Abstract
Pap smear screening can detect cervical cancer early, but is underutilized. Motivational factors play a role in ensuring that women undergo Pap smear screening. This study was conducted to validate the adapted instrument, which was based on the protection motivation theory (PMT), into the Malay language to evaluate the motivational factors for Pap smear screening among women. The original 26-item PMT scale was developed based on seven constructs of the PMT framework. The adaptation involved translation by bilingual experts (n = 4), followed by synthesis (n = 6). Subsequently, we performed content validation (content validation index, CVI) among the health experts (n = 5) and face validation (face validation index, FVI) among women (n = 11). Reliability testing for internal consistency was determined via the confirmatory factor analysis (CFA) of women aged between 21 and 65 years (n = 150). One item was deleted based on the expert consensus, leaving a total of 25 items after the adaptation. The validation yielded a good CVI and FVI. Prior to CFA reliability testing, one item was deleted due to very low factor loading. The CFA indicated a good fit for 24 items. The factor loading (range: 0.45–0.98), average variance extracted (range: 0.44–0.90), and composite reliability (range: 0.69–0.97) indicated that the convergent validity for each construct was acceptable, except for the perceived vulnerability. However, the perceived vulnerability construct was accepted based on expert verification. We confirmed that the translation, cross-cultural, adaptation, and validation of the Malay-version PMT scale were valid and reliable. The scale contains 24 items that represent the seven constructs of the PMT framework.
1. Introduction
Cervical cancer (CC) remains a reproductive health burden and a global health issue. The World Health Organization (WHO) presented a global strategy toward eliminating CC from public health concerns. The vision included a threshold age-standardized rate (ASR) of 4.0 per 100,000 women, with 70% of women screened before the age of 35 years and rescreened by 45 years [1]. Almost 90% of death due to CC occurs in developing countries and low- to middle-income countries (LMICs) as a consequence of the less successful implementation of screening methods [2,3,4]. In Malaysia, 1 in 144 women is diagnosed with CC at an ASR of 6.2 per 100,000 women [5]. The coverage of women undergoing Pap smear screening in Malaysia in 2014–2018 (i.e., 5 years) remained below 40% (23–26%) [6]. The availability of free screening programs at health clinics throughout Malaysia has failed to encourage women to undergo Pap smear screening.
In light of this, motivational factors may play a role in improving the CC screening rate among Malaysian women. The protection motivation theory (PMT) explains how an individual is motivated toward self-protection against health threats [7,8,9]. The PMT framework has been proven to motivate women toward increasing the CC screening rates [10,11,12]. The framework assumes that protection motivation (the individual’s intention to perform a behavior) results from two appraisal processes: The positive function, which includes perceived vulnerability, perceived severity, self-efficacy, and response efficacy; and the negative function of the rewards associated with fear (threat appraisal) and the response costs (coping appraisal) of the adaptive behavior.
The factors that influence knowledge, attitude, awareness, and barriers to CC and Pap smear screening in Malaysia have been identified [13,14,15]. They include less knowledge on the causes and clinical manifestations of CC [13,14] and insufficient information from health care professionals regarding CC and Pap smear screening [13,14]. The factors associated with uptake of Pap smear screening include taking hormonal contraception, higher knowledge and attitude scores [14], and the use of text reminders as educational material [15]. However, there has been no investigation into the motivation and personal potential variables. Hence, we assessed how motivation can influence screening behavior by translating the available PMT scale [16] into the Malay language and performed cross-cultural adaptation.
The original PMT scale was developed by Laleh Hassani in 2014 for Iranian women to measure the intention for the first Pap smear screening [16]. The instrument is a theory-based framework that is suitable for developing educational intervention material on Pap smear screening [12]. This new Malay-version PMT scale can be used as an instrument to assess women’s motivation toward Pap smear screening and guide the development of an intervention module in the future.
2. Methods
Overview: In order to produce a Malay-version PMT, this study performed the adaptation process including the translation process and synthesis. We further validated the cross-cultural adaptation items via content validation by expert and face validation by women. The validated item was tested for reliability testing using confirmatory factor analysis (CFA) before the finalized Malay-version PMT was formed.
The original PMT scale consists of 26 items encompassing seven constructs scored on a 5-point Likert scale from 0 (completely disagree) to 5 (completely agree). The score is calculated based on individual constructs and can range from 2 to 30. The seven constructs are: perceived vulnerability, perceived severity, response efficacy, self-efficacy, fear (threat appraisal), response cost (coping appraisal), and behavioral intention (protection motivation) toward Pap smear screening. The exploratory factor analysis (EFA) performed by the original author affirmed that the developed PMT scale had a suitable structure [Kaiser–Meyer–Olkin = 0.82; Bartlett’s test of sphericity = 3911.78 (degree of freedom [df] = 406, p < 0.0001)] and the seven constructs jointly accounted for 72.76% of the variance [16]. The EFA is appropriate for scale development, in order to identify the nature of the constructs whereas the CFA is preferred for measurement models or to establish the validity of a set of measures [17,18]. The nature of constructs was discovered by the original author, thus this study proceeded with CFA to test the adaptation set of constructs for internal consistency. We used IBM SPSS Amos version 24 for the statistical analysis.
Permission to use and translate the PMT scale into Malay was obtained from the corresponding author. Creating the Malay-version PMT scale began with adaptation, which included forward- and back-translation and synthesis. This was followed by validation, which consisted of content validity, face validity, and reliability testing.
2.1. Adaptation
The original PMT scale was adapted based on the cross-cultural adaptation by referring to the guidelines of Beaton and Bombardier [19] and consist of translation, synthesis, back-translation, expert committee review, and pre-testing for an understanding of the items.
2.2. Translation
The forward- and back-translation involved four bilingual expert translators with the following qualifications: Masters in Education and Professional Studies, Master of Education in TESL (Teaching English as a Second Language), or Bachelor of Education [Teaching English to Speakers of Other Languages (TESOL)]. The forward-translation (from English to Malay) was conducted by two expert bilingual translators and each translator produced a report of the translation. This was followed by a back-translation (Malay to English) by another two expert bilingual translators, and two translation reports were produced independently.
2.3. Synthesis
The four translation reports were combined into one document after a thorough discussion between the translators and two public health physicians to address any gaps or differences between the respective reports. The process included the decision for the best Malay word to be used that was easy to understand, and suitable phrases for adaptation into the Malaysian culture.
2.4. Validation
2.4.1. Content Validity
Content validation began with a panel of five experts competent in both languages (consisting of a gynecologist, public health physician, family medicine specialist, public health nurse, and health educator information officer) who reviewed the final synthesized report of the translation by comparing each item in both languages (i.e., Malay and English versions). The experts were also asked to check the content of the PMT scale to ensure that the items were culturally appropriate to the Malaysian population.
After completing the cultural adaptation, the experts assessed the content validity index (CVI) to calculate the item-level content validity index (I-CVI) and the scale-level content validity index-average (SCVI-average). The CVI is an index of inter-rater agreement among experts. The experts were asked to evaluate whether the items of the PMT scale were relevant, clear, and essential by rating each item on a 4-point Likert scale (1 = not relevant, 2 = somewhat relevant, 3 = quite relevant, 4 = very relevant). Items with a rating of 1 and 2 were considered invalid and items with a rating of 3 and 4 were considered valid. The CVI was computed by calculating the scale average. An I-CVI of 0.78 and SCVI-average of ≥0.90 indicated that the item had good content validity [20].
2.4.2. Face Validity
Eleven women aged 21–65 years and of different ethnicities, residence locations (urban or rural), education levels, and occupational statuses were purposively selected for pre-testing on face validation for understanding of the items. The face validation testing was aimed at assessing the clarity and comprehensibility of the translated items. The women were required to award scores from 1 (item not clear and not understandable) to 4 (item very clear and understandable) based on the clarity and comprehensibility of the translated items in the PMT scale. Scores of 3 and 4 were recategorized as 1 (clear and understandable) and scores of 1 and 2 were recategorized as 0 (not clear and understandable). The face validity index (FVI) was computed by calculating the scale average [20].
2.5. Reliability Testing
Reliability testing for internal consistency via confirmatory factor analysis (CFA) was conducted online through Google Forms in multiple WhatsApp groups among 150 women aged 21–65 years throughout Malaysia. The sample size should be greater than the number of items (i.e., N > p), with the recommended N:p ratios ranging from 5 with a minimum N > 100 [21,22]. As the PMT scale contained a total of 26 items, the sample size of 150 was adequate and exceeded the minimum sample requirement of 130.
As previous studies have determined the factors and items of the PMT scale [16], we only conducted a confirmatory study of the translated PMT scale among the 150 women. The study aimed at confirming whether the seven constructs involving the 26 items fit the measurement model well. To achieve good psychometric characteristics, high standardized factor loadings (>0.40) are preferred [23,24]. Higher factor loading values indicate higher levels of reliability. Values between 0.60 and 0.70 are considered to be “acceptable in exploratory research” and values of 0.70–0.90 range from “satisfactory” to “good” [24].
Additionally, we examined the average variance extracted (AVE) regarding the grand mean value of the squared loadings of the indicators associated with the construct. An AVE of ≥0.50 indicates that the construct explains ≥50% percent of the variance of the indicators that comprise the construct [24]. The composite reliability (CR) represents the aggregation of the indicators under a latent variable with a value that should be >0.6 [24,25]. If the AVE is <0.5 but the CR is >0.6, the convergent validity of the construct remains adequate [26]. To confirm the fitness of the CFA measurement model, the fitness of the measurement model for the construct validity assessment was required to yield the following values: comparative fit index (CFI) and goodness fit index (GFI) > 0.90, root mean square error of approximation (RMSEA) < 0.08, and chi-square (ChiSq/df) < 5 [26,27].
3. Results
3.1. Cross-Cultural Adaptation
Prior to the forward and back-translation and synthesis, several changes were made to adapt the PMT scale to the Malaysian culture. The term “husband” in item PS3 was changed to “partner”, as unmarried women who are sexually active should also undergo CC screening. Item SE1 was deleted as the statement was more toward the behavioral intention rather than self-efficacy. Furthermore, the word “periodically” was added to item SE7 to emphasize the need for repeat screening. Items PM1 and PM2 were repositioned because the “intend” statement should precede the “plan” statement (Table 1).

Table 1.
The cross-cultural adaptation, content validity, and face validity index of the Malay version of the PMT scale.
3.2. Content Validity and Face Validity Index
The inter-expert CVI was 0.8–1 with an SCVI-average of 0.90. The inter-women FVI was 0.8–1 with an SFVI-average of 0.95. The results were considered to indicate good CVI and FVI [20]. Table 1 shows the cross-cultural adaptation, synthesis changes, CVI, and FVI of the Malay version of the PMT scale.
3.3. Descriptive Analysis for Reliability Testing
Table 2 lists the characteristic profiles of the women involved in the reliability testing. The mean age was 39.5 years (SD 9.69), the majority were of Malay ethnicity (78%), married (78.7%), had higher education levels (74.7%), were employed (70.7%), had a personal income of <MYR4851 (68%), and were urban residents (70.7%). The majority were sexually active (76.7%), had heard of CC screening (96.7%), and had not undergone CC screening in the last 3 years (70%).

Table 2.
The demographic profile of women for reliability testing.
Normal data distribution was confirmed using basic descriptive analyses examining the pattern and shape of the sample distribution on the PMT scale. Table 3 lists the analyses results. The mean score for each construct was as follows: perceived vulnerability, 11.56 (SD 2.18); perceived severity, 15.82 (SD 2.78); fear (threat appraisal), 8.30 (SD 3.41); response costs (coping appraisal), 6.03 (SD 2.54); response efficacy, 17.69 (SD 2.81); self-efficacy, 22.85 (SD 5.53); and protection motivation, 12.72 (SD 3.04). The skewness and kurtosis values were within the acceptable range of normal distribution of the dataset score from −2 to +2 [28].

Table 3.
The description of the PMT scale construct.
3.4. Confirmatory Factor Analysis
The CFA was performed on 25 items of the PMT scale after one item had been deleted during the synthesis changes of cross-cultural adaptation. Factor loading for all items was >0.4 and ranged from 0.45 (PS4) to 0.98 (PM3); the exceptions were for items PV1 (0.07) and PV3 (0.37). Item PV1 was eliminated from the measurement model due to the very low factor loading. Item PV3 was maintained as its factor loading was close to 0.4 if rounded and because the item was required for complementing the perceived vulnerability construct, as suggested by the expert verification (Table 4).

Table 4.
The confirmation factor analysis (CFA).
The Cronbach’s alpha, AVE, and CR for all constructs was accepted based on their values of >0.6, 0.4, and 0.6 respectively. Thus, the convergent validity was accepted for perceived severity, fear (threat appraisal), response cost (coping appraisal), response efficacy, self-efficacy, and protection motivation. The exception was perceived vulnerability, which yielded an alpha = 0.35, AVE = 0.24, and CR = 0.37, which were less than the expected value. Due to the need to retain the construct, verification was obtained from the same expert in the cross-cultural adaptation. Table 4 shows the overall CFA results.
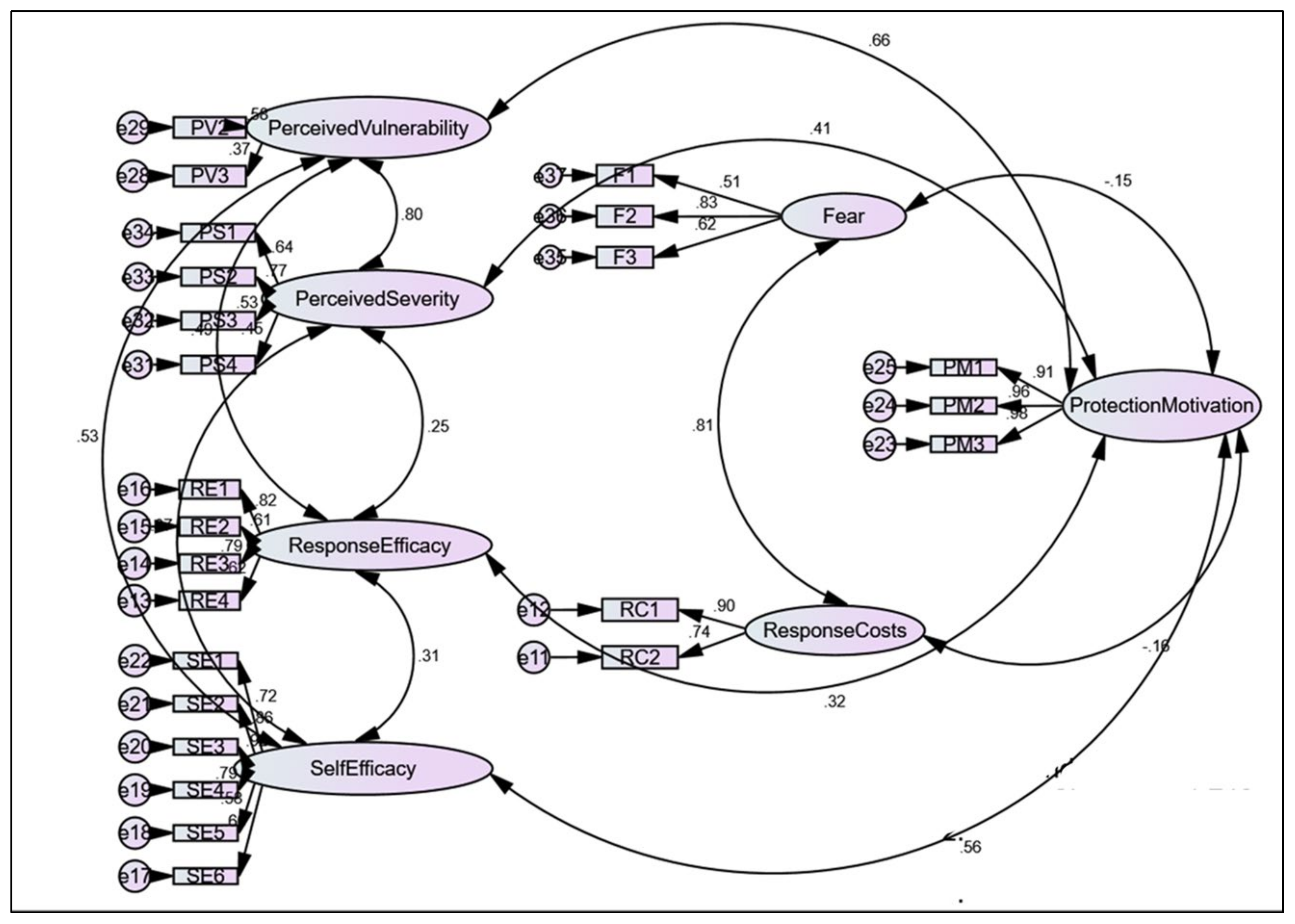
After deleting item PV1, the fitness of the measurement model for construct validity assessment was fit based on the ChiSq/df = 1.746; RMSEA = 0.071; GFI = 0.814, and CFI = 0.906. Table 5 summarizes the difference before and after PV1 deletion according to the description of the fitness indices. Figure 1 presents the finalized overview of the CFA among the seven constructs and 24 items of the Malay-version PMT scale.

Table 5.
The fitness of measurement model for the construct validity assessment.
Figure 1.
The finalized overview of the confirmatory factor analysis. The circle shape represents the unobserved variables, the rectangle shape represents the observed variables of PMT items (PV = perceived vulnerability, PS = perceived severity, RE = response efficacy, SE = self-efficacy, F = fear, RC = response costs, PM = protection motivation) and the oval shape represents the seven PMT constructs. The double headed arrow shows the correlation between the PMT construct.
4. Discussion
The translation, cross-cultural adaptation, and validation of the Malay-version PMT scale yielded satisfactory reliability and validity results for the 24 items when tested among women throughout Malaysia. One item of the self-efficacy construct (I will take have the Pap) was deleted during cross-cultural adaptation. Ideally, the adaptation of the questionnaire into a different culture can affect the actual meaning of the words. The original PMT scale was in Farsi [16] and the item “I will take have the Pap” was acceptable as a self-efficacy construct based on the local context. However, the content validity expert in the present study stated that the item was more appropriate as a protection motivation (intention) construct when translated into Malay. The translation process may encounter difficulty when two different languages have nonequivalent words and may lead to different meanings [29]. In addition, the cross-cultural adaptation process not only focuses on the translation, but also on an appropriate cultural adaptation that is suitable for a new setting [19]. The justification to the adaptation process is the ability to place the host culture [30] as well as achieve a balance between the original source and the new version of the adaptation [19]. Thus, the decision to delete the item was appropriate.
One item of the perceived vulnerability construct (I do not have any problems in my reproduction organ, so it is impossible to have cervical cancer) was deleted during CFA reliability validation due to the very low factor loading (0.07). After deleting the item, the fitness of measurement model for the construct validity assessment was fit (ChiSq/df = 1.746, RMSEA = 0.071, GFI = 0.814, CFI = 0.906). The item was identified as a reverse code item during the translation. Thus, this might have affected the women’s understanding when selecting the appropriate scale for the item and resulted in the very low factor loading of the CFA. The other item of perceived vulnerability construct (Among my relatives, no one has cervical cancer and neither do I) was accepted, even though the factor loading was 0.37, which was slightly less than the acceptable value (>0.4). This item needed to be retained to achieve the perceived vulnerability construct. Prior to the expert’s content validation, the translation of the item into Malay was meaningful and the item was necessary to evaluate the perceived vulnerability construct. The decision on whether to delete or retain an item was subject to the content validity expert, wherein weaker loadings could be retained [24].
Based on our results, the Malay-version PMT scale was acceptable for Malaysian women in different demographic settings. Our selection criteria were women aged 21–65 years who were eligible for CC screening without limiting for other factors. Our aim was to test the clarify and reliability of the adapted validated instrument among Malaysian women. Thus, the reliability testing was conducted electronically via Google Forms in multiple WhatsApp groups throughout Malaysia. With this method, we were able to eliminate geographic barriers and capture a variety of demographic settings. The majority of our respondents were Malay, with higher education levels, and from urban areas. Nevertheless, the characteristics of the other ethnicities also contributed to the finalized CFA model. Mohamad Marzuki [29], who used the same approach via WhatsApp groups, also captured the same respondent characteristics that we did.
Malaysia has a multi-ethnic population that uses Malay as the national language. To identify the clarity of the content, we selected Chinese and Indian women as representatives of other ethnic groups during the face validation. The I-FVI (0.8–1.0) and SFVI-average (0.95) proved the clarity of the items among a multi-ethnic group. Furthermore, the involvement of 22% non-Malay respondents (Chinese, Indian, natives of Sabah, and natives of Sarawak) in the reliability testing also contributed to the acceptance-finalized model of the CFA. This respondent heterogeneity may be extended to the findings and can be generalized to all Malaysian women.
Although our findings confirmed the finalized fitness model of the Malay-version PMT scale, the use of Google Forms during the reliability testing might have affected our findings. The respondents answered the online questionnaire without guidance and this could have affected their understanding of the items. This limitation could also have affected the deleted item.
5. Conclusions
We confirmed that the translated, cross-culturally adapted, and validated Malay-version PMT scale as a valid and reliable tool to be used in the Malaysian population. This 24-item instrument represents the seven constructs based on the PMT framework: perceived vulnerability, perceived severity, fear (threat appraisal), response cost (coping appraisal), response efficacy, self-efficacy, and protection motivation (intention). The Malay-version PMT scale is valid for assessing women’s motivation toward CC screening. Further research is needed to explore the promotion of lifelong screening among women and developing tailored interventions based on the PMT scale.
Author Contributions
Conceptualization, R.R., A.M.N. and E.M.W.M.; Data curation, R.R., A.M.N., R.A.R. and K.T.C.; Formal analysis, R.R. and A.M.N.; Methodology, A.M.N. and E.M.W.M.; Supervision, A.M.N., R.A.R. and K.T.C.; Validation, R.R., E.M.W.M. and S.M.H.; Writing—original draft, R.R.; Writing—review and editing, R.R., A.M.N., R.A.R., K.T.C., S.M.H. and E.M.W.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by UNIVERSITI KEBANGSAAN MALAYSIA (grant number FF-2021-499).
Institutional Review Board Statement
The validation process was part of the clinical research approved by the Universiti Kebangsaan Malaysia Medical Research Ethics Committee (protocol code: FF-2021-499; date of approval: 29 October 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available in this article.
Acknowledgments
We thank the Universiti Kebangsaan Malaysia for the support and technical guidance in conducting this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gultekin, M.; Ramirez, P.T.; Broutet, N.; Hutubessy, R. World Health Organization call for action to eliminate cervical cancer globally. Int. J. Gynecol. Cancer 2020, 30, 426–427. [Google Scholar] [CrossRef] [Green Version]
- Cohen, P.A.; Jhingran, A.; Oaknin, A.; Denny, L. Cervical cancer. Lancet 2019, 393, 169–182. [Google Scholar] [CrossRef]
- Smith, R.A.; Andrews, K.S.; Brooks, D.; Fedewa, S.A.; Manassaram-Baptiste, D.; Saslow, D.; Wender, R.C. Cancer screening in the United States 2019: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J. Clin. 2019, 69, 184–210. [Google Scholar] [CrossRef] [PubMed]
- Curry, S.J.; Krist, A.H.; Owens, D.K.; Barry, M.J.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Kubik, M.; et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA 2018, 320, 674–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Institut Kanser Negara. Summary of Malaysia National Cancer, Registry Report 2012–2016; Institut Kanser Negara: Putrajaya, Malaysia, 2019. [Google Scholar]
- National Health and Morbidity Survey (NHMS). Fact Sheet: National Health and Morbidity Survey 2019, Non-Communicable Diseases, Health Care Demand and Health Literacy; Ministry of Health Malaysia: Shah Alam, Malaysia, 2020. [Google Scholar]
- Pourebrahim-Alamdari, P.; Mehrabi, E.; Nikkhesal, N.; Nourizadeh, R.; Esmaeilpour, K.; Mousavi, S. Effectiveness of motivationally tailored interventions on cervical cancer screening: A systematic review and meta-analysis. Int. J. Womens Health Reprod. Sci. 2021, 9, 86–90. [Google Scholar] [CrossRef]
- Chamroonsawasdi, K.; Chottanapund, S.; Tunyasitthisundhorn, P.; Phokaewsuksa, N.; Ruksujarit, T.; Phasuksathaporn, P. Development and validation of a questionnaire to assess knowledge, threat and coping appraisal, and intention to practice healthy behaviors related to non-communicable diseases in the Thai population. Behav. Sci. 2017, 7, 20. [Google Scholar] [CrossRef] [Green Version]
- Rogers, R.W. Cognitive and psychological processes in fear appeals and attitude change: A revised theory of protection motivation. In Social Psychophysiology: A Sourcebook; Guilford: New York, NY, USA, 1983; pp. 153–176. [Google Scholar]
- Bai, Y.; Liu, Q.; Chen, X.; Gao, Y.; Gong, H.; Tan, X.; Zhang, M.; Tuo, J.; Zhang, Y.; Xiang, Q.; et al. Protection motivation theory in predicting intention to receive cervical cancer screening in rural Chinese women. Psycho-Oncology 2018, 27, 442–449. [Google Scholar] [CrossRef]
- Malmir, S.; Barati, M.; Jeihooni, A.K.; Bashirian, S.; Hazavehei, S.M.M. Effect of an educational intervention based on protection motivation theory on preventing cervical cancer among marginalized women in west Iran. Asian Pac. J. Cancer Prev. 2018, 19, 755. [Google Scholar]
- Dehdari, T.; Hassani, L.; Hajizadeh, E.; Shojaeizadeh, D.; Nedjat, S.; Abedini, M. Effects of an educational intervention based on the protection motivation theory and implementation intentions on first and second pap test practice in Iran. Asian Pac. J. Cancer Prev. 2014, 15, 7257–7261. [Google Scholar] [CrossRef] [Green Version]
- Seng, L.M.; Rosman, A.N.; Khan, A.; Haris, N.M.; Mustapha, N.A.S.; Husaini, N.S.M.; Zahari, N.F. Awareness of cervical cancer among women in Malaysia. Int. J. Health Sci. 2018, 12, 42. [Google Scholar]
- Romli, R.; Shahabudin, S.; Saddki, N.; Mokhtar, N. Cervical cancer and pap smear screening: Knowledge, attitude and practice among working women in northern state of Malaysia. Med. J. Malays. 2019, 74, 8–14. [Google Scholar]
- Romli, R.; Shahabudin, S.; Saddki, N.; Mokhtar, N. Effectiveness of a health education program to improve knowledge and attitude towards cervical cancer and pap smear: A controlled community trial in Malaysia. Asian Pac. J. Cancer Prev. 2020, 21, 853. [Google Scholar] [CrossRef]
- Hassani, L.; Dehdari, T.; Hajizadeh, E.; Shojaeizadeh, D.; Abedini, M.; Nedjat, S. Development of an instrument based on the protection motivation theory to measure factors influencing women’s intention to first pap test practice. Asian Pac. J. Cancer Prev. 2014, 15, 1227–1232. [Google Scholar] [CrossRef] [Green Version]
- DeCoster, J. Overview of Factor Analysis; University of Alabama: Tuscaloosa, AL, USA, 1998. [Google Scholar]
- Hurley, A.E.; Scandura, T.A.; Schriesheim, C.A.; Brannick, M.T.; Seers, A.; Vandenberg, R.J.; Williams, L.J. Exploratory and confirmatory factor analysis: Guidelines, issues, and alternatives. J. Organ. Behav. 1997, 18, 667–683. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [Green Version]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef]
- Dimitrov, D.M. Statistical Methods for Validation of Assessment Scale Data in Counseling and Related Fields; John Wiley & Sons: New York, NY, USA, 2014. [Google Scholar]
- Kyriazos, T.A. Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology 2018, 9, 2207. [Google Scholar] [CrossRef] [Green Version]
- DeVon, H.A.; Block, M.E.; Moyle-Wright, P.; Ernst, D.M.; Hayden, S.J.; Lazzara, D.J.; Savoy, S.M.; Kostas-Polston, E. A psychometric toolbox for testing validity and reliability. J. Nurs. Scholarsh. 2007, 39, 155–164. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Dash, G.; Paul, J. CB-SEM vs. PLS-SEM methods for research in social sciences and technology forecasting. Technol. Forecast. Soc. Change 2021, 173, 121092. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J. RE Anderson Multivariate Data Analysis: A Global Perspective; Pearson Prentice Hall: Hoboken, NJ, USA, 2010. [Google Scholar]
- Hair, J.F.; Babin, B.J.; Anderson, R.E.; Black, W.C. Multivariate Data Analysis, 8th ed.; Cengage Learning EMEA: Hampshire, UK, 2019. [Google Scholar]
- Marzuki, M.F.M.; Yaacob, N.A.; Yaacob, N.M. Translation, cross-cultural adaptation, and validation of the Malay version of the system usability scale questionnaire for the assessment of mobile apps. JMIR Hum. Factors 2018, 5, e10308. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.Y. Cross-cultural adaptation. In Oxford Research Encyclopedia of Communication; Oxford University Press: Oxford, UK, 2017. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).