Associations of Place-Based Factors with Service Use and Consumer-Reported Unmet Service Needs Among Older Adults Using Publicly Funded Home- and Community-Based Services in the United States
Abstract
1. Introduction
1.1. Conceptual Framework
2. Methods
2.1. Data Source and Survey Methods
2.2. Study Sample
2.3. Ascertainment of Main Outcomes: HCBS Use and Consumer-Reported Unmet HCBS Needs
2.4. Ascertainment of Place-Based Factors (Independent Variables)
- Education: (i) Percent population who are high school dropouts (includes people of compulsory school attendance age or above who were not enrolled in school and were not high school graduates).
- Economic stability: (i) Percent non-employed for population aged 16–64 years [measured as (not in labor force + unemployed between 16 and 64 years)/(civilian + not in labor force between 16 and 64 years)]. (ii) Percent population in households earning less than 100% of the federal poverty line. We included poverty among adults aged < 65 years as a ZIP code-level indicator of economic stability because this measure, while not specific to older adults, reflects broader community economic conditions that influence the availability of informal caregivers and local workforce capacity; factors that indirectly affect HCBS access and adequacy for the older population.
- Social context: (i) Percent population white, Black, and Hispanic in the area. (ii) Percent population foreign-born (i.e., born outside the United States). (iii) Percent single-parent families with dependents aged < 18 years. (iv) Percent “high-needs” population (includes proportion of residents in an area who are aged 65 years and older, women, or children < 5 years).
- Neighborhood and physical environment: (i) Percent households living in crowded housing units [measured as (tenure by occupants per room − (owner-occupied + renter-occupied))/(total occupied housing units)]. (ii) Percent households with no vehicle (as an indicator of access to transportation).
- Healthcare service access: As an indicator for telehealth capability, we evaluated 2 PBFs—internet access and broadband service coverage: (i) Internet access was determined by asking if any member of the household has access to the internet; “access” refers to whether or not someone in the household uses or can connect to the internet, regardless of whether or not they pay for the service. (ii) Similarly access to broadband services was asked in a follow-up question to internet access, with broadband (high-speed) internet service referring to cable, fiber optic, or DSL (digital subscriber line) mode of high-speed internet service delivery. (iii) In regard to the availability of social services, we ascertained the median total number of all social services available in an area and median total number of elderly/disabled social services available in the entire ZIP code, available per square mile within the ZIP code, and per square mile within the ZIP code including only those services with at least one consumer.
2.5. Covariates
2.6. Statistical Analysis Plan
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- LeBlanc, A.J.; Tonner, M.C.; Harrington, C. Medicaid 1915(c) home and community-based services waivers across the states. Health Care Financ. Rev. 2000, 22, 159–174. [Google Scholar] [PubMed] [PubMed Central]
- Bercaw, L.E.; Levinson, A.; Fletcher, D.; Shuman, S.B.; Hughes, S.; Peddada, S.; Walsh, E.G. Assessing Disparities in Medicaid Home- and Community-Based Services: A Systematic Review. J. Aging Soc. Policy 2023, 35, 302–321. [Google Scholar] [CrossRef] [PubMed]
- Shippee, T.P.; Bucy, T.I.; Parikh, R.R.; Wolf, J.M.; Shewmaker, P.; Mulcahy, J.F.; Skarphol, T.; Giordano, S.; Isvan, N.; Jutkowitz, E. Service Utilization and Consumer-Reported Unmet Needs in Medicaid Home- and Community-Based Services for Older Adults. J. Aging Soc. Policy 2024, 16, 1–15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fabius, C.D.; Parikh, R.; Wolf, J.M.; Giordano, S.; Fashaw-Walters, S.; Jutkowitz, E.; Shippee, T. Racial and ethnic differences in unmet needs among older adults receiving publicly-funded home and community-based services. J. Am. Geriatr. Soc. 2024, 72, 3520–3529. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Parikh, R.R. How Social Determinants of Health Influence Health Promotion in Long-Term Care. In Health Promotion in Long-Term Care Facilities: The Present Scenario and Future Demands; Springer Nature: Cham, Switzerland, 2025; pp. 137–154. [Google Scholar]
- Fabius, C.D.; Okoye, S.M.; Wu, M.M.J.; Jopson, A.D.; Chyr, L.C.; Burgdorf, J.G.; Ballreich, J.; Scerpella, D.; Wolff, J.L. The Role of Place in Person- and Family-Oriented Long-Term Services and Supports. Milbank Q. 2023, 101, 1076–1138. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferris, R.E.; Glicksman, A.; Kleban, M.H. Environmental Predictors of Unmet Home-and Community-Based Service Needs of Older Adults. J. Appl. Gerontol. 2016, 35, 179–208. [Google Scholar] [CrossRef] [PubMed]
- Chong, N.; Akobirshoev, I.; Caldwell, J.; Kaye, H.S.; Mitra, M. The relationship between unmet need for home and community-based services and health and community living outcomes. Disabil. Health J. 2022, 15, 101222. [Google Scholar] [CrossRef] [PubMed]
- Caperon, L.; Saville, F.; Ahern, S. Developing a socio-ecological model for community engagement in a health programme in an underserved urban area. PLoS ONE 2022, 17, e0275092. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hinton, E.; Diana, A. Medicaid Authorities and Options to Address Social Determinants of Health [Internet]. Kaiser Family Foundation. 2024. Available online: https://www.kff.org/medicaid/issue-brief/medicaid-authorities-and-options-to-address-social-determinants-of-health-sdoh/ (accessed on 17 March 2025).
- Gaugler, J.E.; Borson, S.; Epps, F.; Shih, R.A.; Parker, L.J.; McGuire, L.C. The intersection of social determinants of health and family care of people living with Alzheimer’s disease and related dementias: A public health opportunity. Alzheimer’s Dement. J. 2023, 19, 5837–5846. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liang, Z.; Nau, C.; Xie, F.; Vogel, R.; Chen, W. The Application of Community-Based Information from the American Community Survey in a Large Integrated Health Care Organization. Perm. J. 2020, 25, 1–3. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 2003, 19, 716–723. [Google Scholar] [CrossRef]
- McFadden, D. Conditional Logit Analysis of Qualitative Choice Behavior. 1972. Available online: https://escholarship.org/content/qt61s3q2xr/qt61s3q2xr_noSplash_b3b3c42b0811c55fa76c45e7743d1a91.pdf (accessed on 17 March 2025).
- Siconolfi, D.; Shih, R.A.; Friedman, E.M.; Kotzias, V.I.; Ahluwalia, S.C.; Phillips, J.L.; Saliba, D. Rural-Urban Disparities in Access to Home- and Community-Based Services and Supports: Stakeholder Perspectives From 14 States. J. Am. Med. Dir. Assoc. 2019, 20, 503–508.e1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miyawaki, C.E.; McClellan, A.; Russell, D.; Bouldin, E.D. Comparing Unmet Service Needs Between Rural and Urban Family Caregivers of People Living with Alzheimer’s Disease and Related Dementias: A Multisite Study. Gerontologist 2024, 64, gnae083. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Weaver, R.H.; Roberto, K.A. Location Matters: Disparities in the Likelihood of Receiving Services in Late Life. Int. J. Aging Hum. Dev. 2021, 93, 653–672. [Google Scholar] [CrossRef] [PubMed]
- Karlin, N.J. Older adult service usage assessment: Evidence from two rural samples. Act. Adapt. Aging 2018, 42, 305–327. [Google Scholar] [CrossRef]
- Utz, R.L. Caregiver Respite: An Essential Component of Home- and Community-Based Long-Term Care. J. Am. Med. Dir. Assoc. 2022, 23, 320–321. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Green, M.R.; Hughes, M.C.; Afrin, S.; Vernon, E. Caregiver policies in the United States: A systematic review. J. Public Health Policy 2025, 46, 22–37. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leocadie, M.C.; Roy, M.H.; Rothan-Tondeur, M. Barriers and enablers in the use of respite interventions by caregivers of people with dementia: An integrative review. Arch. Public Health 2018, 76, 72. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Che, R.P.; Cheung, M.C. Factors Associated with the Utilization of Home and Community-Based Services (HCBS) Among Older Adults: A Systematic Review of the Last Decade. J. Gerontol. Soc. Work 2024, 67, 776–802. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.S. The relationship between older Americans act in-home services and low-care residents in nursing homes. J. Aging Health 2014, 26, 250–260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kind, A.J.; Jencks, S.; Brock, J.; Yu, M.; Bartels, C.; Ehlenbach, W.; Greenberg, C.; Smith, M. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann. Intern. Med. 2014, 161, 765–774. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lusk, J.B.; Blass, B.; Mahoney, H.; Hoffman, M.N.; Clark, A.G.; Bae, J.; Ashana, D.C.; Cox, C.E.; Hammill, B.G. Neighborhood socioeconomic deprivation, healthcare access, and 30-day mortality and readmission after sepsis or critical illness: Findings from a nationwide study. Crit. Care 2023, 27, 287. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coughlin, S.S.; Clary, C.; Johnson, J.A.; Berman, A.; Heboyan, V.; Benevides, T.; Moore, J.; George, V. Continuing Challenges in Rural Health in the United States. J. Environ. Health Sci. 2019, 5, 90–92. [Google Scholar] [PubMed] [PubMed Central]
- Dill, J.; Henning-Smith, C.; Zhu, R.; Vomacka, E. Who Will Care for Rural Older Adults? Measuring the Direct Care Workforce in Rural Areas. J. Appl. Gerontol. 2023, 42, 1800–1808. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Leifheit-Limson, E.C.; Fine, J.; Pandolfi, M.M.; Gao, Y.; Liu, F.; Eckenrode, S.; Lichtman, J.H. National Trends and Geographic Variation in Availability of Home Health Care: 2002–2015. J. Am. Geriatr. Soc. 2017, 65, 1434–1440. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fabius, C.D.; Okoye, S.M.; Mulcahy, J.; Burgdorf, J.G.; Wolff, J.L. Associations Between Use of Paid Help and Care Experiences Among Medicare-Medicaid Enrolled Older Adults with and Without Dementia. The journals of gerontology. Ser. B Psychol. Sci. Soc. Sci. 2022, 77, e216–e225. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Konetzka, R.T.; Ellis, E.; Ghazali, N.; Wang, S. The relationship between Medicaid policy and realized access to home- and community-based services. Home Health Care Serv. Q. 2024, 43, 154–172. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Golant, S.M. Aging in the Right Place; Health Professions Press: Baltimore, MD, USA, 2015. [Google Scholar]
- Tine Buffel Phillipson, C. Ageing in Place in Urban Environments; Routledge: Oxfordshire, UK, 2023. [Google Scholar] [CrossRef]
- Versey, H.S. Perceptions of community among suburban and urban-dwelling adults aging in place. J. Aging Stud. 2021, 59, 100969. [Google Scholar] [CrossRef] [PubMed]
- Van Vleet, S.; de Medeiros, K. The Gentrification Acceleration Press Schema: A Critical Examination of Gentrification-Induced Displacement in Later Life. Gerontologist 2025, 65, gnaf107. [Google Scholar] [CrossRef] [PubMed]
- Bookman, A. Innovative models of aging in place: Transforming our communities for an aging population. Community Work. Fam. 2008, 11, 419–438. [Google Scholar] [CrossRef]
- Chung, S.; Kim, M.; Auh, E.Y.Y.; Park, N.S.S. WHO’s Global Age-Friendly Cities Guide: Its Implications of a Discussion on Social Exclusion among Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 8027. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Centers for Disease Control and Prevention. CDC’s New Healthy Aging Data Portfolio. MMWR 2013, 62, 754. [Google Scholar] [PubMed Central]
- Tan, M.; Hatef, E.; Taghipour, D.; Vyas, K.; Kharrazi, H.; Gottlieb, L.; Weiner, J. Including Social and Behavioral Determinants in Predictive Models: Trends, Challenges, and Opportunities. JMIR Med. Inform. 2020, 8, e18084. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Place-Based Factors | No Dementia | Dementia | ||||||
|---|---|---|---|---|---|---|---|---|
| Metropolitan N = 3251 | Micropolitan N = 685 | Small Town N = 404 | Rural N = 270 | Metropolitan N = 643 | Micropolitan N = 117 | Small Town N = 55 | Rural N = 31 | |
| % Consumers with high social needs (includes older adults of age 65 years or more, women, and children) * | 0.21 (0.19, 0.24) | 0.24 (0.21, 0.26) | 0.26 (0.23, 0.28) | 0.28 (0.24, 0.32) | 0.21 (0.19, 0.23) | 0.24 (0.21, 0.26) | 0.26 (0.24, 0.28) | 0.28 (0.24, 0.31) |
| % Black * | 0.09 (0.03, 0.30) | 0.02 (0.01, 0.05) | 0.01 (0.00, 0.03) | 0.00 (0.00, 0.01) | 0.09 (0.03, 0.26) | 0.02 (0.00, 0.04) | 0.01 (0.00, 0.05) | 0.00 (0.00, 0.01) |
| % Hispanic | 0.07 (0.04, 0.14) | 0.05 (0.02, 0.12) | 0.04 (0.02, 0.18) | 0.03 (0.01, 0.07) | 0.08 (0.03, 0.14) | 0.06 (0.02, 0.14) | 0.03 (0.02, 0.08) | 0.04 (0.02, 0.06) |
| % White * | 0.64 (0.40, 0.81) | 0.85 (0.75, 0.92) | 0.86 (0.68, 0.93) | 0.92 (0.81, 0.96) | 0.65 (0.39, 0.80) | 0.83 (0.74, 0.91) | 0.89 (0.72, 0.94) | 0.92 (0.79, 0.94) |
| % Foreign-born * | 0.07 (0.03, 0.14) | 0.03 (0.01, 0.06) | 0.02 (0.01, 0.04) | 0.01 (0.00, 0.02) | 0.08 (0.04, 0.15) | 0.03 (0.01, 0.06) | 0.02 (0.01, 0.04) | 0.01 (0.00, 0.02) |
| % Single-parent household | 0.16 (0.10, 0.22) | 0.14 (0.11, 0.17) | 0.13 (0.10, 0.18) | 0.09 (0.06, 0.14) | 0.14 (0.10, 0.21) | 0.16 (0.13, 0.19) | 0.12 (0.09, 0.16) | 0.11 (0.06, 0.15) |
| % Drop-out | 0.10 (0.06, 0.15) | 0.12 (0.08, 0.15) | 0.11 (0.08, 0.15) | 0.11 (0.07, 0.15) | 0.10 (0.06, 0.15) | 0.11 (0.09, 0.19) | 0.11 (0.08, 0.14) | 0.09 (0.07, 0.14) |
| % Below poverty | 0.13 (0.09, 0.21) | 0.15 (0.11, 0.19) | 0.15 (0.11, 0.19) | 0.13 (0.09, 0.19) | 0.11 (0.07, 0.18) | 0.15 (0.11, 0.21) | 0.14 (0.11, 0.19) | 0.11 (0.07, 0.19) |
| % Non-unemployed | 0.35 (0.32, 0.40) | 0.41 (0.36, 0.45) | 0.42 (0.38, 0.48) | 0.44 (0.38, 0.52) | 0.34 (0.31, 0.38) | 0.39 (0.36, 0.45) | 0.43 (0.37, 0.49) | 0.46 (0.36, 0.50) |
| % Unemployed | 0.053 (0.038, 0.072) | 0.049 (0.036, 0.061) | 0.043 (0.029, 0.060) | 0.043 (0.021, 0.065) | 0.050 (0.036, 0.068) | 0.048 (0.036, 0.067) | 0.047 (0.034, 0.064) | 0.033 (0.020, 0.073) |
| % Crowded housing | 0.021 (0.012, 0.034) | 0.017 (0.010, 0.027) | 0.017 (0.009, 0.032) | 0.014 (0.004, 0.027) | 0.020 (0.012, 0.035) | 0.020 (0.012, 0.034) | 0.020 (0.010, 0.031) | 0.012 (0.002, 0.033) |
| % Household with no car | 0.07 (0.04, 0.12) | 0.06 (0.05, 0.08) | 0.06 (0.04, 0.09) | 0.05 (0.03, 0.07) | 0.06 (0.04, 0.11) | 0.06 (0.05, 0.08) | 0.05 (0.03, 0.08) | 0.05 (0.03, 0.10) |
| Number of all social services available * | 34 (18, 56) | 28 (10, 43) | 11 (6, 17) | 2 (1, 5) | 32 (17, 53) | 23 (12, 38) | 13 (6, 21) | 2 (1, 4) |
| Number of social services per square mile, which have been purchased at least once * | 2.5 (0.6, 5.6) | 0.2 (0.1, 0.3) | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.0) | 2.3 (0.6, 4.7) | 0.2 (0.1, 0.2) | 0.1 (0.0, 0.1) | 0.0 (0.0, 0.0) |
| Number of elderly/disabled person services | 2 (1, 4) | 2 (1, 4) | 1 (0, 2) | 0 (0, 1) | 2 (1, 4) | 2 (0, 4) | 1 (0, 1) | 1 (0, 1) |
| Number of elderly/disabled person services per square mile, which have been purchased at least once * | 0.09 (0.01, 0.37) | 0.01 (0.00, 0.03) | 0.00 (0.00, 0.01) | 0.00 (0.00, 0.00) | 0.09 (0.01, 0.33) | 0.01 (0.00, 0.03) | 0.00 (0.00, 0.01) | 0.00 (0.00, 0.01) |
| Internet access | 0.86 (0.80, 0.90) | 0.81 (0.78, 0.84) | 0.79 (0.74, 0.82) | 0.77 (0.71, 0.81) | 0.87 (0.81, 0.92) | 0.81 (0.78, 0.84) | 0.79 (0.75, 0.82) | 0.79 (0.69, 0.82) |
| Broadband access | 0.85 (0.79, 0.90) | 0.81 (0.78, 0.84) | 0.79 (0.74, 0.82) | 0.77 (0.71, 0.80) | 0.87 (0.80, 0.91) | 0.81 (0.78, 0.84) | 0.78 (0.74, 0.81) | 0.78 (0.69, 0.81) |
| Characteristics | No Dementia | Dementia | ||||||
|---|---|---|---|---|---|---|---|---|
| Metropolitan N = 3251 | Micropolitan N = 685 | Small Town N = 404 | Rural N = 270 | Metropolitan N = 643 | Micropolitan N = 117 | Small Town N = 55 | Rural N = 31 | |
| Female (vs. not Female) * | 71% | 69% | 72% | 66% | 71% | 63% | 80% | 68% |
| Median Age (Interquartile Interval), Years | 74 (69, 81) | 74 (69, 81) | 74 (69, 80) | 74 (69, 82) | 81 (73, 87) | 80 (74, 85) | 81 (72, 88) | 79 (70, 87) |
| Physical Disability * | 58% | 65% | 66% | 62% | 59% | 55% | 57% | 66% |
| Unknown | 68 | 9 | 5 | 6 | 27 | 4 | 2 | 2 |
| Developmental Disability * | 3.1% | 2.7% | 3.8% | 3.1% | 4.9% | 6.4% | 9.8% | 0% |
| Unknown | 107 | 18 | 8 | 9 | 47 | 8 | 4 | 3 |
| Brain Injury * | 7.2% | 6.6% | 13% | 11% | 11% | 11% | 11% | 31% |
| Unknown | 97 | 19 | 6 | 4 | 41 | 8 | 2 | 2 |
| Mental Health Condition | 24% | 25% | 31% | 29% | 35% | 36% | 30% | 30% |
| Unknown | 56 | 10 | 5 | 2 | 37 | 9 | 2 | 1 |
| Multiple Chronic Conditions * | 19% | 22% | 29% | 24% | 73% | 69% | 67% | 81% |
| Medicare Enrollee * | 90% | 91% | 95% | 93% | 91% | 97% | 96% | 100% |
| Unknown | 346 | 60 | 27 | 27 | 78 | 14 | 7 | 3 |
| Marital Status * | ||||||||
| Single | 19% | 15% | 16% | 16% | 14% | 9.1% | 11% | 0% |
| Married/Domestic Partner | 18% | 17% | 22% | 21% | 27% | 21% | 24% | 29% |
| Separated/Divorced | 32% | 32% | 34% | 31% | 21% | 31% | 20% | 29% |
| Widowed | 31% | 36% | 28% | 32% | 39% | 39% | 44% | 43% |
| Unknown | 256 | 31 | 13 | 4 | 45 | 7 | 1 | 3 |
| Living Arrangement * | ||||||||
| Alone | 58% | 65% | 64% | 65% | 27% | 41% | 36% | 30% |
| Family | 38% | 33% | 33% | 32% | 61% | 48% | 57% | 63% |
| Other | 3.7% | 1.9% | 2.9% | 2.4% | 11% | 11% | 7.5% | 7.4% |
| Unknown | 84 | 14 | 25 | 18 | 24 | 3 | 2 | 4 |
| Race/Ethnicity * | ||||||||
| Black or African-American | 31% | 9.6% | 7.2% | 3.5% | 27% | 5.2% | 9.4% | 6.5% |
| Hispanic or Latino | 5.9% | 3.7% | 9.0% | 2.3% | 10% | 10% | 9.4% | 3.2% |
| White | 50% | 82% | 81% | 89% | 48% | 78% | 79% | 81% |
| Asian/Multiracial/Other | 12% | 4.5% | 3.3% | 5.4% | 15% | 6.1% | 1.9% | 9.7% |
| Unknown | 106 | 16 | 13 | 11 | 36 | 2 | 2 | 0 |
| Overall Health * | ||||||||
| Good | 32% | 32% | 33% | 32% | 27% | 31% | 35% | 35% |
| Poor/Fair | 58% | 58% | 50% | 53% | 64% | 56% | 56% | 52% |
| Very Good/Excellent | 9.8% | 9.7% | 17% | 15% | 9.1% | 13% | 9.3% | 13% |
| Unknown | 104 | 17 | 21 | 13 | 19 | 5 | 1 | 0 |
| Proxy Respondent * | 16% | 11% | 9.4% | 7.0% | 66% | 46% | 62% | 52% |
| No Dementia | Dementia | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Metropolitan N = 3251 | Micropolitan N = 685 | Small Town N = 404 | Rural N = 270 | Metropolitan N = 643 | Micropolitan N = 117 | Small Town N = 55 | Rural N = 31 |
| Service Use | ||||||||
| Personal Care * | 40% | 32% | 26% | 27% | 43% | 32% | 33% | 31% |
| Homemaker * | 20% | 23% | 32% | 36% | 14% | 20% | 22% | 26% |
| Delivered Meal | 32% | 37% | 28% | 32% | 30% | 34% | 37% | 26% |
| Adult Day Services * | 7.0% | 1.8% | 1.0% | 1.0% | 10% | 3.2% | 1.8% | 5.7% |
| Transportation | 5.5% | 6.2% | 4.2% | 6.6% | 5.4% | 5.0% | 4.4% | 1.4% |
| Caregiver Support | 1.6% | 3.7% | 1.2% | <0.1% | 4.2% | 7.6% | 4.6% | 2.5% |
| Unmet Service Needs | ||||||||
| Personal Care | 10% | 9.0% | 7.6% | 7.4% | 12% | 14% | 9.4% | 13% |
| Homemaker | 13% | 14% | 13% | 14% | 11% | 18% | 11% | 15% |
| Delivered Meal | 5.4% | 6.4% | 7.5% | 4.3% | 3.9% | 7.9% | 3.2% | 4.0% |
| Adult Day Services | 3.1% | 1.7% | 3.3% | 1.9% | 3.4% | 5.8% | 2.5% | 1.6% |
| Transportation | 10% | 9.3% | 9.9% | 12% | 6.5% | 11% | 3.4% | 11% |
| Caregiver Support * | 1.7% | 2.1% | 3.3% | 1.5% | 3.5% | 2.6% | 4.6% | 3.9% |
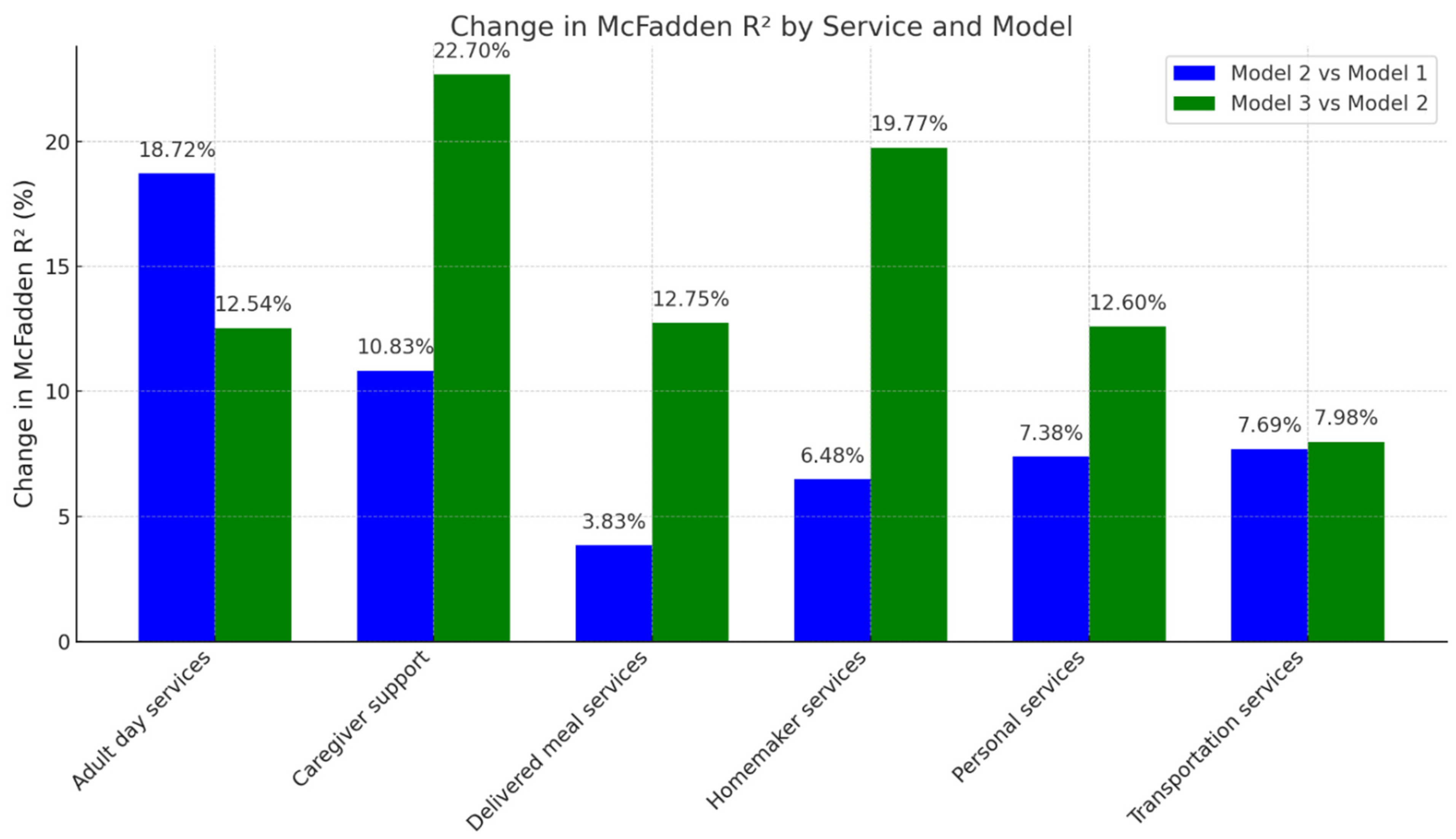
| Service | Model | Mean AIC | Mean McFadden R2 | Change in McFadden R2 (% Change from Previous Model) |
|---|---|---|---|---|
| Personal services | 1 | 6559.22 | 0.244 | NA |
| 2 | 6436.85 | 0.262 | 7.38 | |
| 3 | 6177.83 | 0.295 | 12.60 | |
| Homemaker services | 1 | 5209.37 | 0.247 | NA |
| 2 | 5133.69 | 0.263 | 6.48 | |
| 3 | 4801.23 | 0.315 | 19.77 | |
| Delivered meal services | 1 | 5982.73 | 0.287 | NA |
| 2 | 5918.06 | 0.298 | 3.83 | |
| 3 | 5628.73 | 0.336 | 12.75 | |
| Adult day services | 1 | 2227.03 | 0.235 | NA |
| 2 | 2134.64 | 0.279 | 18.72 | |
| 3 | 2058.82 | 0.314 | 12.54 | |
| Transportation services | 1 | 2146.25 | 0.221 | NA |
| 2 | 2133.19 | 0.238 | 7.69 | |
| 3 | 2106.11 | 0.257 | 7.98 | |
| Caregiver support | 1 | 993.30 | 0.314 | NA |
| 2 | 980.62 | 0.348 | 10.83 | |
| 3 | 894.06 | 0.427 | 22.70 |
| Service | Model | Mean AIC | McFadden R2 | Change in McFadden R2 (% Change from Previous Model) |
|---|---|---|---|---|
| Overall unmet need (all HCBS) | 1 | 6719.86 | 0.061 | NA |
| 2 | 6613.52 | 0.081 | 32.79 | |
| 3 | 6341.08 | 0.123 | 51.85 | |
| Personal services | 1 | 4060.85 | 0.050 | NA |
| 2 | 3988.27 | 0.075 | 50.00 | |
| 3 | 3859.31 | 0.111 | 48.00 | |
| Homemaker services | 1 | 4637.91 | 0.103 | NA |
| 2 | 4571.36 | 0.122 | 18.45 | |
| 3 | 4368.66 | 0.166 | 36.07 | |
| Delivered meal services | 1 | 2622.79 | 0.068 | NA |
| 2 | 2569.39 | 0.100 | 47.06 | |
| 3 | 2465.07 | 0.146 | 46.00 | |
| Adult day services | 1 | 1619.31 | 0.083 | NA |
| 2 | 1620.06 | 0.103 | 24.10 | |
| 3 | 1580.33 | 0.140 | 35.92 | |
| Transportation services | 1 | 3949.89 | 0.060 | NA |
| 2 | 3865.32 | 0.089 | 48.33 | |
| 3 | 3736.40 | 0.126 | 41.57 | |
| Caregiver support/respite | 1 | 1227.06 | 0.130 | NA |
| 2 | 1210.60 | 0.167 | 28.46 | |
| 3 | 1146.41 | 0.232 | 38.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shippee, T.P.; Parikh, R.R.; Musinguzi, N.; Langworthy, B.W.; Wolf, J.M.; Giordano, S.; Jutkowitz, E. Associations of Place-Based Factors with Service Use and Consumer-Reported Unmet Service Needs Among Older Adults Using Publicly Funded Home- and Community-Based Services in the United States. Int. J. Environ. Res. Public Health 2025, 22, 1461. https://doi.org/10.3390/ijerph22091461
Shippee TP, Parikh RR, Musinguzi N, Langworthy BW, Wolf JM, Giordano S, Jutkowitz E. Associations of Place-Based Factors with Service Use and Consumer-Reported Unmet Service Needs Among Older Adults Using Publicly Funded Home- and Community-Based Services in the United States. International Journal of Environmental Research and Public Health. 2025; 22(9):1461. https://doi.org/10.3390/ijerph22091461
Chicago/Turabian StyleShippee, Tetyana P., Romil R. Parikh, Nicholas Musinguzi, Benjamin W. Langworthy, Jack M. Wolf, Stephanie Giordano, and Eric Jutkowitz. 2025. "Associations of Place-Based Factors with Service Use and Consumer-Reported Unmet Service Needs Among Older Adults Using Publicly Funded Home- and Community-Based Services in the United States" International Journal of Environmental Research and Public Health 22, no. 9: 1461. https://doi.org/10.3390/ijerph22091461
APA StyleShippee, T. P., Parikh, R. R., Musinguzi, N., Langworthy, B. W., Wolf, J. M., Giordano, S., & Jutkowitz, E. (2025). Associations of Place-Based Factors with Service Use and Consumer-Reported Unmet Service Needs Among Older Adults Using Publicly Funded Home- and Community-Based Services in the United States. International Journal of Environmental Research and Public Health, 22(9), 1461. https://doi.org/10.3390/ijerph22091461






