Effect of Biomass Fuel Use on Neonatal Outcomes: A Cohort Study of Pregnant Females
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Study Population
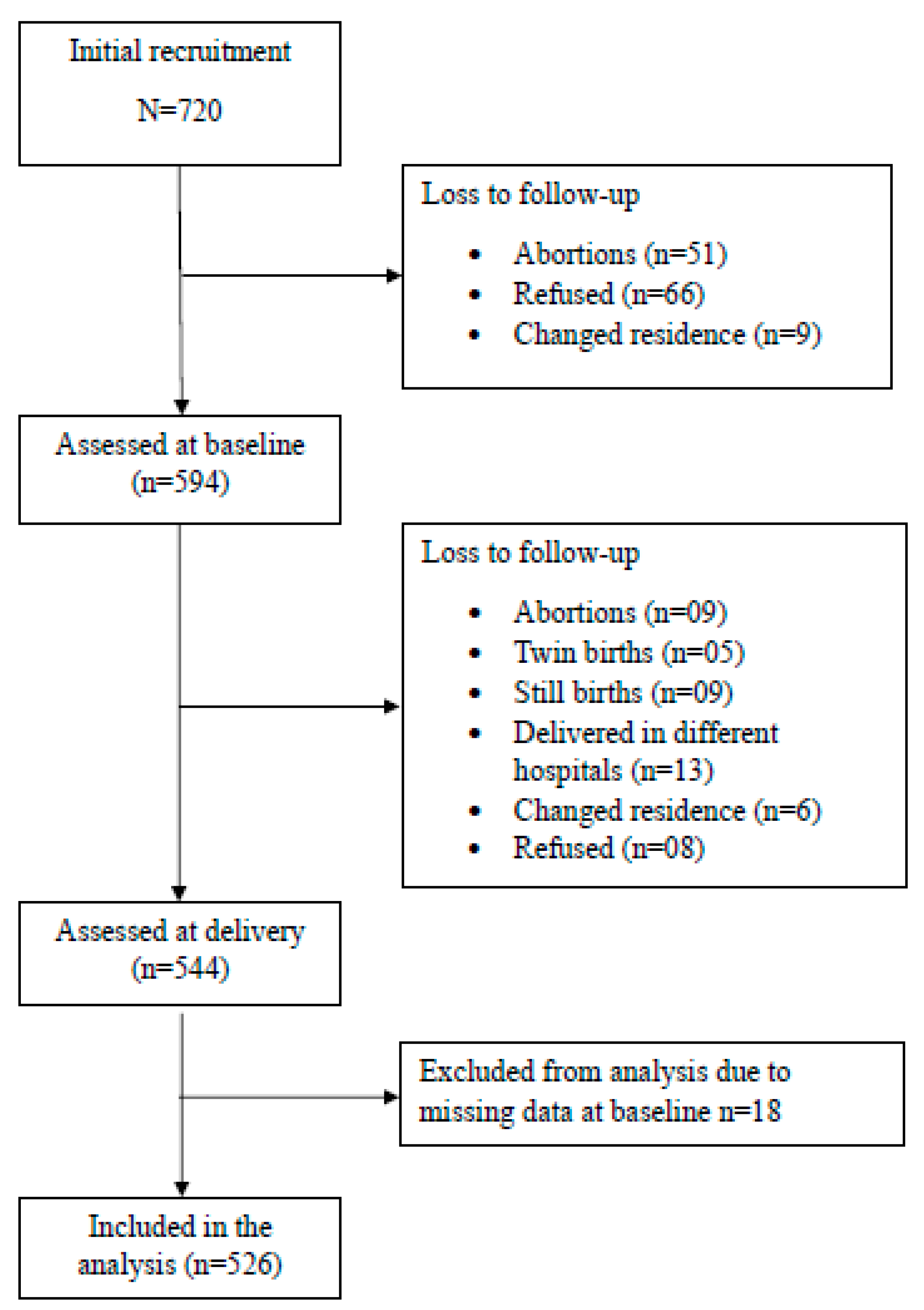
2.3. Recruitment of Study Participants
2.4. Data Collection Procedures
2.4.1. Baseline Questionnaire
2.4.2. Exposure Assessment
2.4.3. Outcome Assessment
2.4.4. Covariates
2.5. Data Analysis
3. Results
Socio-Demographic Characteristics of Families
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APGAR | Appearance, Pulse, Grimace, Activity, and Respiration |
| BMI | Body Mass Index |
| BNBAS | Brazelton Neonatal Behavioural Assessment Scale |
| CHDR | Child Health Development Record |
| CNTH | Colombo North Teaching Hospital |
| CO | Carbon Monoxide |
| CO2 | Carbon Monoxide |
| DCS | Department of Census and Statistics |
| HAP | Household Air Pollution |
| IAP | Indoor Air Pollution |
| IAQ | Indoor Air Quality |
| IQR | Interquartile range |
| LPG | Liquified Petroleum Gas |
| MCH | Maternal and Child Health |
| MOH | Medical Officer of Health |
| PHI | Public Health Inspector |
| PHM | Public Health Midwife |
| PM | Particulate Matter |
| RA | Research Assistant |
| UKe | University of Kelaniya |
References
- Tran, T.P.T.; Le, T.H.; Nguyen, T.N.P.; Hoang, V.M. Rapid response to the COVID-19 pandemic: Vietnam government’s experience and preliminary success. J. Glob. Health 2020, 10, 020502. [Google Scholar] [CrossRef] [PubMed]
- Cincinelli, A.; Martellini, T. Indoor Air Quality and Health. Int. J. Environ. Res. Public Health 2017, 14, 1286. [Google Scholar] [CrossRef] [PubMed]
- Gebremeskel Kanno, G.; Hussen Kabthymer, R. Association of low birthweight with indoor air pollution from biomass fuel in sub-Saharan Africa: A systemic review and meta-analysis. Sustain. Environ. 2021, 7, 1922185. [Google Scholar] [CrossRef]
- Ranathunga, N.; Perera, P.; Nandasena, S.; Sathiakumar, N.; Kasturiratne, A.; Wickremasinghe, A.R. Effects of indoor air pollution due to solid fuel combustion on physical growth of children under 5 in Sri Lanka: A descriptive cross sectional study. PLoS ONE 2021, 16, e0252230. [Google Scholar] [CrossRef] [PubMed]
- Haider, M.R.; Rahman, M.M.; Islam, F.; Khan, M.M. Association of Low Birthweight and Indoor Air Pollution: Biomass Fuel Use in Bangladesh. J. Health Pollut. 2016, 6, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Kana, M.A.; Shi, M.; Ahmed, J.; Ibrahim, J.M.; Ashir, A.Y.; Abdullahi, K.; Bello-Manga, H.; Taingson, M.; Mohammed-Durosinlorun, A.; Shuaibu, M.; et al. Biomass fuel use and birth weight among term births in Nigeria. PLoS Glob. Public Health 2022, 2, e0000419. [Google Scholar] [CrossRef] [PubMed]
- Kanno, G.G.; Anbesse, A.T.; Shaka, M.F.; Legesse, M.T.; Andarge, S.D. Effect of biomass fuel use and kitchen location on maternal report of birth size: Cross-sectional analysis of 2016 Ethiopian Demographic Health Survey data. Public Health Pract. 2021, 2, 100211. [Google Scholar] [CrossRef] [PubMed]
- Mishra, V. Maternal exposure to biomass smoke and reduced birth weight in Zimbabwe*1. Ann. Epidemiol. 2004, 14, 740–747. [Google Scholar] [CrossRef] [PubMed]
- Yucra, S.; Tapia, V.; Steenland, K.; Naeher, L.P.; Gonzales, G.F. Maternal exposure to biomass smoke and carbon monoxide in relation to adverse pregnancy outcome in two high altitude cities of Peru. Environ. Res. 2014, 130, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Vakalopoulos, A.; Dharmage, S.C.; Dharmaratne, S.; Jayasinghe, P.; Lall, O.; Ambrose, I.; Weerasooriya, R.; Bui, D.S.; Yasaratne, D.; Heyworth, J.; et al. Household Air Pollution from Biomass Fuel for Cooking and Adverse Fetal Growth Outcomes in Rural Sri Lanka. Int. J. Environ. Res. Public Health 2021, 18, 1878. [Google Scholar] [CrossRef] [PubMed]
- Department of Census and Statistics (DCS) and Ministry of Health, Nutrition and Indigenous Medicine. Sri Lanka Demographic and Health Survey 2016; Department of Census and Statistics (DCS) and Ministry of Health, Nutrition and Indigenous Medicine: Colombo, Sri Lanka, 2017.
- Elledge, M.F.; Phillips, M.J.; Thornburg, V.E.; Everett, K.H.; Nandasena, S. A Profile of Biomass Stove Use in Sri Lanka. Int. J. Environ. Res. Public. Health 2012, 9, 1097–1110. [Google Scholar] [CrossRef] [PubMed]
- Sly, P.D.; Trottier, B.; Carpenter, D.; Cha’on, U.; Cormier, S.; Galluzzo, B.; Ghosh, S.; Goldizen, F.; Heacock, M.; Jagals, P.; et al. Children’s Environmental Health in South and Southeast Asia: Networking for Better Child Health Outcomes. Ann. Glob. Health 2019, 85, 17. [Google Scholar] [CrossRef] [PubMed]
- Nandasena, Y.L.S.; Wickremasinghe, A.R.; Sathiakumar, N. Air pollution and health in Sri Lanka: A review of epidemiologic studies. BMC Public Health 2010, 10, 300. [Google Scholar] [CrossRef] [PubMed]
- Population by District in Census Years | Open Data Portal—Sri Lanka. Available online: https://data.gov.lk/dataset/population-district-census-years (accessed on 11 November 2024).
- Brazelton, T.B.; Nugent, J.K. The Neonatal Behavioral Assessment Scale; Blackwell: Hoboken, NJ, USA, 2011. [Google Scholar]
- Brazelton Institute | Neonatal Behavioral Assessment Scale (NBAS) | Boston Children’s Hospital. Available online: https://www.childrenshospital.org/research/centers/brazelton-institute-research/nbas (accessed on 24 June 2024).
- Sreeramareddy, C.T.; Shidhaye, R.R.; Sathiakumar, N. Association between biomass fuel use and maternal report of child size at birth - an analysis of 2005-06 India Demographic Health Survey data. BMC Public Health 2011, 11, 403. [Google Scholar] [CrossRef] [PubMed]
- Wylie, B.J.; Coull, B.A.; Hamer, D.H.; Singh, M.P.; Jack, D.; Yeboah-Antwi, K.; Sabin, L.; Singh, N.; MacLeod, W.B. Impact of biomass fuels on pregnancy outcomes in central East India. Environ. Health 2014, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Research with the NBAS—Brazelton Centre UK. Available online: https://www.brazelton.co.uk/research/in-the-nbas/ (accessed on 23 September 2024).
- Fussell, J.C.; Jauniaux, E.; Smith, R.B.; Burton, G.J. Ambient air pollution and adverse birth outcomes: A review of underlying mechanisms. BJOG Int. J. Obstet. Gynaecol. 2024, 131, 538–550. [Google Scholar] [CrossRef]
- The Department of Census and Statistics Vital Statistics—2014. Available online: http://www.statistics.gov.lk/Population/Vital_Statistics-2014 (accessed on 21 June 2024).
- Hartinger, S.M.; Commodore, A.A.; Hattendorf, J.; Lanata, C.F.; Gil, A.I.; Verastegui, H.; Aguilar-Villalobos, M.; Mäusezahl, D.; Naeher, L.P. Chimney stoves modestly improved Indoor Air Quality measurements compared with traditional open fire stoves: Results from a small-scale intervention study in rural Peru. Indoor Air 2013, 23, 342–352. [Google Scholar] [CrossRef]
- Perera, K.K.C.K.; Sugathapala, A.G.T. Fuelwood-fired cookstoves in Sri Lanka and related issues. Energy Sustain. Dev. 2002, 6, 85–94. [Google Scholar] [CrossRef]
| Variable | High Exposure N (%) | Low Exposure N (%) | Chi-Square Test (p-Value) |
|---|---|---|---|
| Mother’s age (years) (mean (sd)) | 28.4 (4.7) | 28.9 (5.0) | t524 = 0.968 (p = 0.333) |
| Spouse’s age (years) (mean (sd)) | 31.7 (4.7) | 32.6 (5.1) | t519 = 2.007 (p = 0.045) |
| Mother’s education level | |||
| Grade 10 or less | 24 (68.6) | 11 (31.4) | (p = 0.005) |
| Up to GCE ordinary level | 207 (58.8) | 145 (41.2) | |
| GCE advanced level or graduate | 62 (44.6) | 77 (55.4) | |
| Spouse’s education level | |||
| Grade 10 or less | 21 (77.8) | 06 (22.2) | (p < 0.001) |
| Up to ordinary level | 216 (58.1) | 156 (41.9) | |
| Advanced level or graduate | 55 (43.7) | 71 (56.3) | |
| Income category (in LKR 1) (n = 521) | |||
| <25,000 | 191 (68.2) | 89 (31.8) | |
| ≥25,000 | 99 (41.1) | 142 (58.9) | |
| History of family member smoking | |||
| Yes | 106 (63.1) | 62 (36.9) | (p = 0.019) |
| No | 187 (52.2) | 171 (47.8) | |
| PM2.5 (µg/m3) (median (IQR)) (n = 303) | 720 | 115.5 | Mann–Whitney U test (p < 0.001) |
| (208–1860) | (65.5–256) | ||
| (n = 168) | (n = 135) | ||
| CO (ppm) (median (IQR)) (n = 258) | 2000 | 1100 | Mann–Whitney U test (p < 0.001) |
| (1200–4066) | (700–1300) | ||
| (139) | (n = 119) |
| Variable | High Exposure 1 | Low Exposure 2 | Statistical Test (p-Value) |
|---|---|---|---|
| Birthweight (n; mean (sd) in g) (n = 526) | 293; 2889 (457. 3) | 233; 3023 (480.5) | t542 = 3.268 (p = 0.001) |
| Low birth weight (n = 526) | |||
| Yes (n (%)) No (n (%)) | 45 (15.3) 248 (84.7) | 23 (9.8) 210 (90.2) | ) |
| Birth length (cm) (n; mean (sd)) | 291; 50.12 (3.15) | 231; 50.60 (3.17) | t520 = 1.711 (p = 0.08) |
| Gestational age (days) * (n; mean (sd)) (n = 469) | 260; 271.29 (10.8) | 209; 271.15 (10.7) | t467 = −0.134 (p = 0.89) |
| Pre-term birth (n = 45) | |||
| Yes (n, (%)) | 21 (7.2) | 24 (10.3) | Fisher’s exact test (p = 1.00) |
| No (n, (%)) | 272 (92.8) | 209 (89.7) | |
| APGAR score (n; mean (sd)) | |||
| 1 min | 288; 9.56 (1.03) | 229; 9.56 (0.94) | t515 = −0.07 (p = 0.94) |
| 5 min | 287; 9.92 (0.39) | 227; 9.95 (0.23) | t512 = 0.827 (p = 0.409) |
| 10 min | 287; 9.96 (0.21) | 226; 9.94 (0.62) | t511 = −0.778 (p = 0.437) |
| Brazelton Neonatal Behavioural Assessment Scale (BNBAS) scores | |||
| Smiles (n; mean (sd)) | 138; 0.79 (1.09) | 118; 0.85 (1.14) | t254 = 0.471 (p = 0.638) |
| Habituation (n; mean (sd)) | 216; 7.15 (0.94) | 172; 7.14 (0.95) | t386 = −0.134 (p = 0.893) |
| Social interaction (n; mean (sd)) | 253; 5.77 (0.85) | 195; 5.80 (0.91) | t446 = 0.294 (p = 0.769) |
| Motor system (n; mean (sd)) | 252; 6.41 (0.69) | 196; 6.55 (0.64) | t446 = 2.077 (p = 0.038) |
| State organization (n; mean (sd)) | 252; 5.68 (0.97) | 196; 5.66 (0.95) | t446 = −0.156 (p = 0.876) |
| State regulation (n; mean (sd)) | 252; 6.27 (0.96) | 196; 6.29 (1.01) | t446 = 0.240 (p = 0.810) |
| Autonomic system (n; mean (sd)) | 252; 5.19 (0.97) | 196; 5.09 (0.94) | t446 = −1.048 (p = 0.295) |
| Supplement items (n; mean (sd)) | 252; 6.35 (0.77) | 196; 6.30 (0.72) | t446 = −0.566 (p = 0.572) |
| Reflexes (n, mean (sd)) | 252; 1.64 (0.16) | 196; 1.65 (0.15) | t446 = 0.740 (p = 0.460) |
| Birth Outcome | Exposure 1 | Unadjusted | Adjusted 2 | ||||
|---|---|---|---|---|---|---|---|
| Regression Coefficient (β) | p-Value | 95% CI of β | Regression Coefficient | p-Value | 95% CI of β | ||
| Birth weight (g) | Low | 0.000 | |||||
| High | −134.1 | 0.001 | −214.8–(−53.5) | −106.8 | 0.003 | −197.6–(−16.0) | |
| Birth length (cm) | Low | 0.000 | 0.000 | ||||
| High | −0.477 | 0.08 | −1.024–0.071 | −0.474 | 0.203 | −1.205–0.257 | |
| Gestational age (days) * | Low | 0.000 | 0.000 | ||||
| High | 0.135 | 0.89 | −1.843–2.113 | −1.459 | 0.255 | −3.975–1.056 | |
| APGAR score (5 min) | Low | 0.000 | 0.000 | ||||
| High | −0.025 | 0.40 | −0.083–0.034 | −0.055 | 0.185 | −0.136–0.026 | |
| Brazelton Neonatal Behavioural Assessment Scale (BNABS) | Low | 0.000 | 0.000 | ||||
| High | −0.133 | 0.038 | −0.259–(−0.007) | −0.130 | 0.075 | −0.272–0.013 | |
| Indoor Air Pollutant | Birth Weight | Birth Length | Gestational Age | APGAR Score | Neonatal Behavioural Assessment Scale (NBAS) |
|---|---|---|---|---|---|
| Particulate matter (PM2.5) | r = −0.009 (n = 303) (p = 0.878) | r = −0.033 (n = 302) (p = 0.573) | r = 0.052 (n = 273) (p = 0.388) | r = 0.075 (n = 295) (p = 0.201) | r = 0.011 (n = 258) (p = 0.858) |
| Carbon monoxide (CO) | r = −0.007 (n = 258) (p = 0.917) | r = −0.064 (n = 257) (p = 0.305) | r = 0.03 (n = 230) (p = 0.651) | r = 0.02 (n = 251) (p = 0.653) | r = −0.044 (n = 219) (p = 0.519) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wickremasinghe, R.; Tipre, M.; Perera, R.; Godamunne, P.; Larson, R.R.; Leader, M.; Lungu, C.T.; Wimalasiri, U.; Perera, P.; Nandasena, S. Effect of Biomass Fuel Use on Neonatal Outcomes: A Cohort Study of Pregnant Females. Int. J. Environ. Res. Public Health 2025, 22, 1336. https://doi.org/10.3390/ijerph22091336
Wickremasinghe R, Tipre M, Perera R, Godamunne P, Larson RR, Leader M, Lungu CT, Wimalasiri U, Perera P, Nandasena S. Effect of Biomass Fuel Use on Neonatal Outcomes: A Cohort Study of Pregnant Females. International Journal of Environmental Research and Public Health. 2025; 22(9):1336. https://doi.org/10.3390/ijerph22091336
Chicago/Turabian StyleWickremasinghe, Rajitha, Meghan Tipre, Ruwanthi Perera, Pavithra Godamunne, Rodney R. Larson, Mark Leader, Claudiu T. Lungu, Udaya Wimalasiri, Priyantha Perera, and Sumal Nandasena. 2025. "Effect of Biomass Fuel Use on Neonatal Outcomes: A Cohort Study of Pregnant Females" International Journal of Environmental Research and Public Health 22, no. 9: 1336. https://doi.org/10.3390/ijerph22091336
APA StyleWickremasinghe, R., Tipre, M., Perera, R., Godamunne, P., Larson, R. R., Leader, M., Lungu, C. T., Wimalasiri, U., Perera, P., & Nandasena, S. (2025). Effect of Biomass Fuel Use on Neonatal Outcomes: A Cohort Study of Pregnant Females. International Journal of Environmental Research and Public Health, 22(9), 1336. https://doi.org/10.3390/ijerph22091336








