Burkett, B. Phases of the swim-start in Paralympic swimmers are influenced by severity and type of disability. J. Appl. Biomech. 2014, 30, 643–648. [Google Scholar] [CrossRef]
- Daly, D.J.; Malone, L.A.; Smith, D.J.; Vanlandewijck, Y.; Steadward, R.D. The contribution of starting, turning, and finishing to total race performance in male Paralympic swimmers. Adapt. Phys. Act. Q. 2001, 18, 316–333. [Google Scholar] [CrossRef]
- Ranke, M.B.; Wit, J.M. Growth hormone-past, present and future. Nat. Rev. Endocrinol. 2018, 14, 285–300. [Google Scholar] [CrossRef] [PubMed]
- Birzniece, V.; Nelson, A.E.; Ho, K.K.Y. Growth hormone and physical performance. Trends Endocrinol. Metab. 2011, 22, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Ali, Z.A.; Callaghan, C.J.; Lim, E.; Ali, A.A.; Nouraei, S.A.R.; Akthar, A.M.; Boyle, J.R.; Varty, K.; Kharbanda, R.K.; Dutka, D.P.; et al. Remote ischemic preconditioning reduces myocardial and renal injury after elective abdominal aortic aneurysm repair: A randomized controlled trial. Circulation 2007, 116 (Suppl. S11), 1–98. [Google Scholar] [CrossRef]
- Lalonde, F.; Curnier, D.Y. Can Anaerobic Performance Be Improved by Remote Ischemic Preconditioning? J. Strength Cond. Res. 2015, 29, 80–85. [Google Scholar] [CrossRef]
- De Sousa-De Sousa, L.; Tebar Sanchez, C.; Maté-Muñoz, J.L.; Hernández-Lougedo, J.; Barba, M.; Lozano-Esteban, M.D.C.; Garnacho-Castaño, M.V.; García-Fernández, P. Application of Capacitive-Resistive Electric Transfer in Physiotherapeutic Clinical Practice and Sports. Int. J. Environ. Res. Public Health 2021, 18, 12446. [Google Scholar] [CrossRef]
- Duñabeitia, I.; Arrieta, H.; Torres-Unda, J.; Gil, J.; Santos-Concejero, J.; Gil, S.M.; Irazusta, J.; Bidaurrazaga-Letona, I. Effects of a capacitive-resistive electric transfer therapy on physiological and biomechanical parameters in recreational runners: A randomized controlled crossover trial. Phys. Ther. Sport 2018, 32, 227–234. [Google Scholar] [CrossRef]
- Perret, C. Elite-adapted wheelchair sports performance: A systematic review. Disabil. Rehabil. 2017, 39, 164–172. [Google Scholar] [CrossRef]
- Moses, L.; Oakford, R. Tables of Random Permutations; Stanford University Press: Redwood City, CA, USA, 1963. [Google Scholar]
- Feitosa, W.G.; Correia, R.D.A.; Barbosa, T.M.; Castro, F.A.D.S. Performance of disabled swimmers in protocols or tests and competitions: A systematic review and meta-analysis. Sport. Biomech. 2019, 21, 255–277. [Google Scholar] [CrossRef]
- Neiva, H.P.; Marques, M.C.; Barbosa, T.M.; Izquierdo, M.; Viana, J.L.; Marinho, D.A. Effects of 10 min vs. 20 min passive rest after warm-up on 100 m freestyle time-trial performance: A randomized crossover study. J. Sci. Med. Sport 2017, 20, 81–86. [Google Scholar] [CrossRef]
- Costa, G.D.C.T.; Galvão, L.; Bottaro, M.; Mota, J.F.; Pimentel, G.D.; Gentil, P. Effects of placebo on bench throw performance of Paralympic weightlifting athletes: A pilot study. J. Int. Soc. Sports Nutr. 2019, 16, 9. [Google Scholar] [CrossRef] [PubMed]
- Moses, L.E. Non-parametric statistics for psychological research. Psychol. Bull. 1952, 49, 122–143. [Google Scholar] [CrossRef] [PubMed]
- Lix, L.M.; Keselman, J.C.; Keselman, H.J. Consequences of Assumption Violations Revisited: A Quantitative Review of Alternatives to the One-Way Analysis of Variance F Test. Rev. Educ. Res. 2016, 66, 579–619. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- de Ullibarri Galparsoro, L.; Pita Fernández, S. Medidas de concordancia: El índice de Kappa [Concordance measures: The Kappa index]. Cad Aten Primaria 1999, 6, 169–171. (In Spanish) [Google Scholar]
- Dingley, A.A.; Pyne, D.B.; Youngson, J.; Burkett, B. Effectiveness of a Dry-Land Resistance Training Program on Strength, Power, and Swimming Performance in Paralympic Swimmers. J. Strength Cond. Res. 2015, 29, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Brehm, J.W.; Self, E.A. The intensity of motivation. Annu. Rev. Psychol. 1989, 40, 109–131. [Google Scholar] [CrossRef]
- Corbett, J.; Barwood, M.J.; Ouzounoglou, A.; Thelwell, R.; Dicks, M. Influence of Competition on Performance and Pacing during Cycling Exercise. Med. Sci. Sport. Exerc. 2012, 44, 509–515. [Google Scholar] [CrossRef]
- Williams, E.L.; Jones, H.S.; Sparks, S.A.; Marchant, D.C.; Midgley, A.W.; Mc Naughton, L.R. Competitor presence reduces internal attentional focus and improves 16.1km cycling time trial performance. J. Sci. Med. Sport 2015, 18, 486–491. [Google Scholar] [CrossRef]
- Fousekis, K.; Chrysanthopoulos, G.; Tsekoura, M.; Mandalidis, D.; Mylonas, K.; Angelopoulos, P.; Koumoundourou, D.; Billis, V.; Tsepis, E. Posterior thigh thermal skin adaptations to radiofrequency treatment at 448 kHz applied with or without Indiba® fascia treatment tools. J. Phys. Ther. Sci. 2020, 32, 292–296. [Google Scholar] [CrossRef][Green Version]
- Wallace, P.J.; McKinlay, B.J.; Cheung, S.S. Comment on: “Endurance Performance is Influenced by Perceptions of Pain and Temperature: Theory, Applications and Safety Considerations”. Sport. Med. 2018, 48, 2671–2673. [Google Scholar] [CrossRef] [PubMed]
- Stevens, C.J.; Mauger, A.R.; Hassmèn, P.; Taylor, L. Endurance Performance is Influenced by Perceptions of Pain and Temperature: Theory, Applications and Safety Considerations. Sport. Med. 2017, 48, 525–537. [Google Scholar] [CrossRef]
- Ryan, N.M.; John, M.H.; Robert, R. The effect of massage on acceleration and sprint performance in track & field athletes. Complement. Ther. Clin. Pract. 2018, 30, 1–5. [Google Scholar] [CrossRef]
- Stephenson, B.T.; Tolfrey, K.; Goosey-Tolfrey, V.L. Mixed Active and Passive, Heart Rate-Controlled Heat Acclimation Is Effective for Paralympic and Able-Bodied Triathletes. Front. Physiol. 2019, 10, 1214. [Google Scholar] [CrossRef] [PubMed]
- Glazachev, O.S.; Kofler, W.; Dudnik, E.N.; Zapara, M.A.; Samartseva, V.G. Effect of Adaptation to Passive Hyperthermia on Aerobic Performance and Cardio-Respiratory Endurance in Amateur Athletes. Hum. Physiol. 2020, 46, 66–73. [Google Scholar] [CrossRef]
- Zapara, M.A.; Dudnik, E.N.; Samartseva, V.G.; Kryzhanovskaya, S.Y.; Susta, D.; Glazachev, O.S.; Zapara, M.A.; Dudnik, E.N.; Samartseva, V.G.; Kryzhanovskaya, S.Y.; et al. Passive Whole-Body Hyperthermia Increases Aerobic Capacity and Cardio-Respiratory Efficiency in Amateur Athletes. Health 2020, 12, 14–26. [Google Scholar] [CrossRef][Green Version]
- West, D.J.; Dietzig, B.M.; Bracken, R.M.; Cunningham, D.J.; Crewther, B.T.; Cook, C.J.; Kilduff, L.P. Influence of post-warm-up recovery time on swim performance in international swimmers. J. Sci. Med. Sport 2013, 16, 172–176. [Google Scholar] [CrossRef]
- Gray, S.R.; De Vito, G.; Nimmo, M.A.; Farina, D.; Ferguson, R.A. Skeletal muscle ATP turnover and muscle fiber conduction velocity are elevated at higher muscle temperatures during maximal power output development in humans. Am. J. Physiol.—Regul. Integr. Comp. Physiol. 2006, 290, R376–R382. [Google Scholar] [CrossRef]
- Corbett, J.; Neal, R.A.; Lunt, H.C.; Tipton, M.J. Adaptation to Heat and Exercise Performance Under Cooler Conditions: A New Hot Topic. Sport. Med. 2014, 44, 1323–1331. [Google Scholar] [CrossRef]
- Faulkner, S.; Hupperets, M.; Hodder, S.; Havenith, G. Conductive and evaporative precooling lowers mean skin temperature and improves time trial performance in the heat. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. S1), 183–189. [Google Scholar] [CrossRef]
- Soultanakis, H.N.; Nafpaktiitou, D.; Mandaloufa, S.M. Impact of cool and warm water immersion on 50-m sprint performance and lactate recovery in swimmers. J. Sports Med. Phys. Fitness 2015, 55, 267–272. [Google Scholar] [PubMed]
- Ramos e Côrte, A.C.; Ramos Lopes, G.H.; Moraes, M.; de Oliveira, R.M.; Brioschi, M.H.; Hernandez, A.J. The importance of thermography for injury prevention and performance improvement in olympic swimmers: A series of case study. Int. Phys. Med. Rehabil. J. 2018, 3, 137–141. [Google Scholar] [CrossRef]

| Variable | Descriptive Measures |
|---|---|
| Age (years) | 22.7 ± 2.3 |
| Weight (Kg) | 58.1 ± 8.9 |
| Height (cm)) | 168.5 ± 11.8 |
| Daily training (hours) | 3.9 ± 0.8 |
| Better style | |
| Back | 28.6% |
| Breaststroke | 14.3% |
| Butterfly | 14.3% |
| Crawl | 28.6% |
| Subject | Group | Test 50 m (Average Two Tests) | Test 100 m (Average Two Tests) | ||||
|---|---|---|---|---|---|---|---|
| Borg Pre | Seconds | Borg Post | Borg Pre | Seconds | Borg Post | ||
| 91491a0b | A | 13 | 34.12 | 14.5 | 12.5 | 72.95 | 17.5 |
| B | 12 | 34.38 | 18.5 | 10 | 72.32 | 18.5 | |
| C | 16.5 | 34.45 | 18 | 15.5 | 74.99 | 19 | |
| 62856cb2 | A | 13 | 39.39 | 15 | 13 | 86.53 | 15 |
| B | 10.5 | 36.3 | 16 | 9.5 | 80.85 | 16 | |
| C | 11.5 | 37.93 | 13 | 11.5 | 80.06 | 14 | |
| b535ee0c | A | 14 | 39.22 | 16 | 15 | 83.1 | 18.5 |
| B | 15 | 37.26 | 18 | 15 | 82.67 | 19 | |
| C | 12 | 39.57 | 15 | 13.5 | 83.07 | 17 | |
| e867d12c | A | 14.5 | 31.12 | 16.5 | 14 | 69.82 | 19.5 |
| B | 11.5 | 31.44 | 14.5 | 11.5 | 68.41 | 16 | |
| C | 11 | 30.06 | 16 | 10.5 | 66.22 | 15.5 | |
| c271b626 | A | 11 | 32.58 | 16.5 | 10.5 | 70.81 | 16 |
| B | - | - | - | - | - | - | |
| C | 13 | 33.97 | 16.5 | 14 | 73.1 | 17 | |
| 1b936d0d | A | 12 | 34.51 | 16.5 | 10 | 74.97 | 16.5 |
| B | - | - | - | - | - | - | |
| C | - | - | - | - | - | - | |
| Treatment Group | Borg Scale 50 mts Test | Borg Scale 100 mts Test | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean Difference (CI. 95%) | Mean ± SD | Mean Difference (CI. 95%) | |||
| Pre | Post | Pre | Post | |||
| A (treatment) | 12.9 ± 1.2 | 15.8 ± 0.8 | 2.91 (1.17, 4.65) | 12.5 ± 1.9 | 17.1 ± 1.6 | 4.66 (2.95, 6.38) |
| B (Placebo) | 12.2 ± 1.9 | 16.7 ± 1.8 | 4.50 (1.66, 7.33) | 11.5 ± 2.4 | 17.3 ± 1.6 | 5.87 (2.60, 9.14) |
| C (Control) | 12.8 ± 2.1 | 15.7 ± 1.8 | 2.90 (1.06, 4.73) | 13 ± 2 | 16.5 ± 1.8 | 3.50 (2.33, 4.66) |
| Treatment Group | Time Obtained in 50 m Test | Time Obtained in 100 m Test | ||
|---|---|---|---|---|
| Mean ± SD | CI. 95% | Mean ± SD | CI. 95% | |
| A (treatment) | 35.1 ± 3.4 | 31.55, 38.75 | 76.3 ± 6.8 | 69.15, 83.57 |
| B (Placebo) | 34.8 ± 2.5 | 30.75, 38.92 | 76 ± 6.8 | 65.21, 86.89 |
| C (Control) | 35.1 ± 3.7 | 30.59, 39.79 | 75.4 ± 6.5 | 67.38, 83.58 |
| Personal Record | 31.2 ± 1.8 | 29.31, 33.20 | 68.4 ± 3.3 | 64.97, 71.92 |
| Test Compared to Friedman | Ranks by Group | p-Value (Sig. 95%) | Test Effect Size | |||
|---|---|---|---|---|---|---|
| Group A | Group B | Group C | Personal Record | |||
| Borg Scale 50 m | 1.38 | 2.63 | 2 | - | 0.16 | 0.44 |
| Borg Scale 100 m | 1.88 | 2.5 | 1.65 | - | 0.42 | 0.21 |
| Times 50 m | 2.75 | 2.5 | 3 | 1.75 | 0.55 | 0.17 |
| Times 100 m | 3.75 | 2.5 | 2.5 | 1.25 | 0.05 * | 0.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Sousa-De Sousa, L.; Espinosa, H.G.; Maté-Muñoz, J.L.; Lozano-Estevan, M.d.C.; Cerrolaza-Tudanca, S.; Rozalén-Bustín, M.; Fernández-Carnero, S.; García-Fernández, P. Effects of Capacitive-Resistive Electric Transfer on Sports Performance in Paralympic Swimmers: A Stopped Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 14620. https://doi.org/10.3390/ijerph192114620
De Sousa-De Sousa L, Espinosa HG, Maté-Muñoz JL, Lozano-Estevan MdC, Cerrolaza-Tudanca S, Rozalén-Bustín M, Fernández-Carnero S, García-Fernández P. Effects of Capacitive-Resistive Electric Transfer on Sports Performance in Paralympic Swimmers: A Stopped Randomized Clinical Trial. International Journal of Environmental Research and Public Health. 2022; 19(21):14620. https://doi.org/10.3390/ijerph192114620
Chicago/Turabian StyleDe Sousa-De Sousa, Luis, Hugo G. Espinosa, Jose Luis Maté-Muñoz, Maria del Carmen Lozano-Estevan, Sara Cerrolaza-Tudanca, Manuel Rozalén-Bustín, Samuel Fernández-Carnero, and Pablo García-Fernández. 2022. "Effects of Capacitive-Resistive Electric Transfer on Sports Performance in Paralympic Swimmers: A Stopped Randomized Clinical Trial" International Journal of Environmental Research and Public Health 19, no. 21: 14620. https://doi.org/10.3390/ijerph192114620
APA StyleDe Sousa-De Sousa, L., Espinosa, H. G., Maté-Muñoz, J. L., Lozano-Estevan, M. d. C., Cerrolaza-Tudanca, S., Rozalén-Bustín, M., Fernández-Carnero, S., & García-Fernández, P. (2022). Effects of Capacitive-Resistive Electric Transfer on Sports Performance in Paralympic Swimmers: A Stopped Randomized Clinical Trial. International Journal of Environmental Research and Public Health, 19(21), 14620. https://doi.org/10.3390/ijerph192114620










