Rehabilitating Soldiers for Load Carriage Tasks: An International Perspective
Abstract
1. Introduction
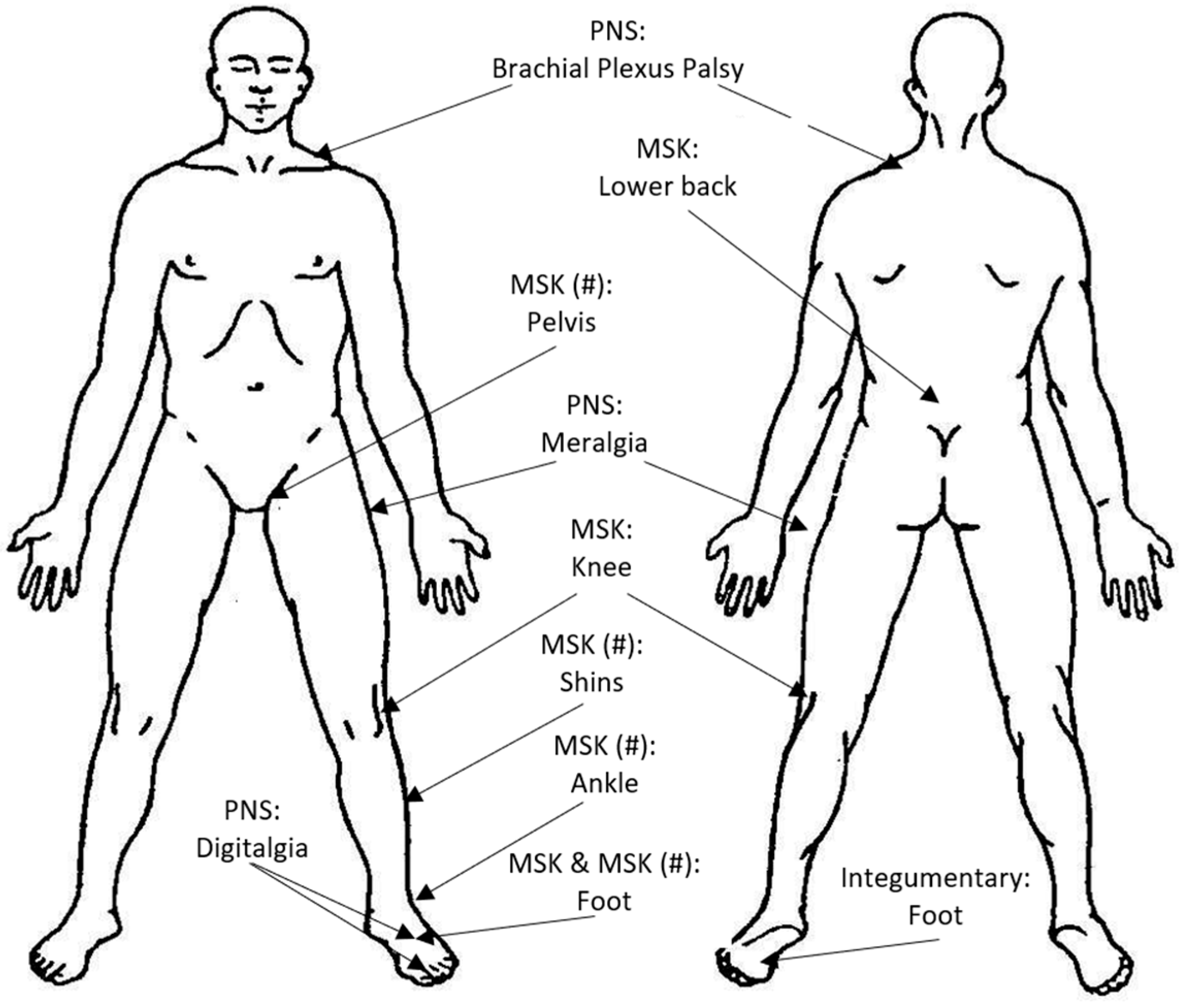
2. Load Carriage Injuries
2.1. Integumentary System
2.2. Peripheral Nervous System
2.3. The Musculoskeletal System
3. The Initial Treatment Stage
4. The Reconditioning Stage
5. The Occupational Conditioning Stage
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PICO | Program-Induced Cumulative Overload |
| PRAI | Physical Resilience Against Injury |
References
- Roth, J. The Logistics of the Roman Army at War (264 B.C.–A.D. 235); Brill Publishers: Boston, MA, USA, 1998. [Google Scholar]
- Melson, C.D. U.S. Marine Rifleman in Vietnam 1965-73; Osprey Publishing: Oxford, UK, 1998. [Google Scholar]
- Knapik, J.; Reynolds, K. Chapter 11: Load carriage in military operations: A review of historical, physiological, biomechanical and medical aspects. In Military Quantitative Physiology: Problems and Concepts in Military Operational Medicine; Borden Institute: Bethesda, MD, USA, 2012; pp. 303–337. [Google Scholar]
- Orr, R.; Pope, R.; Lopes, T.J.A.; Leyk, D.; Blacker, S.; Bustillo-Aguirre, B.S.; Knapik, J.J. Soldier load carriage, injuries, rehabilitation and physical conditioning: An international approach. Int. J. Environ. Res. Public Health 2021, 18, 4010. [Google Scholar] [CrossRef]
- Johnston, M. At the Front Line: Experiences of Australian Soldiers in World War 2; Cambridge University Press: Cambridge, UK, 1996. [Google Scholar]
- Porter, S.C. The Soldier’s Load. In Infantry; U.S. Army Infantry School: Fort Benning, GA, USA, 1992; pp. 19–22. [Google Scholar]
- McKay, G. Delta Four: Australian Rifleman in Vietnam; Allen & Unwin: Crows Nest, QLD, Australia, 1996. [Google Scholar]
- Hastings, M.; Jenkins, S. The Battle for the Falklands; W W Norton & Coy: New York, NY, USA, 1983. [Google Scholar]
- Solgere, A.L. A soldier’s load revisited. In Marine Corps Gazette; Marine Corps Association: Quantico, VA, USA, 1999; pp. 35–36. [Google Scholar]
- Taylor, J. Last Out: 4 R.A.R./N. Z. (ANZAC) Battalion’s Second Tour in Vietnam; Allen & Unwin: Crows Nest, QLD, Australia, 2001. [Google Scholar]
- Gardner, H. Fighting Afghanistan’s Opium Dependency as a Means of Disrupting al Qaeda’s Illicit Funding. Master’s Thesis, Boston University, Boston, MA, USA, 2006. [Google Scholar]
- Brune, P. A Bastard of a Place: The Australians in Papua; Allen & Unwin: Crows Nest, QLD, Australia, 2003. [Google Scholar]
- Camp, D. Toktong Ridge runners—1st Battalion, 7th Marines. In Leatherneck; United States Marine Corps: Philadelphia, PA, USA, 2000; p. 40. [Google Scholar]
- Kraft, N.G. Lessons learned from a light infantry company during Operation Anaconda. Infantry 2002, 91, 28–31. [Google Scholar]
- Dean, C. Task Force Devil Combined Arms Assessment Team: The Modern Warrior’s Combat Load. In US Army Center for Army Lessons Learned; Center for Army Lessons Learned (CALL): Leavenworth County, KS, USA, 2003. [Google Scholar]
- Armstrong, N.C.; Izard, R. Reducing the burden on the dismounted soldier. J. Sci. Med. Sport 2017, 20, S148. [Google Scholar] [CrossRef]
- Bujold, A. The Dismounted Soldier: A Critical Analysis on the Associated Complications with Load Carriage System Design to Protect and Increase Survivability. Monarch. Work. Pap. Ser. 2023, 1–22. [Google Scholar]
- Lothian, N.V. The load carried by the soldier. J. R. Army Med. Corps 1921, 38, 448–458. [Google Scholar] [CrossRef]
- Marshall, S.L.A. The Soldier’s Load and the Mobility of a Nation; The Marine Corps Association: Quantico, VA, USA, 1980. [Google Scholar]
- Pal, M.S.; Majumdar, D.; Bhattacharyya, M.; Kumar, R.; Majumdar, D. Optimum load for carriage by soldiers at two walking speeds on level ground. Int. J. Ind. Ergon. 2009, 39, 68–72. [Google Scholar] [CrossRef]
- Patton, J.F.; Kaszuba, J.; Mello, R.P.; Reynolds, K.L. Physiological responses to prolonged treadmill walking with external loads. Eur. J. Appl. Physiol. Occup. Physiol. 1991, 63, 89–93. [Google Scholar] [CrossRef]
- Pederson, A.V.; Stokke, R.; Mamen, A. Effects of extra load position on energy expenditure in treadmill running. Eur. J. Appl. Physiol. 2007, 102, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Lyons, J.; Allsopp, A.; Bilzon, J. Influences of body composition upon the relative metabolic and cardiovascular demands of load-carriage. Occup. Med. Lond 2005, 55, 380–384. [Google Scholar] [CrossRef] [PubMed]
- Vaz, M.; Karaolis, N.; Draper, A.; Shetty, P. A compilation of energy costs of physical activities. Public Health Nutr. 2005, 8, 1153–1183. [Google Scholar] [CrossRef]
- Bilzon, J.; Allsopp, A.; Tipton, M.J. Assessment of physical fitness for occupations encompassing load-carriage tasks. Occup. Med. Lond 2001, 51, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Bhambhani, Y.; Maikala, R. Gender differences during treadmill walking with graded loads: Biomechanical and physiological comparisons. Eur. J. Appl. Physiol. 2000, 81, 75–83. [Google Scholar] [CrossRef]
- Bhambhani, Y.; Buckley, S.; Maikala, R. Physiological and biomechanical responses during treadmill walking with graded loads. Eur. J. Appl. Physiol. 1997, 76, 544–551. [Google Scholar] [CrossRef]
- Charteris, J.; Scott, P.A.; Nottrodt, J.W. Metabolic and kinematic responses of African women head loaded carriers under controlled conditions of load and speed. Ergonomics 1989, 32, 1539–1550. [Google Scholar] [CrossRef]
- Goslin, B.R.; Rorke, S.C. The perception of exertion during load carriage. Ergonomics 1986, 29, 677–686. [Google Scholar] [CrossRef]
- Pimental, N.; Shapiro, Y.; Pandolf, K.B. Comparison of uphill and downhill walking and concentric and eccentric cycling. Ergonomics 1982, 25, 373–380. [Google Scholar] [CrossRef]
- Robertson, R.J.; Caspersen, C.J.; Allison, T.G.; Skrinar, G.S.; Abbott, R.A.; Metz, K.E. Differentiated perceptions of exertion and energy cost of young women while carrying loads. Eur. J. Appl. Physiol. Occup. Physiol. 1982, 49, 69–78. [Google Scholar] [CrossRef]
- Datta, S.R.; Chatterjee, B.B.; Roy, B.N. Maximum permissible weight to be carried on the head by a male worker from Eastern India. J. Appl. Physiol. 1975, 38, 132–135. [Google Scholar] [CrossRef]
- Chung, M.K.; Lee, Y.J.; Lee, I.; Choi, K.I. Physiological workload evaluation of carrying soft drink beverage boxes on the back. Appl. Ergon. 2005, 36, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Samanta, A.; Chatterjee, B.B. Energy expenditure in manual load carriage. Ind. Health 1981, 19, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Engels, H.J.; Smith, C.R.; Wirth, J.C. Metabolic and hemodynamic responses to walking with shoulder-worn exercise weights: A brief report. Clin. J. Sport Med. 1995, 5, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Blacker, S.D.; Fallowfield, J.L.; Bilzon, J.L.J.; Willems, M.E.T. Physiological responses to load carriage during level and downhill treadmill walking. Med. Sport. 2009, 13, 116–124. [Google Scholar] [CrossRef]
- Larsson, J.; Dencker, M.; Bremander, A.; Olsson, M.C. Cardiorespiratory responses of load carriage in female and male soldiers. Appl. Ergon. 2022, 101, 103710. [Google Scholar] [CrossRef]
- Faghy, M.A.; Brown, P.I. Thoracic load carriage-induced respiratory muscle fatigue. Eur. J. Appl. Physiol. 2014, 114, 1085–1093. [Google Scholar] [CrossRef]
- Phillips, D.B.; Stickland, M.K.; Petersen, S.R. Ventilatory responses to prolonged exercise with heavy load carriage. Eur. J. Appl. Physiol. 2016, 116, 19–27. [Google Scholar] [CrossRef]
- Phillips, D.B.; Ehnes, C.M.; Stickland, M.K.; Petersen, S.R. The impact of thoracic load carriage up to 45 kg on the cardiopulmonary response to exercise. Eur. J. Appl. Physiol. 2016, 116, 1725–1734. [Google Scholar] [CrossRef]
- Orr, R.; Pope, R.; Johnston, V.; Coyle, J. Soldier self-reported reductions in task performance associated with operational load carriage. J. Aust. Strength Cond. 2013, 21, 39–46. [Google Scholar]
- Lewinski, W.J.; Dysterheft, J.L.; Dicks, N.D.; Pettitt, R.W. The influence of officer equipment and protection on short sprinting performance. Appl. Ergon. 2015, 47, 65–71. [Google Scholar] [CrossRef]
- Marins, E.F.; Cabistany, L.; Bartel, C.; Dawes, J.; Del Vecchio, F.B. Effects of personal protective equipment on the performance of federal highway policemen in physical fitness tests. J. Strength Cond. Res. 2020, 34, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.; Tan, M.; Tan, P. Effects of loaded march on marksmanship performance. J. Sci. Med. Sport 2017, 20, S176. [Google Scholar] [CrossRef]
- Gil-Cosano, J.; Orantes-Gonzalez, E.; Heredia-Jimenez, J. Effect of carrying different military equipment during a fatigue test on shooting performance. Eur. J. Sport Sci. 2019, 19, 186–191. [Google Scholar] [CrossRef]
- Jaworski, R.L.; Jensen, A.; Niederberger, B.; Congalton, R.; Kelly, K.R. Changes in combat task performance under increasing loads in active duty marines. Mil. Med. 2015, 180, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Giles, G.E.; Hasselquist, L.; Caruso, C.M.; Eddy, M.D. Load carriage and physical exertion influence cognitive control in military scenarios. Med. Sci. Sports Exerc. 2019, 51, 2540–2546. [Google Scholar] [CrossRef] [PubMed]
- Loverro, K.L.; Brown, T.N.; Coyne, M.E.; Schiffman, J.M. Use of body armor protection with fighting load impacts soldier performance and kinematics. Appl. Ergon. 2015, 46, 168–175. [Google Scholar] [CrossRef]
- Kelly, K.; Niederberger, B.; Givens, A.; Bernards, J.; Orr, R. Profiling injuries sustained following implementation of a progressive load carriage program in United States marine corps recruit training. Work 2024, 77, 1391–1399. [Google Scholar] [CrossRef]
- Knapik, J.J.; Reynolds, K.; Orr, R.; Pope, R. Load carriage-related paresthesias (Part 2): Meralgia paresthetica. J. Spec. Oper. Med. 2017, 17, 94–100. [Google Scholar] [CrossRef]
- Knapik, J.J.; Reynolds, K.; Orr, R.; Pope, R. Load carriage-related paresthesias: Part 1: Rucksack palsy and digitalgia paresthetica. J. Spec. Oper. Med. 2016, 16, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.I. A Greek Army on the March: Soldiers and Survival in Xenophon’s Anabasis; Cambridge University Press: New York, NY, USA, 2007. [Google Scholar]
- Knapik, J.J.; Harman, E.A.; Steelman, R.A.; Graham, B.S. A systematic review of the effects of physical training on load carriage performance. J. Strength Cond. Res. 2012, 26, 585–597. [Google Scholar] [CrossRef]
- Renatus, F. Vegetius: Epitome of Military Science, 2nd ed.; Liverpool University Press: Liverpool, UK, 1996. [Google Scholar]
- Schram, B.; Orr, R.; Niederberger, B.; Givens, A.; Bernards, J.; Kelly, K.R. Cardiovascular Demand Differences Between Male and Female US Marine Recruits During Progressive Loaded Hikes. J. Strength Cond. Res. 2024, 38, e454–e458. [Google Scholar] [CrossRef]
- Kucera, K.L.; Marshall, S.W.; Wolf, S.H.; Padua, D.A.; Cameron, K.L.; Beutler, A.I. Association of injury history and incident injury in cadet basic military training. Med. Sci. Sports Exerc. 2016, 48, 1053. [Google Scholar] [CrossRef]
- Birrell, S.A.; Hooper, R.H. Initial subjective load carriage injury data collected with interviews and questionnaires. Mil. Med. 2007, 172, 306–311. [Google Scholar] [CrossRef]
- Gibson, N.; Drain, J.R.; Larsen, P.; Michael, S.; Groeller, H.; Sampson, J.A. A comprehensive analysis of injuries during army basic military training. Mil. Med. 2024, 189, 652–660. [Google Scholar] [CrossRef]
- Schram, B.; Canetti, E.; Orr, R.; Pope, R. Injury rates in female and male military personnel: A systematic review and meta-analysis. BMC Women’s Health 2022, 22, 310. [Google Scholar] [CrossRef]
- Heagerty, R.; Sharma, J.; Clayton, J.L. A retrospective analysis of five years musculoskeletal injury data in British infantry recruits. Ann. Musculoskelet. Med. 2017, 2, 032–038. [Google Scholar] [CrossRef]
- Hall, N.; Constantinou, M.; Brown, M.; Beck, B.; Kuys, S. Prevalence of musculoskeletal injuries in New Zealand Army recruits as defined by physical therapy service presentations. Mil. Med. 2022, 187, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Stannard, J.; Finch, C.; Dabovich, P.; Fortington, L. Musculoskeletal Injury in Australian Infantry Personnel: A Cross-sectional Study to Understand Prevention Priorities. Mil. Med. 2025, 190, e682–e689. [Google Scholar] [CrossRef]
- Roy, T.C.; Faller, T.N.; Richardson, M.D.; Taylor, K.M. Characterization of limited duty neuromusculoskeletal injuries and return to duty times in the US Army during 2017–2018. Mil. Med. 2022, 187, e368–e376. [Google Scholar] [CrossRef] [PubMed]
- Grimm, P.D.; Mauntel, T.C.; Potter, B.K. Combat and noncombat musculoskeletal injuries in the US military. Sports Med. Arthrosc. 2019, 27, 84–91. [Google Scholar] [CrossRef]
- Alcover, K.C.; Howard, K.; Poltavskiy, E.; Derminassian, A.D.; Nickel, M.S.; Allard, R.J.; Dao, B.; Stewart, I.J.; Howard, J.T. Disease and non-battle injury in deployed military: A systematic review and meta-analysis. Mil. Med. 2024, 189, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Saleby, M.; Ahlinder, L.; Schüler, M.; Taube, F. Descriptive analysis of diseases, non-battle injuries and climate among deployed Swedish military personnel. BMJ Mil. Health 2024, 1–5. [Google Scholar] [CrossRef]
- Hayhurst, D.; Warner, M.; Stokes, M.; Fallowfield, J. Musculoskeletal injury in military specialists: A 2-year retrospective study. BMJ Mil. Health 2024, 170, 242–247. [Google Scholar] [CrossRef]
- Stannard, J.; Fortington, L. Musculoskeletal injury in military special operations forces: A systematic review. BMJ Mil. Health 2021, 167, 255–265. [Google Scholar] [CrossRef]
- Dresti, S.; Mellino, E.; Palazzo, M.; Solidoro, M.; Orr, R. Profiling” Noncombat” Musculoskeletal Injuries in Special Operations Forces: A Systematic Review. J. Spec. Oper. Med. 2025, 25, 96–111. [Google Scholar] [CrossRef]
- Hotaling, B.; Theiss, J.; Cohen, B.; Wilburn, K.; Emberton, J.; Westrick, R. Self-reported musculoskeletal injury healthcare-seeking behaviors in US Air Force special warfare personnel. J. Spec. Oper. Med. 2021, 21, 72–77. [Google Scholar] [CrossRef]
- Wolski, L.; Stannard, J.; Toohey, L.; Fogarty, A.; Drew, M. Musculoskeletal complaint epidemiology in Australian special operation forces trainees. Mil. Med. 2023, 188, e3539–e3546. [Google Scholar] [CrossRef]
- Dijksma, I.; Zimmermann, W.; Hertenberg, E.; Lucas, C.; Stuiver, M. One out of four recruits drops out from elite military training due to musculoskeletal injuries in the Netherlands Armed Forces. BMJ Mil. Health 2022, 168, 136–140. [Google Scholar] [CrossRef]
- Orr, R.; Johnston, V.; Coyle, J.; Pope, R. Reported load carriage injuries of the Australian Army soldier. J. Occup. Rehabil. 2015, 25, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Hauschild, V.; Roy, T.; Grier, T.; Schuh, A.; Jones, B. Foot Marching, Load Carriage, and Injury Risk; Technical Information Paper No. 12-054-0616; Army Public Health Center: Aberdeen Proving Ground, MD, USA, 2016. [Google Scholar]
- Orr, R.; Coyle, J.; Johnston, V.; Pope, R. Self-reported load carriage injuries of military soldiers. Int. J. Inj. Control Saf. Promot. 2016, 24, 1–9. [Google Scholar] [CrossRef]
- Fox, B.D.; Judge, L.W.; Dickin, D.C.; Wang, H. Biomechanics of military load carriage and resulting musculoskeletal injury: A review. J. Orthop. Surg. 2020, 1, 6–11. [Google Scholar]
- Hoffman, J.R.; Church, D.D.; Hoffman, M.W. Overuse Injuries in Military Personnel. In The Mechanobiology and Mechanophysiology of Military-Related Injuries. Studies in Mechanobiology, Tissue Engineering and Biomaterials; Gefen, A., Epstein, Y., Eds.; Springer: Cham, Switzerland, 2015; Volume 19. [Google Scholar] [CrossRef]
- Knapik, J.; Johnson, R.; Ang, P.; Meiselman, H.; Bensel, C.; Johnson, W.; Flynn, B.; Hanlon, W.; Kirk, J.; Harman, E.; et al. Road March Performance of Special Operations Soldiers Carrying Various Loads and Load Distributions; T14-93; Military Performance Division, US Army Research Institute of Environmental Medicine: Natick, MA, USA, 1993. [Google Scholar]
- Reynolds, K.; White, J.; Knapik, J.; Witt, C.; Amoroso, P. Injuries and risk factors in a 100-mile (161-km) infantry road march. Prev. Med. 1999, 28, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Knapik, J.J.; Reynolds, K.L.; Staab, J.; Vogel, J.A.; Jones, B. Injuries associated with strenuous road marching. Mil. Med. 1992, 157, 64–67. [Google Scholar] [CrossRef]
- Knapik, J.J.; Reynolds, K.L.; Barson, J. Risk factors for foot blisters during road marching: Tobacco use, ethnicity, foot type, previous illness, and other factors. Mil. Med. 1999, 164, 92–97. [Google Scholar] [CrossRef]
- Bush, R.A.; Brodine, S.; Shaffer, R. The Association of Blisters with Musculoskeletal Injuries in Male Marine Recruits. J. Am. Podiatr. Med. Assoc. 2000, 90, 194–198. [Google Scholar] [CrossRef]
- Spiezia, F.; Oliva, F.; Maffulli, N. Loaded marches: The military safe and effective tool to combat readiness. Br. Med. Bull. 2025, 154, ldaf005. [Google Scholar] [CrossRef] [PubMed]
- McShea, J.P.; Powell, J.E.; Dolomisiewicz, E.A.; Pasquina, P.F.; Miller, M.E. Isolated mononeuropathy from rucksack palsy: A case series. Mil. Med. 2021, 186, e1043–e1047. [Google Scholar] [CrossRef] [PubMed]
- Massey, E.W. Digitalgia paresthetica in the foot. JAMA 1978, 239, 1393–1394. [Google Scholar] [CrossRef] [PubMed]
- DePrado, M.; Cuervas-Mons, M.; Golano, P.; Rabat, E.; Vaquero, J. The tarsal tunnel syndrome. FuB Sprunggelenk 2015, 13, 227–236. [Google Scholar] [CrossRef]
- Ahmad, M.; Tsang, K.; MacKenney, P.J.; Adedapo, A.O. Tarsal tunnel syndrome: A literature review. Foot Ankle Surg. 2012, 18, 149–152. [Google Scholar] [CrossRef]
- Boulware, D.R. Backpacking-Induced Paresthesias. Wilderness Environ. Med. 2003, 14, 161–166. [Google Scholar] [CrossRef]
- Henderson, K.K.; Parker, J.; Heinking, K.P. Mountaineering-induced bilateral plantar paresthesia. J. Osteopath. Med. 2014, 114, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Fargo, M.V.; Konitzer, L.N. Meralgia Paresthetic due to Body Armor Wear in U.S. Soldiers Serving in Iraq: A Case Report and Review of the Literature. Mil. Med. 2007, 172, 663–665. [Google Scholar] [CrossRef] [PubMed]
- Sanders, B.; Nemeth, W.C. Hip and Thigh Injuries. In Athletic Injuries and Rehabilitation; Zachazewski, J.E., Magee, D.J., Quillen, W.S., Eds.; W.B. Saunders: Philadelphia, PA, USA, 1996. [Google Scholar]
- Makela, J.P.; Ramstad, R.; Mattila, V.; Pihlajamaki, H. Brachial plexus lesions after backpack carriage in young adults. Clin. Orthop. Relat. Res. 2006, 452, 205–209. [Google Scholar] [CrossRef]
- Charteris, J. Load stress; a carrier strain: Implications for military and recreational backpacking. Ergonomics 2000, 1, 25–47. [Google Scholar]
- Knapik, J.J.; Reynolds, K.L.; Harman, E. Soldier load carriage: Historical, physiological, biomechanical, and medical aspects. Mil. Med. 2004, 169, 45–56. [Google Scholar] [CrossRef]
- Wilson, W.J. Brachial Plexus Palsy in Basic Trainees. Mil. Med. 1987, 152, 519–522. [Google Scholar] [CrossRef]
- Kawabata, H. Brachial plexus palsy. In Brachial Plexus Palsy; Kawai, H., Kawabata, H., Eds.; World Scientific: Singapore, 2000; pp. 31–64. [Google Scholar]
- Hadid, A.; Belzer, N.; Shabshin, N.; Epstein, Y.; Gefen, A. Deformations in the shoulder tissues during load carriage: A computational model. J. Strength Cond. Res. 2015, 29, S144–S148. [Google Scholar] [CrossRef]
- LaFiandra, M.E.; Harman, E. The distribution of forces between the upper and lower back during load carriage. Med. Sci. Sports Exerc. 2004, 36, 460–467. [Google Scholar] [CrossRef]
- Bessen, R.J.; Belcher, V.W.; Franklin, R.J. Rucksack Paralysis with and Without Rucksack Frames. Mil. Med. 1987, 152, 372–375. [Google Scholar] [CrossRef]
- Pester, S.; Smith, P.C. Stress fractures in lower extremities of soldiers in basic training. Orthop. Rev. 1992, 21, 297–303. [Google Scholar]
- van Dijk, J. Chapter 3—Common Military Task: Marching. In Optimizing Operational Physical Fitness. RTO-TR-HFM-080; NATO Research and Technology Organisation: Brussels, Belgium, 2009. [Google Scholar]
- Milgrom, C.; Giladi, M.; Stein, M.; Kashtan, H.; Margulies, J.Y.; Chisin, R.; Steinberg, R.; Aharonson, Z. Stress fractures in military recruits. J. Bone Joint Surg. 1985, 67, 732–735. [Google Scholar] [CrossRef] [PubMed]
- Greaney, R.B.; Gerber, F.H.; Laughlin, R.L.; Kmet, J.P.; Metz, C.D.; Kilchenski, T.S.; Rama Rao, B.; Silverman, E.D. Distribution and Natural History of Stress Fractures in U.S. Marine Recruits. Radiology 1983, 146, 339–346. [Google Scholar] [CrossRef]
- Kelly, E.; Jonson, S.; Cohen, M.; Shaffer, R. Stress fractures of the pelvis in female Navy recruits: An analysis of possible mechanisms of injury. Mil. Med. 2000, 165, 142–146. [Google Scholar] [CrossRef]
- Holt, K.G.; Wagenaar, R.C.; Kubo, M.; LaFiandra, M.E.; Obusek, J.P. Modulation of force transmission to the head while carrying a backpack load at different walking speeds. J. Biomech. 2005, 38, 569–574. [Google Scholar] [CrossRef]
- Orr, R.M.; Pope, R. Gender differences in load carriage injuries of Australian Army soldiers. BMC Musculoskelet. Disord. 2016, 17, 1–8. [Google Scholar] [CrossRef]
- Pope, R. Prevention of pelvic stress fractures in female army recruits. Mil. Med. 1999, 164, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Rome, K.; Handoll, H.H.G.; Ashford, R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst. Rev. 2005, 2, CD000450. [Google Scholar] [CrossRef]
- Nordin, M.; Frankel, V.H. Basic Biomechanics of the Musculoskeletal System, 3rd ed.; Lippincott, Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Ross, R.A. Stress fractures in Royal Marine recruits. Mil. Med. 2002, 167, 560–565. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, F. Injuries during Marine Corps officer basic training. Mil. Med. 2000, 165, 515–520. [Google Scholar] [CrossRef]
- Wooldridge, J.D.; Schilling, B.K.; Young, D.L.; Radzak, K.N. Musculoskeletal injury concealment in the Reserve Officers’ training corps: A survey of cadets’ reporting behaviors. Mil. Med. 2023, 188, e3522–e3531. [Google Scholar] [CrossRef]
- Smith, L.; Westrick, R.; Sauers, S.; Cooper, A.; Scofield, D.; Claro, P.; Warr, B. Underreporting of musculoskeletal injuries in the US Army: Findings from an infantry brigade combat team survey study. Sports Health 2016, 8, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Cohen, B.S.; Pacheco, B.M.; Foulis, S.A.; Canino, M.C.; Redmond, J.E.; Westrick, R.B.; Hauret, K.G.; Sharp, M.A. Surveyed reasons for not seeking medical care regarding musculoskeletal injury symptoms in US Army trainees. Mil. Med. 2019, 184, e431–e439. [Google Scholar] [CrossRef]
- Sauers, S.E.; Smith, L.B.; Scofield, D.E.; Cooper, A.; Warr, B.J. Self-management of unreported musculoskeletal injuries in a US Army brigade. Mil. Med. 2016, 181, 1075–1080. [Google Scholar] [CrossRef]
- Elliman, T.D.; Cohen, B.S.; Heaton, K.J.; Proctor, S.P. Physical injuries, treatment-seeking, and perceived barriers to treatment in US Army Drill Sergeants. Mil. Med. 2022, 187, 1403–1411. [Google Scholar] [CrossRef]
- Dartt, C.E.; Gregory, A.B.; de la Motte, S.J.; Ricker, E.A. Determinants of Medical Care-Seeking Behavior for Musculoskeletal Conditions During US Marine Corps Training: A Thematic Analysis. J. Athl. Train. 2024, 59, 1203–1212. [Google Scholar] [CrossRef]
- Campbell, P.; Pope, R.; Simas, V.; Canetti, E.; Schram, B.; Orr, R. The effects of early physiotherapy treatment on musculoskeletal injury outcomes in military personnel: A narrative review. Int. J. Environ. Res. Public Health 2022, 19, 13416. [Google Scholar] [CrossRef]
- Rhon, D.I.; Fraser, J.J.; Sorensen, J.; Greenlee, T.A.; Jain, T.; Cook, C.E. Delayed rehabilitation is associated with recurrence and higher medical care use after ankle sprain injuries in the United States military health system. J. Orthop. Sports Phys. Ther. 2021, 51, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Feigel, E.D.; Sterczala, A.J.; Krajewski, K.T.; Sekel, N.M.; Lovalekar, M.; Peterson, P.A.; Koltun, K.J.; Flanagan, S.D.; Connaboy, C.; Martin, B.J.; et al. Physiological characteristics predictive of passing military physical employment standard tasks for ground close combat occupations in men and women. Eur. J. Sport Sci. 2024, 24, 1247–1259. [Google Scholar] [CrossRef]
- Robinson, J.; Roberts, A.; Irving, S.; Orr, R. Aerobic Fitness is of Greater Importance Than Strength and Power in the Load Carriage Performance of Specialist Police. Int. J. Exerc. Sci. 2018, 11, 987–998. [Google Scholar] [CrossRef] [PubMed]
- MacInnis, M.J.; Gibala, M.J. Physiological adaptations to interval training and the role of exercise intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef]
- Wen, D.; Utesch, T.; Wu, J.; Robertson, S.; Liu, J.; Hu, G.; Chen, H. Effects of different protocols of high intensity interval training for VO2max improvements in adults: A meta-analysis of randomised controlled trials. J. Sci. Med. Sport. 2019, 22, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Swinton, P.A.; Schoenfeld, B.J.; Murphy, A. Dose–response modelling of resistance exercise across outcome domains in strength and conditioning: A meta-analysis. Sports Med. 2024, 54, 1579–1594. [Google Scholar] [CrossRef] [PubMed]
- Iversen, V.M.; Norum, M.; Schoenfeld, B.J.; Fimland, M.S. No time to lift? Designing time-efficient training programs for strength and hypertrophy: A narrative review. Sports Med. 2021, 51, 2079–2095. [Google Scholar] [CrossRef] [PubMed]
- Orr, R.M.; Robinson, J.; Hasanki, K.; Talaber, K.A.; Schram, B.; Roberts, A. The relationship between strength measures and task performance in specialist tactical police. J. Strength Cond. Res. 2022, 36, 757–762. [Google Scholar] [CrossRef]
- Molloy, J.M.; Pendergrass, T.L.; Lee, I.E.; Chervak, M.C.; Hauret, K.G.; Rhon, D.I. Musculoskeletal injuries and United States Army readiness part I: Overview of injuries and their strategic impact. Mil. Med. 2020, 185, e1461–e1471. [Google Scholar] [CrossRef]
- Schleip, R. Chapter 11. Mechanotransduction: From the cellular level to the whole body. In Textbook Osteopathic Medicine: Textbook Osteopathic Medicine; Mayer, J., Standen, C., Eds.; Elsevier Health Sciences: Philadelphia, PA, USA, 2018. [Google Scholar]
- Segreti, A.; Fossati, C.; Mulè, M.T.; Fanale, V.; Crispino, S.P.; Coletti, F.; Parisi, F.R.; Zampogna, B.; Vasta, S.; Mannacio, E. Assessment of cardiopulmonary capacity in deconditioned athletes because of knee injury. J. Sports Med. Phys. Fit. 2024, 64, 615–623. [Google Scholar] [CrossRef]
- Talbot, L.A.; Brede, E.; Metter, E.J. Influence of self-managed rehabilitation on work efficiency in active duty military with a knee injury. Mil. Med. 2021, 186, 486–492. [Google Scholar] [CrossRef]
- Mala, J.; Szivak, T.K.; Flanagan, S.D.; Comstock, B.A.; Laferrier, J.Z.; Maresh, C.M.; Kraemer, W.J. The role of strength and power during performance of high intensity military tasks under heavy load carriage. US Army Med. Dep. J. 2015, 2015, 3–11. [Google Scholar]
- Kraemer, W.J.; Vescovi, J.D.; Volek, J.S.; Nindl, B.C.; Newton, R.U.; Patton, J.F.; Dziados, J.E.; French, D.N.; Häkkinen, K. Effects of concurrent resistance and aerobic training on load-bearing performance and the army physical fitness test. Mil. Med. 2004, 169, 994–999. [Google Scholar] [CrossRef]
- Kraemer, W.; Mazzetti, S.; Nindl, B.C.; Gotshalk, L.; Volek, J.; Marx, J.; Dohi, K.; Gomez, P.S.; Miles, M.; Fleck, J.; et al. Effect of resistance training on women’s strength/power and occupational performances. Med. Sci. Sports Exerc. 2001, 33, 1011–1025. [Google Scholar] [CrossRef]
- Orr, R.; Knapik, J.; Pope, R. Avoiding Program-Induced Cumulative Overlead (PICO). J. Spec. Oper. Med. 2016, 16, 61–64. [Google Scholar] [CrossRef]
- Milgrom, C.; Finestone, A.S. The effect of stress fracture interventions in a single elite infantry training unit (1983–2015). Bone 2017, 103, 125–130. [Google Scholar] [CrossRef]
- Bulmer, S.; Drain, J.R.; Tait, J.L.; Corrigan, S.L.; Gastin, P.B.; Aisbett, B.; Rantalainen, T.; Main, L.C. Quantification of recruit training demands and subjective wellbeing during basic military training. Int. J. Environ. Res. Public Health 2022, 19, 7360. [Google Scholar] [CrossRef]
- Maupin, D.; Schram, B.; Orr, R. Tracking training load and its implementation in tactical populations: A narrative review. Strength Cond. J. 2019, 41, 1–11. [Google Scholar] [CrossRef]
- Kaikkonen, P. Post-exercise heart rate variability: A new approach to evaluation of exercise-induced physiological training load. In Studies in Sport, Physical Education and Health; University of Jyväskylä: Jyväskylä, Finland, 2015. [Google Scholar]
- Tomes, C.D.; Canetti, E.F.; Schram, B.; Orr, R. Ultra-short-term versus short-term measures of heart rate variability in specialist police units: A pilot reliability study. Physiol. Rep. 2025, 13, e70182. [Google Scholar] [CrossRef]
- Moore, E.; Fuller, J.T.; Buckley, J.D.; Saunders, S.; Halson, S.L.; Broatch, J.R.; Bellenger, C.R. Impact of cold-water immersion compared with passive recovery following a single bout of strenuous exercise on athletic performance in physically active participants: A systematic review with meta-analysis and meta-regression. Sports Med. 2022, 52, 1667–1688. [Google Scholar] [CrossRef]
- Higgins, T.; Cameron, M.; Climstein, M. Evaluation of passive recovery, cold water immersion, and contrast baths for recovery, as measured by game performances markers, between two simulated games of rugby union. J. Strength Cond. Res. 2022. [Google Scholar] [CrossRef]
- Chen, R.; Ma, X.; Ma, X.; Cui, C. The effects of hydrotherapy and cryotherapy on recovery from acute post-exercise induced muscle damage—A network meta-analysis. BMC Musculoskelet. Disord. 2024, 25, 749. [Google Scholar] [CrossRef] [PubMed]
- Brown, F.; Gissane, C.; Howatson, G.; Van Someren, K.; Pedlar, C.; Hill, J. Compression garments and recovery from exercise: A meta-analysis. Sports Med. 2017, 47, 2245–2267. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Frey, B.; Day, C. Development and validation of a military fear avoidance questionnaire. Front. Rehabil. Sci. 2022, 3, 979776. [Google Scholar] [CrossRef] [PubMed]
- Fountaine, C.J. Shareable Resource: Ten Training Principles to Guide Exercise Prescription. ACSM’s Health Fit. J. 2024, 28, 88. [Google Scholar] [CrossRef]
- Vickery-Howe, D.M.; Drain, J.R.; Clarke, A.C.; Dascombe, B.J.; Hoolihan, B.; Middleton, K.J. The effect of weapon handling during load carriage across a range of military-relevant walking speeds. Ergonomics 2024, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Orr, R.; Pope, R.; Johnston, V.; Coyle, J. Load carriage: Minimising soldier injuries through physical conditioning-A narrative review. J. Mil. Veterans Health 2010, 18, 31–38. [Google Scholar]
- Mala, J.; Szivak, T.K.; Kraemer, W.J. Improving performance of heavy load carriage during high-intensity combat-related tasks. Strength Cond. J. 2015, 37, 43–52. [Google Scholar]
- Boffey, D.; Harat, I.; Gepner, Y.; Frosti, C.L.; Funk, S.; Hoffman, J.R. The physiology and biomechanics of load carriage performance. Mil. Med. 2019, 184, e83–e90. [Google Scholar] [CrossRef]
- Faghy, M.A.; Shei, R.J.; Armstrong, N.C.; White, M.; Lomax, M. Physiological impact of load carriage exercise: Current understanding and future research directions. Physiol. Rep. 2022, 10, e15502. [Google Scholar] [CrossRef]
- Beekley, M.D.; Alt, J.; Buckley, C.M.; Duffey, M. Effects of heavy load carriage during constant-speed, simulated, road marching. Mil. Med. 2007, 172, 592–595. [Google Scholar] [CrossRef]
- Chatterjee, S.; Chatterjee, T.; Bhattacharyya, D.; Sen, S.; Pal, M. Effect of heavy load carriage on cardiorespiratory responses with varying gradients and modes of carriage. Mil. Med. Res. 2018, 5, 1–7. [Google Scholar] [CrossRef]
- Pal, M.S.; Majumdar, D.; Pramanik, A.; Chowdhury, B.; Majumdar, D. Optimum load for carriage by Indian soldiers on different uphill gradients at specified walking speed. Int. J. Ind. Ergon. 2014, 44, 260–265. [Google Scholar] [CrossRef]
- Fox, A.J.; Wanivenhaus, F.; Burge, A.J.; Warren, R.F.; Rodeo, S.A. The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat. 2015, 28, 269–287. [Google Scholar] [CrossRef] [PubMed]
- Stemper, B.D.; Pintar, F.A.; Baisden, J.L. Lumbar spine injury biomechanics. In Accidental Injury: Biomechanics and Prevention; Springer: New York, NY, USA, 2015; pp. 451–470. [Google Scholar]
- Anderson, M.; Grier, T.; Canham-Chervak, M.; Bushman, T.; Jones, B.H. Occupation and other risk factors for injury among enlisted US Army Soldiers. Public Health 2015, 129, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Sarah, J.; Gribbin, T.; Lisman, P.; Murphy, K.; Deuster, P. Systematic review of the association between physical fitness and musculoskeletal injury risk: Part 2—Muscular endurance and muscular strength. J. Strength Cond. Res. 2017, 31, 3218–3234. [Google Scholar] [CrossRef] [PubMed]
- Rappole, C.; Grier, T.; Anderson, M.K.; Hauschild, V.; Jones, B.H. Associations of age, aerobic fitness, and body mass index with injury in an operational Army brigade. J. Sci. Med. Sport 2017, 20, S45–S50. [Google Scholar] [CrossRef]
- Jones, B.H.; Hauret, K.G.; Dye, S.K.; Hauschild, V.D.; Rossi, S.P.; Richardson, M.D.; Friedl, K.E. Impact of physical fitness and body composition on injury risk among active young adults: A study of Army trainees. J. Sci. Med. Sport 2017, 20, S17–S22. [Google Scholar] [CrossRef]
- Leyk, D.; Rohde, U.; Erley, O.; Gorges, W.; Wunderlich, M.; Ruther, T.; Essfeld, D. Recovery of hand grip strength and hand steadiness after exhausting manual stretcher carriage. Eur. J. Appl. Physiol. 2006, 96, 593–599. [Google Scholar] [CrossRef]
- Leyk, D.; Rohde, U.; Erley, O.; Gorges, W.; Essfeld, D.; Erren, T. Maximal manual stretcher carriage: Performance and recovery of male and female ambulance workers. Ergonomics 2007, 50, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Blacker, S.; Fallowfield, J.; Bilzon, J.; Willems, M. Neuromuscular Function Following Prolonged Load Carriage on Level and Downhill Gradients. Aviat. Space Environ. Med. 2010, 81, 745–753. [Google Scholar] [CrossRef]
- Harman, E.A.; Gutekunst, D.J.; Frykman, P.N.; Sharp, M.A.; Nindl, B.C.; Alemany, J.A.; Mello, R.P. Prediction of simulated battlefield physical performance from field-expedient tests. Mil. Med. 2008, 173, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Washif, J.A.; Kok, L.-Y. Relationships between vertical jump metrics and sprint performance, and qualities that distinguish between faster and slower sprinters. J. Sci. Sport Exerc. 2022, 4, 135–144. [Google Scholar] [CrossRef]
- Pihlainen, K.; Santtila, M.; Häkkinen, K.; Kyröläinen, H. Associations of physical fitness and body composition characteristics with simulated military task performance. J. Strength Cond. Res. 2018, 32, 1089–1098. [Google Scholar] [CrossRef]
- Hydren, J.R.; Borges, A.S.; Sharp, M.A. Systematic review and meta-analysis of predictors of military task performance: Maximal lift capacity. J. Strength Cond. Res. 2017, 31, 1142–1164. [Google Scholar] [CrossRef] [PubMed]
- Jukic, I.; García-Ramos, A.; Baláš, J.; Malecek, J.; Omcirk, D.; Tufano, J.J. Ergogenic effects of lifting straps on movement velocity, grip strength, perceived exertion and grip security during the deadlift exercise. Physiol. Behav. 2021, 229, 113283. [Google Scholar] [CrossRef]
- Sternäng, O.; Reynolds, C.A.; Finkel, D.; Ernsth-Bravell, M.; Pedersen, N.L.; Dahl Aslan, A.K. Factors associated with grip strength decline in older adults. Age Ageing 2015, 44, 269–274. [Google Scholar] [CrossRef]
- Reilly, T.; Olinek, S. Predicting casualty evacuation performance for the Canadian land forces command. Occup. Ergon. 2013, 11, 1–9. [Google Scholar] [CrossRef]
- Vaara, J.P.; Groeller, H.; Drain, J.; Kyröläinen, H.; Pihlainen, K.; Ojanen, T.; Connaboy, C.; Santtila, M.; Agostinelli, P.; Nindl, B.C. Physical training considerations for optimizing performance in essential military tasks. Eur. J. Sport Sci. 2022, 22, 43–57. [Google Scholar] [CrossRef]
- Williford, H.N.; Duey, W.J.; Olson, M.S.; Howard, R.; Wang, N. Relationship between fire fighting suppression tasks and physical fitness. Ergonomics 1999, 42, 1179–1186. [Google Scholar] [CrossRef]
- Botta, W.C.; Franchini, E.; Gabriel-Costa, D.; Campos, F.A. Physical tests to predict combat task performance among Brazilian air force infantry cadets. Mil. Med. 2023, 188, 3095–3101. [Google Scholar] [CrossRef] [PubMed]
- Treloar, A.K.L.; Billing, D.C. Effect of load carriage on performance of an explosive, anaerobic military task. Mil. Med. 2011, 176, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Silk, A.J.; Billing, D.C. Development of a valid simulation assessment for a military dismounted assault task. Mil. Med. 2013, 178, 315–320. [Google Scholar] [CrossRef]
- Hunt, A.P.; Tofari, P.J.; Billing, D.C.; Silk, A.J. Tactical combat movements: Inter-individual variation in performance due to the effects of load carriage. Ergonomics 2016, 59, 1232–1241. [Google Scholar] [CrossRef]
- Larsson, J.; Olsson, M.C.; Bremander, A.; Dencker, M. Physiological demands and characteristics of movement during simulated combat. Mil. Med. 2023, 188, 3496–3505. [Google Scholar] [CrossRef]
- Department of Army. Sniper Training: Field Manual 23-10; Headquarters, Department of the Army: Washington, DC, USA, 1994. [Google Scholar]
- Coulacoglou, C.; Saklofske, D.H. Executive function, theory of mind, and adaptive behavior. In Psychometrics and Psychological Assessment; Elsevier: Amsterdam, The Netherlands, 2017; pp. 91–130. [Google Scholar]
- Hepdarcan, I.; Can, S. Psychometric characteristics of the n-back task: Construct validity across age and stimulus type, internal consistency, test-retest and alternate forms reliability. Curr. Psychol. 2025, 44, 2050–2059. [Google Scholar] [CrossRef]
- Maraj, C.S.; Lackey, S.J.; Badillo-Urquiola, K.A.; Hudson, I.L. Assessment of Kim’s game strategy for behavior cue detection: Engagement, flow, & performance aspects. In Proceedings of the International Conference on Virtual, Augmented and Mixed Reality, Toronto, ON, Canada, 17–22 July 2016; pp. 156–163. [Google Scholar]
- Lu, J.; Kobelsky, E.; Fung, J.; Sogomonian, T.; Edger-Lacoursière, Z.; Nedelec, B. Rehabilitation Interventions for Fear Avoidance Beliefs and Behaviors in Sudden Onset Musculoskeletal Conditions: A Scoping Review. J. Burn Care Res. 2025, 46, 620–641. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orr, R.; Knapik, J.J.; Rodgers, R.; Cassidy, R.; Rousseau, J.; Van Tiggelen, D.; Pope, R. Rehabilitating Soldiers for Load Carriage Tasks: An International Perspective. Int. J. Environ. Res. Public Health 2025, 22, 1286. https://doi.org/10.3390/ijerph22081286
Orr R, Knapik JJ, Rodgers R, Cassidy R, Rousseau J, Van Tiggelen D, Pope R. Rehabilitating Soldiers for Load Carriage Tasks: An International Perspective. International Journal of Environmental Research and Public Health. 2025; 22(8):1286. https://doi.org/10.3390/ijerph22081286
Chicago/Turabian StyleOrr, Robin, Joseph J. Knapik, Rachel Rodgers, Robyn Cassidy, Jacques Rousseau, Damien Van Tiggelen, and Rodney Pope. 2025. "Rehabilitating Soldiers for Load Carriage Tasks: An International Perspective" International Journal of Environmental Research and Public Health 22, no. 8: 1286. https://doi.org/10.3390/ijerph22081286
APA StyleOrr, R., Knapik, J. J., Rodgers, R., Cassidy, R., Rousseau, J., Van Tiggelen, D., & Pope, R. (2025). Rehabilitating Soldiers for Load Carriage Tasks: An International Perspective. International Journal of Environmental Research and Public Health, 22(8), 1286. https://doi.org/10.3390/ijerph22081286







