Abstract
Background: Globally, socioeconomic disparities persist across the trajectory of chronic kidney disease and are pronounced among people with kidney failure. Unmet health-related social needs contribute to these disparities, but limited guidance exists about how best to address them. To guide implementation, we conducted a rapid scoping review to identify and characterize interventions that address health-related social needs among people with kidney failure. Methods: We adapted established scoping review methods to conduct a rapid review. We searched Embase, PubMed, CINAHL, SCOPUS, and PsychInfo for articles and conference abstracts published since 2013 that described interventions to address health-related social needs as identified in the Centers for Medicare and Medicaid Services’ Accountable Health Communities Health-Related Social Needs Screening Tool. We applied the RE-AIM framework (Reach, Effectiveness, Adoption, Implementation, Maintenance) to synthesize findings and characterize intervention components. Results: Our review identified three articles and five conference abstracts that described diverse interventions to address health-related social needs among people with kidney failure. Six targeted social support, one addressed food insecurity, and one addressed transportation needs. Two pilot studies to address social support reported high recruitment and retention rates. One study formally tested an intervention to address social support among adolescents with kidney failure and reported negative findings (no change in social exclusion). The level of detail about intervention implementation varied across studies, but none described excluded participants or intervention fidelity, adaptations, or cost. Conclusions: Despite recent attention, there remains a lack of evidence to guide interventions addressing health-related social needs among people with kidney failure. From limited available data, interventions to address social support may be feasible and acceptable.
1. Introduction
Chronic kidney disease is a major public health concern with a global prevalence of approximately 10% [1]. End-stage kidney disease, or kidney failure, is increasing worldwide due to epidemiological transitions (e.g., population aging and increases in noncommunicable diseases such as hypertension, diabetes and obesity) and expanded availability of renal replacement therapies [2]. From 1990 to 2017, the number of people with kidney failure initiating dialysis or receiving a kidney transplant increased by 43.1% and 34.4%, respectively [3]; and average global prevalence of treated kidney failure is now 823 per million population [4]. Within and across countries, socioeconomic disparities persist across the trajectory of chronic kidney disease and are pronounced among people with treated kidney failure [4,5,6]. In the United States, for example, neighborhood poverty is associated with worse dialysis survival [7], quality of dialysis care [8], and kidney transplant waitlisting and outcomes [9]. Due to structural factors such as structural racism, a higher proportion of Black or Hispanic individuals with kidney failure live in disinvested and high-poverty neighborhoods compared to White individuals (62.2% or 65.4% versus 26.6%) [10].
People with kidney failure, particularly those from historically disadvantaged groups, often experience unmet health-related social needs [11]. The United States Centers for Medicare and Medicaid Services (CMS) define health-related social needs as “an individual’s unmet, adverse social conditions that contribute to poor outcomes” [12]. Health-related social needs include food insecurity, housing instability, community safety concerns, difficulty paying utilities, and challenges with transportation. Recent estimates of food insecurity among people receiving hemodialysis in the United States range from 35 to 60 percent [13,14]. A body of research is beginning to demonstrate the impact of health-related social needs on dialysis outcomes such as survival, hospitalization, and health-related quality of life [15,16,17]. At the same time, major reports such as the National Academies of Sciences, Engineering, and Medicine’s Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health have called for healthcare systems to address patients’ unmet social needs [18]. Screening for health-related social needs is now a health system strategy to reduce acute care spending and advance health equity among patient populations with chronic disease, and CMS requires dialysis facilities to conduct such screenings as part of value-based care [19].
Despite recent attention, limited guidance exists about approaches to address health-related social needs among people with kidney failure [20]. A recent systematic review documented that peer support interventions may improve patient-level outcomes like self-efficacy and psychological well-being for this population [21]. However, such interventions have not directly targeted upstream health-related social needs. Moreover, to advance health equity, an understanding of how interventions to address health-related social needs are delivered is needed, in addition to what these interventions entail [22]. Frameworks from implementation science, defined as “the scientific study of methods to promote the systematic uptake of research findings and evidence-based practices into routine practice” [23], can guide this discovery. Given this context, we conducted a rapid scoping review to identify interventions that address health-related social needs among people with kidney failure. We applied the RE-AIM framework (Reach, Effectiveness, Adoption, Implementation, Maintenance) [24], an established implementation science framework, to synthesize findings and characterize intervention components.
2. Methods
2.1. Design
While scoping reviews and systematic reviews both synthesize existing research on a particular topic, they differ in that the main purpose of scoping reviews is to identify knowledge gaps rather than to answer a specific research question [25]. Further, rapid reviews are “a form of knowledge synthesis that accelerates the process of conducting a traditional systematic review through streamlining or omitting a variety of methods to produce evidence in a resource-efficient manner” [26]. We followed established scoping review methodology from the Joanna Briggs Institute [27]. Given that payers in the United States are currently requiring dialysis facilities to screen patients for health-related social needs as part of value-based care, we adapted our approach to article screening for timeliness as described below. We report our search and results in alignment with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews (PRISMA-ScR) checklist [28].
2.2. Search and Selection
In collaboration with an informaticist, we developed a search strategy to identify recent relevant scientific and grey literature, including conference abstracts. We identified health-related social needs from the CMS Accountable Health Communities Health-Related Social Needs Screening Tool, including food insecurity, housing instability, transportation challenges, difficulty paying utilities, financial strain, and social support [29]. In December 2023, we conducted a search of Embase, PubMed, CINAHL, SCOPUS, and PsychInfo for articles and conference abstracts written in English and published since 2013 (see Supplemental Table S1 for the full search terms and yields from each database search). We applied the PICOS (population, intervention, comparison, outcome, study type) framework to define study eligibility criteria [30], and included articles or conference abstracts of intervention studies if they addressed health-related social needs among people with kidney failure (Table 1). Conceptually, the Health-Related Social Needs Screening Tool screens for social support needs with one item related to instrumental social support (“…If for any reason you need help with day-to-day activities…do you get the help you need?”) and one related to loneliness or social isolation (“how often do you feel lonely or isolated from those around you?). Therefore, we conceptualized interventions to promote social connection or engagement as “interventions to address social support.” We included studies regardless of which type of kidney replacement therapy participants were receiving, and regardless of outcome. We included randomized and nonrandomized studies. We excluded studies of people with earlier stages of chronic kidney disease.

Table 1.
Study Eligibility Criteria.
Our literature search resulted in 9869 studies. After automated removal of duplicates, we screened titles and abstracts for 8007 unique studies. A team of three trained reviewers each independently screened approximately 600 titles and abstracts and met biweekly to discuss findings and establish consensus. Subsequently, one reviewer screened remaining titles and abstracts. Fully, 31 articles or conference abstracts were selected for full-text screening. At this phase, we screened reference lists from selected articles but did not identify other potentially eligible studies. Two reviewers (DP and KT) independently screened each full-text article or conference abstract for inclusion and resolved discrepancies via discussion. Twenty-three articles were excluded: three studies were excluded due to their population, ten studies due to their intervention, and ten studies due to their design. Finally, eight studies met inclusion criteria and were included in the scoping review (Figure 1).
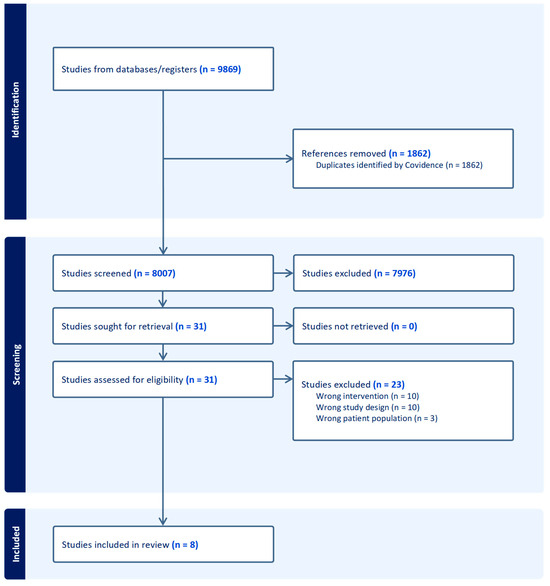
Figure 1.
PRISMA Diagram.
2.3. Data Extraction and Synthesis
We applied the RE-AIM framework to guide data extraction and synthesis. Since it was constructed in 1999, the RE-AIM framework has expanded to incorporate contextual factors that impact RE-AIM domains and to explicitly address health equity (Supplemental Figure S1) [24]. Each of the five RE-AIM domains includes assessment questions for intervention planning or evaluation. We adapted a data extraction form from a scoping review by Hirchak and colleagues that used RE-AIM assessment questions to synthesize included studies and incorporated a health equity lens [31]. For example, one assessment question related to Reach was, “Authors describe engagement strategies or equity issues related to participation.” Two reviewers (DP and KT) piloted and refined the extraction tool before use via discussion and consensus.
3. Results
3.1. Description of Studies
Of the eight studies included in this review, three were full-text articles [32,33,34] and five were conference abstracts (Table 2) [35,36,37,38,39]. Seven were conducted in the United States [33,34,35,36,37,38]. Of those, six were conducted in cities with large academic medical centers [33,34,35,36,38]. Of the three full-text studies reporting funding, one was funded by the Dutch Kidney Foundation [34], one by the National Institute on Aging [33], and one by a university [32].

Table 2.
Characteristics of Included Studies.
Two of the studies in the review were pilot studies (a single-group prospective study [34] and one randomized controlled trial [33]) and six were program evaluations or quality improvement projects [32,35,36,37,38,39]. Only the randomized controlled trial enrolled intervention and control groups [33]. Of the seven studies with single groups, three studies [32,36,37] used a pre-post design and the remaining four studies reported post-intervention outcomes [35,37,38,39]. Except for one program evaluation with 2964 patients [35], studies had small sample sizes ranging from 10 to 34 participants. Four studies purposefully sampled socially disadvantaged groups with kidney failure. Of those four, samples included undocumented immigrants [34], older adults with low socioeconomic status [33], adults obtaining food bank bags from the dialysis facility [38], and children living in minoritized communities [36]. The remaining studies did not provide details about participant socioeconomic status.
Intervention characteristics and study outcomes varied across studies. Six out of eight studies targeted social support [32,33,34,36,37,39]. One program targeted food insecurity [38] and a separate program targeted transportation needs within a broader care coordination service [35]. Of the six studies targeting social support, three delivered the intervention via participant peers [32,34,37]. In two studies, participant peers were defined based on demographic and social characteristics (e.g., adolescents, undocumented immigrants) [32,34]. The remaining three studies delivered the intervention via medical students [39] or multidisciplinary teams. In the studies involving multidisciplinary teams, one delivered the intervention via a triad of nurse, occupational therapist, and handyman [33]. The other was a unit-based “Psychosocial Power Team,” including nursing, massage therapy, recreational therapy, social work, and psychology [36]. The two studies addressing food insecurity or transportation needs featured organizational partnerships (e.g., a dialysis facility and a food bank) [35,38]. Participants received interventions at healthcare facilities (dialysis facility or hospital) [34,36,37,38,39], their own homes [33], or a remote camp [32]. When reported in detail, intervention duration lasted between one week [32] and six months [34]. Both pilot studies and two program evaluations reported some aspect of intervention feasibility and acceptability [33,34,38,39]. Four studies evaluated resolution of the health-related social need [32,33,36,38]. Two studies used a validated measure of a health-related social need [32,33]. In the two other studies in which authors measured the targeted health-related social need, they either developed their own measure or did not describe it in detail [36,38]. Two reported clinical outcomes (interdialytic weight gain and visit adherence) [35,37].
3.2. Application of RE-AIM Framework
Table 3 presents RE-AIM data extracted from the three full-text articles included in this review. We were unable to extract RE-AIM data from conference abstracts because reporting was inherently limited due to word count restrictions. Each of the three full-text articles used multi-method or mixed methods designs (i.e., quantitative and qualitative methods) to evaluate reach, effectiveness, adoption, implementation, or maintenance. Regarding reach, none of the articles described individuals who were excluded from studies or interventions. One study detailed recruitment via a culturally concordant study team member [34]. Regarding effectiveness, none of the studies measured attrition by participant characteristics; however, two studies targeted structurally disadvantaged groups (undocumented immigrants and Black older adults with low incomes) and reported reasons for participants leaving the studies [33,34]. Regarding adoption, all three studies discussed the number of staff who delivered the interventions, but only one study described the representativeness of the staff member [34]. None of the studies provided details on intervention fidelity, adaptations, or cost. One study discussed a plan for intervention sustainability via establishment of a non-profit organization [34].

Table 3.
RE-AIM Domains Characterized in Full-Text Studies.
Table 3.
RE-AIM Domains Characterized in Full-Text Studies.
| Cervantes (2023) [34] | Crews (2019) [33] | Sattoe (2013) [32] | |
|---|---|---|---|
| Reach | |||
| Authors reported characteristics of excluded individuals | No | No | No |
| Authors described engagement strategies or equity issues related to participation | Yes: Culturally concordant study team member conducted in-person recruitment | No | No |
| Authors use qualitative methods to understand reach or recruitment | No | No | Yes: Semi-structured interview elicited rationale of referring nephrologists |
| Effectiveness | |||
| Authors identify primary outcome | Yes: Feasibility and acceptability | Yes: Feasibility and acceptability | Yes: Self-efficacy, self-management; autonomy in social participation |
| Authors discussed effectiveness across subgroups | n/a: Study targeted a subgroup | n/a: Study targeted a subgroup | No |
| Authors measured broader outcome (e.g., quality of life) | No | No | Yes: Health-related quality of life |
| Authors measured short-term attrition by participant characteristics | n/a: Study targeted subgroup; reported reasons for attrition | n/a: Study targeted subgroup; reported reasons for attrition | No |
| Authors used qualitative methods to understand outcomes | Yes: Structured interview to elicit value of peer support intervention | Yes: Focus groups to inform adaptation of existing intervention and potential value of adapted version | Yes: Semi-structured interview elicited value of camp and mechanisms of action |
| Adoption | |||
| Authors discussed number and representativeness of staff who delivered the program | Yes: One culturally concordant study staff member led peer support group meetings | Yes: 3 staff per participant; no description of representativeness | Yes: 1-to-1 ratio of “buddy” to attendee; no description of representativeness |
| Authors reported characteristics of participating and non-participating settings | No | No | No |
| Authors used qualitative methods to understand staff participation | n/a: Intervention delivered by study staff | No | Yes: Semi-structured interview elicited “buddy” experience |
| Implementation | |||
| Authors reported intervention fidelity | No | No | No |
| Authors reported adaptations made to intervention during study | No | No | No |
| Authors reported adaptations that might be needed to promote equity | No | No | No |
| Authors reported intervention cost (time or money) | No | No | No |
| Authors reported multi-level context that either facilitated or hindered implementation | Yes: Enrolled participants from hospital on same day of the week; participants preferred hospital setting for group meetings | No | No |
| Authors used qualitative methods to understand implementation | Yes: Semi-structured interview elicited participants’ perspectives about value of peer support group | No | Yes: Semi-structured interviews elicited “buddy” experience with implementation |
| Maintenance | |||
| Authors reported primary outcome, broader outcome, subgroup effects, or attrition over the long-term | n/a: Pilot study | n/a: Pilot study | No |
| Authors discussed alignment to organizational mission or sustainability of business model | Yes: Participants formalized peer support group via nonprofit organization and social media | No | No |
| Authors use qualitative methods to understand setting level institutionalization | Yes: Semi-structured interviews elicited participants’ motivation for starting a nonprofit | No | No |
4. Discussion
Our scoping review identified a nascent evidence base for interventions addressing health-related social needs among people with kidney failure. In small pilot studies, interventions to address health-related social needs were feasible and acceptable to participants [33,34]. Single group program evaluations targeted different populations across varying levels of socioeconomic status. They intervened upon different health-related social needs, and used different measures for social needs and outcomes. This heterogeneity limits our ability to draw conclusions about intervention effectiveness and generalize findings. Of the five domains in the RE-AIM framework, the three full-text studies provided some detail about effectiveness and adoption, but limited detail about reach, implementation, and maintenance.
We conducted our literature search in December 2023. Since that time, new projects have formed to address socioeconomic disparities in kidney failure and dialysis by addressing health-related social needs and other contributing factors. For example, as part of the Eliminating Racism and Structural in Equities in Kidney Disease (ERASE-KD) Consortium, a multidisciplinary team in New York began testing a community health worker (CHW) intervention to help people with kidney disease address health-related social needs and navigate the kidney transplantation process (https://erasekd.org/ (accessed on 28 January 2025)) [20]. Unfortunately, project funding from the United States National Institutes of Health was abruptly terminated in May 2025 [40]. Additionally, an abstract presented in April 2024 at the World Congress of Nephrology reported results from a randomized controlled trial of a CHW intervention in Colorado with Latinx individuals with kidney failure. Between one-fifth and one-third of participants reported difficulty accessing food, housing, transportation, medicine, or paying for utilities in the past year. The abstract did not report resolution of health-related social needs, but the study did find differences in levels of patient activation between intervention and control groups post-intervention [41]. Lastly, an abstract presented by Novick and colleagues at the American Society of Nephrology Kidney Week in 2024 described a pilot CHW intervention with 17 dually eligible adults receiving dialysis in Texas. Participants had high rates of health-related social needs at baseline (e.g., 70% reported housing instability) though post-intervention measures were not reported [42].
Multisector partnerships and CHW interventions are promising mechanisms to address unmet social needs and advance health equity in the dialysis population. In most studies included in our review, either participant peers [32,34,37] or medical providers (or medical students) [33,36] delivered the interventions, raising concerns about replicability, costs, scalability, and sustainability. In particular, peer-delivered interventions (e.g., for peer support) are impactful but may lack formal structures needed for scale [21]. In the context of health-related social service delivery for people who have traditionally been underserved due to structural inequities such as racism [43], CHWs are quickly emerging as effective agents in addressing their needs. According to a recent return-on-investment analysis, every dollar invested in a CHW intervention addressing social needs would return $2.47 to an average Medicaid payer within the fiscal year [44]. Medicare has begun to reimburse CHW services as detailed in the Calendar Year 2024 Physician Fee Schedule, creating a pathway for scalability and sustainability.
Our review has important implications for future research and practice. In particular, more rigorous study designs that include pre- and post-testing, control groups, and/or randomization are needed, powered by larger sample sizes [20]. When researchers test interventions to address health-related social needs, they can use waitlist control groups to address ethical concerns and use standardized measures. They can apply implementation science frameworks to enhance reporting about implementation, strengthen external validity, capture information about process, and promote sustainability. Researchers should be open to reporting intervention cost, adaptations, and implementation challenges. Additionally, they should capture health-related social needs and clinical outcomes to deepen our understanding of causal pathways. Lastly, research to address health-related social needs should explore the role of dialysis facilities and large dialysis organizations. Beginning in 2025 via the Quality Incentive Program, CMS will hold dialysis facilities accountable for collecting data on food insecurity, housing instability, transportation needs, utility issues, and interpersonal safety [19]. These changes suggest that dialysis facilities may soon be held accountable for addressing health-related social needs within their patient populations, though the evidence base for how to do so is underdeveloped. Regardless of reporting requirements, the kidney community must do the hard work of learning new ways to care for people with kidney failure and complex social needs. A recent report from the National Institutes of Diabetes and Digestive and Kidney Diseases outlined potential solutions, including multi-level interventions (i.e., at patient, provider, and community level), improved data collection on unmet health-related social needs, and integrating community health workers with the healthcare team [45].
This study has some important limitations. A single reviewer conducted the majority of title and abstract screenings and may have inadvertently excluded relevant studies [46]. The reporting of studies included in the conference abstracts was inherently limited in the information provided. These limitations are balanced by key strengths, including the expansiveness and systematic nature of our literature search and application of an implementation science framework to guide synthesis of findings. Moreover, we are not aware of existing reviews of interventions to address health-related social needs among people with kidney failure, particularly among historically disadvantaged groups.
In conclusion, despite recent attention, there remains a lack of evidence to guide interventions addressing health-related social needs among people with kidney failure. New research is urgently needed given the high burden of health-related social needs in this population and the persistence of health inequities. Implementation science frameworks can help ensure that new research is externally valid and that interventions are adopted and sustainable.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph22091330/s1, Figure S1: RE-AIM and PRISM Frameworks with Equity Lens; Table S1: PubMed Search Strategy.
Author Contributions
Conceptualization, K.S.T. and H.-R.H.; methodology K.S.T. and H.-R.H.; formal analysis, K.S.T., D.P. and Y.T.; writing—original draft, K.S.T.; writing—review and editing, K.S.T., D.P., Y.T., D.C.C. and H.-R.H.; funding acquisition, K.S.T. All authors have read and agreed to the published version of the manuscript.
Funding
This project was supported through a grant from the Johns Hopkins Mid-Atlantic Center for Cardiometabolic Health Equity (MACCHE). MACCHE is supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number P50MD017348. The content is solely the responsibility of the authors and does not necessarily represent the official views of MACCHE or the National Institutes of Health.
Acknowledgments
We thank Stella Seal for her support with this review.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Francis, A.; Harhay, M.N.; Ong, A.C.M.; Tummalapalli, S.L.; Ortiz, A.; Fogo, A.B.; Fliser, D.; Roy-Chaudhury, P.; Fontana, M.; Nangaku, M.; et al. Chronic kidney disease and the global public health agenda: An international consensus. Nat. Rev. Nephrol. 2024, 20, 473–485. [Google Scholar] [CrossRef]
- Thurlow, J.S.; Joshi, M.; Yan, G.; Norris, K.C.; Agodoa, L.Y.; Yuan, C.M.; Nee, R. Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am. J. Nephrol. 2021, 52, 98–107. [Google Scholar] [CrossRef]
- Cockwell, P.; Fisher, L. The global burden of chronic kidney disease. Lancet 2020, 395, 662–664. [Google Scholar] [CrossRef]
- Bello, A.K.; Okpechi, I.G.; Levin, A.; Ye, F.; Damstere, S.; Arrueboe, S.; Donnere, J.-A.; Caskey, F.J.; Cho, Y.; Davids, M.R.; et al. An update on the global disparities in kidney disease burden and care across world countries and regions. Lancet Glob. Health 2024, 12, e382–e395. [Google Scholar] [CrossRef] [PubMed]
- Crews, D.C. Chapter 21—Poverty and renal disease. In Chronic Kidney Disease in Disadvantaged Populations; García-García, G., Agodoa, L.Y., Norris, K.C., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 209–217. Available online: https://www.sciencedirect.com/science/article/pii/B9780128043110000212 (accessed on 7 March 2025). [CrossRef]
- Akrawi, D.S.; Li, X.; Sundquist, J.; Sundquist, K.; Zoller, B. End stage renal disease risk and neighbourhood deprivation: A nationwide cohort study in sweden. Eur. J. Intern. Med. 2014, 25, 853–859. [Google Scholar] [CrossRef]
- Kimmel, P.L.; Fwu, C.W.; Eggers, P.W. Segregation, income disparities, and survival in hemodialysis patients. J. Am. Soc. Nephrol. 2013, 24, 293–301. [Google Scholar] [CrossRef]
- Qi, A.C.; Butler, A.M.; Joynt Maddox, K.E. The role of social risk factors in dialysis facility ratings and penalties under A medicare quality incentive program. Health Aff. 2019, 38, 1101–1109. [Google Scholar] [CrossRef]
- Purnell, T.S.; Luo, X.; Crews, D.C.; Bae, S.; Ruck, J.M.; Cooper, L.A.; Grams, M.E.; Henderson, M.L.; Waldram, M.M.; Johnson, M.; et al. Neighborhood poverty and sex differences in live donor kidney transplant outcomes in the united states. Transplantation 2019, 103, 2183–2189. [Google Scholar] [CrossRef]
- United States Renal Data System. 2024 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2024. Available online: https://usrds-adr.niddk.nih.gov/2024 (accessed on 7 March 2025).
- Hall, Y.N. Social determinants of health: Addressing unmet needs in nephrology. Am. J. Kidney Dis. 2018, 72, 582–591. [Google Scholar] [CrossRef]
- Centers for Medicare & Medicaid Services. Social Drivers of Health and Health-Related Social Needs. Available online: https://www.cms.gov/priorities/innovation/key-concepts/social-drivers-health-and-health-related-social-needs (accessed on 21 October 2024).
- Novick, T.; Osuna, M.; Crews, D. The health-related social needs screening tool among hemodialysis patients: An evaluation of sensitivity and specificity. Kidney Med. 2023, 5, 100702. [Google Scholar] [CrossRef]
- Taylor, K.S.; Novick, T.; Santos, S.R.; Chen, Y.; Smith, O.W.; Perrin, N.A.; Crews, D.C. Material need insecurities among people on hemodialysis: Burden, sociodemographic risk factors, and associations with substance use. Kidney360 2023, 4, 1590–1597. [Google Scholar] [CrossRef]
- Novick, T.K.; Mader, M.J.; Johansen, K.L.; Matsui, E.C.; Montgomery, E.; Jacobs, E.A.; Crews, D.C. Unstable housing and mortality among US veterans receiving dialysis. JAMA Netw. Open 2023, 6, e2344448. [Google Scholar] [CrossRef]
- Starr, M.C.; Wightman, A.; Munshi, R.; Li, A.; Hingorani, S. Association of food insecurity and acute health care utilization in children with end-stage kidney disease. JAMA Pediatr. 2019, 173, 1097–1099. [Google Scholar] [CrossRef]
- Taylor, K.S.; Santos, S.R.; Novick, T.K.; Chen, Y.; Smith, O.; Perrin, N.; Crews, D.C. Food insecurity and risk of hospitalization among adults receiving in-center hemodialysis. Clin. J. Am. Soc. Nephrol. 2025, 20, 547–554. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation’s Health. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health; The National Academies Press: Washington, DC, USA, 2019. [Google Scholar]
- Tummalapalli, S.L.; Lu, A.; Cervantes, L. Regulatory and payment changes addressing the social determinants of kidney health. J. Am. Soc. Nephrol. 2024, 35, 1778–1781. [Google Scholar] [CrossRef] [PubMed]
- Bentley-Edwards, K.; Glover, L.; Johnson, A.E.; Mohottige, D.; Obayemi, J.E.; Olague, S.; Thompson, M.; Tummalapalli, S.L.; Urbanski, M.; Barnhart, H.; et al. Testing interventions that address kidney health disparities. J. Am. Soc. Nephrol. 2025, 36, 970–972. [Google Scholar] [CrossRef]
- Longley, R.M.; Harnedy, L.E.; Ghanime, P.M.; Arroyo-Ariza, D.; Deary, E.C.; Daskalakis, E.; Sadang, K.G.; West, J.; Huffman, J.C.; Celano, C.M.; et al. Peer support interventions in patients with kidney failure: A systematic review. J. Psychosom. Res. 2023, 171, 111379. [Google Scholar] [CrossRef]
- Shelton, R.C.; Chambers, D.A.; Glasgow, R.E. An extension of RE-AIM to enhance sustainability: Addressing dynamic context and promoting health equity over time. Front. Public Health 2020, 8, 134. [Google Scholar] [CrossRef]
- Bauer, M.S.; Damschroder, L.; Hagedorn, H.; Smith, J.; Kilbourne, A.M. An introduction to implementation science for the non-specialist. BMC Psychol. 2015, 3, 32–39. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Harden, S.M.; Gaglio, B.; Rabin, B.; Smith, M.L.; Porter, G.C.; Ory, M.G.; Estabrooks, P.A. RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Front. Public Health 2019, 7, 64. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Hamel, C.; Michaud, A.; Thuku, M.; Skidmore, B.; Stevens, A.; Nussbaumer-Streit, B.; Garritty, C. Defining rapid reviews: A systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. J. Clin. Epidemiol. 2021, 129, 74–85. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Billioux, A.; Verlander, K.; Anthony, S.; Alley, D. Standardized screening for health-related social needs in clinical settings: The accountable health communities screening tool. NAM Perspect. 2017. [Google Scholar] [CrossRef]
- Brown, P.; Brunnhuber, K.; Chalkidou, K.; Chalmers, I.; Clarke, M.; Fenton, M.; Forbes, C.; Glanville, J.; Hicks, N.J.; Moody, J.; et al. How to formulate research recommendations. BMJ. 2006, 333, 804–806. [Google Scholar] [CrossRef]
- Hirchak, K.A.; Oluwoye, O.; Nadeau, M.; Richardson, M.; Bajet, K.; Brigman, M.; Herron, J.L.; Hernandez-Vallant, A.; Vasquez, A.; Pham, C.; et al. Coming together for something good: Recommendations from a scoping review for dissemination and implementation science to improve indigenous substance use disorder treatment. Front. Public Health 2023, 11, 1265122. [Google Scholar] [CrossRef]
- Sattoe, J.N.T.; Jedeloo, S.; van Staa, A. Effective peer-to-peer support for young people with end-stage renal disease: A mixed methods evaluation of camp COOL. BMC Nephrol. 2013, 14, 279. [Google Scholar] [CrossRef]
- Crews, D.C.; Delaney, A.M.; Walker Taylor, J.L.; Cudjoe, T.K.M.; Nkimbeng, M.; Roberts, L.; Savage, J.; Evelyn-Gustave, A.; Roth, J.; Han, D.; et al. Pilot intervention addressing social support and functioning of low socioeconomic status older adults with ESRD: The seniors optimizing community integration to advance better living with ESRD (SOCIABLE) study. Kidney Med. 2019, 1, 13–20. [Google Scholar] [CrossRef]
- Cervantes, L.; Rizzolo, K.; Indovina, K.A.; Camacho, C.; Hazel, C.A.; Alamillo, X.; Chandler, M.; Chonchol, M.; Welles, C.C.; Steiner, J.F.; et al. Assessment of a peer support group intervention for undocumented latinx immigrants with kidney failure. JAMA Netw. Open 2023, 6, e2319277. [Google Scholar] [CrossRef]
- Zheng, S.; Pravoverov, L.; Nazarova, A.; Adey, D.; Goes, N.B. Optimal transition for transplant recipients: A model of care in an integrated health care system. Am. J. Transplant. 2020, 20, 594. [Google Scholar]
- Whaley, K.; Hermetz, M.G.; Vogt, B.A.; Grisham, A.; Van Der Eems, T.J.; Bignall, O.N.; Dawson, A.E. “The psychosocial power team”: A multidisciplinary approach to mitigating health inequities for pediatric patients on hemodialysis. J. Am. Soc. Nephrol. 2022, 33, 561. [Google Scholar] [CrossRef]
- Varghese, A.S. Implementing a support person as an intervention for hemodialysis patients to improve fluid regimen adherence. Hemodial. Int. 2021, 25, A8. [Google Scholar]
- McCall, E.T.; Abdel-Rahman, E.M. Improving food insecurity in patients with ESKD on hemodialysis: Partnership with local food bank. J. Am. Soc. Nephrol. 2021, 32, 290. [Google Scholar] [CrossRef]
- Barrera, J.A.; Chen, E.C.; Kanak, M.M.; Kim, D.S.; Liu, J.; Wang, A.; Wong, C.; Nguyen, L. Team’s positive experience with a longitudinal mentoring program for chronic hemodialysis children. Hemodial. Int. 2013, 17, 156–157. [Google Scholar]
- Liesman, J. How will the budget cuts affect you if you’re chronic? 2025. Available online: https://www.healthcentral.com/news/chronic-health/how-will-the-budget-cuts-affect-chronic-people (accessed on 23 June 2025).
- Cervantes, L.; Powe, N.; Hasnaina-Wynia, R.; Cukor, D.; Camacho, C.; McBeth, L.; Mann, S.; Steiner, J.; Chonchol, M. Community health worker intervention for latinx individuals with kidney failure: A randomized controlled trial. Kidney Int. Rep. 2024, 9, S280. [Google Scholar] [CrossRef]
- Novick, T.K.; Giraldo, D.A.; Osuna-Diaz, M.M.; Jacobs, E.; Crews, D. Pilot Data from a Community Health Worker Intervention for Patients on Hemodialysis. 2024. Available online: https://www.asn-online.org/education/kidneyweek/2024/program-abstract.aspx?controlId=4126441 (accessed on 1 July 2025).
- Bailey, Z.D.; Feldman, J.M.; Bassett, M.T. How structural racism works—Racist policies as a root cause of U.S. racial health inequities. N. Engl. J. Med. 2021, 384, 768–773. [Google Scholar] [CrossRef]
- Kangovi, S.; Mitra, N.; Grande, D.; Long, J.A.; Asch, D.A. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Aff. 2020, 39, 207–213. [Google Scholar] [CrossRef]
- Han, D.C.; Patzer, R.E.; Cervantes, L.; Knight, R.; Purnell, T.S.; Powe, N.R.; Edwards, D.P.; Norris, K.C. Designing interventions addressing structural racism to reduce kidney health disparities: A report from a national institute of diabetes and digestive and kidney diseases workshop. J. Am. Soc. Nephrol. 2022, 33, 2141–2152. [Google Scholar] [CrossRef]
- Waffenschmidt, S.; Knelangen, M.; Sieben, W.; Buhn, S.; Pieper, D. Single screening versus conventional double screening for study selection in systematic reviews: A methodological systematic review. BMC Med. Res. Methodol. 2019, 19, 132. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).